Method Verification in Microbiology Labs: When and How to Ensure Regulatory Compliance
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on the critical requirements for method verification in microbiology laboratories.
Method Verification in Microbiology Labs: When and How to Ensure Regulatory Compliance
Abstract
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on the critical requirements for method verification in microbiology laboratories. It clarifies the foundational distinction between method validation and verification, detailing specific scenarios—such as implementing a new FDA-cleared test, testing new sample matrices, or meeting CLIA, ISO 15189, and cGMP standards—that mandate verification. The content offers a methodological framework for planning and executing verification studies, including key performance parameters like accuracy, precision, and reportable range. It further addresses troubleshooting common pitfalls, optimizing ongoing quality control, and understanding when full validation is necessary, empowering professionals to build robust, reliable, and compliant laboratory testing processes.
Verification vs. Validation: Defining the Foundation of Reliable Microbiology Testing
In the regulated environment of a microbiology laboratory, the terms "verification" and "validation" represent distinct but complementary processes essential for ensuring the reliability and accuracy of test methods. Understanding this distinction is not merely an academic exercise but a fundamental requirement for compliance with regulatory standards and for ensuring patient safety [1]. Within the context of microbiology research and drug development, these processes confirm that laboratory methods are fit for their intended purpose, whether for diagnosing infectious diseases, testing pharmaceutical products for microbial contamination, or characterizing complex microbial communities [2] [3].
This guide provides a detailed framework for differentiating method verification from validation, with a specific focus on the circumstances that necessitate verification within microbiology laboratory research. The clarification of these concepts is critical for researchers, scientists, and drug development professionals who must navigate the stringent requirements of regulatory bodies such as the FDA, CLIA, and international pharmacopeias [2] [1].
Core Definitions and Regulatory Context
Defining Verification and Validation
In laboratory practice, "verification" and "validation" are often used interchangeably, but they describe fundamentally different processes based on the origin and regulatory status of the method in question.
Verification is a process performed for unmodified, FDA-approved or cleared tests. It is a one-time study that demonstrates a test performs in line with the manufacturer's established performance characteristics when used as intended in the operator's specific environment [2]. In the pharmaceutical industry, method verification is defined as the ability to verify that a method can perform reliably and precisely for its intended purpose, often applied to compendial methods like USP chapters <61>, <62>, and <71> [1].
Validation, in contrast, establishes that an assay works as intended for non-FDA cleared tests. This applies to laboratory-developed tests (LDTs) and modified FDA-approved tests. Modifications can include using different specimen types, sample dilutions, or test parameters such as changing incubation times, any of which could affect the assay's performance and thus require full validation [2]. The United States Pharmacopeia (USP) Chapter <1225> defines validation as "a process by which it is established, through laboratory studies, that the performance characteristics of a method meet the requirements for its intended analytical applications" [1].
Regulatory Requirements and Guidance
Method verification is required by the Clinical Laboratory Improvement Amendments (CLIA) for all non-waived systems (tests of moderate or high complexity) before reporting patient results [2]. Regulatory agencies, including the Food and Drug Administration (FDA), Medicine and Healthcare Regulatory Agency (MHRA), and ICH, require these processes to ensure patient safety and result reliability [1].
Table 1: Regulatory Guidance Documents for Verification and Validation
| Document | Focus Area | Application |
|---|---|---|
| CLIA (42 CFR 493.1253) | Laboratory testing | Verification of non-waived systems [2] |
| USP <1225> | Compendial procedures | Validation of compendial procedures [1] |
| USP <1226> | Compendial procedures | Verification of compendial procedures [1] |
| USP <1223> | Microbiological methods | Validation of alternative microbiological methods [1] |
| ICH Q2(R2) | Analytical procedures | Validation of analytical methods [1] |
| EU 5.1.6 | Microbiological quality | Alternative methods for control of microbiological quality [1] |
When is Method Verification Required in Microbiology?
Method verification is a mandatory process in specific scenarios within the microbiology laboratory. The requirement is triggered by the introduction of a new test system or significant changes to existing systems.
Primary Scenarios Requiring Verification
Implementation of a New Unmodified FDA-Cleared Test: Before any patient results are reported, the laboratory must verify that the test performs as claimed by the manufacturer in their specific environment [2]. This is the most common scenario for verification in clinical microbiology laboratories.
Major Changes in Procedures or Instrument Relocation: Verification is required when there are significant changes to the testing environment or methodology that could impact performance, such as moving an instrument to a new location or making substantial changes to the testing process not classified as a modification requiring full validation [2].
The Lifecycle Perspective
Method verification is not a "one-and-done" activity. A vigilant oversight approach throughout a product's lifecycle is necessary. Re-verification or validation may be required when changes occur, including [1]:
- Formulation or concentration updates
- Material source changes
- Manufacturing process updates
- Manufacturing location changes
- Reagent changes due to vendor changes or discontinuation
- Implementation of modern microbiological methods to replace traditional ones
Key Performance Characteristics for Verification
For an unmodified FDA-approved test, CLIA regulations require laboratories to verify specific performance characteristics. The exact approach depends on whether the assay is qualitative, quantitative, or semi-quantitative, with qualitative and semi-quantitative being more common in microbiology labs [2].
Table 2: Verification Criteria for Qualitative/Semi-Quantitative Microbiology Assays
| Performance Characteristic | Minimum Sample Requirement | Sample Types | Calculation Method |
|---|---|---|---|
| Accuracy | 20 clinically relevant isolates | Combination of positive and negative samples; can include standards, controls, reference materials, proficiency tests, or de-identified clinical samples [2] | (Number of results in agreement / Total number of results) × 100 [2] |
| Precision | 2 positive and 2 negative samples tested in triplicate for 5 days by 2 operators | Controls or de-identified clinical samples [2] | (Number of results in agreement / Total number of results) × 100 [2] |
| Reportable Range | 3 samples | Known positives for qualitative assays; range of positives near upper and lower cutoff values for semi-quantitative assays [2] | Verify laboratory's established reportable result (e.g., Detected, Not detected) [2] |
| Reference Range | 20 isolates | De-identified clinical samples or reference samples known to be standard for the laboratory's patient population [2] | Verify expected result for a typical sample from the laboratory's patient population [2] |
The acceptance criteria for these performance characteristics should meet the stated claims of the manufacturer or what the CLIA director determines to be acceptable [2].
Experimental Design and Protocols for Verification
Creating a Verification Plan
A written verification plan, reviewed and signed off by the laboratory director, is essential before commencing the study. This plan should include [2]:
- Type of verification and purpose of the study
- Purpose of the test and method description
- Detailed study design including:
- Number and type(s) of samples
- Type of quality assurance and quality controls
- Number of replicates, days, and analysts
- Performance characteristics evaluated and acceptance criteria
- Materials, equipment, and resources needed
- Safety considerations
- Expected timeline for completion
Method-Specific Considerations
Microbiological methods present unique challenges for verification studies. For example, with antimicrobial susceptibility testing methods, knowing what organisms to use, how to interpret results, and what to consider when using non-FDA breakpoints with an FDA-cleared AST panel is not clearly defined [2]. This highlights the importance of leveraging resources such as clinical microbiologists and laboratory leaders who are specifically trained to oversee this process.
In microbiome research, methodological variations such as the choice of 16S rRNA hypervariable region for amplification, sequencing platform technology, and geographic location of sample sources can significantly impact results [3]. These factors must be considered when designing verification studies for microbiome methods.
Statistical Approaches for Verification Studies
Selecting appropriate statistical methods is crucial for accurate verification. Recent comparative studies have shown that simplified algebraic methods for estimating variability, while easy to use, can overestimate the contribution of between-strain and within-strain variability due to the propagation of experimental variability in nested experimental designs [4]. Mixed-effect models and multilevel Bayesian models provide more unbiased estimates for all levels of variability, though they come with higher complexity [4].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful verification studies require carefully selected materials and reagents. The following table outlines essential components for microbiology method verification studies.
Table 3: Essential Research Reagents and Materials for Microbiology Verification
| Reagent/Material | Function in Verification | Application Examples |
|---|---|---|
| Clinical Isolates | Serve as positive and negative controls for accuracy studies [2] | Verify detection of target microorganisms (e.g., MRSA, ESBL) |
| Reference Materials | Provide standardized samples with known characteristics [2] | ATCC strains for microbial identification verification |
| Proficiency Test Samples | External assessment of method performance [2] | CAP surveys for laboratory accreditation |
| De-identified Clinical Samples | Assess method performance with real patient specimens [2] | Verify recovery of pathogens from stool, respiratory, or blood samples |
| Quality Controls | Monitor precision and reproducibility [2] | Daily QC for automated identification and susceptibility systems |
| Culture Media | Support microbial growth for traditional methods [1] | Verification of media lots for growth promotion tests |
The distinction between verification and validation is fundamental to maintaining quality and compliance in microbiology laboratories. Verification is required when implementing unmodified FDA-cleared tests and ensures these tests perform as intended in your specific laboratory environment. Through careful planning, execution, and documentation of performance characteristics including accuracy, precision, reportable range, and reference range, laboratories can confidently implement methods that generate reliable results. As methodology in microbiology continues to evolve, with increasing implementation of modern molecular techniques and microbiome analyses, maintaining rigorous approaches to verification and validation becomes increasingly important for both patient safety and scientific progress.
In clinical microbiology and drug development, regulatory standards provide the essential framework for ensuring that diagnostic tests and products are safe, reliable, and effective. These regulations govern every stage of the testing lifecycle, from initial development and verification to ongoing clinical use. For researchers and scientists, understanding when method verification is required under these frameworks is fundamental to maintaining regulatory compliance and delivering high-quality patient care.
The Clinical Laboratory Improvement Amendments (CLIA) establish quality standards for all laboratory testing in the United States, while ISO 15189 specifies requirements for quality and competence in medical laboratories globally. The In Vitro Diagnostic Regulation (IVDR) creates a robust regulatory framework for in vitro diagnostic devices in the European Union, and Current Good Manufacturing Practice (cGMP) regulations ensure the quality of pharmaceutical products in the US. Navigating this complex regulatory landscape requires a clear understanding of the specific requirements for test verification and validation under each framework, particularly for microbiology tests which present unique challenges due to the complexity of biological systems and the critical importance of accurate antimicrobial susceptibility testing.
Core Regulatory Frameworks: Definitions and Applications
CLIA (Clinical Laboratory Improvement Amendments)
CLIA establishes quality standards for all laboratory testing in the United States to ensure the accuracy, reliability, and timeliness of patient test results. CLIA regulations apply to laboratory-developed tests (LDTs) and require that laboratories establish and verify performance specifications for all tests [5]. CLIA categorizes tests based on complexity (waived, moderate, or high complexity) and specifies that method verification is required for any non-waived system before reporting patient results [6]. This includes any new assay or equipment and when there are major changes in procedures or instrument relocation.
ISO 15189
ISO 15189 is an international standard that specifies requirements for quality and competence in medical laboratories. The standard was recently updated in 2022 and includes specific requirements for the verification and validation of examination processes [7]. Laboratories complying with ISO 15189:2012 may find that they largely comply with Annex I of the IVDR, though manufacturing processes required under IVDR Annex I are not covered by ISO 15189 alone [8]. This standard is particularly important for laboratories operating in international contexts or those seeking to demonstrate the highest levels of quality.
IVDR (In Vitro Diagnostic Regulation)
IVDR (EU 2017/746) is the European regulation governing in vitro diagnostic medical devices, with the goal of improving clinical safety and creating fair market access [8]. IVDR introduced a risk-based classification system with four classes (A, B, C, D) and requires more rigorous clinical evidence for devices [9]. Under IVDR, performance evaluation is a continuous process throughout the device lifecycle and must demonstrate scientific validity, analytical performance, and clinical performance [9]. For in-house devices (also known as LDTs), IVDR Article 5.5 imposes specific constraints, including the requirement for appropriate quality management systems and justification for use over commercially available tests [8].
cGMP (Current Good Manufacturing Practice)
cGMP regulations, enforced by the FDA, contain minimum requirements for the methods, facilities, and controls used in manufacturing, processing, and packing of drug products [10]. These regulations ensure that a product is safe for use and that it has the ingredients and strength it claims to have. The CGMP regulations for drugs are primarily outlined in 21 CFR Parts 210 and 211 [10]. For pharmaceutical manufacturers, compliance with cGMP is essential for drug approval and marketing.
Table 1: Comparison of Key Regulatory Frameworks
| Framework | Jurisdiction/Scope | Primary Focus | Key Verification/Validation Requirements |
|---|---|---|---|
| CLIA | United States; Clinical laboratory testing | Laboratory testing accuracy and reliability | Verification of accuracy, precision, reportable range, and reference range for non-waived tests [6] |
| ISO 15189 | International; Medical laboratories | Quality management and technical competence | Validation and verification procedures for examination processes [7] |
| IVDR | European Union; In vitro diagnostic devices | Device safety and performance throughout lifecycle | Performance evaluation including scientific validity, analytical performance, and clinical performance [9] |
| cGMP | United States; Drug manufacturing | Pharmaceutical product quality and consistency | Manufacturing process controls, quality standards, and documentation [10] |
When is Method Verification Required?
Method verification is a foundational requirement across regulatory frameworks to ensure tests perform as expected in your specific laboratory environment. The specific triggers for verification depend on the test type and regulatory context.
Verification vs. Validation: A Critical Distinction
Understanding the distinction between verification and validation is essential for proper regulatory compliance:
Verification is a one-time study for unmodified FDA-cleared or approved tests meant to demonstrate that a test performs in line with previously established performance characteristics when used as intended by the manufacturer [6]. It confirms that test performance specifications are met in the user's environment.
Validation is a more extensive process meant to establish that an assay works as intended. This applies to non-FDA cleared tests (e.g., laboratory-developed tests) and modified FDA-approved tests [6]. Validation is also an ongoing process to monitor and ensure that the test continues to perform as expected throughout its use [5].
Specific Triggers for Method Verification
Method verification is required in the following circumstances:
Implementation of new unmodified FDA-cleared tests: Before reporting patient results, laboratories must verify that the manufacturer's performance claims are met in their hands [6].
Major changes to existing procedures: This includes instrument relocation, significant reagent lot changes, or updates to software that could affect test performance [6].
For IVDR compliance: Verification is needed when implementing CE-marked in vitro diagnostic devices to ensure performance in your specific laboratory environment [7].
When modifying FDA-approved tests: Any changes to the assay not specified as acceptable by the manufacturer (e.g., different specimen types, sample dilutions, or test parameters) require validation before implementation [6].
For microbiology tests specifically, verification and validation procedures must be tailored to account for the complexity of biological systems, the diversity of microorganisms, and the critical importance of antimicrobial susceptibility testing [7] [6].
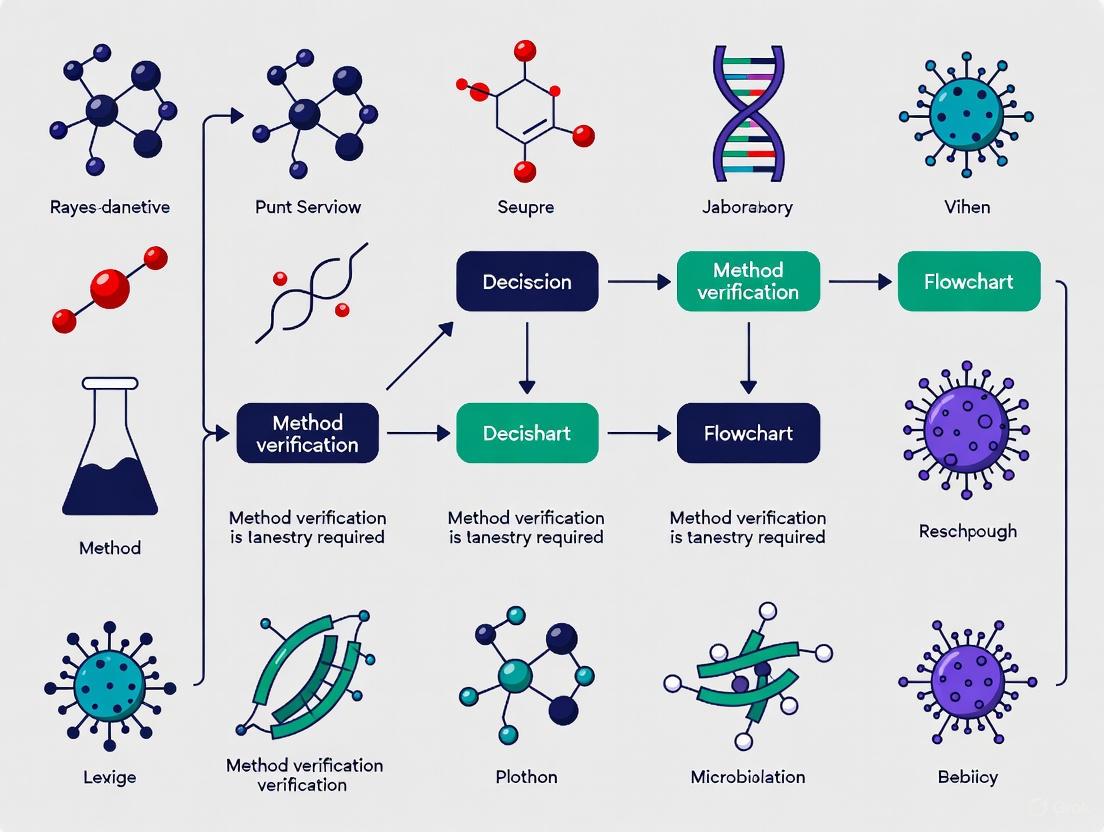
Diagram 1: Method Verification Decision Pathway
Experimental Design for Method Verification
Core Performance Characteristics
When designing a verification study for a clinical microbiology test, specific performance characteristics must be evaluated based on regulatory requirements. For qualitative and semi-quantitative assays commonly used in microbiology, the following criteria must be verified:
Accuracy: Confirm the acceptable agreement of results between the new method and a comparative method [6]. For qualitative assays, use a combination of positive and negative samples. A minimum of 20 clinically relevant isolates is recommended [6].
Precision: Confirm acceptable within-run, between-run and operator variance [6]. Test a minimum of 2 positive and 2 negative samples in triplicate for 5 days by 2 operators. For fully automated systems, user variance assessment may not be needed [6].
Reportable Range: Confirm the acceptable upper and lower limit of the test system [6]. For qualitative assays, verify with known positive samples for the detected analyte. A minimum of 3 samples is recommended.
Reference Range: Confirm the normal result for the tested patient population [6]. Use a minimum of 20 isolates, including de-identified clinical samples or reference samples with results known to be standard for the laboratory's patient population.
Table 2: Verification Study Design Parameters for Microbiology Tests
| Performance Characteristic | Minimum Sample Size | Sample Types | Testing Protocol | Acceptance Criteria |
|---|---|---|---|---|
| Accuracy | 20 clinically relevant isolates [6] | Combination of positive and negative samples; may include standards, controls, reference materials, proficiency tests, or de-identified clinical samples [6] | Comparison between new method and reference method | Percentage of agreement should meet manufacturer's stated claims or laboratory director's determination [6] |
| Precision | 2 positive and 2 negative samples [6] | Controls or de-identified clinical samples with high to low values for semi-quantitative assays [6] | Tested in triplicate for 5 days by 2 operators [6] | Percentage of results in agreement should meet manufacturer's claims [6] |
| Reportable Range | 3 samples [6] | Known positive samples for qualitative assays; range of positive samples near cutoffs for semi-quantitative assays [6] | Testing samples that fall within the reportable range | Laboratory establishes reportable result parameters (e.g., "Detected", "Not detected") [6] |
| Reference Range | 20 isolates [6] | De-identified clinical samples or reference samples representative of laboratory's patient population [6] | Testing samples representative of laboratory's patient population | Expected result for a typical sample in laboratory's patient population [6] |
Creating a Verification Plan
A comprehensive verification plan should be documented and signed off by the laboratory director before commencing the study. This plan should include [6]:
- Type of verification and purpose of study: Clearly state whether the study is for verification or validation and the regulatory basis.
