Mycoplasma Contamination in Cell Culture: A Complete Guide to Detection, Eradication, and Prevention
Mycoplasma contamination is a pervasive and serious problem in cell culture, affecting an estimated 15-35% of cell lines and jeopardizing research integrity, drug discovery, and bioproduction.
Mycoplasma Contamination in Cell Culture: A Complete Guide to Detection, Eradication, and Prevention
Abstract
Mycoplasma contamination is a pervasive and serious problem in cell culture, affecting an estimated 15-35% of cell lines and jeopardizing research integrity, drug discovery, and bioproduction. This comprehensive guide addresses the four core needs of researchers and drug development professionals: understanding the foundational biology and impacts of mycoplasma, applying the latest detection and eradication methodologies, implementing troubleshooting and optimization strategies for sensitive cell lines, and validating decontamination success through comparative analysis of available tools. By synthesizing current best practices, this article provides a actionable framework for safeguarding cell cultures and ensuring reliable, reproducible experimental data.
Understanding the Invisible Enemy: The Biology and Impact of Mycoplasma Contamination
What Are Mycoplasmas? Defining the Unique Biology of a Problematic Contaminant
Mycoplasmas represent a significant and persistent challenge in cell culture laboratories worldwide. As the smallest self-replicating organisms known to science, these unique bacteria contaminate an estimated 15-35% of continuous cell cultures, jeopardizing research integrity and biopharmaceutical production [1] [2]. Their unusual biological characteristics—particularly the absence of a cell wall—make them resistant to common antibiotics and difficult to detect without specialized methods. For researchers and drug development professionals, understanding mycoplasma biology and implementing robust contamination control measures is essential for protecting experimental validity and ensuring product safety.
FAQ: Understanding Mycoplasma Biology
What are mycoplasmas and why are they problematic for cell culture? Mycoplasmas are a genus of bacteria that belong to the class Mollicutes, which literally means "soft skin" [3]. They are distinguished from other bacteria by their complete lack of a cell wall, which renders them naturally resistant to many common antibiotics like penicillin that target cell wall synthesis [3] [4] [2]. They are among the smallest self-replicating organisms, with diameters typically ranging from 0.2 to 0.3 micrometers [3] [2]. This small size allows them to pass through many antibacterial filters and makes them invisible under routine light microscopy, enabling contamination to go unnoticed without specific testing [5].
How does mycoplasma contamination affect my cells and experimental data? Mycoplasma contamination can profoundly alter cell physiology and function, leading to unreliable experimental data. Documented effects include:
- Chromosomal aberrations and disruption of nucleic acid synthesis [1]
- Changes in cell membrane antigenicity [1]
- Inhibition of cell proliferation and metabolism [1]
- Decreased transfection rates and changes in gene expression profiles [1]
- Interference with virus production and cell death in severe cases [1] Because mycoplasmas are parasitic and depend on their host for nutrients, they compete with cells for biosynthetic precursors, drastically altering cellular metabolism [5].
What are the most common sources of mycoplasma contamination in the laboratory? Contamination typically originates from laboratory personnel, contaminated reagents, or cross-contamination from infected cell lines. While over 190 mycoplasma species exist, only about 20 species from human, bovine, and porcine sources contaminate cell cultures [1]. A limited number of species account for the majority of cases, as shown in the table below.
Table 1: Most Prevalent Mycoplasma Species in Cell Culture Contamination
| Species | Origin | Approximate Prevalence |
|---|---|---|
| M. arginini | Bovine | Among the 8 species accounting for ~95% of contamination [1] |
| M. fermentans | Human | Among the 8 species accounting for ~95% of contamination [1] |
| M. hominis | Human | Among the 8 species accounting for ~95% of contamination [1] |
| M. hyorhinis | Porcine | Among the 8 species accounting for ~95% of contamination [1] |
| M. orale | Human | Among the 8 species accounting for ~95% of contamination [1] |
| M. pirum | Human | Among the 8 species accounting for ~95% of contamination [1] |
| M. salivarium | Human | Among the 8 species accounting for ~95% of contamination [1] |
| Acholeplasma laidlawii | Bovine | Among the 8 species accounting for ~95% of contamination [1] |
Troubleshooting Guide: Detection and Elimination
Problem: Suspected Mycoplasma Contamination
Observation: Cells show decreased proliferation rate, reduced saturation density, or abnormal morphology, but no visible bacterial contamination under standard microscopy.
Potential Causes and Solutions:
Cause: Early-stage mycoplasma contamination without high microbial loads.
- Solution: Implement routine testing using sensitive methods. PCR-based detection can identify over 60 species of Mycoplasma, Acholeplasma, Spiroplasma, and Ureaplasma, including the top contaminating species [1].
Cause: Chronic, low-level infection altering cell behavior without causing cell death.
Cause: Contamination with species that do not grow in standard culture media.
- Solution: Employ multiple detection methods simultaneously. The European Pharmacopeia recommends both direct culture and indicator cell culture methods to detect the broadest range of species [5].
Problem: Confirmed Mycoplasma Contamination
Observation: Positive test result for mycoplasma in valuable cell line.
Elimination Strategies:
Antibiotic Treatment:
- Protocol: Use antibiotics specifically effective against mycoplasma, such as macrolides (clarithromycin), tetracyclines (doxycycline), or fluoroquinolones (levofloxacin) [4]. Standard cell culture antibiotics like penicillin and streptomycin are ineffective due to the lack of mycoplasma cell wall [1].
- Considerations: Treatment requires 2-3 weeks with continuous antibiotic exposure, followed by thorough testing to confirm eradication [6]. Be aware that persistent antibiotic use can lead to resistant strains [2].
Physical Methods:
- Heat Inactivation: For certain reagents and sera, heat treatment at 56°C for 45 minutes can eliminate mycoplasma.
- Filtration: Use 0.1μm pore size filters for sterilizing media and reagents, as standard 0.22μm filters may not retain smaller mycoplasma cells [2].
Last Resort:
- If elimination fails, the contaminated culture should be discarded to prevent laboratory-wide contamination. Always maintain proper seed stock banking to facilitate recovery from such events [1].
Mycoplasma Detection Methodologies
PCR-Based Detection Protocol
PCR detection offers rapid, sensitive identification of mycoplasma contamination and is accepted by regulatory authorities including the FDA and European Pharmacopeia when properly validated [5].
Table 2: Comparison of Major Mycoplasma Detection Methods
| Method | Principle | Duration | Sensitivity | Regulatory Status |
|---|---|---|---|---|
| Direct Culture | Growth on agar/broth; observe "fried egg" colonies | 4-5 weeks [1] | High for cultivable species | Gold standard [5] |
| Indirect Culture (Hoechst Staining) | DNA fluorescence staining of indicator cells | 3-5 days [1] [5] | Detects non-cultivable species | EP-compliant [5] |
| PCR-Based | Amplification of 16S rRNA genes | 1 day [1] | Broad detection (>60 species) [1] | Accepted by EMA/FDA when validated [5] |
Experimental Workflow:
- Sample Collection: Collect supernatant from test cell culture after 72 hours without antibiotic treatment.
- DNA Extraction: Use commercial nucleic acid extraction kits to isolate DNA from both free-floating and cell-associated mycoplasma.
- PCR Setup: Employ universal primers targeting the 16S rRNA gene with a touchdown PCR protocol to enhance sensitivity and specificity [1].
- Inhibition Control: Include test material spiked with known mycoplasma to detect any PCR inhibition [5].
- Analysis: Electrophoretic separation or real-time detection of amplified products.
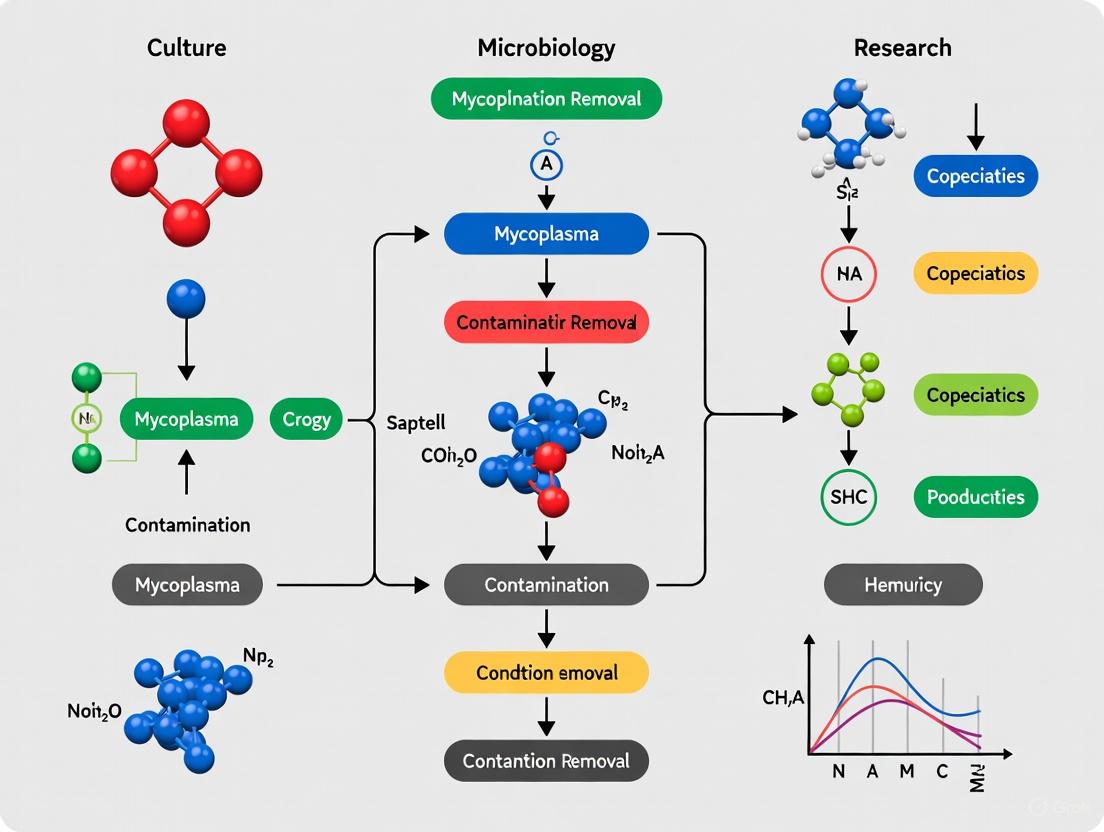
Mycoplasma Detection Workflow
Direct Culture Method Protocol
The agar and broth culture method remains the gold standard for mycoplasma detection with sensitivity of 1-10 CFU/mL [5].
Detailed Methodology:
- Media Preparation: Prepare both agar and broth media specifically formulated to support mycoplasma growth, containing necessary sterols, fatty acids, and nutrients.
- Inoculation: Inoculate test material directly into broth media and onto agar plates. Include positive controls using known mycoplasma species (e.g., M. pneumoniae and M. orale).
- Incubation: Incubate agar plates aerobically and anaerobically at 36±1°C for 14 days. Incubate broth cultures for 21 days.
- Subculture: Transfer broth cultures to fresh agar plates at 3-4 day intervals during the incubation period.
- Colony Examination: Examine all agar plates microscopically for characteristic "fried egg" colonies resulting from central growth into the agar and peripheral surface growth [3].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Mycoplasma Management
| Reagent/Category | Specific Examples | Function and Application |
|---|---|---|
| Detection Kits | MycoProbe Detection Kit, MycoFluor Detection Kit | Fluorescent or enzymatic detection of contaminants [7] [2] |
| DNA Stains | Hoechst 33258, DAPI (4',6-diamidino-2-phenylindole) | Fluorescent DNA binding for microscopic visualization [1] [5] |
| PCR Components | Universal 16S rRNA primers, thermostable DNA polymerase | Amplification of mycoplasma-specific sequences [1] |
| Culture Media | Agar and broth formulations for fastidious organisms | Support growth of diverse mycoplasma species [5] |
| Effective Antibiotics | Macrolides, Tetracyclines, Fluoroquinolones | Treatment of established contaminations [4] |
| Sterilization Filters | 0.1μm pore size membrane filters | Removal from heat-sensitive reagents [2] |
Prevention Strategies for Cell Culture Facilities
Comprehensive Prevention Protocol:
- Quarantine System: Implement mandatory quarantine for all newly acquired cell lines until mycoplasma testing is completed [1].
- Aseptic Technique: Enforce strict aseptic techniques including proper personal protective equipment, dedicated laminar flow hoods, and never reusing pipette tips between cultures [1] [2].
- Cell Banking: Establish comprehensive cell banking systems following the seed stock principle to ensure rapid recovery from contamination events [1].
- Quality Control: Routinely test all cell cultures, media, sera, and reagents for mycoplasma contamination [1].
- Environmental Control: Regularly certify biosafety cabinets and laboratory equipment to prevent contamination spread through malfunctioning equipment [1].
Mycoplasma Prevention Strategy
Vigilance against mycoplasma contamination requires understanding their unique biology and implementing a multifaceted approach to detection, elimination, and prevention. Their lack of a cell wall, small size, and stealthy effects on cell cultures make them a formidable adversary in research and bioproduction settings. By establishing routine monitoring with sensitive detection methods, maintaining strict aseptic techniques, and having validated elimination protocols ready, research and drug development professionals can safeguard their work against this invisible threat. The implementation of these practices is not merely about contamination control—it is fundamental to research reproducibility and the development of safe, effective biopharmaceutical products.
Global Incidence of Mycoplasma Contamination
Mycoplasma contamination is a pervasive and serious problem in cell culture laboratories worldwide. The table below summarizes the key statistics on its global incidence.
| Statistical Measure | Reported Incidence | Context and Sources |
|---|---|---|
| Global Average for Continuous Cell Lines | 15% - 35% [8] [1] | This is the most commonly cited range, with some extreme incidences reported as high as 65-80% [9]. |
| Primary Cell Culture Contamination | Minimum of 1% [1] | Primary cultures are generally less susceptible than continuous cell lines. |
| Incidence of Multiple Species Contamination | 7% - 60% [9] | Many cell cultures are infected with two or more different mycoplasma species simultaneously. |
Frequently Asked Questions (FAQs)
1. What makes mycoplasma contamination so problematic compared to other contaminants? Mycoplasma contamination is often called a "silent" problem because it doesn't cause turbidity in the culture medium and the bacteria are too small to be seen with a standard light microscope [10] [11]. They lack a rigid cell wall, making them resistant to common antibiotics like penicillin and streptomycin [1] [10]. Most alarmingly, they can drastically alter your cell's physiology, leading to unreliable data [1] [10].
2. What are the most common mycoplasma species found in contaminated cell cultures? While over 190 species exist, only a handful account for the vast majority of contaminations. The top species and their common origins are [1] [9]:
- Human Origin (from lab personnel): M. orale, M. fermentans, M. hominis, M. salivarium
- Bovine Origin (from fetal bovine serum): M. arginini, A. laidlawii
- Porcine Origin (from trypsin): M. hyorhinis
3. How does mycoplasma contamination spread so efficiently in a lab? The primary source is most often the laboratory personnel themselves, who can generate aerosols carrying mycoplasma through talking, coughing, or sneezing [10]. Once a single contaminated culture is introduced, cross-contamination can spread it via shared equipment, water baths, incubators, and through aerosols created during pipetting [10] [9]. Studies show that live mycoplasma can be recovered from laminar flow hood surfaces up to six days after working with a contaminated culture [9].
Troubleshooting Guide: Detection and Prevention
Problem: How do I detect a potential mycoplasma contamination?
Observational Signs: While not definitive, your cell culture may show subtle changes [10] [11]:
- Reduced rate of cell proliferation
- Changes in cell morphology and aggregation
- Poor transfection efficiencies
- Persistent unexplained cell death
Confirmatory Testing Methods: The following table compares the most common definitive testing methodologies.
| Method | Principle | Advantages | Disadvantages |
|---|---|---|---|
| PCR-Based [1] | Amplifies mycoplasma-specific DNA sequences (e.g., 16S rRNA). | Rapid (hours to a day), highly sensitive, can detect multiple species, meets regulatory standards [8] [1]. | Cannot distinguish between viable and non-viable organisms. |
| Microbiological Culture [1] [9] | Grows mycoplasma on specialized agar plates to form "fried-egg" colonies. | Considered the "gold standard"; highly specific. | Very slow (takes 4-5 weeks), requires specific expertise, cannot detect all species [1]. |
| DNA Staining (e.g., Hoechst) [1] [9] | Uses a fluorescent dye that binds to DNA. Filamentous staining outside the nucleus indicates contamination. | Relatively fast and inexpensive. | Can yield false positives from cytoplasmic DNA or cell debris; requires an indicator cell line and expert interpretation [12] [1]. |
| Newer Methods | A 2025 study describes a colocalization method using DNA dye (Hoechst) and a cell membrane dye (WGA) [12]. | Minimizes interference from host cell DNA by detecting mycoplasma specifically on the plasma membrane, improving accuracy over DNA staining alone [12]. | Method is still emerging and may not be widely available in all labs. |
The following workflow outlines a systematic approach for diagnosing mycoplasma contamination in the lab:
Problem: How can I prevent mycoplasma contamination?
The core strategy for prevention revolves around strict aseptic technique and rigorous testing. The following diagram maps the key defensive actions in an integrated lab safety plan:
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential reagents and kits used for mycoplasma detection and control.
| Reagent/Kits | Primary Function | Key Considerations |
|---|---|---|
| PCR-Based Detection Kits [8] [1] | Rapid, sensitive detection of mycoplasma DNA in cell culture samples. | Look for kits that detect a broad range of species, including the top 8 contaminants. Ensure they meet guidelines like the European Pharmacopoeia [1]. |
| Hoechst 33258 / DAPI Stains [1] [9] | DNA-binding fluorescent dyes used in staining assays to visualize mycoplasma DNA. | Interpretation can be tricky; requires experience and may need an indicator cell line. Can produce false positives from host cell debris [12] [1]. |
| Microbiological Culture Media [1] [9] | Supports the growth of viable mycoplasma from a sample for definitive confirmation. | The gold standard but very slow. Requires both broth and agar media, and a long incubation period (up to 5 weeks) [1]. |
| Mycoplasma Removal Antibiotics (e.g., Plasmocin) [10] [13] | Treatment of contaminated cultures using antibiotics like macrolides, tetracyclines, or quinolones. | Not a substitute for good technique. Used as a last resort for irreplaceable cells. Treatment requires sufficient duration and concentration, followed by confirmation testing [10] [13]. |
| Validated, Mycoplasma-Free Sera (FBS) [10] [9] | Critical cell culture component that must be sourced from reputable suppliers to avoid introducing contamination. | A historical source of bovine-origin mycoplasma. Reputable suppliers now provide rigorously tested, filtered sera, greatly reducing this risk [9]. |
Frequently Asked Questions
What are the primary species of Mycoplasma I should be concerned about? Over 190 species of Mycoplasma exist, but contamination in cell culture is predominantly caused by a limited number of species from human, bovine, and porcine origins [1]. The table below summarizes the most common culprits, which account for approximately 95% of all contaminations [1].
Table 1: Primary Mycoplasma Species in Cell Culture Contamination
| Origin | Primary Species | Common Source |
|---|---|---|
| Human | M. orale, M. fermentans, M. hominis, M. pirum, M. salivarium | Laboratory personnel, oropharyngeal tract [1] [9] |
| Bovine | M. arginini, Acholeplasma laidlawii | Fetal Bovine Serum (FBS), Newborn Calf Serum [1] [9] |
| Porcine | M. hyorhinis | Trypsin sourced from swine [1] [9] |
Why is Mycoplasma contamination considered such a serious problem? Mycoplasma contamination is a major issue because it is pervasive, difficult to detect, and can drastically alter your research data. An estimated 15-35% of continuous cell lines are affected [1] [9]. Unlike bacterial contamination, it does not cause turbidity in the medium and is invisible to the naked eye under a standard microscope [10]. Furthermore, because Mycoplasma lack a cell wall, they are resistant to common antibiotics like penicillin and streptomycin [10] [1]. The consequences for your cells can be severe, including:
- Chromosomal aberrations [1]
- Disruption of cell metabolism and growth [10]
- Changes in gene expression and virus production [10] [1]
- Decreased transfection rates and cell death [10] [1]
What is the single most significant source of Mycoplasma contamination? The largest percentage of Mycoplasma contamination is of human origin [10] [14] [9]. Laboratory personnel are considered the major source, as talking, sneezing, or coughing can generate aerosols that carry human-specific species like M. orale directly into cultures or onto lab equipment [14] [9].
If FBS and trypsin are sources, should I be concerned about all batches? While Fetal Bovine Serum (FBS) and porcine trypsin are known sources of bovine and porcine Mycoplasma species, their impact has decreased due to advancements in manufacturing and quality control [10]. However, the risk is not zero. It remains the responsibility of the end user to verify that these reagents come from reputable suppliers who perform adequate filtration and provide certification that products are mycoplasma-free [14] [9].
How easily can contamination spread in my laboratory? Extremely easily. A single contaminated culture can spread Mycoplasma throughout the lab. Studies have shown that after handling an infected culture, live Mycoplasma can be isolated from various surfaces in the laminar flow hood (e.g., pipettors, discard pans) and can even survive on these surfaces for four to six days [14] [9]. A clean culture subcultured in the same hood can test positive within just six weeks [14] [9]. Cross-contamination via shared incubators, water baths, and reagents is a significant risk [14].
Experimental Protocols for Detection and Prevention
Routine testing is your best defense against the pervasive and costly effects of Mycoplasma contamination. The following workflow outlines the core processes for maintaining a contamination-free lab.
Protocol 1: PCR-Based Detection Polymerase Chain Reaction (PCR) is a rapid, sensitive, and widely used method for detecting Mycoplasma [10] [1].
