Fundamentals of Microbiological Method Verification: A Comprehensive Guide to Study Design for Reliable Lab Results
This article provides researchers, scientists, and drug development professionals with a comprehensive framework for designing robust microbiological method verification studies.
Fundamentals of Microbiological Method Verification: A Comprehensive Guide to Study Design for Reliable Lab Results
Abstract
This article provides researchers, scientists, and drug development professionals with a comprehensive framework for designing robust microbiological method verification studies. Covering foundational concepts, practical methodology, troubleshooting strategies, and validation protocols, it translates regulatory requirements into actionable verification plans. Readers will learn to differentiate verification from validation, establish acceptance criteria, address common pitfalls, and implement defensible verification protocols compliant with CLIA, ISO 16140, and other relevant standards for both clinical and pharmaceutical quality control environments.
Core Principles and Regulatory Landscape of Microbiological Method Verification
In laboratory environments, particularly within pharmaceutical development, clinical diagnostics, and food safety, the demand for accurate and reliable testing is non-negotiable [1]. Two cornerstone processes—method validation and method verification—serve as critical pillars to ensure this reliability. While the terms are sometimes used interchangeably, they represent distinct concepts with different applications, scopes, and regulatory implications. Understanding this distinction is not merely an academic exercise; it is a fundamental requirement for researchers and scientists designing microbiological studies, ensuring regulatory compliance, and maintaining data integrity. This guide provides an in-depth technical examination of method verification versus validation, specifically framed within the context of microbiological method verification study design research.
Core Definitions and Conceptual Framework
What is Method Validation?
Method validation is a comprehensive, documented process that proves an analytical method is acceptable for its intended use [1]. It establishes the performance characteristics and limitations of a method and its domains of applicability [2]. This process is typically undertaken when a method is newly developed, significantly altered, or used for a new product or formulation [2].
In practice, validation involves rigorous testing and statistical evaluation to assess parameters such as accuracy, precision, specificity, detection limit, quantitation limit, linearity, and robustness [1]. The International Council for Harmonisation (ICH) guideline Q2(R2) provides a recognized framework for the validation of analytical procedures, underscoring its global regulatory importance [3].
What is Method Verification?
Method verification, in contrast, is the process of confirming that a previously validated method performs as expected in a specific laboratory setting [1]. It is a one-time study meant to demonstrate that a test performs in line with previously established performance characteristics when used as intended by the manufacturer and under the actual conditions of the receiving laboratory [4] [2].
Essentially, while validation asks, "Does this method work for its intended purpose in general?", verification asks, "Can my laboratory successfully perform this already-validated method and achieve the established performance standards?" [5].
The table below synthesizes the key differences between these two critical processes.
Table 1: Core Differences Between Method Validation and Method Verification
| Comparison Factor | Method Validation | Method Verification |
|---|---|---|
| Primary Objective | To establish and document method performance characteristics for a novel or modified method [1] [2]. | To confirm a lab can reproduce the performance of a pre-validated method [1] [5]. |
| Typical Initiating Event | Development of a new method; significant method modification; use in a new matrix [4] [2]. | Adoption of an unmodified, FDA-cleared or compendial method (e.g., USP, EP) in a new lab [4] [2]. |
| Scope | Comprehensive assessment of all relevant performance parameters [1]. | Limited, targeted assessment of critical parameters to confirm performance in a specific context [1] [4]. |
| Regulatory Basis | ICH Q2(R2), USP <1225> [1] [3]. | CLIA regulations, USP <1226> [4] [2]. |
| Resource Intensity | High (time, cost, expertise) [1]. | Moderate, more efficient [1]. |
Method Verification in Detail: A Focus on Microbiological Study Design
For microbiological methods, verification studies are required by the Clinical Laboratory Improvement Amendments (CLIA) for non-waived systems before reporting patient results [4]. The following section outlines the key considerations and methodologies for designing a robust verification study.
Determining the Study Purpose and Type
The first step is unequivocally determining whether the activity is a verification or a validation. For a clinical microbiology lab, a verification is for unmodified FDA-approved or cleared tests, while a validation is necessary for laboratory-developed tests (LDTs) or modified FDA-approved methods [4]. Furthermore, the assay type—qualitative, quantitative, or semi-quantitative—must be defined as it directly influences the verification design and acceptance criteria [4].
Establishing the Verification Study Design and Protocols
For an unmodified FDA-approved test, laboratories are required to verify specific performance characteristics. The following table details the experimental protocols for verifying qualitative and semi-quantitative microbiological assays, as suggested by CLIA standards [4].
Table 2: Method Verification Protocols for Qualitative/Semi-Quantitative Microbiological Assays
| Performance Characteristic | Minimum Sample & Design Requirements | Recommended Samples & Sources | Calculation & Acceptance Criteria |
|---|---|---|---|
| Accuracy | Minimum of 20 clinically relevant isolates; combination of positive and negative samples [4]. | Standards/controls, reference materials, proficiency tests, de-identified clinical samples tested in parallel with a validated method [4]. | (Number of results in agreement / Total results) × 100. Must meet manufacturer's stated claims or lab director's determination [4]. |
| Precision | Minimum of 2 positive and 2 negative samples tested in triplicate for 5 days by 2 operators (if not fully automated) [4]. | Controls or de-identified clinical samples [4]. | (Number of results in agreement / Total results) × 100. Must meet manufacturer's stated claims or lab director's determination [4]. |
| Reportable Range | Minimum of 3 known positive samples [4]. | Samples positive for the detected analyte; for semi-quantitative, use samples near the upper/lower manufacturer cutoffs [4]. | Verification that the laboratory can report results as defined (e.g., "Detected," "Not detected," Ct value cutoff) [4]. |
| Reference Range | Minimum of 20 isolates [4]. | De-identified clinical or reference samples representing the laboratory's typical patient population [4]. | Verification that the manufacturer's reference range is appropriate for the lab's patient population; re-definition may be necessary [4]. |
The Verification Plan
A formal, written verification plan is a cornerstone of a successful study. This document, which requires review and sign-off by the laboratory director, should include [4]:
- The type of verification and the purpose of the study.
- A detailed description of the test and its intended use.
- A comprehensive study design outlining the number and types of samples, quality controls, replicates, and performance characteristics to be evaluated with defined acceptance criteria.
- A list of all required materials, equipment, and resources.
- Safety considerations and a projected timeline for completion.
The Scientist's Toolkit: Key Reagents and Materials for Method Verification
The successful execution of a method verification study relies on a suite of critical reagents and materials. The selection of these components is vital to ensure the integrity and reproducibility of the study.
Table 3: Essential Research Reagent Solutions for Microbiological Verification
| Reagent/Material | Function in Verification Study | Application Example |
|---|---|---|
| Reference Strains | Provide known, standardized microorganisms for spiking studies to assess accuracy, precision, and detection limits. | Using ATCC strains of S. aureus and P. aeruginosa to challenge a new sterility test method [4]. |
| Clinical Isolates | Offer real-world, clinically relevant microorganisms to ensure the method performs with diverse strains found in the patient population. | Using 20 de-identified patient isolates to verify a new MRSA detection assay [4]. |
| Certified Reference Materials | Act as a gold standard for method comparison, providing a benchmark for accuracy and helping to establish the reportable range. | Using a certified quantitative microbial standard to verify the reportable range of an automated cell counter [5]. |
| Quality Controls (Positive/Negative) | Monitor the daily performance and consistency of the test system, ensuring it is functioning correctly throughout the verification process. | Including a positive control (a known weak positive) and a negative control in each run of a PCR-based verification study [4]. |
| Selective and Non-Selective Media | Support the growth and differentiation of target microorganisms; used in comparative studies for accuracy assessment. | Using Tryptic Soy Broth (TSB) for the recovery of a wide range of microorganisms in a growth-based rapid method [6]. |
The Regulatory and Lifecycle Context
The Evolving Regulatory Landscape
Regulatory guidance clearly demarcates the requirements for validation and verification. Validation is governed by guidelines such as ICH Q2(R2) and USP <1225>, while verification is addressed in documents like USP <1226> and CLIA regulations [1] [4] [2]. Furthermore, the regulatory environment is evolving to accommodate modern techniques. The recent publication of USP <73> on ATP-bioluminescence for short shelf-life products, effective August 2025, lowers the barrier for using these rapid microbiological methods (RMMs) by no longer requiring alternative method validation, acknowledging their reliability [6].