- Purpose of test and method description: Detail the intended use of the test and a complete description of the methodology.
- Study design specifics: Include the number and type of samples, quality assurance and quality control procedures, number of replicates, days of testing, number of analysts, and performance characteristics to be evaluated.
- Materials and equipment: List all required resources for the study.
- Safety considerations: Address any biosafety requirements for handling microbiology specimens.
- Timeline for completion: Establish realistic timeframes for completing the verification study.
Special Considerations for Microbiology Testing
Antimicrobial Susceptibility Testing (AST)
Verification of antimicrobial susceptibility testing methods presents unique challenges due to the biological variability of microorganisms and the critical importance of accurate results for patient care. When verifying AST methods, particular attention should be paid to [7]:
- Selection of appropriate reference strains that represent the expected susceptibility profiles
- Inclusion of resistant, intermediate, and susceptible isolates to challenge the system
- Comparison with reference methods such as broth microdilution
- Careful interpretation of results when using non-FDA breakpoints with an FDA-cleared AST panel
Molecular Microbiology Assays
For molecular tests such as PCR-based methods, verification must include assessment of [5]:
- Analytical sensitivity (limit of detection) for each target
- Analytical specificity, including cross-reactivity with genetically similar organisms
- Inhibition controls and their effectiveness
- Specimen stability and nucleic acid extraction efficiency
Laboratory-Developed Tests (LDTs) and IVDR Compliance
For laboratories developing their own tests, the regulatory requirements are more extensive. Under IVDR, in-house devices must comply with specific requirements including [8]:
- The devices must not be transferred to another legal entity
- Implementation of appropriate quality management systems (e.g., ISO 15189)
- The product may not be made on an industrial scale
- Documentation justifying why an equivalent commercially available device is not used
The timeline for IVDR compliance for in-house devices is progressive, with full justification for use over commercially available tests required by May 2028 [8].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagent Solutions for Microbiology Verification Studies
| Reagent/Resource | Function in Verification/Validation | Regulatory Considerations |
|---|---|---|
| Reference Strains | Provide quality control organisms with known characteristics for accuracy and precision studies [6] | Must be traceable to recognized collections (e.g., ATCC, NCTC) |
| Clinical Isolates | Challenge the test with real-world samples representing the laboratory's patient population [6] | Should be de-identified and used in accordance with ethical guidelines |
| Quality Control Materials | Monitor assay performance during verification and ongoing quality assurance [5] | Should include positive, negative, and internal controls as appropriate |
| Analyte-Specific Reagents (ASRs) | Building blocks for laboratory-developed tests; primers, probes, antibodies [5] | FDA-defined category; laboratories using ASRs assume responsibility for test validation |
| Proficiency Testing Samples | Assess test performance through external quality assessment programs [5] | CLIA requires participation for regulated analyses |
| Reference Standards | Serve as comparator for method comparison studies [7] | Should represent the current gold standard or reference method |
The regulatory landscape encompassing CLIA, ISO 15189, IVDR, and cGMP presents a complex but essential framework for ensuring the quality and reliability of microbiology tests in both clinical and research settings. Method verification serves as a critical bridge between regulatory requirements and practical laboratory implementation, with specific triggers and protocols depending on the test type and regulatory jurisdiction.
As regulations continue to evolve, particularly with the full implementation of IVDR and updates to ISO standards, microbiology laboratories must maintain vigilant compliance with verification and validation requirements. By understanding the distinct requirements of each regulatory framework and implementing robust verification protocols, researchers and laboratory professionals can ensure the generation of reliable, reproducible data that advances both patient care and drug development.
In the regulated environment of a microbiology laboratory, method verification is not merely a best practice but a fundamental requirement to ensure the reliability, accuracy, and precision of test results. It serves as a critical demonstration that a laboratory can competently perform a previously validated method under its specific conditions, using its unique analysts and equipment. The triggers for method verification are bound by a complex framework of legal mandates, technical necessities, and regulatory expectations that vary across industries and jurisdictions. A failure to perform verification when required can have severe consequences, including regulatory citations, product recalls, and, most importantly, compromises to product safety and patient health. This guide provides an in-depth examination of the specific situations that legally and technically necessitate method verification, offering a structured framework for researchers, scientists, and drug development professionals to ensure compliance and uphold the highest standards of data integrity.
Distinguishing Between Verification and Validation
A foundational step in understanding the requirements is to clearly distinguish between method verification and method validation. These terms are often incorrectly used interchangeably, yet they describe two distinct processes with different objectives and regulatory implications.
Method Validation is the process of establishing, through extensive laboratory studies, that the performance characteristics of an analytical method are suitable for its intended analytical purpose. It is the initial demonstration that a method works. Validation is required for non-FDA cleared methods, such as laboratory-developed tests (LDTs) or modified FDA-approved methods [2]. The core parameters established during validation, as outlined in guidelines like ICH Q2(R2), include specificity, accuracy, precision, linearity, range, detection limit, and quantitation limit [11] [12].
Method Verification, in contrast, is the one-time study meant to demonstrate that a pre-validated or FDA-approved method performs in line with its previously established performance characteristics when it is introduced into a laboratory for the first time and used as intended by the manufacturer [2]. It is the process of confirming a method's performance in a user's hands.
The table below summarizes the key differences:
Table 1: Core Differences Between Method Validation and Verification
| Aspect | Method Validation | Method Verification |
|---|---|---|
| Objective | To establish method performance characteristics for a new method [11]. | To confirm a laboratory can achieve the method's validated performance claims [2] [13]. |
| When Performed | For new, non-cleared, or significantly modified methods [2]. | When implementing a previously validated method in a new laboratory [13]. |
| Regulatory Focus | ICH Q2(R2), FDA for LDTs [11] [12]. | CLIA for clinical labs; FDA for compendial methods (e.g., USP) [2] [14] [11]. |
| Scope of Work | Extensive testing of all performance parameters [11]. | Limited testing of key parameters like accuracy and precision for the lab's specific use [2]. |
Legal and Regulatory Triggers for Method Verification
Legal and regulatory requirements are the most unambiguous triggers for method verification. Compliance is not optional, and these mandates are enforced through routine inspections by agencies such as the FDA, CMS, and accreditation bodies.
Implementing a New FDA-Cleared or Approved Method
In clinical diagnostics, the Clinical Laboratory Improvement Amendments (CLIA) explicitly require that for any unmodified, FDA-cleared or approved test system of moderate or high complexity, the laboratory must perform method verification before reporting patient results [2]. This is a legal requirement under 42 CFR 493.1253. The verification must demonstrate that the test's performance specifications, as claimed by the manufacturer, can be met by the laboratory.
Using Compendial Methods for Pharmaceutical Products
For pharmaceutical quality control, the U.S. Food and Drug Administration (FDA) mandates verification for compendial methods. As stated in the FDA guidance "Analytical Procedures and Methods Validation for Drugs and Biologics," a laboratory does not need to re-validate a method from an FDA-recognized source like the United States Pharmacopeia (USP). Instead, it must verify that the method is suitable for use under the actual conditions of use [14] [11]. Recent FDA inspections have shown a "hyper-focus" on this requirement, with inspectors specifically requesting product-specific reports proving that methods, including USP monographs, have been verified [14]. The verification must comply with general chapters such as USP <1226> "Verification of Compendial Procedures" [14].
Adhering to International Standards for Food and Feed Testing
For food and feed testing laboratories, the ISO 16140 series provides the standard for microbiological method validation and verification. According to ISO 16140-3, a laboratory must perform verification to demonstrate it can satisfactorily perform a method that has been validated through an interlaboratory study [13]. This process often involves two stages: implementation verification (proving the lab can perform the method correctly on a known item) and item verification (proving the method works for the specific food items tested by the lab) [13].
Technical and Operational Triggers for Method Verification
Beyond explicit regulatory mandates, several technical and operational changes within a laboratory trigger the need for verification to ensure ongoing data integrity.
Changes in Laboratory Infrastructure or Equipment
Significant changes to the laboratory environment that could affect analytical performance necessitate re-verification or partial verification. This includes:
- Introduction of new instrumentation of the same type and model. While a full IOPQ (Installation, Operational, and Performance Qualification) is required for equipment under cGMP [15], a method verification is still needed to confirm the method performs as expected on the new instrument.
- Relocation of the testing system to a new laboratory with different environmental conditions (e.g., temperature, humidity).
- Changes to critical software or the Laboratory Information Management System (LIMS) that processes analytical data [15].
Changes in Reagents or Critical Materials
A change in the source of a critical reagent, such as culture media, antisera, or key biochemical substrates, requires verification to confirm that the new material produces results equivalent to those obtained with the original material. This ensures the method's specificity and accuracy are not compromised.
Changes in Analyst Personnel
While routine analyst training is part of quality control, a significant turnover in staff or the introduction of the method to a new group of analysts may trigger a limited verification to ensure that the new personnel can execute the method with the same level of precision and accuracy as demonstrated in the original verification study.
Experimental Protocols for Method Verification
The design of a verification study depends on whether the method is qualitative or quantitative. The following protocols, aligned with CLSI and ISO standards, provide a framework for a robust verification plan.
Verification of Qualitative Methods
Qualitative methods provide a binary result (e.g., detected/not detected, present/absent). The following table outlines the key performance characteristics to verify for a qualitative microbiological assay, such as a PCR test for a specific pathogen or a sterility test.
Table 2: Verification Protocol for Qualitative Microbiological Methods
| Performance Characteristic | Experimental Protocol & Minimum Sample Sizes | Acceptance Criteria |
|---|---|---|
| Accuracy | Test a minimum of 20 clinically relevant isolates or samples with a combination of known positive and negative status [2]. Use reference materials, proficiency test samples, or de-identified clinical samples previously tested with a validated method. | The percentage of agreement should meet the manufacturer's stated claims or a lab-director-defined threshold (e.g., ≥95%) [2]. |
| Precision | Test a minimum of 2 positive and 2 negative samples in triplicate over 5 days by 2 different operators [2]. For fully automated systems, operator variance may not be needed. | Results should be 100% reproducible for each sample type, or meet a predefined percentage agreement. |
| Reportable Range | Verify using a minimum of 3 known positive samples for the detected analyte [2]. | The method should correctly identify all positive samples as "detected." |
| Reference Range | Verify using a minimum of 20 isolates or samples that represent the standard result for the laboratory's patient population (e.g., samples negative for the target organism) [2]. | The method should correctly identify all negative samples as "not detected." |
Verification of Quantitative Methods
Quantitative methods provide a numerical value (e.g., microbial colony counts, CFU/mL). The verification of a method like microbial enumeration (as per USP <61>) would focus on different parameters.
Table 3: Key Verification Parameters for Quantitative Microbiological Methods
| Performance Characteristic | Experimental Protocol | Acceptance Criteria |
|---|---|---|
| Accuracy | Analyze a certified reference material (CRM) with a known microbial count. Compare the mean result from multiple replicates to the certified value. | Recovery should be within the certified range or meet predefined limits (e.g., 70-130%). |
| Precision | Perform multiple replicates (e.g., n=6) of the same sample in the same run (repeatability) and across different days/analysts (intermediate precision). | The relative standard deviation (RSD) should be within the manufacturer's claims or a predefined limit (e.g., <15-20% for HPLC, adapted for microbiology) [16]. |
| Linearity & Range | Test a dilution series of a microbial suspension across the claimed reportable range of the method. | The method's response should be linear across the range, with an R² value of >0.98, for example. |
| Specificity | Challenge the method with closely related species or strains to ensure it accurately quantifies the target microorganism without interference. | The method should correctly identify and quantify the target organism without significant interference. |
The Verification Workflow
The following diagram illustrates the logical sequence of activities in a comprehensive method verification process, from planning to final implementation.
The Scientist's Toolkit: Essential Reagents and Materials
A successful verification study relies on high-quality, traceable materials. The following table details key reagent solutions and their critical functions in the verification process.
Table 4: Essential Research Reagent Solutions for Method Verification
| Reagent / Material | Function in Verification |
|---|---|
| Certified Reference Materials (CRMs) | Well-characterized microorganisms with defined profiles and known counts; used as the gold standard for establishing accuracy and precision [17]. |
| Quality Control Organisms | Used to monitor test validity, verify instrument performance, and serve as positive and negative controls during verification runs [17]. |
| Proficiency Test (PT) Samples | Blinded samples of known content provided by an external program; used to independently verify a laboratory's competency and the accuracy of its methods [17]. |
| In-House Isolates | Well-characterized strains isolated from the laboratory's own environment or historical samples; used to challenge the method's specificity and ensure it is relevant to the lab's specific testing needs [17]. |
| Standardized Culture Media | Verified for growth promotion properties using specific QC strains; ensures the medium supports the growth of target microorganisms, a critical factor in method accuracy [17]. |
Consequences of Non-Compliance
Failing to perform required method verification carries significant risks. Regulatory bodies like the FDA can issue Form 483 observations during inspections, demanding immediate corrective actions. For clinical laboratories, CMS can revoke CLIA certification, halting all patient testing [2]. Beyond compliance, the technical risks are profound: inaccurate test results can lead to flawed scientific conclusions, release of unsafe products, misdiagnosis of patients, and ultimately, harm to public health and the company's reputation [17]. The financial impact of investigating and correcting errors, repeating studies, and potential litigation can be substantial.
Method verification is a non-negotiable pillar of quality assurance in the microbiology laboratory. The triggers are clear: the legal mandates of CLIA for clinical labs, the FDA's requirements for compendial methods, and the technical necessities driven by changes in equipment, reagents, or personnel. By understanding these triggers and implementing a structured, protocol-driven verification process, laboratories can confidently ensure their methods are fit-for-purpose, their data is reliable, and their operations remain in a state of regulatory compliance. A proactive approach to verification is not just a regulatory hurdle but a fundamental component of scientific excellence and patient safety.
In microbiology laboratory research, the accurate classification of testing methods is a fundamental prerequisite for determining when and how method verification is required. Assays are broadly categorized as qualitative, quantitative, or semi-quantitative, each with distinct purposes, performance characteristics, and verification protocols [6]. Understanding these categories is critical for researchers and drug development professionals because the category dictates the validation and verification pathway a method must undergo before implementation [13].
The principles of method validation and verification are codified in standards such as the ISO 16140 series for the food chain and guidelines from bodies like the Clinical and Laboratory Standards Institute (CLSI) for clinical microbiology [13] [6]. Validation establishes that a method is fit for its intended purpose, while verification is the process by which a laboratory demonstrates that it can successfully perform a previously validated method [13] [6]. This distinction is crucial for regulatory compliance and ensuring the reliability of data in both research and diagnostic settings.
Defining the Core Assay Categories
Qualitative Assays
Qualitative methods are designed to detect the presence or absence of a specific microorganism or microbial component in a sample, providing a binary result [18] [6]. These methods do not determine the quantity of the organism present. They are typically used for detecting pathogens like Listeria monocytogenes, Salmonella, and Escherichia coli O157:H7, where even very low levels (e.g., 1 CFU) in a large sample portion (e.g., 25g to 375g) are significant [18].
A key feature of most qualitative methods is an amplification step, such as enrichment, to increase the target microorganism to a detectable level [18]. This step breaks the direct link to the initial concentration in the sample. Results are reported as "Detected or Not Detected" or "Positive or Negative" per the tested weight or volume (e.g., Not detected/25 g) [18].
Quantitative Assays
Quantitative methods measure the numerical concentration of specified microorganisms in a sample, reported as colony-forming units (CFU) or most probable number (MPN) per unit of weight or volume (e.g., CFU/g) [18]. These methods are essential for enumerating microbial indicators (e.g., aerobic plate count, Enterobacteriaceae) or specific organisms like Staphylococcus aureus [18].
These methods require careful serial dilution to achieve a countable range of colonies on an agar plate (e.g., 25-250 colonies) for accurate measurement [18]. The limit of detection (LOD) for quantitative plate count methods is typically 10 or 100 CFU/g, while MPN methods have an LOD of around 3 MPN/g [18]. If no target organisms are detected, the result is reported as "less than" the LOD (e.g., <10 CFU/g), which is not equivalent to a qualitative "Negative" result [18].
Semi-Quantitative Assays
Semi-quantitative methods occupy a middle ground, providing results on an ordinal scale rather than a precise numerical value [19]. These assays use numerical values or signals to determine a cutoff but report a qualitative or categorized result (e.g., "small," "moderate," "large" or a cycle threshold (Ct) value from PCR) [6] [19].
From a metrological perspective, semi-quantitative results can be ranked, but the units are not necessarily identical across the entire measuring interval [19]. These methods are often considered to have less-than-optimal quality indicators for trueness and precision compared to fully quantitative methods but offer more information than purely qualitative tests [19]. They communicate that the measurement has an inherent uncertainty while still providing a useful scale for interpretation.
Table 1: Core Characteristics of Microbiological Assay Categories
| Characteristic | Qualitative Assays | Quantitative Assays | Semi-Quantitative Assays |
|---|---|---|---|
| Primary Objective | Detection/identification | Enumeration | Relative estimation/categorization |
| Result Type | Binary (e.g., Positive/Negative) | Numerical (e.g., CFU/g) | Ordinal/Categorical (e.g., 1+, 2+, 3+) |
| Data Scale | Nominal [19] | Ratio [19] | Ordinal [19] |
| Key Performance Characteristics | Accuracy, Specificity [6] | Precision, Reportable Range [6] | Cut-off determination, Categorization accuracy [6] |
| Typical LOD | 1 CFU/test portion [18] | 10-100 CFU/g (plate count); 3 MPN/g (MPN) [18] | Varies, based on cut-off |
| Common Examples | Pathogen screening (e.g., Salmonella) [18] | Aerobic plate count, indicator organisms [18] | Some PCR assays with Ct values, antigen tests with graded results [6] |
Method Verification Protocols and Requirements
The Verification Mandate in Regulated Laboratories
Method verification is a mandatory requirement in regulated laboratory environments before reporting patient or research results. The Clinical Laboratory Improvement Amendments (CLIA) in the United States requires verification for all non-waived test systems of moderate or high complexity [6]. This process is distinct from validation: verification confirms that a pre-validated, unmodified FDA-cleared or approved method performs according to manufacturer claims in the user's laboratory, while validation establishes method performance for laboratory-developed tests or significantly modified FDA-approved methods [6].
In the food testing sector, the ISO 16140 series provides a structured framework for method verification, delineating it as the second essential stage after method validation [13]. According to ISO 16140-3, verification involves two stages: implementation verification (demonstrating the laboratory can correctly perform the method using items from the validation study) and item verification (demonstrating competency with challenging items specific to the laboratory's scope) [13].
Category-Specific Verification Criteria
The verification requirements differ significantly based on the assay category. The table below summarizes the core verification criteria for each category as guided by CLSI standards.
Table 2: Verification Criteria by Assay Category
| Verification Characteristic | Qualitative Assays | Quantitative Assays | Semi-Quantitative Assays |
|---|---|---|---|
| Accuracy | ≥20 positive/negative samples; calculate % agreement [6] | Statistical comparison of means against reference method | Similar to qualitative, but with samples spanning reportable categories |
| Precision | 2 positive & 2 negative samples in triplicate for 5 days by 2 operators [6] | Within-run, between-run, and between-operator variance | Assess reproducibility of categorical assignments across runs and operators |
| Reportable Range | 3 known positive samples [6] | Verification of upper and lower limits of quantification | Verification of cut-off values and categorical boundaries [6] |
| Reference Range | ≥20 samples representing "normal" population [6] | Establish normal values for patient population | Verify categorical distributions match expected population patterns |
Experimental Design for Verification Studies
Designing a robust verification study requires careful planning. The first step is creating a verification plan that includes the type and purpose of the study, test method description, detailed study design (number/type of samples, replicates, operators), performance characteristics to be evaluated with acceptance criteria, required materials, and a timeline [6].
For qualitative and semi-quantitative assays common in microbiology, acceptable samples for verification can include reference materials, proficiency test samples, de-identified clinical samples previously tested with a validated method, or well-characterized isolates [6]. The number of samples should be sufficient to provide statistical confidence, with a minimum of 20 samples recommended for accuracy assessment [6].