- Sample Collection: Collect a sample of the cell culture supernatant. For higher sensitivity, use a sample that has been cultured for at least 2-3 days without antibiotics.
- DNA Extraction: Isolate DNA from the sample using a standard commercial DNA extraction kit.
- PCR Amplification: Perform PCR using universal primers targeted to the 16S rRNA gene of Mycoplasma, which is highly conserved. A "touchdown" PCR protocol is often used to increase sensitivity [1].
- Analysis: Analyze the PCR products by gel electrophoresis. The appearance of a specific band indicates a positive result. This method can identify over 60 species and meets European Pharmacopeia guidelines [1].
Protocol 2: Microbiological Culture Method This method is the gold standard but is more time-consuming [10] [1].
- Inoculation: Inoculate a liquid medium (e.g., mycoplasma broth) with your test sample.
- Incubation: Incubate the broth for a period of four to five weeks.
- Subculture: At defined intervals, subculture the broth onto specialized Mycoplasma agar plates.
- Colony Identification: After incubation, examine the agar plates for the appearance of characteristic "fried-egg" shaped colonies, which signal a positive result [1].
The Scientist's Toolkit: Key Research Reagent Solutions
Having the right reagents and materials is crucial for both preventing and tackling Mycoplasma contamination.
Table 2: Essential Reagents for Mycoplasma Management
| Item | Function & Importance |
|---|---|
| Mycoplasma Detection Kit (PCR) | Provides primers, controls, and buffers for sensitive and specific detection of Mycoplasma DNA in cell cultures [10] [15]. |
| Mycoplasma Removal Antibiotics | Formulations containing antibiotics like macrolides, tetracyclines, or quinolones (e.g., Plasmocin) are used to treat contaminated cultures, as they target Mycoplasma's unique biology [10] [13] [15]. |
| Mycoplasma-Free FBS & Trypsin | Sera and trypsin from reputable suppliers that have been rigorously tested and certified as "Mycoplasma-Free" are critical for preventing bovine and porcine-derived contamination [14] [9]. |
| Hoechst 33258 Stain | A fluorescent DNA stain used in the indirect culture method to detect Mycoplasma filaments in the cytoplasm of infected indicator cells [1]. |
| Antibiotic/Antimycotic Solutions | While ineffective against Mycoplasma, these are used to control other bacterial and fungal contaminants, preventing overgrowth that can mask Mycoplasma presence [16]. |
Mycoplasma contamination represents one of the most significant challenges in cell culture research, affecting an estimated 15-35% of continuous cell lines [1]. These bacteria, the smallest self-replicating organisms, lack a cell wall and can persistently infect cultures while evading detection, ultimately compromising experimental integrity and drug development research. This technical support center provides comprehensive troubleshooting guides and FAQs to help researchers identify, address, and prevent the multifaceted effects of mycoplasma contamination on cellular systems.
Key Effects of Mycoplasma Contamination on Host Cells
Mycoplasma contamination exerts a wide spectrum of effects on host cells, impacting nearly every aspect of cellular physiology and potentially invalidating experimental results. The table below summarizes the primary documented effects:
| Affected Cellular Parameter | Specific Effects | Impact on Research Data |
|---|---|---|
| Cell Metabolism & Growth | Depletion of essential nutrients (amino acids, sugars, nucleic acid precursors) [17]; Decreased cell proliferation rate; Reduced saturation density [2] | Altered cellular response in metabolic assays; unreliable growth curves and viability assays |
| Gene Expression & Function | Changes in gene expression profiles [1]; Disruption of nucleic acid synthesis [1] [10]; Decreased transfection efficiency [1] [10] | Incorrect conclusions in transcriptomics and gene regulation studies; failed or variable transfections |
| Genomic Stability | Chromosomal aberrations and instability [18] [1] | Invalidated genetic studies and data from stable cell lines |
| Signaling Pathways | Activation of NF-κB inflammatory pathway; Inhibition of p53-mediated responses [18] | Skewed results in studies of inflammation, apoptosis, and cell cycle regulation |
| Virus Production & Membrane Function | Altered virus production [1]; Changes in membrane antigenicity [1] | Compromised vaccine development and immunology research |
| Cell Viability | Induction of cell death [1] | General failure of cell cultures and experiments |
Mycoplasma-Host Cell Interaction: Signaling Pathways
Mycoplasmas significantly modulate host cell signaling pathways, primarily through interactions between transcriptional factors. The following diagram illustrates the key pathways involved:
Mycoplasma Modulation of Host Signaling Pathways: Mycoplasmas initiate host cell interactions through membrane components like LAMPs (lipid-associated membrane proteins) and the lipopeptide MALP-2 [18]. These ligands bind to host Toll-like receptors (TLR2/6), triggering a dual signaling response. One arm activates the NF-κB pathway, driving the production of pro-inflammatory cytokines (e.g., TNF-α, IL-6) [18]. Concurrently, mycoplasmas can activate the Nrf2 pathway, inducing anti-inflammatory mediators like heme oxygenase-1 (HO-1) [18]. A critical pathological effect is the inhibition of the p53 tumor suppressor pathway, which disrupts normal cell cycle control and apoptosis, potentially contributing to cellular transformation [18].
FAQs: Mycoplasma Contamination Troubleshooting
Q1: My cell culture isn't turbid, but the cells are growing slowly and transfections are failing. Could this be mycoplasma?
Yes, these are classic signs of mycoplasma contamination. Unlike most bacteria, mycoplasma does not cause media turbidity [19] [2] [10]. The organisms consume essential nutrients from the medium, starving the host cells and leading to reduced proliferation rates and metabolic disturbances [17] [10]. The contamination can also interfere with molecular processes, causing failed or inefficient transfections [1] [10]. You should test your culture immediately.
Q2: I obtained a cell line from a collaborator, and it tested positive for mycoplasma. How can I prevent it from spreading in my lab?
Immediately quarantine the contaminated culture and any reagents used with it [10]. Do not place it in a shared incubator, as mycoplasma can spread via aerosols [1] [10]. Inform your collaborator. To prevent this, always quarantine and test new cell lines for mycoplasma before merging them with your existing cell stocks [15] [10].
Q3: Are the standard Penicillin/Streptomycin antibiotics in my medium effective against mycoplasma?
No, they are completely ineffective for preventing or treating mycoplasma. Mycoplasma lack a cell wall, rendering antibiotics that target cell wall synthesis, like penicillin, useless [1] [2] [10]. Their resistance to other common antibiotics like streptomycin makes them a persistent problem [1]. Relying on standard antibiotics can mask bacterial contamination but allows silent mycoplasma contamination to flourish.
Q4: What is the most reliable method to detect mycoplasma in my cultures?
The most sensitive and specific method is the polymerase chain reaction (PCR) [6] [20] [1]. It can rapidly and reliably detect over 60 species of Mycoplasma, Acholeplasma, and Ureaplasma [1]. Other recognized methods include the microbiological culture assay (considered the historical gold standard but slow) and DNA staining with fluorochromes (e.g., Hoechst 33258 or DAPI), though the latter requires experience to interpret correctly [1] [10].
Mycoplasma Detection and Elimination: Experimental Protocols
Protocol 1: Detection by PCR
PCR is the preferred method for its sensitivity and speed [20] [1].
- Sample Collection: Centrifuge 1 mL of cell culture supernatant (from a culture without antibiotics for at least 2-3 days) for 6 minutes at 13,000 g. Discard the supernatant and wash the pellet with PBS [20].
- DNA Extraction: Re-suspend the pellet in PBS and incubate at 95°C for 15 minutes. Use a commercial DNA clean-up system to extract and purify the DNA [20].
- PCR Amplification: Use universal primers targeting the 16S rRNA gene of mycoplasma. A typical reaction uses 35 cycles of 94°C for 4s, 65°C for 8s, and 72°C for 16s [20]. Always include appropriate positive and negative controls.
- Analysis: Run the PCR product on a 1.4% agarose gel. A positive result is indicated by an amplification product of 515-525 bp [20]. Species identification can be performed by digesting the PCR product with specific restriction enzymes [20].
Protocol 2: Elimination via Antibiotic Treatment
While discarding contaminated cultures is often safest, irreplaceable lines can be treated with specific antibiotics.
- Antibiotic Selection: Use antibiotics specifically designed to target mycoplasma, such as Plasmocin, BM-Cyclin, Baytril (enrofloxacin), or Ciprobay (ciprofloxacin). These are often from the macrolide, tetracycline, or quinolone families [6] [20] [10].
- Treatment Procedure: Replace spent medium with fresh medium containing the selected antibiotic. Treat cells for the recommended duration (e.g., 1-2 weeks), maintaining cultures at a higher cell density and with slightly elevated serum concentration (5-10% more) to counteract potential antibiotic toxicity [20]. Ensure thorough mixing to break up cell clumps and give the antibiotic access to all mycoplasma [20].
- Post-Treatment Validation: After treatment, passage the cells in antibiotic-free medium for at least 14 days before re-testing for mycoplasma using a highly sensitive method like PCR to confirm complete eradication [20].
Research Reagent Solutions for Mycoplasma Management
| Reagent / Material | Primary Function | Application Notes |
|---|---|---|
| Plasmocin | Antibiotic elimination of mycoplasma | Effective for decontaminating chronically infected cell lines; treatment typically lasts 1-2 weeks [20]. |
| BM-Cyclin | Antibiotic elimination of mycoplasma | A combination of two antibiotics effective against a broad range of mycoplasma species [20]. |
| MycoFluor Mycoplasma Detection Kit | Detection via fluorescent staining | Uses a fluorescent dye to stain DNA; reveals extranuclear mycoplasma contamination when viewed under a fluorescence microscope [2]. |
| PCR-Based Detection Kits | Sensitive molecular detection | Rapid and qualitative detection of over 60 species; meets European Pharmacopeia guidelines [1]. |
| 0.1 µm Pore Size Filter | Preventive sterilization | Filters media and reagents to physically remove mycoplasma; standard 0.22 µm filters are insufficient [19]. |
| Mycoplasma Removal Agent (MRA) | Antibiotic elimination | An effective option cited in comparative eradication studies [20]. |
Prevention Best Practices
A robust prevention strategy is the most effective way to protect your research.
- Routine Testing: Implement a policy of testing all cell cultures for mycoplasma every 1-2 months [15].
- Quarantine New Lines: Always quarantine and test new cell lines from external sources before introducing them to your main culture facility [1] [10].
- Aseptic Technique: Adhere to strict aseptic technique, including wearing proper PPE (gloves, lab coat) and working in a certified biosafety cabinet [1] [10].
- Quality Reagents: Source sera, media, and reagents from trusted suppliers that provide mycoplasma-free certification [10].
- Avoid Indiscriminate Antibiotic Use: Do not rely on standard penicillin/streptomycin in routine culture, as this masks low-level contamination and promotes the development of antibiotic-resistant strains [19] [1] [10].
- Maintain Good Cell Banking: Use a seed stock system to ensure you always have a clean, low-passage stock to return to if working stocks become contaminated [1].
Mycoplasma contamination represents one of the most significant and persistent challenges in cell culture research, with profound implications for data integrity and research reproducibility. These minimal, cell wall-deficient bacteria infect an estimated 15-35% of continuous cell lines [6] [1], often evading detection while fundamentally altering cellular physiology and function. The consequences extend beyond simple inconvenience to encompass wasted resources, erroneous conclusions, and compromised therapeutic development [21]. This technical support center provides comprehensive troubleshooting guidance to help researchers identify, address, and prevent mycoplasma contamination in their experimental systems.
FAQs: Understanding Mycoplasma Contamination
Q1: What makes mycoplasma contamination so problematic compared to other biological contaminants?
Mycoplasma contamination presents unique challenges due to several factors:
- Size and structure: As the smallest self-replicating organisms (typically <1µm) lacking a cell wall, they evade detection by routine microscopy and are resistant to common antibiotics like penicillin that target cell wall synthesis [1] [2].
- Stealth characteristics: Contamination doesn't produce turbidity in culture medium [2], allowing infections to persist unnoticed while significantly altering cellular characteristics [6].
- Pervasive effects: Mycoplasmas can affect virtually every cellular parameter, including chromosome integrity, membrane composition, metabolic pathways, and gene expression profiles, leading to experimental artifacts and spurious results [6] [1].
Contemporary contamination primarily occurs through:
- Cross-contamination: Improper handling techniques that transfer infected media between cultures [1].
- Laboratory personnel: Human-borne mycoplasma species introduced through inadequate aseptic technique [22].
- Contaminated reagents: Although less common with modern quality control, contaminated serum and reagents remain potential sources [22].
- Equipment malfunction: Faulty laminar flow systems that disperse contaminated aerosols [1].
Q3: Why don't standard antibiotic cocktails prevent mycoplasma contamination?
Routine cell culture antibiotics are typically ineffective because:
- β-lactam antibiotics (penicillin, ampicillin) target cell wall synthesis, which mycoplasmas lack [1].
- Aminoglycosides (streptomycin, gentamycin) show variable efficacy, with many mycoplasma strains exhibiting resistance at concentrations routinely used in cell culture [1].
- Prolonged antibiotic use can promote selection of resistant strains while providing a false sense of security [1].
Troubleshooting Guides
Guide 1: Detecting Mycoplasma Contamination
Symptoms and Initial Observations
While mycoplasma contamination often presents no visible signs, these indicators warrant investigation:
- Decreased cell proliferation rates despite regular medium changes [2]
- Reduced saturation density in adherent cultures [2]
- Agglutination in suspension cultures [2]
- Unexplained changes in cellular metabolism or gene expression patterns [1]
Table 1: Comparison of Mycoplasma Detection Methods
| Method | Principle | Time Required | Sensitivity | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Direct Culture | Growth on specialized agar/broth | 4-5 weeks | High | Historical "gold standard" | Slow; not all strains grow well [1] |
| DNA Staining (Hoechst) | Fluorescent dye binding to DNA | 1-2 days | Moderate | Visual confirmation; cost-effective | Subjective interpretation; requires expertise [1] [22] |
| PCR-based Methods | Amplification of mycoplasma-specific 16S rRNA sequences | 1-2 days | High (~6.3 pg DNA) [22] | Broad species coverage (92%); rapid; specific [22] | Requires specialized equipment; possible false positives |
Recommended Protocol: PCR-Based Detection
A robust PCR protocol utilizing ultra-conserved eukaryotic and mycoplasma sequence primers can detect approximately 92% of all Mycoplasmatota species [22]:
Sample Preparation:
- Collect cell culture supernatant (1mL) and pellet by centrifugation (13,000 × g, 6 minutes)
- Wash pellet twice with phosphate-buffered saline (PBS)
- Resuspend in 100μL PBS and incubate at 95°C for 15 minutes
- Extract DNA using commercial clean-up systems [20]
PCR Reaction Setup:
- Use universal primers targeting 16S rRNA gene
- Include internal control (eukaryotic DNA) to confirm reaction validity
- Apply touchdown PCR protocol to enhance sensitivity and specificity [22]
Interpretation:
- Positive control: 166-191 bp amplification product indicates mycoplasma DNA
- Internal control: 105 bp product confirms presence of eukaryotic DNA and reaction validity [22]
Guide 2: Eliminating Mycoplasma Contamination
Antibiotic Treatment Strategies
When valuable cell lines cannot be replaced, antibiotic treatment provides a practical elimination approach:
Table 2: Antibiotic Efficacy in Mycoplasma Eradication
| Antibiotic | Target | Treatment Duration | Success Rate | Considerations |
|---|---|---|---|---|
| Plasmocin | Dual mechanism | 14 days | 78-84% [20] | Well-tolerated by most cell lines |
| BM-Cyclin | Protein synthesis | 7 days cycles | Variable | Can be cytotoxic with extended use |
| Baytril (Enrofloxacin) | DNA gyrase | 7-14 days | Effective for resistant strains [6] | Alternative for Plasmocin failures |
| MycoZap | Multiple targets | 3-7 days | High in combination approaches | Commercial combination product |
Comprehensive Elimination Protocol
Pre-treatment Considerations:
- Always begin with backup frozen stocks when possible
- Confirm contamination with specific PCR before treatment
- Prepare treatment media freshly for each application
Treatment Procedure (using Plasmocin as example):
- Culture preparation: Start with healthy, 50-60% confluent cultures in fresh medium
- Antibiotic application: Add Plasmocin directly to culture medium according to manufacturer specifications
- Optimized culture conditions: Maintain cells at higher densities with 5-10% increased FBS concentration to counter potential antibiotic toxicity [20]
- Treatment duration: Continue treatment for 14 days with regular medium changes containing antibiotics
- Monitoring: Observe cells daily for signs of stress or cytotoxicity
Post-treatment Verification:
- Maintain cells in antibiotic-free medium for at least 14 days
- Test for mycoplasma using PCR at days +14, +28, and +42 post-treatment
- Only consider cells cured after three consecutive negative tests over 6 weeks [20]
Contingency for Resistant Strains:
- For Plasmocin-resistant contaminants, alternative antibiotics (Baytril, BM-Cyclin, Ciprobay, MRA) have proven effective in achieving 100% eradication rates in resistant cases [20]
Guide 3: Preventing Mycoplasma Contamination
Comprehensive Prevention Strategy
Implementing a multi-layered approach significantly reduces contamination risk:
Laboratory Practice Fundamentals:
- Aseptic technique: Strict adherence to protocols including proper PPE and biosafety cabinet use [1] [23]
- Quarantine procedures: Isolate new cell lines until mycoplasma status is confirmed [1]
- Cell banking: Implement seed stock systems with regular testing to ensure backup availability [1]
- Equipment maintenance: Regular certification of biosafety cabinets and laminar flow systems [1]
Technical Safeguards:
- Sterile filtration: Use 0.1μm filters for media and reagent sterilization [2]
- Single-use systems: Pre-sterilized, disposable consumables minimize cross-contamination [23]
- Environmental monitoring: Regular screening of incubators, water baths, and work surfaces
Quality Control Program:
- Routine testing: Schedule mycoplasma screening at regular intervals (e.g., monthly)
- Cell line authentication: STR profiling to ensure identity and purity [24]
- Documentation: Maintain detailed records of testing results and cell line history
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Mycoplasma Management
| Reagent/Category | Specific Examples | Function/Application | Notes |
|---|---|---|---|
| Detection Reagents | Hoechst 33258, MycoFluor | DNA staining for visualization | Requires fluorescence microscopy [2] |
| PCR Kits | Universal 16S rRNA primers, commercial kits | Molecular detection | High sensitivity and specificity [22] |
| Elimination Antibiotics | Plasmocin, BM-Cyclin, Enrofloxacin | Treatment of contaminated cultures | Target-specific mechanisms [20] |
| Culture Media Components | High-quality FBS, specialized supplements | Maintain cell health during treatment | Enhanced concentrations during antibiotic treatment [20] |
| Sterilization Supplies | 0.1μm filters, validated sterile containers | Preventative contamination control | Critical for reagent preparation [2] |
Mycoplasma contamination represents a significant threat to research integrity, with the potential to compromise years of experimental work and substantial research investment. The implementation of rigorous detection protocols, strategic elimination approaches, and comprehensive prevention strategies provides a framework for safeguarding cell culture systems. By adopting these troubleshooting guidelines and maintaining vigilant quality control practices, researchers can protect the validity of their data, ensure the reproducibility of their findings, and uphold the highest standards of scientific rigor in cell culture-based research.
Actionable Strategies: From Reliable Detection to Effective Eradication
Mycoplasma contamination is one of the most pervasive and challenging issues in cell culture, affecting an estimated 15-35% of continuous cell lines worldwide [10]. These minute prokaryotes lack cell walls and can profoundly alter cell physiology, metabolism, and experimental outcomes while remaining undetectable by routine microscopy [9] [2]. For researchers and drug development professionals, implementing robust detection strategies is crucial for data integrity and regulatory compliance. This guide examines the three gold-standard methods—microbiological culture, PCR, and DNA staining—providing technical protocols, troubleshooting advice, and reagent solutions to safeguard your research against these stealth contaminants.
▎Frequently Asked Questions (FAQs)
Q1: Why is mycoplasma contamination so problematic in cell culture?
Mycoplasma contamination poses a significant threat because it:
- Escapes visual detection: Due to their small size (0.1–0.3 µm) and lack of cell wall, they don't cause turbidity in media [10] [25].
- Alters cellular functions: Contamination affects cell metabolism, gene expression, proliferation, and can cause chromosomal aberrations [26] [10] [25].
- Resists common antibiotics: Their lack of a cell wall makes them resistant to penicillin, streptomycin, and other antibiotics targeting cell wall synthesis [9] [10].
- Spreads easily: A single contaminated culture can spread mycoplasma throughout the laboratory via aerosols, shared equipment, or poor technique [9] [27].
The main sources include:
- Laboratory personnel: Human oral/respiratory flora (e.g., M. orale, M. fermentans) introduced via talking, coughing, or improper aseptic technique [9] [10].
- Cross-contamination: From infected cell lines, especially when new lines are introduced without proper quarantine and testing [10].
- Reagents: While less common today, contaminated animal-derived products like fetal bovine serum (source of M. arginini, A. laidlawii) or trypsin (source of M. hyorhinis) can be sources [9].
Q3: We perform regular visual checks of our cultures. Is this sufficient to detect mycoplasma?
No, visual inspection alone is not sufficient. Mycoplasma contamination does not produce the visible turbidity typical of other bacterial infections [2]. While chronic contamination might eventually cause subtle changes like decreased proliferation rate or altered morphology, these signs often appear late and are non-specific [25]. Regular testing using one of the gold-standard methods is essential for reliable detection.
Q4: Can we use the same 0.2µm filters that prevent bacterial contamination to remove mycoplasma from media?