The Method Lifecycle and "Fitness-for-Purpose"
Method validation and verification are part of a broader method lifecycle. A newer, crucial concept is "Fitness-for-Purpose"—a demonstration that a method delivers expected results in a previously unvalidated matrix [5]. This is particularly relevant when applying a validated method to a new food matrix or sample type. The decision to perform a full validation, a verification, or a "fitness-for-purpose" study depends on the degree of change and the associated public health or detection risk [5].
The distinction between method validation and method verification is a fundamental concept that underpins reliable laboratory testing in drug development and clinical research. Validation is a comprehensive process to establish a method's performance, while verification is a targeted confirmation that a pre-validated method works in a specific lab's hands. For microbiological methods, a well-designed verification study—rooted in a solid plan, appropriate sample sizes, and clear acceptance criteria—is not just a regulatory hurdle but a critical component of quality assurance. As the field advances with new rapid microbiological methods and evolving regulatory guidance, a deep understanding of these principles ensures that researchers and scientists can navigate the complexities of method qualification, ultimately guaranteeing the safety and efficacy of pharmaceutical products and the accuracy of clinical diagnostics.
For researchers and scientists designing microbiological method verification studies, navigating the intersecting requirements of major regulatory frameworks is fundamental to ensuring data integrity, patient safety, and regulatory compliance. The Clinical Laboratory Improvement Amendments (CLIA) in the U.S., the international quality standard ISO 15189 for medical laboratories, and the European Union's In Vitro Diagnostic Regulation (IVDR) collectively shape the standards for laboratory testing. While CLIA provides a mandatory, compliance-focused structure for U.S. laboratories, ISO 15189 is a voluntary, international standard emphasizing continual improvement and risk management. The IVDR presents a product-centric regulatory framework for manufacturers placing devices on the European market. This guide provides an in-depth technical comparison of these frameworks, with a specific focus on their implications for the design and execution of microbiological method verification studies.
CLIA (Clinical Laboratory Improvement Amendments)
CLIA is a U.S. federal regulatory standard established to ensure the accuracy, reliability, and timeliness of patient test results regardless of where a test is performed [7]. Its primary focus is on analytical testing phases. Compliance with CLIA regulations is mandatory for all clinical laboratories in the United States that report patient-specific results for health assessment [7] [8]. Laboratories are subject to routine inspections by the Centers for Medicare & Medicaid Services (CMS) or CMS-approved accrediting organizations [7].
ISO 15189 (Medical laboratories — Requirements for quality and competence)
ISO 15189 is an international standard that specifies requirements for quality and competence in medical laboratories [8]. Its core objective is to promote patient welfare and satisfaction through confidence in the quality of laboratory results [9]. A major focus of the updated 2022 version is on risk management, making patient safety central to all laboratory processes [9]. Unlike CLIA, ISO 15189 accreditation is voluntary and serves as a demonstration of a laboratory's commitment to a high level of quality and continuous improvement [7].
IVDR (In Vitro Diagnostic Regulation)
The IVDR (EU) 2017/746 is the European Union's regulatory framework for in vitro diagnostic medical devices [10]. It is a product-centric regulation that applies to manufacturers placing IVD devices on the EU market. A cornerstone of the IVDR is a new, stricter risk-based classification system (Class A-D), with most devices now requiring a conformity assessment by a Notified Body [11]. The regulation emphasizes robust clinical evidence, performance evaluation, and stringent post-market surveillance [11]. Key transition periods for legacy devices are in effect from 2025 to 2027 [10] [11].
Table: High-Level Comparison of CLIA, ISO 15189, and IVDR
| Feature | CLIA | ISO 15189 | IVDR |
|---|---|---|---|
| Jurisdiction | United States | International | European Union |
| Nature | Mandatory regulation | Voluntary accreditation | Mandatory product regulation |
| Primary Focus | Analytical phase quality; regulatory compliance | Total testing process; continuous improvement; patient safety | Device safety, performance, and lifecycle monitoring |
| Governing Body | Centers for Medicare & Medicaid Services (CMS) | International Organization for Standardization (ISO) | European Commission |
| Applicability | Clinical laboratories | Medical laboratories | Manufacturers of in vitro diagnostics |
Detailed Requirements for Method Verification
Method verification is the process of confirming that a validated test performs as expected in a laboratory's own environment before reporting patient results [4]. For non-waived, FDA-cleared tests, CLIA requires verification of specific performance characteristics [4].
CLIA Requirements for Verification of Microbiological Methods
For qualitative and semi-quantitative microbiological assays (e.g., PCR, antigen tests), CLIA requires verification of several key performance characteristics [4]. The following protocols outline standard methodologies.
Table: CLIA Method Verification Protocol for Qualitative/Semi-Quantitative Assays
| Performance Characteristic | Recommended Protocol (Microbiology) | Acceptance Criteria |
|---|---|---|
| Accuracy | Test a minimum of 20 clinically relevant isolates (positive and negative). Use standards, controls, proficiency samples, or clinical specimens previously tested with a validated method [4]. | Percentage of agreement = (Number of agreements / Total results) × 100. Should meet manufacturer's stated claims or criteria set by the laboratory director [4]. |
| Precision | Test a minimum of 2 positive and 2 negative samples in triplicate over 5 days by 2 different operators. Use controls or de-identified clinical samples [4]. | Percentage of agreement = (Number of agreements / Total results) × 100. Should meet manufacturer's stated claims or director-defined criteria [4]. |
| Reportable Range | Verify using a minimum of 3 samples. For qualitative assays, use known positive samples. For semi-quantitative, use samples near the cutoff values [4]. | The laboratory confirms that it can accurately report results as defined (e.g., "Detected," "Not detected," or with a specific Ct value cutoff) [4]. |
| Reference Range | Verify using a minimum of 20 isolates. Use de-identified clinical samples or reference materials that represent the laboratory's patient population [4]. | The laboratory confirms the manufacturer's reference range is appropriate for its patient population, or re-defines it if necessary [4]. |
ISO 15189 and IVDR Considerations for Verification
ISO 15189 emphasizes the verification and validation of examination procedures to ensure they are suitable for their intended use [8]. It mandates that laboratories must "verify the ability to achieve the required performance" and that examination procedures must be "appropriate for the intended use" [8]. This aligns with CLIA but is embedded within a broader quality management system that requires documented procedures, personnel competence, and risk management across the entire testing process (pre-examination, examination, and post-examination) [8].
The IVDR imposes requirements on the manufacturer, not the clinical laboratory directly. However, laboratories using IVDR-compliant devices must be aware that the manufacturer's provided performance claims (e.g., sensitivity, specificity) are backed by a stringent performance evaluation and clinical evidence dossier assessed by a Notified Body [11]. The laboratory's verification study often uses this manufacturer data as the benchmark for acceptance criteria.