For quantitative methods, precision is typically evaluated through repeated testing of samples across multiple days and by different operators to establish reproducibility. The reportable range must be verified by testing samples at both the upper and lower limits of quantification to ensure linearity and recovery throughout the measuring interval.
Decision Framework and Practical Implementation
Selection Criteria and Verification Workflow
Choosing between qualitative, quantitative, or semi-quantitative methods depends entirely on the research or testing objective. A qualitative method is appropriate when the goal is to detect the presence of a specific microorganism, particularly pathogens, even at very low levels [18]. A quantitative method is necessary when the numerical concentration of microorganisms is critical, such as in potency assays or when monitoring microbial loads [18]. Semi-quantitative methods are useful when relative abundance or categorization within ranges provides sufficient information for decision-making.
The following workflow diagram illustrates the decision process for selecting and verifying microbiological methods:
Essential Research Reagents and Materials
Successful method verification requires specific, high-quality reagents and materials. The following table details essential solutions and their functions in verification studies.
Table 3: Key Research Reagent Solutions for Method Verification
| Reagent/Material | Function in Verification | Application Across Categories |
|---|---|---|
| Reference Materials | Provide ground truth for accuracy assessment; characterized samples with known properties [6] | Qualitative, Quantitative, Semi-Quantitative |
| Proficiency Test Samples | External quality assessment; independently characterized samples [6] | Qualitative, Quantitative, Semi-Quantitative |
| Quality Controls (Positive/Negative) | Monitor assay performance; verify proper function of test system [6] | Qualitative, Quantitative, Semi-Quantitative |
| Well-Characterized Isolates | Assess accuracy and specificity; verify identification capabilities [6] | Qualitative, Semi-Quantitative |
| Serial Dilution Materials | Establish countable range; perform quantitative measurements [18] | Primarily Quantitative |
| Selective and Differential Media | Isolate and identify target microorganisms; confirm cultural characteristics [18] | Qualitative, Quantitative |
The distinction between qualitative, quantitative, and semi-quantitative assays is fundamental to microbiology laboratory research and directly determines when and how method verification is required. As outlined in this guide, each category has distinct purposes, performance characteristics, and verification protocols mandated by regulatory frameworks and international standards.
Method verification is not a one-size-fits-all process but must be tailored to the specific assay category and intended use. By following the structured approaches, experimental protocols, and decision frameworks presented here, researchers and drug development professionals can ensure their microbiological methods are properly verified, compliant with regulatory requirements, and capable of generating reliable, reproducible data for both research and clinical applications.
Executing Method Verification: A Step-by-Step Protocol for Microbiology Labs
In microbiology laboratory research, method verification is a fundamental process required to demonstrate that a laboratory can successfully perform a pre-validated, standardized method before using it for routine testing [13]. It is a critical checkpoint within a broader quality management system, confirming that a method's established performance characteristics can be reproduced in a specific laboratory's environment, with its specific personnel and equipment. Understanding when verification is required—as opposed to the more extensive process of method validation—is essential for regulatory compliance, data integrity, and patient safety in drug development.
The terms verification and validation are often used interchangeably, but they describe distinct activities [2]. A validation is a comprehensive process that establishes that an assay works as intended; this is required for non-FDA-cleared tests, such as laboratory-developed methods (LDM) or modified FDA-approved tests [2]. In contrast, a verification is a one-time study for unmodified, FDA-approved or cleared tests, demonstrating that the test performs in line with the manufacturer's established performance characteristics when used as intended in the user's specific environment [2]. According to the ISO 16140 series, verification consists of two stages: implementation verification (demonstrating the lab can perform the method correctly) and (food) item verification (demonstrating the method works for specific sample types within the lab's scope) [13]. For clinical laboratories, verification is mandated by the Clinical Laboratory Improvement Amendments (CLIA) for all non-waived testing systems before patient results can be reported [2].
Core Components of a Microbiology Verification Plan
A well-structured verification plan serves as the blueprint for the entire study. This pre-approved document details the what, how, and when of the verification activity, ensuring it is executed systematically and meets all regulatory requirements. The essential components of this plan are detailed below.
Statement of Purpose and Test Definition
The plan must begin with a clear statement of its purpose and a detailed description of the test method. This section should explicitly state whether the activity is a verification or a validation, define the intended use of the test, and describe the methodological principle [2]. For a verification, this includes confirming that the method is unmodified and FDA-approved or cleared. It should also specify the type of assay—qualitative (providing a binary result such as "detected/not detected"), quantitative (providing a numerical value), or semi-quantitative (using a numerical cutoff to determine a qualitative result) [2]. This clarity sets the scope and regulatory basis for all subsequent activities.
Detailed Study Design and Experimental Protocols
The study design is the technical core of the plan, specifying the performance characteristics to be evaluated, the acceptance criteria, and the experimental methodology for each. For an unmodified FDA-approved test, CLIA requires verification of accuracy, precision, reportable range, and reference range [2]. The following sections provide detailed experimental protocols for these key characteristics in the context of qualitative and semi-quantitative microbiology assays.
Verification of Accuracy
Accuracy confirms the acceptable agreement of results between the new method and a comparative method [2].
- Experimental Protocol: Use a minimum of 20 clinically relevant isolates or samples [2]. For qualitative assays, use a combination of positive and negative samples. For semi-quantitative assays, use a range of samples with high to low values. Acceptable specimens can include certified reference materials, proficiency test samples, or de-identified clinical samples previously characterized by a validated method [2]. Test all samples using the new method and compare the results to those obtained from the comparative method.
- Calculation and Acceptance Criteria: Calculate accuracy as the number of results in agreement divided by the total number of results, multiplied by 100. The acceptable percentage of accuracy should meet the manufacturer's stated claims or a level determined by the Laboratory Director [2].
Verification of Precision
Precision confirms acceptable variance within a run, between runs, and between different operators [2].
- Experimental Protocol: Use a minimum of two positive and two negative samples, tested in triplicate over five days by two different operators [2]. If the system is fully automated, testing for user variance may not be required. The samples can be controls or de-identified clinical samples.
- Calculation and Acceptance Criteria: Calculate precision for each level of testing (e.g., within-run, between-day, between-operator) as the number of results in agreement divided by the total number of results, multiplied by 100. The acceptance criteria should align with the manufacturer's claims or the Laboratory Director's specifications [2].
Verification of Reportable Range
The reportable range confirms the acceptable upper and lower limits of the test system [2].
- Experimental Protocol: Verify using a minimum of three samples [2]. For qualitative assays, use known positive samples. For semi-quantitative assays, use a range of positive samples near the upper and lower ends of the manufacturer-determined cutoff values.
- Evaluation: The reportable range is defined as what the laboratory establishes as a reportable result (e.g., "Detected," "Not detected," or a specific cycle threshold (Ct) value cutoff). Verification involves testing samples to confirm they fall within and are correctly reported across this defined range [2].
Verification of Reference Range
The reference range confirms the normal expected result for the tested patient population [2].
- Experimental Protocol: Verify using a minimum of 20 isolates [2]. Use de-identified clinical samples or reference samples with a result known to be standard for the laboratory’s patient population (e.g., samples negative for MRSA for an MRSA detection assay).
- Evaluation: The reference range is verified by testing samples representative of the laboratory's patient population. If the manufacturer's reference range does not represent this population, the laboratory must screen additional samples and potentially redefine the reference range [2].
Materials, Equipment, and Resource Requirements
This section provides a comprehensive list of all resources required to execute the verification study. This includes specific materials, validated equipment, and other critical resources.
- Research Reagent Solutions: The plan must catalog all critical reagents, their sources (e.g., certified reference materials, proficiency test samples, commercially prepared media), and quality control requirements (e.g., growth promotion testing for media, certificate of analysis review) [2] [20].
- Validated Equipment and Systems: All equipment used in the verification—such as incubators, pipettes, centrifuges, PCR systems, and the Laboratory Information Management System (LIMS)—must be listed. The plan should reference their current Installation, Operational, and Performance Qualification (IOPQ) status, which is a non-negotiable requirement for cGMP testing and strongly recommended for all clinical labs [15] [20]. IOPQ ensures equipment is installed correctly, operates according to specifications, and performs consistently under real-world conditions [15].
Table: Essential Research Reagent Solutions and Materials for Microbiological Verification
| Item Category | Specific Examples | Function in Verification |
|---|---|---|
| Reference Microorganisms | ATCC strains; certified reference materials from national collections [20] | Serves as positive controls and challenge organisms for accuracy, precision, and specificity testing. |
| Culture Media | Tryptic Soy Agar (TSA); Mueller Hinton Broth; Selective and differential agars [20] | Supports microbial growth for testing; quality is verified through growth promotion and sterility checks. |
| Clinical Isolates & Samples | De-identified patient samples; proficiency test samples; contrived samples [2] | Provides a clinically relevant matrix for verifying method performance against a comparative method. |
| Molecular Biology Reagents | PCR master mixes; primers and probes; DNA extraction kits [2] | Essential for molecular methods like real-time PCR for pathogen detection and identification. |
Safety Considerations and Project Timeline
The verification plan must explicitly address laboratory safety protocols for handling biological specimens, chemical hazards, and any other potential risks. This includes requirements for personal protective equipment (PPE), biosafety levels, and waste disposal procedures [2].
Finally, the plan should outline a realistic timeline for completion, including key milestones for each phase of the verification (e.g., protocol finalization, sample acquisition, testing phase, data analysis, and report writing). This facilitates project management and ensures timely implementation of the new method.
The Verification Workflow and Director Approval
The entire verification process, from planning to final approval, follows a logical sequence of activities with the Laboratory Director's oversight as a constant thread. The following diagram visualizes this workflow and the critical approval gates.
Diagram: Microbiology Method Verification and Approval Workflow
The Role of the Laboratory Director
The Laboratory Director's role is paramount throughout the verification process. As highlighted in the workflow, the Director holds ultimate responsibility for reviewing and signing off on the verification plan before any testing begins [2]. This review ensures the study design is scientifically sound, addresses all required performance characteristics, and has appropriate acceptance criteria. Furthermore, after the study is executed and a final report is compiled, the Director must provide final approval, confirming that the data demonstrate the method is acceptable for clinical use [2]. This final approval is a regulatory requirement under CLIA and signifies the formal acceptance of the method into the laboratory's test menu.
Regulatory Framework and Essential Documentation
A successful verification is not only about the science but also about rigorous documentation that provides an auditable trail of the entire process.
The Three-Part Documentation Structure
The verification process generates a structured documentation package that transforms experimental data into a legally defensible and auditable record [21].
- The Validation/Verification Protocol: This is the pre-approved master document that details the entire plan—purpose, scope, study design, acceptance criteria, and methodologies [2] [21]. It is the commitment document that is signed before the study begins.
- Raw Data: All data generated during the execution of the protocol must be meticulously recorded and maintained. This includes instrument printouts, worksheets, calculation records, and notes on any deviations from the protocol [21].
- The Final Verification Report: This report summarizes the results against each acceptance criterion defined in the protocol. It must clearly state whether the method passed or failed each criterion, discuss any deviations, and provide a final conclusion on the method's fitness for use. This report requires the final signature of approval from the Laboratory Director [2] [21].
Key Regulatory Standards and Guidelines
Adherence to globally recognized standards is critical for regulatory compliance. Key guidance documents for microbiology verification include:
- CLSI M52: Verification of Commercial Microbial Identification and AST Systems [2].
- CLSI EP12-A2: User Protocol for Evaluation of Qualitative Test Performance [2].
- ISO 16140-3: Protocol for the verification of reference methods and validated alternative methods in a single laboratory [13].
- USP General Chapters: Such as <1225> for validation of compendial procedures and <1226> for verification of compendial procedures [21] [14].
Table: Quantitative Sample Requirements for Verification of Qualitative/Semi-Quantitative Assays
| Performance Characteristic | Minimum Sample Number | Sample Type Recommendations | Experimental Replication |
|---|---|---|---|
| Accuracy | 20 isolates/samples [2] | Combination of positive and negative clinical isolates; reference materials [2] | Single test per sample, compared to a reference method [2]. |
| Precision | 2 positive + 2 negative samples [2] | Controls or de-identified clinical samples [2] | Triplicate testing for 5 days by 2 operators [2]. |
| Reportable Range | 3 samples [2] | Known positives; samples near cutoff values [2] | Testing to verify upper and lower limits of detection/reporting [2]. |
| Reference Range | 20 isolates/samples [2] | Samples representative of the lab's patient population [2] | Testing to confirm normal expected results [2]. |
Developing a robust verification plan is a critical, non-negotiable step in implementing any new microbiological method in a research or diagnostic setting. This process, culminating in the formal approval of the Laboratory Director, ensures that methods perform reliably in a specific laboratory environment, thereby safeguarding data integrity, regulatory compliance, and ultimately, patient safety. As regulatory scrutiny intensifies—with the FDA increasingly focused on documented validation and verification—adhering to a structured framework with clear components, detailed experimental protocols, and comprehensive documentation is not just a best practice but a fundamental requirement for any credible microbiology laboratory involved in drug development and clinical research.
In biomedical and clinical research, sample size determination is the process of calculating the number of participants or observations needed for a successful experiment that can yield generalizable results to the broader population [22]. This calculation is a critical aspect of study design that directly impacts the scientific validity and statistical soundness of research outcomes [23] [22]. Appropriate sample size selection balances scientific rigor with ethical considerations and resource allocation, ensuring that studies have adequate power to detect clinically significant effects without unnecessarily exposing subjects to risk or consuming excessive resources [24].
Within microbiology laboratories, the principles of sample size determination extend beyond clinical studies to inform method verification and validation processes. When implementing new diagnostic methods, laboratories must conduct studies with sufficient sample sizes to confidently establish method performance characteristics, including accuracy, precision, and reportable ranges [2]. The determination of appropriate sample size therefore serves as a cornerstone for researchers seeking to draw precise inferences across the spectrum of biomedical and clinical investigations [22].
Key Statistical Concepts in Sample Size Determination
Core Components and Definitions
Table 1: Fundamental Statistical Concepts for Sample Size Calculation
| Concept | Definition | Role in Sample Size Calculation | Common Values |
|---|---|---|---|
| Null Hypothesis (H₀) | Statement that no relationship or difference exists between variables | Forms the basis for statistical testing; sample size determines ability to reject when false | No effect or no difference |
| Alternative Hypothesis (H₁) | Statement that a specific relationship or difference exists | Represents the effect the study aims to detect | Specific effect size |
| Significance Level (α) | Probability of rejecting H₀ when it is actually true (Type I error) | Sets threshold for statistical significance; lower α requires larger sample size | 0.05, 0.01, 0.001 |
| Power (1-β) | Probability of correctly rejecting H₀ when H₁ is true | Primary determinant of sample size; higher power requires larger sample size | 0.8, 0.9, 0.95 |
| Effect Size | Magnitude of the effect of practical or clinical importance | Larger effect sizes require smaller samples; most challenging parameter to specify | Varies by field and context |
| Standard Deviation | Measure of variability in the data | More variable data requires larger sample sizes | Estimated from pilot studies or literature |
Error Types and Statistical Power
Statistical hypothesis testing involves balancing two potential errors [23]. A Type I error (false positive) occurs when the null hypothesis is incorrectly rejected, while a Type II error (false negative) happens when the null hypothesis is incorrectly retained. The probability of committing a Type I error is denoted by α (significance level), while the probability of a Type II error is denoted by β. Statistical power, defined as 1-β, represents the probability of correctly detecting an effect when one truly exists [23] [22].
The relationship between these elements is crucial: reducing the risk of one error type typically increases the risk of the other unless sample size is increased. For most clinical trials, a power of 0.8 (80%) is considered optimal, meaning there is an 80% chance of detecting a specified effect size if it truly exists [22]. However, higher power (90% or 95%) may be required for studies where missing a true effect would have serious consequences [23].
Sample Size Calculation by Study Design
Cross-Sectional Studies and Surveys
Cross-sectional studies measure prevalence or proportion of characteristics in a population at a specific point in time [22]. The sample size formula for estimating a proportion is:
$$n = \frac{(Z_{1-α/2})^2 \times p \times (1-p)}{d^2}$$
Where:
- n = required sample size
- Z₁₋α/₂ = critical value from standard normal distribution (1.96 for 95% confidence)
- p = estimated proportion or prevalence
- d = margin of error (precision) [22]
Table 2: Sample Size Requirements for Cross-Sectional Studies (95% Confidence Level)
| Expected Prevalence | Margin of Error (d) | Required Sample Size | Application Example |
|---|---|---|---|
| 0.5 (50%) | 0.05 (5%) | 385 | Prevalence of antibiotic resistance |
| 0.2 (20%) | 0.05 (5%) | 246 | Prevalence of hospital-acquired infection |
| 0.1 (10%) | 0.05 (5%) | 139 | Prevalence of rare pathogen |
| 0.05 (5%) | 0.03 (3%) | 203 | Prevalence of specific genetic marker |
| 0.5 (50%) | 0.03 (3%) | 1068 | High-precision prevalence studies |
Example Calculation: In a study to determine the prevalence of liver diseases in a population where previous research indicated a 9% prevalence, with 95% confidence level and 5% margin of error [22]:
- Z₁₋α/₂ = 1.96
- p = 0.09
- d = 0.05
- Calculation: n = (1.96² × 0.09 × 0.91) / 0.05² = 126
Comparative and Experimental Studies
For studies comparing two groups, different formulas apply based on the outcome type (continuous vs. categorical) [23] [24]. For two independent proportions, the sample size per group is calculated as:
$$n = \frac{(Z{1-α/2} + Z{1-β})^2 \times [p1(1-p1) + p2(1-p2)]}{(p1 - p2)^2}$$
Where:
- p₁ and p₂ = expected proportions in the two groups
- Z₁₋α/₂ and Z₁₋β = critical values for Type I and Type II errors [23]
For continuous outcomes comparing two means, the formula becomes:
$$n = \frac{(Z{1-α/2} + Z{1-β})^2 \times 2σ^2}{d^2}$$
Where:
- σ = standard deviation of the outcome variable
- d = clinically important difference to detect [24]
Figure 1: Sample Size Determination Workflow
Special Considerations for Microbiome Studies
Microbiome studies present unique challenges for sample size calculation due to the high-dimensional nature of microbiome data and specific features like compositionality, sparsity, and heterogeneous distribution of microbial taxa [25]. Power calculations for microbiome studies must account for whether microbiome features are hypothesized to be the outcome, exposure, or mediator in the analysis [25]. Specialized statistical approaches and R scripts have been developed to address these unique requirements, moving beyond classic sample size calculations that don't accommodate the intrinsic features of microbiome datasets [25].
Sample Size in Method Verification and Validation
Method Verification in Microbiology Laboratories
In clinical microbiology laboratories, method verification studies are required by the Clinical Laboratory Improvement Amendments (CLIA) for non-waived systems before reporting patient results [2]. These studies demonstrate that a laboratory can reliably implement a previously validated method. It's crucial to distinguish between verification (confirming proper performance of an FDA-approved method) and validation (establishing performance characteristics for laboratory-developed or modified methods) [2] [13].
The ISO 16140 series provides international standards for method validation and verification in food chain microbiology, outlining a two-stage process [13]:
- Method validation establishes that a method is fit for purpose
- Method verification demonstrates that a laboratory can properly perform the validated method [13]
Table 3: Minimum Sample Requirements for Method Verification of Qualitative/Semi-Quantitative Assays
| Performance Characteristic | Minimum Samples | Sample Types | Acceptance Criteria |
|---|---|---|---|
| Accuracy | 20 clinically relevant isolates | Combination of positive and negative samples; range of values for semi-quantitative assays | Meets manufacturer claims or laboratory director determination |
| Precision | 2 positive + 2 negative tested in triplicate for 5 days by 2 operators | Controls or de-identified clinical samples | Meets manufacturer claims or laboratory director determination |
| Reportable Range | 3 samples | Known positives; samples near cutoff values for semi-quantitative assays | Laboratory-established reportable result verified |
| Reference Range | 20 isolates | De-identified clinical samples representing patient population | Expected result for typical sample verified |
Specimen Collection and Quality Considerations
The reliability of microbiological analyses depends heavily on appropriate specimen selection, collection technique, and transport conditions [26] [27]. Even with perfect sample size calculations, results will be compromised by poor specimen management. Key principles include:
- Collect specimens before antibiotic administration whenever possible [27]
- Prefer tissue, fluid, or aspirates over swabs when feasible [27]
- Use appropriate transport media and conditions (temperature, time) [26] [27]
- Ensure proper specimen labeling with specific site information [27]
For anaerobic cultures, special collection procedures are essential. Swabs are generally unacceptable due to oxygen exposure, inhibitory substances in swab materials, and small specimen volumes. Instead, needle aspirates or tissue biopsies should be placed into anaerobic transport media and transported at room temperature [26].