Not reliably. The small size and flexible membrane of mycoplasma (0.1–0.3 µm) allow them to potentially pass through 0.2 µm filters [9] [10]. For maximum protection, use 0.1 µm pore size filters for sterilizing media and reagents, and apply low differential pressure (5-10 psi) during filtration [9].
▎Detection Method Comparisons
Table 1: Gold-Standard Mycoplasma Detection Methods at a Glance
| Method | Principle | Detection Sensitivity | Time to Result | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Microbiological Culture | Growth on specialized agar and in broth media, observed for "fried-egg" colonies [28] [29]. | High (≤10 CFU/mL) [30] | 28+ days [28] | Regarded as the ultimate reference; required by pharmacopeias [30]. | Extremely slow; requires expertise; cannot detect non-cultivable species [28] [29]. |
| DNA Staining (e.g., Hoechst) | Stains extranuclear DNA on the surface of indicator cells using a fluorescent dye [28] [2]. | Moderate to High [29] | 1-2 days (including indicator cell co-culture) [28] | Visually demonstrates contamination location; relatively inexpensive. | Can be difficult to interpret; host cell DNA can cause false positives [12] [29]. |
| PCR/qPCR | Amplifies mycoplasma-specific DNA sequences (e.g., 16S rRNA genes) [28] [30]. | High (a few genome copies) [28] | 2.5 hours to 5 hours [28] | Rapid, highly sensitive, and specific; ideal for high-throughput screening. | Risk of false positives from contamination; does not distinguish viable/non-viable cells [28]. |
Advanced Workflow for Mycoplasma Detection
The following diagram summarizes the decision-making process for selecting and implementing the primary detection methods.
▎Detailed Experimental Protocols
Protocol 1: Detection by Microbiological Culture
Principle: This method inoculates sample supernatant into both liquid broth and onto solid agar media specially formulated to support the fastidious growth of mycoplasma. The cultures are monitored for microbial growth, which is confirmed by the appearance of characteristic "fried-egg" colonies on agar plates [28].
Procedure:
- Sample Preparation: Aseptically collect at least 1 mL of supernatant from the test cell culture at the end of its growth phase, without antibiotics [28].
- Inoculation:
- Inoculate 0.1 mL - 0.2 mL of the sample into a tube of liquid mycoplasma broth medium.
- Inoculate 0.1 mL onto a solid mycoplasma agar plate and spread evenly.
- Incubation:
- Incurate both broth and agar cultures aerobically at 36°C ± 1°C with 5-10% CO₂.
- For a comprehensive test, also incubate a separate set of cultures anaerobically.
- Monitoring and Subculture:
- Examine the broth daily for color change (indicating growth) and the agar weekly for colony formation.
- On days 3, 7, and 14, subculture 0.1 mL from the broth onto a fresh agar plate.
- Result Interpretation:
Protocol 2: Detection by DNA Fluorochrome Staining
Principle: A DNA-binding fluorescent dye, such as Hoechst 33258, is used to stain DNA in a fixed cell culture. Under a fluorescence microscope, mycoplasma contamination appears as bright, extranuclear speckles or filaments on the surface of the host cells [2]. Using an indicator cell line like Vero cells can amplify the signal and improve reliability [28] [29].
Procedure:
- Sample Inoculation onto Indicator Cells:
- Seed sterile coverslips in a culture dish with an indicator cell line (e.g., Vero cells).
- The next day, inoculate the test sample supernatant onto the indicator cells.
- Incubate for 3-5 days to allow potential mycoplasma to proliferate [28].
- Fixing and Staining:
- Rinse the cells with PBS and fix with a freshly prepared mixture of acetic acid and methanol (1:3) for 5-10 minutes.
- Air dry the fixed cells.
- Stain with Hoechst 33258 solution (e.g., 0.05 - 0.1 µg/mL in PBS) for 15-30 minutes in the dark.
- Mounting and Visualization:
- Rinse the coverslip gently with deionized water to remove excess stain.
- Mount the coverslip on a glass slide with a mounting medium.
- Examine under a fluorescence microscope with appropriate filters (e.g., excitation ~365 nm, emission ~450 nm).
- Result Interpretation:
Troubleshooting Tip: To mitigate interference from host cell cytoplasmic DNA, which can cause false positives, a co-localization method using a combination of DNA stain (Hoechst) and a cell membrane dye (e.g., WGA) has been developed. This confirms contamination by showing mycoplasma DNA is localized to the plasma membrane [12].
Protocol 3: Detection by PCR/qPCR
Principle: This method uses polymerase chain reaction (PCR) to amplify specific, conserved regions of the mycoplasma genome (e.g., the 16S rRNA gene) present in a sample. Real-time PCR (qPCR) allows for the detection and quantification of the amplified DNA during the reaction, providing rapid results [28] [30].
Procedure:
- Sample Preparation:
- Collect 0.1 - 0.5 mL of cell culture supernatant.
- Extract genomic DNA according to the instructions of your commercial DNA extraction kit. Include both positive (known mycoplasma DNA) and negative (nuclease-free water) controls.
- Reaction Setup:
- Prepare the PCR master mix according to the kit's instructions. Most commercial mycoplasma detection kits use primers targeting the 16S rRNA gene to detect a broad spectrum of species (up to 100) [28].
- A recent pharmacopoeia-compliant assay uses a simplified design with just two primers and two hydrolysis probes to detect 11 relevant species [30].
- Aliquot the mix into PCR tubes and add the extracted template DNA.
- Amplification:
- Place the tubes in a real-time PCR instrument.
- Run the appropriate cycling program (typically 40-45 cycles of denaturation, annealing, and extension).
- Result Interpretation:
- Positive Result: A clear amplification curve that crosses the threshold within the cycle limit. Specificity is confirmed by the probe's fluorescence signal [30].
- Negative Result: No amplification curve is detected, or the signal does not cross the threshold.
▎Research Reagent Solutions
Table 2: Essential Reagents for Mycoplasma Detection
| Reagent / Kit | Function / Application | Example Products / Components |
|---|---|---|
| Specialized Culture Media | Supports the fastidious growth of mycoplasma for the culture method. Contains beef heart infusion, yeast extract, horse serum, and other essential nutrients [28]. | Mycoplasma Broth, Mycoplasma Agar |
| Fluorescent DNA Stains | Binds to DNA, allowing visualization of mycoplasma (extranuclear DNA) under a fluorescence microscope. | Hoechst 33258, DAPI [10] [29] |
| Broad-Spectrum PCR Kits | Contains optimized primers and probes for the highly sensitive and specific detection of a wide range of mycoplasma species by PCR/qPCR. | ATCC Universal Mycoplasma Detection Kit, MycoSEQ Detection System, MycoTOOL Test (Roche) [28] |
| Indicator Cell Lines | Used in the DNA staining method to amplify low-level mycoplasma contamination, making it easier to detect. | Vero cells (recommended by pharmacopeias) [28] |
Effectively combating mycoplasma contamination requires a strategic defense built on prevention, routine monitoring, and precise detection. No single detection method is perfect; the choice depends on your specific needs for speed, regulatory compliance, and visual confirmation. For the highest assurance, particularly with irreplaceable cell lines or in regulated environments, using a combination of these gold-standard methods is the most robust strategy. By integrating the protocols and troubleshooting guides provided in this technical center, research and development teams can significantly reduce the risk of mycoplasma compromising their valuable work.
A Step-by-Step Protocol for PCR-Based Detection in Cell Culture Supernatant
Mycoplasma contamination is a serious and prevalent issue in cell culture laboratories, affecting an estimated 15-30% of continuous cell lines worldwide [26]. These contaminants severely compromise cellular characteristics, leading to experimental artefacts and spurious results by altering cell metabolism, slowing proliferation, and causing chromosomal aberrations [31] [32] [25]. Unlike bacterial or fungal contaminants, mycoplasma often go undetected by routine light microscopy due to their small size (0.1-0.3 μm) and lack of a cell wall [26] [25]. PCR-based detection has become the preferred method for identifying mycoplasma contamination because it offers high sensitivity, specificity, and rapid results compared to traditional culture methods that can take several weeks [32] [33].
Principle of Direct Detection from Culture Supernatant
Traditional PCR-based detection involves three steps: cell culture supernatant collection, DNA isolation, and PCR amplification. However, researchers have developed a modified approach that allows cell culture supernatant to be used directly for PCR without the need for DNA extraction [31]. This modification offers significant advantages:
- Time Efficiency: Eliminates the DNA extraction step, providing faster results
- Enhanced Sensitivity: Prevents loss of mycoplasma DNA that can occur during extraction, particularly important when contamination levels are very low [31]
- Practicality: Simplifies the workflow while maintaining detection capability
This direct method can detect less than 10 colony-forming units (CFU) of the most frequently encountered mycoplasma contaminants in mammalian cell cultures, making it suitable for routine testing in research and biopharmaceutical production [33].
Materials and Equipment
Research Reagent Solutions
Table: Essential Reagents for PCR-Based Mycoplasma Detection
| Reagent/Equipment | Function/Purpose | Specifications/Notes |
|---|---|---|
| Cell Culture Supernatant | Sample containing potential mycoplasma contaminants | Collect from cultured cells without disturbing adherent cells |
| PCR Master Mix | Contains DNA polymerase, dNTPs, and reaction buffer | Use kits specifically validated for mycoplasma detection [32] |
| Mycoplasma-Specific Primers | Amplify target mycoplasma DNA sequences | Designed for conserved regions across common contaminant species |
| Internal Control DNA | Monitor PCR inhibition and reaction efficiency | Amplifies at ~481 bp; absence indicates potential issues [32] |
| Positive Control | Verify assay functionality | Contains known mycoplasma DNA sequence |
| Negative Control | Detect contamination in reagents | Nuclease-free water instead of template |
| Agarose Gel Electrophoresis System | Visualize PCR products | Confirm expected band sizes |
| Thermal Cycler | Amplify DNA through temperature cycling | Standard PCR cycling capabilities |
Step-by-Step Protocol
Sample Collection and Preparation
- Collect Cell Culture Supernatant: Aseptically remove 100-500 μL of supernatant from your cell culture, taking care not to disturb adherent cells.
- Heat Treatment: Transfer 100 μL of supernatant to a sterile amplification tube and incubate at 95°C for 5 minutes [32].
- Storage: Processed samples can be stored at 2-8°C for up to one week if not used immediately.
- Pre-PCR Processing: Briefly centrifuge the sample for 5 seconds to pellet any cellular debris before use in PCR.
PCR Reaction Setup
Table: PCR Reaction Components for Mycoplasma Detection
| Component | Volume per Reaction | Final Concentration |
|---|---|---|
| JumpStart Taq DNA Polymerase/Rehydration Buffer Mix | 23 μL | 1× |
| Processed Sample or Control | 2 μL | - |
| Total Volume | 25 μL | - |
Preparation Notes:
- For the negative control, add 2 μL of DNA-free water instead of sample
- For the positive control, use specialized reaction tubes if provided in commercial kits [32]
- Mix contents by flicking tubes gently; avoid vortexing to prevent shearing DNA
- Incubate all reaction tubes at room temperature for 5 minutes before thermal cycling
Thermal Cycling Conditions
Place reaction tubes in a thermal cycler programmed with the following parameters:
- Initial Denaturation: 94°C for 30 seconds
- Amplification Cycles (40 cycles):
- Denaturation: 94°C for 30 seconds
- Annealing: 55°C for 30 seconds
- Extension: 72°C for 40 seconds
- Final Extension: 72°C for 5-10 minutes
- Hold: 4°C until analysis [32]
Analysis of Results
After PCR completion, analyze products using agarose gel electrophoresis:
- Load 8 μL of each PCR reaction directly onto a 1.5-2% agarose gel containing a DNA-intercalating dye
- Perform electrophoresis until adequate separation is achieved (migration of 2.5-3.0 cm)
- Visualize bands under UV light and interpret results:
Result Interpretation:
- Negative Sample: Band at approximately 481 bp (internal control) with no band at 270 bp
- Positive Sample: Band in the range of 270 ± 8 bp (heaviness indicates contamination level)
- Inhibited Sample: No bands at all, requiring DNA extraction to remove inhibitors [32]
- Heavily Contaminated Samples: May show only the 270 bp band with absent internal control
Troubleshooting Guide
Table: Common PCR Issues and Solutions in Mycoplasma Detection
| Problem | Possible Causes | Recommended Solutions |
|---|---|---|
| No Amplification | Poor template quality or quantity | Ensure proper sample collection and heat treatment [31] |
| PCR inhibitors in sample | Perform DNA extraction to remove inhibitors [32] | |
| Insufficient enzyme activity | Verify polymerase concentration and storage conditions [34] | |
| Weak or Faint Bands | Low level contamination | Increase number of PCR cycles to 40 [34] |
| Suboptimal primer annealing | Optimize annealing temperature in 1-2°C increments [34] | |
| Insufficient Mg2+ concentration | Optimize Mg2+ concentration for maximum yield [34] | |
| Non-Specific Bands | Low annealing temperature | Increase annealing temperature by 2-3°C [35] |
| Excess primers | Optimize primer concentration (usually 0.1-1 μM) [34] | |
| Contaminated reagents | Prepare fresh working stocks and use dedicated equipment [35] | |
| Smeared Bands | Degraded DNA template | Ensure proper sample storage and handling [34] |
| Excessive cycle number | Reduce number of cycles to minimum necessary [34] | |
| Contaminated primers | Switch to new primer sets with different sequences [35] |
Frequently Asked Questions (FAQs)
Q1: How frequently should I test my cell cultures for mycoplasma contamination? Regular testing is essential for maintaining contamination-free cell lines. The frequency depends on your specific application, but for valuable cell lines, testing should be performed at least monthly or when exchanging lines with other laboratories. Strict adherence to good laboratory practices and routine testing are highly recommended for successful mycoplasma control [32].
Q2: Can I use this direct method for all types of cell cultures? The direct PCR method using culture supernatant works well for most standard cell lines. However, for primary cells, stem cells, or sensitive cell lines, you may need to optimize the sample volume or consider DNA extraction if inhibition occurs. For particularly valuable cultures, commercial elimination reagents like Mynox or Mynox Gold are recommended for treatment [26].
Q3: What are the most common mycoplasma species that contaminate cell cultures? The strains most commonly contaminating cell cultures include Mycoplasma arginini, Mycoplasma fermentans, Mycoplasma hyorhinis, Mycoplasma orale, and Mycoplasma bovis [25]. A well-designed PCR assay should detect all these common contaminants.
Q4: My PCR shows inconsistent results. What should I check first? First, verify that all necessary reagents were added to the reaction and were free from contamination. Then, systematically check the quality of your template DNA and optimize Mg2+ concentration and annealing temperatures, as these factors affect PCR stringency and are likely to address most issues [35].
Q5: What should I do if my cell culture tests positive for mycoplasma? When contamination is confirmed, the safest course is to dispose of the culture immediately. If the cell line is irreplaceable, consider using specialized elimination reagents like Mynox which can remove mycoplasma from infected cultures in just a few days through a biophysical mechanism that avoids antibiotics [26]. Always verify elimination success with follow-up testing.
The direct PCR detection method from cell culture supernatant provides a rapid, sensitive, and practical approach for monitoring mycoplasma contamination. By eliminating the DNA extraction step, this protocol saves time while improving detection sensitivity for low-level contamination. Regular implementation of this testing protocol, combined with good laboratory practices, is essential for maintaining the integrity of cell-based research and ensuring experimental reproducibility.
Frequently Asked Questions (FAQs)
Q1: What are the primary antibiotics used to treat mycoplasma contamination in cell culture? The most common antibiotics for eliminating mycoplasma are tetracyclines, quinolones, and macrolides. Plasmocin, a commercially prepared reagent, is a specifically formulated combination that is highly effective and commonly used. These antibiotics target essential bacterial processes without a cell wall, such as protein synthesis and DNA replication [10] [13].
Q2: Why are standard antibiotics like penicillin ineffective against mycoplasma? Mycoplasma lack a rigid cell wall [36] [10]. Antibiotics such as penicillin and streptomycin work by targeting and disrupting the cell wall synthesis of bacteria [10]. Because mycoplasma do not have this structure, they are naturally resistant to these common cell culture antibiotics [10] [37].
Q3: What is a major consideration when using tetracyclines in cell culture? Tetracyclines inhibit protein synthesis by preventing the attachment of aminoacyl-tRNA to the ribosomal acceptor site [38]. A critical consideration is that they are toxic to certain intracellular bacteria, such as those in the genera Rickettsia and Ehrlichia [36]. If your research involves culturing these organisms, tetracyclines cannot be used for mycoplasma decontamination.
Q4: How long does a typical antibiotic treatment regimen last? Treatment regimens can vary by product, but often last one to two weeks. For example, Plasmocin is typically added to culture media at 25 μg/mL for one to two weeks [13]. It is crucial to follow the specific protocol for the antibiotic you are using.
Q5: How do I confirm that the mycoplasma contamination has been eliminated? After completing the antibiotic treatment, culture your cells without any antibiotics for one to two weeks [13]. Then, test the culture again using a reliable detection method, such as PCR, to confirm the absence of mycoplasma [10] [13]. A single negative test immediately after treatment is not sufficient confirmation, as the contamination level might only be suppressed below the detection limit [10].
Troubleshooting Guide
Problem: Contamination Persists After Treatment
- Potential Cause 1: Incorrect antibiotic concentration or treatment duration.
- Solution: Ensure the antibiotic is used at the recommended concentration and that the full treatment course is completed without interruption. Under-dosing can select for resistant mycoplasma [10].
- Potential Cause 2: The specific mycoplasma strain is resistant to the antibiotic used.
- Solution: Antibiotic susceptibilities can vary considerably between mycoplasma species and even between strains of the same species [36]. Consider trying an antibiotic from a different class (e.g., switch from a tetracycline to a quinolone) or using a combination product like Plasmocin.
- Potential Cause 3: Re-contamination from an untreated source.
- Solution: The original culture may have been successfully treated, but the contamination was reintroduced from another contaminated cell line, reagent, or equipment in the lab [10]. Quarantine all treated cultures and thoroughly decontaminate the workspace and equipment. Use a product like Myco-Out Mycoplasma Removal Spray on surfaces [37].
Problem: Cells Appear Unhealthy or Die During Treatment
- Potential Cause: Cytotoxicity from the antibiotic.
- Solution: Some antibiotics can be toxic to certain cell lines at the concentrations required to kill mycoplasma. Optimize the dose and duration, or try a different, less cytotoxic anti-mycoplasma antibiotic [10] [37]. Always include a control well of uninfected cells to monitor the antibiotic's effects on cell health.
Antibiotic Mechanisms and Data
Mechanisms of Action
The following diagram illustrates the cellular mechanisms of the primary antibiotic classes used against mycoplasma.
Quantitative Antibiotic Data
The table below summarizes key information on antibiotic classes used for mycoplasma eradication.
Table 1: Antibiotic Classes for Mycoplasma Elimination
| Antibiotic Class | Molecular Target | Primary Effect | Common Examples | Key Considerations |
|---|---|---|---|---|
| Tetracyclines [38] [39] | 30S ribosomal subunit | Inhibits protein synthesis by blocking tRNA attachment [38] [39]. | Tetracycline, Doxycycline, Minocycline | Bacteriostatic [39]; Toxic to some intracellular bacteria (e.g., Rickettsia) [36]. |
| Quinolones [40] | DNA gyrase (Topo II) & Topoisomerase IV | Inhibits DNA replication and transcription by blocking bacterial topoisomerases [40]. | Ciprofloxacin, Moxifloxacin | Bactericidal; Varying resistance in some mycoplasma species [36]. |
| Macrolides | 50S ribosomal subunit | Inhibits protein synthesis. | - | Often used in commercial combination kits. |
| Lincosamides [36] | 50S ribosomal subunit | Inhibits protein synthesis. | Clindamycin | Used in combination with daptomycin for in vitro decontamination [36]. |
Experimental Protocols
Protocol 1: Standard Antibiotic Treatment with Plasmocin
This protocol outlines the general procedure for using a commercial antibiotic like Plasmocin to eliminate mycoplasma contamination [13].
- Confirmation of Contamination: Verify mycoplasma contamination using a reliable detection method (e.g., PCR, fluorescence staining) before starting treatment.
- Preparation of Medicated Medium: Supplement your standard cell culture medium with Plasmocin at a working concentration of 25 µg/mL [13]. Ensure the antibiotic is fully dissolved and the medium is sterile.
- Treatment Phase: Culture the contaminated cells in the medicated medium. Pass the cells as you normally would, maintaining continuous exposure to the antibiotic for a period of 1 to 2 weeks [13].
- Post-Treatment Phase & Validation: After the treatment period, culture the cells in standard antibiotic-free medium for 1 to 2 weeks [13].
- Clearance Test: Perform at least two additional mycoplasma tests at weekly intervals after the antibiotic-free period to confirm complete eradication [13].
Protocol 2: In-house Antibiotic Treatment for Challenging Contaminants
This protocol is adapted from recent research demonstrating successful decontamination of Mycoplasma arginini and M. orale from cultures of intracellular bacteria [36].
- Identify Contaminant: If possible, identify the mycoplasma species, as susceptibility can vary [36].
- Prepare Antibiotic Cocktail: Use a combination of daptomycin (a lipopeptide that disrupts the cell membrane) and clindamycin (a lincosamide that inhibits protein synthesis) [36].
- Treatment and Passage: Culture the contaminated cells in medium containing the antibiotic cocktail. The specific concentration and duration may require optimization, but the combination has proven effective against multiple Rickettsia and Ehrlichia cultures [36].
- Validation: Following treatment, use a specific detection method like a multiplex PCR assay to confirm the absence of the mycoplasma species that were previously identified [36].
