Troubleshooting Low Accuracy in Microbiological Method Verification: A Strategic Guide for Researchers
This article provides a comprehensive guide for researchers and drug development professionals facing challenges with low accuracy during microbiological method verification.
Troubleshooting Low Accuracy in Microbiological Method Verification: A Strategic Guide for Researchers
Abstract
This article provides a comprehensive guide for researchers and drug development professionals facing challenges with low accuracy during microbiological method verification. It covers foundational principles from ISO, USP, and CLSI standards, explores methodological applications for qualitative and quantitative assays, details a systematic troubleshooting protocol to diagnose and correct accuracy issues, and outlines validation strategies to demonstrate method comparability and robustness. By integrating regulatory requirements with practical solutions, this guide aims to equip scientists with the knowledge to ensure data reliability, regulatory compliance, and patient safety.
Understanding Method Verification: Principles, Standards, and Common Pitfalls
Core Definitions: Verification vs. Validation
In pharmaceutical and clinical laboratory sciences, verification and validation are distinct but complementary processes essential for ensuring method and test reliability.
Verification confirms through objective evidence that specified requirements have been fulfilled. In laboratory practice, this means demonstrating that a method or test system performs according to its pre-defined specifications in your specific environment. For example, a laboratory performing CLIA-waived tests must verify that the test performs as stated by the manufacturer before implementing it for patient testing [1].
Validation establishes through objective evidence that a process consistently produces a result meeting its predetermined specifications and quality attributes. Validation provides a higher degree of assurance and is required for laboratory-developed tests (LDTs) or methods that are modified or created within the laboratory. For Rapid Microbiological Methods (RMMs), validation demonstrates the method is accurate, precise, specific, and robust for its intended purpose, proving equivalency or superiority to traditional compendial methods [2] [3].
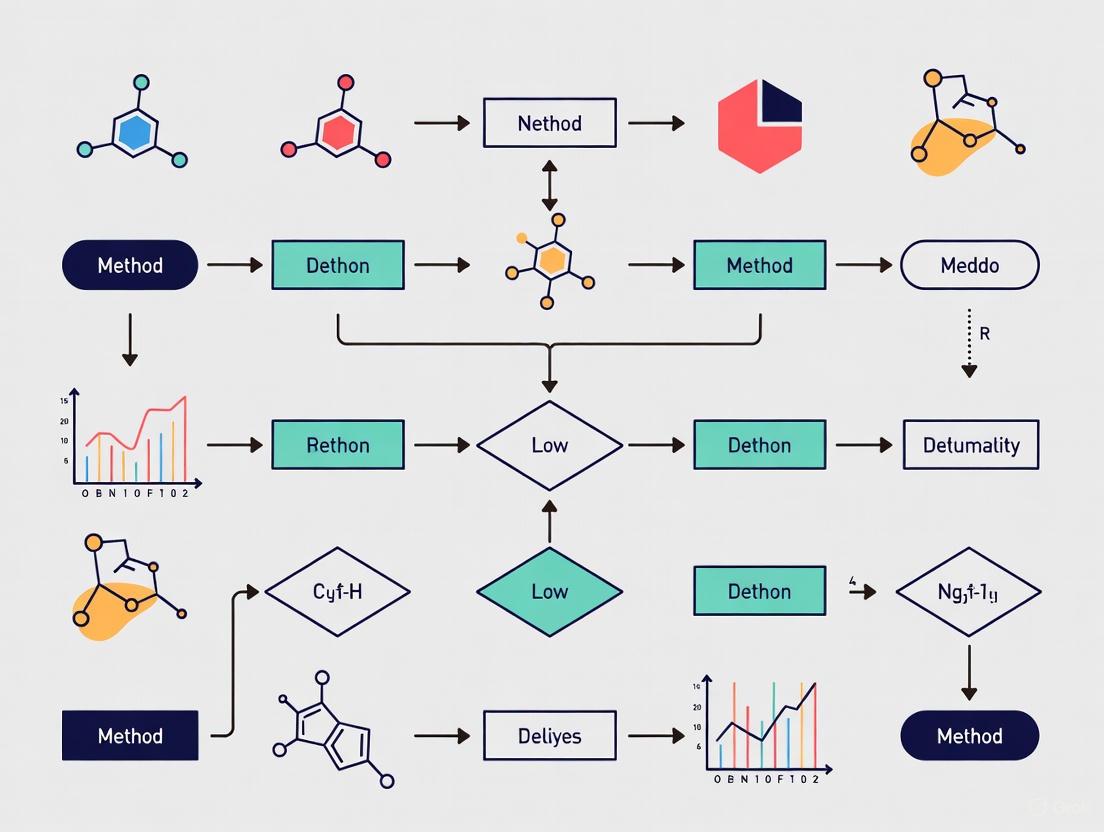
The relationship between these processes can be visualized as follows:
Regulatory Frameworks and Requirements
CLIA Proficiency Testing Requirements
The Clinical Laboratory Improvement Amendments (CLIA) establish quality standards for laboratory testing. CLIA requires laboratories to enroll in Proficiency Testing (PT) programs for regulated analytes, with updated acceptance limits effective January 1, 2025 [4] [1].
PT evaluates a laboratory's testing performance compared to peer laboratories. The Centers for Medicare & Medicaid Services (CMS) enforces these regulations, with bolded analytes in the CAP Surveys catalog indicating CMS-regulated tests [1].
The table below summarizes selected 2025 CLIA acceptance limits for key analytes:
Table 1: Selected CLIA 2025 Proficiency Testing Acceptance Limits
| Analyte or Test | NEW 2025 CLIA Criteria | Previous Criteria |
|---|---|---|
| Chemistry | ||
| Glucose | Target Value ± 6 mg/dL or ± 8% (greater) | Target Value ± 6 mg/dL or ± 10% (greater) |
| Creatinine | Target Value ± 0.2 mg/dL or ± 10% (greater) | Target Value ± 0.3 mg/dL or ± 15% (greater) |
| Hemoglobin A1c | Target Value ± 8% | None (Newly regulated) |
| Potassium | Target Value ± 0.3 mmol/L | Target Value ± 0.5 mmol/L |
| Toxicology | ||
| Digoxin | Target Value ± 15% or ± 0.2 ng/mL (greater) | None (Newly regulated) |
| Phenytoin | Target Value ± 15% or ± 2 mcg/mL (greater) | Target Value ± 25% |
| Hematology | ||
| Leukocyte Count | Target Value ± 10% | Target Value ± 15% |
| Hemoglobin | Target Value ± 4% | Target Value ± 7% |
| Immunology | ||
| Unexpected Antibody Detection | 100% accuracy | 80% accuracy |
Pharmaceutical Microbiology Validation Frameworks
For Rapid Microbiological Methods (RMMs) in pharmaceutical manufacturing, validation follows structured frameworks outlined in USP <1223> and Ph. Eur. 5.1.6 [2] [3]. These guidelines require demonstrating method equivalency to traditional compendial methods through defined validation parameters.
The complete RMM validation workflow encompasses multiple critical stages:
Key Research Reagent Solutions for Method Validation
Successful method validation requires specific reagents and materials to generate scientifically sound evidence. The table below details essential reagents and their functions:
Table 2: Essential Research Reagents for Microbiological Method Validation
| Reagent/Material | Function in Validation | Application Examples |
|---|---|---|
| Certified Reference Materials | Provides standardized benchmarks for accuracy assessment; verifies method calibration | Quantifying known microbial concentrations for accuracy studies [5] |
| Strain Collections (ATCC) | Well-characterized microorganisms for specificity and detection limit studies | Challenge studies to demonstrate method detection capabilities [2] |
| Culture Media | Supports microbial growth for compendial method comparison | Parallel testing for equivalency demonstration [5] |
| Validation Samples (Spiked) | Samples with known contaminant levels for recovery studies | Matrix interference testing and detection limit studies [2] |
| Quality Control Materials | Monitors method performance precision and reproducibility | Routine system suitability testing [5] |
Troubleshooting Low Accuracy in Microbiological Methods
FAQ: How do I investigate low accuracy during method verification?
Q: Our microbiological method verification shows consistently low accuracy compared to reference methods. What systematic approach should we take to identify the root cause?
A: Troubleshoot low accuracy by investigating these key areas:
- Matrix Interference Effects: Product components can inhibit or enhance microbial detection. Conduct matrix interference studies by spiking product samples with known microbial levels and comparing recovery rates to control samples [2].
- Sample Preparation Consistency: Inconsistent sample handling directly impacts accuracy. Validate each preparation step and document any deviations. Automated systems can reduce variability [5].
- Reference Method Discrepancies: Ensure your reference method is properly validated. Discrepancies may reflect issues with the comparator method rather than your new method [2] [3].
- Instrument Calibration Status: Verify equipment calibration using certified reference materials. Document calibration dates and results [5].
- Operator Technique Variability: Implement robust training and competency assessment programs. Conduct intermediate precision studies with different operators [2].
FAQ: How do CLIA PT changes impact our verification processes?
Q: With the updated CLIA PT acceptance limits effective 2025, must we re-verify all our methods?
A: According to the College of American Pathologists, laboratories are not required to repeat prior verifications based solely on updated CLIA PT criteria. However, you should review performance goals used in subsequent verifications. CLIA PT acceptance limits are not intended as validation/verification performance goals, which should be based on clinical needs and manufacturer's FDA-approved labeling [1].
FAQ: What documentation is required for audit-ready validation?
Q: What essential documentation must we prepare to demonstrate RMM validation during regulatory audits?
A: Comprehensive documentation is crucial for audit readiness. Your validation package should include [2]:
- Validation Protocol: Pre-approved document defining scope, acceptance criteria, and experimental design
- Equivalency Study Data: Parallel testing results comparing RMM to compendial methods
- Risk Assessment: Documentation of potential failure modes and control strategies
- Standard Operating Procedures: Detailed instructions for method performance
- Training Records: Evidence of personnel competency on the new method
- Final Validation Report: Comprehensive summary with conclusions and management approval
Experimental Protocol: Demonstrating Method Equivalency
This protocol provides a standardized methodology for demonstrating equivalency between Rapid Microbiological Methods and traditional compendial methods, a common regulatory requirement [2] [3].
Materials and Equipment
- Reference method materials (agar plates, broth media, etc.)
- RMM system and associated reagents
- Certified microbial reference strains (at least 5-6 representative species)
- Product samples (for matrix studies)
- Diluents and neutralizers as appropriate
Procedure
- Study Design: Conduct parallel testing of samples using both RMM and the compendial reference method. Include appropriate controls.
- Sample Preparation: Prepare identical sample sets for both methods using aseptic technique.
- Inoculation: Inoculate samples with low, medium, and high concentrations of target microorganisms.
- Incubation/Analysis: Process samples according to both methods' standard procedures.
- Data Collection: Record quantitative results from both methods for statistical comparison.
- Statistical Analysis: Apply appropriate statistical tests (e.g., Student's t-test, F-test) to demonstrate equivalency.
Acceptance Criteria
Establish pre-defined acceptance criteria for accuracy (e.g., recovery rates within 70-130%), precision (e.g., CV ≤ 15%), and equivalency (e.g., no statistically significant difference between methods) [2].
Frequently Asked Questions (FAQs)
Q1: What is the critical difference between method validation and method verification, and when is each required?
Method validation is a comprehensive process that proves an analytical method is acceptable for its intended use and is required when developing new methods. Method verification is the process of confirming that a previously validated method performs as expected under your specific laboratory conditions [6].
- Validation is essential for new drug applications, clinical trials, and novel assay development [6].
- Verification is acceptable and efficient for implementing standard or compendial methods (e.g., from USP, EPA, AOAC) in a laboratory [6].
Q2: Why are traditional, growth-based microbiological methods particularly challenging for accuracy and sterility testing?
Conventional growth-based methods, while compendial, have several inherent limitations that can impact accuracy [7]:
- Inability to Detect All Contamination: They are inefficient in detecting all microbial contaminants present in a sample [7].
- Inability to Discriminate Viability: They cannot distinguish between viable and non-viable microorganisms, which can lead to overestimation of viable bioburden [7].
- Lengthy Time-to-Result: They are time-consuming, delaying critical decisions in manufacturing and research [7].
- False Results: They are susceptible to both false-positive and false-negative results, compromising data reliability [7].
Q3: How should I handle non-detect (ND) results in microbial enumeration studies to ensure accurate concentration estimates?
A common misconception is to treat microbial non-detects as "censored" data less than a detection limit (e.g., <1 CFU), a practice borrowed from analytical chemistry. This is incorrect for discrete microbial data and can introduce bias [8].
- Correct Approach: Report the raw observation (e.g., 0 microorganisms) and the analytical sample size (e.g., volume tested). This preserves the probabilistic information needed for accurate statistical analysis and concentration estimation, consistent with how positive observations are handled [8].
- Underlying Science: Unlike chemistry, where signals come from vast numbers of molecules, microbiology deals with discrete objects. A non-detect means no microorganisms were observed in the specific volume tested, which is a probabilistic outcome related to the true concentration and recovery efficiency [8].
Q4: What special considerations are needed for methods used in low-microbial-biomass environments?
Samples with low microbial biomass (e.g., certain human tissues, purified water, cleanroom environments) are disproportionately affected by contamination, which can compromise accuracy and lead to false conclusions [9]. Key strategies include:
- Rigorous Contamination Controls: Use single-use, DNA-free consumables; decontaminate equipment with bleach or UV-C to remove DNA; and employ personal protective equipment (PPE) to limit human-derived contamination [9].
- Comprehensive Controls: Always include negative controls (e.g., empty collection vessels, swabs of the air, aliquots of preservation solution) that undergo the exact same processing as experimental samples. These are essential for identifying contaminating sequences [9].
Troubleshooting Guide: Low Accuracy in Microbiological Method Verification
This guide addresses common pitfalls that compromise the accuracy of your verified method.
Problem 1: Inaccurate results due to poor specificity and interference.
- Potential Cause: The method cannot distinguish the target analyte from other components in the sample matrix, such as impurities, degradation products, or the sample background itself [10].
- Solution:
- Confirm Specificity: Demonstrate that the method can assess the analyte unequivocally in the presence of these potential interferents. For microbial methods, this may involve testing the method with samples containing related but non-target microbial strains to ensure no cross-reactivity [10].
- Use Appropriate Controls: Include controls that mimic the sample matrix without the target analyte to identify any background signal.
Problem 2: High variability and poor precision undermining accuracy.
- Potential Cause: Uncontrolled variations in the testing procedure, including differences between analysts, equipment, reagents from different suppliers, or day-to-day operations [10].
- Solution:
- Assess Intermediate Precision: Design your verification study to include multiple runs by different analysts on different days using different equipment if possible. This evaluates the method's robustness in your lab [10].
- Standardize Reagents and Protocols: Use reagents from qualified suppliers and adhere strictly to the standard operating procedure (SOP). Investigate the robustness of the method by deliberately introducing small, validated changes to understand its tolerance [10].
Problem 3: Failure to detect low-level contaminants, leading to false negatives.
- Potential Cause: The method's Limit of Detection (LOD) is not suitable for the intended application, or contaminants are introduced during sample handling [10] [9].
- Solution:
- Verify the LOD: Confirm the method's LOD—the lowest concentration of analyte that can be reliably detected—under your laboratory's specific conditions. This is distinct from the Limit of Quantitation (LOQ), which is the lowest level that can be quantified with acceptable accuracy and precision [10].
- Implement Low-Biomass Precautions: If testing low-biomass samples, follow the stringent contamination control measures outlined in FAQ A4. The impact of contamination is magnified in these samples [9].
Problem 4: Non-detects (NDs) are handled incorrectly, biasing concentration estimates.
- Potential Cause: Reporting NDs as "<" values and treating them as censored data, which is a statistical approach misapplied from analytical chemistry [8].
- Solution:
- Report Raw Data: Always report the raw microbial count (zero) and the sample size tested. This allows for proper statistical modeling that accounts for the probabilistic relationship between the observation and the true concentration [8].
- Use Appropriate Statistical Models: Utilize methods like Maximum Likelihood Estimation (MLE) that can correctly incorporate both positive and non-detect results based on the sample volume and method recovery efficiency [8].
Problem 5: The method is not robust under normal operating conditions in your lab.
- Potential Cause: The method's performance is highly sensitive to minor, inevitable variations in the analytical environment [10].
- Solution:
- Test Robustness During Verification: As part of verification, test the method's performance under deliberate, slight variations in operational parameters (e.g., incubation temperature fluctuations, reagent incubation times, different analyst techniques). This demonstrates the method's reliability in your hands [10].
Core Parameter Definitions and Experimental Protocols
The table below summarizes the core validation parameters, their definitions, and key verification experiments.
Table 1: Core Validation Parameters and Verification Experiments
| Parameter | Definition | Key Verification Experiments |
|---|---|---|
| Accuracy | The closeness of agreement between the measured value and a reference value accepted as true [10]. | - Spike known concentrations of the target microorganism into the product or sample matrix.- Compare the results from the new method to those from a validated reference method.- Analyze certified reference materials (CRMs), if available. |
| Precision | The closeness of agreement between a series of measurements from multiple sampling of the same homogenous sample. It has three tiers: repeatability, intermediate precision, and reproducibility [10]. | - Repeatability: Analyze multiple replicates of the same sample by the same analyst under the same conditions in a single session.- Intermediate Precision: Analyze the same sample across different days, with different analysts, or using different equipment within the same lab. |
| Specificity | The ability to assess the target analyte unequivocally in the presence of other components that may be expected to be present (e.g., impurities, degradation products, sample matrix) [10]. | - Test the method with samples containing structurally similar or common contaminating microorganisms to ensure no cross-reactivity.- Test the method with the sample matrix without the target analyte to confirm the absence of interfering signals. |
| LOD / LOQ | LOD: The lowest concentration of an analyte that can be detected, but not necessarily quantified, under stated experimental conditions [10].LOQ: The lowest concentration of an analyte that can be quantified with acceptable levels of accuracy and precision [10]. | - For microbial methods, this often involves analyzing samples with progressively lower concentrations of the target microorganism.- LOD is typically the level at which the method transitions from intermittent detection to consistent non-detection.- LOQ is the lowest level where acceptable accuracy and precision (e.g., %CV) are consistently demonstrated. |
Method Verification and Troubleshooting Workflow
The diagram below outlines a logical workflow for verifying a microbiological method and troubleshooting low accuracy issues.
Research Reagent and Material Solutions
Table 2: Essential Materials for Microbiological Method Verification and Troubleshooting
| Item | Function in Verification/Research |
|---|---|
| Reference Microbial Strains | Certified strains used for spiking studies to establish accuracy, precision, LOD, and LOQ. They provide a known, quantifiable signal. |
| DNA-Free Reagents and Consumables | Specially treated reagents, water, and plasticware (e.g., tubes, filters) that minimize the introduction of contaminating DNA, which is critical for verifying methods for low-biomass samples [9]. |
| Negative Controls | Sterile samples or buffers that are processed alongside experimental samples. They are essential for identifying background contamination from reagents or the laboratory environment [9]. |
| Sample Preservation Solutions | Solutions (e.g., 95% ethanol, commercial kits like OMNIgene) that stabilize the microbial community in a sample from the moment of collection until analysis, preventing shifts that could affect accuracy [11]. |
| Culture Media | Growth substrates used in traditional compendial methods. Their quality, pH, and composition must be verified to ensure they support the growth of target and recovery microorganisms [7]. |
Troubleshooting Guide: Resolving Low Accuracy in Method Verification
Q1: My method verification studies are consistently showing low accuracy against the reference method. What are the primary root causes I should investigate?
Low accuracy, indicating a systematic error or bias in your results, can stem from several sources. The following table outlines common causes and investigative actions based on principles from international standards.
| Root Cause Category | Specific Examples | Investigative Actions & Troubleshooting Steps |
|---|---|---|
| Sample & Protocol Issues | Inconsistent sampling techniques or locations; improper sample homogenization; deviation from validated protocol timing [12]. | Audit aseptic techniques; implement timed protocols; verify sample mixing procedures; replicate sampling to assess inherent variability [12]. |
| Reagent & Equipment Problems | Contaminated plastic consumables (e.g., pipette tips, assay tubes); reagents not equilibrated to ambient temperature; incorrect pipette calibration [12]. | Perform background contamination checks on consumables; document reagent temperature equilibration; verify pipette calibration records and technician training [12]. |
| Method Suitability | Failure to demonstrate method suitability for the specific product (e.g., sample matrix interference) [13] [3]. | Re-run method suitability testing; spike product with known microorganisms to confirm recovery is not inhibited [13]. |
| Definition of 'Accuracy' | Applying an incorrect statistical model for the method type (qualitative vs. quantitative); attempting a direct statistical comparison of CFU to a non-growth-based signal where it is invalid [13]. | Consult USP <1223> and ISO 16140-2 for appropriate equivalence models (e.g., non-inferiority for qualitative methods, correlation curves for quantitative methods) [13] [14]. |
Q2: I am using a validated commercial test kit, but my in-house verification is failing. Is the kit faulty, or is my process wrong?