Practical Implementation and Tools
Sample size calculation need not be done manually, with several specialized software tools available [24]:
- G*Power: Statistical software package for power analysis
- OpenEpi: Open-source online calculator for various study designs
- PS Power and Sample Size Calculation: Practical tool for studies with dichotomous, continuous, or survival outcomes
- Sample Size Calculator: Web-based tool for common study designs
These tools vary in their interfaces, mathematical formulas, and assumptions, so researchers should understand the underlying principles to select appropriate tools and interpret results correctly [24].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Materials for Microbiological Studies and Verification
| Material/Reagent | Function/Application | Key Considerations |
|---|---|---|
| Anaerobic Transport Medium (ATM) | Preserves viability of anaerobic organisms during transport | Specimens must be transported at room temperature; swabs not acceptable [26] |
| Flocked Swabs | Improved specimen collection and release | More effective than Dacron, rayon, or cotton swabs for many applications [27] |
| Specialized Media | Selective growth of target microorganisms | Different media required for MRSA vs. C. difficile surveillance cultures [26] |
| Quality Controls | Verification of method performance | Include positive, negative, and quantitative controls as appropriate [2] |
| Reference Strains | Method verification and quality assurance | Well-characterized strains for accuracy assessment [2] |
Effect Size Determination Strategies
The effect size is often the most challenging parameter to specify in sample size calculations [24]. Several approaches can be used:
- Pilot studies: Conduct small-scale preliminary studies to estimate effect sizes
- Previous research: Consult meta-analyses or similar published studies
- Clinical significance: Determine the minimum effect that would be clinically meaningful
- Standardized values: Use conventional small (0.2), medium (0.5), or large (0.8) effect sizes when no other information is available [24]
When resources are limited, researchers may need to calculate the detectable effect size for a fixed sample size rather than determining sample size for a desired effect. This approach acknowledges constraints while maintaining scientific integrity by explicitly stating the minimum effect that could be detected with available resources [24].
Appropriate sample size determination is fundamental to producing valid, reproducible, and clinically relevant research findings in microbiology and biomedical sciences. By understanding the statistical principles, study design considerations, and field-specific requirements outlined in this guide, researchers can make informed decisions about sample size selection that balance scientific rigor with practical constraints. Proper implementation of these principles during study design, combined with appropriate specimen management and method verification protocols, enhances the quality and impact of microbiological research and diagnostic testing.
In the regulated environment of a microbiology laboratory, introducing a new test method is a significant undertaking. Before any patient or product test results can be reported, laboratories must provide documented evidence that the method performs reliably and as intended for its specific application. This process, known as method verification, is a cornerstone of laboratory quality systems and is mandated by regulations such as the Clinical Laboratory Improvement Amendments (CLIA) for non-waived systems before reporting patient results [2]. It is a one-time study meant to demonstrate that an unmodified, FDA-cleared or approved test performs in line with the manufacturer's established performance characteristics when used in the hands of the laboratory's personnel and with its specific instrumentation [2] [28].
Method verification is distinctly different from method validation. Whereas verification confirms that a previously validated method works as expected in a specific laboratory, validation is a more comprehensive process to establish that a newly developed or significantly modified method is fit for its intended purpose overall [28] [1]. Understanding when verification is required is essential for regulatory compliance and operational efficiency. This guide provides an in-depth technical exploration of how to verify three critical performance characteristics—Accuracy, Precision, and Reportable Range—forming the foundation of a robust method verification study in microbiology laboratory research.
The Regulatory Foundation of Method Verification
Method verification is not optional; it is a regulatory requirement in clinical, pharmaceutical, and food safety testing laboratories. The core requirement stems from CLIA regulations (42 CFR 493.1253), which stipulate that for any non-waived test system (tests of moderate or high complexity), the laboratory must, prior to reporting patient results, verify that it can obtain the performance specifications for accuracy, precision, and reportable range that are comparable to those established by the manufacturer [2] [29]. The laboratory must also verify the manufacturer's reference range for its patient population [2].
This requirement applies in several specific scenarios within a laboratory:
- Implementation of a new, unmodified FDA-cleared/approved method: This is the primary scenario for verification [2].
- Major changes in procedures or instrument relocation: Any significant change that could affect performance necessitates re-verification [2].
- As a requirement for laboratory accreditation: Standards such as ISO/IEC 17025 require laboratories to verify that they can properly perform standardized methods [28] [30].
The following diagram illustrates the decision pathway for determining when method verification is required.
Experimental Protocols for Verifying Critical Performance Characteristics
A well-designed verification study is based on a written plan that details the samples, replicates, and acceptance criteria. This section provides detailed experimental protocols for accuracy, precision, and reportable range.
Accuracy
Accuracy expresses the closeness of agreement between a test result and an accepted reference value [1]. It verifies that the new method produces results that are correct and agree with a comparative method.
Experimental Protocol for Qualitative/Semi-Quantitative Assays:
- Sample Number: A minimum of 20 clinically relevant isolates or specimens is recommended [2]. For initial verification of qualitative molecular assays, 50 positive and 50 negative specimens are suggested [31].
- Sample Type: Use a combination of positive and negative samples. Acceptable materials can include reference standards, proficiency test samples, well-characterized patient samples, or de-identified clinical samples tested in parallel with a validated method [2] [31].
- Experimental Design: Test samples using the new method and a comparative method (reference method). The testing should be performed blinded and spread over a minimum of five days to capture typical laboratory variation [31].
- Calculation: Calculate the percentage of agreement: (Number of results in agreement / Total number of results) × 100 [2].
- Acceptance Criteria: The observed agreement should meet the manufacturer's stated claims or a limit determined by the laboratory director [2].
Precision
Precision expresses the closeness of agreement between a series of measurements obtained from multiple sampling of the same homogeneous sample under prescribed conditions [1]. It confirms the test's repeatability and reproducibility.
Experimental Protocol (CLSI-based):
- Sample Number: A minimum of 2 positive and 2 negative samples [2]. For a comprehensive precision study, three levels are recommended: one near the limit of detection, one low, and one high [31].
- Replicates: Test samples in triplicate for 5 days by 2 operators. If the system is fully automated, operator variance may not be needed [2]. A robust protocol can involve testing replicates twice daily over 20 working days [31].
- Experimental Design: The experiment is designed to identify within-run, between-run, and between-day variances. These individual variances can be combined to understand the assay's total variance [31].
- Calculation: Calculate the percentage of agreement for qualitative tests. For quantitative tests, calculate the standard deviation (SD) and coefficient of variation (CV) [2] [31].
- Acceptance Criteria: The precision should meet the manufacturer's claims. For quantitative assays, the mean CV values should typically not exceed 15% (and 20% at the lower limit of quantitation) [31].
Reportable Range
The reportable range is the range of analyte values that a method can directly measure without dilution, concentration, or other special pre-treatment. It verifies the acceptable upper and lower limits of the test system [2] [29].
Experimental Protocol for Qualitative/Semi-Quantitative Assays:
- Sample Number: Verify using a minimum of 3 samples [2].
- Sample Type: For qualitative assays, use known positive samples. For semi-quantitative assays, use a range of positive samples near the upper and lower ends of the manufacturer-determined cutoff values (e.g., Cycle threshold (Ct) values) [2].
- Experimental Design: The reportable range is verified by testing samples that fall within and, if necessary, just outside the claimed range to confirm the limits.
- Evaluation: The reportable range is defined as what the laboratory establishes as a reportable result (e.g., "Detected," "Not detected," or a specific Ct value cutoff), verified by testing these samples [2].
The table below summarizes the key parameters for designing these verification experiments.
Table 1: Experimental Design Summary for Verification Studies
| Performance Characteristic | Minimum Sample Number/Type | Replicates & Duration | Key Calculation | Acceptance Criteria |
|---|---|---|---|---|
| Accuracy [2] [31] | 20-40 clinical isolates/specimens; combination of positives and negatives. | Testing spread over ≥5 days. | % Agreement = (Agreed results / Total results) × 100 | Meets manufacturer's stated claims or lab director's criteria. |
| Precision [2] [31] | Min. 2 positive & 2 negative samples; or 3 levels (low, medium, high). | Triplicate testing for 5 days with 2 operators (if applicable). | % Agreement; or Standard Deviation (SD) / Coefficient of Variation (CV). | Meets manufacturer's claims; CV typically <15%. |
| Reportable Range [2] | Min. 3 samples; known positives or samples near cutoffs. | Single testing may be sufficient. | Verification that results are reportable across the range. | Lab-established range (e.g., "Detected"/"Not detected") is confirmed. |
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful method verification relies on well-characterized materials. The following table lists essential reagents and materials used in verification experiments.
Table 2: Key Reagents and Materials for Verification Studies
| Reagent/Material | Function in Verification | Examples & Notes |
|---|---|---|
| Reference Standards & Panels [31] | Provide an accepted reference value for accuracy studies. Used to challenge the assay's detection capabilities. | Commercially available panels with known concentrations of analyte (e.g., SeraCare AccuSeries). |
| Quality Control (QC) Materials [2] [31] | Used to monitor precision and verify the test is performing within established parameters during the verification. | Commercially available QC materials at different levels (positive, negative, low, high). |
| Proficiency Testing (PT) Materials [2] [31] | Blinded samples with assigned values; provide an external benchmark for assessing accuracy. | Samples obtained from accredited PT providers. |
| Well-Characterized Patient Samples [2] [31] | Used as a comparative method in accuracy studies or to challenge the reportable range. | De-identified residual clinical samples previously tested by a validated method. |
| Clinically Relevant Isolates [2] | Used to verify accuracy, specificity, and reference range for microbiological methods. | Isolates from culture collections or clinical isolates representing relevant strains. |
Integrating Verification into the Broader Laboratory Context
Method verification is not an isolated event but a critical component of the total laboratory testing lifecycle. A well-executed verification study provides confidence in the initial performance of a method. However, the laboratory must create an ongoing process to monitor and re-assess the assay to ensure it continues to meet its desired purpose throughout its operational life [2]. This includes routine quality control, participation in proficiency testing, and diligent investigation of any aberrant results.
Furthermore, the principles of verification extend beyond clinical diagnostics. In food safety testing, for example, the ISO 16140 series provides a harmonized global protocol for method verification, requiring laboratories to demonstrate competency through a two-stage process: implementation verification (showing the lab can perform the method correctly) and (food) item verification (showing the method works with the specific items tested by the lab) [13] [30]. This underscores that verification is universally about proving capability and fitness-for-purpose in a local context.
In conclusion, verifying accuracy, precision, and reportable range provides the foundational evidence that a microbiological test method is reliable and ready for use. By adhering to structured experimental protocols and using appropriate materials, researchers and laboratory professionals can ensure regulatory compliance, generate high-quality data, and ultimately, support the safety of patients and consumers.
In microbiology laboratories, ensuring the reliability and accuracy of testing methods is paramount across clinical, pharmaceutical, and food safety domains. While the terms are sometimes used interchangeably, method validation and method verification represent distinct processes with specific regulatory requirements. Method validation is the comprehensive process of establishing that an analytical procedure's performance characteristics meet requirements for its intended analytical application, typically for laboratory-developed tests or modified FDA-approved methods [2]. Conversely, method verification demonstrates that a previously validated method performs as expected within a specific laboratory setting, applicable to unmodified FDA-approved or cleared tests [2] [32].
The fundamental distinction lies in their purpose and scope: validation creates the evidence that a method is fit-for-purpose, while verification confirms that a laboratory can successfully implement a previously validated method [32]. Before a new test enters routine use, its reliability must be established within the specific laboratory where it will be used, as required by international standards and regulations [7]. This guide examines the application of these critical processes across three key domains, providing technical specifications, experimental protocols, and regulatory frameworks essential for researchers, scientists, and drug development professionals.
Domain-Specific Requirements and Regulatory Frameworks
Clinical Microbiology Laboratories
In clinical microbiology, method verification is mandated by the Clinical Laboratory Improvement Amendments (CLIA) for all non-waived testing systems before patient results can be reported [2]. Laboratories must verify specific performance characteristics for unmodified FDA-approved tests, including accuracy, precision, reportable range, and reference range [2]. The recent implementation of the In Vitro Diagnostic Regulation (IVDR) in Europe and updated ISO 15189:2022 standards have further emphasized the need for robust verification procedures in clinical settings [7].
For antimicrobial susceptibility testing, verification becomes particularly complex when using non-FDA breakpoints with FDA-cleared panels, requiring careful consideration of organism selection, result interpretation, and acceptance criteria [2]. Laboratory leaders and clinical microbiologists provide essential oversight to ensure verification studies meet both regulatory requirements and the specific needs of the patient population served [2].
Pharmaceutical Quality Control Microbiology
Pharmaceutical quality control (QC) microbiology operates under Good Manufacturing Practice (GMP) regulations, where method verification serves as the primary method development strategy for compendial methods [1]. The United States Pharmacopeia (USP) chapters provide validated methods for microbiological examination of nonsterile products, sterility testing, and bacterial endotoxin testing, which laboratories must verify for their specific samples and settings [1].
Regulatory agencies including the FDA, Medicine and Healthcare Regulatory Agency (MHRA), and International Council for Harmonisation (ICH) mandate that test methods meet specific performance requirements before being used for product release [1]. Unlike one-time activities, pharmaceutical method verification requires ongoing vigilance throughout the product lifecycle, with re-verification necessary for formulation changes, material source updates, manufacturing process modifications, or reagent vendor changes [1].
Food Safety Testing
Food safety laboratories follow the ISO 16140 series for method validation and verification, with specific protocols for alternative method validation and laboratory implementation [13]. The process involves two distinct stages: implementation verification demonstrates the user laboratory can correctly perform the method, while food item verification confirms the method performs effectively for challenging items within the laboratory's scope [13].
A key concept in food safety testing is fitness-for-purpose, which evaluates whether a method validated for specific matrices will produce accurate results for a new matrix type [32]. Food matrix grouping systems categorize products with similar characteristics, with AOAC guidelines recognizing eight food categories divided into 92 subcategories, plus environmental sampling categories [32]. Verification must account for potential matrix effects, where substances like pectin or high fat content might interfere with detection methods [32].
Table 1: Comparative Analysis of Verification Requirements Across Domains
| Aspect | Clinical Microbiology | Pharmaceutical QC | Food Safety Testing |
|---|---|---|---|
| Primary Regulation | CLIA, ISO 15189, IVDR | GMP, USP, ICH | ISO 16140 series, AOAC |
| Typical Methods | FDA-cleared tests, laboratory-developed tests | Compendial methods (USP <61>, <62>, <71>) | Alternative proprietary methods |
| Key Parameters | Accuracy, precision, reportable range, reference range | Accuracy, precision, specificity, robustness | Relative accuracy, relative detection level, inclusivity |
| Sample Requirements | 20+ clinical isolates, combination of positive/negative | Product-specific, spiked samples | Food category representatives, 5+ food categories |
| Ongoing Requirements | Ongoing quality control, periodic re-verification | Lifecycle management, change control | Matrix extensions, method modifications |
Experimental Design and Protocols
Determining Sample Sizes and Acceptance Criteria
Proper experimental design for method verification requires careful consideration of sample sizes and acceptance criteria tailored to each domain. In clinical microbiology, accuracy verification typically requires a minimum of 20 clinically relevant isolates combining positive and negative samples, while precision studies need 2 positive and 2 negative samples tested in triplicate for 5 days by 2 operators [2]. For food safety testing, verification studies should include samples from at least 5 different food categories to establish fitness-for-purpose across matrices [32].
Acceptance criteria should align with manufacturer claims for FDA-cleared tests or be determined by the laboratory director when implementing laboratory-developed tests [2]. Quantitative acceptance criteria might include >95% accuracy compared to reference methods or <5% coefficient of variation for precision studies, though specific thresholds depend on the test's clinical, pharmaceutical, or food safety application [2] [1].
Core Verification Parameters and Protocols
Accuracy confirmation requires demonstrating acceptable agreement between the new method and a comparative reference method [2]. For qualitative clinical tests, this involves testing known positive and negative samples and calculating the percentage of agreement [2]. In pharmaceutical settings, accuracy expresses "the closeness of agreement between the value which is accepted either as a conventional true value or an accepted reference value and the value found" [1].
Precision verification confirms acceptable within-run, between-run, and operator variability [2]. Precision studies should incorporate multiple replicates across different days and analysts to establish repeatability and intermediate precision [1]. Statistical measures include standard deviation, coefficient of variation, and confidence intervals [1].
Specificity demonstrates the method's ability to assess the analyte unequivocally in the presence of potentially interfering components [1]. For microbial detection methods, this includes testing against near-neighbor organisms to ensure no cross-reactivity.
Limit of Detection (LOD) and Limit of Quantitation (LOQ) establish the lowest amount of detectable microorganisms [1]. These parameters are particularly critical when implementing modern microbiological methods claiming detection below 1 CFU, requiring demonstration of reproducibility at these low levels [1].
Table 2: Sample Size Requirements for Verification Studies
| Parameter | Clinical Microbiology | Pharmaceutical QC | Food Safety Testing |
|---|---|---|---|
| Accuracy | 20+ clinical isolates or samples | Product-specific, typically 3 lots | Representative food categories |
| Precision | 2 positive + 2 negative samples in triplicate over 5 days with 2 operators | Minimum 3 replicates at 3 different levels | According to ISO 16140-3 |
| Reportable Range | 3 samples with known analyte concentrations | Not always applicable | Range spanning expected results |
| Reference Range | 20 isolates representing patient population | Established during validation | Not typically verified |
| Specificity | Not always required for verification | Testing against interferents and near-neighbors | Inclusivity/exclusivity panel |
Decision Framework and Workflows
When Verification is Required: A Decision Framework
Determining when method verification is required follows a logical decision pathway based on regulatory domain, method type, and intended use. The following diagram illustrates the key decision points across different microbiology laboratory settings:
This decision pathway highlights that verification applies to standardized methods in their intended settings, while validation remains necessary for novel methods or significant modifications. Food safety testing requires additional fitness-for-purpose assessments when applying methods to new matrix types.
Method Verification Workflow
The actual execution of method verification follows a systematic workflow encompassing planning, execution, and documentation phases:
This workflow emphasizes the staged approach to verification, beginning with comprehensive planning, moving through rigorous experimental execution, and concluding with thorough documentation and implementation. Each stage requires specific expertise and documentation to meet regulatory expectations.
Essential Research Reagents and Materials
Successful method verification requires carefully selected reagents, reference materials, and controls that ensure reliable performance assessment. The following table details essential materials across verification activities:
Table 3: Essential Research Reagents and Materials for Method Verification
| Material Category | Specific Examples | Application in Verification | Technical Considerations |
|---|---|---|---|
| Reference Strains | ATCC strains, NCTC strains | Accuracy studies, specificity testing | Purity confirmation, proper storage and maintenance |
| Clinical Isolates | De-identified patient samples, banked isolates | Accuracy verification, reference range studies | Relevant to patient population, proper storage conditions |
| Quality Controls | Commercial controls, proficiency test materials | Precision studies, ongoing monitoring | Stability verification, proper reconstitution |
| Culture Media | Selective agars, enrichment broths, chromogenic media | Comparative studies, inclusivity/exclusivity | Lot-to-lot consistency, growth promotion testing |
| Molecular Reagents | PCR master mixes, extraction kits, primers/probes | Molecular method verification | Inhibition assessment, efficiency testing |
| Food Matrices | Representative food categories, artificially contaminated samples | Fitness-for-purpose studies | Homogeneity, stability, appropriate inoculation levels |
Troubleshooting and Quality Assurance
Even well-designed verification studies may encounter challenges requiring systematic troubleshooting. Common issues include failure to meet accuracy criteria, which may stem from improper reference method selection or sample-related issues [7]. When discrepancies occur between new and reference methods, laboratories should employ discrepancy testing using a third method or expert referral to resolve differences [7].