The workflow for a typical decontamination experiment is summarized below.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Mycoplasma Management
| Reagent / Kit | Primary Function | Brief Description & Utility |
|---|---|---|
| Plasmocin | Mycoplasma Elimination | A commercially available, formulated antibiotic mixture widely used for prophylactic treatment and eradication of mycoplasma from cell cultures [13]. |
| Myco-Sniff Mycoplasma PCR Detection Kit | Mycoplasma Detection | A highly sensitive and specific PCR-based kit for rapid detection of mycoplasma contamination in cell cultures [37]. |
| Daptomycin & Clindamycin | Mycoplasma Elimination (In-house) | An effective antibiotic combination for in vitro clearance of common contaminants like M. arginini and M. orale, especially useful for cultures of sensitive intracellular bacteria [36]. |
| Myco-Visible Mycoplasma Rapid Test Kit | Mycoplasma Detection | An immunochromatographic test device that delivers results in under an hour, ideal for routine monitoring without needing specialized equipment [37]. |
| Myco-Out Mycoplasma Removal Spray | Laboratory Decontamination | A ready-to-use spray for surface decontamination of laminar flow cabinets and equipment to prevent the spread of mycoplasma in the lab [37]. |
Mycoplasma contamination represents one of the most significant and challenging problems in cell culture research, affecting an estimated 15-35% of continuous cell cultures [1]. These minimal bacteria lack cell walls, rendering conventional antibiotics like penicillin ineffective and contributing to their persistence as stubborn contaminants [2] [1]. While antibiotics remain a first-line defense, researchers increasingly face mycoplasma strains that demonstrate resistance or develop tolerance through biofilm formation [41]. This technical guide explores advanced physical methods and in vivo passaging techniques that effectively eradicate mycoplasma contamination when standard approaches fail, providing researchers with practical solutions for preserving precious cell lines and maintaining experimental integrity.
FAQs: Understanding Mycoplasma Contamination
What makes mycoplasma particularly difficult to eliminate using standard antibiotics?
Mycoplasma possess unique biological characteristics that complicate conventional antibiotic treatment. Their natural resistance to beta-lactam antibiotics (such as penicillin) stems from the absence of a cell wall, which is the target mechanism for these drugs [2] [1]. Additionally, mycoplasma can form biofilm structures that substantially increase their resistance profile. Research on Mycoplasma pneumoniae demonstrates that biofilm-grown bacteria can survive erythromycin concentrations up to 512 µg/mL, which represents 8,500-128,000 times the minimal inhibitory concentration (MIC) for planktonic cells [41]. This enhanced tolerance necessitates alternative eradication strategies beyond conventional antibiotic regimens.
How does in vivo passaging through mice eliminate mycoplasma contamination?
The in vivo passaging method leverages the mammalian immune system and physiological environment to clear mycoplasma contamination from patient-derived organoids (PDOs). This approach involves injecting contaminated cells into immunocompromised mice, allowing tumors to establish, then re-isolating and re-establishing the cell culture from the harvested xenografts [42]. A recent study demonstrated 100% effectiveness (9/9 colorectal cancer PDOs) in eliminating mycoplasma contamination using this technique, as confirmed by PCR detection methods [42]. The process essentially "resets" the culture by exploiting the biological disparity between mammalian cells and mycoplasma parasites within a living system.
Are there physical or chemical methods that can target mycoplasma without antibiotics?
Yes, several non-antibiotic approaches show efficacy against mycoplasma. Hydrogen peroxide (H₂O₂) has demonstrated particular promise, as mycoplasma biofilm towers show no enhanced defense against this treatment despite their increased resistance to antibiotics [41]. Additionally, proper filtration of culture media, serum, and reagents through 0.1μm sterilization filters can physically remove mycoplasma due to their small size (typically <1μm) [2]. These methods provide valuable alternatives when antibiotic resistance or concerns about cellular toxicity limit treatment options.
What are the limitations of these advanced eradication methods?
While effective, these approaches present significant practical challenges. The in vivo passaging method requires animal facilities, appropriate ethical approvals, extended timeframes (weeks to months), and specialized expertise in xenograft techniques [42]. Hydrogen peroxide treatment, while effective, must be carefully optimized to balance mycoplasma eradication with potential cytotoxicity to the cultured cells [41]. Additionally, these methods generally require subsequent validation of cell line identity and functionality, as the decontamination process may select for cellular subpopulations with altered characteristics.
Troubleshooting Guides
Implementing In Vivo Passaging for Mycoplasma Decontamination
Table 1: In Vivo Passaging Protocol for Mycoplasma Decontamination
| Step | Procedure | Key Considerations |
|---|---|---|
| 1. Cell Preparation | Harvest 2×10⁶ cells from mycoplasma-positive culture | Maintain cell viability through proper handling techniques |
| 2. Inoculation | Subcutaneously inject cells into JAX NOD.CB17-PrkdcSCID-J mice | Use immunocompromised mice to support xenograft establishment |
| 3. Tumor Monitoring | Allow tumors to grow to ~0.5 cm³ | Typically takes 2-4 weeks depending on cell line |
| 4. Harvest | Euthanize mice, excise tumor tissue | Follow institutional animal care guidelines |
| 5. Processing | Mechanically digest tumor, filter through 70μm mesh | Use gentleMACs Dissociator with appropriate program |
| 6. Re-establishment | Culture 1.25×10⁵ cells in Matrigel domes with appropriate media | Include authentication steps to confirm human origin |
This protocol successfully eliminated mycoplasma contamination from 100% of tested colorectal cancer patient-derived organoids (n=9) while preserving their phenotypic and genotypic characteristics [42]. Following re-establishment, researchers should verify the absence of mycoplasma using PCR-based detection methods before returning decontaminated lines to general culture circulation.
Implementing Hydrogen Peroxide Treatment for Mycoplasma Biofilms
Table 2: Non-Antibiotic Anti-Mycoplasma Agents
| Agent | Mechanism of Action | Effective Concentration | Application Notes |
|---|---|---|---|
| Hydrogen Peroxide | Oxidative damage to bacterial components | Varies by mycoplasma species and culture conditions | Biofilm towers show no enhanced defense against H₂O₂ [41] |
| Filtration (0.1μm) | Physical removal of mycoplasma from liquids | N/A | Effective for media, serum, and reagent sterilization [2] |
| Antibiotic Combinations | Multiple simultaneous targets | Below individual MICs when used synergistically | Moxifloxacin + doxycycline shows synergistic effects [41] [43] |
Hydrogen peroxide treatment capitalizes on the fact that mycoplasma biofilm development is associated with attenuated production of this native virulence factor [41]. This creates a vulnerability that researchers can exploit therapeutically. Treatment protocols should be empirically optimized for specific cell lines, as sensitivity to oxidative stress varies considerably between different mammalian cell types.
Detection and Verification Methods
Accurate detection is essential for both diagnosing contamination and confirming successful eradication. Researchers should employ multiple complementary methods:
- PCR-based Detection: The Sigma LookOut Mycoplasma PCR Detection Kit identifies 19 mycoplasma species, including the seven species that account for 95% of contamination events [42]. This method offers high sensitivity and specificity.
- Fluorescent Staining: Using DNA-binding dyes like Hoechst 33258 allows visual identification of mycoplasma contamination through filamentous cytoplasmic staining patterns [1].
- Microbiological Assays: Culture methods, while time-consuming (4-5 weeks), provide definitive confirmation through observation of characteristic "fried egg" colonies [1].
Regular monitoring using these techniques enables early detection and intervention before widespread contamination occurs.
Experimental Protocols
Detailed Methodology: In Vivo Passaging for Mycoplasma Decontamination
Materials Required:
- Mycoplasma-contaminated cells (2×10⁶ cells minimum)
- JAX NOD.CB17-PrkdcSCID-J mice (or similar immunocompromised model)
- gentleMACS Dissociator with appropriate tubes (Miltenyi Biotec)
- 70μm cell strainers
- Matrigel (Corning) or similar extracellular matrix
- Cell culture media optimized for specific cell type
- Mycoplasma detection kit (e.g., Sigma LookOut Mycoplasma PCR Detection Kit)
Procedure:
- Cell Preparation: Harvest mycoplasma-positive cells using standard dissociation techniques appropriate for the cell type. Count and resuspend in appropriate buffer to achieve concentration for injection.
Xenograft Establishment: Subcutaneously inject 2×10⁶ cells in a volume of 100-200μL into the flank of each mouse. Monitor animals regularly for tumor formation.
Tumor Monitoring: Palpate injection sites regularly until tumors reach approximately 0.5cm³ volume. This typically requires 2-8 weeks depending on the cell line's tumorigenicity.
Harvest: Euthanize mice according to approved animal protocols. Excise tumors aseptically and place in sterile DMEM or PBS on ice.
Processing: Transfer tumor tissue to C-tubes with 10mL DMEM. Process using gentleMACS Dissociator with the mimpTumor01.01 program run twice. Filter resulting suspension through 70μm filters and centrifuge at 500 × g for 5 minutes.
Re-establishment: Resuspend cell pellet and plate 1.25×10⁵ cells in 50μL domes composed of 30% cell suspension in media and 70% Matrigel. Maintain in optimized culture media.
Validation: After organoids establish (typically 1-3 weeks), test for mycoplasma using PCR detection. Authenticate cells to confirm human origin and appropriate characteristics [42].
Workflow Visualization: In Vivo Passaging Method
Workflow Visualization: Antibiotic Synergy Against Biofilms
Research Reagent Solutions
Table 3: Essential Reagents for Advanced Mycoplasma Management
| Reagent/Category | Specific Examples | Function/Application | Notes |
|---|---|---|---|
| Mycoplasma Detection Kits | Sigma LookOut Mycoplasma PCR Detection Kit | Identifies 19 mycoplasma species | Includes species accounting for 95% of contaminations [42] |
| Specialized Media | SP-4 Broth | Mycoplasma culture medium | Supports fastidious growth requirements [41] |
| Dissociation Reagents | gentleMACS Dissociator | Tissue processing for xenografts | Mechanical dissociation preserves cell viability [42] |
| Extracellular Matrix | Matrigel (Corning) | 3D support for re-established organoids | Essential for patient-derived organoid culture [42] |
| Antibiotic Alternatives | Hydrogen Peroxide | Oxidative eradication of mycoplasma | Effective against biofilm-protected mycoplasma [41] |
| Validated Cell Culture Media | DMEM/F12 with specialized supplements | Patient-derived organoid maintenance | Recipe includes B27, Noggin, R-Spondin 1 [42] |
Mycoplasma contamination presents a persistent challenge in cell culture laboratories, but the methods outlined in this technical guide provide robust solutions when conventional antibiotics fail. The in vivo passaging technique offers a reliable approach for eliminating mycoplasma from precious cell lines, particularly patient-derived organoids, with demonstrated 100% efficacy in validated studies [42]. Meanwhile, non-antibiotic strategies including hydrogen peroxide treatment and synergistic antibiotic combinations target mycoplasma through mechanisms that bypass common resistance pathways [41] [43]. Implementation of these advanced techniques, combined with rigorous detection methods and preventive measures, enables researchers to safeguard their cellular models and maintain the integrity of their experimental systems against this pervasive contaminant.
Mycoplasma contamination represents one of the most significant and persistent challenges in cell culture laboratories, affecting an estimated 15-35% of continuous cell lines worldwide [1] [9]. These minute bacteria lack cell walls, making them resistant to common antibiotics like penicillin and streptomycin, and their small size (0.1-0.3 μm) allows them to pass through standard sterilization filters [25] [10]. The development of a robust decontamination protocol is therefore essential for rescuing valuable, irreplaceable cell lines and maintaining research integrity, particularly in pharmaceutical development where contamination can compromise product quality and regulatory approval [26].
Quantitative Comparison of Mycoplasma Elimination Methods
The following table summarizes the key characteristics of major antibiotic-based elimination methods, providing a basis for protocol selection.
| Method/Reagent | Key Components | Treatment Duration | Reported Efficacy | Key Considerations |
|---|---|---|---|---|
| Mynox [26] | Surfactin (lipopeptide) | ~6 days (one passage) | High | Biophysical mechanism; no antibiotics; can affect some eukaryotic cells. |
| Mynox Gold [26] | Surfactin + Ciprofloxacin | 4 passages | >90% | For sensitive/primary cells; combination reduces resistance risk. |
| Plasmocin [20] | Proprietary antibiotic mixture | 14 days (typical) | 84% (78% in first attempt) | Simple, practical approach; some strains may require a second round. |
| Myco-4 [44] | Biological agent + Antibiotics | Multi-step process | High | Broad spectrum; low cytotoxicity; low resistance risk. |
| General Antibiotics [25] | e.g., Ciprofloxacin, Doxycycline | Multiple passages | Variable | Prolonged use may trigger resistance or toxicity. |
Detailed Experimental Protocols for Decontamination
Protocol 1: Two-Phase Antibiotic Treatment (e.g., Plasmocin, Myco-4)
This methodology is recommended for permanent cell lines and represents a common approach for several commercial reagents.
- Principle: Combines an initial aggressive phase to reduce mycoplasma load with a sustained maintenance phase to eliminate residual contaminants [20] [44].
- Procedure:
- Preparation: Initiate treatment when cultures are at high cell density (90-100% confluent). Use fresh growth medium supplemented with 5-10% higher concentration of Fetal Bovine Serum (FBS) to help cells withstand potential antibiotic toxicity [20].
- Starter/Treatment Phase: Replace spent medium with fresh medium containing the designated "Starter" or treatment concentration of the antibiotic. For example, with Myco-4, use the "Starter Treatment" vial [44]. Incubate for the specified period, typically 24-48 hours.
- Maintenance Phase: After the initial phase, replace the medium with fresh medium containing the recommended "Maintenance" concentration of the antibiotic. The maintenance phase typically lasts 10-14 days, with medium changes every 2-3 days to replenish the antibiotic [20].
- Recovery: Following the maintenance phase, passage the cells at least 2-3 times in antibiotic-free medium to allow recovery.
- Key Technical Considerations:
Protocol 2: Surfactin-Based Biophysical Treatment (e.g., Mynox)
This protocol is suitable for robust cell lines where avoiding traditional antibiotics is a priority.
- Principle: Uses surfactin, a cyclic lipopeptide, to selectively integrate into and disrupt the mycoplasma membrane, causing osmotic influx and disintegration [26].
- Procedure:
- Application: Add Mynox reagent directly to the culture medium of contaminated cells.
- Incubation: Incubate for the recommended period, which is approximately 6 days (equivalent to one cell culture passage or medium change) [26].
- Mechanism and Outcome: The treatment selectively eliminates contaminated cells. The culture is restarted from the surviving healthy cells, which resume normal morphology and proliferation rates [26].
Decision Workflow for Mycoplasma Decontamination
The following diagram illustrates the logical decision-making process for selecting and implementing a decontamination strategy.
The Scientist's Toolkit: Key Reagent Solutions
The table below details essential reagents used in the fight against mycoplasma contamination.
| Reagent / Kit | Primary Function | Specific Application Notes |
|---|---|---|
| Mynox [26] | Mycoplasma elimination via membrane disruption | Antibiotic-free; uses surfactin; can affect some eukaryotic cells. |
| Mynox Gold [26] | Mycoplasma elimination for sensitive cells | Combination of surfactin and ciprofloxacin; reduces resistance risk. |
| Plasmocin [20] | Antibiotic-based mycoplasma eradication | Proprietary antibiotic mixture; treatment typically over 14 days. |
| Myco-4 [44] | Multi-step mycoplasma elimination | Combination of a biological agent and antibiotics; broad spectrum. |
| PCR Mycoplasma Test Kit [44] | Detection of mycoplasma contamination | Rapid, sensitive method; detects cultivable and non-cultivable species. |
| DAPI Stain [44] | DNA fluorochrome staining for detection | Indirect detection method; requires fluorescence microscopy. |
Troubleshooting Guide & FAQs
FAQ 1: The contamination recurred after a seemingly successful treatment. What went wrong?
- Potential Cause: The most likely cause is the development of antibiotic resistance or an insufficient treatment duration that failed to eradicate all mycoplasma particles [20] [44].
- Solution:
- Re-test: Confirm the recurrence with a validated detection method (e.g., PCR) [20].
- Switch Reagents: Use a different elimination reagent with a distinct mode of action. For example, if a quinolone-based product (e.g., ciprofloxacin) failed, switch to a product with a biophysical mechanism (e.g., Mynox) or a combination therapy (e.g., Mynox Gold) [26] [44].
- Extend Treatment: If using the same reagent is necessary, consider a second, longer treatment cycle, ensuring high cell density and serum concentration to mitigate cytotoxicity [20].
FAQ 2: My cells are showing signs of stress or death during the antibiotic treatment. How should I proceed?
- Potential Cause: Cytotoxicity from the elimination reagent is a common risk, particularly for sensitive or primary cells [26] [20].
- Solution:
- Optimize Conditions: As outlined in experimental protocols, maintain cells at high density and increase the FBS concentration in the medium by 5-10% to support cell health [20].
- Adjust Dosage: For non-commercial antibiotic mixtures, verify the concentration. When using commercial kits, ensure you are following the manufacturer's dilution instructions precisely.
- Use Gentler Reagents: For subsequent attempts, select reagents specifically formulated for sensitive cells, such as Mynox Gold, which is designed for primary and stem cells [26].
FAQ 3: How do I validate that the decontamination protocol was successful?
- Procedure: Successful eradication must be confirmed experimentally post-treatment.
- Passage Cells: Passage the treated cells at least 2-3 times in antibiotic-free medium [20]. This allows any residual mycoplasma, previously suppressed but not killed, to proliferate to detectable levels.
- Perform Detection Assay: After the passages, use a highly sensitive detection method. PCR-based testing is recommended for its sensitivity and speed, allowing detection of both cultivable and non-cultivable species [25] [44].
- Timing: Test for mycoplasma at least 14 days after the conclusion of treatment to ensure the contamination has been permanently resolved and is not merely below the detection limit [20].
Experimental Validation Workflow Post-Treatment
The diagram below outlines the critical steps for validating successful mycoplasma eradication after any decontamination protocol.
A robust mycoplasma decontamination protocol is a critical component of modern cell culture management. The success of such protocols hinges on the careful selection of elimination reagents based on cell line sensitivity, strict adherence to treatment cycles and durations, and rigorous post-treatment validation. By integrating the quantitative data, detailed methodologies, and troubleshooting guidance outlined in this document, researchers and drug development professionals can effectively rescue valuable cell lines, safeguard experimental integrity, and ensure compliance with manufacturing standards.
Advanced Problem-Solving: Managing Resistant Contamination and Sensitive Cell Lines
FAQs: Understanding and Managing Resistant Mycoplasma
Q1: What are the primary mechanisms of antibiotic resistance in Mycoplasma?
Mycoplasma species develop resistance primarily through point mutations in their genomic DNA. For macrolide antibiotics (e.g., azithromycin), mutations in the V region of the 23S rRNA gene (specifically at positions A2063G and A2064G) are the most common mechanism. These mutations alter the drug's binding site on the bacterial ribosome, reducing treatment efficacy [45] [46]. For fluoroquinolones (e.g., moxifloxacin), resistance is often linked to mutations in the quinolone resistance-determining regions (QRDRs) of the parC (encoding topoisomerase IV) and gyrA (encoding DNA gyrase) genes [47].
Q2: Why are mycoplasma infections in cell culture particularly difficult to treat? Mycoplasma contamination is challenging in cell culture due to several factors: the bacteria lack a cell wall, rendering common antibiotics like penicillins and cephalosporins ineffective; they are visually undetectable by light microscopy; and they can profoundly alter host cell physiology and experimental data, often without causing turbidity in the culture medium [13] [9]. Their small, pliable size allows them to potentially pass through standard 0.2µm sterilization filters [9].
Q3: What is resistance-guided therapy and when should it be used? Resistance-guided therapy is a two-stage treatment approach. The initial phase uses a non-macrolide antibiotic (like doxycycline) to reduce bacterial load, followed by a second antibiotic selected based on the results of macrolide resistance testing. This strategy is recommended for managing Mycoplasma genitalium infections and has demonstrated cure rates of >90% [48]. It should be employed whenever macrolide resistance testing is available, especially in regions with high resistance rates.
Q4: What are the consequences of mycoplasma contamination in a research setting? Mycoplasma contamination can extensively affect cell physiology and metabolism, leading to unreliable and irreproducible experimental results [13] [9]. Consequences include altered cell growth and morphology, changes in gene expression profiles, interference with metabolic assays, and contamination of biological products, ultimately jeopardizing research integrity and causing significant losses of time and resources [9].
Q5: My cells are contaminated with mycoplasma. What is the first step I should take? The immediate first step is to quarantine the contaminated culture. Move the infected flasks or plates to a separate, designated incubator to prevent the spread to other cell lines [13]. Following quarantine, you can begin to assess your options for treatment or disposal.
Troubleshooting Guides
Guide 1: Diagnosing Persistent Infection After Antibiotic Treatment
Problem: A test of cure (TOC) returns positive after a completed course of antibiotics.
Investigation & Solutions:
- Confirm Treatment Failure:
- Action: Ensure the TOC was performed at the recommended time (e.g., 21 days after treatment completion for M. genitalium to avoid false negatives from residual DNA) [48].
- Action: Re-test to confirm the positive result.
Investigate Resistance:
Escalate Treatment:
- Action: If macrolide resistance is confirmed or suspected, the recommended regimen is doxycycline (100 mg orally twice daily for 7 days) followed by moxifloxacin (400 mg orally once daily for 7 days) [48].
- Action: For cell culture, if initial treatment with an antibiotic like Plasmocin fails, consider a longer treatment course or a switch to a different, validated antibiotic after consulting the literature on mycoplasma eradication [13].
Guide 2: Handling Multidrug-Resistant (MDR) Mycoplasma Strains
Problem: Infection persists despite treatment with both macrolides and fluoroquinolones.