This common dilemma requires a structured investigation to isolate the problem. Follow the diagnostic workflow below to identify the most likely source of the failure.
Q3: The colony counts from my alternative method don't match the traditional CFU counts. Does this automatically mean my alternative method is inaccurate?
Not necessarily. A difference in counts does not automatically equate to inaccuracy. USP <1223> clarifies that the Colony-Forming Unit (CFU) itself is an estimate that can underreport the true number of microorganisms due to clumping, physiological state, and recovery limitations of growth-based methods [13]. Your alternative method (e.g., based on viability staining) might be providing a more accurate count of individual cells.
- Key Consideration: The core principle is to demonstrate equivalence or non-inferiority in assessing the product's microbiological quality and safety, not to achieve an identical count [13]. If the alternative method consistently detects microbial contamination and your validation data supports that it is as good as or better than the compendial method for its intended purpose, a numerical difference may be acceptable.
Q4: How do I handle highly variable results (poor repeatability) when performing ATP bioluminescence testing?
Poor repeatability in ATP tests is a frequent issue, often traced to procedural inconsistencies. The table below lists critical checkpoints.
| Checkpoint | Common Issue | Corrective Action |
|---|---|---|
| Sample Homogeneity | Microorganisms distributed unevenly [12]. | Mix sample thoroughly before analysis; collect multiple samples from same location to assess variability [12]. |
| Reagent Handling | Luminase enzyme activity fluctuates [12]. | Allow enzyme to reach ambient temperature (e.g., 1 hour) before use [12]. |
| Pipetting Technique | Inaccurate or inconsistent liquid transfer [12]. | Ensure clean, calibrated pipettes; train analysts on technique; avoid reusing tips [12]. |
| Assay Timing | Reaction timing deviations between runs [12]. | Strictly adhere to protocol timing for reagent addition and measurement. |
| Background Contamination | Contaminated consumables inflating readings [12]. | Perform background checks on assay tubes; discard batches with high background RLU [12]. |
Experimental Protocols for Key Verification Studies
Protocol 1: Equivalence Demonstration for a Quantitative Method
This protocol aligns with the "Results Equivalence" option in USP <1223> and the method comparison study in ISO 16140-2 [13] [14].
- Sample Preparation: Prepare a set of samples (e.g., drug product placebo, buffer) contaminated with a low level of a representative microorganism (e.g., E. coli, S. aureus). Use a dilution series to obtain a range of microbial concentrations.
- Parallel Testing: Test each sample in parallel using both the alternative method and the compendial (reference) method. Ensure a sufficient number of replicates (e.g., n=3 per level) are performed to power the statistical analysis.
- Data Analysis: Plot the results from the alternative method (signal, count) against the results from the reference method (CFU). Generate a calibration curve or correlation curve.
- Statistical Evaluation: Evaluate the correlation for linearity, slope, and intercept. The alternative method is considered equivalent if the results show a consistent, predictable relationship with the reference method, demonstrating it is fit for its intended quantitative purpose [13].
Protocol 2: Verification of a Qualitative (Presence/Absence) Method
This protocol is critical for methods like sterility testing.
- Sample Inoculation: Prepare test samples by inoculating them with a low level of microorganisms (near the method's limit of detection). Also include uninoculated negative controls.
- Blinded Testing: Test the inoculated and control samples using the alternative method in a blinded fashion.
- Comparison to Reference: Compare the results (Positive/Negative) from the alternative method to those obtained from the compendial sterility test method.
- Calculation of Performance: Calculate the alternative method's Specificity (ability to correctly identify negative samples) and Sensitivity (ability to correctly identify positive samples). The method is considered non-inferior if its sensitivity meets or exceeds a pre-defined acceptance criterion relative to the compendial method [13] [14].
The Scientist's Toolkit: Essential Research Reagent Solutions
| Item / Reagent | Critical Function in Verification Studies |
|---|---|
| Strain Panel of Microorganisms | Used for challenging the method to demonstrate specificity and accuracy. Should include compendial strains, relevant environmental isolates, and stressed cells [15]. |
| Product-Specific Matrix | The actual product or placebo is essential for method suitability testing to prove the sample does not interfere with the alternative method's signal [13] [3]. |
| Reference Culture Media | Required for the compendial method and for the preparation and titration of the inoculum used in the study [15]. |
| Neutralizing Agents | Critical for testing sanitizers or biocide-containing products to ensure any antimicrobial activity is neutralized during the test, allowing for the recovery of viable microorganisms. |
| Certified Reference Materials | Used for instrument calibration and to provide a known value for establishing the accuracy and linearity of quantitative alternative methods. |
Identifying the Root Causes of Low Accuracy in Microbiological Contexts
FAQ: What are the most common root causes of low accuracy in microbiological method verification?
Low accuracy in microbiological method verification often stems from a range of factors, from sample-related issues to procedural errors. The table below summarizes the most frequent root causes and their impacts on data accuracy.
| Root Cause Category | Specific Issue | Impact on Accuracy |
|---|---|---|
| Sample & Matrix Effects | Presence of inhibitory substances in the product matrix [16] | Causes false negatives by preventing microbial growth, leading to underestimation of bioburden. |
| Method Suitability | Failure to perform or document suitability testing [16] [17] | Generates scientifically invalid data, as the method is not proven to work for the specific product. |
| Microbial Distribution | Low colony-forming unit (CFU) counts where Poisson distribution applies [18] [19] | Introduces significant inherent statistical variability, making counts less reliable and precise. |
| Culture Media | Use of media that fails Growth Promotion Tests (GPT) [17] | Compromises the ability to detect microorganisms, resulting in false negatives and invalidating tests. |
| Laboratory Technique | Improper sample handling, dilution errors, and incubation conditions [5] [19] | Introduces variability and bias, affecting both precision and accuracy of microbial enumeration. |
| Data Integrity | Incorrect colony counting and lack of a second-person verification [17] | Leads to transcription errors and unverified data, directly impacting the reported results' reliability. |
FAQ: How can I troubleshoot a "suitability test failure" for my product?
A suitability test failure indicates that your product's formulation inhibits the growth of the microorganisms you are testing for. The following workflow provides a step-by-step troubleshooting guide for this scenario.
Troubleshooting Protocol:
- Confirm Failure: Verify that the failure is due to the non-recovery of the spiked organism in the presence of the product, not a laboratory error [16].
- Incorporate Inactivating Agents: Modify the method by adding suitable neutralizing agents to your dilution blank or enrichment medium. Common neutralizers include:
- Lecithin and Polysorbate 80 to neutralize quaternary ammonium compounds and phenolics.
- Sodium Thiosulfate to neutralize halogen-based disinfectants.
- Histidine to neutralize aldehyde-based disinfectants.
- Validate the effectiveness of the neutralizer by demonstrating the recovery of the spiked organism in the presence of both the product and the neutralizer [16] [19].
- Increase Diluent Volume: Substantially increase the volume of diluent used during the initial sample preparation. This dilutes the inhibitory substance to a level where it no longer affects microbial growth [16].
- Evaluate Alternative Methods: If the pour-plate method is used, switch to the membrane filtration method. This technique physically separates microorganisms from the inhibitory product, after which the membrane is transferred to a nutrient medium, thus bypassing the inhibition [16].
- Report Inherent Microbicidal Activity: If, despite all efforts, the spiked organism cannot be recovered, this demonstrates a powerful inherent antimicrobial property of the product. Per USP guidance, you can report that the product is not likely to be contaminated with the specified microorganism due to its pronounced microbicidal activity. Ongoing monitoring is still required [16].
FAQ: How does statistical variability at low microbial counts affect accuracy, and how can it be managed?
At low microbial counts (typically below 100 CFU), microorganisms are not evenly distributed in a suspension but follow a Poisson distribution. This is a fundamental source of variability that can lead to inaccurate counts [18] [19].
Experimental Protocol to Quantify Variability:
- Preparation: Create a suspension with a low, target concentration of a non-pathogenic microorganism (e.g., Staphylococcus aureus ATCC 6538) at approximately 10 CFU/mL. Confirm the concentration using a validated method.
- Sample Plating: Independently plate one hundred 0.1 mL aliquots of this suspension onto soybean-casein digest agar plates.
- Incubation and Counting: Incubate the plates as per method requirements and count the CFUs on each plate.
- Data Analysis: Tabulate the results. You will observe that the counts are not uniform. A significant number of plates (theoretically ~37% at a mean of 1 CFU/plate) will have zero colonies, while others will have 1, 2, or more.
The table below illustrates the expected distribution from such an experiment, highlighting the inherent variability.
| Aliquot Number (Example) | CFU Count (per 0.1 mL) |
|---|---|
| 1 | 0 |
| 2 | 1 |
| 3 | 2 |
| 4 | 0 |
| 5 | 1 |
| ... | ... |
| 100 | 1 |
| Mean Calculated Concentration | ~10 CFU/mL |
Management Strategy: To manage this variability, increase the number of replicates and the sample volume tested. The root sum of squares approach can be used to estimate the total combined error from independent sources like CFU/plate variability, number of replicates, and dilution errors [18]. Averaging results from a larger number of replicates (e.g., 3-5 plates per sample) provides a more accurate and precise estimate of the true microbial concentration.
FAQ: What are the critical reagent and material solutions for successful method verification?
The reliability of your method verification is highly dependent on the quality and suitability of your reagents. The table below lists key materials and their critical functions.
| Research Reagent / Material | Function in Method Verification |
|---|---|
| Qualified Culture Media | Supports the growth of target microorganisms; must pass Growth Promotion Tests (GPT) with a recovery of ≥80% for each indicator organism [19] [17]. |
| Neutralizing Agents | Inactivates antimicrobial properties of the test product (e.g., lecithin, polysorbate 80, sodium thiosulfate) to enable recovery of microorganisms [16]. |
| Certified Reference Strains | Serves as positive controls for growth promotion and method suitability testing, providing a benchmark for expected recovery [5] [19]. |
| Environmental Isolates | Strains isolated from your own manufacturing environment; critical for proving the method can detect the organisms actually present in your context [19]. |
| Membrane Filters | Used in the membrane filtration method to separate microbes from inhibitory product matrices, thereby facilitating accurate enumeration [16]. |
FAQ: What are the regulatory consequences of inadequate method verification?
Regulatory agencies like the FDA consider inadequate method verification a serious violation of Current Good Manufacturing Practices (CGMP). Recent warning letters highlight direct consequences [17]:
- Product Adulteration: Drugs released using methods with failed media Growth Promotion Tests (GPT) or without proper suitability testing are deemed "adulterated" [17].
- Inadequate Investigations: Citing "human error" for GPT failures without a specific, documented root cause analysis is unacceptable. This leads to a requirement for retrospective reviews and robust Corrective and Preventive Actions (CAPA) [17].
- Compromised Data Integrity: Allowing a single analyst to perform plate counting, data entry, and evaluation without a secondary check leads to incorrect counts and is a critical data integrity failure [17].
- Recommended External Audit: In severe cases, the FDA may recommend halting production and employing an external consultant with expertise in sterile manufacturing to conduct a comprehensive evaluation [17].
The Impact of Sample Matrix and Microbial Variability on Results
Frequently Asked Questions (FAQs)
FAQ 1: Why do I get different results when testing the same microbial sample on different days? Microbiological systems possess numerous uncontrollable variables, leading to inherent experimental complexity and variability [20]. Key factors contributing to day-to-day differences include:
- Test System Variability: Minor fluctuations in incubation temperature, humidity, and the age/physiology of the microbial culture can significantly alter results [20].
- Operator Variability: Manual techniques like pipetting, inoculating surfaces, or applying a wipe can vary slightly between scientists and even from one repetition to the next by the same individual [20].
- Test Substance Variability: The age and storage conditions of disinfectants or antimicrobial agents can affect their stability and activity. Slight variations between production lots of a substance can also be a factor [20].
FAQ 2: What is a "matrix effect" and how does it impact my analytical results? The matrix refers to all components of your sample other than the analyte you are trying to measure [21]. Matrix effects occur when co-extracted components from the sample interfere with the detection of your target analyte, most commonly in techniques like LC-MS or GC-MS [21] [22]. This interference can cause either suppression or enhancement of the analyte signal, leading to inaccurate quantification [21]. For instance, matrix components can interfere with the ionization efficiency of an analyte in a mass spectrometer, causing a loss of signal [22].
FAQ 3: My method works perfectly with pure cultures, but fails with real-world samples. Why? This is a classic symptom of matrix effects or issues with sample preparation [21]. Real-world samples (e.g., food, clinical specimens, environmental samples) contain a complex mixture of components that are not present in pure solvent or culture standards. These matrix components can:
- Suppress or enhance analyte detection [21] [22].
- Interfere with the extraction of the target microbe or analyte from the sample [23].
- Be toxic to the microbes or inhibit their growth, leading to underestimation of counts [23].
FAQ 4: How can heterogeneous distribution of microbes in a sample affect my test results? Microbes are often not distributed uniformly in a sample (heterogeneity), which is a major source of test result variability [23]. This affects different stages of testing:
- Source Variability (VSOURCE): Biofilms form in localized patches on surfaces and interfaces, meaning two samples taken centimeters apart can have bioburdens that vary by an order of magnitude [23].
- Sample Variability (VSAMPLE): In viscous or non-aqueous fluids (like fuels or oils), microbes tend to clump, making replicate samples highly variable [23].
- Specimen Variability (VSPECIMEN): When you draw a small aliquot from a heterogeneous sample for testing, it may not be representative of the whole [23].
Troubleshooting Guides
Guide 1: Diagnosing and Quantifying Matrix Effects
Problem: Suspected matrix effect causing inaccurate quantification of an analyte.
Experimental Protocol: The following post-extraction addition method is a standard approach to quantify matrix effect [21] [22].
Prepare Samples: For a fixed concentration method, prepare at least five (n=5) replicates of each of the following [21]:
- Solvent Standard: The analyte dissolved in a neat solvent.
- Matrix-Matched Standard: A blank matrix extract (from the same type of sample, but known to be free of the analyte) spiked with the same concentration of analyte after the extraction process.
Analysis: Analyze all samples under identical instrument conditions within a single analytical run [21].
Calculation: Calculate the Matrix Effect (ME) factor for each analyte using the formula:
- ME (%) = [(B - A) / A] × 100
- Where A is the average peak response of the analyte in the solvent standard.
- Where B is the average peak response of the analyte in the matrix-matched standard [21].
- ME (%) = [(B - A) / A] × 100
Interpretation:
- ME ≈ 0%: No significant matrix effect.
- ME > 0%: Matrix-induced signal enhancement.
- ME < 0%: Matrix-induced signal suppression.
- As a rule of thumb, if the absolute ME value is greater than 20%, action should be taken to compensate for the effect to ensure accurate reporting [21].
Guide 2: Mitigating Microbial Heterogeneity in Samples
Problem: High variability in microbial counts between replicate samples or test specimens.
Solutions and Best Practices:
- Increase Sample Volume: For heterogeneous sources like fuels or oils, collecting a larger sample volume reduces the risk of missing microbial clumps and provides a more representative sample [23].
- Vigorous and Standardized Shaking: Use an adjustable, wrist-action shaker to disperse microbial flocs uniformly throughout the sample container before drawing a specimen for testing. This eliminates operator fatigue and ensures consistent force is applied to all samples [23].
- Use of Surfactants: Adding a surface-active agent (e.g., CTAB or Tween 80) can help break up clumps and improve the homogeneity of the bioburden in the sample [23].
- Separate Sample Phases: If a sample has multiple phases (e.g., oil, emulsion, and water), separate them into different containers and test each phase individually [23].
Diagram 1: Sources of Variability in Microbial Testing. This diagram traces the progression of variability from the original source to the final result, highlighting where errors are introduced [23].
Problem: General concerns about the reliability, reproducibility, and defensibility of microbiological method data.
Recommended Practices:
- Use Authenticated Biomaterials: Start experiments with traceable, authenticated, and low-passage reference microorganisms. Routinely evaluate biomaterials throughout the research workflow to ensure genotypic and phenotypic stability [24].
- Robust Calibration and Maintenance: Regularly calibrate and maintain all laboratory equipment, including pipettes, scales, and analytical instruments. Calibration is the most critical step for ensuring data accuracy [25].
- Operator Training and Standardization: Ensure all personnel are thoroughly trained on manual techniques. Use detailed, descriptive procedures to minimize inherent variability between scientists [20] [25].
- Publish and Share Negative Data: Contribute to the broader scientific community by making negative data (e.g., where a correlation was not found) accessible. This helps other researchers avoid dead ends and improves the overall efficiency of scientific progress [24].
Table 1: Common Sources of Variability in Antimicrobial Testing [20]
| Source Category | Specific Factor | Impact on Results |
|---|---|---|
| Test System | Temperature/Humidity fluctuations | Alters microbial physiology and reaction rates. |
| Microbial strain and age | Different strains and older cultures can react differently to antimicrobials. | |
| Growth media composition | Slight differences in brand or batch affect microbial physiology and metabolism. | |
| Operator | Pipetting technique | Affects the volume of inoculum or reagent added. |
| Inoculation of surfaces | Leads to uneven distribution of microbes on test carriers. | |
| Manipulation (e.g., wiping) | Differences in pressure and technique during manual steps. | |
| Test Substance | Age and storage conditions | Active ingredients degrade over time, reducing efficacy. |
| Variation between production lots | Slight differences in composition between batches. | |
| Dilution water hardness | High mineral content can decrease the efficacy of some antimicrobials. |
Table 2: Interpreting Matrix Effect Calculations [21]
| Matrix Effect (ME) Value | Interpretation | Recommended Action |
|---|---|---|
| ± 10% | Minimal matrix effect | No action typically required. |
| ± 10% to ± 20% | Moderate matrix effect | Monitor closely; action may be needed for critical methods. |
| > ± 20% | Significant matrix effect | Action required. Use matrix-matched calibration, improve sample cleanup, or apply a correction factor. |
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents and Materials for Reliable Microbiological Testing
| Item | Function | Key Considerations |
|---|---|---|
| Authenticated Reference Strains | Provides a standardized, traceable baseline for method verification and comparison. | Use ATCC or other recognized repository strains specified by regulatory guidelines (e.g., EPA) [24] [20]. |
| Standardized Growth Media | Supports consistent and reproducible microbial growth. | Follow recommended formulations (e.g., from EPA); be aware that different batches can introduce variability [20]. |
| Surfactants (e.g., Tween 80, CTAB) | Aids in dispersing microbial clumps in heterogeneous samples, improving homogeneity and representativeness [23]. | Optimize type and concentration for your specific sample matrix to avoid inhibiting microbial growth. |
| Matrix-Matched Blank Extracts | Serves as the baseline for quantifying and compensating for matrix effects in analytical methods [21] [22]. | Must be sourced from the same sample type (e.g., organic strawberries) known to be free of the target analyte. |
| Laboratory-Grade Hard Water | Used for diluting disinfectants to simulate real-world use conditions and test efficacy under standardized challenges [20]. | Hardness (PPM calcium) must be consistent, as it is known to decrease the efficacy of some antimicrobials. |
| Calibration Standards | Used to calibrate instruments and ensure the accuracy of quantitative measurements [25]. | Should be traceable to national or international standards. Prepare in both solvent and matrix for comparison. |
Implementing Robust Verification Protocols for Qualitative and Quantitative Assays
Frequently Asked Questions
Q1: What are the most common causes of low accuracy in a microbiological method verification? Low accuracy in microbiological method verification often stems from several key issues:
- Matrix Interference: The product itself (e.g., gels, creams, high-sugar solutions) can inhibit microbial growth or cause false positives/negatives, leading to poor recovery of microorganisms. [2]
- Improper Sample Handling: Inconsistent sample collection, storage, or preparation can compromise microbial viability and introduce errors. [5]
- Insufficient Method Equivalency Data: Failing to adequately demonstrate that the Rapid Microbiological Method (RMM) performs equivalently to the compendial method in accuracy, precision, and specificity. [2] [3]
- Incorrectly Defined Limits: The limits of detection (LOD) and quantitation (LOQ) may not be suitably validated for the method's intended use, causing sensitivity issues. [2]
Q2: How many samples and replicates are sufficient to demonstrate method precision? The required number of samples and replicates depends on the validation parameter and the associated risk. The following table summarizes quantitative recommendations based on pharmacopeial guidance and best practices. [2] [26]
| Validation Parameter | Experimental Design (Samples & Replicates) | Acceptance Criteria |
|---|---|---|
| Repeatability | A minimum of 6 valid replicates at a target concentration of 100% (or 3 concentrations, e.g., 50%, 100%, 150%, with 3 replicates each). [26] | Relative Standard Deviation (RSD) of not more than 10-15%, depending on the method's criticality. [2] |
| Intermediate Precision | Multiple analyses performed on different days, by different analysts, using different equipment. The number of replicates should mirror the repeatability study. [2] | The overall RSD from the combined intermediate precision data should be within 15-20%, demonstrating no significant variance between the different conditions. [2] |
Q3: What acceptance criteria should be used for accuracy (recovery) studies? Accuracy is measured by the percentage recovery of known concentrations of microorganisms from the product matrix. The table below outlines typical acceptance criteria. [2] [26]
| Microbial Concentration Level | Target Recovery Range | Experimental Protocol |
|---|---|---|
| High Concentration (e.g., for microbial enumeration) | 70% - 150% | Inoculate the product matrix or a placebo with a known, high concentration (e.g., 100 CFU) of a challenge organism. Recover and enumerate using the verified method. Compare the result to the inoculum count. |
| Low Concentration (e.g., at LOD/LOQ) | 50% - 200% | Inoculate the product matrix with a low concentration of a challenge organism (at or near the method's LOD/LOQ). The recovery rate at this level has a wider acceptable range due to higher inherent variability. |
The Scientist's Toolkit: Key Reagents and Materials
The following table details essential materials for executing a robust microbiological method verification. [2] [5]
| Item | Function in Verification |
|---|---|
| Certified Reference Materials | Provides standardized, traceable microbial strains with known characteristics for inoculum preparation, ensuring the accuracy and reproducibility of challenge studies. [5] |
| Neutralizing Agents | Inactivates antimicrobial properties of the product matrix or residual disinfectants in samples, allowing for accurate recovery of viable microorganisms. |
| Growth Media and Supplements | Supports the growth and recovery of microorganisms; used in compendial parallel testing and for the revival of challenge organisms. |
| Product-Specific Matrix (Placebo) | Allows for interference testing without the confounding variable of an active pharmaceutical ingredient, helping to isolate matrix-specific effects. |
Detailed Experimental Protocols
Protocol 1: Demonstrating Method Equivalency through Parallel Testing This protocol is designed to validate a Rapid Microbiological Method (RMM) against a compendial method, as required by USP <1223> and Ph. Eur. 5.1.6. [2] [3]
- Define Scope: Clearly state the method's purpose (e.g., bioburden testing, sterility testing), sample type, and target microorganisms. [2]
- Select Challenge Strains: Choose appropriate compendial and product-specific isolates. [2]
- Prepare Inoculum: Create suspensions of challenge organisms at target concentrations in a product placebo and the actual product matrix. [2]
- Parallel Testing: Test each inoculated sample type in parallel using both the RMM and the compendial method (e.g., plate count). Use a statistically significant number of replicates (e.g., n≥3 per level). [2]
- Statistical Comparison: Analyze the results using statistical tests (e.g., t-tests, F-tests) to demonstrate equivalency. The RMM should show no significant difference from the compendial method in accuracy, precision, and specificity. [2] [3]
The workflow for this protocol is outlined below.