Precision failures often indicate operator technique issues, instrumentation problems, or reagent inconsistencies [1]. Implementing additional training, verifying equipment calibration, and testing new reagent lots can identify root causes. For food safety testing, matrix inhibition represents a frequent challenge, particularly with high-fat foods, acidic products, or materials containing PCR inhibitors [32]. Sample preparation modifications, dilution strategies, or inclusion of amplification controls can mitigate these effects.
Quality assurance extends beyond initial verification through ongoing monitoring. Clinical laboratories must establish ongoing processes to monitor and reassess assays, ensuring they continue to meet desired purposes throughout their lifecycle [2]. Pharmaceutical implementations require vigilant oversight of product lifecycles, with re-verification triggered by manufacturing process changes, formulation updates, or material source modifications [1].
Method verification serves as a critical gateway ensuring microbiology testing reliability across clinical, pharmaceutical, and food safety domains. While regulatory frameworks and specific requirements differ between CLIA, GMP, and ISO standards, the fundamental principle remains consistent: laboratories must demonstrate competence in performing standardized methods within their specific environments and for their intended applications. The increasing implementation of modern microbiological methods, coupled with evolving regulations such as IVDR in Europe, underscores the ongoing importance of robust verification practices.
Successful verification requires careful planning, appropriate sample selection, statistical rigor, and comprehensive documentation. By understanding domain-specific requirements, implementing systematic workflows, and employing troubleshooting strategies when challenges arise, laboratories can ensure their methods produce reliable results supporting patient care, product quality, and food safety. As method technologies continue advancing, verification practices must similarly evolve, maintaining the crucial balance between innovation implementation and result reliability.
Beyond Implementation: Troubleshooting and Sustaining Verification Quality
Common Verification Pitfalls and How to Resolve Discrepant Results
Within the framework of a microbiology laboratory, method verification is a regulatory and scientific requirement when introducing a previously validated method into a new laboratory setting. This technical guide details the common pitfalls encountered during this process and provides a systematic approach for resolving analytical discrepancies. Covering critical aspects from poor acceptance criteria setting to the intricacies of discrepant analysis, this document equips researchers and drug development professionals with the protocols and decision-making tools necessary to ensure data integrity and regulatory compliance.
Method verification is "the ability to verify that a method can perform a method reliably and precisely for its intended purpose" [1]. In microbiology, this process is distinct from full method validation. Verification is typically performed when a laboratory adopts a standard compendial method, such as those found in the USP, EP, or AOAC, to confirm it performs as expected under the lab’s specific conditions, instruments, and sample matrices [28] [32]. This is a primary method development strategy in Quality Control (QC) Microbiology labs, which often benefit from methods pre-validated by pharmacopeial chapters [1]. Understanding when and how to conduct a rigorous verification is fundamental to a strong release testing program, ensuring patient safety, and meeting the expectations of regulatory agencies like the FDA and MHRA [33] [1].
Common Pitfalls in Method Verification
Despite clear guidelines, several common pitfalls can compromise the verification process. These often stem from a lack of thorough understanding of the method's requirements and the unique characteristics of the sample being tested.
Inadequate Acceptance Criteria and Planning
A frequent critical mistake is the use of generic, non-specific acceptance criteria without scientific justification for the method at hand [34].
- The Problem: Relying on predefined Standard Operating Procedure (SOP) criteria without evaluating their suitability for the specific method and product. For instance, failing an FTIR identification method for a 97% spectral match against an arbitrary 98% criterion with no foundational data is a common error [34].
- The Resolution: All acceptance criteria in the verification protocol must be reviewed against known method performance data from development or literature. Criteria should be reasonable, reflecting the method's actual capability and what is considered acceptable for the product's intended use [34].
Failure to Investigate All Potential Interferences
Verification must demonstrate that the method's final result is not affected by potential interferences, a parameter known as specificity [34].
- The Problem: Overlooking constituents of a complex sample matrix or reagents used in the sample preparation process (e.g., solvents, buffers, derivatization reagents) [34].
- The Resolution: Conduct a thorough review of all potential interferences during the protocol design phase. This is especially critical for complex sample matrices or methods involving multiple reagents [34].
Neglecting Sample Stability and lifecycle Changes
A method's performance must be consistent over the entire lifecycle of the product it tests, including potential changes in the sample itself [34].
- The Problem: Failing to consider how sample composition changes over time, such as through degradation during a stability program. If a method is intended for stability testing, the verification must demonstrate its suitability for aged samples [34].
- The Resolution: Anticipate the long-term use of the method. For stability-indicating methods, this may require incorporating forced degradation studies into the verification protocol to prove the method can accurately analyze degraded samples [34]. Furthermore, any changes in product formulation, manufacturing process, or reagent sources necessitate re-verification to ensure the method's parameters are still met [1].
Insufficient Method Optimization
Treating verification as a simple checkbox exercise, without ensuring the method is truly optimized for the laboratory environment, leads to future problems.
- The Problem: Implementing a method without fine-tuning it for local conditions. This contrasts with the validation process, where optimization of specificity, sensitivity, and solution stability is incorporated [33].
- The Resolution: Even for a verified method, limited optimization may be needed to ensure robustness. Typical activities include improving method specificity and sensitivity for the local context and establishing system suitability criteria [33].
Resolving Discrepant Results: A Framework for Discrepant Analysis
Discrepant results occur when a new, more sensitive method (e.g., a Nucleic Acid Amplification (NAA) test) produces a positive result where a less sensitive gold standard method (e.g., culture) is negative [35]. This creates a quandary for evaluation. Discrepant analysis is a procedure to resolve these conflicting results, but it must be applied carefully to avoid statistical bias [35].
The Concept and Statistical Pitfalls
The core process of discrepant analysis involves retesting the discrepant samples (e.g., New Test Positive / Gold Standard Negative) with a third, "resolving" test to determine their true status [35].
- Inherent Bias: This approach is inherently biased in favor of the new test. By only investigating results that weaken the new test's apparent performance, any reclassification by the resolving test can only improve the calculated sensitivity, specificity, and Positive Predictive Value (PPV) of the new test [35].
- Impact of Prevalence: The magnitude of this bias depends on disease prevalence. At low prevalence (common in microbiology), the bias in sensitivity is larger. The bias also increases if the new test and the resolving test are not independent (e.g., two PCR tests targeting the same gene) [35].
Table 1: Impact of Discrepant Analysis on Test Statistics (Hypothetical CMV Example)
| Statistical Metric | Before Discrepant Analysis | After Discrepant Analysis | Change | Key Implication |
|---|---|---|---|---|
| Sensitivity | 155/(155+15) = 91.2% | 193/(193+15) = 92.8% | +1.6% | Increased confidence in detecting true positives. |
| Specificity | 790/(790+40) = 95.2% | 828/(828+2) = 99.7% | +4.5% | Increased confidence in true negative results. |
| Positive Predictive Value (PPV) | 155/(155+40) = 79.5% | 193/(193+2) = 98.9% | +19.4% | A physician's decision to treat may change based on this higher value. |
Recommended Protocols for Unbiased Resolution
To mitigate the bias of traditional discrepant analysis, the following protocols are recommended.
Protocol 1: Comprehensive Gold Standard Definition
This protocol aims to establish a more robust reference method before analysis begins.
- Objective: To avoid the bias of selectively retesting only discrepant samples by applying a resolving test to all samples or a random subset of concordant samples [35].
- Methodology:
- Define a Composite Gold Standard: Incorporate a third, independent test into the gold standard for all samples, not just the discrepant ones. This could be a different analytical technique or clinical correlation [35].
- Blinded Evaluation: The resolving test should be performed by analysts blinded to the results of the new and old tests.
- Statistical Analysis: Calculate the new test's performance characteristics (sensitivity, specificity) against this polished, composite gold standard.
Protocol 2: Analysis of Test Independence and Dependence
This protocol guides the selection of an appropriate resolving test to minimize overestimation of performance.
- Objective: To select a resolving test that minimizes statistical dependence, thereby reducing bias [35].
- Methodology:
- Independence Assessment: Evaluate the principles of the new test and potential resolving tests. Avoid using tests that are technologically similar (e.g., two different PCR tests for the same target) [35].
- Select an Independent Test: Choose a resolving test based on a different technological principle (e.g., use an antigen assay to resolve discrepancies between a culture and an NAA test) [35].
- Statistical Modeling: Acknowledge in the report that some bias may remain and, if possible, model its potential extent based on estimated prevalence and test dependence [35].
The following workflow diagrams the decision-making process for resolving discrepant results, incorporating these protocols to minimize bias.
The Scientist's Toolkit: Essential Reagents and Materials
Successful verification and discrepant resolution rely on high-quality, well-characterized reagents and materials.
Table 2: Key Research Reagent Solutions for Method Verification
| Item | Function in Verification / Discrepant Analysis | Critical Quality Attribute(s) |
|---|---|---|
| Reference Standards | Used to calibrate instruments and demonstrate accuracy and linearity of the method. | Certified purity and concentration, traceability to a primary standard. |
| Characterized Microbial Strains | Used to challenge the method's specificity, limit of detection (LOD), and accuracy by spiking samples. | Well-documented identity (genetically confirmed), viability, and known CFU. |
| Sample Matrices | The actual materials (e.g., food, tissue) used to verify the method works in the intended context. | Represents the true product, free of interfering contaminants; consistency between batches. |
| Culture Media & Reagents | Supports growth and detection of target microorganisms; buffers and chemicals used in sample prep. | Performance tested (e.g., fertility, selectivity), lot-to-lot consistency, absence of inhibitors. |
| Molecular Assay Components | Primers, probes, enzymes, and dNTPs for NAA tests used in modern methods or discrepant analysis. | High specificity, sensitivity, and purity; validated to work together without inhibition. |
Navigating method verification in the microbiology laboratory requires meticulous planning, a deep understanding of potential pitfalls, and a statistically sound approach to resolving discrepancies. By setting scientifically justified acceptance criteria, thoroughly investigating specificity, and implementing unbiased discrepant analysis protocols, researchers can generate reliable, defensible data. This rigorous approach ensures that methods are truly fit-for-purpose, ultimately safeguarding product quality and patient safety while maintaining compliance with global regulatory standards.
In the clinical microbiology laboratory, method verification is not a one-time event but a crucial component of an ongoing lifecycle. The Clinical Laboratory Improvement Amendments (CLIA) mandate that laboratories perform verification studies for unmodified FDA-approved tests before reporting patient results [2]. This process demonstrates that a test performs according to established performance characteristics in the operator's specific environment. While initial verification establishes a baseline, the dynamic nature of laboratory testing necessitates a structured approach to re-verification when changes occur to processes or products.
A lifecycle approach ensures that method performance remains consistent, reliable, and compliant despite evolving conditions. This technical guide examines the triggers and protocols for re-verification within the broader context of when method verification is required in microbiology laboratory research, providing researchers and drug development professionals with a framework for maintaining data integrity throughout a method's operational lifetime.
The Verification and Validation Lifecycle Framework
The process validation lifecycle, as outlined in pharmaceutical manufacturing, provides a valuable model for microbiology laboratories. This lifecycle consists of three iterative phases that ensure continuous method reliability [36].
The diagram above illustrates this continuous cycle. Process Design establishes the initial method parameters and performance characteristics. Process Qualification confirms that the method operates reliably under specified conditions. Continued Process Verification involves ongoing monitoring to ensure the method remains in a state of control [36]. When changes are introduced, the cycle returns to the appropriate phase for re-verification, creating a robust system for maintaining method integrity.
Triggers for Method Re-verification
Regulatory and Operational Change Classifications
Re-verification is required whenever a change has the potential to affect the method's performance characteristics. The following table categorizes common triggers for re-verification in microbiology laboratories.
| Change Category | Specific Examples | Recommended Re-verification Scope |
|---|---|---|
| Instrument/System Changes | Instrument relocation, major hardware/software upgrades, replacement with different model [2] | Full verification (Accuracy, Precision, Reportable Range, Reference Range) |
| Reagent/Component Changes | New reagent lot from different manufacturer, changes in critical consumables affecting performance | Limited verification (Accuracy and Precision minimum) |
| Process Modifications | Changes to specimen types, sample dilutions, or incubation times not specified as acceptable by manufacturer [2] | Validation study required (as this constitutes a modification) |
| Methodology Updates | Implementation of new FDA-approved method replacing existing method | Full verification study |
| Corrective Actions | Following major instrument repairs or performance issues identified by quality control | Targeted verification based on affected performance characteristics |
For unmodified FDA-approved tests, verification is a one-time study demonstrating performance aligns with manufacturer claims. However, when modifications are introduced—defined as changes not specified as acceptable by the manufacturer—the process transitions from verification to validation [2]. Validation establishes that a modified or laboratory-developed test works as intended for its new application.
Designing the Re-verification Study
Determining the Study Scope
The scope of re-verification should be commensurate with the significance of the change. A risk-based approach should guide which performance characteristics require re-assessment. CLIA regulations require verification of several key analytical performance characteristics for non-waived testing systems [2]:
- Accuracy: The agreement between the new method and a comparative method
- Precision: The reproducibility of results (within-run, between-run, between-operators)
- Reportable Range: The verified upper and lower limits of the test system
- Reference Range: The normal expected results for the tested patient population
Experimental Protocols for Key Performance Characteristics
The following table outlines detailed experimental protocols for verifying critical performance characteristics of qualitative and semi-quantitative microbiological assays, which are most common in microbiology settings [2].
| Performance Characteristic | Minimum Sample Requirements | Experimental Design | Acceptance Criteria |
|---|---|---|---|
| Accuracy | 20 clinically relevant isolates [2] | Combination of positive and negative samples tested against comparative method | Percentage of agreement meets manufacturer claims or laboratory-established criteria |
| Precision | 2 positive and 2 negative samples tested in triplicate for 5 days by 2 operators [2] | If system is fully automated, operator variance testing may not be required | Percentage of agreement between replicates meets manufacturer claims |
| Reportable Range | 3 samples with known values [2] | For qualitative assays: known positive samples; for semi-quantitative: samples near cutoff values | Laboratory establishes reportable result parameters (e.g., "Detected," "Not detected") |
| Reference Range | 20 isolates representing patient population [2] | De-identified clinical samples or reference materials with known expected results | Verified normal results for laboratory's specific patient population |
Statistical analysis should extend beyond simple percent agreement calculations. For quantifying variability in microbial responses, mixed-effects models and Bayesian approaches are recommended over simplified algebraic methods, which can overestimate variability contributions, especially in nested experimental designs [4].
The Researcher's Toolkit: Essential Materials for Verification Studies
Successful verification studies require carefully selected materials and controls. The following table outlines essential research reagent solutions for conducting method verification in microbiology.
| Resource Category | Specific Examples | Function in Verification Studies |
|---|---|---|
| Reference Materials | ATCC strains, proficiency test samples, commercial controls [2] | Provide characterized samples with known properties for accuracy assessment |
| Clinical Samples | De-identified residual patient specimens [2] | Represent real-world matrix for verifying method performance with actual patient samples |
| Statistical Framework | CLSI EP12-A2, CLSI M52, CLSI MM03-A2 [2] | Standardized protocols for evaluating qualitative test performance and microbial identification systems |
| Quality Control Tools | Individualized Quality Control Plan (IQCP) templates [2] | Framework for developing laboratory-specific quality control protocols |
| Data Analysis Resources | Mixed-effects models, Bayesian statistical methods [4] | Advanced statistical tools for quantifying variability and uncertainty in microbial data |
When sourcing materials, laboratories should prioritize well-characterized reference materials that represent the full analytical measurement range. For molecular methods, this includes samples with known target concentrations spanning the reportable range.
Implementing Continued Process Verification
The final phase of the lifecycle involves ongoing monitoring to ensure the method remains in control during routine operation. Continued Process Verification (CPV) involves systematic data collection during production to verify process performance remains within established parameters [36].
Implementation requires:
- Establishing ongoing data collection protocols for key performance indicators
- Implementing statistical process control methods to detect deviations
- Maintaining comprehensive documentation of all process monitoring activities
- Establishing clear action limits triggering investigation when exceeded
Technology plays a crucial role in CPV implementation. Automated monitoring systems, electronic batch records, and advanced data analytics help identify trends, detect anomalies, and flag potential risks before they escalate into significant problems [36].
A proactive lifecycle approach to method verification and re-verification ensures microbiology laboratories maintain the highest standards of data quality and regulatory compliance. By establishing clear protocols for initial verification, defining triggers for re-verification, and implementing robust continued process verification, researchers and drug development professionals can confidently generate reliable results despite evolving methods and processes.
This structured approach ultimately supports the core mission of microbiology laboratories: providing accurate, timely, and clinically relevant data that advances both patient care and scientific understanding of microbial systems.
In the context of microbiology laboratory research, method verification is a one-time study required by regulations such as the Clinical Laboratory Improvement Amendments (CLIA) for implementing unmodified, FDA-approved tests before reporting patient results [2]. It confirms that a test performs according to manufacturer-established performance characteristics in the user's environment. However, the process of ensuring quality does not end with successful verification. A robust post-verification quality assurance system is essential to maintain analytical quality, ensure patient safety, and support reliable research outcomes throughout the method's lifecycle.
This ongoing system must proactively address two critical challenges: managing unplanned downtime and administering effective proficiency testing. These components act as the continuous monitoring pillars that safeguard the integrity of laboratory data long after the initial verification is complete, directly impacting a laboratory's operational stability and the credibility of its research.
The Pillars of Post-Verification Quality Assurance
A sustainable quality system rests on multiple interdependent components. Proficiency Testing and Downtime Management are central pillars, supported by comprehensive documentation and a culture of continuous improvement.
Proficiency Testing as an Ongoing Quality Monitor
Proficiency Testing is a fundamental external quality assessment tool. PT involves the regular analysis of characterized materials, which are treated as "blind" samples to evaluate both laboratory and analyst competency [37]. These programs are mandated by most accreditation bodies and provide an objective measure of a laboratory's ability to produce reliable results.
Core Components and Best Practices
PT samples are characterized materials designed to represent routine samples in terms of matrix, analytes, and concentrations [37]. Participants analyze these samples according to their standard operating procedures and confidentially report results to the PT provider for evaluation against assigned reference values [37]. Successful performance indicates that the laboratory's verified methods remain under control and that staff can perform testing competently.
Best practices for PT include [37]:
- Treat PT samples identically to routine patient or research samples in preparation, analysis, and reporting.
- Ensure all analysts who report data perform PT at least annually to document individual competency.
- Maintain rigorous documentation of all PT activities, from sample receipt to corrective actions.
- Use PT results as a verification tool for continuous method monitoring after the initial validation.
Statistical Evaluation of PT Performance
PT providers use standardized statistical methods to evaluate participant performance. The two primary approaches are:
- z-score: Used when uncertainty calculations are not required. The formula is
z = (x - X)/σ, wherexis the lab's reported value,Xis the reference value, andσis the standard deviation. Scores between -2 and 2 are acceptable, scores between 2 and 3 are questionable, and scores beyond ±3 are unacceptable [37]. - En-value: Applied in interlaboratory comparisons where laboratories report uncertainty calculations. The formula is
En = (x - X)/√(U_lab² + U_ref²), whereU_labandU_refare the expanded uncertainties of the lab and reference value, respectively. Results withEnvalues between -1 and 1 are acceptable [37].