Investigation & Solutions:
- Confirm Dual-Class Resistance:
- Consider Alternative Agents:
- Action (Clinical): Explore newer or less commonly used antibiotics. Pristinamycin has been used effectively in some settings for MDR M. genitalium, and drugs like sitafloxacin and solithromycin are under investigation [49] [47].
- Action (Research): For irreplaceable cell lines, consider extended treatment with a combination of antibiotics, though this carries risks and should be followed by rigorous testing. The most reliable method to eliminate MDR contamination and protect other cultures is often to discard the contaminated cells and restart from a clean, frozen stock [13] [9].
Guide 3: Preventing the Spread of Resistant Mycoplasma in the Laboratory
Problem: Contamination or resistant infections are recurring.
Investigation & Solutions:
- Audit Aseptic Technique:
- Action: Reinforce strict aseptic technique. Ensure proper use of personal protective equipment (PPE), limit clutter in the biosafety cabinet, and thoroughly disinfect all items with 70% ethanol before introducing them into the hood [13].
Review Source and Quarantine Procedures:
Implement a Routine Testing Schedule:
- Action: Establish a schedule for periodic mycoplasma testing for all cell lines in culture. A best practice is to test cells each time a new bank is frozen down [13].
Quantitative Data on Resistance Patterns
Table 1: Documented Macrolide and Fluoroquinolone Resistance Rates
Table summarizing resistance rates from recent studies across different regions and Mycoplasma species.
| Mycoplasma Species / Location | Sample Size | Macrolide Resistance Rate | Fluoroquinolone Resistance Rate | Key Mutation(s) | Citation |
|---|---|---|---|---|---|
| M. genitalium (Northwest England) | 759 patients | 55.5% (418/753 tested samples) | 20.6% (7/34 tested samples) | Not Specified | [50] |
| M. pneumoniae (Southern Italy, Post-Pandemic) | 305 positive cases | 7.5% (Overall); 12.6% (Age 10-14) | Not Reported | A2063G (96% of resistant cases) | [45] |
| M. genitalium (Tokyo, Japan) | 188 samples | 94.4% | 65.5% (parC S83I); 22.5% (gyrA) |
A2058G/A2059G (23S rRNA); parC S83I |
[47] |
Table 2: Impact of 23S rRNA Mutation Burden on Clinical Outcomes
Meta-analysis data on the differential effects of single versus double mutations in M. pneumoniae [46].
| Outcome Measure | Wild-Type Strain | Single Mutation (A2063G) | Double Mutation (A2063G + A2064G) |
|---|---|---|---|
| Fever Duration (Hazard Ratio, HR) | Reference | HR = 3.66 (95% CI: 1.89–7.09) | HR = 5.32 (95% CI: 4.27–6.61) |
| Risk of Severe Illness (HR) | Reference | HR = 5.89 (95% CI: 2.03–17.08) | HR = 7.80 (95% CI: 2.51–24.18) |
| Hospital Stay (Mean Difference) | Reference | MD = -3.33 days (longer) | MD = -3.33 days (longer) |
Experimental Protocols
Protocol 1: Detection of Macrolide Resistance Mutations via PCR and Sequencing
Principle: This protocol amplifies the domain V region of the Mycoplasma 23S rRNA gene, followed by Sanger sequencing to identify point mutations (A2063G, A2064G) associated with macrolide resistance [45] [46].
Methodology:
- DNA Extraction: Extract nucleic acids from clinical samples (e.g., respiratory specimens, urethral swabs) or cell culture supernatant using a commercial kit.
- PCR Amplification:
- Primers: Use primers targeting the domain V region of the 23S rRNA gene.
- Reaction Mix: KOD One PCR Master Mix, forward and reverse primers, nuclease-free water, and template DNA.
- Cycling Conditions:
- Initial Denaturation: 94°C for 2 minutes
- 35 Cycles: Denaturation at 98°C for 10 seconds, Annealing at 60°C for 5 seconds, Extension at 68°C for 5 seconds.
- Final Extension: 68°C for 1 minute.
- Gel Electrophoresis: Analyze PCR products by 1% agarose gel electrophoresis to confirm successful amplification.
- PCR Product Purification: Purify amplicons using an ExoSAP-IT or QIAquick PCR Purification Kit.
- Sanger Sequencing: Perform direct Sanger sequencing of the purified amplicons.
- Sequence Analysis: Align obtained sequences with a reference strain (e.g., M. pneumoniae or M. genitalium G37) using software like BioEdit or MEGA to identify mutations at positions A2063 and A2064 [45].
Protocol 2: Eradication of Mycoplasma from Cell Culture
Principle: Infected cells are treated with a proven anti-mycoplasma antibiotic for a sustained period, followed by a washout period and rigorous testing to confirm eradication [13].
Methodology:
- Quarantine: Immediately move contaminated cultures to a designated quarantine incubator.
- Antibiotic Treatment:
- Reagent: Add an antibiotic like Plasmocin to the culture media at a concentration of 25 µg/mL.
- Duration: Maintain the cells in the antibiotic-containing media for a continuous period of 14 days, with regular passaging as needed.
- Antibiotic Washout: After the treatment period, culture the cells in standard antibiotic-free media for 1-2 weeks.
- Test of Cure (TOC):
- Timing: Perform mycoplasma testing at the end of the washout period.
- Method: Use a highly sensitive method such as PCR or a commercial mycoplasma detection kit.
- Validation: If the TOC is negative, confirm the cells are mycoplasma-free over at least two additional passages before considering them cured. If positive, consider a second, longer treatment cycle or disposal of the culture [13].
Visualization: Resistance Testing and Management Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Mycoplasma Management
| Reagent / Kit | Function / Application | Brief Description |
|---|---|---|
| Plasmocin | Treatment of cell culture contamination | A commonly used antibiotic formulation specifically designed to eradicate mycoplasma from contaminated cell lines without immediate cytotoxicity at the recommended concentration [13]. |
| Nucleic Acid Extraction Kit (e.g., QIAamp Viral RNA Mini Kit) | Sample Preparation for PCR | Used to isolate high-quality DNA from clinical samples (urine, swabs) or cell culture supernatant for subsequent molecular detection and resistance testing [47]. |
| PCR Master Mix (e.g., KOD One) | Amplification of target genes | A ready-to-use mix containing a thermostable DNA polymerase, dNTPs, and buffer, optimized for high-fidelity amplification of specific gene targets like 23S rRNA, parC, and gyrA [47]. |
| Mycoplasma Detection Kit (Commercial) | Routine screening of cell cultures | Provides all necessary components for a highly sensitive and specific test (often via PCR or enzymatic activity) to regularly monitor cell lines for mycoplasma contamination [13]. |
| Sanger Sequencing Services | Identification of resistance mutations | Used to determine the nucleotide sequence of PCR amplicons, allowing for the identification of specific point mutations conferring antibiotic resistance [45] [47]. |
FAQs: Mycoplasma Management in Sensitive Cultures
What makes mycoplasma particularly problematic for stem cell and primary cultures? Mycoplasma contamination is especially detrimental for sensitive cultures like stem cells and primary cells because it causes subtle but critical alterations in cell physiology without immediate cell death. These contaminants consume essential nutrients from the culture medium, compete with your cells for resources, and can induce chromosomal abnormalities, alter metabolic pathways, and change cell membrane antigenicity [51] [25]. Unlike bacterial contamination that often causes obvious turbidity, mycoplasma can reach concentrations of 10⁸ organisms per milliliter without visible changes, making them silent disruptors of your experimental data [51].
Why do traditional antibiotic approaches often fail or cause cytotoxicity in sensitive cultures? Many common antibiotics target cell wall synthesis, but mycoplasma lack a cell wall, rendering antibiotics like penicillin ineffective [51] [28]. While some antibiotics can be effective, prolonged use often leads to antibiotic-resistant strains or introduces cytotoxic effects that disproportionately affect sensitive stem cell and primary cultures [51] [52]. Furthermore, studies have shown that antibiotics can alter gene expression in cultured cells, potentially compromising your experimental outcomes [51].
What is the most reliable method to detect mycoplasma in valuable cultures? For definitive detection, a multimodal approach is recommended. The table below compares the most common detection methods:
Table: Comparison of Mycoplasma Detection Methods
| Method | Time Required | Key Advantage | Key Limitation | Best for Sensitive Cultures? |
|---|---|---|---|---|
| Culture Method [28] [25] | Up to 4 weeks | Considered a gold standard; high reliability [25] | Very time-consuming; requires specialized media [28] | No, due to slow results |
| DNA Fluorochrome Staining (e.g., Hoechst) [28] [25] | 1-2 days | Rapid; can be visualized with fluorescence microscope | Can yield false positives from host cell DNA fragments [12] [53] | Yes, when combined with membrane stain [12] |
| PCR-based Methods [28] [25] | 2.5 to 5 hours [28] | Extremely fast and highly sensitive [25] | Risk of false positives from non-viable cells [28] | Yes, for rapid screening |
| Colocalization (New Method) [12] [53] | ~1 day | Minimizes interference from cytoplasmic DNA; highly accurate [12] | Requires specific staining and analysis workflow | Yes, excellent for accuracy |
A novel method combining DNA staining (e.g., Hoechst) with a cell membrane fluorescent dye has been developed to quickly and directly screen for mycoplasma. This colocalization approach accurately assesses contamination by determining if the DNA signal is located on the plasma membrane surface, effectively minimizing false positives from degraded host cell DNA [12] [53].
If I discover contamination, should I attempt to salvage my sensitive stem cell culture? The decision to salvage or discard contaminated cultures depends on the cell's value and replacement cost. For irreplaceable seed stocks, treatment is necessary. However, for cultures used in ongoing experiments, starting a new culture from a clean, frozen stock is often safer and more time-efficient. Continuing experiments with contaminated cells generally produces unreliable results and risks cross-contaminating other cultures in your lab [52].
Troubleshooting Guide: Decontamination and Prevention
Problem 1: Recurring Mycoplasma Contamination After Treatment
Possible Causes and Solutions:
- Source not identified: The original source of contamination (e.g., lab personnel, contaminated reagents, new cell lines) has not been eliminated [51] [13].
- Solution: Implement strict testing protocols for all new cell lines and reagents. Quarantine new cultures until tested negative [13].
- Incomplete eradication: The treatment did not fully eliminate all mycoplasma, leading to regrowth.
- Solution: After any antibiotic treatment, culture cells for 1-2 weeks without antibiotics and then re-test to confirm successful clearance [13].
- Cross-contamination: Contamination is spreading from infected cultures or equipment.
Problem 2: High Cytotoxicity Observed During Decontamination
Possible Causes and Solutions:
- Antibiotic toxicity: The concentration or type of antibiotic is toxic to your sensitive cells.
- Solution: Titrate the antibiotic to find the lowest effective dose. Consider using combination reagents specifically designed to be less toxic to host cells, such as Procellaria Anti-Mycoplasma Treatment Reagent [25].
- Prolonged treatment: Excessively long treatment times increase stress on host cells.
- Solution: Follow treatment durations precisely. For heat treatment, do not exceed 41°C for more than 18 hours, as this can severely stress or kill many primary cells [25].
- Cell stress: The contaminated cells are already weakened.
- Solution: Ensure optimal culture conditions during treatment. If cytotoxicity remains high, preserving the cells by freezing and then treating the recovered culture after thawing may be an option.
Experimental Protocols for Detection and Decontamination
Protocol 1: Enhanced Mycoplasma Detection via DNA and Membrane Colocalization
This protocol mitigates the false positives common with Hoechst staining alone [12] [53].
Key Research Reagent Solutions:
- DNA Fluorescent Dye (e.g., Hoechst): Binds to DNA in both the host cell nucleus and mycoplasma [12] [53].
- Cell Membrane Fluorescent Dye (e.g., WGA): Labels the cell membrane, providing a spatial reference [12].
- Permeabilization Solution (0.2% Triton-X-100 in PBS): Permeabilizes cells for staining internal structures if required [54].
- Blocking Solution (5% normal goat serum and 5% BSA in PBS): Reduces non-specific antibody binding [54].
Methodology:
- Culture cells on sterile glass coverslips in a multi-well plate until they reach 50-70% confluency.
- Aspirate the medium and wash cells gently with pre-warmed PBS.
- Fix cells with an appropriate fixative (e.g., 4% formaldehyde in PBS) for 15 minutes at room temperature.
- (Optional) Permeabilize cells with 0.2% Triton-X-100 in PBS for 10 minutes [54].
- Incubate with the cell membrane dye (e.g., WGA conjugated to a red fluorophore) for 20-30 minutes, protected from light.
- Without washing, add the DNA stain (e.g., Hoechst) and incubate for an additional 10-15 minutes, protected from light.
- Wash coverslips thoroughly with PBS and mount on glass slides.
- Visualize using a fluorescence microscope with appropriate filter sets. Positive mycoplasma contamination is indicated by small, speckled blue (Hoechst) fluorescence that co-localizes with the red membrane stain at the cell surface, not inside the nucleus or cytoplasm [12] [53].
Protocol 2: Low-Cytotoxicity Antibiotic Treatment for Sensitive Cells
This protocol uses a phased antibiotic approach to minimize stress on valuable cultures.
Key Research Reagent Solutions:
- Plasmocin: A commonly used antibiotic effective against mycoplasma [13].
- Mycoplasma Elimination Reagent (e.g., Procellaria P-CMR-001): A combination reagent designed to be less toxic to host cells [25].
- Base Culture Medium: Your standard medium without antibiotics.
Methodology:
- Quarantine: Immediately move the contaminated culture to a dedicated incubator or separate workspace [13].
- Shock Treatment: a. Gently dissociate and pellet the cells. b. Resuspend the cell pellet in fresh medium containing a "shock" concentration of the selected antibiotic (e.g., Plasmocin at 25 µg/mL) [13] or the manufacturer's recommended dose of a dedicated elimination reagent [25]. c. Culture the cells for 1-2 weeks, passaging as needed but maintaining the antibiotic pressure.
- Antibiotic-Free Culture: a. After the treatment period, passage the cells into antibiotic-free medium. b. Culture for a further 1-2 weeks [13].
- Confirmation: a. Test the culture for mycoplasma using a reliable method (e.g., the colocalization method above or PCR) to confirm eradication. b. Only return the culture to your main stock after confirming it is mycoplasma-free.
The Scientist's Toolkit: Essential Reagents for Mycoplasma Management
Table: Key Reagents for Decontaminating Sensitive Cultures
| Reagent / Kit | Function | Application Notes |
|---|---|---|
| Plasmocin [13] | Antibiotic for mycoplasma eradication | Effective for shock treatment; use at 25 µg/mL for 1-2 weeks. |
| Anti-Mycoplasma Treatment Reagent (e.g., Pricella P-CMR-001) [25] | Combination reagent for elimination | Designed to be less toxic to host cells; follow manufacturer's instructions. |
| Hoechst 33258/33342 [12] [53] [55] | DNA-binding fluorescent dye | For staining nucleic acids in mycoplasma and host cells. |
| Wheat Germ Agglutinin (WGA) [12] | Cell membrane fluorescent stain | Used in colocalization to distinguish surface-bound mycoplasma. |
| Mycoplasma Detection PCR Kit [28] [25] | Molecular detection of mycoplasma DNA | Fast and sensitive; ideal for routine screening of valuable stocks. |
| Senescence β-galactosidase Staining Kit [54] | Detects cellular senescence | Monitor stress-induced senescence in cultures post-decontamination. |
Workflow Diagram for Mycoplasma Management
The following diagram illustrates the critical decision pathway for managing mycoplasma contamination in sensitive cultures, from detection to resolution.
Technical Support Center
Troubleshooting Guide: Mycoplasma Contamination
Q1: My entire cell culture inventory is potentially contaminated with mycoplasma. What are my immediate first steps?
A1: Implement immediate containment and assessment protocols:
- Quarantine Immediately: Move all potentially contaminated cultures to a designated, separate incubator to prevent cross-contamination to clean cultures [13] [10].
- Cease All Experiments: Discontinue any ongoing experiments using the affected cultures, as mycoplasma alters cell physiology and will compromise data integrity [26] [9].
- Assess the Scope: Test all cell lines in the laboratory to determine the full extent of the contamination. This includes lines that show no obvious signs of infection, as effects can be subtle [10].
Q2: How can I confirm a mycoplasma contamination?
A2: Detection is challenging as mycoplasma is invisible under standard light microscopy. You must use specific detection methods, summarized in the table below [25] [9] [10].
| Method | Principle | Duration | Key Advantage | Key Disadvantage |
|---|---|---|---|---|
| Microbiological Culture | Grows mycoplasma on agar plates [25]. | Up to 4 weeks [25]. | Considered the "gold standard" by regulatory bodies [10]. | Very time-consuming [25]. |
| DNA Fluorochrome Staining | Stains mycoplasma DNA for fluorescent detection [25] [9]. | A few hours [25]. | Relatively fast and simple [25]. | Results can be tricky to interpret [10]. |
| Polymerase Chain Reaction (PCR) | Amplifies specific mycoplasma DNA sequences [25]. | A few hours [25]. | Highly sensitive, rapid, and simple [25] [10]. | Does not distinguish between live and dead organisms [25]. |
Q3: What are the most effective methods to eliminate mycoplasma from a valuable, irreplaceable cell line?
A3: While discarding cultures is often safest, valuable lines can be treated with specific reagents. The choice depends on your cell type and tolerance.
| Method | Mode of Action | Treatment Duration | Key Considerations |
|---|---|---|---|
| Antibiotic Treatment (e.g., Plasmocin) | Targets protein/DNA synthesis in mycoplasma [13]. | 1-2 weeks [13]. | Common and relatively easy; risk of generating antibiotic-resistant strains with improper use [26] [10]. |
| Mynox | Uses surfactin to disrupt the mycoplasma membrane biophysically [26]. | ~6 days [26]. | Antibiotic-free; eliminates risk of resistance; can be harsh on some eukaryotic cells [26]. |
| Mynox Gold | Combines surfactin (membrane disruption) with ciprofloxacin (antibiotic) [26]. | 4 cell culture passages [26]. | Designed for sensitive/primary cells; combination therapy virtually eliminates resistance risk [26]. |
Critical Note: After any treatment, culture cells without antibiotics for 1-2 weeks and then re-test to confirm successful eradication [13].
Q4: How can I prevent future mycoplasma outbreaks in the lab?
A4: Prevention hinges on strict aseptic technique and rigorous lab management.
- Quarantine & Test New Cell Lines: Always quarantine and test new cell lines from external sources before introducing them to your main culture facility [13] [10].
- Maintain Aseptic Technique: Always wear proper PPE (lab coat, gloves). Work in an uncluttered hood, spray all items with 70% ethanol, and avoid movements that disrupt airflow [13].
- Avoid Routine Antibiotics: Using standard antibiotics like penicillin/streptomycin in culture media can mask bacterial contamination without affecting mycoplasma, leading to undetected outbreaks [10].
- Use Quality Reagents: Source sera, media, and reagents from trustworthy suppliers who test for mycoplasma [9] [10].
- Educate All Personnel: Proper training is critical, as laboratory personnel are a major source of mycoplasma contamination through aerosols generated by talking, coughing, or pipetting [9] [10].
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials used for the prevention, detection, and elimination of mycoplasma contamination.
| Reagent / Material | Function / Application |
|---|---|
| Mynox | A non-antibiotic reagent that eliminates mycoplasma by selectively disrupting its cell membrane via surfactin [26]. |
| Mynox Gold | A combination reagent (surfactin + ciprofloxacin) for eliminating mycoplasma from sensitive and primary cells, minimizing resistance risk [26]. |
| Plasmocin | A common antibiotic mixture used to treat mycoplasma-contaminated cells over a 1-2 week period [13]. |
| Mycoplasma Detection Kit (PCR-based) | Commercial kit for rapid, sensitive, and specific detection of mycoplasma DNA in cell culture samples [13] [25]. |
| DAPI / Hoechst Stains | DNA-binding fluorochromes used in DNA staining methods to visually detect mycoplasma DNA under a fluorescence microscope [25] [10]. |
Experimental Workflow for Contamination Crisis Management
The diagram below outlines the logical workflow for managing a widespread mycoplasma contamination crisis, from initial suspicion to process improvement.
Mycoplasma Testing Pathway
This flowchart illustrates the pathway for choosing the most appropriate mycoplasma detection method based on your lab's needs.
Optimizing Cell Culture Conditions to Support Recovery Post-Treatment
Troubleshooting Guides
Guide 1: Troubleshooting Post-Treatment Cell Recovery
Problem: Poor Cell Growth After Mycoplasma Elimination
- Potential Cause 1: Residual cytotoxicity from the elimination reagents.
- Solution: Ensure you perform the recommended number of post-treatment washes with fresh, pre-warmed culture medium. Gradually wean cells from the treatment reagents if the protocol allows. [26]
- Potential Cause 2: Persistent metabolic stress or underlying damage from the original contamination.
- Potential Cause 3: The cell line is sensitive, and the treatment was too harsh.
- Solution: For future treatments of the same cell line, consider a milder antibiotic or a physical removal method like Mynox, which works via a biophysical mechanism and is antibiotic-free. For primary or stem cells, Mynox Gold is specifically recommended. [26]
Problem: Recurrence of Mycoplasma Contamination After Treatment
- Potential Cause 1: Incomplete eradication, where the contamination falls below detection levels but is not fully eliminated.
- Solution: Extend the treatment duration and ensure the reagent concentration is sufficient. Always confirm eradication using a detection method different from your initial test after a treatment-free period. [10]
- Potential Cause 2: Re-introduction from a contaminated source or cross-contamination in the lab.