Comparative Analysis of Quality Control and Personnel Requirements
Quality Control (QC) and Proficiency Testing (PT)
A 2025 global survey of QC practices highlights practical differences in how accredited laboratories implement QC. CLIA labs are overwhelmingly once-a-day QC users, aligning with the CLIA minimum requirement, while ISO 15189 labs show more variation in frequency, with a more balanced distribution across once, twice, or three times per day [12]. The same survey found that ISO labs are more likely to use multi-rule "Westgard Rules" on all tests compared to CLIA labs [12].
CLIA mandates successful participation in a CMS-approved proficiency testing (PT) program for regulated analytes [13]. New, stricter PT acceptance criteria were fully implemented in 2025 [13]. For example, the allowable total error for microbiology-based glucose is now ± 8% or ± 6 mg/dL (whichever is greater), tightened from the previous ± 10% [13]. ISO 15189 also requires participation in inter-laboratory comparisons, such as PT, but as part of a broader external quality assessment scheme used for continual improvement.
Personnel Qualifications
CLIA regulations specify detailed personnel qualifications for different roles (director, supervisor, testing personnel) and based on test complexity (moderate or high). Recent updates effective in 2025 have refined these requirements, including changes to permitted degrees and the addition of continuing education requirements for high-complexity lab directors [14]. Grandfathering clauses protect currently employed personnel if their employment is continuous [14].
ISO 15189, under its "Resource Requirements" (Clause 6), mandates that personnel be competent and have the appropriate education, training, experience, and skills, but does not prescribe specific degree or hour requirements like CLIA [8]. The laboratory must define the necessary competence for each role and provide evidence that personnel meet these requirements [8].
Table: Comparison of Key Laboratory Processes
| Process | CLIA | ISO 15189:2022 |
|---|---|---|
| QC Frequency | Primarily once per day (minimum requirement) [12]. | More varied; can be once, twice, or three times per day based on risk [12]. |
| QC Rules | Less frequent use of multi-rule Westgard Rules [12]. | More frequent use of multi-rule Westgard Rules on all tests [12]. |
| Proficiency Testing (PT) | Mandatory, with specific graded analytes and 2025-updated acceptance criteria [13]. | Required as part of external quality assessment (EQA), used for performance monitoring and improvement. |
| Personnel | Specific, regulated degree and experience requirements for each role [14]. | Competency-based requirements defined by the laboratory [8]. |
| Risk Management | Implied in quality assessment but not explicitly mandated as a formal process. | A major focus; requires proactive risk management across all processes to benefit patient safety [9]. |
Essential Research Reagents and Materials
The following reagents and materials are critical for executing a compliant microbiological method verification study.
Table: Research Reagent Solutions for Method Verification
| Reagent/Material | Function in Verification |
|---|---|
| Certified Reference Materials | Provides a metrologically traceable standard for verifying accuracy and reportable range. |
| Commercial Quality Controls (Assayed/Lyophilized) | Used for precision (repeatability and reproducibility) studies and ongoing quality control. |
| Characterized Clinical Isolates | Essential for accuracy studies; provides samples with known identity/characteristics for comparison. |
| Proficiency Testing (PT) Samples | Used as an external benchmark for verifying assay accuracy and performance. |
| Storage and Stability Solutions | Ensures the integrity of reagents and samples throughout the verification timeline. |
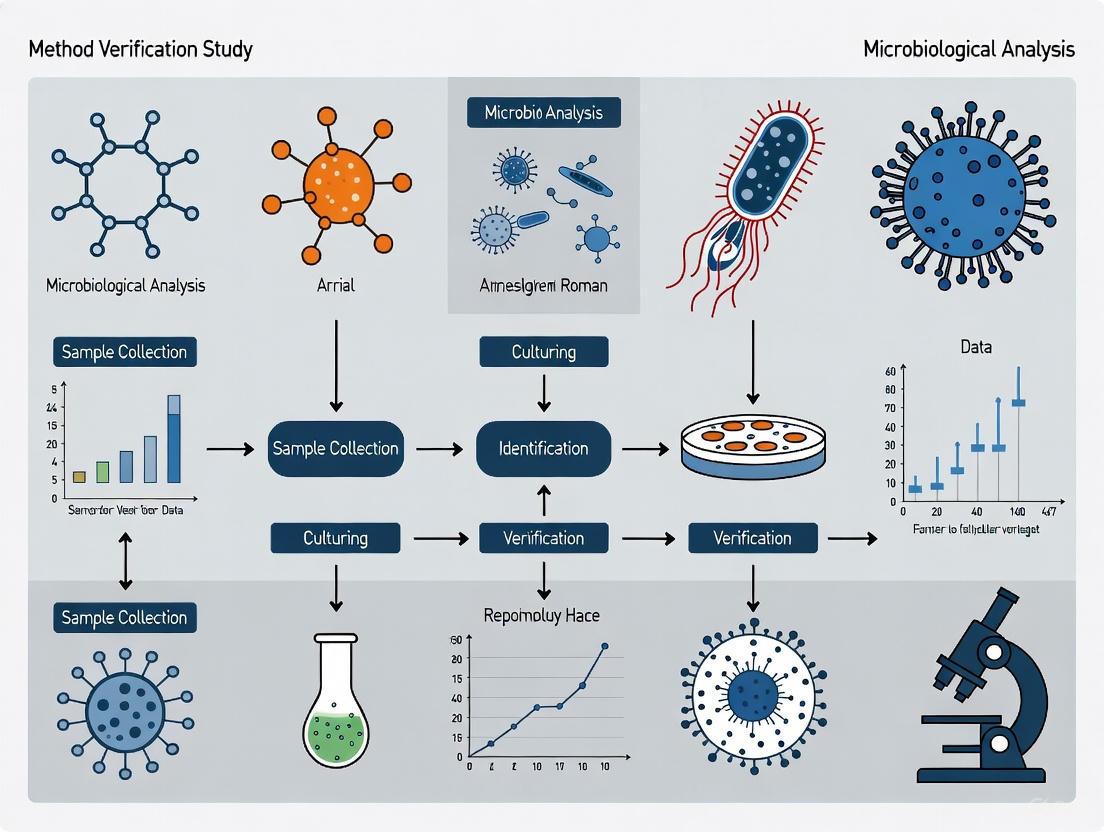
Method Verification Workflow
The following diagram maps the logical workflow for planning and executing a method verification study, integrating considerations from CLIA, ISO 15189, and manufacturer's (IVDR) claims.
Method Verification Workflow Diagram
The regulatory frameworks of CLIA, ISO 15189, and IVDR, while distinct in their scope and application, are not mutually exclusive. A modern clinical microbiology laboratory must often operate within the boundaries of multiple standards. CLIA provides the foundational, compliance-based floor for U.S. operations. ISO 15189 offers a ceiling for achieving excellence through a holistic, risk-based quality management system. The IVDR ensures that the diagnostic devices themselves are safe and effective. A robust microbiological method verification study is not merely a regulatory checkbox but a critical scientific undertaking. It synthesizes the manufacturer's (IVDR) performance claims with the laboratory's specific environment and patient population, following structured protocols (CLIA) within a system dedicated to continuous quality improvement and patient safety (ISO 15189). Understanding the requirements and synergies between these frameworks is fundamental to designing a verification study that is both scientifically sound and regulatorily compliant.
In the rigorous world of pharmaceutical, clinical, and food safety microbiology, the concepts of method validation and method verification are foundational to ensuring the reliability of laboratory data. Although these terms are sometimes used interchangeably, they represent distinct, critical processes within the method lifecycle. Method validation is the process of establishing, through laboratory studies, that the performance characteristics of a method meet the requirements for its intended analytical applications [15]. In contrast, method verification is "the ability to verify that a method can perform reliably and precisely for its intended purpose" within a specific laboratory setting [15]. Essentially, verification demonstrates that a laboratory can successfully execute a method that has already been validated elsewhere [5].