Table 1: Proficiency Testing Statistical Evaluation Criteria
| Statistical Method | Calculation | Acceptable Range | Application Context |
|---|---|---|---|
| z-score | z = (x - X)/σ |
-2 ≤ z ≤ 2 |
Chemical/biological analyses without uncertainty reporting |
| En-value | En = (x - X)/√(U_lab² + U_ref²) |
-1 ≤ En ≤ 1 |
Interlaboratory comparisons with uncertainty calculations |
Responding to Unacceptable PT Results
When PT results are unacceptable, laboratories must implement a structured corrective action process [37]:
- Immediate Root Cause Analysis: Investigate potential sources of error including sample preparation, instrument calibration, reagent quality, calculation errors, and environmental conditions.
- Documentation: Record all findings from the investigation and the identified root cause.
- Corrective Action Implementation: Address the root cause through staff retraining, procedure modification, equipment repair, or process changes.
- Verification of Effectiveness: Retest corrected systems with quality controls or subsequent PT to confirm problem resolution.
Managing and Preventing Laboratory Downtime
Unplanned downtime represents a critical failure in laboratory quality systems, directly impacting research continuity, data integrity, and operational costs. A 2025 survey revealed that nearly 60% of lab professionals experience significant downtime due to equipment failures and missed calibration schedules [38].
Quantifying the Impact of Downtime
The financial implications of unplanned downtime are substantial. For a medium to large laboratory, costs can exceed $100,000 per hour [39]. These costs include both direct financial losses and indirect operational impacts.
Table 2: Comprehensive Costs of Laboratory Downtime
| Cost Category | Specific Examples | Financial Impact |
|---|---|---|
| Direct Revenue Loss | Lost testing revenue during outage | Up to $4,167/hour for a lab with $100,000 daily revenue [39] |
| Operational Expenses | Staff overtime, emergency repairs, expedited shipping | $5,000-$10,000 per major incident [39] |
| Compliance Impacts | Regulatory penalties, accreditation jeopardy | Case-dependent, potentially severe |
| Reputational Damage | Loss of client trust, negative impact on research collaborations | Long-term business impact |
Strategic Approaches to Minimize Downtime
Effective downtime management requires a proactive, systematic approach combining technology, standardized processes, and strategic planning.
Technology and Infrastructure Solutions:
- Implement real-time monitoring systems for critical equipment to detect issues before they cause failures. Currently, only 30% of laboratories leverage such technology [38].
- Deploy redundant systems and backup servers for essential instruments and data management systems [39].
- Utilize Laboratory Information Management Systems with guaranteed uptime (e.g., 99.9% uptime guarantees) to ensure data accessibility [39].
- Maintain stable power supplies and environmental controls to prevent facility-related disruptions [39].
Process and Procedural Controls:
- Establish and enforce preventive maintenance schedules for all laboratory equipment, strictly adhering to manufacturer recommendations [40] [39].
- Develop comprehensive Standard Operating Procedures for routine operations, emergency response, and downtime contingencies [41] [39].
- Create clear communication protocols for reporting issues and coordinating responses during system failures [41].
- Conduct regular emergency drills to ensure staff preparedness for unexpected downtime events [39].
The Scientist's Toolkit: Essential Research Reagent Solutions
Microbiology laboratories rely on specialized quality control materials to maintain assay validity and ensure reliable results post-verification.
Table 3: Essential Quality Control Materials for Microbiology Laboratories
| Reagent Solution | Function | Application Examples |
|---|---|---|
| Quality Control Organisms | Well-characterized microorganisms with defined profiles used to validate testing methodologies and monitor instrument, operator, and reagent quality [17]. | Growth promotion testing, diagnostic positive controls, antimicrobial susceptibility testing verification. |
| Certified Reference Materials | Quantitative materials certified for specific analytes, used for method validation, calibration, and ensuring traceability [17]. | Equipment calibration, method verification, qualifying new reagent lots. |
| Proficiency Test Standards | Characterized materials with assigned values for interlaboratory comparison, assessing analytical performance and competency [37] [17]. | External quality assessment, staff competency evaluation, comparative method performance. |
| Environmental Isolates | In-house or commercially prepared wild-type strains representing laboratory-specific microflora, crucial for challenging test methods with relevant organisms [17]. | Method robustness testing, disinfectant efficacy studies, environmental monitoring validation. |
Integrating Documentation and Continuous Improvement
Complete and accessible documentation forms the historical record of laboratory quality, providing what has been described as the "voice" of the analytical process [40]. This history includes method verification data, daily quality control results, proficiency testing outcomes, equipment maintenance records, and documentation of any deviations or corrective actions [40].
Effective documentation enables continuous feedback loops through [41]:
- Regular team debriefs to discuss process effectiveness and emerging challenges
- Performance dashboards tracking turnaround times, error rates, and equipment utilization
- Anonymous feedback channels that encourage staff to report concerns without fear of blame
This systematic approach to quality management shifts laboratory operations from reactive firefighting to proactive foresight, creating an environment where scientific excellence can thrive [41].
In microbiology laboratory research, successful method verification represents merely the starting point for sustainable quality management. The ongoing integration of rigorous proficiency testing and strategic downtime prevention creates a robust framework that maintains analytical quality, supports research integrity, and ensures patient safety throughout the method lifecycle. By implementing these post-verification quality assurance strategies, laboratories can transform quality management from a regulatory requirement into a strategic asset that enhances research credibility and operational excellence.
Leveraging Quality Control Organisms and Reference Materials for Ongoing Accuracy
In the landscape of microbiology laboratory research, demonstrating that a method is performing reliably does not end with its initial implementation. Method verification is the foundational process that establishes a laboratory's capability to correctly perform a validated method before routine use, while ongoing accuracy is maintained through continuous quality control (QC) practices [2] [32]. Within this framework, quality control organisms and reference materials are the cornerstone tools that provide objective evidence of performance, ensuring that diagnostic, pharmaceutical, and food safety test results are accurate, reliable, and reproducible over time. This guide details the strategic use of these materials to uphold the highest standards of data integrity in research and development.
Understanding Method Verification and Ongoing QC
Before delving into materials and protocols, it is crucial to distinguish between the initial demonstration of competency and its continuous monitoring.
The Role of Method Verification
Method verification is a one-time study required for unmodified, FDA-approved tests before a laboratory can report patient or product results. It is mandated by regulations like the Clinical Laboratory Improvement Amendments (CLIA) and confirms that a test's performance characteristics—accuracy, precision, reportable range, and reference range—align with the manufacturer's claims in the user's specific environment [2]. This process answers the question: "Can our laboratory perform this test correctly?"
The Transition to Ongoing Quality Control
Once a method is verified, the focus shifts to ongoing quality control. This is the continuous process of monitoring the test system to ensure it remains in a state of control during routine use. QC organisms are used daily, weekly, or per batch to detect deviations caused by reagent lot changes, instrument calibration drift, or operator technique [42] [43]. This process answers the question: "Is our test still performing correctly today?"
The relationship between these processes and the broader context of method establishment is outlined below.
A Framework for Selecting QC Organisms and Materials
Selecting the right QC organisms is a strategic decision based on the test method and its intended use. The following guide provides a structured approach to this selection.
Critical Attributes of High-Quality Reference Materials
Regardless of the format, all reference materials should possess key attributes to ensure reliability and compliance [42] [44]:
- Traceability and Authenticity: Strains must be traceable to internationally recognized culture collections (e.g., ATCC, NCTC) to ensure authenticity.
- Low Passage Level: Organisms should be at a low passage number (e.g., ≤3 passages from the reference culture) to prevent genetic drift and phenotypic changes.
- Standardized Formats: Use ready-to-use formats like lyophilized pellets or quantitative stocks to minimize preparation error and enhance reproducibility.
- Accreditation: Preference should be given to materials produced under ISO 17034 accreditation, which certifies the producer as a competent Reference Material Producer [44].
Experimental Protocols for Verification and Ongoing QC
This section provides detailed methodologies for leveraging QC organisms in key laboratory activities.
Protocol for Verifying a Qualitative Diagnostic Assay
This protocol is designed to fulfill the initial verification requirements for a test like a pathogen-specific PCR.
- Objective: To verify the accuracy, precision, and reportable range of a new qualitative assay in your laboratory [2].
- QC Materials Required:
- A panel of at least 20 characterized isolates spanning positive and negative targets [2].
- These can be sourced from reference materials, proficiency test samples, or de-identified clinical samples previously tested with a validated method.
- Procedure:
- Test the entire panel of 20 samples using the new method.
- For accuracy assessment, compare the results to those obtained from a reference or comparative method. Calculate the percentage agreement: (Number of results in agreement / Total number of results) * 100 [2].
- For precision assessment, select at least 2 positive and 2 negative samples. Test these in triplicate over five different days, preferably by two different operators. Calculate the percent agreement for each sample across all runs [2].
- Acceptance Criteria: The performance must meet the manufacturer's stated claims or criteria determined by the laboratory director [2].
Protocol for Growth Promotion Testing of Culture Media
This is a classic example of ongoing QC in pharmaceutical and food testing laboratories.
- Objective: To ensure that each batch of prepared culture media supports the growth of target organisms and demonstrates selectivity where required.
- QC Materials Required:
- Procedure:
- Inoculate a sample of the new media batch with a small, quantified inoculum (e.g., ≤100 CFU) of the appropriate QC organism.
- Simultaneously, inoculate a sample of a current, satisfactory batch of media with the same organism as a control.
- Incubate both under specified conditions.
- Examine for growth. For nutritive media, growth on the new batch must be comparable to the control. For selective media, it must inhibit or allow growth as expected [1] [44].
- Acceptance Criteria: Growth must be as described in pharmacopeial standards such as USP <61> and <62> [1].
Quantitative QC for Modern Methods
For rapid microbiological methods and molecular assays, quantitative controls are essential.
- Objective: To validate or verify the detection limit of a quantitative or alternative method.
- QC Materials Required: Quantitative reference materials like Epower or Quanti-Cult, which deliver a specific, certified range of CFU per pellet [42] [44].
- Procedure:
- Use a quantitative pellet with a known, low CFU count (e.g., 10-100 CFU).
- Incorporate this material directly into the test method as a sample.
- The method must be able to consistently detect the target at this low level to confirm its Limit of Detection (LOD) [1].
- Acceptance Criteria: The method must detect the analyte or microorganism at or below the claimed LOD with a defined statistical confidence (e.g., ≥95% detection rate).
The Researcher's Toolkit: Essential QC Reagents and Solutions
The table below summarizes key products and their applications for maintaining ongoing accuracy.
Table: Essential QC Reagents and Their Functions in the Microbiology Laboratory
| Product Name/Type | Format | Primary Function | Key Applications |
|---|---|---|---|
| KWIK-STIK / Culti-Loops [42] [44] | Qualitative lyophilized pellet on a swab | Provides viable microorganisms for qualitative QC | Daily control of reagents/media; verification/validation; ID & AST system QC [42] |
| Epower / Quanti-Cult [42] [44] | Quantitative lyophilized pellet | Delivers a specific, certified range of CFU | Method validation; disinfectant efficacy testing; enumeration method QC [42] |
| Helix Elite Molecular Standards [43] | Swab or pellet format (inactivated or live) | Acts as a control for nucleic acid extraction and amplification | Validation & routine QC of molecular diagnostic assays (e.g., PCR, NGS) [43] |
| Custom QC Solutions [42] | Variable (bacteria, fungi, phage, nucleic acids) | Provides control for unique or proprietary laboratory methods | Environmental isolate controls; diagnostic assay development; viral stock production [42] |
Navigating Regulatory Standards and Best Practices
Adherence to international standards is not merely a regulatory hurdle but a blueprint for scientific rigor.
- ISO 16140 Series: This is the cornerstone standard for the validation and verification of microbiological methods in the food and feed chain. ISO 16140-2 covers the validation of alternative methods, while ISO 16140-3 provides the protocol for verification in a single laboratory [13].
- Pharmacopeial Standards (USP/EP): Chapters such as USP <1223>, <1225>, and <1226> provide guidance for validating and verifying compendial methods in the pharmaceutical industry [1].
- CLSI Guidelines: Documents like CLSI M52 and EP12-A2 offer detailed frameworks for verifying commercial microbial identification and qualitative test performance in clinical laboratories [2].
A best practice is to implement an Individualized Quality Control Plan (IQCP) which leverages a risk-management approach to tailor QC frequency based on the validated stability of the test system and the laboratory's specific environment and operational factors [2].
In the rigorous world of microbiology research and drug development, the path to reliable data is paved with disciplined quality practices. Method verification establishes a laboratory's right to use a method, but it is the strategic and consistent use of well-characterized quality control organisms and reference materials that safeguards ongoing accuracy. By integrating these materials into a framework of robust experimental protocols and adhering to international standards, laboratories can move beyond simple compliance to achieve a state of demonstrated and sustained excellence, ensuring that every result reported is worthy of trust.
Advanced Scenarios: When Verification is Not Enough and Full Validation is Needed
In the rapidly evolving field of clinical microbiology, laboratory-developed tests (LDTs) and modified methods serve as critical tools for addressing unmet diagnostic needs. An LDT is defined as an in vitro diagnostic test that is developed, manufactured, and used within a single laboratory [45]. These tests are particularly valuable when no FDA-approved assay exists for a particular pathogen, specimen type, or patient population [45]. Similarly, any modification to an FDA-cleared or approved assay that alters the manufacturer's clinical claims about intended use constitutes a significant change that transforms the test into an LDT [46]. The regulatory landscape governing these tests is complex, with oversight primarily falling under the Clinical Laboratory Improvement Amendments (CLIA) administered by the Centers for Medicare and Medicaid Services (CMS) [46].
The distinction between validation and verification represents a fundamental concept in laboratory medicine. Verification is a one-time study for unmodified FDA-approved tests meant to demonstrate that a test performs in line with previously established performance characteristics when used as intended by the manufacturer [2]. In contrast, validation is a comprehensive process that establishes that a non-FDA cleared test (e.g., LDTs) or modified FDA-approved test works as intended for its specific application [2]. This distinction is not merely semantic but carries significant implications for the rigor of testing required before implementing a new method in clinical practice.
The Regulatory Imperative: Why Validation is Non-Negotiable
CLIA Requirements and Beyond
Under CLIA regulations, all LDTs are classified as high-complexity tests, subjecting them to the most stringent quality control, proficiency testing, and personnel requirements [46]. Laboratories must demonstrate the analytical validity of their LDTs, establishing the technical performance characteristics of the assay [46]. While CLIA does not explicitly require establishments of clinical validity—demonstrating that the test is fit for its intended purpose in assisting physicians with medical decisions—this expectation is enforced by major accrediting organizations such as the College of American Pathologists (CAP) and The Joint Commission [46].
The New York State Department of Health provides one of the most structured regulatory frameworks for LDTs, requiring a risk assessment and explicit approval before patient testing may commence [47]. Their tiered evaluation system classifies tests based on potential risk, with higher-risk categories requiring more comprehensive review. This model exemplifies the increasing regulatory scrutiny facing LDTs as they play an expanding role in patient care [47].
The FDA's Evolving Role in LDT Oversight
The FDA has historically exercised "enforcement discretion" by deferring LDT oversight to CMS under CLIA, but this position has shifted in recent years [46]. The agency now asserts that advances in technology and the expanding role of LDTs in clinical decision-making compel more direct regulatory oversight. Although a proposed rule to classify LDTs as devices was nullified in March 2025, the regulatory landscape remains dynamic, with ongoing debates about the appropriate balance between innovation and patient safety [15].
Table 1: Key Definitions in Laboratory Test Regulation
| Term | Definition | Regulatory Context |
|---|---|---|
| Laboratory-Developed Test (LDT) | An in vitro diagnostic test that is developed, manufactured, and used within a single laboratory [45] | CLIA high-complexity category; requires laboratory-specific validation [46] |
| Modified FDA-Approved Test | An assay with changes to intended use or testing procedure not specified as acceptable by the manufacturer [2] | Considered an LDT; requires full validation [47] |
| Method Verification | Process confirming that an unmodified FDA-approved test performs according to manufacturer specifications in your laboratory [2] | CLIA requirement for non-waived test systems [2] |
| Method Validation | Process establishing that an LDT or modified test works as intended for its specific application [2] | Required before implementing any LDT; must establish analytical performance [47] |
When is Method Verification or Validation Required?: A Decision Framework
Understanding when verification versus validation is required is fundamental to regulatory compliance in the microbiology laboratory. The following decision pathway provides guidance for navigating this critical determination:
Specific Scenarios Requiring Validation
Beyond the decision framework above, several specific scenarios necessitate complete method validation:
- Commercially distributed assays not cleared/approved by the FDA: Tests labeled Research Use Only (RUO) or Investigational Use Only (IUO) without an FDA Investigational Device Exemption require full LDT validation [47].
- Tests with modified intended use: Changes to specimen type, type of analysis (qualitative vs. quantitative), purpose of the assay (screening, diagnosis, prognosis), or target population compared to the FDA-approved package insert or NYS approval letter [47].
- Tests employing new technologies: Methods that incorporate newer technology/platforms compared to standard methods, even if the clinical claim remains unchanged [47].
- Tests for clinical trials: LDTs used for participant management decisions in IRB-approved research, including tests influencing enrollment, treatment arm assignment, safety, toxicity, or dosing [47].
The Validation Protocol: A Step-by-Step Methodology
Core Analytical Performance Characteristics
For any LDT or modified method, validation must establish specific performance characteristics. The following table summarizes the key parameters, testing approaches, and acceptance criteria for qualitative microbiological assays:
Table 2: Validation Parameters for Qualitative Microbiological LDTs
| Performance Characteristic | Experimental Approach | Sample Size & Type | Acceptance Criteria |
|---|---|---|---|
| Accuracy | Compare results between new method and comparative method | Minimum 20 clinically relevant isolates (positive and negative) [2] | Percentage of agreement should meet manufacturer claims or laboratory-defined criteria [2] |
| Precision | Test positive and negative samples in triplicate for 5 days by 2 operators | Minimum 2 positive and 2 negative samples [2] | >95% agreement between replicates and operators [2] |
| Reportable Range | Verify upper and lower detection limits | Minimum 3 known positive samples [2] | Consistent detection of analytes across claimed range [2] |
| Reference Range | Establish normal results for patient population | Minimum 20 isolates from representative population [2] | Expected results align with manufacturer claims or published literature [2] |
| Specificity | Challenge assay with near-neighbor organisms | Panels of closely related non-target organisms | No cross-reactivity with non-target organisms |
| Limit of Detection | Serial dilutions of target organism | Dilutions spanning expected clinical range | Consistent detection at claimed concentration |
Advanced Validation Considerations
For laboratories implementing more complex methodologies, additional validation elements may be necessary:
Equipment Validation under Quality Systems For laboratories operating under current Good Manufacturing Practices (cGMP) or similar quality frameworks, equipment validation follows a rigorous Installation Qualification (IQ), Operational Qualification (OQ), and Performance Qualification (PQ) protocol [15]. This process, known as IOPQ, provides documented evidence that equipment is properly installed, functions according to specifications, and performs consistently under actual processing conditions [15].
Matrix Extension Studies When applying a validated method to new sample types (matrices), laboratories must conduct fitness-for-purpose evaluations. The International Organization for Standardization (ISO) 16140 series provides guidance on validating methods across different matrix categories, with more extensive testing required for matrices with greater differences from originally validated types [13].
Essential Research Reagents and Materials
Successful validation and implementation of LDTs requires carefully selected reagents and materials. The following toolkit represents essential components for developing and validating microbiological assays:
Table 3: Research Reagent Solutions for Microbiology LDT Development
| Reagent/Material | Function | Application Examples |
|---|---|---|
| Reference Strains | Positive controls for target organisms | ATCC strains for accuracy and precision studies |
| Clinical Isolates | Real-world validation samples | 20+ well-characterized isolates for method comparison |
| Analyte-Specific Reagents (ASRs) | Core detection components | Antibodies, primers, probes for target detection |
| Molecular Grade Water | Negative control and dilution medium | Background contamination assessment |
| Quality Control Panels | Ongoing performance monitoring | Commercial QC materials for daily verification |
| Culture Media | Organism propagation and recovery | Supports growth of target and challenge organisms |
Implementation Workflow: From Validation to Routine Use
The process of moving a validated LDT into routine clinical use requires careful planning and documentation. The following workflow outlines the critical path from validation to implementation:
Documentation and Review Processes
Comprehensive documentation is essential throughout the validation process. The validation plan should include detailed protocols for each performance characteristic, predefined acceptance criteria, and a clear description of the statistical methods for data analysis [2]. Any deviations from the planned protocol must be documented with justifications. The final validation report should provide a comprehensive summary of all studies conducted, complete with raw data, statistical analyses, and a definitive conclusion regarding whether the test meets all predefined criteria for clinical implementation [47] [2].