Guide 2: Troubleshooting Mycoplasma Detection Post-Treatment
Problem: Inconsistent or Unclear Detection Results After Treatment
- Potential Cause 1: Residual components from the treatment reagents (e.g., antibiotics) are interfering with the detection assay.
- Potential Cause 2: The detection method used lacks sensitivity or specificity.
- Solution: Use a highly sensitive and validated method. A PCR-based protocol, like the one described, can detect a broad spectrum of mycoplasma species with high sensitivity and can be used as a universal standard. [22]
Frequently Asked Questions (FAQs)
FAQ 1: Why are my cells not returning to their normal proliferation rate immediately after mycoplasma treatment? Mycoplasma contamination causes significant damage to host cells, including altered metabolism and gene expression. Even after successful eradication, cells require time to recover from this stress. During recovery, optimize culture conditions with high-quality media and closely monitor cell health. A gradual return to normal proliferation over several passages is common. [10] [26] [25]
FAQ 2: How long should I quarantine cell cultures after mycoplasma treatment? Treated cells should be kept in quarantine and regularly tested for mycoplasma until they have consistently tested negative through at least two full passages after the treatment protocol is complete. This ensures any low-level contamination is detected. [10]
FAQ 3: What is the most reliable way to confirm mycoplasma is gone after treatment? The most reliable confirmation is to obtain consistent negative results using a highly sensitive detection method, such as a validated PCR assay. It is recommended to use a different method for post-treatment confirmation than the one used for initial detection to avoid assay-specific interferences. Testing should be performed after the cells have been passaged in antibiotic-free medium. [10] [22] [25]
FAQ 4: Can I use standard antibiotics like Penicillin/Streptomycin to prevent mycoplasma regrowth after treatment? No. Mycoplasma lack a cell wall, making them naturally resistant to common antibiotics like penicillin and streptomycin. Using these will not prevent mycoplasma regrowth and may mask other bacterial contaminations. [10] [56]
Experimental Protocols for Detection and Removal
Protocol 1: Universal PCR-Based Mycoplasma Detection
This protocol is adapted from a study that designed a PCR method to establish a universal standard for routine testing. [22]
- Principle: Utilizes ultra-conserved primers targeting the 16S rRNA gene of mycoplasma, covering 92% of all species in the class Mollicutes. The protocol includes an internal control to confirm the presence of amplifiable eukaryotic DNA.
- Key Reagents:
- Primers: Specific primer pairs for mycoplasma DNA and a control primer pair for eukaryotic DNA (e.g., Uc48-primer).
- DNA Extraction Kit: For extracting DNA from cell culture supernatant and cell pellet.
- PCR Master Mix: Containing DNA polymerase, dNTPs, and buffer.
- Methodology:
- Harvest cell culture supernatant and a small portion of the cell pellet.
- Extract genomic DNA from the samples.
- Set up a four-primer PCR reaction containing both the mycoplasma-specific and eukaryotic control primers.
- Run the PCR with appropriate cycling conditions.
- Analyze the PCR products by gel electrophoresis. The presence of a 166–191 bp band indicates mycoplasma contamination. A 105 bp control band confirms a successful PCR reaction.
Protocol 2: Mycoplasma Elimination Using Antibiotic Treatment
- Principle: Application of antibiotics that target mycoplasma protein or DNA synthesis, such as macrolides, tetracyclines, or quinolones, to eradicate the contamination. [10] [25]
- Key Reagents:
- Methodology:
- Choose an appropriate antibiotic based on your cell line's sensitivity.
- Add the antibiotic to the culture medium at the recommended concentration.
- Treat the cells for the recommended duration, typically spanning several cell culture passages (e.g., 4-14 days). The exact length is critical for success. [10] [26]
- During treatment, maintain the cells in quarantine.
- After treatment, passage the cells in antibiotic-free medium and confirm eradication using a reliable detection method.
Workflow for Post-Treatment Recovery
The following diagram illustrates the critical steps for recovering cells after mycoplasma treatment, from initial treatment to the restoration of healthy cultures.
Data Presentation
Table 1: Comparison of Mycoplasma Elimination Methods
| Method | Mechanism of Action | Typical Success Rate | Key Advantages | Key Disadvantages/Cautions |
|---|---|---|---|---|
| Antibiotic Treatment [10] [25] | Inhibits protein or DNA synthesis | Varies; specific products claim >90% [26] | Widely available, relatively easy to use | Risk of generating antibiotic-resistant strains; can be toxic to sensitive cells [10] [56] |
| Mynox [26] | Biophysical; surfactin disrupts mycoplasma membrane | >90% [26] | Antibiotic-free, no resistance risk, fast (∼6 days) | Can affect some eukaryotic cells; goal is to rescue a subset of healthy cells [26] |
| Mynox Gold [26] | Combination of surfactin and ciprofloxacin | >90% [26] | Low resistance risk, recommended for sensitive/primary cells | Treatment requires 4 cell passages [26] |
| Photodynamic Therapy [57] | Light-activated photosensitizer generates reactive oxygen species | Effective in model systems [57] | Novel approach, avoids chemicals | Experimental; requires specialized equipment [57] |
Table 2: Quantitative Effects of Mycoplasma Contamination on Cell Cultures
| Parameter Affected | Documented Impact of Contamination |
|---|---|
| Mycoplasma Concentration [56] | Can reach 107 – 108 organisms/mL in culture |
| Global Contamination Rate [10] [26] [22] | Estimated to affect 15–35% of continuous cell lines |
| Cell Proliferation [10] [11] [25] | Reduced rate of growth and proliferation |
| Metabolic Processes [10] [25] | Drastic changes in cell metabolism and nutrient depletion |
| Genetic Integrity [10] [56] [25] | Can cause chromosomal aberrations and instability |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Mycoplasma Management
| Reagent Category | Example Products | Function & Application |
|---|---|---|
| Elimination Reagents | Mynox, Mynox Gold, B-M Cyclin, Ciprofloxacin, Pricella Anti-Mycoplasma Reagent [56] [26] [25] | Used to eradicate mycoplasma from contaminated cell cultures. Mechanisms range from antibiotic action to biophysical membrane disruption. |
| PCR Detection Kits | Various commercial and in-house PCR/qPCR kits [10] [22] [25] | Provide a rapid, sensitive, and specific method for detecting mycoplasma DNA in cell culture samples. |
| DNA Stains for Detection | Hoechst stain, DAPI [10] [22] | Fluorochromes that bind DNA, allowing visualization of mycoplasma on the host cell surface via fluorescence microscopy. |
| Microbiological Culture Media | PPLO broth, Mycoplasma agar plates [10] [22] | Used in the gold-standard culture method for growing and detecting viable mycoplasma, though it is time-consuming. |
| Photosensitizers (Experimental) | Methylene Blue [57] | Used in antimicrobial photodynamic therapy (aPDT) to generate reactive oxygen species that kill mycoplasma upon light activation. |
Mycoplasma contamination represents one of the most significant challenges in cell culture research, with studies indicating that 15-35% of cell lines worldwide are affected, with extreme incidences reaching 65-80% in some laboratories [9]. These minute bacteria lack a cell wall, making them resistant to many common antibiotics and allowing them to pass through standard 0.22 μm sterilization filters used in cell culture workflows [58] [9]. The insidious nature of mycoplasma contamination lies in its ability to persistently infect cultures without causing visible turbidity or cell death, while simultaneously altering cell proliferation, metabolism, and causing chromosomal aberrations that compromise research integrity [58]. This technical support guide provides comprehensive strategies for preventing, detecting, and managing mycoplasma contamination through proper isolation protocols, quarantine procedures, and laboratory workflow design.
FAQs: Understanding Mycoplasma Contamination
Q1: What makes mycoplasma contamination particularly problematic in cell culture research?
Mycoplasma contamination presents unique challenges due to several biological characteristics:
- Size and filtration resistance: Measuring only 0.3-0.8 μm in diameter, mycoplasmas can pass through filters designed to prevent bacterial and fungal contamination [58] [9].
- Antibiotic resistance: The absence of a cell wall makes mycoplasmas highly resistant to common antibiotics like penicillin and streptomycin that target cell wall synthesis [58] [13].
- Stealth characteristics: Contamination does not produce turbidity in culture media and is undetectable by visual inspection under a conventional microscope [58] [9].
- Profound research impact: Mycoplasma infection can dysregulate hundreds of host genes, alter cellular metabolism, affect chromatin accessibility in ATAC-seq studies, and compromise the interpretation of gene expression studies [58].
The primary sources of mycoplasma contamination have evolved over time, with current risks including:
Table: Common Sources of Mycoplasma Contamination
| Source Type | Specific Examples | Preventive Measures |
|---|---|---|
| Cross-contamination | Infected cell lines spreading to other cultures | Strict quarantine of new cell lines, dedicated equipment |
| Laboratory Personnel | M. orale, M. fermentans, M. hominis from oropharyngeal tract | Proper PPE, aseptic technique [9] |
| Reagents & Sera | Previously a major source from bovine serum | Use reputable suppliers, filtration testing [9] |
| Laboratory Environment | Contaminated equipment, surfaces, incubators | Regular cleaning, disinfection protocols [58] |
Historically, bovine serum was a significant contamination source, but today cross-contamination from infected cultures and laboratory personnel represent the most common routes of infection [9] [22]. Research demonstrates that a single infected culture can contaminate an entire laboratory workspace, with live mycoplasma recoverable from surfaces days after initial exposure [9].
Q3: How can laboratory design and workflow minimize cross-contamination risks?
Effective laboratory workflow design incorporates both spatial separation and procedural controls:
Figure 1: Laboratory workflow for new cell line integration
- Physical separation: Establish dedicated quarantine areas with separate incubators for new or untested cell lines, physically isolated from main culture areas [58] [13].
- Unidirectional workflow: Implement a clean-to-dirty workflow where personnel handle quarantined materials after working with established, clean cell lines.
- Containment equipment: Utilize Biological Safety Cabinets (BSCs) with proper airflow and regular maintenance to provide a sterile working environment [59].
- Access control: Limit access to critical culture areas and establish clear boundaries between clean and potentially contaminated spaces [59].
Troubleshooting Guides
Problem: Suspected Mycoplasma Contamination in Cell Cultures
Initial Assessment and Containment
- Immediate isolation: Immediately move suspected cultures to a designated quarantine area with separate equipment [60] [13].
- Cease all work: Stop all procedures involving potentially contaminated cultures to prevent further spread [60].
- Notify personnel: Alert all laboratory members to ensure coordinated response and prevent accidental use of contaminated materials [60].
- Environmental control: Increase cleaning frequency of shared equipment, incubators, and workspaces with appropriate disinfectants [58] [61].
Detection and Diagnosis
Multiple detection methods are available with varying sensitivity, specificity, and time requirements:
Table: Mycoplasma Detection Method Comparison
| Method | Principle | Time to Result | Sensitivity | Common Applications |
|---|---|---|---|---|
| PCR Assay | Amplification of mycoplasma-specific 16S rRNA regions | 3-4 hours [58] | High (92% species coverage) [22] | Routine screening, rapid detection |
| Microbiological Culture | Growth on specific mycoplasma broth/agar | 1-2 weeks [22] | Moderate (limited to cultivable strains) | Historical gold standard |
| DNA Staining | Hoechst staining of mycoplasma DNA | Several hours | Variable (subjective interpretation) [22] | Supplementary testing |
| ELISA | Detection of mycoplasma antigens | 1-2 days | Species-specific | Targeted detection |
The PCR method described in [22] provides excellent coverage, detecting 92% of all Mycoplasmatota species with primers targeting ultra-conserved 16S rRNA regions. For most laboratories, PCR represents the optimal balance of speed, sensitivity, and specificity for routine screening.
Eradication Protocols
For valuable, irreplaceable cell lines, eradication may be attempted:
- Antibiotic treatment: Use specific anti-mycoplasma antibiotics like Plasmocin at 25 μg/mL for 1-2 weeks [13].
- Post-treatment validation: Culture cells without antibiotics for 1-2 weeks after treatment completion, then retest for mycoplasma [13].
- Cryopreservation: Create new frozen stocks from successfully treated cultures after confirming eradication.
- Last resort: If contamination persists after multiple treatment cycles, discard the cultures to protect other cell lines [13].
Problem: Establishing Effective Prevention Protocols
Laboratory Workflow Design Principles
Figure 2: Personnel workflow through containment zones
- Zonal segregation: Designate separate areas for clean cell culture work, quarantine of new lines, and processing of potentially contaminated materials [59].
- Equipment dedication: Assign specific equipment (pipettes, centrifuges, media) to quarantine areas to prevent cross-contamination [61].
- HVAC considerations: Implement proper air handling systems with HEPA filtration for laboratory exhaust air, particularly important at BSL-3 and BSL-4 containment levels [59].
- Traffic control: Establish single-direction workflow patterns from clean to potentially contaminated areas [59].
Administrative Controls
- Training programs: Implement comprehensive training on aseptic techniques, contamination recognition, and emergency response protocols [61] [59].
- Documentation systems: Maintain detailed records of cell line sources, testing history, and any contamination events.
- Regular monitoring: Establish a scheduled testing protocol for all cell lines, recommending testing every 1-2 months for active cultures and all new frozen stocks [13].
- Crisis response plan: Develop clear procedures for contamination events, including identification, containment, communication, and decontamination [60].
Research Reagent Solutions
Table: Essential Reagents for Mycoplasma Prevention and Detection
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| PCR Detection Kits | MycoStrip [58] | Rapid, specific detection of mycoplasma contamination |
| Culture Media | DMEM, RPMI 1640, α-MEM [58] | Cell line maintenance with appropriate supplements |
| Antibiotic Treatments | Plasmocin [13] | Eradication of established mycoplasma infections |
| Disinfectants | 70% ethanol, bleach solutions [58] [13] | Surface decontamination and spill management |
| Personal Protective Equipment | Lab coats, gloves, face protection [58] [59] | Creating barrier between personnel and cultures |
| Supplemental Reagents | Heat-inactivated FBS, GlutaMAX [58] | Supporting optimal cell growth and function |
Effective prevention of mycoplasma contamination requires a multifaceted approach integrating rigorous laboratory design, consistent procedural adherence, and regular monitoring. By implementing strategic workflow segregation, maintaining strict quarantine protocols for new cell lines, and establishing comprehensive detection methodologies, research facilities can significantly reduce their contamination risk. The most critical factor for success remains a culture of contamination awareness where all personnel recognize their role in maintaining cell culture integrity. Through these coordinated efforts, laboratories can protect their research investments and ensure the reliability of their scientific data in the ongoing challenge against mycoplasma contamination.
Ensuring Success: Validating Eradication and Comparing Removal Technologies
Frequently Asked Questions (FAQs)
Q1: What does "post-eradication validation" mean, and why is it a critical phase? Post-eradication validation is the process of confirming that mycoplasma contamination has been completely eliminated from a cell culture following a treatment regimen. This phase is critical because mycoplasma contamination can persist at low, undetectable levels and lead to a resurgence if the validation is not thorough. Incomplete eradication can compromise experimental results, leading to erroneous data concerning cell physiology, metabolism, and gene expression [62] [9] [1]. A rigorous validation schedule ensures the reliability of your research and the integrity of your cell lines.
Q2: My cells have been treated with an antibiotic like Plasmocin. How soon should I begin validation testing? You should begin the validation process immediately after completing the antibiotic treatment course. The essential first step is to culture the treated cells for a period of one to two weeks without any antibiotics in the medium [13]. This antibiotic-free period is crucial to allow any potential surviving mycoplasma to proliferate to detectable levels, preventing false-negative results from carryover antibiotics that might suppress but not eliminate the contamination.
Q3: What is the recommended schedule for post-eradication monitoring? A multi-stage testing schedule is recommended to ensure long-term eradication. The following table summarizes a standard validation timeline:
| Time Point After Treatment | Action Required |
|---|---|
| Immediately after | Culture cells in antibiotic-free medium for 1-2 weeks [13]. |
| At the end of 2 weeks | Perform the first definitive mycoplasma test. |
| If positive | Initiate a second, potentially longer, treatment cycle [13]. |
| If negative | Continue to monitor cells and re-test periodically. |
| Every month | Perform periodic re-testing for at least 3 months to ensure contamination does not re-emerge [63]. |
Q4: What are the most reliable methods for testing after eradication? A combination of methods is often used for robust validation. The choice depends on factors like sensitivity, speed, and available lab equipment.
| Method | Principle | Key Advantage | Key Disadvantage | Time to Result |
|---|---|---|---|---|
| PCR-Based Assays [1] [28] | Detects mycoplasma-specific DNA sequences (e.g., 16S rRNA). | High sensitivity, rapid, can detect multiple species. | May detect DNA from non-viable cells. | 2.5 hours to 5 hours [28] |
| Direct Culture [1] [28] | Grows mycoplasma on specialized agar to form "fried-egg" colonies. | Considered a gold standard; high specificity. | Very slow, requires specialized media and expertise. | Up to 4-5 weeks [1] [28] |
| Indirect DNA Staining (Hoechst) [1] [12] | Fluorescent dye binds to DNA, revealing mycoplasma on cell surfaces. | Faster than direct culture. | Requires expertise to interpret; can have false positives from cell debris [12]. | 1-2 days |
Q5: What should I do if my first post-treatment test comes back positive? A positive test result after treatment indicates that the eradication was not fully successful. Your options are:
- Re-treat with Antibiotics: Subject the cells to a second, potentially longer, course of a mycoplasma-removal antibiotic (e.g., Plasmocin for 1-2 weeks) [13]. Some persistent contaminations may require switching to a different class of antibiotic.
- Discard the Culture: This is often the safest and most recommended course of action, especially for non-critical or replaceable cell lines. This prevents the risk of the contamination spreading to other cultures in your lab, which can happen easily during routine handling [9] [64].
Troubleshooting Guide
| Problem | Possible Cause | Solution |
|---|---|---|
| Inconsistent test results after treatment. | 1. Antibiotic carryover causing false negatives. 2. Low-level contamination not detected by a single test. | 1. Ensure a full 1-2 week culture in antibiotic-free media before testing [13]. 2. Use a combination of two different testing methods (e.g., PCR and DNA staining) for confirmation [64]. |
| Contamination re-emerges months after a "clean" test. | Inadequate long-term monitoring; cross-contamination from another source in the lab. | 1. Implement the recommended long-term monthly testing schedule for at least 3 months [63]. 2. Review aseptic techniques and decontaminate incubators and workstations. Quarantine all new cell lines [13] [9]. |
| Difficulty interpreting Hoechst stain results. | Fluorescence from apoptotic bodies or cellular debris can be mistaken for mycoplasma [12]. | Use a confirmatory method like PCR. A newer method using a combination of DNA stain and a cell membrane dye can help colocalize signals to the cell surface, improving accuracy [12]. |
Experimental Workflow for Post-Eradication Validation
The following diagram outlines the key decision points in the post-eradication validation process.
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in Validation |
|---|---|
| Mycoplasma Removal Agents (MRAs) | Antibiotics specifically formulated to eradicate mycoplasma. Examples include Plasmocin and BM Cyclin. They are used during the treatment phase prior to validation [13] [64]. |
| Antibiotic-Free Cell Culture Medium | Essential for the post-treatment culture period. It ensures that any residual mycoplasma can replicate, making them detectable and preventing false-negative test results [13]. |
| PCR-Based Detection Kit | Kits (e.g., ATCC Universal Mycoplasma Detection Kit) provide primers and components to rapidly and sensitively detect mycoplasma DNA, ideal for routine post-validation checks [1] [65] [28]. |
| Hoechst 33258 DNA Stain | A fluorescent dye used in indirect detection methods. It binds to DNA, allowing visualization of mycoplasma contamination (appearing as filamentous staining outside the cell nucleus) under a fluorescence microscope [1]. |
| Validated Mycoplasma Test Service | Outsourcing testing to a specialized service (e.g., ATCC testing service) provides an unbiased, expert assessment, which is valuable for critical cell lines or for confirming in-house results [63] [65]. |
Mycoplasma contamination represents a critical and persistent challenge in cell culture laboratories, with estimated contamination rates of 15-35% in continuous cell lines worldwide [10] [9]. These smallest known free-living organisms lack cell walls and are resistant to common antibiotics like penicillin and streptomycin, allowing them to persist unnoticed while altering cellular metabolism, gene expression, and proliferation [10] [9]. The consequences extend beyond compromised research data to include product recalls in biopharmaceutical manufacturing and potential risks to patient safety [66] [26]. This technical guide provides a comparative analysis of elimination methodologies framed within the broader context of mycoplasma contamination removal research, specifically addressing the practical challenges faced by researchers and drug development professionals.
Comparative Analysis of Elimination Methods
The table below provides a quantitative comparison of the three primary mycoplasma elimination approaches based on recent scientific literature and commercial product evaluations.
Table 1: Quantitative Comparison of Mycoplasma Elimination Methods
| Method Category | Specific Reagents/Techniques | Reported Efficacy | Treatment Duration | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Antibiotics | Plasmocin [20] [67] | 78-84% success rate across 58 cell lines [20] | 1-2 weeks [13] [67] | Simple, inexpensive, practical for most labs [20] | Risk of resistance development [67] |
| Daptomycin + Clindamycin [68] | Successful decontamination of multiple cultures [68] | Not specified | Effective against M. arginini and M. orale co-contaminations [68] | Specific to certain mycoplasma species | |
| Ciprofloxacin [26] | Component of combination therapy [26] | 4 passages | Works in combination with biological agents | Resistance potential when used alone | |
| Physical Methods | Autoclave [10] | 100% effective on surfaces/equipment | Immediate | Complete elimination on treatable items | Not applicable to cell cultures |
| Filtration (0.1μm) [9] | Effective for solutions | Immediate | Prevents contamination in media/sera | Not applicable to established cultures | |
| UV Irradiation + BKC Wiping [69] | Effectively inhibits mycoplasma growth on surfaces | 20 minutes UV + wiping | Effective for biosafety cabinet decontamination | Ineffective against endotoxins [69] | |
| Novel Reagents | Mynox (surfactin-based) [26] | >90% success rate [26] | 6 days (single passage) [26] | Antibiotic-free, biophysical mechanism prevents resistance [26] | Can affect some eukaryotic cells [26] |
| Mynox Gold (surfactin + ciprofloxacin) [26] | >90% success rate [26] | 4 passages [26] | Combination virtually eliminates resistance risk [26] | Longer treatment duration | |
| Plasmocure [67] | Effective reduction to undetectable levels [67] | 2 weeks [67] | No resistance development observed [67] | Requires continuation with Primocin to maintain effect [67] |
Decision Framework for Method Selection
Diagram 1: Mycoplasma Elimination Decision Framework
Troubleshooting Guides & FAQs
FAQ 1: What factors should guide my choice between antibiotic and non-antibiotic elimination methods?