Protocol 2: Determining Limit of Detection (LOD) and Limit of Quantitation (LOQ) This methodology aligns with the scientific, risk-based approach emphasized in modern pharmacopeias. [2] [26]
- Sample Preparation: Serially dilute a microbial suspension to very low concentrations in a product-specific matrix.
- Testing Dilutions: Test multiple replicates (recommended n≥5) at each dilution level using the verified method.
- Calculate LOD: The LOD is the lowest concentration level at which ≥95% of the replicates give a positive detection signal (for qualitative methods) or a measurable signal above background (for quantitative methods). [2]
- Calculate LOQ: The LOQ is the lowest concentration level that can be quantified with acceptable accuracy (e.g., 50-200% recovery) and precision (e.g., RSD ≤35%). This must be confirmed by direct experimental verification of recovery rates and precision at the claimed LOQ. [2] [26]
The logical relationship for establishing LOD and LOQ is as follows.
Troubleshooting Low Accuracy
If your verification study reveals low microbial recovery, investigate these areas:
- Conduct a Matrix Interference Study: Systematically spike the product with known microbes and compare recovery in the product versus a neutral buffer. If recovery is low in the product, optimize the sample preparation procedure, incorporate dilution, or use a neutralizing agent. [2]
- Verify Inoculum Viability and Count: The starting concentration of your challenge organism must be accurate. Use plate count methods to confirm the inoculum's viable count independently of the method being verified. [2]
- Review Sample Holding Conditions: Ensure that the time and temperature between sample inoculation and testing do not lead to microbial death or proliferation. [5]
Core Concepts: Accuracy and Precision
For qualitative microbiological assays, verifying accuracy and precision is a fundamental requirement before implementing a new, unmodified FDA-cleared test for clinical or research use [27].
- Accuracy confirms the acceptable agreement of results between the new method and a comparative method [27].
- Precision confirms acceptable reproducibility of results, assessing within-run, between-run, and operator variance [27].
The following workflow outlines the core process for planning and executing these verification studies:
Experimental Protocols
Protocol for Accuracy Testing
Accuracy testing demonstrates that your new method correctly identifies target organisms compared to a reference standard [27].
Detailed Methodology:
Sample Selection and Preparation:
Testing Procedure:
- Test all selected samples using the new qualitative assay.
- In parallel, test the same samples using a well-characterized comparative method. This could be the method currently in use in your lab or a reference method [27].
Data Analysis and Acceptance Criteria:
- Calculate the percentage agreement between the new method and the comparative method.
- Formula: (Number of results in agreement / Total number of results) × 100 [27].
- Compare the calculated percentage to the manufacturer's stated claims for accuracy or to a laboratory-defined acceptance criterion approved by the lab director [27].
Protocol for Precision Testing
Precision testing evaluates the reproducibility of your assay results under defined conditions, encompassing repeatability and intermediate precision [28] [27].
Detailed Methodology:
Sample Selection:
Testing Procedure for Intermediate Precision:
Data Analysis and Acceptance Criteria:
Essential Research Reagent Solutions
The table below lists key materials required for conducting accuracy and precision studies:
| Item | Function in Verification |
|---|---|
| Reference Materials & Controls | Certified microbial strains or clinical samples with known status; serve as the benchmark for accuracy testing [27]. |
| De-identified Clinical Samples | Previously characterized patient samples used to verify accuracy and precision in a clinically relevant matrix [27]. |
| Proficiency Test Samples | Externally sourced samples of known, but blinded, identity; provide an unbiased assessment of assay accuracy [27]. |
| Culture Media | Supports growth and viability of challenge microorganisms; used in specificity and accuracy studies [28]. |
| Challenge Microorganisms | A panel of relevant microbial strains used to demonstrate the method's specificity and ability to detect the target in the presence of other organisms [28]. |
Troubleshooting Low Accuracy
FAQ: Why is my new assay showing low accuracy compared to my reference method?
Low accuracy typically manifests as a consistent discrepancy between the results from the new method and the reference method. The following diagram illustrates a logical troubleshooting path for this issue:
Specific Troubleshooting Steps:
- Confirm Sample Quality and Matrix: Ensure samples are stored correctly and are not degraded. For new sample matrices (e.g., different food types, swabs), assess for potential interferents like pectin (inhibits PCR) or high fat content (impedes microorganism access). A method validated for one matrix may not be accurate for another without a fitness-for-purpose study [29].
- Investigate Specificity: The method's ability to correctly identify the target analyte may be compromised. Challenge the assay with closely related non-target organisms to confirm it does not produce false positives. For molecular methods, verify primer/probe specificity [28].
- Re-evaluate the Reference Standard: The comparative method itself may have limitations or be imperfect. Investigate the performance characteristics of your reference method to ensure it is a reliable benchmark [27].
FAQ: My precision study shows high variation between runs and operators. What should I check?
High variation in precision studies points to issues with the method's reproducibility.
Troubleshooting Steps:
- Standardize Operator Technique: This is a common source of variation. Ensure all personnel are thoroughly trained on the standardized protocol. Observe technicians performing the assay to identify deviations in technique [30] [27].
- Check Reagent and Equipment Consistency: Use the same lots of reagents and consumables throughout the study where possible. If different instruments are used, ensure they are properly calibrated and maintained. Document all reagent lots and equipment IDs [31].
- Review Environmental Controls: For methods involving microbial growth, small variations in incubation time or temperature can significantly impact results. Monitor and record environmental conditions to ensure they remain within the manufacturer's specified range throughout the study [28].
Sample Size Requirements for Verification Studies
The table below summarizes the minimum sample sizes and key parameters for accuracy and precision testing as recommended by guidelines:
| Parameter | Minimum Sample Size | Sample Types | Key Calculation |
|---|---|---|---|
| Accuracy [27] | 20 isolates/samples | Combination of positive and negative samples; clinically relevant isolates. | % Agreement = (Results in Agreement / Total Results) × 100 |
| Precision (Intermediate) [27] | 2 positive + 2 negative samples | Tested in triplicate over 5 days by 2 operators. | % Agreement = (Concordant Results / Total Results) × 100 |
| Reportable Range [27] | 3 samples | Known positive samples (for qualitative); samples near upper/lower cutoff (for semi-quantitative). | Confirm result is within the established reportable range. |
| Reference Range [27] | 20 isolates/samples | De-identified clinical or reference samples representing the patient population. | Verify against manufacturer's claims or re-define for local population. |
Failure to properly verify and document performance specifications is a common regulatory citation. The table below lists frequent errors and their solutions:
| Pitfall | Consequence | Solution |
|---|---|---|
| No verification performed; "out-of-the-box" use [30]. | Serious regulatory citation; risk to patient safety and data integrity [30]. | Perform and document full verification before clinical/research use [30]. |
| Only partial verification (e.g., accuracy but not precision) [30]. | Incomplete performance profile; unreliable results for one or more characteristics [30]. | Use a standardized protocol verifying all required parameters [30]. |
| Data exists but is not properly signed, dated, or stored [30]. | Citation during inspection; data may be considered invalid [30]. | Store signed/dated documents in an accessible, version-controlled location [30]. |
| Using a test for a sample matrix not specified by the manufacturer without a fitness-for-purpose study [29]. | Potential for inaccurate results due to matrix interference [29]. | Conduct a matrix extension study to confirm the test performs accurately in the new matrix [29]. |
Protocols for Quantitative and Semi-Quantitative Assay Verification
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between assay validation and verification? A1: Validation is a process to establish that a new or modified assay (such as a laboratory-developed test or a modified FDA-approved test) works as intended. In contrast, verification is a one-time study performed for unmodified, FDA-approved tests to demonstrate that the test performs according to established manufacturer specifications in your laboratory environment [32].
Q2: What are the core performance characteristics that must be verified for a semi-quantitative assay? A2: For semi-quantitative assays, the essential verification parameters are Accuracy, Precision, Reportable Range, and Reference Range [32]. These characteristics confirm the assay provides reliable and reproducible ordinal results (e.g., "negative," "low positive," "high positive").
Q3: My verification shows a high rate of false negatives. What could be the cause? A3: A high false-negative rate often indicates an issue with the assay's diagnostic sensitivity. Potential causes include [33] [34]:
- Improper sample storage or transport, leading to analyte degradation.
- Incorrect incubation times or temperatures.
- Reagent or equipment failure.
- The predefined cutoff value may not be optimal for your specific patient population.
Q4: What is the recommended sample size for verifying accuracy in a qualitative or semi-quantitative assay? A4: It is recommended to use a minimum of 20 positive and negative clinical samples or well-characterized isolates to verify accuracy. For semi-quantitative assays, these should cover a range from high to low values [32].
Q5: How do I handle discrepancies between my verification data and the manufacturer's claims? A5: First, repeat the experiment to rule out one-off operational errors. If discrepancies persist, investigate potential interfering substances in your sample matrix and confirm you are using the correct reference standard. Laboratory leaders, such as clinical microbiologists, should be consulted to review the data and determine if the method is acceptable for clinical use despite the discrepancy [32] [33].
Troubleshooting Low Accuracy in Method Verification
Low accuracy, indicating a failure to establish acceptable agreement with a reference method, is a common challenge. The following guide helps diagnose and resolve the underlying issues.
Troubleshooting Logic and Workflow
The diagram below outlines a systematic approach to troubleshooting low accuracy.
Detailed Investigation Steps
1. Check Sample Integrity & Handling
- Problem: Degraded samples, improper storage conditions, or use of an incorrect sample matrix can yield misleading results [34].
- Action: Verify that all samples were collected, transported, and stored according to the verification plan. Use certified reference materials or previously characterized clinical samples where possible [34].
2. Investigate Reagents & Equipment
- Problem: Expired or improperly reconstituted reagents, and poorly calibrated equipment are frequent sources of error [34].
- Action: Confirm that all reagents are within their expiry date and have been prepared correctly. Review equipment maintenance and calibration logs to ensure instruments are functioning within specified parameters.
3. Review Operator Technique & Protocol
- Problem: Deviations from the standard operating procedure (SOP), such as incorrect incubation times or pipetting errors, directly impact accuracy [34].
- Action: Ensure all personnel are thoroughly trained on the protocol. Implement a review of the technique and consider having a second operator perform the assay to rule out individual error.
4. Re-evaluate Reference Standard & Data Analysis
- Problem: An inappropriate reference standard or flawed statistical analysis can create a false impression of inaccuracy [33].
- Action: Confirm the reference method is the gold standard or a well-validated predicate method. Re-analyze the data using appropriate statistical tools for qualitative/semi-quantitative data, such as contingency tables and inter-rater agreement metrics [33].
Verification Protocols and Data Presentation
Core Verification Experiments and Sample Sizes
The table below summarizes the key experiments, their objectives, and the minimum sample sizes required for verifying qualitative and semi-quantitative assays [32].
| Performance Characteristic | Objective | Minimum Sample Sizes & Design |
|---|---|---|
| Accuracy | To confirm acceptable agreement with a comparative method. | Qualitative: 20+ clinical isolates (combination of positive and negative).Semi-quantitative: 20+ isolates with a range of high to low values [32]. |
| Precision | To confirm acceptable variance (within-run, between-run, between operators). | 2 positive and 2 negative samples, tested in triplicate for 5 days by 2 operators [32]. |
| Reportable Range | To confirm the assay's upper and lower detection limits. | Minimum of 3 known positive samples. For semi-quantitative, include samples near the cutoff values [32]. |
| Reference Range | To confirm the expected "normal" result for the patient population. | Minimum of 20 isolates from the laboratory's typical patient population [32]. |
Example Protocol: Precision Verification for a Semi-Quantitative Assay
This protocol provides a detailed methodology for verifying the precision of a semi-quantitative assay, such as an ELISA-based microneutralization assay [35].
1. Experimental Design
- Samples: Select a minimum of two positive samples with high values and two with low values. Include negative controls [32].
- Replicates: Test each sample in triplicate.
- Duration & Operators: Perform testing over five days with two different analysts [32].
2. Materials and Equipment
- Pre-characterized sample panels (positive and negative).
- All assay reagents (buffers, substrates, etc.).
- calibrated pipettes, incubator, plate reader.
- Data recording sheets or LIMS.
3. Step-by-Step Procedure
- Day 1: Operator 1 prepares all reagents and runs the first batch of triplicates for all samples. Records all raw data and results.
- Day 2-5: Operators 1 and 2 alternate running the assay in triplicate, ensuring independent preparation and execution where applicable.
- Data Analysis: Calculate the percentage of results in agreement for each sample level across all runs and operators. The formula is:
(Number of results in agreement / Total number of results) * 100[32]. - Acceptance Criterion: The calculated percentage of agreement should meet or exceed the manufacturer's stated claims or a pre-defined limit set by the laboratory director [32].
The Scientist's Toolkit: Essential Research Reagents
| Item | Function / Application |
|---|---|
| Certified Reference Materials (CRMs) | Well-characterized microorganisms or analytes with defined profiles used to validate testing methodologies and ensure accuracy [34]. |
| Quality Control (QC) Organisms | Strains with predictable biochemical reactions used to monitor the performance of test methods, reagents, and operators in routine testing [34]. |
| In-House Isolates | Organisms isolated from the laboratory's own environment or historical samples, critical for ensuring tests are validated against relevant, local strains [34]. |
| Clinical Isolates & Bioburden Samples | De-identified patient samples or product samples used to verify assay performance with real-world matrices and assess microbial load [32] [7]. |
| Proficiency Test (PT) Standards | Commercially provided samples used to benchmark laboratory performance against peers and ensure ongoing compliance and accuracy [34]. |
Best Practices for Inoculum Preparation and Standardization
In microbiological method verification research, the accuracy and reproducibility of results are fundamentally dependent on the quality of the initial inoculum. Inoculum preparation and standardization is a critical preliminary step in antimicrobial susceptibility testing (AST) and various microbiological assays. Inconsistent or inaccurate inoculum preparation is a frequent, yet often overlooked, source of error that can lead to incorrect Minimum Inhibitory Concentration (MIC) determinations, misleading susceptibility categorizations, and ultimately, compromised research conclusions. This guide addresses the core principles and common pitfalls of inoculum preparation to help researchers troubleshoot issues related to low accuracy in their experimental results.
Core Concepts and Definitions
Inoculum: A suspension of microorganisms prepared for introducing into culture media for testing purposes. Inoculum Effect (IE): A phenomenon where the observed MIC of an antimicrobial agent depends on the initial density of bacteria inoculated into the assay [36]. This effect is most pronounced for β-lactam antibiotics against strains expressing β-lactamase enzymes. Colony Forming Unit (CFU): A unit used to estimate the number of viable microorganisms in a sample. McFarland Standard: A scale used to standardize the approximate number of bacteria in a liquid suspension based on turbidity.
FAQs on Inoculum Preparation
Q1: Why is inoculum standardization so critical for antimicrobial susceptibility testing?
The initial density of bacteria in an AST directly influences the outcome, a phenomenon known as the inoculum effect (IE). For certain antibiotic-bacterium combinations, even small variations in the starting inoculum within the acceptable range can lead to major discrepancies in the MIC value. One study demonstrated that for carbapenem-resistant Enterobacteriaceae, each 2-fold reduction in inoculum resulted in a 1.26 log₂-fold reduction in meropenem MIC. This effect can be sufficient to change the categorical interpretation of an isolate from "resistant" to "susceptible," leading to potential errors in research conclusions and their clinical application [36].
Q2: What is the target inoculum density for standard broth microdilution tests?
For reference broth microdilution (BMD) AST, the Clinical and Laboratory Standards Institute (CLSI) mandates a standardized inoculum density of 5 × 10⁵ CFU/ml, with an allowable range of 2 × 10⁵ to 8 × 10⁵ CFU/ml [36]. Adherence to this range is essential for achieving reproducible and accurate results that are comparable across different laboratories and studies.
Q3: My prepared inoculum suspension is at the correct McFarland turbidity. Why is my final CFU/ml still inaccurate?
Turbidity standards provide an approximation, but several factors can cause a deviation from the expected cell density:
- Temperature Exposure: Exposing the inoculum suspension to increased temperature can lead to cell death or affect the cell division cycle, artificially altering the number of viable cells (CFU) [37].
- Culture Age and Viability: Using an culture that is too old or not in the optimal growth phase can result in a high proportion of non-viable cells, meaning the turbidity reflects both live and dead cells.
- Mixing and Technique: Inadequate mixing of the suspension before sampling or improper serial dilution techniques can lead to inconsistent cell distribution and inaccurate counts [38].
- Organism Characteristics: Clumping or chaining behavior in some bacterial species (e.g., Staphylococcus aureus) means that one colony may not originate from a single cell, making turbidity correlations less reliable.
Q4: What are the best sources for preparing a standardized inoculum?
The source of growth significantly impacts the final viable count. Studies comparing different methods have found that inocula prepared from broth suspensions of organisms harvested from 24- and 48-hour anaerobe blood agar plates yielded the most consistent and highest viable counts across various organisms when adjusted to the 0.5 McFarland standard. This method often produces higher counts than using overnight broth cultures adjusted to the same turbidity [39]. Using overnight agar cultures is an acceptable and often preferred alternative procedure [40].
Troubleshooting Guides
Guide: Inconsistent Results in Susceptibility Tests
Problem: High variability in MIC readings or zone of inhibition diameters between replicate experiments. Potential Causes and Solutions:
- Cause: Inoculum density outside the validated range.
- Solution: Consistently use viable count methods (pour or spread plate) to verify the actual CFU/ml of your working suspension, rather than relying solely on turbidity. Store verified dilutions at 2-8°C for short-term use [41].
- Cause: Uncontrolled Inoculum Effect.
- Solution: Be aware that for specific drug-bug combinations (e.g., β-lactams against ESBL-producers), the IE can be pronounced. If erratic results persist, test at both the standard and a higher inoculum to investigate the presence of a significant IE [36].
- Cause: Improper storage and handling of the inoculum.
Guide: Unexpected Quantitative Results in Culture-Based Assays
Problem: Microbial counts on plates are consistently higher or lower than theoretically calculated. Potential Causes and Solutions:
- Cause: Errors in serial dilution technique.