Understanding when verification is required—as opposed to a full validation or a simpler qualification—is a fundamental compliance and scientific decision. This guide provides researchers, scientists, and drug development professionals with a structured framework for determining verification necessity, ensuring both regulatory compliance and data integrity.
The Regulatory and Standards Framework
Globally, regulatory authorities and standards organizations provide clear, albeit sometimes differing, expectations for method verification. A summary of key guidance across major sectors is provided in the table below.
Table 1: Regulatory and Standards Framework for Method Verification
| Authority/Standard | Sector | Key Guidance/Document | Verification Requirement Summary |
|---|---|---|---|
| FDA, EMA, ICH | Pharmaceutical | ICH Q2(R2), USP <1226>, USP <1225> | Verification required for compendial (e.g., USP, EP) methods or previously validated methods transferred to a new laboratory [15] [16]. |
| CLIA | Clinical Microbiology | 42 CFR 493.1253 | Verification is mandated for unmodified, FDA-cleared/approved tests before reporting patient results [4]. |
| ISO | Food & Feed Testing | ISO 16140 Series (Parts 1, 3) | Two-stage verification: "implementation verification" and "(food) item verification" to demonstrate laboratory competency and method suitability for specific items [17]. |
| AOAC, FDA | Food Safety | AOAC Guidelines, FDA 21 CFR 211 | Each laboratory must perform verification to show it can correctly execute a validated method with its specific operators and environment [5]. |
The core principle unifying these regulations is that the burden of proof is on the testing laboratory. Even when using a method perfectly validated by a pharmacopeia or a kit manufacturer, a laboratory must still verify that the method performs as expected in its own hands, with its specific equipment, reagents, and personnel [15] [5].
When is Verification Required? A Decision Framework
The necessity for verification is triggered by specific scenarios in the laboratory. The following decision pathway provides a visual guide to determining when verification is the required course of action.
Diagram 1: Method Verification Decision Pathway
The decision framework outlines three primary scenarios mandating verification. The specific protocols and experimental designs for each scenario, however, differ based on the method type and regulatory context.
Verification of Compendial Methods
In pharmaceutical quality control (QC) microbiology, many standard methods like sterility testing (USP <71>) and microbial enumeration (USP <61>) are validated by the pharmacopeia. The laboratory's task is not to re-validate these methods but to perform verification that the method is suitable for the specific product (sample matrix) and the laboratory setting [15]. The core objective is to demonstrate that the sample itself does not interfere with the method's ability to recover microorganisms.
Verification of Commercial Kits and FDA-Cleared Tests
When implementing an unmodified, commercially available test kit or an FDA-cleared/approved method, laboratories are required to perform a verification study [4] [16]. This process verifies that the laboratory can achieve the performance characteristics (e.g., accuracy, precision) claimed by the manufacturer. For Clinical Laboratory Improvement Amendments (CLIA) compliance, this is a one-time study for non-waived systems before reporting patient results [4].
Method Transfer Between Laboratories
When a validated method is transferred from one laboratory to another (e.g., from an R&D center to a QC lab, or to a contract testing organization), the receiving laboratory must perform verification. This demonstrates that the method can be executed successfully in the new environment, producing results equivalent to those generated by the originating laboratory.
Distinguishing Verification from Validation and Qualification
A critical skill for scientists is to discern when verification is sufficient versus when a more extensive validation is needed. The table below clarifies the distinctions and appropriate applications for each.
Table 2: Comparison of Validation, Verification, and Qualification
| Aspect | Method Validation | Method Verification | Method Qualification |
|---|---|---|---|
| Definition | Establishing performance characteristics for a new method's intended use [15]. | Demonstrating a lab can perform a pre-validated method correctly [15] [5]. | A phase-appropriate approach for early development where full validation is not yet required [16]. |
| Scope | Broad, to prove the method itself is fit-for-purpose. | Narrow, to prove laboratory proficiency with the method. | Flexible and risk-based, covering critical parameters for the development stage. |
| When Used | - Novel method development- Modern/alternative method implementation [15]- Significant method modification. | - Compendial methods [15]- Unmodified commercial kits [16]- Method transfer. | - Early-stage drug development (e.g., Phase I) [16]- Methods for processes not yet locked. |
| Key Parameters | Accuracy, Precision, Specificity, LOD, LOQ, Linearity, Range, Robustness [15]. | Accuracy, Precision, Reportable Range, Reference Range (as per CLIA) [4]. | Risk-based selection of critical parameters (e.g., specificity, accuracy for safety-related tests) [16]. |
A key differentiator is that verification is for established methods, while validation is for novel or significantly changed methods. Furthermore, in early-stage drug development where processes are fluid, a full validation may be premature. In these cases, a phase-appropriate "qualification" is often the recommended strategy, reserving the term "validation" for later-stage (Phase III and commercial) methods [16].
Experimental Protocols for Core Verification Activities
Protocol for Verification of a Qualitative Compendial Method
This protocol is suited for methods like USP <61> for non-sterile products.
- 1. Purpose: To verify that a compendial qualitative method (e.g., test for specified microorganisms) is suitable for use with a specific product matrix in the user's laboratory.
- 2. Experimental Design:
- Sample Preparation: Use a minimum of 20 test samples. These can be artificially contaminated with low levels (typically 10-100 CFU) of appropriate challenge organisms specified in the compendial chapter [4] [15].
- Control Strains: Use ATCC or equivalent reference strains.
- Testing: Execute the compendial method exactly as written on the contaminated samples and appropriate negative controls.
- 3. Data Analysis:
- Calculate the Accuracy as (Number of correct positive identifications / Total number of challenged samples) x 100 [4].
- The acceptance criterion is typically successful detection and identification of the challenge organism in all contaminated samples, with negative controls showing no growth.
- 4. Documentation: The verification report must include the compendial method reference, details of samples and challenge organisms, raw data, calculations, and a statement of acceptance.
Protocol for Verification of a Quantitative Method (CLIA Framework)
This protocol is based on CLIA requirements for an unmodified, FDA-cleared quantitative test.
- 1. Purpose: To verify the performance of an unmodified quantitative method in the user's laboratory.
- 2. Experimental Design:
- Accuracy: Compare results from the new method against a reference method or known standard for a minimum of 20 samples [4].
- Precision:
- Within-run: Test a minimum of 2 positive and 2 negative samples in triplicate in a single run.
- Between-run & Operator: Test the same samples over 5 days by 2 different operators [4].
- 3. Data Analysis:
- Accuracy: Calculate the percentage agreement or bias compared to the reference value.
- Precision: Calculate the standard deviation and coefficient of variation (%CV) for the replicate measurements. The results should meet the manufacturer's stated claims or laboratory-defined criteria.
- 4. Additional CLIA Requirements: The laboratory must also verify the Reportable Range (upper and lower limits) using at least 3 samples and the Reference Range (normal values) using a minimum of 20 samples from the laboratory's patient population [4].
The Scientist's Toolkit: Essential Reagents and Materials
Successful verification studies rely on high-quality, traceable materials. The following table details essential items for a microbiological verification toolkit.