Answer: The choice depends on three primary factors: (1) Cell line sensitivity - Novel reagents like Mynox are recommended for sensitive primary or stem cells [26]; (2) Resistance concerns - Antibiotics like Plasmocin may lead to resistance development with prolonged use (one month) [67], while surfactant-based methods avoid this risk [26]; (3) Contamination severity - Co-contaminations with multiple mycoplasma species may respond better to specific antibiotic combinations like daptomycin + clindamycin [68]. For most standard cell lines, antibiotic treatment represents the most practical first-line approach, while novel reagents are preferable for valuable or sensitive cultures where resistance must be avoided.
FAQ 2: How do I validate successful mycoplasma elimination post-treatment?
Answer: Proper validation requires a multi-step approach: (1) Culture cells without antibiotics for 1-2 weeks after treatment completion to allow potential contaminants to proliferate [13]; (2) Use highly sensitive detection methods - PCR is currently the most sensitive and specific method, capable of detecting mycoplasma DNA sequences even at low levels [20] [67]; (3) Test at multiple time points - Successful decontamination should show permanent elimination with no mycoplasma detection at day +14 post-treatment and later time points [20]; (4) Consider qPCR quantification for absolute quantification of mycoplasma levels, which can detect reductions to less than 1 mycoplasma per contaminated cell [67].
FAQ 3: What are the most common reasons for treatment failure, and how can they be addressed?
Answer: Treatment failures typically occur due to:
- Antibiotic Resistance: Certain mycoplasma strains develop resistance, particularly with single-agent antibiotic regimens [67]. Solution: Use combination therapies like Mynox Gold (surfactin + ciprofloxacin) that virtually eliminate resistance risk [26], or employ sequential treatments with different mechanisms of action [20].
- Incomplete Access to Contaminants: Mycoplasmas trapped in cell clusters or clumps may be physically shielded from antibiotics [20]. Solution: Break up cell clusters during treatment and ensure thorough mixing for optimal reagent distribution [20].
- Recontamination from Laboratory Equipment: Standard cleaning methods like ethanol wiping may not eliminate mycoplasma from biosafety cabinets [69]. Solution: Implement evidence-based cleaning protocols using UV irradiation (200 mJ/cm² for 20 minutes) combined with benzalkonium chloride wiping [69].
Experimental Protocols for Mycoplasma Elimination
Protocol 1: Standard Antibiotic Treatment with Plasmocin
Methodology: Based on established protocols with demonstrated efficacy across multiple cell lines [20] [13] [67]:
- Preparation: Replace spent medium with fresh growth medium supplemented with 5-10% higher concentration of fetal bovine serum to counterbalance potential antibiotic toxicity [20].
- Antibiotic Application: Add Plasmocin directly to culture medium at 25μg/mL [13]. Prepare antibiotic dilutions fresh for each treatment cycle.
- Treatment Duration: Maintain continuous antibiotic exposure for 1-2 weeks [13] [67].
- Culture Conditions: Keep cultures at higher cell densities during treatment and ensure thorough mixing to break up cell clusters, allowing physical access of antibiotics to membrane-attached mycoplasmas [20].
- Validation Phase: After treatment, culture cells without antibiotics for 1-2 weeks, then test for mycoplasma using PCR methods [13].
Protocol 2: Novel Reagent Treatment with Mynox
Methodology: Adapted from manufacturer protocols and independent evaluations [26]:
- Reagent Application: Add Mynox reagent directly to contaminated cell culture during a single passage or medium change.
- Treatment Duration: Incubate for approximately 6 days [26].
- Mechanism of Action: The surfactin component integrates selectively into mycoplasma membranes, compromising integrity and causing osmotic influx that leads to complete disintegration [26].
- Post-Treatment Recovery: The treatment selectively eliminates contaminated cells while allowing healthy cells to recover with native morphology and normal proliferation rates [26].
- Validation: Test treated cultures using a mycoplasma detection kit to confirm complete elimination.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents for Mycoplasma Elimination Research
| Reagent/Category | Specific Examples | Function/Mechanism | Application Context |
|---|---|---|---|
| Conventional Antibiotics | Plasmocin [20] [67] | Dual mechanism against mycoplasma proteins | First-line treatment for standard cell lines |
| Daptomycin + Clindamycin [68] | Combination therapy targeting cell membrane | Specific for M. arginini and M. orale contaminants | |
| Ciprofloxacin [26] | Inhibits DNA gyrase and topoisomerase IV | Component of combination therapies | |
| Novel Biological Reagents | Mynox (surfactin) [26] | Cyclic lipopeptide that disrupts mycoplasma membranes | Antibiotic-free elimination for resistance concerns |
| Mynox Gold (surfactin + ciprofloxacin) [26] | Combined biophysical and antibiotic mechanism | For sensitive/primary cells with minimal resistance risk | |
| Detection & Validation | PCR-Based Detection [68] [20] | Amplification of mycoplasma-specific DNA sequences | Gold standard for confirmation pre- and post-treatment |
| qPCR Quantification [67] | Absolute quantification of mycoplasma per cell | Precise measurement of elimination efficacy | |
| Hoechst 33342 Staining [67] | Fluorescent DNA staining for visualization | Supplementary method for contamination visualization |
The comparative analysis presented herein demonstrates that effective mycoplasma elimination requires a strategic approach tailored to specific research contexts. While conventional antibiotics offer practical and cost-effective solutions for most applications, novel reagents provide critical alternatives for sensitive cell types and resistance-prone scenarios. Physical methods remain essential for preventative control but are insufficient alone for established contaminations. The ongoing development of combination therapies and quantitative validation methods represents significant advances in the field, enabling researchers to preserve invaluable cell lines and maintain scientific integrity in cell-based research and biopharmaceutical development.
Mycoplasma contamination represents one of the most pervasive and challenging issues in cell culture research, affecting an estimated 15-35% of continuous cell lines and up to 62% of cell cultures worldwide [10] [70]. These minute bacteria (0.2-0.8 μm) lack cell walls, rendering them resistant to common antibiotics like penicillin and streptomycin and allowing them to pass through standard 0.2μm sterilization filters [10]. The consequences of contamination are severe, including altered cell metabolism, gene expression changes, chromosomal aberrations, and unreliable research data [10]. Unlike bacterial or fungal contaminants that cause media turbidity, mycoplasma contamination often progresses invisibly, with cultures appearing normal under routine microscopic examination while producing compromised results [71].
The development of commercial elimination kits like Plasmocin and Myco-Off addresses the critical need for reliable decontamination strategies that can salvage valuable cell lines without the cytotoxicity associated with traditional antibiotic cocktails. These solutions offer targeted approaches to eradicate mycoplasma while preserving cell viability, providing researchers with practical tools to combat this persistent problem. This technical support center document provides comprehensive guidance on evaluating, selecting, and implementing these commercial solutions within a structured contamination management framework.
Understanding Mycoplasma Contamination
Biology and Challenges
Mycoplasma species belong to the class Mollicutes and are characterized by their small genome size, absence of a cell wall, and parasitic nature [10]. They attach to host cell membranes and fuse with them, eventually replicating to outnumber host cells by a thousand-fold [10]. Their biological characteristics present unique challenges for containment and elimination:
- Size and Filter Avoidance: With diameters of 0.2-0.8μm and the ability to shrink due to flexible membranes, mycoplasma pass through standard 0.2μm filters used for media sterilization [10].
- Antibiotic Resistance: The lack of a cell wall makes them naturally resistant to beta-lactam antibiotics (penicillin, streptomycin, gentamicin) that target cell wall synthesis [10].
- Stealth Proliferation: Contamination doesn't produce turbidity or dramatic pH shifts in media, allowing it to remain undetected for extended periods [70] [71].
Understanding contamination sources is crucial for prevention and effective elimination implementation:
- Human Origin: Laboratory personnel are the primary contamination source, with aerosols generated by talking, coughing, or pipetting carrying various Mycoplasma species [10].
- Cross-Contamination: Contaminated cell lines spread mycoplasma to other cultures in shared incubators or through poor aseptic technique [10].
- Reagents and Serum: While improving due to manufacturing advances, bovine serum and porcine-derived trypsin can introduce mycoplasma of bovine origin [10].
- Lab Equipment: Incubators, water baths, and biosafety cabinets can harbor microorganisms without regular cleaning [72].
Comprehensive Comparison of Commercial Kits
Mycoplasma Elimination Kits Comparison
The following table summarizes key commercial solutions for mycoplasma elimination, their mechanisms, advantages, and limitations:
| Product Name | Mechanism of Action | Advantages | Limitations | Treatment Duration | Cytotoxicity Concerns |
|---|---|---|---|---|---|
| Myco-Off | Disrupts mycoplasma metabolism and replication pathways [71] | Targeted action, low cytotoxicity, ready-to-use format, suitable for sensitive cell lines [71] | Requires treatment cycles and post-treatment monitoring [71] | Days to weeks (depending on contamination degree) [71] | Minimal cytotoxic stress reported [71] |
| Antibiotic Cocktails (e.g., macrolides, tetracyclines, quinolones) | Combination antibiotics that suppress or kill mycoplasma [71] | Accessible, broad spectrum against many species [71] | Potential cytotoxic effects on sensitive cells, may induce antibiotic resistance [71] | Multiple cycles often required [71] | Can be cytotoxic to stem cells, hybridomas, and other sensitive lines [71] |
| Discard & Restart | Physical elimination of contaminated cultures [71] | Definitive removal of contamination, avoids chemical stress on cells [71] | Loss of valuable or irreplaceable cell lines, significant experiment delays [71] | N/A | None (no chemical treatment) [71] |
Note: While Plasmocin is a widely used commercial solution, specific current data regarding its mechanism and performance was not available in the search results.
Performance Considerations
When selecting a mycoplasma elimination kit, several performance factors must be considered:
- Treatment Efficacy: Complete eradication often requires extended treatment cycles (days to weeks) with careful monitoring [71].
- Cell Line Compatibility: Sensitive lines (stem cells, hybridomas, neuronal cultures) may respond better to low-toxicity options like Myco-Off versus traditional antibiotic cocktails [71].
- Resistance Development: Antibiotic-based solutions may induce resistance with improper use, necessitating combination approaches or alternative mechanisms [71].
Detection Methods and Verification
Mycoplasma Detection Methods Comparison
Effective elimination requires reliable pre- and post-treatment detection. The table below compares primary detection methodologies:
| Method | Principle | Time Required | Cost per Sample | Sensitivity | Advantages | Disadvantages |
|---|---|---|---|---|---|---|
| PCR-Based Detection | Amplifies mycoplasma-specific gene targets [70] | <1 day [70] | $20-30 [70] | 98% reliability [70] | Fast, affordable, sensitive [70] | Requires PCR equipment and expertise [70] |
| Microbiological Culture | Grows mycoplasma in specialized media [10] | 4-5 weeks [70] | $400-2,000 [70] | 100% reliability [70] | Definitive, considered gold standard [70] | Extremely long turnaround, expensive [70] |
| DNA Staining (DAPI/Hoechst) | Fluorescent staining of mycoplasma DNA [10] | <1 day [70] | $200-1,000 [70] | 50% reliability [70] | Fast, visual confirmation [70] | Lower sensitivity, subjective interpretation [10] |
| qPCR Detection | Real-time PCR amplification with fluorescent probes [70] | <1 day | ~$20-30 (similar to conventional PCR) | Higher sensitivity than conventional PCR [70] | Most sensitive molecular method, quantitative potential [70] | Requires specialized equipment [70] |
Detection Workflow
The following diagram illustrates the typical workflow for mycoplasma detection using the most common methods:
Post-Elimination Verification
After implementing any elimination protocol, thorough verification is essential:
- Timeline: Test treated cultures across multiple passages (typically 3-5) over 2-4 weeks to ensure contamination has not returned [71].
- Method Selection: PCR-based methods are ideal for post-treatment monitoring due to their sensitivity and rapid turnaround time [70].
- Documentation: Maintain detailed records of treatment parameters, testing dates, and results for quality assurance and regulatory compliance.
Experimental Protocols
Mycoplasma Elimination Protocol Using Commercial Kits
The following workflow details the general procedure for implementing commercial mycoplasma elimination kits:
Detailed Step-by-Step Procedure
Pre-Treatment Assessment
- Confirm mycoplasma contamination using a reliable detection method (PCR recommended) [70].
- Assess cell line value and sensitivity to determine if elimination is preferable to discarding.
- Create backup frozen stocks if available before treatment initiation.
Treatment Phase
- Prepare treatment medium according to manufacturer instructions.
- For Myco-Off: Add liquid solution directly to culture medium during routine media changes [71].
- Maintain treatment for recommended duration (typically days to weeks, depending on contamination severity) [71].
- Monitor cells daily for signs of stress or cytotoxicity.
Post-Treatment Verification
- After treatment completion, passage cells 2-3 times in antibiotic-free medium.
- Test for mycoplasma contamination using PCR or other sensitive methods [70].
- Repeat testing over multiple passages (recommended: 3 passages over 2-3 weeks) to ensure complete eradication [71].
- Only return cells to main culture system after consistent negative results.
The Researcher's Toolkit
Essential Research Reagent Solutions
The following table catalogues essential reagents and materials for effective mycoplasma management:
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Myco-Off | Targeted mycoplasma elimination reagent [71] | Low cytotoxicity; suitable for sensitive cell lines; ready-to-use liquid format [71] |
| PCR Detection Kits (e.g., VenorGeM, MycoTOOL) | Detect mycoplasma DNA in cell cultures [73] [74] | High sensitivity (98%); results in <1 day; requires PCR equipment [70] |
| DAPI/Hoechst Stain | Fluorescent DNA staining for microscopic detection [10] | Rapid screening (<1 day); subjective interpretation; lower sensitivity [70] |
| Antibiotic Cocktails (macrolides, tetracyclines, quinolones) | Broad-spectrum mycoplasma suppression [71] | Potential cytotoxicity; resistance development concerns [71] |
| Quality Sera and Reagents | Prevention of initial contamination [72] | Source from reputable suppliers; test new lots for mycoplasma [72] |
| Cryopreservation Materials | Maintain contamination-free backup stocks [10] | Preserve uncontaminated cell lines; create working and master cell banks [10] |
FAQs and Troubleshooting Guides
Frequently Asked Questions
Q1: How often should I test my cell cultures for mycoplasma contamination? A: Testing should be performed at minimum every 6 months, with additional testing recommended upon receipt of new cell lines and before large-scale experiments [70]. For core facilities or cell banks, more frequent testing (quarterly) is advisable.
Q2: Can I use common antibiotics like penicillin-streptomycin to prevent mycoplasma contamination? A: No. Mycoplasma lack cell walls, making them naturally resistant to antibiotics that target cell wall synthesis (e.g., penicillin, streptomycin) [10]. Indiscriminate antibiotic use can mask contamination while allowing mycoplasma to proliferate undetected.
Q3: What is the most reliable method to detect mycoplasma contamination? A: PCR-based detection offers the best combination of sensitivity (98%), speed (<1 day), and cost ($20-30/sample) for most research applications [70]. For regulatory purposes, the microbiological culture method (28-day incubation) remains the gold standard despite its long turnaround time [74].
Q4: Should I attempt to eliminate mycoplasma or simply discard contaminated cultures? A: For replaceable cell lines with available clean frozen stocks, discarding is recommended. For valuable, irreplaceable, or unique cell lines, elimination attempts with commercial kits like Myco-Off may be justified, provided strict quarantine and verification protocols are followed [71].
Troubleshooting Common Issues
Problem: Incomplete Clearance After Treatment
- Possible Causes: Insufficient treatment duration, inadequate reagent concentration, or antibiotic-resistant mycoplasma strains.
- Solutions: Extend treatment cycles, ensure proper reagent concentration according to manufacturer guidelines, consider switching to a reagent with a different mechanism of action, and confirm complete eradication with multiple verification tests across several passages [71].
Problem: Cell Stress or Cytotoxicity During Treatment
- Possible Causes: Overly aggressive treatment, sensitive cell line, or incorrect reagent concentration.
- Solutions: Reduce treatment concentration, increase recovery intervals between treatments, or switch to a lower-toxicity option like Myco-Off for sensitive cells [71].
Problem: Recurring Contamination After Successful Treatment
- Possible Causes: Cross-contamination from other cultures, contaminated reagents, or inadequate lab practices.
- Solutions: Implement strict quarantine procedures for new cell lines, test all incoming reagents and sera, review and reinforce aseptic techniques among lab personnel, and ensure regular decontamination of shared equipment [72] [10].
Problem: Inconsistent Detection Results
- Possible Causes: Sampling error, insufficient sensitivity of detection method, or interpretation errors.
- Solutions: Test during active cell growth, use positive controls, employ multiple detection methods for confirmation, and ensure personnel are properly trained in method-specific interpretation criteria [73] [70].
Mycoplasma contamination remains a significant threat to cell culture research integrity, but commercial elimination kits like Plasmocin and Myco-Off provide valuable tools for addressing this challenge. These solutions enable researchers to salvage irreplaceable cell lines while maintaining experimental timelines. Successful implementation requires careful consideration of cell line sensitivity, contamination severity, and appropriate verification protocols.
A comprehensive approach combining regular monitoring with reliable detection methods, prompt intervention using targeted elimination reagents, and strict adherence to aseptic techniques represents the most effective strategy for maintaining contamination-free cell cultures. By integrating these commercial solutions within a robust quality management framework, researchers can protect their investments in cell line development and ensure the reliability of their scientific data.
Mycoplasma contamination represents a critical challenge in cell culture, forcing researchers to make a difficult decision: discard valuable cultures or attempt a resource-intensive treatment. This analysis evaluates the economic and scientific factors to guide this decision, supporting the integrity of research on mycoplasma contamination removal.
The table below summarizes the core considerations for each approach.
| Factor | Discarding Contaminated Lines | Treating Contaminated Lines |
|---|---|---|
| Direct Costs | Cost of re-establishing culture; loss of irreplaceable primary or engineered cells [26]. | Cost of elimination reagents (e.g., Mynox, Mynox Gold) and validation testing [26] [75]. |
| Time Investment | Time to thaw new stock or re-derive cell line (weeks to months). | Treatment duration ranges from a few days to several weeks [26] [75]. |
| Technical Success | 100% effective in removing the contaminant. | >90% success rate with best-practice protocols; risk of treatment failure or resistance [26]. |
| Impact on Cell Phenotype | Guaranteed genetic and phenotypic stability (if using low-passage stock). | Risk of permanent alterations in metabolism, gene expression, and function due to contamination [26] [10]. |
| Risk of Spread | Eliminates risk of cross-contaminating other cultures immediately. | High risk of lab-wide spread if quarantine protocols fail [10] [76]. |
Frequently Asked Questions (FAQs)
FAQ 1: Under what conditions is it unequivocally better to discard a contaminated cell line?
Discarding the culture is the most prudent course of action in these scenarios [26] [10] [75]:
- The cell line is readily replaceable from a certified cell bank or your own low-passage frozen stock.
- The research is time-sensitive, and the weeks required for treatment and validation would cause critical delays.
- The cell line is used for critical applications like drug screening, biopharmaceutical production, or gene expression studies, where any lingering effects of contamination could compromise data integrity [26] [10].
- The contamination is widespread in the laboratory, and drastic containment measures are needed.
FAQ 2: When might treating a contaminated cell line be a justifiable risk?
Treatment can be a viable strategy when [26] [10] [75]:
- The cell line is irreplaceable or unique (e.g., primary cells, genetically modified lines, or lines that took years to establish).
- The cost and time to re-develop or obtain a new line are prohibitive.
- You have the capacity to strictly quarantine the culture throughout the treatment and validation process.
- You are using a well-characterized protocol and can commit to comprehensive post-treatment validation.
FAQ 3: What are the hidden long-term costs of treating a contaminated culture?
Beyond reagent costs, treatment introduces significant hidden costs [26] [77] [24]:
- Extended Labor: Weeks of dedicated effort for treatment, passaging, and monitoring.
- Validation Testing: Costs for PCR, staining, or other assays to confirm eradication before, during, and after treatment.
- Uncertainty in Research: Even after "successful" treatment, subtle, persistent effects on cell metabolism and gene expression can lead to unreliable data, potentially invalidating long-term projects and publications [77].
FAQ 4: How does mycoplasma contamination affect experimental data and reproducibility?
Mycoplasma contamination severely compromises data integrity and is a major source of irreproducible results. Effects include [26] [10] [75]:
- Altered Cell Metabolism: Mycoplasmas compete for essential nutrients, starving the host cells.
- Changes in Gene Expression: Contamination can lead to chromosomal aberrations and altered transcriptome profiles.
- Cytopathic Effects: Can inhibit cell growth and proliferation, induce cell death, and cause morphological changes.
- Interference with Assays: Contamination can decrease transfection efficiency and skew results in virtually every type of cellular assay.