- Solution: Use fresh, sterile diluent (e.g., 0.1% peptone saline) for each dilution series. Ensure each dilution tube is mixed thoroughly before transferring to the next. Use a new pipette tip for each transfer to prevent carryover [41].
- Cause: Degradation or quality issues with the culture media.
- Solution: Check the expiry date of the media. Look for signs of degradation like color change, cracking, or excessive moisture. Avoid repeated melting and overheating of agar media, as this can degrade key components and affect growth [38].
- Cause: Incorrect pH of the culture medium.
- Solution: Measure the pH of the medium within the specified temperature range (e.g., 10-37°C) using a properly calibrated pH meter with a suitable electrode. Overheating during sterilization or contaminated water can alter the pH [38].
Data Presentation
Table 1: Impact of Inoculum Effect on MIC for Different Antibiotic Classes
| Antibiotic Class | Example Agent | Organism Type | Observed MIC Change with High Inoculum* | Clinical/Risk Implication |
|---|---|---|---|---|
| β-lactams (Carbapenems) | Meropenem | Carbapenem-resistant Enterobacteriaceae (CRE) | 8.3 ± 1.8 log₂ dilutions (∼315-fold increase) | Major shift; can cause false susceptible (minor error) at low inoculum [36] |
| β-lactams (Cephalosporins) | Cefepime | ESBL-producing E. coli/Klebsiella (Resistant/SDD) | 1.6 log₂-fold increase per 2-fold inoculum increase | Significant shift affecting categorical interpretation [36] |
| β-lactam/β-lactamase inhibitor | Ceftazidime-Avibactam | CZA-resistant Enterobacteriaceae (non-NDM) | Modest IE (2.9 log₂ difference from highest to lowest inoculum) | Less pronounced effect compared to other β-lactams [36] |
Note: *High inoculum is typically 100-fold greater than the CLSI standard of 5 x 10⁵ CFU/ml, unless otherwise specified. SDD = Susceptible-Dose Dependent.
Table 2: Standardized Inoculum Preparation Protocols for Different Microorganism Types
| Microorganism Type | Recommended Growth Medium | Incubation Conditions | Expected Broth Density | Dilution Method for ~10-100 CFU | Enumeration Method |
|---|---|---|---|---|---|
| Aerobic Bacteria | Soybean Casein Digest Broth | 30-35°C for 24 hours | ~10⁹ CFU/ml | Serial dilution in 0.1% peptone saline [41] | Pour Plate or Spread Plate [41] |
| Anaerobic Bacteria | Cooked Meat Medium | 30-35°C for 24-48 hours | ~10⁸ CFU/ml | Serial dilution in 0.1% peptone saline [41] | Pour Plate (anaerobic conditions) |
| Yeast | Soybean Casein Digest Broth | 20-25°C for 48-72 hours | ~10⁸ CFU/ml | Serial dilution in 0.1% peptone saline [41] | Spread Plate |
| Mold | Soybean Casein Digest Broth | 30-35°C for 120 hours | ~10⁸ CFU/ml | Serial dilution in 0.1% peptone saline [41] | Spread Plate |
Experimental Protocols
Detailed Protocol: Inoculum Preparation and Standardization by Direct Colony Suspension
This is a standard method for preparing an inoculum from fresh agar plates.
Principle: To create a standardized suspension of microorganisms directly from isolated colonies on an agar plate, adjusted to a specific turbidity, which can then be diluted to the precise density required for testing [40] [41] [39].
Materials:
- Working culture slants or plates (18-24 hours old for bacteria; 48-72 hours for yeast)
- Sterile saline, phosphate-buffered saline, or 0.1% peptone water
- McFarland 0.5 turbidity standard or a photometric device
- Sterile swabs or inoculation loops
- Sterile test tubes
- Vortex mixer
- Spectrophotometer (optional, for precise turbidity)
Procedure:
- Harvest Colonies: Using a sterile loop or swab, gently select several well-isolated colonies of similar morphology from the agar plate.
- Prepare Initial Suspension: Transfer the colonies into a tube containing sterile saline or peptone water.
- Vortex: Vortex the suspension vigorously for 15-30 seconds to achieve a smooth, homogenous suspension without clumps.
- Adjust Turbidity: Compare the suspension's turbidity against the McFarland 0.5 standard under good light. Add more bacteria or diluent until the turbidity matches the standard. This results in a suspension of approximately 1-2 x 10⁸ CFU/ml for most bacteria.
- Confirm Density (Critical for Verification): Perform a viable count to confirm the exact density. Make serial dilutions (e.g., 10⁻¹ to 10⁻⁸) of the standardized suspension in 0.1% peptone saline [41]. For each dilution, use either the pour plate method (mixing 1 ml with molten agar) or the spread plate method (spreading 0.1 ml on the surface of pre-poured agar). Incubate plates and count colonies to calculate the CFU/ml of the original suspension.
- Prepare Working Dilution: Dilute the standardized suspension in broth or saline to achieve the final target density required for your specific test (e.g., 5 x 10⁵ CFU/ml for BMD).
Detailed Protocol: Investigating the Inoculum Effect
Principle: To evaluate the impact of bacterial inoculum density on the MIC of an antimicrobial agent by testing a range of inocula against a dilution series of the antibiotic.
Materials:
- Standardized bacterial suspension (~1-2 x 10⁸ CFU/ml)
- Cation-adjusted Mueller-Hinton Broth (CAMHB)
- Antimicrobial stock solution
- Sterile 96-well microdilution trays or tubes
- Multipipette
Procedure:
- Prepare Antibiotic Dilutions: Create a 2-fold serial dilution of the antimicrobial agent in CAMHB across the wells of a microdilution tray, as per standard BMD.
- Prepare Inoculum Dilutions: Create a separate 2-fold serial dilution of the standardized bacterial suspension in CAMHB to cover a range below and above the CLSI standard (e.g., from ~10⁴ to 10⁷ CFU/ml).
- Inoculate Trays: Transfer a fixed volume (e.g., 10 µl) of each bacterial inoculum dilution to the corresponding row of wells containing the antibiotic dilutions. This creates an orthogonal matrix where each well has a unique combination of antibiotic concentration and inoculum density.
- Incubate: Incubate the trays at 35±2°C for 16-20 hours.
- Read and Interpret: Determine the MIC for each inoculum level. The MIC is the lowest concentration of antimicrobial that completely inhibits visible growth. An inoculum effect is typically defined as an ≥8-fold increase in MIC when the inoculum is increased 100-fold above the CLSI standard [36].
Workflow Visualization
Inoculum Prep Workflow and Pitfalls
The Scientist's Toolkit
Table 3: Essential Reagents and Materials for Inoculum Standardization
| Item | Function/Benefit | Key Considerations |
|---|---|---|
| 0.1% Peptone Saline | Diluent for preparing serial dilutions. Reduces cell clumping and protects viability compared to plain saline. | Ensure sterility. Prepare fresh frequently or validate storage conditions [41]. |
| McFarland Standards | Provides a visual turbidity reference for standardizing initial bacterial suspensions to ~1-2 x 10⁸ CFU/ml. | Handle carefully; check for precipitation or aging. Replace as recommended. |
| Soybean Casein Digest Agar/Broth | A general-purpose growth medium for cultivating a wide range of non-fastidious aerobic and anaerobic bacteria. | Check for expiration and signs of degradation like discoloration or excessive moisture [38] [41]. |
| Cooked Meat Medium | Recommended for the cultivation and maintenance of anaerobic bacteria for inoculum preparation. | Provides a reducing environment necessary for the growth of strict anaerobes [41]. |
| Sterile Loops/Swabs | For aseptically transferring microbial colonies from solid media to suspension. | Use disposable, pre-sterilized items to prevent cross-contamination. |
Utilizing Certified Reference Materials and Quality Control Organisms
Troubleshooting Guides
FAQ: Addressing Common Issues with CRMs and QC Organisms
Q1: Our method verification results show consistently low accuracy. What is the first element to investigate?
A: The first elements to investigate are the Certified Reference Materials (CRMs) and Quality Control (QC) organisms you are using. You must confirm that the CRM is appropriate for your specific matrix and method. Using an incorrect CRM or QC organism is a primary source of inaccuracy [29]. Begin by verifying the certificate of analysis for the CRM to ensure it is within its validity period and has been stored according to the manufacturer's specifications. Improper storage conditions can compromise microbial viability and lead to inaccurate counts [42].
Q2: When we perform a dilution series of a QC organism for a quantitative method, our results are imprecise. What are the potential causes?
A: Imprecise results in a dilution series often stem from technical errors in sample handling or issues with the QC organism itself. Key areas to check include:
- Pipetting Technique: Ensure calibrated pipettes and proper technique are used to avoid volumetric errors [42].
- Homogeneity of the Culture: The microbial suspension must be thoroughly mixed before each dilution step to ensure a homogeneous distribution of cells. A lack of homogeneity is a common source of variation [28].
- QC Organism Viability: The QC organism may be stressed or non-viable due to improper storage or repeated sub-culturing. Use freshly cultured or properly reconstituted organisms from a reputable source [5].
Q3: Our negative controls are showing growth, compromising our verification study. What should we do?
A: Growth in negative controls indicates contamination, which severely compromises data integrity. Your troubleshooting should focus on sterility [42]:
- Aseptic Technique: Re-train personnel on strict aseptic techniques.
- Sterilization Procedures: Verify the effectiveness of autoclave cycles and the sterility of all media, reagents, and equipment (e.g., pipette tips, dilution tubes) used in the process.
- Environmental Contamination: Monitor the air and surfaces in your laminar flow hood or biosafety cabinet to ensure they are not the source of contamination.
Q4: We are verifying a method for a new food matrix not listed in the CRM's validation certificate. Is the CRM still fit for purpose?
A: Not necessarily. A method validated for one matrix may not be accurate for another due to interfering substances (e.g., fats, acids, inhibitors) [29]. You must perform a "fitness-for-purpose" or matrix extension study. This involves testing the new matrix spiked with the CRM and demonstrating that the method can recover the target microorganisms with acceptable accuracy and precision, as defined by guidelines like those in the ISO 16140 series [29] [14].
Q5: What is the difference between method validation and method verification in this context?
A: This is a critical distinction. Method validation is the process of proving that a method is fit for its intended purpose, typically conducted by the test kit manufacturer or a reference laboratory according to international standards (e.g., ISO 16140-2) [29] [14]. Method verification is your laboratory's responsibility: it is the process of demonstrating that your lab can successfully perform the already-validated method and get the correct results using appropriate CRMs and QC organisms [29] [14]. Troubleshooting low accuracy is a key part of the verification process.
Experimental Protocol: Verification of Method Accuracy Using CRMs
This protocol provides a detailed methodology for verifying the accuracy of a quantitative microbiological method, a common requirement in pharmaceutical and food testing laboratories.
1. Principle To confirm that a laboratory's execution of a validated quantitative method (e.g., pour plate, membrane filtration) can recover a known number of microorganisms from a Certified Reference Material with an accuracy meeting predefined criteria.
2. Materials and Reagents
- Certified Reference Material (e.g., Pseudomonas aeruginosa ATCC 9027, 1000 CFU/vial)
- Non-selective culture medium (e.g., Soybean Casein Digest Agar)
- Diluents (e.g., Buffered Peptone Water, Phosphate Buffered Saline)
- Sterile pipettes and dilution tubes
- Incubator set to appropriate temperature (e.g., 30-35°C)
3. Procedure
- Reconstitution: Aseptically reconstitute the CRM according to the manufacturer's instructions.
- Dilution Series: Perform a serial dilution of the reconstituted CRM in your chosen diluent to achieve a target countable range (e.g., 20-80 CFU for spread plates).
- Inoculation and Plating: Inoculate the test method (e.g., pour plate) in triplicate with at least three appropriate dilution levels.
- Incubation: Incubate the plates under the conditions specified by the method.
- Enumeration: Count the colonies on the plates and calculate the CFU/mL for each dilution level.
4. Calculation of Accuracy Calculate the percentage recovery for each dilution level.
- Percentage Recovery (%) = (Observed CFU Count / Expected CFU Count) x 100
The expected CFU count is derived from the CRM's certificate and your dilution factor.
5. Acceptance Criteria According to pharmacopeial standards and industry best practices, the acceptable range for recovery of quantitative methods is typically 50% to 200% [28]. The mean recovery from your triplicate tests should fall within this range. Tighter internal limits (e.g., 70%-130%) may be set based on product or method requirements.
Data Presentation: Key Validation Parameters and Acceptance Criteria
The table below summarizes critical validation parameters that should be assessed during method validation and monitored during verification using CRMs and QC organisms. These parameters are essential for diagnosing the root causes of low accuracy [28].
Table 1: Critical Validation Parameters for Microbiological Methods
| Parameter | Definition | Typical Acceptance Criteria | Role of CRMs/QCs |
|---|---|---|---|
| Accuracy | Closeness of agreement between the measured value and the true value. | Recovery of 50% - 200% for quantitative methods [28]. | CRMs provide the "true value" to calculate percentage recovery. |
| Precision | Closeness of agreement between a series of measurements. | Expressed as Standard Deviation or Coefficient of Variation. Low variation in replicate tests. | QC organisms are used in repeatability studies to measure variation. |
| Specificity | Ability to unequivocally assess the target microorganism in the presence of other components. | All challenge microorganisms are recovered without interference [28]. | QC organisms are used to challenge the method to ensure it detects the target. |
| Limit of Detection (LOD) | The lowest number of microorganisms that can be detected. | Consistent detection of a low-level challenge (<100 CFU) [28]. | Diluted QC organisms are used to establish the minimal detectable level. |
| Robustness | Reliability of the method under small, deliberate variations in parameters. | Method performs acceptably under varied conditions (e.g., different technicians, incubation times). | QC organisms are tested under the varied conditions to ensure consistent performance. |
Workflow Diagram: Troubleshooting Low Accuracy
The following diagram outlines a systematic workflow for troubleshooting low accuracy in microbiological method verification, from initial observation to resolution.
Systematic troubleshooting workflow for low accuracy in method verification.
The Scientist's Toolkit: Research Reagent Solutions
This table details essential materials used for ensuring accuracy in microbiological method verification.
Table 2: Essential Research Reagents for Quality Assurance
| Item | Function & Importance | Key Considerations for Use |
|---|---|---|
| Certified Reference Materials (CRMs) | Provides a traceable, known quantity of microorganisms to validate method accuracy and establish a baseline for recovery calculations [29]. | Must be appropriate for the tested matrix and method. Always check the scope of validation and certificate of analysis [29] [14]. |
| Quality Control (QC) Organisms | Used for routine monitoring of method performance, including precision, specificity, and robustness. Typically from in-house or commercially sourced strains [5]. | Maintain proper storage and passage records to prevent genetic drift and loss of viability, which can affect results [5]. |
| Selective and Non-Selective Culture Media | Supports the growth and/or differentiation of target microorganisms. The foundation of most culture-based methods. | Performance testing is critical. Check for sterility and productivity (ability to support growth of low numbers of target organisms) [42] [28]. |
| Reference Methods | The standardized method (e.g., from USP, ISO, Ph. Eur.) against which an alternative method is compared during validation [43] [14]. | Serves as the benchmark. Your verification study must demonstrate that your results are comparable to those obtained by the reference method. |
Diagnosing and Correcting Low Accuracy: A Systematic Troubleshooting Protocol
Investigating Sample Collection, Transport, and Interference Issues
FAQs on Sample Integrity
What are the most critical pre-analytical factors affecting the accuracy of microbiological tests?
The most critical factors are often related to sample collection and transport. Using an inappropriate collection device (e.g., a dry swab when fluid is required), exceeding recommended transport times, or storing samples at incorrect temperatures can significantly reduce microbial viability and lead to false-negative results [44]. Furthermore, contamination during collection, often from improper skin cleansing or exposure to environmental microbes, can cause false-positive results [45] [44].
How can I troubleshoot issues with contaminated cultures?
Recurring contamination often points to systemic issues. Key areas to investigate include:
- Personnel Practices: Ensure adherence to proper aseptic technique, hand hygiene, and use of personal protective equipment (PPE) [45].
- Environmental Controls: Verify the performance of biosafety cabinets, HEPA filters, and HVAC systems. Implement routine environmental monitoring using air samplers and surface swabs to identify contamination sources [45].
- Equipment & Reagents: Confirm that sterilizers are functioning correctly and that culture media and reagents are sterile and not expired [45].
Our method verification studies show low accuracy compared to compendial methods. What should we check?
Low accuracy in verification can stem from several issues. First, ensure the alternative method has been properly validated according to guidelines like USP <1223>, which requires demonstrating equivalency in accuracy, precision, and specificity [46]. Second, review sample preparation; components of your sample (e.g., particulates, pigments, or antimicrobial properties) may interfere with the detection method [47]. Finally, confirm that all laboratory equipment, including incubators and pipettes, has undergone proper Installation, Operational, and Performance Qualification (IOPQ) to ensure it functions as specified [48].
Troubleshooting Guides
Guide 1: Troubleshooting Invalid or Discarded Samples
Samples that are improperly collected, labeled, or transported are often rejected, causing delays.
- Problem: Sample is received in the lab with an inappropriate transport device or is leaking.
- Solution: Create and distribute a detailed specimen collection manual to all clinical personnel. Standardize kits for specific tests to ensure the correct swabs, containers, and transport media are used [44].
- Problem: Sample transport time exceeds the stability window.
- Solution: Refer to the table below for stability requirements and optimize laboratory logistics, such as using pneumatic tube systems for appropriate specimens or implementing runner services [44].
- Problem: Inadequate sample volume, especially for critical tests like Blood Cultures or CSF analysis.
- Solution: For adult blood cultures, drawing 20 mL and inoculating one aerobic and one anaerobic bottle with 10 mL each is critical. Low volumes adversely affect organism recovery [44]. For CSF, establish clear protocols for prioritizing tests when volume is low.
Guide 2: Troubleshooting Discordant Results in Method Verification
When your new method yields results that differ from the validated compendial method, follow this logical path to identify the source of interference or error.
Acting on the Diagnosis:
- Sample Interference: Modify the sample preparation protocol to remove interferents, for example, through dilution, filtration, or centrifugation [47].
- Equipment Not Qualified: Perform or re-perform Installation, Operational, and Performance Qualification (IOPQ) on the instrument. This confirms it is installed correctly, operates to manufacturer specs, and performs consistently in your lab environment [48].
- Incomplete Method Validation: Revisit the validation study. USP <1223> requires demonstrating equivalency through accuracy, precision, specificity, limit of detection, and robustness [46].
- Viable But Non-Culturable (VBNC) Organisms: Some rapid methods detect metabolic markers from organisms that traditional culture methods cannot grow. This may not be an error but a more sensitive detection, which should be understood and documented as part of the method's performance [47].
Data Presentation
Sample Transport and Stability Requirements
The following table summarizes key transport conditions for various sample types to maintain sample integrity before analysis [44].
| Specimen Type | Preferred Transport Device | Transport Temperature | Maximum Transport Delay (if delayed) | Special Handling Notes |
|---|---|---|---|---|
| Abscess/Aspirate | Anaerobic transport vial (fluid) or jar (tissue) | Room Temperature | ≤ 2 hours | Aspirates are superior to swabs. Deliver immediately for anaerobic culture. |
| Blood Culture | Aerobic & Anaerobic blood culture bottles | Room Temperature | ≤ 2 hours | Draw 20 mL blood total (10 mL per bottle). Inadequate volume reduces sensitivity. |
| Cerebrospinal Fluid (CSF) | Sterile, leak-proof container | Room Temperature | ≤ 15 minutes | Do not refrigerate. Prioritize microbiology lab delivery for culture. |
| Urine | Sterile, leak-proof container | Refrigerated | ≤ 30 minutes | Must be refrigerated if transport is delayed beyond 30 minutes. |
| Stool | Enteric pathogen transport vial | Refrigerated | ≤ 1 hour | Refrigerate promptly if transport is delayed. |
| Swab (Aerobic) | Liquid Amies Elution Swab (ESwab) or equivalent | Room Temperature | ≤ 2 hours | Swabs are inferior to tissue or fluid for fungal/mycobacterial culture. |
Comparison of Microbial Detection Methods
Understanding the principles and limitations of different methods is crucial for selecting and troubleshooting the right assay [49] [47].
| Method Type | Examples | Time to Result | Key Advantages | Key Limitations/Interference |
|---|---|---|---|---|
| Traditional Culture | Disk diffusion, Broth dilution | Days to weeks | Low cost, well-understood | Slow, labor-intensive, subjective, cannot detect VBNC [49] [47] |
| Growth-Based Rapid | Bioluminescence (ATP), Colorimetry | Hours to 1-2 days | Faster than traditional methods | May require enrichment; can be affected by sample turbidity or pigments [47] |
| Viability-Based Rapid | Flow Cytometry | Hours | Can detect VBNC states, high sensitivity | Complex sample prep, instrument cost, can be limited to filterable liquids [49] [47] |
| Molecular-Based Rapid | PCR, DNA Sequencing | Hours | High specificity and sensitivity, identifies organisms | Detects DNA from dead cells, requires technical expertise, higher cost per test [49] [45] [47] |
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function |
|---|---|
| Liquid Amies Elution Swab (ESwab) | Maintains viability of a wide range of aerobic and facultative anaerobic organisms during transport, superior to dry swabs [44]. |
| Anaerobic Transport Vial | Preserves an anaerobic atmosphere for strict anaerobic bacteria, which can be killed by oxygen exposure during transport [44]. |
| Resazurin Dye | An oxidation-reduction indicator used in assays to measure microbial growth; a color change from blue to pink/purple indicates metabolic activity [49]. |
| Adenosine Triphosphate (ATP) Reagents | Used in bioluminescence-based rapid methods. Luciferase enzymes react with ATP from viable microbes to produce light, quantifying microbial load [47]. |
| Blood Culture Bottles (Aerobic/Anaerobic) | Contain specialized media and resins to neutralize antimicrobial agents in the sample, improving the recovery of microorganisms from blood [44]. |
Optimizing Neutralization Strategies for Antimicrobial Products
Frequently Asked Questions (FAQs)
Q1: What is method suitability testing and why is it critical for microbiological quality control?