Table 3: Essential Research Reagent Solutions for Verification Studies
| Reagent/Material | Function in Verification | Key Considerations |
|---|---|---|
| Reference Strains (e.g., ATCC, NCTC) | Served as challenge organisms for accuracy, specificity, and limit of detection studies. | Purity, viability, and proper lineage documentation are critical. Must be appropriate for the method and sample matrix. |
| Certified Reference Materials | Provide a "conventional true value" for quantifying accuracy and calibrating measurements. | Source and certification documentation must be available. |
| Inhibitory/Interfering Substances | Used in robustness testing to evaluate the method's resilience to slight variations. | Examples include varying pH, salinity, or specific components known to be in the sample matrix. |
| Quality Control Strains | Used for ongoing monitoring of method performance pre- and post-verification. | Should be different from the reference strains used in the initial verification. |
| Standardized Culture Media | Supports the growth and recovery of challenge organisms. | Must be qualified and prepared according to compendial or manufacturer specifications. |
Determining the necessity for verification is a fundamental, non-negotiable step in the implementation of any microbiological method within a regulated environment. The requirement is clearly triggered in three core scenarios: when adopting a compendial method, when implementing an unmodified commercial kit or FDA-cleared test, and when transferring a validated method to a new laboratory. By adhering to the structured decision framework and experimental protocols outlined in this guide, researchers and drug development professionals can ensure their laboratories generate reliable, defensible data, thereby upholding the highest standards of product quality and patient safety. A disciplined approach to verification is not merely a regulatory hurdle; it is a cornerstone of scientific rigor in applied microbiology.
In clinical and microbiological laboratories, the classification of test methods into qualitative, quantitative, and semi-quantitative categories is fundamental to research design, method verification, and data interpretation. These categories correspond to established scales of measurement in metrology, each with distinct statistical properties and applications [18].
The ordinal, difference, and ratio scales deal with properties that can be measured and apply to quantitative methods, which report quantitative results, typically concentrations. The nominal scale applies to qualitative methods, which report categorical results without numerical values [18]. Semi-quantitative assays occupy a unique position, providing results on an ordinal scale where values can be ranked but lack the precise numerical relationships of true quantitative measurements [18] [19].
Understanding these distinctions is particularly crucial for method verification study design in microbiological research, where the choice of assay type directly impacts validation protocols, statistical analysis methods, and the interpretation of results in drug development contexts.
Defining the Core Assay Categories
Qualitative Assays
Qualitative assays determine the presence or absence of an analyte and provide a binary "yes/no" result [20] [4]. These tests examine nominal properties where only equality matters, and results cannot be ordered or ranked [18]. The output is reported using descriptive terms such as "positive/negative," "reactive/non-reactive," or "detected/not detected" [20] [4].
Examples in Practice:
- Diagnostic tests for pathogens (e.g., SARS-CoV-2 via qualitative RT-PCR) [20]
- Pregnancy tests detecting human chorionic gonadotrophin [20]
- Presence of specific genetic markers [4]
Quantitative Assays
Quantitative assays report precise numerical concentrations of an analyte, employing calibration curves with multiple points to calculate exact values for unknown specimens [20]. These methods utilize the ratio scale, characterized by equally sized units, a natural zero point, and constant ratio relationships between quantity values [18].
Key Characteristics:
- Results expressed in standardized units (e.g., BAU/mL, IU/mL) [20]
- Require comparison to international standards for harmonization [20]
- Enable longitudinal monitoring and precise threshold determination [20]
Semi-Quantitative Assays
Semi-quantitative assays measure approximate concentrations and report results on an ordinal scale with multiple arbitrary steps or categories without standard measurement units [20] [19]. They provide more information than qualitative tests but less precision than fully quantitative methods [18].
Distinguishing Features:
- Results are ordinal and can be ranked (e.g., "small," "moderate," "large") but lack precisely defined intervals between categories [18]
- May use numerical values to determine cutoffs but report qualitative results [4]
- Often employ a single calibrator or limited calibration curve to establish cutoff values [20]
- Recognized as having "less-than-optimal quality indicators for trueness, precision, and detectability" compared to quantitative methods [18]
Common Applications:
- Urine test strips with multiple result categories [19]
- Serologic antibody tests for SARS-CoV-2 that estimate levels without precise quantification [20]
- Screening tests for drugs of abuse with graded results [19]
Table 1: Comparative Analysis of Assay Categories
| Characteristic | Qualitative | Semi-Quantitative | Quantitative |
|---|---|---|---|
| Scale Type | Nominal | Ordinal | Ratio |
| Result Format | Binary (e.g., Positive/Negative) | Multiple ordered categories | Precise numerical value with units |
| Statistical Analysis | Contingency tables, Bayesian statistics | Ordinal scale statistics | Parametric statistics |
| Calibration | Single cutoff point | Limited calibration points | Multi-point calibration curve |
| Uncertainty Communication | Probability of classification error | Estimated concentration ranges | Measurement uncertainty with confidence intervals |
| Example Methods | Pregnancy tests, pathogen presence | Urine test strips, graded serology | Therapeutic drug monitoring, antibody quantification |
Method Verification and Validation Frameworks
Distinguishing Verification from Validation
In laboratory medicine, verification confirms that a previously validated method performs as expected in a user's laboratory, while validation establishes that an assay works as intended for its specific application [4]. Verification is required for unmodified FDA-cleared tests, whereas validation is necessary for laboratory-developed tests or modified FDA-approved methods [4].
The ISO 16140 series provides standardized protocols for method validation in microbiology, with specific parts addressing different validation scenarios [17]:
- Part 2: Validation of alternative (proprietary) methods against a reference method
- Part 3: Verification of reference methods in a single laboratory
- Part 4: Protocol for method validation in a single laboratory
- Part 5: Factorial interlaboratory validation for non-proprietary methods
- Part 6 & 7: Validation of confirmation and identification procedures [17]
Verification Criteria for Different Assay Types
For qualitative and semi-quantitative assays, verification requires specific approaches that differ from quantitative methods [4]:
Accuracy Verification:
- Minimum of 20 clinically relevant isolates recommended
- Combination of positive and negative samples for qualitative assays
- Range of samples with high to low values for semi-quantitative assays
- Calculation: (Number of results in agreement / Total number of results) × 100 [4]
Precision Verification:
- Minimum of 2 positive and 2 negative samples tested in triplicate for 5 days by 2 operators
- For semi-quantitative assays: samples spanning high to low values
- Fully automated systems may not require user variance testing [4]
Reportable Range Verification:
- Minimum of 3 known positive samples for qualitative assays
- Samples near upper and lower cutoff values for semi-quantitative assays
- Verification that results fall within the manufacturer's established reportable range [4]
Experimental Design and Statistical Approaches
Statistical Methods for Qualitative and Semi-Quantitative Data
The evaluation of qualitative and semi-quantitative assays requires specialized statistical approaches distinct from those used for quantitative data. Standard method validation parameters for quantitative assays do not apply to these formats [19].
Recommended Statistical Tools:
- Contingency tables for comparing method outcomes
- Bayesian statistics for probability-based assessments
- Statistical hypothesis testing for inter-rater agreement [19]
- Measures of accordance and concordance for interlaboratory studies of qualitative methods [19]
For novel digital measures and complex data structures, advanced statistical methods including confirmatory factor analysis (CFA), multiple linear regression, and correlation analyses have shown utility in establishing relationships between measures, particularly when traditional reference standards are unavailable [21].
Study Design Considerations
Key factors in validation study design significantly impact the ability to detect meaningful relationships between measures:
Temporal Coherence: Alignment of data collection periods between compared methods [21]
Construct Coherence: Similarity between the theoretical constructs being assessed by different measures [21]
Data Completeness: Implementation of strategies to maximize complete data capture across all measures [21]
Studies with strong temporal and construct coherence demonstrate stronger correlations and more reliable validation outcomes [21].