Troubleshooting Guide: Decontamination Protocol
For researchers who must attempt decontamination, the following workflow provides a detailed methodology. This protocol is adapted from general guidelines and specific product information [26] [78] [75].
Detailed Protocol Steps
Confirm and Quarantine: Use a validated detection method (e.g., PCR, DNA staining) to confirm mycoplasma contamination. Immediately move the contaminated culture to a dedicated, quarantined incubator and workspace to prevent cross-contamination [10] [76] [75].
Select Elimination Method: Choose a mycoplasma-specific elimination reagent. Standard antibiotics like penicillin and streptomycin are ineffective due to mycoplasma's lack of a cell wall [10] [75]. Options include:
- Non-antibiotic reagents (e.g., Mynox): Uses surfactin to disrupt the mycoplasma membrane via a biophysical mechanism, avoiding resistance [26].
- Specialized antibiotic cocktails (e.g., Mynox Gold, MycoAway): Combines antibiotics like ciprofloxacin with surfactin. These are often recommended for sensitive primary cells [26] [75].
Treatment Application:
- Dissociate and count cells, diluting them in antibiotic-free medium [78].
- Add the elimination reagent at the manufacturer's recommended concentration. It is critical to use antibiotic-free medium during treatment to ensure the reagent is effective and to avoid masking persistent contamination [78] [76].
Monitor and Passage: Observe cells daily for signs of toxicity (e.g., vacuolation, sloughing, decreased confluency). Culture the cells for the recommended treatment period, typically 4 to 6 passages [78] [75], with the reagent present.
Validate Eradication: After the treatment period, remove the elimination reagent and culture the cells in antibiotic-free medium for an additional 4 to 6 passages [78].
Decision Point & Re-establishment:
- If Eradicated: Expand the clean culture and create a new, large stock of frozen vials to serve as a future backup.
- If Not Eradicated: Discard the culture. Consider using a different elimination reagent if the cell line is irreplaceable, but be aware of the increasing time investment and accumulating genetic drift.
The Scientist's Toolkit: Key Research Reagents
The following table lists essential materials for the detection and elimination of mycoplasma contamination.
| Reagent / Kit | Primary Function | Key Features & Considerations |
|---|---|---|
| PCR Detection Kit [10] [75] | Detection / Validation | Rapid, sensitive, and specific. Detects mycoplasma DNA. Essential for initial diagnosis and post-treatment validation. |
| Mynox [26] | Elimination | Non-antibiotic reagent using surfactin. Biophysical mode of action disintegrates mycoplasma membrane; low risk of resistance. |
| Mynox Gold [26] | Elimination | Combination of ciprofloxacin and surfactin. Recommended for sensitive/primary cells. High success rate (>90%). |
| MycoAway [75] | Elimination | Antibiotic cocktail (e.g., tetracycline, macrolides). Effective and non-toxic for most mammalian cells; typically requires 2 weeks of treatment. |
| DAPI / Hoechst Stains [10] [11] | Detection | DNA-binding fluorochromes. Stain extranuclear mycoplasma DNA. Requires fluorescence microscopy; interpretation can be subjective. |
| Microbiological Culture [10] | Detection | Gold standard method. Involves growing mycoplasma on agar plates. Highly sensitive but slow, requiring up to 4 weeks for results. |
Building a Validation Dossier for Regulatory Compliance and Quality Assurance
Troubleshooting Guides & FAQs: Mycoplasma Contamination in Cell Culture
Frequently Asked Questions
Q1: My cells are growing slowly and look abnormal, but the media isn't cloudy. Could this be mycoplasma contamination?
Yes, these are classic signs of mycoplasma contamination. Unlike typical bacteria that cause turbidity, mycoplasma contamination doesn't cloud the culture medium but can cause subtle changes including decreased cell proliferation rates, poorer adhesion for adherent cells, and morphological changes [10] [25]. These organisms lack a cell wall and are too small (0.1-0.8 µm) to be seen with standard light microscopy, making them difficult to detect without specific testing [2].
Q2: Why are the standard antibiotics in my culture media not preventing mycoplasma contamination?
Mycoplasma lack a rigid cell wall, making them naturally resistant to common cell culture antibiotics like penicillin and streptomycin that target cell wall synthesis [10] [1]. In fact, routine use of these antibiotics can mask contamination by eliminating other bacteria while allowing mycoplasma to proliferate undetected [1].
Q3: What is the most reliable method to detect mycoplasma contamination in our cell lines?
The table below compares the primary detection methods recommended by regulatory bodies:
Table 1: Comparison of Mycoplasma Detection Methods
| Method | Principle | Duration | Advantages | Disadvantages | Regulatory Status |
|---|---|---|---|---|---|
| Microbiological Culture | Grows mycoplasma on specialized agar plates | 4-5 weeks | Gold standard, high specificity | Very time-consuming | EMA gold standard [10] |
| DNA Fluorochrome Staining | Fluorescent dyes (e.g., Hoechst) bind to mycoplasma DNA | 1-2 days | Visual confirmation, relatively fast | Subjective interpretation [10] | Chinese Pharmacopoeia method [25] |
| PCR-Based Detection | Amplifies specific mycoplasma DNA sequences | Hours | Rapid, highly sensitive, identifies species | May detect non-viable organisms [10] | Meets European Pharmacopoeia standards [1] |
Q4: We've identified mycoplasma contamination in a valuable, irreplaceable cell line. What are our treatment options?
For irreplaceable cell lines, several elimination strategies exist, each with different mechanisms and success rates:
Table 2: Mycoplasma Elimination Strategies
| Method | Mechanism of Action | Treatment Duration | Success Rate | Considerations |
|---|---|---|---|---|
| Antibiotic Treatment | Inhibits protein or DNA synthesis | Multiple passages | Variable | Risk of resistance, cell toxicity [25] |
| Mynox | Membrane disruption via surfactin | ~6 days | >90% | Antibiotic-free, biophysical action [26] |
| Mynox Gold | Combined surfactin + ciprofloxacin | 4 passages | >90% | For sensitive/primary cells, minimal resistance [26] |
| Heat Treatment | Thermal inactivation at 41°C | 5-18 hours | Variable | High risk of cell line damage [25] |
Q5: What documentation is essential for including mycoplasma testing in a regulatory validation dossier?
Your validation dossier should include: (1) Certificate of Analysis for all testing reagents; (2) Standard Operating Procedures for detection methods; (3) Raw data and interpretation records; (4) Personnel training records; (5) Equipment qualification and maintenance logs; (6) Environmental monitoring data [79] [80]. For CMC regulatory dossiers, you must demonstrate that testing occurs throughout the manufacturing process and that any changes are properly reported to Health Authorities [79].
Experimental Protocols for Mycoplasma Detection and Elimination
Protocol 1: PCR-Based Mycoplasma Detection
Principle: This method amplifies specific 16S rRNA gene sequences unique to Mycoplasma, Acholeplasma, and Ureaplasma species using universal primers [1].
Materials:
- PCR master mix with thermostable DNA polymerase
- Species-specific primers
- Positive and negative controls
- DNA extraction kit
- Thermal cycler
- Agarose gel electrophoresis equipment
Procedure:
- Collect 200µL of cell culture supernatant after 72 hours of growth
- Extract DNA using commercial kit following manufacturer's instructions
- Prepare PCR reaction mix with touchdown PCR protocol
- Run amplification: Initial denaturation 95°C/5min; 35 cycles of 95°C/30s, 60°C/30s, 72°C/45s; Final extension 72°C/7min
- Analyze products on 1.5% agarose gel
- Include appropriate positive and negative controls in each run
Validation Parameters: Test sensitivity must detect ≤100 CFU/mL; specifically identify the top 8 contaminating species including M. arginini, M. fermentans, M. hyorhinis, and M. orale [1].
Protocol 2: Mycoplasma Elimination with Combination Reagents
Principle: Simultaneously disrupts mycoplasma membranes and inhibits DNA replication while minimizing host cell damage [26] [25].
Materials:
- Pricella Anti-Mycoplasma Treatment Reagent (Cat. No.: P-CMR-001) or equivalent
- Complete growth medium
- Quaternary ammonium disinfectant
- Mycoplasma detection kit for confirmation
Procedure:
- Identify contaminated cultures through validated detection methods
- Prepare treatment medium with recommended concentration of elimination reagent
- Replace existing medium with treatment medium
- Incubate for specified duration (typically 4-6 days)
- Replace with fresh treatment medium if required by protocol
- Passage cells with standard medium after treatment period
- Quarantine treated cells and test for mycoplasma contamination after 3-5 passages
- Confirm elimination with two different detection methods
Quality Control: Maintain detailed records of treatment dates, reagent lot numbers, and all test results. Only return cells to general culture after obtaining three consecutive negative results over 2-3 weeks [26].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Mycoplasma Management
| Reagent/Kit | Function | Application Notes |
|---|---|---|
| Mycoplasma Elimination Reagents | Removes contamination from valuable cell lines | Mynox uses surfactant-based mechanism; Mynox Gold combines surfactin + ciprofloxacin [26] |
| PCR Detection Kits | Rapid, specific identification of mycoplasma species | Can detect >60 species in hours; choose kits meeting pharmacopoeia standards [1] |
| DNA Fluorochrome Stains | Visualizes mycoplasma DNA attached to host cells | Hoechst 33258 or DAPI staining; requires fluorescence microscopy [10] [1] |
| Selective Culture Media | Grows mycoplasma for confirmation | Essential for regulatory compliance; requires 4-5 week incubation [10] |
| Mycoplasma-Specific Antibiotics | Targets mycoplasma without affecting host cells | Effective options include macrolides, tetracyclines, and quinolones [10] |
Workflow Visualization
Mycoplasma Contamination Management Workflow
Quality System for Regulatory Compliance
Conclusion
Mycoplasma contamination presents a formidable challenge, but it is not insurmountable. A proactive, multi-pronged strategy that integrates rigorous detection, informed selection of eradication methods tailored to specific cell lines, and robust validation is paramount for success. The key takeaway is that prevention through strict aseptic technique, regular testing, and careful quarantine of new cell lines is infinitely more effective than decontamination. For the future of biomedical research, embracing these comprehensive contamination control plans is non-negotiable. It is the foundation upon which reliable preclinical data, successful drug development, and ultimately, translational clinical breakthroughs are built. As cell models like organoids and stem cells become more complex, the imperative for mycoplasma-free cultures will only intensify, making these practices central to research excellence.
References
- 1. Mycoplasma Contamination [https://www.atcc.org/the-science/authentication/mycoplasma-contamination]
- 2. Mycoplasma Contamination | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/biological-contamination/mycoplasma-contamination.html]
- 3. Mycoplasma [https://en.wikipedia.org/wiki/Mycoplasma]
- 4. Mycoplasma Infection Types: Causes & Prevention [https://my.clevelandclinic.org/health/diseases/23545-mycoplasma]
- 5. What is Mycoplasma? [https://www.sartorius.com/en/knowledge/science-snippets/what-is-mycoplasma-693938]
- 6. Mycoplasma contamination of cell cultures [https://pmc.ncbi.nlm.nih.gov/articles/PMC3463982/]
- 7. Troubleshooting Guide: MycoProbe Mycoplasma Detection ... [https://www.rndsystems.com/resources/technical/troubleshooting-guide-mycoprobe-mycoplasma-detection-kit]
- 8. Mycoplasma Testing Market Size, Share [https://www.fortunebusinessinsights.com/mycoplasma-testing-market-108687]
- 9. Prevention and Detection of Mycoplasma Contamination in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3584481/]
- 10. Mycoplasma Contamination in Cell Culture | Detection & ... [https://www.capricorn-scientific.com/knowledge-center/mycoplasma-contamination-cell-culture]
- 11. Mycoplasma contamination of cell cultures [https://bioscience.lonza.com/lonza_bs/CH/en/mycoplasma-contamination-in-cell-culture]
- 12. A new method for detecting mycoplasma in cell cultures ... [https://www.sciencedirect.com/science/article/pii/S2405580825002201]
- 13. Mycoplasma Contamination: Prevention, Testing & Treatment [https://blog.cellsignal.com/mycoplasma-contamination]
- 14. What Causes a Mycoplasma Contamination? [https://news.minerva-biolabs.com/informative-articles/2024/03]
- 15. Troubleshooting Cell Culture Contamination: A Practical ... [https://www.yeasenbio.com/blogs/cell/troubleshooting-cell-culture-contamination-a-practical-solution-guide]
- 16. Cell Culture Troubleshooting [https://www.sigmaaldrich.com/US/en/applications/cell-culture-and-cell-culture-analysis/cell-culture-troubleshooting?srsltid=AfmBOoqauii-bB2cNmZkqlNw9Mf-DtjPPn23qVSz98_vHoY8oyqXwa49]
- 17. How Does Mycoplasma Contamination Affect Cell Culture? [https://www.eppendorf.com/us-en/lab-academy/life-science/cell-biology/how-does-mycoplasma-contamination-affect-cell-culture/]
- 18. Effects of Mycoplasmas on the Host Cell Signaling Pathways [https://pmc.ncbi.nlm.nih.gov/articles/PMC7238135/]
- 19. Cell Culture Contamination Troubleshooting [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/cell-culture-troubleshooting-contamination?srsltid=AfmBOooY5K2Kvv-cPRI92BGkJdftbDHX39unvgvQLTifnr2pVYiBRo9u]
- 20. Treatment of Mycoplasma Contamination in Cell Cultures ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3470117/]
- 21. The Importance of Mycoplasma Testing in Cell Culture [https://cellculturecompany.com/the-importance-of-mycoplasma-testing-in-cell-culture/]
- 22. A PCR protocol to establish standards for routine mycoplasma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10192841/]
- 23. Cell culture challenges: Contamination & prevention [https://greenelephantbiotech.com/blog/cell-culture-challenges-contamination-prevention/]
- 24. A Beginner's Guide to Cell Culture: Practical Advice for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10000895/]
- 25. The Guide to Mycoplasma Contamination Treatment [https://www.procellsystem.com/resources/cell-culture-academy/the-guide-to-mycoplasma-contamination-treatment-2100]
- 26. How to Eliminate a Mycoplasma Contamination? [https://news.minerva-biolabs.com/informative-articles/2025/08]
- 27. Mycoplasma Contamination Why It ... [https://hardydiagnostics.com/media/wysiwyg/MICRObits/Pharma/2025/06-June/microbits-pharma-june-2025-newsletter.html]
- 28. Mycoplasma Detection in Cell Cultures [https://www.rapidmicrobiology.com/test-method/rapid-detection-of-mycoplasmas]
- 29. How to Handle Mycoplasma in Cell Culture? [https://www.creative-bioarray.com/support/how-to-handle-mycoplasma-in-cell-culture.htm]
- 30. Simple, specific, rapid, and pharmacopoeia-compliant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12441703/]
- 31. Detection of Mycoplasma Contamination Directly from ... [https://pubmed.ncbi.nlm.nih.gov/27978415/]
- 32. Optimized PCR-based Detection of Mycoplasma - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3197068/]
- 33. A highly sensitive internally-controlled real-time PCR assay ... [https://www.sciencedirect.com/science/article/pii/S104510561930137X]
- 34. PCR Troubleshooting Guide | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/cloning/cloning-learning-center/invitrogen-school-of-molecular-biology/pcr-education/pcr-reagents-enzymes/pcr-troubleshooting.html]
- 35. PCR Troubleshooting: Common Problems and Solutions [https://www.mybiosource.com/learn/pcr-troubleshooting-common-problems-and-solutions/]
- 36. Molecular identification and antibiotic clearance of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11792515/]
- 37. Mycoplasma Contamination in Cell Culture [https://www.mpbio.com/jp/life-sciences/cell-biology/contamination-management/mycoplasma-detection-removal?srsltid=AfmBOorxufO2AImGUfRTqWrlqeGaTmbyiN-vR2pFCrwqseyWMon4IX6d]
- 38. Tetracycline Antibiotics: Mode of Action, Applications ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC99026/]
- 39. Mechanisms of Antibacterial Drugs | Microbiology [https://courses.lumenlearning.com/suny-microbiology/chapter/mechanisms-of-antibacterial-drugs/]
- 40. Mechanism of action of and resistance to quinolones - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3815421/]
- 41. Eradication of Mycoplasma pneumoniae biofilm towers by ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0329571]
- 42. Effects and Eradication of Mycoplasma Contamination on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10530407/]
- 43. Postoperative Disseminated Mycoplasma hominis Infection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12410094/]
- 44. Mycoplasma et Décontamination [https://www.itwreagents.com/rest-of-world/fr/cb-cc-mycoplasma-et-decontamination]
- 45. Prevalence of Macrolide-Resistant Mycoplasma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12602751/]
- 46. Association between point mutations of macrolide-resistant ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1682167/full]
- 47. Spread of dual-class drug-resistant of Mycoplasma ... [https://www.medrxiv.org/content/10.1101/2025.09.10.25335488v1.full-text]
- 48. Mycoplasma genitalium - STI Treatment Guidelines [https://www.cdc.gov/std/treatment-guidelines/mycoplasmagenitalium.htm]
- 49. Mycoplasma genitalium infections: current treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5589104/]
- 50. Mycoplasma genitalium treatment strategies in the era of ... [https://pubmed.ncbi.nlm.nih.gov/40555261/]
- 51. 细胞培养污染故障排除 [https://www.sigmaaldrich.com/HK/zh/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/cell-culture-troubleshooting-contamination?srsltid=AfmBOoqQIWMGQmtC1WDByKONAhqZPz2ENZ-OSgodWWNQwZYJo0JoX2eT]
- 52. Troubleshooting Cell Culture Contamination [https://www.creative-bioarray.com/support/troubleshooting-cell-culture-contamination-a-comprehensive-guide.htm]
- 53. A new method for detecting mycoplasma in cell cultures ... [https://pubmed.ncbi.nlm.nih.gov/40678803/]
- 54. Protocol to assess the cytotoxicity of autologous human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12483667/]
- 55. Multi-assay assessment of cytotoxicity reveals multiple ... [https://www.nature.com/articles/s41598-025-86792-4]
- 56. Mycoplasma [https://unclineberger.org/tissueculture/contaminant/mycoplasmacontam/]
- 57. Mycoplasma Removal from Cell Culture Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3589884/]
- 58. , Diagnosis and Eradication of Prevention ... Mycoplasma [https://pmc.ncbi.nlm.nih.gov/articles/PMC10668599/]
- 59. Biosafety/Biocontainment Plan Guidance: Provision ... [https://www.selectagents.gov/compliance/guidance/biosafety/provision.htm]
- 60. Preventing & Managing Mycoplasma Contamination in Labs [https://www.marathonls.com/mycoplasma-contamination-how-to-stop-current-outbreaks-and-prevent-future-ones/?srsltid=AfmBOorbpH8zmf8G6jYf0QHHBg9TuqlLexh3uqpkIvKUyW6robLB099K]
- 61. Controlling Cross-Contamination in Research Facilities [https://dycem.com/blog/controlling-cross-contamination-in-research-facilities/]
- 62. Prevention, Diagnosis and Eradication of Mycoplasma ... [https://pubmed.ncbi.nlm.nih.gov/38023772/]
- 63. Effective strategies to eliminate mycoplasma contamination [https://www.news-medical.net/whitepaper/20241204/Effective-strategies-to-eliminate-mycoplasma-contamination-in-laboratory-incubators.aspx]
- 64. : Where Does It Come From and How to... Mycoplasma Contamination [https://blog.addgene.org/mycoplasma-contamination-where-does-it-come-from-and-how-to-prevent-it]
- 65. Mycoplasma Testing for Quality Control [https://www.atcc.org/microbe-products/applications/quality-control/mycoplasma-testing]
- 66. Mycoplasma Testing Market Outlook 2027 [https://www.pharmiweb.com/press-release/2025-11-19/mycoplasma-testing-market-outlook-2027-key-developments-and-future-scope]
- 67. Evaluation of mycoplasma removal reagents using qPCR ... [https://www.sciencedirect.com/science/article/abs/pii/S0003269718307036]
- 68. Molecular identification and antibiotic clearance of ... [https://pubmed.ncbi.nlm.nih.gov/39817787/]
- 69. Cleaning methods for biosafety cabinet to eliminate ... [https://www.sciencedirect.com/science/article/pii/S2352320424002128]
- 70. Prevent Research Setbacks with Effective Mycoplasma ... [https://www.labmanager.com/prevent-research-setbacks-with-effective-mycoplasma-screening-33285]
- 71. Comparative Assessment of Mycoplasma Elimination ... [https://www.randox-lifesciences.com/comparative-assessment-of-mycoplasma-elimination-approaches-in-cell-culture-focus-on-myco-off/]
- 72. Troubleshooting Common Cell Culture Contamination Issues [https://cellculturecompany.com/troubleshooting-common-cell-culture-contamination-issues/]
- 73. Comparison Mycoplasma test kits for cell culture (research to ... [https://incelligence.de/en/cell-culture/cell-culture-contamination/mycoplasma-test-kits]
- 74. Comparison of Five Commercial Molecular Assays for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9945500/]
- 75. Basics of Cell Culture Quality Control: Contamination [https://info.abmgood.com/cell-culture-quality-control-contamination]
- 76. Prevention of Contaminations in Cell Culture [https://ibidi.com/content/436-prevention-of-contaminations]
- 77. The costs of using unauthenticated, over-passaged cell lines [https://pubmed.ncbi.nlm.nih.gov/18072586/]
- 78. Cell Culture Contamination | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/biological-contamination.html]
- 79. CMC Regulatory Dossier Compliance: A GMP Requirement [https://www.propharmagroup.com/thought-leadership/cmc-regulatory-dossier-compliance-a-gmp-requirement]
- 80. Quality compliance in the development of cell-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4685435/]