Method suitability testing is a process that evaluates and neutralizes the inherent antimicrobial activity of a pharmaceutical product during microbial limit tests. It is critical because it ensures the reliability of quality control results. If antimicrobial activity is not properly neutralized, it can inhibit the growth of microorganisms present in the product, leading to "false negatives." This creates a risk that contaminated products could be released to the market, as the test would fail to detect contaminants that could multiply during storage or use, posing potential health risks to consumers [50] [51].
Q2: According to pharmacopeial standards, what should be done if a product's antimicrobial activity cannot be neutralized?
If all suitable neutralization methods (such as dilution, chemical neutralization, or membrane filtration) have been exhausted and the antimicrobial activity still cannot be neutralized during a sterility test, it can be assumed that the failure to recover inoculated microorganisms is due to the product's antimicrobial properties. This indicates that the product is not likely to be contaminated with the non-recovered test microorganisms. However, it is crucial to first demonstrate that all feasible neutralization strategies have been attempted [52].
Q3: What are the common causes of low accuracy or "false negatives" in microbial recovery tests?
The most common cause of false negatives is the presence of residual antimicrobial activity that has not been adequately neutralized. This can stem from:
- Active Pharmaceutical Ingredients (APIs): The drug substance itself may have antimicrobial properties [50].
- Preservatives: Chemicals added to the product to inhibit microbial growth [53].
- Disinfectant Residues: Traces of disinfectants used on manufacturing equipment or testing surfaces can carry over into the test sample and inhibit growth [54]. Without an effective neutralizer in the culture media, these residues can prevent the growth of microorganisms that are actually present, compromising the test's accuracy [54].
Q4: How do I select the right neutralizer for my product?
There is no single universal neutralizer for all substances. The selection depends on the specific antimicrobial agent present. A systematic approach is required:
- Identify the Antimicrobial Agent: Determine the source of the activity (e.g., API, preservative, disinfectant).
- Consult Literature and Standards: Refer to pharmacopeia and scientific literature for known effective neutralizers for that agent [54].
- Experimental Validation: Test the candidate neutralizer for both efficacy (its ability to stop the antimicrobial activity) and toxicity (that it is not inherently toxic to the microorganisms you are trying to recover) [54] [53]. For complex products, a combination of neutralizers may be necessary.
Q5: What are some specific neutralizers used for common antimicrobial agents?
The table below lists some common neutralizing agents and their applications [50] [54] [53].
| Neutralizing Agent | Commonly Used To Neutralize |
|---|---|
| Polysorbate (Tween) 80 | Phenolics, iodine, alcohols, parabens |
| Lecithin | Quaternary ammonium compounds, benzalkonium chloride, chlorhexidine |
| Sodium Thiosulfate | Halogens (e.g., chlorine), aldehydes |
| Sodium Pyruvate / Cysteine | Hydrogen peroxide and other oxidizing agents |
| Beta-lactamase | Beta-lactam antibiotics (e.g., penicillins) |
| Dilution | General method to reduce concentration of antimicrobial substance |
Troubleshooting Low Microbial Recovery
Low microbial recovery during method suitability testing indicates that the neutralization strategy is not effective. The following troubleshooting guide outlines common problems and proven solutions based on recent research.
| Problem | Possible Cause | Solution & Experimental Protocol to Trial |
|---|---|---|
| Low recovery of challenge organisms | Residual activity of preservatives or APIs. | Protocol: Validate a chemical neutralizer system. Prepare in-house neutralizing systems using cost-effective materials like polysorbate 80, cetomacrogol 1000, and polyoxyl 40 hydrogenated castor oil in various combinations (e.g., 1-3% concentrations). Test for toxicity and efficacy per USP <1227> by inoculating a low count (10²-10³ CFU) of standard strains and comparing recovery to controls [53]. |
| Persistent inhibition despite neutralizer | High potency of antimicrobial product. | Protocol: Increase dilution factor with diluent warming. Perform sequential trials of increasing dilution factors (e.g., 1:10, 1:20, up to 1:200). Combine this with warming the diluent to 35-40°C to improve solubility and efficacy of the neutralizer. This method successfully neutralized 18 out of 40 challenging products in a recent study [50] [51]. |
| No growth in filtration methods | Antimicrobial agent binding to filter or not being rinsed effectively. | Protocol: Optimize filtration and rinsing. Use different membrane filter types (e.g., varying materials and pore sizes) and implement multiple rinsing steps with a larger volume (e.g., 3 x 100 mL) of a rinsing fluid that contains a neutralizer like polysorbate 80 or lecithin. This was critical for neutralizing 13 challenging antimicrobial drugs [50]. |
| Inconsistent results across microbial strains | Neutralizer is effective for some organisms but not others. | Protocol: Employ a universal neutralizer and include a broader range of challenge strains. Use a combination neutralizer, such as D/E Neutralizing Agar containing lecithin, polysorbate 80, and sodium thiosulfate. Include environmentally isolated and resilient strains like Burkholderia cepacia and Aspergillus niger in your suitability tests alongside standard strains [50] [54] [53]. |
Workflow for Neutralization Strategy Optimization
The following diagram illustrates a systematic workflow for developing an effective neutralization strategy, integrating the troubleshooting solutions from the table above.
The Scientist's Toolkit: Key Reagent Solutions
The table below details essential reagents and materials used in developing and optimizing neutralization strategies.
| Reagent / Material | Function in Neutralization | Brief Explanation & Application |
|---|---|---|
| Polysorbate 80 (Tween 80) | Non-ionic surfactant | Neutralizes phenolic compounds, iodine, and alcohols by solubilizing them and preventing their action on microbes. Often used at 1-5% concentration [50] [53]. |
| Lecithin | Phospholipid | Acts as a surface-active agent to neutralize quaternary ammonium compounds, chlorhexidine, and parabens by binding to them. Commonly used at ~0.7% concentration [50] [54]. |
| Sodium Thiosulfate | Reducing agent | Effective against halogen-based disinfectants (e.g., chlorine) and aldehydes by reducing them to inactive forms [54]. |
| D/E Neutralizing Agar | Universal neutralizer | A combination of lecithin, polysorbate 80, and sodium thiosulfate designed to inactivate a wide spectrum of disinfectants in environmental monitoring [54]. |
| Beta-lactamase | Enzymatic inactivator | Specifically hydrolyzes and inactivates beta-lactam antibiotics (e.g., penicillins) during the testing of antibiotic products [54]. |
| Membrane Filters | Physical separation | Used in membrane filtration methods to separate microorganisms from the antimicrobial product. Different materials (cellulose nitrate, acetate) and pore sizes are tested for optimal recovery [50]. |
Frequently Asked Questions (FAQs)
FAQ 1: What is the purpose of method suitability testing in microbiological quality control? Method suitability testing verifies that the analytical method can reliably detect microorganisms in a product by neutralizing any inherent antimicrobial activity. It ensures that the test results accurately reflect the microbial quality of the product and are not falsely negative due to residual antimicrobial effects from the product's formulation [50] [51].
FAQ 2: Why is neutralization critical, and what happens if it is not achieved? According to compendial guidelines like the USP, if a product's antimicrobial activity cannot be neutralized, it is assumed that the inhibited microorganisms are not present. This assumption can be risky, as it may lead to the release of contaminated products, potentially resulting in health risks to consumers or even death if contaminants multiply during storage or use [50] [51].
FAQ 3: What are the most common challenges faced during method suitability testing? Challenges often involve effectively neutralizing the antimicrobial properties of the Active Pharmaceutical Ingredient (API) or preservatives. This may require optimizing dilution factors, selecting appropriate chemical neutralizers, or employing membrane filtration with multiple rinsing steps to achieve acceptable microbial recovery without toxic effects on the test microorganisms [50] [51].
FAQ 4: How do you select the appropriate neutralization method for a challenging product? Selection follows a structured approach, beginning with simple dilution and progressively incorporating more complex strategies. This can include increasing dilution factors, adding chemical neutralizers like polysorbate (Tween) and lecithin, using membrane filtration with different filter types, or combining these methods. The optimal method is confirmed by demonstrating acceptable recovery of standard microbial strains [50].
Troubleshooting Guides
Guide 1: Systematic Approach to Neutralization
Problem: Low microbial recovery during method suitability tests for a non-sterile oral suspension.
Investigation & Solution:
- Initial Check: Perform a 1:10 dilution of the product in a buffered peptone solution. If microbial recovery remains below acceptable limits, proceed with optimization.
- Dilution & Heat: Test a 1:10 dilution with the diluent warmed to
45°Cto enhance solubility and dispersion of the product. - Add Chemical Neutralizers: If recovery is still low, incorporate chemical neutralizers into the dilution medium. A common effective combination is
1-5% Polysorbate 80with0.7% Lecithin[50]. - Membrane Filtration: For products with strong antimicrobial activity (e.g., antibiotics), use membrane filtration. Pass the diluted product through a
0.45µmmembrane filter, followed by multiple rinses (e.g.,3 x 100mL) with buffered peptone solution to ensure complete removal of antimicrobial residues before placing the membrane on the culture medium [50].
Guide 2: Troubleshooting Low Counts in Filtration Methods
Problem: Low microbial counts are observed even after membrane filtration and rinsing.
Potential Causes and Corrective Actions:
- Cause 1: Toxicity of the Filter Membrane.
- Action: Test different types of membrane filters (e.g., cellulose nitrate vs. mixed cellulose ester) to identify one with no inherent toxicity to microorganisms [50].
- Cause 2: Inadequate Rinsing.
- Action: Increase the volume or number of rinses with a suitable rinsing fluid (e.g., buffered sodium chloride-peptone solution) to ensure all antimicrobial agent traces are removed from the filter.
- Cause 3: Physical Retention of Microbes.
- Action: For viscous products, consider increasing the pre-filtration dilution factor or using a surfactant in the dilution fluid to reduce viscosity and improve microbial passage through the filter [50].
Data Presentation
The following table consolidates strategies from a study of 133 pharmaceutical products, detailing the methods used to neutralize 40 challenging products [50].
| Product Category | Number of Products | Primary Neutralization Method | Key Parameters & Reagents |
|---|---|---|---|
| Products with mild inherent activity | 18 | Dilution with Diluent Warming | 1:10 dilution, diluent warmed to 45°C |
| Excipient-driven activity | 8 | Dilution with Surfactant | 1:10 dilution, plus 1% Tween 80 |
| Potent Antimicrobials | 13 | High Dilution & Membrane Filtration | Dilution factors from 1:100 to 1:200, multiple rinses with 100-200mL of buffered peptone solution, various filter types |
Table 2: Acceptance Criteria for Microbial Quality of Non-Sterile Products
Acceptance criteria for non-sterile pharmaceutical products vary by dosage form and intended use, as per the United States Pharmacopeia (USP) [50].
| Dosage Form & Intended Use | Total Aerobic Microbial Count (TAMC) (CFU/g or mL) | Total Yeast & Mold Count (TYMC) (CFU/g or mL) | Specific Pathogens to be Absent (in 1 g or 1 mL) |
|---|---|---|---|
| Oral Use (Nonaqueous) | 10³ | 10² | Escherichia coli |
| Oral Use (Aqueous) | 10² | 10¹ | E. coli, Burkholderia cepacia |
| Cutaneous Use | 10² | 10¹ | Staphylococcus aureus, Pseudomonas aeruginosa |
| Inhalation Use | 10² | 10¹ | S. aureus, P. aeruginosa, B. cepacia, bile-tolerant Gram-negative bacteria |
Experimental Protocols
Protocol 1: Standard Method Suitability Test for Microbial Enumeration
Objective: To validate the method for Total Aerobic Microbial Count (TAMC) and Total Combined Yeast and Mold Count (TYMC) by neutralizing the product's antimicrobial activity.
Materials:
- Test Strains: Staphylococcus aureus (ATCC 6538), Pseudomonas aeruginosa (ATCC 9027), Bacillus subtilis, Candida albicans (ATCC 10231), Aspergillus brasiliensis (ATCC 16404) [50].
- Culture Media: Soybean-Casein Digest Agar (SCDA/Tryptone Soy Agar) for TAMC, Sabouraud Dextrose Agar (SDA) for TYMC [50].
- Diluent: Buffered sodium chloride-peptone solution.
- Neutralizing Agents: Polysorbate 80 (Tween 80), Lecithin.
Procedure:
- Inoculum Preparation: Suspend colonies of each test strain in diluent and adjust the turbidity to match a 0.5 McFarland standard. Prepare serial dilutions to obtain a working inoculum of
< 100 CFUper test volume [50]. - Test Preparation: Mix the product with the chosen diluent and neutralizers according to the strategy being validated (e.g.,
1:10dilution with1% Tween 80). - Inoculation: Add the prepared inoculum (not exceeding
1%of the volume of the test preparation) to the product-diluent mixture. - Control Preparation: Add the same volume of inoculum to a separate container with diluent only (no product) to act as a growth control.
- Plating & Incubation:
- For TAMC, spread
1 mLof the inoculated test preparation and control onto SCDA plates. Incubate at30-35°Cfor3-5 days. - For TYMC, spread
1 mLonto SDA plates. Incubate at20-25°Cfor5-7 days.
- For TAMC, spread
- Calculation & Interpretation: After incubation, count the colonies and calculate the percentage recovery for each microorganism.
- Recovery (%) = (CFU from test preparation / CFU from control) × 100%.
- The method is suitable if the average recovery of each test microorganism is not less than
70%[50].
The Scientist's Toolkit
Table 3: Essential Reagents for Method Suitability Testing
| Reagent / Material | Function in Neutralization |
|---|---|
| Polysorbate 80 (Tween 80) | Surfactant that neutralizes preservatives like parabens and phenol derivatives by solubilizing and inactivating them [50]. |
| Lecithin | Used to neutralize quaternary ammonium compounds and other preservatives by forming complexes with them [50]. |
| Buffered Peptone Solution | A general-purpose diluent that maintains osmotic balance and pH, preventing shock to microorganisms during testing. |
| Dey-Engley (D/E) Neutralizing Broth | A general-purpose neutralizing medium effective against a wide range of disinfectants and antimicrobial agents [55]. |
| Membrane Filters (0.45µm) | Used in filtration methods to separate microorganisms from the antimicrobial product solution, which is then rinsed away [50]. |
Method Selection Workflow
The following diagram illustrates the decision-making process for selecting a neutralization method, synthesized from the described protocols [50].
This technical support document synthesizes information from current scientific literature and pharmacopeial guidelines to provide a practical resource for troubleshooting method suitability in microbiological testing. The protocols and data presented are intended for use by qualified professionals in a controlled laboratory setting.
Correcting for Equipment Malfunction and Reagent Degradation
Troubleshooting Guide: Systematic Problem-Solving for Researchers
What is a structured approach to troubleshooting accuracy issues in microbiological method verification?
Think of troubleshooting as a funnel: start with a broad overview and systematically narrow down to identify the root cause. This logical process helps technicians think critically, saving time and resources [56].
The Repair Funnel Method:
- Start with Preliminary Questions: What was the last action before the issue occurred? How frequent is the problem? Check instrument logbooks and software logs for error messages. Historical information and good record-keeping help establish what normal performance looks like [56].
- Isolate the Problem Area: Focus on three main areas to isolate the issue: Is it method-related, mechanical, or operation-related? [56]
- Reproduce the Issue: Determine if it is a recurring problem. Modify parameters to see if you can reproduce the issue. Ensuring you can duplicate the problem is essential to understanding the root cause [56].
- Resist Multiple Fixes: Avoid trying multiple fixes at once, as this causes confusion and delays. Document each step meticulously instead [56].
How can I determine if my accuracy problem is due to equipment malfunction or reagent degradation?
Begin by verifying your method parameters and then systematically isolate components. This "half-splitting" technique efficiently narrows down the potential source.
Step-by-Step Isolation Protocol:
- Confirm Method Parameters: Verify that the method matches what is supposed to be run. Even in labs with locked-down methods, parameters can change accidentally due to software updates or accidental saves. Meticulously check each parameter [56].
- Inspect and Calibrate: For equipment, start with easy fixes. Check for and replace common consumables. Perform maintenance tasks and verify calibration using certified reference materials. Keeping calibration logs helps track performance trends [57].
- Test Reagents: Verify the purity and integrity of all reagents. Use positive and negative controls to establish a baseline for comparison. By comparing your samples to these controls, you can identify deviations that may indicate reagent degradation [58].
- Use Half-Splitting: Instruments often have modular components. For example, in a system with a chromatograph and a mass spectrometer, design an experiment to isolate whether the problem lies on the chromatography side or the mass spectrometer side. This allows you to focus your repair and maintenance efforts correctly [56].
What are the specific steps for investigating suspected microbiological contamination?
Microbiological contamination requires a thorough investigation of the entire production line and factory environment to find the source of the contaminating organism [59].
Investigation Methodology:
- Joint Facility Visit: The process begins with a joint visit to the facility by a microbiologist and a process technician. Understanding the problem on-site is crucial [59].
- Extensive Sampling: Perform extensive sampling all along the production line. This includes raw materials and the product at different stages (e.g., before and after an inactivation step like a heat process). Environmental sampling should include open surfaces with product contact, packaging areas, air, and rinsing water after Clean-in-Place (CIP) processes [59].
- Process Verification: Measure critical process parameters, such as temperatures and effective time in any heat process, inside the actual product. Based on this data, perform calculations to determine if the inactivation process is sufficient to kill the microorganism in focus [59].
- Review Routines and Records: Scrutinize routines for cleaning and disinfection. Review protocols from microbiological analyses over time to understand how the problem may have developed [59].
Frequently Asked Questions (FAQs)
Q: What are the most common equipment failures that lead to inaccurate results?
Common equipment issues often relate to calibration, temperature control, and mechanical wear. The table below summarizes frequent failures and their corrective actions.
Table 1: Common Laboratory Equipment Failures and Corrective Actions
| Failure Type | Examples of Equipment Affected | Troubleshooting Action |
|---|---|---|
| Calibration Errors | Analytical balances, pipettes, spectrophotometers | Recalibrate using certified reference materials according to manufacturer guidelines. Maintain detailed calibration logs [57]. |
| Temperature Control Failures | Incubators, freezers, thermal cyclers | Check for blocked air vents, faulty sensors, or compressor failures. Clean air filters and monitor temperature logs [57]. |
| Mechanical Wear and Tear | Centrifuges, pipettes, shakers | Inspect for misalignment, loose parts, or unusual noises/vibrations. Perform regular lubrication and scheduled inspections [57]. |
| Contamination and Clogging | Pipettes, chromatography systems, spectrophotometers | Flush with appropriate cleaning solutions. Use filtered reagents and implement routine decontamination procedures [57]. |
| Electrical and Power Issues | All electronic instruments | Check power sources, cables, and fuses. Use surge protectors and Uninterruptible Power Supply (UPS) systems for critical instruments [57]. |
Q: How can I prevent cross-contamination from lab tools during sample preparation?
Improperly cleaned tools are a major source of contamination, and up to 75% of laboratory errors occur during the pre-analytical phase [58]. The choice of tool material and strict cleaning protocols are critical.
Prevention Strategies:
- Select the Right Probe: The choice of homogenizer probe impacts contamination risk. While durable, stainless steel probes require meticulous cleaning between samples, which is time-consuming and risks residual analytes. Disposable plastic probes can virtually eliminate cross-contamination for sensitive assays. Hybrid probes offer a middle ground with a stainless steel outer shaft and a disposable plastic inner rotor [58].
- Validate Cleaning Procedures: For reusable tools, validate your cleaning procedures. Run a blank solution after cleaning to ensure no residual analytes are present [58].