The Researcher's Toolkit: Essential Materials and Reagents
Table 2: Essential Research Reagents and Materials for Method Verification Studies
| Reagent/Material | Function in Verification Studies | Application Context |
|---|---|---|
| Quality Control Organisms | Well-characterized microorganisms with defined profiles to validate testing methodologies and monitor instrument, operator, and reagent quality [22]. | Pharmaceutical, food, and clinical testing laboratories |
| International Standards | Reference materials that ensure results correspond to specific numerical values and harmonize results across different laboratories [20]. | Quantitative serologic assays (e.g., WHO International Standard for anti-SARS-CoV-2 immunoglobulin) |
| Calibrators | Materials with known analyte concentrations used to establish calibration curves for quantitative and semi-quantitative assays [20]. | All quantitative and semi-quantitative method validation |
| Proficiency Test Materials | Samples of known composition but unknown to analysts used to validate laboratory competency and method performance [22]. | Ongoing quality assurance for all method types |
| Reference Materials | Certified materials used for method validation, equipment calibration, and quality control [22]. | Implementation of new methods and routine quality monitoring |
The precise categorization of assay methods into qualitative, quantitative, and semi-quantitative formats provides the foundation for appropriate method verification study design in microbiological research and drug development. Understanding the fundamental measurement scales underlying these categories enables researchers to select appropriate statistical methods, design rigorous validation protocols, and correctly interpret results within the framework of regulatory requirements.
As novel technologies continue to emerge, particularly in digital health and complex biomarker detection, the principles of method validation and verification remain essential for ensuring analytical reliability and clinical utility across all assay formats. The standardized approaches outlined in international standards such as the ISO 16140 series provide critical guidance for maintaining methodological rigor while accommodating technological innovation in pharmaceutical development and clinical diagnostics.
Within the framework of microbiological method verification study design research, a Verification Plan serves as the foundational document that ensures a laboratory can successfully perform a validated method before implementing it for routine testing [17]. This is distinct from method validation, which is the initial process of establishing that an assay works as intended, often for non-FDA cleared tests [4]. In contrast, verification is a one-time study for unmodified FDA-approved or cleared tests, meant to demonstrate that the test performs in line with previously established performance characteristics when used as intended by the manufacturer [4]. A meticulously crafted and approved plan is critical for regulatory compliance, data integrity, and ensuring the reliability of results reported from the clinical or food testing laboratory.
Core Components of a Verification Plan
A comprehensive verification plan acts as a detailed roadmap for the entire study. It must be clear, unambiguous, and provide sufficient detail to enable consistent execution. The essential components are:
- Type of Verification and Purpose of Study: The plan must clearly state whether the activity is a verification or a validation, as the requirements differ significantly [4]. It should also describe the purpose of the test and a brief method description.
- Details of Study Design: This is the core of the plan, specifying the performance characteristics that will be evaluated and the rigorous protocols for doing so. According to CLIA standards for non-waived systems, this must include Accuracy, Precision, Reportable Range, and Reference Range [4]. The plan must detail the number and type(s) of samples, the type of quality assurance and quality controls that will be used, the number of replicates (including how many days and how many analysts), and, crucially, the pre-defined acceptance criteria for each characteristic [4].
- Materials, Equipment, and Resources: A complete list of all materials, equipment, reagents, and any other resources needed to execute the study must be included.
- Safety Considerations: The plan should address any specific safety protocols for handling microbiological specimens or other hazardous materials.
- Expected Timeline for Completion: A projected timeline with key milestones helps in tracking the progress of the verification study.
The following workflow diagram illustrates the logical sequence and key decision points in developing a microbiological method verification plan:
Quantitative Requirements: Structuring the Verification Study
The verification study's design must be backed by empirical evidence and adhere to statistically sound principles. The tables below summarize the key quantitative requirements for verifying qualitative and semi-quantitative microbiological assays, based on established guidelines [4].
Table 1: Sample Size and Composition Requirements for Verification Studies
| Performance Characteristic | Minimum Sample Number | Sample Type & Composition |
|---|---|---|
| Accuracy | 20 isolates [4] | A combination of positive and negative samples for qualitative assays; a range of samples with high to low values for semi-quantitative assays [4]. |
| Precision | 2 positive and 2 negative samples [4] | Tested in triplicate for 5 days by 2 operators. If the system is fully automated, user variance testing may not be needed [4]. |
| Reportable Range | 3 samples [4] | For qualitative assays, use known positive samples; for semi-quantitative, use samples near the upper and lower manufacturer cutoffs [4]. |
| Reference Range | 20 isolates [4] | Use de-identified clinical or reference samples representative of the laboratory's patient population [4]. |
Table 2: Experimental Protocols and Acceptance Criteria
| Performance Characteristic | Experimental Protocol | Calculation & Acceptance Criteria |
|---|---|---|
| Accuracy | Test the minimum number of samples, comparing results between the new method and a comparative method [4]. | (Number of results in agreement / Total number of results) × 100. The percentage must meet the manufacturer's stated claims or criteria set by the Laboratory Director [4]. |
| Precision | Test the required samples in triplicate over multiple days with multiple operators, as specified [4]. | (Number of results in agreement / Total number of results) × 100. The percentage must meet the manufacturer's stated claims or director-defined criteria [4]. |
| Reportable Range | Verify the upper and lower limits by testing samples that fall within the reportable range [4]. | The laboratory establishes what constitutes a reportable result (e.g., "Detected," "Not detected," Ct value cutoff), verified by testing [4]. |
| Reference Range | Verify the normal result for the tested patient population using the required number of samples [4]. | The expected result for a typical sample is verified. If the manufacturer's range doesn't represent the lab's population, the range may need re-defining [4]. |
The Scientist's Toolkit: Essential Research Reagent Solutions
Executing a verification plan requires specific, high-quality materials. The following table details key reagents and their critical functions in the verification process.
Table 3: Essential Materials for Microbiological Method Verification
| Item | Function in Verification |
|---|---|
| Clinical Isolates & Reference Strains | Well-characterized microbial strains used as positive controls, for accuracy testing, and for challenging the method with relevant organisms [4]. |
| Quality Control (QC) Materials | Commercially available controls or de-identified clinical samples used to monitor the precision and ongoing performance of the method during the verification study [4]. |
| Selective and Non-Selective Agar Media | Various growth media used for the recovery of microorganisms, essential for verifying that the method performs as expected across different culture conditions [17]. |
| Molecular Detection Reagents | Kits containing primers, probes, and enzymes for PCR-based verification studies, used to confirm the identity of isolates and verify molecular assay performance [23]. |
| Antimicrobial Susceptibility Testing (AST) Panels | For verifying AST methods, these panels contain predefined antibiotics at specific concentrations to establish accurate and precise minimum inhibitory concentration (MIC) results [4]. |
Director Approval: The Final Verification Gateway
The laboratory director's approval is not a mere formality but a critical regulatory and quality gate. Before starting the study, the written verification plan must be reviewed and signed off by the lab director [4]. This endorsement signifies that the director, who bears ultimate responsibility for the quality and integrity of the laboratory's results, has verified that:
- The plan is scientifically sound and aligns with regulatory requirements (e.g., CLIA) [4] and standards (e.g., ISO 16140 series for microbiological methods) [17].
- The study design is robust, with appropriate sample sizes, acceptance criteria, and methodologies to demonstrate the method is under control.
- The laboratory has the requisite resources, including trained personnel and equipment, to successfully complete the verification.
The director's approval transforms the verification plan from a proposal into an authorized protocol, enabling the laboratory to proceed with the testing phase and ultimately implement a reliable and compliant testing method.