For laboratories in New York State or those seeking CAP accreditation, explicit approval of the validation package by the regulatory body may be required before patient testing can commence [47]. Even after implementation, continuous monitoring through quality control procedures, proficiency testing, and periodic reassessment is necessary to ensure ongoing test performance [2].
The validation imperative for LDTs and modified methods represents a critical balance between innovation and patient safety. As the regulatory landscape continues to evolve, microbiology laboratories must maintain rigorous validation practices while responding to emerging infectious diseases and specialized patient needs. The framework outlined in this guide provides a roadmap for developing, validating, and implementing reliable laboratory-developed tests that meet both clinical needs and regulatory expectations. Through robust validation protocols and comprehensive documentation, laboratories can ensure the analytical validity and clinical utility of their tests while advancing the field of diagnostic microbiology.
In the tightly regulated landscape of microbiology laboratories, the implementation of modern or alternative analytical methods is a common necessity driven by technological advancement, process improvement, or the need for greater efficiency. However, before a new method can replace an established compendial method (such as those in the United States Pharmacopeia - USP), laboratories must rigorously demonstrate equivalency—a process that proves the new method generates results that are statistically equivalent or superior to the original method for its intended purpose [48].
This requirement is foundational to ensuring that changes in methodology do not compromise the integrity of data used for critical decisions regarding product quality, patient safety, or research outcomes. Method equivalency is not a single study but a strategic framework that aligns with the analytical procedure lifecycle, emphasizing that method capability must be maintained throughout its use [49]. This guide provides a detailed roadmap for researchers and drug development professionals to navigate the complexities of method equivalency within the broader context of mandatory method verification.
Key Concepts and Regulatory Framework
Distinguishing Between Validation, Verification, and Equivalency
A clear understanding of terminology is critical for planning and regulatory compliance. The following table clarifies the distinct purposes of these related concepts.
Table: Core Concepts in Microbiology Method Management
| Term | Definition | Primary Goal | Typical Context |
|---|---|---|---|
| Method Validation [32] | The initial testing of a method's performance characteristics (e.g., accuracy, precision) to confirm it is fit-for-purpose. | To establish that the method works for its intended use, often for a particular matrix or category. | Developing a new method (in-house or commercial); required before it can be used. |
| Method Verification [2] [32] | The testing performed by a laboratory to demonstrate it can successfully execute a validated method and obtain correct results. | To prove the laboratory's competency in performing a pre-validated method within its specific environment. | Implementing a new, unmodified, FDA-cleared or compendial method in a lab for the first time. |
| Method Equivalency [50] [48] | A formal assessment comparing a new (alternative) method to an existing compendial or reference method. | To demonstrate that the alternative method produces equivalent or better results than the original method. | Replacing an established method with an alternative method (e.g., modern, more efficient). |
Method equivalency is a cornerstone of change management in a regulated environment. As stated in USP stimuli, the lifecycle perspective challenges the notion of validation as a one-time event, treating it instead as a continuous process of ensuring analytical fitness for purpose [49]. When a method changes, equivalency studies bridge the gap between the original validation and the new method's ongoing verification.
The Regulatory Imperative and Lifecycle Approach
Regulatory bodies require that any alternative method used instead of a compendial method must be shown to be equivalent [48]. This is not merely a bureaucratic hurdle; it is a fundamental component of a robust control strategy. Specifications, which include the analytical procedures and acceptance criteria, are critical quality standards that are proposed by the manufacturer and must be approved by regulatory authorities [50].
The modern paradigm, reinforced by ICH Q14 and USP <1220>, embraces an Analytical Procedure Lifecycle approach [49]. This framework integrates method development (Stage 1), method validation (Stage 2), and ongoing performance verification (Stage 3). Method equivalency sits at the intersection of these stages, ensuring that any method change does not detrimentally impact the "reportable result"—the final analytical value used for quality decisions [49].
Strategic Approaches to Demonstrating Equivalency
There is no single, universally prescribed path for demonstrating equivalency. The International Council for Harmonisation (ICH) and USP provide guidance, but the specific strategy often depends on the nature of the method and the risk associated with the change [50] [51]. A risk-based approach is widely recommended, where the rigor of the equivalency study is commensurate with the criticality of the method and the magnitude of the change [51].
Table: Strategies for Demonstrating Method Equivalency
| Strategy | Description | Key Application |
|---|---|---|
| Performance Equivalence | The alternative method demonstrates equivalent or better performance for validation criteria like accuracy, precision, specificity, and detection limits [48]. | A comprehensive approach suitable for all method types, particularly when the new technology differs significantly from the original. |
| Results Equivalence | The alternative and compendial methods generate equivalent numerical results for the same samples. Statistical tolerance intervals are used for comparison [48]. | Ideal for quantitative methods (e.g., microbial enumeration) where direct numerical comparison is possible. |
| Decision Equivalence | The alternative method yields the same pass/fail (or positive/negative) decisions as the compendial method. The frequency of correct decisions must be non-inferior [48]. | Well-suited for qualitative methods (e.g., pathogen detection like Salmonella or Listeria) where the outcome is a binary decision [18]. |
| Acceptable Procedure | The alternative method is validated against a reference material with known properties, rather than directly against the compendial method [48]. | Useful when a well-characterized standard is available, and direct comparison to the compendial method is impractical. |
The following workflow diagram outlines the key decision points and activities in a method equivalency study, from planning through to implementation.
Designing and Executing the Equivalency Study
Critical Experimental Design Parameters
A well-designed study protocol is the foundation of a successful equivalency demonstration. The protocol should be based on a deep knowledge of the methods and the product being tested [50]. Key parameters to define include:
- Sample Selection: Use a sufficient number of samples that are representative of the material routinely tested. This should include samples that challenge the method across its reportable range (e.g., low, medium, and high microbial counts for quantitative tests, or positive and negative samples for qualitative tests) [2]. For a formal study, a minimum of 20 relevant isolates or samples may be used [2].
- Replication Strategy: The study should employ the same replication strategy that will be used for routine sample analysis to generate the reportable result. This means the validation should capture the same sources of variation (e.g., within-run, between-run, different analysts) expected during routine use [49].
- Acceptance Criteria: Predefine statistical and performance-based acceptance criteria. For example, for accuracy in a qualitative test, the percentage of agreement between the two methods should meet the manufacturer's stated claims or a laboratory-defined threshold [2]. USP <1010> presents numerous statistical tools for designing and evaluating equivalency protocols [50].
Statistical and Data Analysis Methods
While basic statistical tools (mean, standard deviation) may sometimes be sufficient, more sophisticated analysis is often required [50]. The revised USP <1225> encourages a combined evaluation of accuracy and precision using statistical intervals that account for both bias and variability simultaneously, providing a more rigorous assessment of total error [49].
For results equivalence, statistical tests like equivalence tests or the calculation of tolerance intervals are used to show that the differences between the two methods' results are within an acceptable margin [48]. For decision equivalence, statistical analysis focuses on the rate of concordance (e.g., the percentage of samples where both methods give the same positive/negative result) and demonstrating non-inferiority [48].
The Scientist's Toolkit: Key Reagents and Materials
Successful execution of an equivalency study relies on high-quality, well-characterized materials. The following table details essential research reagent solutions and their functions.
Table: Essential Research Reagents for Method Equivalency Studies
| Reagent/Material | Function in Equivalency Studies |
|---|---|
| Reference Strains | Well-characterized microorganisms from culture collections (e.g., ATCC) used as positive controls and for challenge tests to confirm method performance [17]. |
| In-House Isolates | Environmental or product-specific isolates used to challenge the method with strains relevant to the laboratory's specific context and to meet regulatory expectations for environmental monitoring [17]. |
| Quality Control (QC) Organisms | Specialized microbial controls with defined profiles used to monitor the validity of the test method, including instrument, operator, and reagent performance during the study [17]. |
| Proficiency Test (PT) Standards | Commercially available samples with assigned values or known properties, used to provide an external benchmark for testing accuracy and to supplement equivalency data [17]. |
| Certified Reference Materials (CRMs) | Pre-measured, single-use materials certified for specific parameters (e.g., bioburden, specific organisms), used for calibrating equipment and validating alternative methods via an "acceptable procedure" [17] [48]. |
Navigating Method Suitability and Fitness for Purpose
Once an alternative method has been demonstrated as equivalent to a compendial method for one product, it is considered validated for use. However, before it can be applied to a new product, the laboratory must demonstrate method suitability (also referred to as fitness-for-purpose for new matrices) [32] [48].
Method suitability testing proves the absence of a product matrix effect that could interfere with the method's outcome. This involves testing the specific product with the validated method to ensure appropriate sample preparation, reagent sensitivity, and recovery of challenge organisms [48]. For qualitative methods, demonstrating recovery of challenge organisms (as in USP <62> and <71>) is often sufficient. Quantitative methods require additional validation of accuracy and precision parameters for the new product [48]. The diagram below illustrates this relationship between method equivalency and suitability.
Demonstrating equivalency is a critical, non-negotiable step in the lifecycle of an analytical procedure. It is the rigorous process that ensures the data generated by modern, efficient methods are as reliable and meaningful as those produced by traditional compendial methods. A successful strategy involves:
- Adopting a Risk-Based Approach: Tailoring the depth of the equivalency study to the criticality of the method and the significance of the change [51].
- Selecting the Right Equivalency Strategy: Choosing among performance, results, or decision equivalence based on whether the method is quantitative or qualitative [48].
- Leveraging the Right Tools: Utilizing well-characterized reference strains, QC organisms, and certified materials to ensure the integrity of the study [17].
- Embedding in a Lifecycle Framework: Viewing equivalency not as a one-off project, but as a key activity within a continuous analytical procedure lifecycle that includes ongoing performance verification [49].
By following this structured approach, microbiology laboratories can confidently implement innovative technologies, enhance efficiency, and maintain the highest standards of data quality and regulatory compliance.
In the tightly regulated world of pharmaceutical microbiology, ensuring the reliability of equipment and software is not merely a best practice but a fundamental requirement. For clinical microbiology laboratories venturing into areas like sterility testing for advanced therapies, adopting the framework of Installation Qualification (IQ), Operational Qualification (OQ), and Performance Qualification (PQ), collectively known as IOPQ, is critical [52]. This terminology, while central to current Good Manufacturing Practices (cGMP) regulated by the US Food and Drug Administration (FDA), is often unfamiliar in clinical laboratories, leading to frequent oversights in its performance and documentation [52].
This qualification process provides the documented evidence that equipment and software are installed correctly, operate according to specifications, and perform consistently and reliably for their intended purpose in the cGMP environment [52] [53]. While the broader thesis of laboratory operations encompasses when method verification is required, this foundational step of IOPQ ensures that the very tools used for testing are fundamentally sound. It is the prerequisite that makes subsequent method verification and validation activities meaningful and reliable.
IOPQ: The Three-Stage Qualification Framework
The IOPQ process is a sequential, evidence-based approach to establishing the fitness of equipment and software. Each stage builds upon the previous one, creating a comprehensive lifecycle of qualification from installation to sustained performance.
Installation Qualification (IQ)
IQ is the first step, serving to verify and document that equipment has been delivered as specified and is installed correctly according to the manufacturer's requirements and approved design specifications in the intended environment [53]. It confirms that the "pieces are in the right place."
- Objective: To ensure the equipment or software is received correctly and installed in a suitable environment with all necessary utilities and services.
- Key Documentation: Purchase order, manufacturer's delivery slips, equipment manuals, installation drawings, and certifications for installation personnel.
- Typical Verification Points:
- Verify correct model and serial number against purchase specifications.
- Confirm installation site prerequisites (e.g., space, power, environmental controls, network connectivity).
- Document installation of hardware, firmware, and software.
- Ensure calibration of critical components is current.
Operational Qualification (OQ)
Following a successful IQ, OQ is performed to demonstrate that the installed equipment or software will function according to its operational specifications in the selected environment [52] [53]. It answers the question, "Does it operate as intended under controlled conditions?"
- Objective: To provide documented evidence that system controls and functions operate as specified across their intended ranges.
- Key Documentation: A protocol detailing tests, acceptance criteria, and raw data results.
- Typical Verification Points:
- Verify system controls and alarm functions (e.g., temperature alarms in an incubator, user access controls in software).
- Test operational ranges (e.g., temperature uniformity across a range of setpoints in a controlled temperature unit).
- Execute predefined test scripts for software functions, including data integrity features aligned with ALCOA+ principles (Attributable, Legible, Contemporaneous, Original, and Accurate) [54].
Performance Qualification (PQ)
The final stage, PQ, provides documented evidence that the equipment and software, as integrated systems, can perform consistently and effectively according to pre-defined criteria under actual production or testing conditions [52] [53]. It proves that "it works consistently for my specific use case."
- Objective: To ensure the system consistently produces results that meet acceptance criteria under routine operating conditions.
- Key Documentation: A protocol using actual or simulated product (e.g., challenge organisms, production samples) to demonstrate performance.
- Typical Verification Points:
- For a blood culture system: Demonstrate reliable detection and no cross-contamination using inoculated blood culture bottles.
- For a Laboratory Information Management System (LIMS): Verify end-to-end data workflow accuracy from sample login to final report generation.
- Establish that the system maintains stability and performance over an appropriate time period (e.g., 3 consecutive runs).
The logical relationship and workflow between these stages can be visualized as a sequential, interdependent process.
IOPQ vs. Clinical Laboratory Requirements
A significant challenge for clinical microbiology laboratories is the cultural and regulatory shift required when moving from traditional clinical standards to cGMP environments. The table below summarizes the key distinctions.
Table 1: Contrasting IOPQ in cGMP with Traditional Clinical Laboratory Practices
| Aspect | cGMP Environment (IOPQ Focus) | Traditional Clinical Lab (CLIA/CAP Focus) |
|---|---|---|
| Primary Goal | Ensure product quality and patient safety by proving process/equipment reliability [52] [53]. | Ensure accuracy and reliability of individual patient test results [6]. |
| Regulatory Driver | FDA cGMP; focus on process validation and equipment qualification [52]. | CLIA/CMS; focus on analytical test method verification [6] [52]. |
| Key Terminology | Installation, Operational, and Performance Qualification (IOPQ) [52]. | Method verification/validation; IQ/OQ often overlooked [52]. |
| Documentation Emphasis | Extensive, prospective documentation (protocols) proving control over the entire system lifecycle [53]. | Documentation of analytical performance characteristics (accuracy, precision) for test methods [6]. |
| Example: Incubator | Full IOPQ: IQ (power, location), OQ (temp mapping, alarm function), PQ (growth promotion with product media) [52]. | Verification may be limited to temperature monitoring and growth promotion tests, often without formal IQ/OQ [52]. |
As shown in Table 1, while the College of American Pathologists (CAP) has requirements (COM.30550 and COM.30575) that touch on qualification, the depth and formality of a full IOPQ process under cGMP are often not fully realized in the clinical setting [52]. This gap becomes critically important when laboratories undertake tests falling under cGMP, such as sterility testing for cellular therapies.
Detailed Experimental Protocols for Key IOPQ Activities
To translate the IOPQ framework into actionable steps, detailed experimental protocols are essential. The following methodologies provide a template for qualifying common systems in a microbiology lab operating under cGMP.
Protocol for Qualifying a Controlled Temperature Unit (e.g., Incubator)
This protocol outlines the PQ stage for an incubator used in a sterility test method.
- 1. Objective: To demonstrate that the incubator maintains conditions suitable for the growth of compendial strains when used with specific culture media, simulating routine sterility testing conditions.
- 2. Materials and Reagents:
- Qualified incubator (IQ and OQ completed).
- Sterile growth media (e.g., Tryptic Soy Broth, Fluid Thioglycollate Medium).
- Reference strains: <Staphylococcus aureus> (ATCC 6538), <Bacillus subtilis> (ATCC 6633), <Pseudomonas aeruginosa> (ATCC 9027), <Clostridium sporogenes> (ATCC 11437).
- 3. Methodology:
- Inoculate separate containers of media with a low inoculum (fewer than 100 CFU) of each challenge organism.
- Include uninoculated negative controls for each media type.
- Place all containers in the incubator at the specified temperature (e.g., 20-25°C for bacteria, 30-35°C for fungi and aerobes).
- Arrange samples to represent the entire chamber volume, including potential cold/hot spots identified during OQ mapping.
- Incubate for the sterility test duration (e.g., 14 days).
- Observe for growth visually at defined intervals (e.g., days 3, 7, and 14).
- 4. Acceptance Criteria:
- All inoculated media containers must show visible growth within the recommended time frame (e.g., 3 days for bacteria).
- All negative control containers must show no growth throughout the 14-day incubation period.
- 5. Data Analysis and Reporting: Document the time to visible growth for each organism. Any deviation from acceptance criteria must be investigated, and the root cause addressed before the incubator is released for cGMP use.
Protocol for Qualifying a Blood Culture System for Sterility Testing
This protocol describes the PQ for an automated blood culture system adapted for sterility testing of cellular therapy products.
- 1. Objective: To verify that the blood culture system can reliably detect low levels of contaminating microorganisms in a simulated product matrix.
- 2. Materials and Reagents:
- Qualified blood culture instrument (IQ/OQ complete).
- Blood culture bottles (e.g., aerobic and anaerobic).
- Reference strains: <Staphylococcus epidermidis> (ATCC 12228), <Propionibacterium acnes> (ATCC 6919), <Candida albicans> (ATCC 10231).
- Sterile cell culture medium (simulating the product matrix).
- 3. Methodology:
- Prepare a low-concentration inoculum for each challenge organism (e.g., 10-100 CFU).
- Aseptically inoculate blood culture bottles with the challenge organism in the simulated product matrix.
- Inoculate at least three replicates per organism.
- Load bottles into the qualified system and run for the standard protocol duration (e.g., 5-7 days).
- Include uninoculated negative controls.
- 4. Acceptance Criteria:
- The system must flag all inoculated bottles as positive within the expected detection time for each organism.
- All negative control bottles must remain negative for the duration of the run.
- There must be no evidence of cross-contamination between bottles.
- 5. Data Analysis and Reporting: Document the time to detection for each positive bottle. Confirm organism identity from positive bottles to ensure the system detected the correct challenge organism. The system is deemed qualified only upon meeting all acceptance criteria.
The Scientist's Toolkit: Essential Research Reagent Solutions
Executing robust IOPQ studies requires the use of well-characterized materials. The following table details key reagents and their critical functions in qualification experiments.
Table 2: Essential Reagents for Microbial Qualification Studies
| Reagent/Material | Function in IOPQ Experiments | Key Characteristics & Standards |
|---|---|---|
| Reference Strains | Challenge organisms used in PQ studies (e.g., for growth promotion, method validation) to demonstrate system performance [52]. | Must be traceable to recognized culture collections (e.g., ATCC); well-defined physiological characteristics [55]. |
| Culture Media | Supports the growth of challenge organisms and production microflora; the "matrix" for the performance test [52]. | Must meet compendial specifications (e.g., USP, EP, JP); require their own quality control (sterility, growth promotion) [55]. |
| Microbial Enumeration Tests | Standardized methods to quantify viable microorganisms, used for preparing challenge inocula and verifying test results [55]. | Follows harmonized pharmacopeial methods like USP <61>; ensures accuracy and reproducibility of microbial counts [55]. |
Integration with Broader Method Verification Frameworks
The successful completion of IOPQ for equipment and software does not replace the need for analytical test method verification or validation; rather, it enables it. In a cGMP environment, IOPQ is the foundational step that ensures the tools are reliable. Once equipment is qualified, the laboratory must still demonstrate that the specific analytical method (e.g., a sterility test or microbial enumeration test) is suitable for its intended purpose, a process defined by standards such as the ISO 16140 series for microbiological methods [13].