- Maintain a Clean Environment: Disinfect lab surfaces with solutions like 70% ethanol or 5-10% bleach. For specific contaminants like residual DNA, use specialized decontamination solutions (e.g., DNA Away) to create a DNA-free environment [58].
- Handle Multi-well Plates with Care: To reduce well-to-well contamination, spin down sealed plates to bring liquid into the well and remove it from the seal. Remove seals slowly and carefully [58].
Q: What criteria should I use to validate that a corrective action has successfully restored method accuracy?
After implementing a fix, you must demonstrate that the method is now reliable, reproducible, and under control. Objective performance data is essential for establishing confidence [60].
Validation Criteria for Corrective Actions:
- Demonstrate Reproducibility: If a sample run indicates the system is fixed, repeat the test to ensure consistency and reproducible results [56].
- Check Specificity and Sensitivity: Ensure the method can accurately detect the target analyte without interference (specificity) and that it is capable of detecting low concentrations of the analyte (sensitivity) [60].
- Verify Against Controls: Use control samples to establish a baseline. Compare your results to these controls to confirm that deviations have been corrected [58]. In microbiological contexts, compare results to the laboratory's historical solvent control values for the particular tester strain [61].
- Review Quality Control Charts: Implement and monitor control charts for key parameters to ensure the process remains stable and within predetermined limits [61] [60].
Workflow Visualization
The following diagram illustrates the logical workflow for systematically troubleshooting low accuracy in microbiological research, integrating the concepts of the repair funnel and half-splitting.
Figure 1: Systematic Troubleshooting Workflow for Low Accuracy.
The Scientist's Toolkit: Research Reagent and Material Solutions
Proper selection and use of materials are fundamental to preventing and correcting issues related to reagent degradation and equipment malfunction.
Table 2: Essential Research Reagents and Materials for Troubleshooting Accuracy
| Item | Function in Troubleshooting | Key Considerations |
|---|---|---|
| Certified Reference Materials | Used for calibrating instruments to ensure measurement accuracy and traceability to standards [57]. | Must be NIST-traceable or equivalent. Stability and storage conditions are critical [62]. |
| Total Organic Carbon (TOC) Analyzer | An acceptable method for detecting organic residue contaminants on equipment surfaces when evaluating cleaning effectiveness [62]. | Justify suitability by confirming the contaminant is organic and contains oxidizable carbon. Account for background carbon levels [62]. |
| Disposable Homogenizer Probes | Single-use probes (plastic or hybrid) minimize the risk of cross-contamination between samples during the initial sample preparation step [58]. | Ideal for high-throughput labs or sensitive assays. Plastic may not be suitable for very tough, fibrous samples [58]. |
| Selection Oligos | Short, complementary oligonucleotides immobilized on beads used to purify gene-construction oligos by stringent hybridization, removing error-containing sequences [63]. | Useful for cleaning up large pools of microarray-derived oligos. Adds burden of synthesizing complementary oligos [63]. |
| Decontamination Solutions | Specialized solutions (e.g., DNA Away, 70% ethanol, 10% bleach) used to eliminate residual analytes from lab surfaces, tools, and equipment [58]. | Choose a solution specific to the contaminant of concern (e.g., DNA, microbes). Part of routine lab cleaning protocols. |
Mitigating Human Error through Training and Competency Assessment
Foundational Concepts: Human Error and Competency
In the context of microbiological method verification, human error refers to unintentional actions or decisions by personnel that result in an undesirable or incorrect outcome, ultimately compromising data accuracy. [64] These errors are influenced by individual, organizational, and contextual factors. A common framework categorizes them into [65] [64]:
- Perceptual Errors: Incorrect interpretation of data or situations.
- Judgment Errors: Incorrect decisions due to cognitive biases or lack of information.
- Execution Errors: Mistakes in performing a task, such as incorrect action or omission.
Competency and Confidence Assessment Modeling (CCAM) is a systematic approach that moves beyond simple knowledge testing to reveal exactly where an individual's skills, knowledge, and capability gaps lie. [66] It assesses not just what an employee understands, but also their confidence in that understanding and whether they are likely to apply correct or incorrect procedures in a high-stakes environment. [66]
FAQs: Addressing Common Challenges in Method Verification
FAQ 1: Our method verification studies keep failing to meet accuracy parameters. Could human error be a factor, and how can we pinpoint the specific causes?
Yes, human error is a likely factor. Uncovering the root causes requires assessing both individual competency and systemic issues.
- Implement a Competency and Confidence Tool: Use specialized assessment tools that employ situational judgement tests to categorize what each team member understands, does not understand, or misunderstands. Crucially, these tools also gauge an individual's confidence in their knowledge, identifying employees who are highly confident in incorrect procedures. [66]
- Conduct a Human Error Analysis: Apply techniques like Human Reliability Assessment (HRA) or Fault Tree Analysis to systematically examine errors in operations. This process helps identify underlying factors such as inattention, fatigue, stress, or insufficient training. [65] [64]
FAQ 2: We have experienced technicians, yet inconsistencies persist between different analysts. What strategies can improve precision?
This issue often relates to intermediate precision—the variation introduced by different analysts, equipment, or reagents. [28] Mitigation strategies include:
- Enhanced Cross-Training: Train analysts on adjacent tasks and implement role rotations to build versatility and a better understanding of how different roles interrelate, reducing mistakes. [67]
- Standardization with Visual Aids: Publish and clearly post work procedures in strategic locations. Use visual aids like color-coded checklists, step-by-step instruction posters, and clear labeling to ensure consistent execution of procedures by all personnel. [68]
- Leverage Technology: Automate repetitive and error-prone tasks like data entry and sample tracking. Implementing a Laboratory Information Management System (LIMS) or barcode scanning can significantly reduce errors associated with manual processes. [64] [68]
FAQ 3: How can we proactively reduce the risk of human error before it affects our research outcomes?
A proactive, systematic approach to human risk management is essential. [64]
- Identify Human Risk Factors: Detect factors like fatigue, stress, distraction, and knowledge gaps. [64]
- Assess Risks: Analyze the probability and potential impact of these factors on data quality. [64]
- Develop Controls: Implement improved procedures, targeted training, and ergonomic workspace design. [64]
- Monitor and Improve: Regularly review the effectiveness of controls and encourage a culture where employees report near-misses without fear of punishment to enable continuous improvement. [64] [68]
Troubleshooting Guide: Low Accuracy in Method Verification
Low accuracy, defined as a lack of agreement between the measured value and the true or expected value, can be investigated using the following guide. [28] [69]
Troubleshooting Workflow for Low Accuracy
Common Issues and Corrective Actions
| Error Symptom | Potential Root Cause | Corrective Action Protocol |
|---|---|---|
| Low Microbial Recovery (<50%) [28] | Incorrect sample preparation (e.g., wrong diluent, temperature); Improper technique (e.g., destructive pipetting, over-vigorous mixing). | 1. Re-train on aseptic technique and sample preparation SOPs using visual guides. [68] 2. Verify competency via a practical demonstration assessment. [66] 3. Validate the sample preparation method for "fitness-for-purpose" in the specific matrix to rule out inhibition. [29] |
| High Variation Between Analysts | Lack of intermediate precision; Unclear procedural steps leading to individual interpretation. | 1. Conduct cross-training and role rotations to standardize techniques. [67] 2. Perform a ruggedness/robustness study to establish the method's tolerance to minor variations. [28] [70] 3. Implement detailed, visual work instructions at key benches to reduce ambiguity. [68] |
| False Positive/Negative Results | Lack of specificity in the method; Misidentification of microorganisms; Lack of analyst knowledge. | 1. Challenge the method for specificity using a defined panel of organisms to confirm it detects the target unequivocally. [28] [69] 2. Provide targeted training on microbial morphology and identification techniques. [65] |
| Inconsistent Limit of Detection (LOD) | Inconsistent technique for low-level challenges; Poor reagent quality; Uncalibrated equipment. | 1. Automate serial dilution steps where possible to improve precision. [64] [68] 2. Establish and adhere to a strict reagent qualification and equipment calibration schedule. [70] 3. Use a standardized, low-level challenge (<100 CFU) across all validation experiments. [28] |
The Scientist's Toolkit: Key Reagent and Material Solutions
| Item | Function in Mitigating Error |
|---|---|
| Standardized Reference Strains | Provides a known, stable baseline for challenging method accuracy, precision, and specificity, reducing variability introduced by using wild-type or poorly characterized strains. [28] |
| Qualified Culture Media | Pre-prepared, quality-controlled media ensures consistent microbial growth and recovery. Performance is validated for intended use, preventing errors from poorly performing or inhibitory media. [29] [28] |
| Certified Reference Materials | Materials with a certified number of microorganisms (e.g., via flow cytometry) are used for accurate calibration of methods and training analysts on correct enumeration techniques. [28] |
| AOAC-Validated Matrix Panels | Pre-defined categories of sample types (e.g., dairy, meat) help scientists systematically determine a method's "fitness-for-purpose," preventing errors from applying a test to an unvalidated matrix. [29] |
| Automated Dilution Systems | Reduces human error in one of the most variable and critical steps of microbiological testing, directly improving the accuracy and precision of results. [64] [68] |
Demonstrating Equivalency and Ensuring Ongoing Method Reliability
Establishing Method Equivalency with Compendial Reference Methods
This technical support center provides troubleshooting guides and FAQs to help researchers address specific challenges when establishing equivalency between new microbiological methods and compendial reference procedures.
Troubleshooting Low Accuracy in Method Equivalency Studies
Low accuracy in comparative studies often stems from specific, addressable issues in experimental design and execution. The table below outlines common problems, their underlying causes, and recommended corrective actions.
| Problem Symptom | Potential Root Cause | Corrective Action |
|---|---|---|
| Consistently lower recovery in new method vs. reference | Matrix inhibition or interference | Conduct matrix interference studies; modify sample preparation to neutralize inhibitors [2]. |
| Poor recovery of specific microbial strains | Lack of method specificity for all relevant taxa | Re-assess method specificity against a wider panel of target organisms; may require protocol modification [2]. |
| High variability in accuracy between experiment runs | Inconsistent sample preparation or operator technique | Standardize sample prep SOPs, implement rigorous training, and conduct competency assessments [2]. |
| Inability to detect contaminants at low levels | Limit of Detection (LOD) of new method is higher than claimed | Re-validate LOD using appropriate statistical methods and a sufficient number of low-level samples [71] [2]. |
| Results not comparable despite high precision | Fundamental lack of equivalency; method may measure different attribute | Re-evaluate the fundamental principles of the new method versus the reference method [2]. |
Frequently Asked Questions (FAQs)
Q1: What is the primary regulatory foundation for demonstrating method equivalency? The core guidance is found in USP <1223> and Ph. Eur. 5.1.6. These guidelines mandate a structured comparison through parallel testing, where the new method must demonstrate comparable performance to the compendial method in parameters like accuracy, precision, and specificity. Establishing equivalency is crucial for using the new method for product release decisions [2].
Q2: How many samples are typically needed for a robust equivalency study? There is no single fixed number; it depends on the method's intended use and variability. Regulatory standards emphasize that the sample size must be sufficient to provide a reliable statistical evaluation. You must justify your sample size in the validation protocol based on a risk assessment and statistical considerations to ensure the study has adequate power to detect significant differences [72].
Q3: Our new method's results are precise but inaccurate. What should we investigate first? This discrepancy strongly points to matrix interference or a calibration error. First, perform a spike-recovery experiment with known concentrations of analyte in the specific product matrix. If recovery is poor, investigate and modify the sample preparation procedure to eliminate interfering substances. Simultaneously, verify the calibration standards and curve of the new method against a certified reference material [2].
Q4: What is the critical difference between "verification" and "validation" in this context? Verification is the process of confirming that a compendial method works as intended in your specific laboratory, with your analysts and equipment. Validation is a more extensive process required for non-compendial methods (or those used outside their original scope) to generate comprehensive evidence that the method is fit for its intended purpose. Equivalency studies are a core part of validating an alternative method [72] [2].
Q5: How do we set Alert and Action Limits for a new Rapid Microbiological Method (RMM)? Alert and Action Limits for an RMM must be supported by the data generated during the validation study. These limits should be based on the demonstrated capability of the method and the historical data (if any) from the compendial method. They are not arbitrary but must be scientifically justified and documented to provide clear decision-making criteria for investigators [2].
Experimental Protocol: Establishing Equivalency for a Chromogenic Agar
The following workflow details a typical experiment to validate a new chromogenic agar against standard reference media, based on a published study [73].
Define Purpose and Scope
- Objective: To validate that CHROMagar Orientation medium is equivalent to standard blood and MacConkey agars for detecting and differentiating urinary pathogens, and that it supports accurate antibiotic susceptibility testing.
- Scope: Use for routine urine culture processing in a clinical diagnostics laboratory.
Materials and Reagents
- Test Medium: CHROMagar Orientation powder, prepared according to manufacturer's instructions [73].
- Reference Media: Tryptic Soy Agar (TSA) with 5% sheep blood and MacConkey agar [73].
- Quality Control Strains: Use American Type Culture Collection (ATCC) strains for relevant organisms (e.g., E. coli ATCC 25922, P. aeruginosa ATCC 27853) [73].
- Sample Type: Patient urine samples.
Experimental Procedure
- Inoculation: Inoculate each urine sample simultaneously onto the test medium (CHROMagar Orientation) and the two reference media using a calibrated loop.
- Incubation: Incubate all plates aerobically at 35 ± 2°C for 18-24 hours.
- Parallel Testing: Read all plates after incubation. Record colony counts, morphology, and color characteristics for each medium.
- Identification: Perform standardized biochemical tests for final identification of isolates from all media.
- Antibiotic Susceptibility Testing (AST): For a subset of isolates, perform AST by picking colonies directly from the chromogenic agar and from the reference media. Compare the results (e.g., zone diameters from disk diffusion) [73].
Data Analysis and Acceptance Criteria
- Quantitative Comparison: Compare colony counts for each organism between the chromogenic agar and reference media. Statistically analyze the data (e.g., using a paired t-test), with a target of no significant difference (p > 0.05) [73].
- Qualitative Comparison: Compare the accuracy of presumptive identification based on colony color. The new medium should correctly identify a high percentage (e.g., >95%) of isolates compared to definitive identification methods.
- AST Correlation: The results of AST from colonies picked from the chromogenic agar should show excellent correlation (e.g., 99-100%) with results from colonies picked from reference media [73].
The Scientist's Toolkit: Key Reagent Solutions
| Item | Function in Experiment |
|---|---|
| Chromogenic Agar (e.g., CHROMagar Orientation) | Primary test medium that uses chromogenic substrates to produce distinct colony colors for different microorganisms, allowing for presumptive identification [73]. |
| Reference Media (e.g., Blood Agar, MacConkey Agar) | The compendial or standard media used as a benchmark against which the performance of the new chromogenic medium is compared [73]. |
| ATCC Control Strains | Certified microbial strains used for quality control of media batches, ensuring consistent performance and culture response [73]. |
| Mueller-Hinton Agar | Standardized medium required for performing antibiotic susceptibility testing (e.g., disk diffusion) to verify that growth on the new medium does not affect AST results [73]. |
| Biochemical Test Kits | Used for definitive identification of microbial isolates to resolve any discrepancies or to confirm presumptive identifications made on the chromogenic agar [73]. |
Workflow for Establishing Method Equivalency
This diagram illustrates the critical steps and decision points in a method equivalency study.
Conducting Parallel Testing and Statistical Analysis for Comparability
FAQs and Troubleshooting Guides
What is the fundamental difference between method verification and validation?
Answer: In the context of clinical or pharmaceutical microbiology, verification and validation are distinct processes dictated by regulatory requirements and the nature of the test.
- Verification is a one-time study performed by the laboratory for unmodified FDA-cleared or approved tests. It demonstrates that the test performs according to the manufacturer's established performance characteristics in your specific laboratory environment [32]. It is a confirmation that the test works as claimed when used as intended.
- Validation is a more extensive process to establish that a test works as intended. This is required for non-FDA cleared tests (e.g., laboratory-developed methods) or when an FDA-approved test has been modified in a way not specified as acceptable by the manufacturer [32]. According to international standards, validation provides objective evidence that a given item fulfills its intended use [74].
The following table summarizes the key differences:
| Aspect | Verification | Validation |
|---|---|---|
| Definition | Provision of objective evidence that a given item fulfills specified requirements [74]. | Verification where the specified requirements are adequate for the intended use [74]. |
| Purpose | Confirm manufacturer's claims in your lab [32]. | Establish performance of a new or modified test [32]. |
| Test Type | Unmodified, commercially approved tests [32]. | Laboratory-developed tests (LDTs) or modified approved tests [32]. |
| Scope | Limited to verifying stated performance characteristics [32]. | Comprehensive establishment of all performance characteristics [32]. |
What are the common statistical pitfalls in method comparison studies?
Answer: Using inappropriate statistical methods is a major source of error that can lead to incorrect conclusions about method comparability and mask underlying accuracy issues [75] [76].
- Misuse of Correlation Analysis: Correlation measures the strength of a linear relationship between two methods but cannot detect constant or proportional biases. Two methods can be perfectly correlated yet produce vastly different numerical results, giving a false sense of agreement [75].
- Misuse of t-test: A paired t-test may detect a statistically significant difference that is not clinically meaningful with a large sample size, or fail to detect a large, clinically meaningful difference with a small sample size [75]. It assesses averages, not agreement between individual paired results.
Troubleshooting Guide: If your parallel testing shows a high correlation but you suspect poor accuracy, shift your analysis from correlation to methods that assess agreement.
- Use Difference Plots (Bland-Altman Plots): Plot the differences between the two methods against the average of the two methods. This helps visualize the magnitude of disagreement and identify any bias [75].
- Use Linear Regression Analysis: Techniques like Deming or Passing-Bablok regression are more appropriate for quantifying constant (y-intercept) and proportional (slope) systematic errors between two methods [75].
How do I select samples and determine the sample size for a parallel test?
Answer: A poorly designed parallel test with inadequate sample size is a common cause of unreliable results and low accuracy.
Best Practices for Sample Selection [75]:
- Cover the Entire Clinically Meaningful Range: Use patient samples that cover low, medium, and high values of the analyte being measured.
- Use Fresh Patient Samples: These are preferable as they reflect real-world matrix effects.
- Test Over Multiple Days and Runs: Perform measurements over at least five days and multiple runs to account for day-to-day variability and mimic real-world conditions.
- Randomize Sample Sequence: Analyze samples in a randomized order to avoid carry-over effects and systematic sequence bias.
Guidance on Sample Size:
- Minimum Sample Size: A minimum of 40 patient samples is often recommended, but 100 samples or more is preferable to identify unexpected errors and provide more robust statistical power [75].
- For Qualitative/Semi-Quantitative Assays: A common guideline is to use a minimum of 20 clinically relevant isolates for verifying accuracy, with a combination of positive and negative samples [32].
Troubleshooting Guide: If you are encountering high uncertainty or your results are not accepted during audits, check your sample size and distribution. A small sample size or a narrow concentration range are likely culprits [76].
How is "equivalence" defined and demonstrated for rapid microbiological methods?
Answer: Demonstrating equivalence for Rapid Microbiological Methods (RMM) is challenging because many are fundamentally different from growth-based traditional methods. Regulatory guidance focuses on "decision equivalence" rather than numerical correlation [77].
- Non-Growth-Based Methods: Technologies like Bio-Fluorescent Particle Counters (BFPC) detect viable particles differently than culture methods. They may detect "viable but non-culturable" (VBNC) microorganisms, making a direct correlation between CFU and AFU impossible [77].
- Decision Equivalence: The goal is to demonstrate that the alternative method allows a microbiologist to make the same quality decision (e.g., pass/fail, in-spec/out-of-spec) as the traditional method, consistently [77]. The results do not need to match numerically.
Troubleshooting Guide for RMM Validation:
- Challenge: Performing a traditional parallel test in a Grade A environment by introducing microorganisms is counter-intuitive and risky.
- Potential Solution: One industry-proposed strategy is to perform parallel testing for validation in a lower-grade environment where low levels of natural contamination can be safely monitored, before moving the RMM to the Grade A environment for routine use [77].
What are the key validation parameters to check when troubleshooting low accuracy?
Answer: Accuracy is the closeness of agreement between a measured value and the true value. When troubleshooting low accuracy, you must investigate several interconnected validation parameters [28] [74].