Designing and Executing a Robust Verification Study Protocol
Within the rigorous fields of pharmaceutical development and clinical diagnostics, the reliability of microbiological testing is paramount. Establishing the performance characteristics of a method is a fundamental requirement to ensure that test results are accurate, reproducible, and fit for their intended purpose. This process is a critical component of method verification and validation, which together form the bedrock of quality assurance in regulated laboratories. Method verification demonstrates that a previously validated method performs as expected within a user's laboratory, while method validation provides evidence that a new method is fit for its intended purpose through a rigorous, defined process [17] [24].
This guide provides an in-depth technical examination of the four core performance characteristics—Accuracy, Precision, Reportable Range, and Reference Range—that must be established for microbiological methods. Framed within the broader context of microbiological method verification study design, this whitepaper delivers detailed experimental protocols and data analysis frameworks tailored for researchers, scientists, and drug development professionals.
Core Performance Characteristics: Definitions and Experimental Protocols
The following characteristics represent the foundation for assessing a method's performance. The specific experimental approach varies depending on whether the method is qualitative (e.g., presence/absence of a microorganism) or quantitative (e.g., microbial enumeration).
Accuracy
Accuracy refers to the closeness of agreement between a test result and an accepted reference value, or the proportion of correct results identified by a new method compared to a reference method. It is a measure of correctness [24] [25].
Experimental Protocols:
- For Quantitative Methods (e.g., Bioburden Enumeration): Accuracy is determined by assessing the recovery of known quantities of a microorganism from a sample matrix. A common approach is to inoculate a sterile product or a placebo with a low-level challenge (e.g., <100 Colony Forming Units or CFU) of a specified microorganism and quantify the recovery using the new method. The percentage recovery is calculated as (Result from New Method / Expected Result) × 100. Acceptance criteria often specify a recovery range of 50% to 200% for microbiological methods, reflecting the inherent variability in microbial distribution and recovery [25].
- For Qualitative Methods (e.g., Sterility Testing, Pathogen Detection): Accuracy is evaluated by testing a panel of samples with known status (positive or negative). The panel should include a minimum of 20 clinically relevant isolates or samples, comprising both positive and negative targets [24]. The accuracy is calculated as the percentage of correct results: (Number of Correct Results / Total Number of Results) × 100 [24] [25].
Table 1: Experimental Design for Assessing Accuracy
| Method Type | Sample Number & Type | Challenge Microorganism | Key Calculations | Common Acceptance Criteria |
|---|---|---|---|---|
| Quantitative | Minimum 3 replicates per organism/matrix | <100 CFU of specified strains | % Recovery = (Result from New Method / Expected Result) × 100 | Recovery between 50% and 200% [25] |
| Qualitative | Minimum 20 samples (positive & negative) | Relevant to method's purpose (e.g., E. coli for a coliform test) | % Accuracy = (Number of Correct Results / Total Results) × 100 | Meets manufacturer's claims or a predetermined percentage (e.g., ≥95%) [24] |
Precision
Precision describes the closeness of agreement between a series of measurements obtained from multiple sampling of the same homogeneous sample under prescribed conditions. It is a measure of reproducibility and is typically subdivided into repeatability and intermediate precision [24] [25].
Experimental Protocols:
- Repeatability (Within-test variation): This assesses the variation when the test is performed repeatedly in a short period by the same technician using the same equipment and reagents. A minimum of 2 positive and 2 negative samples (or samples with high and low values for semi-quantitative assays) are tested in triplicate [24]. Results are expressed as standard deviation (SD) or coefficient of variation (CV).
- Intermediate Precision: This assesses the variation within the laboratory under different conditions, such as different days, different analysts, or different reagent lots. The same samples used for repeatability are tested in triplicate over at least 5 days by two different operators [24]. If the system is fully automated, operator variance may not be required.
Table 2: Experimental Design for Assessing Precision
| Precision Level | Experimental Design | Samples | Key Calculations | Common Acceptance Criteria |
|---|---|---|---|---|
| Repeatability | Same day, same analyst, same reagents | Min. 2 positive & 2 negative, tested in triplicate [24] | Standard Deviation (SD), Coefficient of Variation (CV) | CV < 1/4 to 1/6 of the Allowable Total Error (ATE)* [26] |
| Intermediate Precision | Different days (e.g., 5 days), different analysts | Min. 2 positive & 2 negative, tested in triplicate by 2 operators [24] | Standard Deviation (SD), Coefficient of Variation (CV) | CV < 1/3 to 1/4 of the ATE* [26] |
ATE (Allowable Total Error) is a predefined performance goal based on clinical need, biological variation, or regulatory guidance [26].
Reportable Range
The Reportable Range (also known as the analytical measurement range) is the interval between the upper and lower levels of analyte (in this context, microorganisms) that the method can reliably detect and, for quantitative methods, quantify [24] [26]. It defines the limits of what a laboratory can report as a valid result.
Experimental Protocols:
- For Quantitative Methods: The laboratory must verify the manufacturer's claimed range or the range established during validation. This is done by testing a minimum of 3 samples that span the entire range, including concentrations near the upper and lower limits [26]. For microbial enumeration, this could involve testing dilutions of a microbial suspension from a level below the expected lower limit of quantification to a level at or above the upper limit.
- For Qualitative/Semi-Quantitative Methods: The reportable range is often defined by the cutoff values that distinguish a positive from a negative result, or that define different levels of a semi-quantitative assay (e.g., cycle threshold (Ct) cutoffs in PCR). Verification involves testing known samples positive for the analyte at these critical cutoff values [24].
Reference Range
The Reference Range defines the normal or expected result for a specific patient population or sample type. For many microbiological tests, such as those for specific pathogens, the expected result for a typical sample is "not detected" or "negative" [24].
Experimental Protocol:
- The reference range is verified by testing a minimum of 20 samples that are representative of the laboratory's typical patient population [24]. These can be de-identified clinical samples or reference materials with known negative (or normal) status. If the manufacturer's reference range does not align with the laboratory's patient population, additional testing is required, and the reference range may need to be re-defined to reflect the local population [24].
The Method Verification Workflow
The process of establishing performance characteristics is not performed in isolation but follows a logical sequence within a comprehensive verification plan. The workflow below outlines the key stages from initial planning to final implementation of a verified method.
Diagram 1: Method verification workflow.
Relationships Between Performance Characteristics
Understanding how the four core characteristics interrelate is crucial for a holistic assessment of a method's performance. Accuracy and precision, for instance, are distinct but complementary concepts that together form the basis for reliable quantification.
Diagram 2: Performance characteristics relationships.
The Scientist's Toolkit: Essential Research Reagent Solutions
The successful execution of a verification study relies on a set of well-characterized materials and controls. The following table details key reagents and their critical functions in establishing method performance.
Table 3: Essential Reagents for Verification Studies
| Reagent / Material | Function in Verification | Technical Specifications & Examples |
|---|---|---|
| Reference Microorganism Strains | Serves as the ground truth for accuracy and precision studies. | Obtained from recognized culture collections (e.g., ATCC, NCTC). Selected based on method specificity (e.g., E. coli for a coliform test, S. aureus for a coagulase test) [25]. |
| Clinical or Product Isolates | Provides real-world relevance and challenges method specificity. | A minimum of 20 clinically relevant isolates should be used to verify accuracy for qualitative methods [24]. |
| Quality Control (QC) Materials | Used for precision studies and ongoing monitoring of method performance. | Can be commercially available QC strains, in-house prepared samples, or de-identified clinical samples. Should include positive and negative controls [24]. |
| Sample Matrix | Assesses the impact of the sample background on method performance (recovery, interference). | For pharmaceutical testing, this could be a sterile placebo or the actual product without preservatives. For clinical testing, it could be various specimen types (e.g., sputum, urine) [25]. |
| Culture Media & Reagents | The foundational components for growth-based and non-growth-based methods. | Must be qualified for sterility and performance. Selectivity and productivity should be confirmed during specificity and accuracy assessments [25]. |
Establishing the performance characteristics of accuracy, precision, reportable range, and reference range is a non-negotiable requirement in the verification of microbiological methods. This process, guided by international standards such as the ISO 16140 series and CLSI guidelines, ensures that the data generated in the laboratory is scientifically sound, defensible, and ultimately fit for supporting patient care or product quality decisions [17] [24]. A well-designed verification study, founded on a clear plan with predefined acceptance criteria, is not merely a regulatory hurdle but a fundamental pillar of quality in microbiological science. By meticulously following the experimental protocols and leveraging the essential research reagents outlined in this guide, professionals can robustly demonstrate that their methods are reliable and ready for routine use.