The relationship between these activities is hierarchical. IOPQ qualifies the system, while method validation/verification qualifies the procedure performed on that system. For an unmodified, FDA-cleared test used in a clinical lab, this subsequent step is a method verification, confirming accuracy, precision, reportable range, and reference range as required by CLIA [6]. For laboratory-developed tests or modified methods, a full method validation is required [6] [52]. The entire process, from equipment qualification to ongoing method monitoring, ensures data integrity and product quality throughout the data life cycle, adhering to ALCOA+ principles [54].
In the evolving landscape of clinical microbiology, where laboratories increasingly support advanced therapeutic products, the rigorous framework of IOPQ is no longer optional. It is a critical component of the cGMP quality system, providing the documented evidence that equipment and software are installed correctly, operate as intended, and perform reliably for their specific tasks. By systematically implementing IOPQ, laboratories lay a solid foundation of data integrity and operational control. This foundation, in turn, supports all subsequent analytical work, ensuring that method verification and validation activities are built upon a base of proven reliability, ultimately guaranteeing the safety and quality of products that reach patients.
In microbiology laboratory research, the reliability of test results is paramount for patient safety, product quality, and regulatory compliance. Method verification and validation are critical laboratory processes that ensure analytical methods are fit for their intended purpose. Within a broader thesis on when method verification is required, understanding the distinct frameworks provided by leading standards organizations is fundamental for researchers, scientists, and drug development professionals. This technical guide provides an in-depth comparison of three cornerstone standards: the International Organization for Standardization (ISO) 16140 series, the United States Pharmacopeia (USP), and the Clinical and Laboratory Standards Institute (CLSI) guidelines. Each provides a structured approach for evaluating microbiological methods, yet their applications, requirements, and focal points differ significantly across clinical, pharmaceutical, and food safety sectors.
The following diagram illustrates the fundamental distinction between method validation and verification, which is a core concept across all standards and critical for understanding their application.
Understanding Method Verification and Validation
Before delving into comparative frameworks, it is essential to define the core concepts. Although sometimes used interchangeably, method validation and method verification represent distinct processes with different objectives and triggers.
Method Validation is "a process by which it is established, through laboratory studies, that the performance characteristics of a method meet the requirements for its intended analytical applications" [1]. This process is performed to establish the performance characteristics of a method and is required for laboratory-developed tests (LDTs), non-FDA cleared tests, and modified FDA-cleared tests [2].
Method Verification, in contrast, is "the ability to verify that a method can perform a method reliably and precisely for its intended purpose" [1]. It is a one-time study to confirm that a pre-validated or compendial method (e.g., an FDA-cleared or USP method) performs according to its established claims within a specific laboratory's environment [2]. For compendial methods such as those in the USP, the implementation typically involves verifying that the validated method is suitable for the specific sample and lab setting [1].
The requirement for verification is a continuous process throughout a product's lifecycle. It is not a "one and done" activity; re-verification or revalidation becomes necessary when changes occur, such as formulation or concentration updates, material source changes, manufacturing process updates, or reagent vendor changes [1].
Comparative Analysis of ISO, USP, and CLSI Frameworks
The following section provides a detailed comparison of the three standardization bodies, highlighting their primary scope, key documents, and performance parameters.
Core Scope and Application
Table 1: Core Scope and Application of ISO, USP, and CLSI Standards
| Standard | Primary Scope & Industry | Key Documents & Guidance | Governance & Development |
|---|---|---|---|
| ISO 16140 Series | Food and animal feed chain; environmental samples in food/feed production [56] [57]. | ISO 16140-3:2021: Guidance on verification of microbiological methods [56].ISO 16140-4:2020: Specifies protocols for single-laboratory validation of methods for microbiology in the food chain [57]. | Developed by ISO Technical Committee (TC) 34/SC 9 through a working group (WG) of international experts [56] [57]. |
| USP (United States Pharmacopeia) | Pharmaceutical, dietary supplements, probiotics, botanicals, and drug products [58] [59]. | <1223>: Validation of Alternative Microbiological Methods [1].<1225>: Validation of Compendial Procedures [1].<61>, <62>, <71>: Compendial methods for microbial enumeration, sterility, etc. [58]. | A non-profit organization establishing legally recognized standards for medicines and other products in the United States [58]. |
| CLSI (Clinical & Laboratory Standards Institute) | Clinical diagnostics and medical laboratories; laboratory-developed tests (LDTs) and commercial IVDs [60] [61]. | EP19: A framework for using CLSI documents to evaluate clinical laboratory procedures [60] [2].M52: Verification of Commercial Microbial Identification and AST Systems [2].EP12: User protocol for qualitative test performance [2]. | A member-based non-profit developing international laboratory standards via a consensus process involving industry, government, and professionals [60] [61]. |
Performance Parameters and Experimental Protocols
Each framework defines a set of performance parameters that must be tested during validation or verification. The specific parameters required depend on whether the method is quantitative or qualitative.
Table 2: Key Performance Parameters and Their Definitions
| Parameter | Definition | Primary Application |
|---|---|---|
| Accuracy | The closeness of agreement between a test result and an accepted reference value [1]. | Foundational for all frameworks. |
| Precision | The closeness of agreement between a series of measurements from multiple sampling; can include repeatability, intermediate precision, and reproducibility [1]. | Foundational for all frameworks. |
| Specificity | The ability to assess the analyte unequivocally in the presence of potentially interfering components [1]. | Critical for methods distinguishing between organisms or testing complex matrices. |
| Limit of Detection (LOD) | The lowest amount of detectable analyte or microorganisms in a sample [1]. | Essential for qualitative methods (e.g., pathogen detection). |
| Limit of Quantitation (LOQ) | The lowest amount of analyte that can be quantitatively determined with suitable precision and accuracy [1]. | Essential for quantitative methods (e.g., microbial enumeration). |
| Linearity & Range | The ability to obtain results proportional to the analyte amount, and the interval between upper and lower analyte concentrations for which suitability is demonstrated [1]. | Required for quantitative methods to prove the validated working range. |
| Robustness | The capacity of a method to remain unaffected by small, deliberate variations in method parameters [1]. | Evaluated during validation to understand the method's reliability under normal operational variations. |
The experimental protocols for verifying a qualitative method in a clinical laboratory, as guided by CLSI, must meet specific criteria as shown in the workflow below.
Detailed Experimental Protocols for a Qualitative Method Verification (CLSI-based):
Accuracy Verification:
- Methodology: Compare results from the new method against a comparative method (e.g., a reference method or a previously validated method).
- Protocol: Test a minimum of 20 clinically relevant isolates, comprising a combination of positive and negative samples. These can be from reference materials, proficiency test samples, or de-identified clinical specimens [2].
- Data Analysis: Calculate the percentage agreement: (Number of results in agreement / Total number of results) × 100. The acceptance criteria must meet the manufacturer's stated claims or a level determined by the laboratory director [2].
Precision Verification:
- Methodology: Assess the variance within a run, between runs, and between different operators.
- Protocol: Test a minimum of 2 positive and 2 negative samples. These should be tested in triplicate over 5 days by 2 different operators. If the system is fully automated, operator variance may not be required [2].
- Data Analysis: Calculate the percentage agreement for the repeated results. The acceptance criteria should align with the manufacturer's claims or laboratory-defined goals [2].
Reportable Range Verification:
- Methodology: Confirm the upper and lower limits of what the test system can report.
- Protocol: Verify with a minimum of 3 known positive samples. For qualitative assays, this involves testing samples positive for the analyte [2].
- Data Analysis: The reportable range is defined as what the laboratory establishes as a reportable result (e.g., "Detected" or "Not detected"), verified by testing samples within this range [2].
Reference Range Verification:
- Methodology: Confirm the normal or expected result for the tested patient population.
- Protocol: Verify using a minimum of 20 isolates. Use de-identified clinical samples or reference samples with a result known to be standard for the laboratory’s patient population (e.g., samples negative for MRSA when verifying an MRSA detection assay) [2].
- Data Analysis: The reference range is verified by testing samples representative of the laboratory's patient population. If the manufacturer's range is not representative, the laboratory must redefine it using its own population data [2].
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful method evaluation requires specific, high-quality reagents and materials. The following table details essential components for conducting suitability testing, a critical requirement for USP methods, and other verification/validation activities.
Table 3: Essential Reagents and Materials for Method Evaluation
| Reagent / Material | Function & Application in Evaluation |
|---|---|
| Reference Microorganisms | Certified strains used for inoculation (e.g., in suitability testing) to demonstrate the method can recover microbes from the product matrix. Strains are often specified in compendial chapters [58]. |
| Endotoxin Reference Standard | A standardized endotoxin used to validate or verify the Bacterial Endotoxins Test (e.g., USP <85>), ensuring the test system is capable of detecting pyrogenic contaminants [58]. |
| Inactivating Agents / Neutralizers | Substances (e.g., lecithin, polysorbate) incorporated into diluents or media to neutralize antimicrobial properties of the product being tested, crucial for overcoming suitability test failures [59]. |
| Competency Kit (e.g., Viable Surface Sampling) | Tools containing known, stable microbial populations used to validate and periodically verify the competency of personnel and processes in environmental monitoring [58]. |
| Quality Controls | Positive and negative controls, which can be commercial or derived from reference materials, used during verification studies to ensure the test is performing correctly on a given day [2]. |
The landscape of method evaluation in microbiology is structured by the robust frameworks of ISO, USP, and CLSI. While these organizations share the common goal of ensuring reliable and accurate test results, their primary applications are distinct: ISO 16140 serves the food and feed industry, USP provides legally recognized standards for pharmaceuticals and dietary supplements, and CLSI offers detailed guidelines for clinical diagnostics. A thorough understanding of when method verification is required—such as when implementing a new, unmodified compendial method—and when full validation is necessary—for laboratory-developed tests or modified methods—is fundamental for regulatory compliance and, ultimately, patient and consumer safety. As methods evolve, particularly with the adoption of rapid microbiological methods, the principles enshrined in these standards provide the necessary foundation for integrating innovation into the laboratory without compromising quality.
Conclusion
Method verification is not a one-time event but a fundamental component of a continuous quality management system in microbiology laboratories. It is rigorously required when implementing unmodified FDA-cleared tests, introducing new sample matrices, or adhering to evolving regulatory standards like CLIA, ISO 15189, and cGMP. A successful verification strategy hinges on a clear understanding of its distinction from full validation, a meticulously planned experimental design, and robust post-implementation monitoring. For researchers and drug development professionals, mastering these processes is paramount for ensuring patient safety, product quality, and data integrity. As the field advances with new technologies and complex therapies, the principles of rigorous verification and validation will remain the cornerstone of reliable and compliant microbiological diagnostics.
References
- 1. Method Validation/Verification: How Important is it in Your ... [https://www.americanpharmaceuticalreview.com/Featured-Articles/597641-Method-Validation-Verification-How-Important-is-it-in-Your-QC-Microbiology-Laboratory/]
- 2. Planning a Method Verification Study in Clinical ... [https://asm.org/articles/2022/january/planning-a-method-verification-study-in-clinical-m]
- 3. Comparing Published Gut Microbiome Taxonomic Data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8740627/]
- 4. Critical comparison of statistical methods for quantifying ... [https://www.sciencedirect.com/science/article/pii/S016816052200407X]
- 5. Verification and Validation of Tests Used in the Clinical ... [https://www.sciencedirect.com/science/article/abs/pii/S019643991500077X]
- 6. Planning a Method Verification Study in Clinical ... [https://asm.org/articles/2022/january/planning-a-method-verification-study-in-clinical-m?sr_id=23df675c-421d-4816-a54e-4d751ba62574&sr_pos=3]
- 7. How to verify and validate a clinical microbiology test ... [https://pubmed.ncbi.nlm.nih.gov/38977077/]
- 8. In Vitro Diagnostic Regulation (IVDR)—Frequently Asked ... [https://www.thermofisher.com/us/en/home/clinical/ivdr/faqs.html]
- 9. EU IVDR Performance Validation: Key Steps and ... [https://www.makrocare.com/blog/eu-ivdr-performance-validation-report-steps-and-requirements/]
- 10. Current Good Manufacturing Practice (CGMP) Regulations [https://www.fda.gov/drugs/pharmaceutical-quality-resources/current-good-manufacturing-practice-cgmp-regulations]
- 11. Analytical Method Quality & Pharmaceutical Development ... [https://www.rhoworld.com/analytical-method-quality-throughout-the-pharmaceutical-development-lifecycle/]
- 12. Phase Appropriate Method Validation in Drug Development [https://vicihealthsciences.com/phase-appropriate-method-validation/]
- 13. Method validation and method verification - Introduction - ISO [https://committee.iso.org/sites/tc34sc9/home/essential-information/content-left-area/validation-of-methods/method-validation-and-method-ver.html]
- 14. FDA Hyper Focused on Validations and Verifications [https://certified-laboratories.com/blog/fda-hyper-focused-on-validations-and-verifications/]
- 15. All you need to know about equipment validation for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12421869/]
- 16. NonClinical Dose Formulation Analysis Method Validation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2976985/]
- 17. Mastering Quality: New Method Validation, QC Standards, PT [https://www.rapidmicrobiology.com/news/mastering-quality-new-method-validation-qc-standards-and-pt-a-rapidmicrobiology-special-focus]
- 18. Quantitative and Qualitative Microbiological Testing [https://www.eurofinsus.com/food-testing/resources/small-world-it-is-quality-and-quantity-that-matter/]
- 19. Semi-quantitative procedures; half professional or ... [https://myadlm.org/science-and-research/scientific-shorts/2023/semi-quantitative-procedures-half-professional-or-half-amateur-what-is-the-other-half]
- 20. Applying USP 1117 to the Sterile Compounding ... [https://www.americanpharmaceuticalreview.com/Featured-Articles/617763-Applying-USP-1117-to-the-Sterile-Compounding-Microbiology-Lab/]
- 21. Microbiology & Chemical Assay Validation [https://www.labmanager.com/microbiology-chemical-assay-validation-34505]
- 22. Sample size calculation in biomedical, clinical and ... [https://link.springer.com/article/10.1007/s43994-024-00153-x]
- 23. Sample size, power and effect size revisited: simplified and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7745163/]
- 24. Sample size determination: A practical guide for health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10000262/]
- 25. power and sample size calculation for microbiome studies [https://www.sciencedirect.com/science/article/pii/S1933021922017366]
- 26. Specimen Collection Practices for Microbiologic Culture [https://health.ucdavis.edu/blog/lab-best-practice/specimen-collection-practices-for-microbiologic-culture/2020/07]
- 27. A Guide to Utilization of the Microbiology Laboratory for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7108105/]
- 28. Method Validation vs Method Verification: Which is Better ... [https://www.labmanager.com/method-validation-vs-method-verification-which-is-better-for-use-in-laboratories-33982]
- 29. Final 5 CLIA Rule. Part V: Method Validation Process and ... [https://www.westgard.com/clia-a-quality/clia-final-rule/cliafinalrule5.html]
- 30. - assuring the... - New Food Magazine Microbiological methods [https://www.newfoodmagazine.com/article/97500/microbiological-methods-assuring-the-alternatives/]
- 31. Molecular Diagnostics - Part 3: Accuracy and Precision [https://blog.seracare.com/molecular-serology-blog/verification-part3]
- 32. Food Safety Testing: Understanding Microbiological ... [https://www.eurofinsus.com/food-testing/resources/food-safety-testing-understanding-microbiological-method-validation-verification-and-fitness-for-purpose/]
- 33. Top Mistakes in Analytical Method Validation and How to ... [https://www.pharmoutsourcing.com/Featured-Articles/350046-Top-Mistakes-in-Analytical-Method-Validation-and-How-to-Avoid-Them/]
- 34. Common Mistakes in Method Validation and How to Avoid ... [https://www.linkedin.com/pulse/common-mistakes-method-validation-how-avoid-them-part-oona-mcpolin]
- 35. Discrepant Analysis: How Can We Test a Test? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC86720/]
- 36. Key Phases of the Process Validation Lifecycle [https://inglasia.com/process-validation-lifecycle-phases/]
- 37. Passing the Test: Understanding Proficiency Testing [https://www.spectroscopyonline.com/view/passing-the-test-understanding-proficiency-testing]
- 38. New 'Lab of the Future' Survey Reveals More than Half ... [https://www.clinicallab.com/new-lab-of-the-future-survey-reveals-more-than-half-of-lab-professionals-reported-unplanned-downtime-28183]
- 39. Stability and Performance: The Two Most Important ... [https://www.ligolab.com/post/stability-and-performance-the-two-most-important-aspects-of-a-modern-laboratory-operation]
- 40. Basic QC Practices - The Records [https://www.westgard.com/lessons/basic-qc-practices-l/lesson19full.html]
- 41. Improve Productivity by Building Better Systems, Not ... [https://www.labmanager.com/improve-productivity-by-building-better-systems-not-bottlenecks-34317]
- 42. - AB Scientific Quality Control Organisms [https://www.abscientific.com/industrial_solution/quality-control-organisms/]
- 43. Microbial QC and Proficiency Testing Controls [https://www.rapidmicrobiology.com/news/your-trusted-source-for-microbial-qc-controls-and-proficiency-testing]
- 44. | Thermo Fisher Scientific - ZA Microbiology Quality Control [https://www.thermofisher.com/za/en/home/industrial/microbiology/microbiology-quality-control.html]
- 45. Promoting Lab Equity with Laboratory Developed Tests [https://asm.org/articles/2024/january/promoting-lab-equity-with-laboratory-developed-tes]
- 46. Modernization of CLIA: Laboratory Developed Tests (LDTs) [https://myadlm.org/advocacy-and-outreach/position-statements/2021/modernization-of-clia-ldts]
- 47. Test Approval | New York State Department of Health, ... [https://www.wadsworth.org/regulatory/clep/clinical-labs/obtain-permit/test-approval]
- 48. What Are Method Suitability Testing & Method Equivalency ... [https://www.linkedin.com/pulse/what-method-suitability-testing-equivalency-mycoscience]
- 49. USP <1225> Revised: Aligning Compendial Validation with ... [https://investigationsquality.com/2025/11/13/usp-1225-revised-aligning-compendial-validation-with-ich-q2r2-and-q14s-lifecycle-vision/]
- 50. Specification Equivalence: A Practical Approach to Method ... [https://www.biopharminternational.com/view/specification-equivalence-a-practical-approach-to-method-and-acceptance-criteria-equivalence]
- 51. Analytical Method Comparability in Registration and Post ... [https://www.pharmtech.com/view/analytical-method-comparability-registration-and-post-approval-stages-risk-based-approach]
- 52. you need to know about equipment validation for sterility ... [https://pubmed.ncbi.nlm.nih.gov/40788093/]
- 53. Method Qualification and Validation in the Pharmaceutical ... [https://www.biomerieux-industry.com/pharma-quality-control/resources/white-papers/method-qualification-and-validation-pharma-industry]
- 54. Introduction to Pharmaceutical Data Items and Their Structure [https://astrixinc.com/article/introduction-to-pharmaceutical-data-items-and-their-structure/]
- 55. <61> Microbial Enumeration Tests [https://www.usp.org/harmonization-standards/pdg/general-methods/microbial-enumeration]
- 56. ISO 16140-3:2021 Method Verification Roundtable [https://www.neogen.com/en/neocenter/resources/iso-16140-32021-method-verification-roundtable-perspectives-from-the-industry/]
- 57. Method validation - ISO 16140-4:2020 [https://www.iso.org/standard/66325.html]
- 58. Microbiological quality control testing [https://www.usp.org/microbiology]
- 59. USP Testing | Frequently Asked Questions [https://www.eurofinsus.com/food-testing/resources/usp-microbiology-services-frequently-asked-questions/]
- 60. Method Evaluation | Areas of Focus [https://clsi.org/standards-development/specialty-areas/method-evaluation/]
- 61. CLSI: Clinical & Laboratory Standards Institute [https://clsi.org/]