The table below outlines key parameters and how they relate to accuracy issues:
| Parameter | Description | Role in Troubleshooting Accuracy |
|---|---|---|
| Specificity | Ability to resolve the target microorganism in the presence of other compounds or organisms [28]. | Interference from sample matrix (excipients, APIs) can cause false positives/negatives, reducing accuracy. |
| Trueness (Bias) | The closeness of agreement between the average value obtained from a large series of test results and the true or accepted reference value [74]. | Measured as systematic error (bias). A significant bias directly indicates an accuracy problem. |
| Precision | The closeness of agreement between a series of measurements obtained from multiple sampling of the same homogeneous sample under prescribed conditions [28] [74]. | Poor precision (high imprecision) increases random error and makes it difficult to determine the true bias, undermining accuracy. |
| Linearity & Range | The ability of the method to obtain test results directly proportional to the analyte concentration within a given range [28]. | Non-linearity in your range can cause inaccuracies that are concentration-dependent. |
| Limit of Detection (LOD) | The lowest number of microorganisms that can be detected under stated experimental conditions [28]. | An LOD that is higher than claimed can lead to false negatives for low-level contamination, affecting accuracy. |
| Robustness & Ruggedness | Reliability of the method to withstand small, deliberate variations in method parameters (robustness) and reproducibility under different conditions (ruggedness) [28]. | The method may show good accuracy under ideal conditions but be highly susceptible to minor changes (e.g., reagent lot, analyst), leading to inconsistent accuracy. |
Experimental Protocols for Key Experiments
Protocol 1: Parallel Testing for Method Comparability
Objective: To estimate the bias between a new method and a comparative method and assess whether they can be used interchangeably [75].
Materials:
- Test and reference method instruments/reagents
- At least 40-100 unique, fresh patient samples covering the entire reportable range [75]
- Data collection sheet or LIMS system
Methodology:
- Sample Selection: Select samples to cover the entire clinically meaningful measurement range [75].
- Measurement: Analyze each sample using both the new method and the comparative method. The sequence of analysis should be randomized to avoid carry-over effect and bias [75].
- Replication: If possible, perform duplicate measurements for both methods to minimize the effect of random variation [75].
- Duration: Conduct measurements over several days (at least 5) and multiple runs to ensure results are reproducible under real-world conditions [75].
Analysis:
- Graphical Analysis: Create a scatter plot and a difference plot (Bland-Altman plot) to visualize the relationship and agreement between the two methods [75].
- Statistical Analysis: Perform appropriate regression analysis (e.g., Deming, Passing-Bablok) to quantify constant and proportional systematic error. Do not rely on correlation coefficients alone [75].
Protocol 2: Verification of Accuracy for a Qualitative Microbiological Assay
Objective: To verify the accuracy of an unmodified, FDA-cleared qualitative test in your laboratory [32].
Materials:
- New test system and reagents
- A comparative validated method
- At least 20 clinically relevant isolates or samples (a combination of positive and negative samples) [32]
- Samples can be from standards, controls, proficiency test samples, or de-identified clinical samples previously tested with a validated method [32]
Methodology:
- Sample Preparation: Obtain or prepare a panel of samples with known status (positive/negative) for the analyte.
- Testing: Test all samples using the new method according to the manufacturer's instructions.
- Comparison: Compare the results from the new method to those obtained from the comparative method.
Analysis & Acceptance Criteria:
- Calculate the percentage agreement:
(Number of results in agreement / Total number of results) * 100[32]. - The percentage of accuracy should meet the stated claims of the manufacturer or what the CLIA director/Laboratory Director determines is acceptable [32].
Signaling Pathways and Workflows
The Scientist's Toolkit: Research Reagent Solutions
| Category | Item | Function / Application |
|---|---|---|
| Reference Materials | Certified Reference Materials (CRMs), Proficiency Test (PT) Samples [32] | Provides a sample with an assigned "true" value to assess method trueness and estimate bias [74]. |
| Quality Controls | Commercial Quality Control (QC) Materials [32] | Used for daily monitoring of precision and to ensure the test system remains in control during verification studies. |
| Microbial Strains | Clinically Relevant Isolates, ATCC Strains [32] [28] | Used to challenge the method for parameters like specificity, accuracy, and limit of detection. |
| Statistical Tools | CLSI Documents (e.g., EP12-A2, EP09-A3, M52) [32] [75] | Provide standardized protocols and statistical guidance for designing and analyzing method comparison studies. |
| Data Integrity Tools | Laboratory Information Management System (LIMS) [76] | Ensures data is recorded, stored, and maintained in compliance with ALCOA+ principles for audit readiness [78]. |
Performing Robustness and Ruggedness Testing
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between robustness and ruggedness testing?
A1: Robustness testing is an intra-laboratory study that examines how an analytical method's performance is affected by small, deliberate variations in its method parameters. In contrast, ruggedness testing is an inter-laboratory study that measures the reproducibility of results under real-world conditions, such as when different analysts, instruments, or laboratories use the method [79].
- Robustness focuses on internal method parameters (e.g., mobile phase pH, incubation temperature).
- Ruggedness focuses on external, environmental factors (e.g., different analysts, different equipment models) [79].
Q2: Why are these tests critical for microbiological methods in pharmaceutical or clinical settings?
A2: Errors in microbiological testing can have monumental consequences, impacting patient safety, product quality, and business sustainability [34] [79]. Robustness and ruggedness testing act as analytical safeguards by:
- Preventing inaccurate results that could lead to poor decisions.
- Ensuring regulatory compliance with standards from bodies like the FDA, ISO, and ICH [79].
- Saving costs by avoiding expensive investigations, product recalls, and repeated testing that arise from method failures [34] [79].
Q3: A new rapid method for sterility testing is being introduced in our lab. Its robustness is uncertain. What is the first step in troubleshooting?
A3: The first step is to conduct a systematic robustness study to identify the method's critical parameters. This involves deliberately varying key factors within a scientifically justifiable range and monitoring their impact on the results [79]. For a sterility test, this could include small changes in:
- Incubation temperature
- Culture media composition or pH
- Sample incubation time The outcome will show which parameters require tight control and will help you establish defined operating ranges for your standard operating procedure (SOP).
Q4: Our method performs well in one lab but fails in another. Does this indicate a robustness or ruggedness issue?
A4: This is a classic sign of a ruggedness issue. The method is not reproducible across different environments, which may be due to variations in analyst technique, calibration of equipment, or reagent suppliers between the two labs [79]. To address this, a formal ruggedness study should be performed, and the method may need to be refined to make it more tolerant of such inter-laboratory variations.
Q5: What are common pitfalls in sample handling that can compromise robustness?
A5: Proper sample collection and handling are foundational to reliable results. Common pitfalls include [34] [5]:
- Using incorrect containers for samples.
- Transport delays, allowing unwanted organisms to grow and leading to misleading results.
- Improper storage conditions for samples and reagents, which can degrade their integrity. These pre-analytical variables must be strictly controlled in your SOPs to ensure the method's robustness is not undermined before testing even begins.
Troubleshooting Guides
Guide 1: Troubleshooting Low Accuracy Due to Non-Robust Methods
Low accuracy often surfaces when a method is highly sensitive to minor, uncontrolled variations.
| Observation | Potential Cause | Investigation & Solution |
|---|---|---|
| Inconsistent microbial recovery (e.g., colony counts) across runs. | Uncontrolled variation in a critical method parameter (e.g., temperature, culture media pH). | Action: Perform a robustness test using a factorial design to simultaneously evaluate multiple parameters. Identify the sensitive parameter and tighten its control limits in the SOP [79]. |
| High rate of false-positive or false-negative results in sterility tests. | The method is not robust against slight deviations in incubation time or reagent concentration [7]. | Action: Validate the method using well-characterized Quality Control (QC) organisms [34]. Use certified reference materials to ensure the method's detection limit and specificity are maintained under slight parameter changes [34] [5]. |
| Method works for one product matrix but fails for another with slight formulation changes. | The method's performance is not robust across different sample matrices. | Action: Extend robustness testing to include variations in sample matrix composition. This may involve validating the method for each specific product type [80]. |
Guide 2: Troubleshooting Poor Ruggedness During Method Transfer
This guide helps when a method is being transferred to a new site or team and performance degrades.
| Observation | Potential Cause | Investigation & Solution |
|---|---|---|
| Significant difference in results between Analyst A and Analyst B. | Method is too dependent on analyst technique (e.g., sample injection volume, pipetting style). | Action: Conduct a ruggedness study focusing on the "different analysts" factor [79]. Enhance the SOP with more detailed, step-by-step instructions and provide comprehensive, hands-on training to standardize technique. |
| Results differ when using the same model of instrument from different manufacturers. | Unspecified method parameters that vary between instrument brands (e.g., wavelength accuracy, detector characteristics). | Action: Specify the exact instrument model in the method. If multiple instruments must be used, perform a formal ruggedness study to validate the method on all accepted models and document any necessary adjustments [79]. |
| A method validated in an R&D lab fails in a quality control lab. | Differences in environmental conditions (e.g., water purity, room temperature fluctuations) or reagent suppliers. | Action: Before transfer, perform an inter-laboratory ruggedness study. Identify the critical differences and update the method to be more tolerant, or mandate that the receiving lab meets all specified environmental and material conditions [79]. |
Experimental Protocols
Protocol 1: Performing a Robustness Test for a Microbiological Method
This protocol provides a detailed methodology for assessing the robustness of a method, such as a culture-based enumeration test.
1. Define Scope and Parameters: Identify the method parameters to be investigated. For a culture-based method, this might include [79]:
- Incubation temperature
- pH of the culture media
- Concentration of a critical reagent in the media
- Incubation time
2. Establish the Experimental Design: A full or fractional factorial design is highly efficient for simultaneously testing multiple parameters [79].
- For each parameter, select a nominal value (the standard condition) and a high and low value (a small, deliberate variation).
- For example, if the nominal incubation temperature is 37°C, you might test 36°C and 38°C.
3. Execute the Experiment:
- Use a standardized and well-characterized QC organism (e.g., E. coli ATCC 8739) as the test sample [34].
- Run the method with all possible combinations of the high and low parameter values as per your experimental design.
- For each run, measure the predefined critical outcomes, such as Colony Forming Units (CFU)/mL, turbidity, or detection of a specific biochemical reaction.
4. Analyze Data and Draw Conclusions:
- Statistically analyze the results (e.g., using analysis of variance) to determine which parameters have a significant effect on the outcome.
- A parameter is considered non-robust if a small variation leads to a statistically significant change in the result.
- For robust parameters, you can define an acceptable operating range. For non-robust parameters, you must specify tight control limits in the final method.
The workflow for this robustness testing protocol is outlined in the following diagram:
Protocol 2: Designing a Ruggedness Study for Method Transfer
This protocol outlines the steps to validate a method's reproducibility across different conditions.
1. Identify Ruggedness Factors: Determine the real-world variables to test. The most common are [79]:
- Different analysts
- Different instruments
- Different days
- Different laboratories
2. Develop the Study Plan:
- Prepare a set of identical, homogeneous samples spiked with a known concentration of a QC organism [34] [5].
- Distribute the samples to the different analysts, instruments, or labs involved in the study.
- Ensure all participants follow the identical, written method procedure.
3. Execute the Study and Collect Data:
- Each analyst/lab runs the method on the provided samples and reports the results (e.g., CFU count, presence/absence of a pathogen).
- It is critical that the testing is performed independently to simulate true real-world conditions.
4. Analyze Results for Reproducibility:
- Calculate the reproducibility standard deviation and other statistical measures (e.g., % coefficient of variation) across the different conditions.
- Compare the results against pre-defined acceptance criteria. A common criterion is that results from all analysts and instruments should fall within a specified range of the known value or the nominal result.
- If the results meet the acceptance criteria, the method is considered rugged for the tested factors.
Research Reagent Solutions
The following table details key materials essential for successful robustness and ruggedness testing in microbiology.
| Item | Function in Testing | Example & Notes |
|---|---|---|
| QC Organisms & Reference Materials | Serve as verified standards with predictable reactions to validate testing methodologies and monitor test performance [34]. | * Well-characterized strains from culture collections (e.g., ATCC).* Certified Reference Materials (CRMs) quantitatively certified for CFU [34]. |
| Culture Media | Provides the nutritional environment for microbial growth; variations between batches can affect results. | * Use media from multiple lots or suppliers during ruggedness testing.* Perform growth promotion tests on new media lots [34]. |
| Standardized Reagents | Critical for molecular and rapid methods (e.g., PCR master mixes, enzymes). | * Test different batches of reagents during robustness studies.* Use reagents from different vendors if the method allows, to assess ruggedness. |
Integrating Verified Methods into the Quality Management System (QMS)
Troubleshooting Guide: Low Accuracy in Method Verification
Low accuracy during microbiological method verification indicates a systematic discrepancy between your test results and the true value. This guide helps diagnose and resolve the underlying causes [2] [81].
Investigation and Resolution
| Investigation Area | Specific Checks & Common Causes | Corrective & Preventive Actions (CAPA) |
|---|---|---|
| Reference Standards & Materials | ✓ Viability of QC Strains: Check purity, concentration, and physiological state (e.g., sub-lethally damaged).✓ Certification: Use certified reference materials (CRMs) with traceable purity and concentration [34] [81].✓ Storage & Handling: Confirm correct storage temperature and ensure proper resuscitation of cultures. | ✓ Require CRM suppliers' certificates of analysis.✓ Implement viability checks upon receipt and use.✓ Establish robust cell culture and preparation SOPs. |
| Sample Matrix Effects | ✓ Inhibition/Interference: Product components (preservatives, antibiotics) may inhibit microbial growth or cause false positives [2].✓ Physical Properties: Viscosity or particulates can impede sample processing or microbial recovery.✓ Neutralization: Verify the effectiveness of neutralizers in the dilution medium. | ✓ Conduct matrix interference studies by spiking known microbes into the product [2].✓ Dilute the sample to reduce inhibition.✓ Modify the method to include a validated neutralization step. |
| Methodology & Protocol | ✓ Calibration: Equipment (pipettes, incubators) may be out of calibration.✓ Incubation Conditions: Verify temperature, atmosphere, and time match the target organisms' requirements.✓ Selective Agents: Confirm concentration of selective agents is not overly restrictive. | ✓ Re-calibrate all critical equipment.✓ Validate growth promotion properties of media for target organisms.✓ Optimize incubation parameters and agent concentrations. |
| Data Analysis | ✓ Calculation Errors: Review formulas for calculating recovery rates and accuracy.✓ Acceptance Criteria: Ensure pre-defined acceptance criteria (e.g., 70-150% recovery) are appropriate for the sample type [81]. | ✓ Automate calculations where possible to minimize manual errors.✓ Justify acceptance criteria based on regulatory guidance and product-specific validation data. |
Experimental Protocol: Determining Method Accuracy
This protocol provides a detailed methodology for assessing the accuracy of a quantitative microbiological method, a key step in troubleshooting low recovery rates [2] [81].
- 1. Objective: To determine the accuracy of the alternative method by measuring its ability to recover known concentrations of microorganisms from the product matrix.
- 2. Principle: The sample is artificially contaminated (spiked) with a known number of viable microorganisms. The recovery rate is calculated by comparing the count obtained by the alternative method against the count obtained by a reference method (e.g., plate count) and the theoretical spike level.
- 3. Materials & Reagents:
- Test samples (sterile product, if possible)
- Fresh, log-phase cultures of specified reference strains (e.g., Staphylococcus aureus ATCC 6538, Pseudomonas aeruginosa ATCC 9027, Candida albicans ATCC 10231, Aspergillus brasiliensis ATCC 16404)
- Appropriate culture media and diluents
- Equipment: calibrated pipettes, incubator, etc.
- 4. Procedure:
- Preparation of Inoculum: Prepare a suspension of each test microorganism and standardize to a known concentration (e.g., 10^8 CFU/mL).
- Sample Spiking: For each microorganism, spike a known volume of the inoculum into the test product to achieve a target final concentration appropriate for the method's range (e.g., 10^2 to 10^4 CFU/unit). Prepare multiple replicates (minimum n=3).
- Neutralization (if applicable): Immediately mix the spiked sample with a validated neutralizer or a large volume of appropriate diluent to stop antimicrobial activity.
- Testing:
- Test Method: Analyze the spiked samples using the alternative (rapid) method.
- Reference Method: In parallel, analyze identical spiked samples using the compendial (e.g., plate count) method.
- Controls: Include unspiked product (negative control) and a diluent spiked at the same level (positive control to confirm inoculum viability).
- Incubation & Enumeration: Perform all steps according to the validated protocols for each method.
- 5. Data Analysis:
- For each microorganism and replicate, calculate the percent recovery:
- Recovery (%) = (Count from Test Method / Count from Reference Method) × 100
- Calculate the mean recovery and standard deviation for each microorganism across all replicates.
- Compare the mean recovery against pre-defined acceptance criteria.
- For each microorganism and replicate, calculate the percent recovery:
- 6. Acceptance Criteria: Acceptance criteria should be justified and predefined. A common benchmark is a mean recovery of 70-150% for the tested microorganisms [81].
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between method validation and verification in a QMS context? [82]
A1: Validation is a comprehensive process to prove that a new or modified method is fit for its intended purpose. It is performed on a novel method and involves gathering extensive evidence on parameters like accuracy, precision, and robustness to ensure it is suitable for use [81] [82]. Verification is a more limited process to confirm that a compendial or previously validated method works as expected in your specific laboratory, with your specific analysts and equipment. It demonstrates that your lab can competently perform the established method [81] [72].
Q2: Our new rapid method passed validation, but we are getting inconsistent results during routine use. What should we check first in our QMS? [2]
A2: First, investigate within your QMS's deviation and change control systems.
- Personnel Training: Review training records to ensure all operators are consistently trained and competent on the method [2].
- Reagent & Media Control: Check certificates of analysis for new lots of critical reagents, culture media, or substrates. Perform growth promotion tests on new media lots [34].
- Equipment Calibration: Confirm that all equipment used in the method (pipettes, incubators, readers) is within its calibration due date and operating correctly.
- Environmental Conditions: Review environmental monitoring data for any excursions that could have affected the test.
Q3: How can we leverage our QMS to ensure smooth technology transfer of a verified method from R&D to the QC lab? [2]
A3: A robust QMS is critical for successful technology transfer. Key steps include:
- Formal Transfer Protocol: Establish and approve a detailed transfer protocol within the document control system, defining roles, responsibilities, acceptance criteria, and the testing plan.
- Change Control: Initiate a formal change control to manage the introduction of the new method into the QC lab's operations.
- Structured Data Collection: The receiving lab performs an approved test plan, often a side-by-side comparison with the current method or a pre-qualified sample set.
- Documented Report: A final report, summarizing the data against acceptance criteria, should be approved to formally close the transfer and release the method for routine use.
Q4: What are the common pitfalls when integrating a new Rapid Microbiological Method (RMM) into the QMS, and how can we avoid them? [2]
A4: Common pitfalls and their mitigations are:
- Pitfall: Inadequate Validation Scope. Failure to fully challenge the method with relevant product matrices and environmental isolates.
- Mitigation: Base the validation protocol on regulatory guidelines (USP <1223>, Ph. Eur. 5.1.6) and include a risk assessment to ensure all potential interferences are tested [2].
- Pitfall: Poorly Defined SOPs. Vague instructions lead to operator-to-operator variability.
- Mitigation: Write detailed, clear SOPs that cover instrument operation, sample handling, data interpretation, and actionable limits.
- Pitfall: Siloed Implementation. The RMM is treated as a standalone tool rather than an integrated component.
- Mitigation: Ensure the RMM is linked to all relevant QMS processes: deviations, CAPA, change control, and training management [2].
Workflow: Integrating a New Method into the QMS
The following diagram illustrates the logical workflow and critical decision points for integrating a new microbiological method into the QMS, ensuring compliance and robustness.
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and their functions for conducting successful microbiological method verification and validation studies.
| Item | Function & Role in Verification/Validation |
|---|---|
| Certified Reference Materials (CRMs) | Provides a traceable, quantitative standard for calibrating instruments and determining method accuracy and limit of quantification (LOQ) [81]. |
| Quality Control (QC) Strains | Well-characterized microorganisms used to confirm the performance of culture media, reagents, and the test method itself on a routine basis [34]. |
| In-House & Objectionable Isolates | Environmental or product-specific isolates are critical for challenging a method's specificity and robustness, ensuring it detects relevant contaminants [34]. |
| Neutralizing / Dilution Media | Inactivates residual antimicrobial activity from the product matrix, preventing false negatives and enabling accurate microbial recovery during testing [2]. |
| Validated Culture Media | Media that has undergone growth promotion testing to support the growth of a defined panel of microorganisms, which is fundamental for comparability studies against reference methods [2]. |
Planning for Ongoing Verification, Monitoring, and Revalidation
Troubleshooting Guides and FAQs for Microbiological Method Verification
FAQ: Addressing Common Challenges in Microbiological Methods
Q1: Our microbial recovery rates during method verification are consistently low and variable. What are the primary causes?
Low and variable recovery rates often stem from inadequate neutralization of antimicrobial activity in your product or issues with sample preparation techniques. According to the Chinese Pharmacopoeia (2025), the acceptability criterion for recovery is a ratio of 0.5 to 2 when comparing test group counts to control group counts [83]. Key troubleshooting steps include:
- Verify Neutralization Efficacy: Ensure your chosen neutralizers (e.g., lecithin, polysorbate) are effective and non-toxic to microorganisms. Re-perform neutralization efficacy studies as part of your investigation.
- Review Sample Preparation Parameters: For油脂类 (oil-based) or 肠溶及结肠溶制剂 (enteric-coated) products, the 2025 Pharmacopoeia specifies updated parameters, such as a dissolution temperature up to 45°C or even at room temperature, which differs from previous editions. Using outdated procedures will lead to poor recovery [83].
- Confirm Method Suitability: The entire counting method (plate, membrane filtration, or MPN) must be validated for each product type through formal method suitability testing before it is used for routine testing [83].
Q2: We encountered an Out-of-Specification (OOS) result during environmental monitoring. How should we proceed?
An OOS result requires a thorough, documented investigation per cGMP principles. A key regulatory citation from a recent FDA Warning Letter highlights that "Multiple out-of-specification (OOS) results were disregarded without adequate investigation" is a critical failure [84]. Your procedure must include:
- Phase I Investigation: An initial laboratory investigation to assess accuracy. This includes checking for obvious analytical errors, reviewing raw data, and confirming instrument calibration. The investigation must be timely and thorough [84].
- Phase II Investigation: If no clear laboratory error is found, the investigation must escalate. It should include a full OOS investigation and a assessment of potential manufacturing causes [85]. The FDA mandates that investigations closed at Phase I without escalation, despite documented trends, are unacceptable [84].
- Robust CAPA: Implement a comprehensive Corrective and Preventive Action (CAPA) plan based on the investigation's root cause. This plan should be supported by an independent consultant if the issues are systemic [84] [85].
Q3: Our rapid microbiological method (RMM) needs revalidation. What triggers this process?
Revalidation is crucial to ensure your method remains fit-for-purpose. Triggers are outlined in regulatory guidance, including the Chinese Pharmacopoeia 2025 guidance on alternative methods [86]. Revalidation is required when:
- Changes in the Product or Formulation: Any significant change that might affect antimicrobial properties.
- Changes in the Test Method or Equipment: This includes software updates for computerized systems or changes to RMM equipment.
- Routine Monitoring Indicates a Problem: Trends in data, such as drifting control results, can signal the need for re-evaluation.
- Regulatory Requirement: After a predefined period, or when new regulatory guidelines, like the updated EP 5.1.6 or USP <1223>, are adopted [87] [86].
Q4: What are the most critical aspects of equipment qualification for ensuring data integrity in microbiological testing?
Equipment qualification is foundational. The core concept is IOPQ (Installation, Operational, and Performance Qualification). A recent analysis clarified that "equipment calibration is a measurement of accuracy compared with a known standard... In contrast, validation is a series of specification tests to ensure that the equipment functions as intended" [48]. Critical aspects include:
- Performance Qualification (PQ) Under Real Conditions: PQ must demonstrate the equipment performs consistently with your specific samples and methods to meet pre-defined acceptance criteria in a simulated routine environment [48].
- Controlled Software Access: The FDA has cited firms where "Analytical software access was uncontrolled: shared logins, only 'System Administrator' as a user role, and no audit trail review" [84]. Ensure role-based access and routine audit trail reviews are part of your qualification and monitoring.
- Ongoing Monitoring and Re-qualification: Equipment must be maintained under a state of control through regular calibration, preventive maintenance, and periodic reviews, which may include re-qualification.
Key Experimental Protocols for Verification and Troubleshooting
Protocol 1: Conducting a Method Suitability Test (Microbial Count) per Pharmacopoeia
This protocol is essential for verifying that your product's antimicrobial activity has been adequately neutralized.
1. Objective: To demonstrate that the test method accurately enumerates microbial contaminants in the presence of the product.
2. Materials and Reagents:
- Test product
- Appropriate culture media (e.g., TSA, SDA)
- Standardized cultures of challenge organisms (e.g., Staphylococcus aureus, Pseudomonas aeruginosa, Candida albicans, Aspergillus brasiliensis)
- Diluents and neutralizers
3. Methodology:
- Preparation: Prepare the product as per the routine test method.
- Inoculation: Inoculate the product with a known, low concentration (not more than 100 CFU) of each challenge organism.
- Testing and Controls:
- Test Group: Process the inoculated product through the planned enumeration method (e.g., plate count, membrane filtration).
- Product Control: Process the uninoculated product to confirm it is sterile.
- Method Control: Perform the enumeration method on the challenge inoculum without product to determine the baseline count.
- Calculation and Acceptance Criteria: Calculate the recovery for each organism as (Test Group Count - Product Control Count) / Method Control Count. The result must be between 0.5 and 2.0 to prove the method is suitable [83].
Protocol 2: Investigating an Invalidated OOS Result
This protocol outlines a compliant investigation workflow, addressing common FDA citations.
Research Reagent Solutions for Microbiological Testing
The following table details key reagents and materials critical for successful and compliant microbiological method verification.
| Reagent/Material | Function & Importance in Verification |
|---|---|
| Validated Growth Media | Used for microbial enumeration and viability testing. Must pass growth promotion testing with a defined set of compendial strains before use. Failure to do so can invalidate all subsequent test results, as cited in regulatory actions [85]. |
| Specific Neutralizing Agents | Critical for inactivating antimicrobial properties of the test product. Examples include lecithin for quats, polysorbate for phenolics. Effectiveness and non-toxicity must be proven for each product type [83]. |
| Standardized Reference Strains | Used for method suitability testing, growth promotion, and as positive controls. Sourced from a recognized culture collection. Handling, storage, and use within defined passage levels (e.g., not more than 5 subcultures) is mandatory to ensure consistent response [83]. |
| qPCR Master Mixes & Probes | For rapid microbiological methods (RMMs). The Chinese Pharmacopoeia 2025 provides a framework for validating nucleic acid amplification techniques like qPCR. Using kits with TaqMan probes (FAM, ROX, HEX channels) allows for specific, sensitive, and multiplexed detection of bacteria, fungi, and mycoplasma [86]. |
Structured data is vital for planning. The tables below summarize key quantitative information from recent regulatory updates.
Table 1: Updated Regulatory Timelines for Drug Development (2025)
| Procedure | Updated Timeline / Condition | Key Change / Impact | Source |
|---|---|---|---|
| Innovation Drug Clinical Trial Approval | 30-working-day review channel | For qualified products, accelerates initiation of clinical trials. If extended, follows 60-day default license. | [87] |
| Drug Registration Testing | Routine: Shortened by 10 daysRare Disease: Shortened by 20 days | Reduces waiting times for product approval and launch. | [87] |
| Post-Approval Change (PACMP) | Can be submitted for post-approval药学 changes | Expected to shorten change implementation cycles by ~2 months. | [87] |
Table 2: Key Acceptance Criteria in Microbial Method Verification
| Parameter | Pharmacopoeia Acceptance Criterion | Notes & Application |
|---|---|---|
| Microbial Recovery Ratio | 0.5 - 2.0 | Ratio of (Test Group - Product Control) / Method Control. Fundamental for method suitability [83]. |
| Media Growth Promotion | Growth comparable to control media (0.5 - 2.0 ratio) | Must be performed on every batch of media to ensure its ability to support growth [85]. |
| Method Suitability Testing | Required for each product and method | Not a one-time activity; must be repeated if the product or method changes [83]. |
Conclusion
Successfully troubleshooting low accuracy in microbiological method verification requires a systematic approach grounded in a deep understanding of regulatory standards and microbiological principles. By dissecting the verification process—from foundational knowledge and robust protocol design to targeted troubleshooting and rigorous validation—laboratories can pinpoint and rectify the root causes of inaccuracy. The implementation of a continuous verification strategy, integrated within a quality management system, is paramount for sustaining method performance. As the field advances with Rapid Microbiological Methods (RMMs), AI, and increased automation, a proactive and knowledgeable approach to method verification will remain critical for ensuring data integrity, accelerating drug development, and ultimately safeguarding public health.
References
- 1. Get Ready for the PT CLIA Changes:… [https://www.cap.org/calendar/webinars/get-ready-for-the-pt-clia-changes-stay-ahead-stay-compliant]
- 2. Validate Rapid Microbiological Methods for ... [https://www.pharmanow.live/regulatory-landscape/validate-rapid-microbiological-methods]
- 3. A Guide to Validating RMMs Following USP <1223> [https://www.watertechnologies.com/sievers-resource-center/guide-to-validating-rmms]
- 4. 2025 CLIA Acceptance Limits for Proficiency Testing [https://www.westgard.com/clia-a-quality/quality-requirements/2024-clia-requirements.html]
- 5. The Essential Guide to Microbiology Testing: Methods, ... [https://contractlaboratory.com/microbiology-testing-services/]
- 6. Method Validation vs Method Verification: Which is Better ... [https://www.labmanager.com/method-validation-vs-method-verification-which-is-better-for-use-in-laboratories-33982]
- 7. Challenges of growth-based microbiological methods in ... [https://link.springer.com/article/10.1007/s44395-025-00020-6]
- 8. The Critical Importance of Rethinking Microbial Non-detects [https://pmc.ncbi.nlm.nih.gov/articles/PMC6182096/]
- 9. Guidelines for preventing and reporting contamination in ... [https://www.nature.com/articles/s41564-025-02035-2]
- 10. Method Validation Guidelines [https://www.biopharminternational.com/view/method-validation-guidelines]
- 11. Optimizing methods and dodging pitfalls in microbiome research [https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-017-0267-5]
- 12. Why do I have poor repeatability in my ATP tests and what ... [https://my.luminultra.com/hc/en-us/articles/12296793054605-Why-do-I-have-poor-repeatability-in-my-ATP-tests-and-what-can-I-do]
- 13. A Fresh Look at USP <1223> Validation of Alternative ... [https://www.americanpharmaceuticalreview.com/Featured-Articles/177873-A-Fresh-Look-at-USP-1223-Validation-of-Alternative-Microbiological-Methods-and-How-the-Revised-Chapter-Compares-with-PDA-TR33-and-the-Proposed-Revision-to-Ph-Eur-5-1-6/]
- 14. Method validation and method verification - Introduction - ISO [https://committee.iso.org/sites/tc34sc9/home/essential-information/content-left-area/validation-of-methods/method-validation-and-method-ver.html]
- 15. A comprehensive review of the newly revised European ... [https://www.europeanpharmaceuticalreview.com/article/66402/comprehensive-review-newly-revised-european-pharmacopoeia-chapter-5-1-6/]
- 16. USP Testing | Frequently Asked Questions [https://www.eurofinsus.com/food-testing/resources/usp-microbiology-services-frequently-asked-questions/]
- 17. Sterility Testing, GPT and More - Warning Letter of the US ... [https://www.gmp-compliance.org/gmp-news/sterility-testing-gpt-and-more-warning-letter-of-the-us-fda-with-various-deficiencies]
- 18. Understanding the Variability in Bioburden Test Results ... [https://www.pharmtech.com/view/understanding-the-variability-in-bioburden-test-results-in-biomanufacturing]
- 19. Validation of Microbiological Tests [https://www.biopharminternational.com/view/validation-microbiological-tests]
- 20. Variability in Antimicrobial Testing [https://microchemlab.com/information/variability-antimicrobial-testing/]
- 21. Determining Matrix Effects in Complex Food Samples [https://www.waters.com/blog/understanding-sample-complexity-determining-matrix-effects-in-complex-food-samples/?srsltid=AfmBOop00-xym3znbKGVYAGesY6Bl9wC4JUfg6an74gi16y4nlC7UGdw]
- 22. What is matrix effect and how is it quantified? [https://sciex.com/support/knowledge-base-articles/what-is-matrix-effect-how-to-quantify-it_en_us]
- 23. WHAT CONTRIBUTES TO MICROBIOLOGICAL TEST ... [https://biodeterioration-control.com/what-contributes-to-microbiological-test-result-variability/]
- 24. Improving accuracy and reproducibility in life science ... [https://www.atcc.org/resources/white-papers/improving-accuracy-and-reproducibility-in-life-science-research]
- 25. How to Measure and Improve Lab Accuracy and Precision [https://bitesizebio.com/55470/accuracy-and-precision/]
- 26. 详解版本差距:9101 分析方法验证指导原则 - 中国药典 [https://www.yaodian25.com/blog/fenxifangfayanzheng1]
- 27. Planning a Method Verification Study in Clinical ... [https://asm.org/articles/2022/january/planning-a-method-verification-study-in-clinical-m?sr_id=23df675c-421d-4816-a54e-4d751ba62574&sr_pos=3]
- 28. 10 Critical Validation Parameters For Microbiological ... [https://www.outsourcedpharma.com/doc/critical-validation-parameters-for-microbiological-experiments-0001]
- 29. Food Safety Testing: Understanding Microbiological ... [https://www.eurofinsus.com/food-testing/resources/food-safety-testing-understanding-microbiological-method-validation-verification-and-fitness-for-purpose/]
- 30. New Test? Don't Skip Performance Specification Verification [https://staffready.com/2025/08/19/new-test-dont-skip-performance-specification-verification/]
- 31. Analytical Method Validation: Back to Basics, Part II [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-ii]
- 32. Planning a Method Verification Study in Clinical ... [https://asm.org/articles/2022/january/planning-a-method-verification-study-in-clinical-m]
- 33. Evaluation of analytical performance of qualitative and ... [https://www.sciencedirect.com/science/article/abs/pii/S0009898119319552]
- 34. Mastering Quality: New Method Validation, QC Standards, PT [https://www.rapidmicrobiology.com/news/mastering-quality-new-method-validation-qc-standards-and-pt-a-rapidmicrobiology-special-focus]
- 35. Design and validation of a semi-quantitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11971440/]
- 36. The Inoculum Effect in the Era of Multidrug Resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC6105823/]
- 37. Effect of temperature on inoculum as a potential source ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC172212/]
- 38. Problems when preparing culture media [https://www.scharlab.com/lab/in/en/resources/blog-en/problems-when-preparing-culture-media/]
- 39. Preparing inoculum for susceptibility testing of anaerobes [https://pmc.ncbi.nlm.nih.gov/articles/PMC271057/]
- 40. Inoculum standardization in antimicrobial susceptibility ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC272664/]
- 41. SOP for Preparation of Culture Inoculum [https://www.pharmaguideline.com/2010/03/sop-for-preparation-of-culture-inoculum.html]
- 42. Microbial Analysis mistakes Archives [https://metalchem.com/tag/microbial-analysis-mistakes/]
- 43. <61> Microbial Enumeration Tests [https://www.usp.org/harmonization-standards/pdg/general-methods/microbial-enumeration]
- 44. Microbiology Specimen Collection and Transport [https://www.healthcare.uiowa.edu/path_handbook/appendix/micro/micro_spec_collection.html]
- 45. Laboratory Contamination: Identifying and Mitigating Sources [https://www.kewaunee.in/blog/laboratory-contamination-identifying-and-mitigating-sources/]
- 46. A Guide to USP <1223> and Validation of Rapid Methods [https://www.americanpharmaceuticalreview.com/Featured-Articles/613587-Validating-Alternative-Microbiological-Methods-A-Guide-to-USP-1223-and-Validation-of-Rapid-Methods/]
- 47. An Overview of Rapid Microbial-Detection Methods [https://www.pharmtech.com/view/overview-rapid-microbial-detection-methods]
- 48. All you need to know about equipment validation for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12421869/]
- 49. Methods for screening and evaluation of antimicrobial activity [https://pmc.ncbi.nlm.nih.gov/articles/PMC11097785/]
- 50. Optimizing neutralization strategies for microbial testing of non ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12619157/]
- 51. Optimizing neutralization strategies for microbial testing of ... [https://pubmed.ncbi.nlm.nih.gov/41241716/]
- 52. FAQs: Microbiology [https://www.usp.org/frequently-asked-questions/microbiology]
- 53. Evaluation of new formulations for neutralizing ... [https://www.sciencedirect.com/science/article/pii/S2405844023017620]
- 54. Avoiding environmental monitoring 'false negatives' [https://www.europeanpharmaceuticalreview.com/article/78799/overcoming-disinfectant-residues-with-culture-media-neutralisers/]
- 55. Effect of the Use of a Neutralizing Step after Antimicrobial ... [https://www.sciencedirect.com/science/article/pii/S0362028X23052523]
- 56. Teaching Your Lab Staff to Successfully Troubleshoot [https://www.labmanager.com/teaching-your-lab-staff-to-successfully-troubleshoot-32784]
- 57. Avoiding Common Lab Equipment Failures [https://www.linkedin.com/pulse/avoiding-common-lab-equipment-failures-troubleshooting-n4syc]
- 58. How to Reduce Sample Contamination [https://blog.omni-inc.com/blog/how-to-reduce-sample-contamination]
- 59. Trouble shooting microbiological deviations in ... - RISE [https://www.ri.se/en/expertise-areas/services/trouble-shooting-microbiological-deviations]
- 60. Criteria for Validation of Methods in Microbial Forensics [https://pmc.ncbi.nlm.nih.gov/articles/PMC2547046/]
- 61. Recommended criteria for the evaluation of bacterial ... [https://www.sciencedirect.com/science/article/pii/S1383571819300774]
- 62. Questions and Answers on Current Good Manufacturing ... [https://www.fda.gov/drugs/guidances-drugs/questions-and-answers-current-good-manufacturing-practice-requirements-equipment]
- 63. Error Correction in Gene Synthesis Technology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3933390/]
- 64. Prevention & Correction of Human Error For Risk ... [https://www.piranirisk.com/academy/pirani-explains/prevention-correction-of-human-error-for-risk-management]
- 65. Human Error Analysis & Prevention Training Course [https://mercury-training.com/c/7022.html]
- 66. CCAM® Competency & Confidence Assessment Modelling [https://cnet-training.com/programs/ccam/]
- 67. Continuously Updating Training Programs [https://www.orcalean.com/article/strategies-for-minimizing-human-error:-continuously-updating-training-programs]
- 68. 10 Strategies to Reduce Human Error in the Workplace [https://www.inflowinventory.com/blog/reduce-human-error-in-the-workplace/]
- 69. Method Validation/Verification: How Important is it in Your ... [https://www.americanpharmaceuticalreview.com/Featured-Articles/597641-Method-Validation-Verification-How-Important-is-it-in-Your-QC-Microbiology-Laboratory/]
- 70. Validating Rapid Microbiological Methods [http://rapidmicromethods.com/files/validation.php]
- 71. ICH Guidelines for Analytical Method Validation Explained [https://amsbiopharma.com/ich-guidelines-analytical-method/]
- 72. How to verify and validate a clinical microbiology test ... [https://www.sciencedirect.com/science/article/pii/S1198743X24003094]
- 73. Evaluation of Use of a New Chromogenic Agar in Detection of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC104675/]
- 74. Verification of quantitative analytical methods in medical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8199534/]
- 75. Statistical analysis in method comparison studies part one [https://acutecaretesting.org/en/articles/statistical-analysis-in-method-comparison-studies-part-one]
- 76. The Hidden Risks in Analytical Method Validation - [https://pharmuni.com/2025/05/16/the-hidden-risks-in-analytical-method-validation/]
- 77. Equivalence Testing of BFPCs in Grade A Environments [https://www.pda.org/pda-letter-portal/home/full-article/equivalence-testing-of-bfpcs-in-grade-a-environments]
- 78. Leading Pharmaceutical Validation Trends for 2025 [https://www.ellab.com/blog/transforming-the-industry-landscape-leading-pharmaceutical-validation-trends-for-2025/]
- 79. Robustness and Ruggedness Testing in Analytical Chemistry [https://www.labmanager.com/robustness-and-ruggedness-testing-in-analytical-chemistry-34247]
- 80. Comprehensive Microbial Control Strategy [https://www.bioprocessintl.com/qa-qc/beyond-traditional-microbiology-testing-developing-a-comprehensive-strategy-for-microbial-control-and-detection]
- 81. Microbiology & Chemical Assay Validation [https://www.labmanager.com/microbiology-chemical-assay-validation-34505]
- 82. Process Validation and Verification in QMS [https://www.mapcon.com/blog/2025/05/process-validation-vs-verification-key-differences-and-importance]
- 83. 中国药典2020年版与2025年版通则1105和1106实质性差异 ... [https://reguverse.com/nmpa-update/cp-2020-vs-2025-part4-general-1105-1106/]
- 84. FDA Warning Letter Highlights OOS Handling and Stability ... [https://www.gmp-compliance.org/gmp-news/fda-warning-letter-highlights-oos-handling-and-stability-failures]
- 85. Exela Pharma Sciences, LLC - 709859 - 07/02/2025 [https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/warning-letters/exela-pharma-sciences-llc-709859-07022025]
- 86. qPCR技术:药典2025 版下生物制品2小时无菌放行方案 - 制药 [https://pharm.jgvogel.cn/c1547824.shtml]
- 87. gempex速递| 2025年6-7月国内外GMP法规指南汇总 [https://www.gempexchina.com/gmp-knowledge-info/117]