Method verification is a critical, one-time study mandated by the Clinical Laboratory Improvement Amendments (CLIA) for unmodified, FDA-cleared tests before patient results can be reported. Its purpose is to demonstrate that a test's performance characteristics—accuracy, precision, reportable range, and reference range—align with manufacturer claims and are achievable within the user's specific laboratory environment [4]. For clinical microbiology laboratories, this process presents unique challenges, as microbiological methods often do not perfectly fit the parameters designed for analytical chemistry assays.
The foundation of a robust verification study lies in appropriate sample selection and sizing. Using an inadequate number of samples or samples that are not clinically relevant can compromise the entire verification, leading to unreliable test performance data and potential patient safety risks. This guide provides an in-depth technical framework for sample selection and sizing, detailing minimum requirements and the critical importance of clinically relevant isolates to ensure the verification study is both compliant and scientifically sound [4].
Core Principles: Verification vs. Validation and Assay Types
Before designing a verification study, it is essential to define its fundamental purpose, which hinges on two key concepts: the type of study required and the category of the assay itself.
Verification vs. Validation
The terms "verification" and "validation" are often used interchangeably but represent distinct processes with different regulatory requirements:
- Verification: Applies to unmodified, FDA-approved or cleared tests. It is a process that demonstrates a test performs according to its established performance characteristics when used in the laboratory's environment as the manufacturer intended [4].
- Validation: A more extensive process required for laboratory-developed tests (LDTs) or modified FDA-approved tests. Validation establishes that an assay works as intended for its specific application, which may involve different specimen types, sample dilutions, or altered test parameters [4].
This guide focuses on the requirements for method verification.
Qualitative vs. Quantitative Assays
The type of result an assay provides—qualitative, quantitative, or semi-quantitative—directly influences the verification study design, including sample selection and the performance characteristics evaluated [4].
Table: Categories of Microbiological Testing Methods
| Assay Category | Nature of Result | Common Examples in Microbiology |
|---|---|---|
| Qualitative | Binary result (e.g., Detected/Not Detected, Positive/Negative) | PCR detection of a specific pathogen (e.g., mecA gene) [4] |
| Semi-Quantitative | Uses a numerical cutoff to determine a qualitative result | Cycle threshold (Ct) value cutoff in real-time PCR [4] |
| Quantitative | Provides a numerical value | Viral load testing, enumeration of bacteria in a sample |
In clinical microbiology, qualitative and semi-quantitative assays are the most common types requiring verification [4]. The guidance provided herein, including minimum sample sizes, is primarily tailored to these assay types.
Minimum Sample Size Requirements for Verification
The following tables consolidate the minimum sample size requirements for verifying the key performance characteristics of qualitative and semi-quantitative assays, as derived from established clinical laboratory standards [4].
Table 1: Minimum Sample Sizes for Key Verification Characteristics
| Performance Characteristic | Minimum Sample Requirement | Sample Composition Guidelines |
|---|---|---|
| Accuracy | 20 clinically relevant isolates [4] | A combination of positive and negative samples [4]. |
| Precision | 2 positive and 2 negative samples [4] | Tested in triplicate over 5 days by 2 operators (if not fully automated) [4]. |
| Reportable Range | 3 samples [4] | Known positive samples for the detected analyte; for semi-quantitative, use samples near the upper and lower cutoff values [4]. |
| Reference Range | 20 isolates [4] | De-identified clinical or reference samples representing the standard result for the laboratory's patient population [4]. |
Experimental Protocols for Sample Analysis
Adhering to standardized protocols is essential for generating reliable and defensible verification data.
Protocol for Accuracy Verification
- Sample Procurement: Obtain a minimum of 20 well-characterized isolates. These can be from certified reference materials, proficiency test samples, archived clinical samples with previous results from a validated method, or commercially available controls [4].
- Testing: Analyze all samples using the new method according to the manufacturer's instructions.
- Data Analysis: Compare the results from the new method to the known or expected results. Calculate the percent agreement: (Number of results in agreement / Total number of results) × 100 [4].
- Acceptance Criteria: The calculated accuracy must meet or exceed the manufacturer's stated claims or the criteria established by the laboratory director [4].
Protocol for Precision Verification
- Sample Selection: Select at least two positive and two negative samples that represent a range of responses (e.g., strong positive, weak positive) [4].
- Testing Scheme: Test each sample in triplicate, over the course of at least five days, and include two different operators to capture between-run and inter-operator variability. For fully automated systems, operator variance may not be required [4].
- Data Analysis: Calculate the percent agreement for all replicates across all days and operators: (Number of concordant results / Total number of results) × 100 [4].
- Acceptance Criteria: The precision must meet the manufacturer's stated performance or laboratory-defined criteria [4].
Sourcing and Selecting Clinically Relevant Isolates
Meeting the minimum sample size is necessary but insufficient. The clinical relevance of the isolates used is paramount to ensure the verification reflects real-world testing scenarios.
Acceptable sources for isolates and samples include [4]:
- Reference Materials and Standards: Certified strains from culture collections (e.g., ATCC).
- Proficiency Test Samples: These provide well-characterized samples with expected results.
- Quality Control Materials: Commercial controls with established performance.
- De-identified Clinical Samples: Archived patient samples that have previously been tested using a validated method. These are highly valuable as they represent the actual matrix and microbial diversity encountered in the lab.
Criteria for Clinical Relevance
When selecting isolates, consider the following to ensure clinical relevance:
- Representative of Patient Population: The isolates should reflect the spectrum of organisms and strains typically seen in your specific patient population [4]. For example, a verification study for a gastrointestinal panel should include relevant pathogens and commensals found in stool.
- Inclusion of Challenging Strains: The study should include organisms that are known to be difficult to identify or that have borderline characteristics (e.g., near the cutoff value for a semi-quantitative assay) to robustly challenge the method [4].
- Sample Matrices: If the test is approved for multiple sample types (e.g., swabs, tissue, fluid), the verification should include samples from each relevant matrix to ensure consistent performance.
The following diagram illustrates the workflow for selecting and justifying clinically relevant isolates.
The Scientist's Toolkit: Essential Research Reagents and Materials
A successful verification study relies on more than just microbial isolates. The following table details key reagents, materials, and resources essential for planning and executing a method verification study in clinical microbiology.
Table: Essential Research Reagents and Resources for Method Verification
| Item | Function/Application in Verification |
|---|---|
| Certified Reference Strains | Provide genetically and phenotypically well-defined microorganisms; serve as gold standards for accuracy testing [4]. |
| Commercial Quality Controls | Assayed controls with established expected values; used for precision and reproducibility studies [4]. |
| Proficiency Test (PT) Panels | External, blinded samples used to objectively assess the accuracy and reliability of the testing method [27]. |
| CLSI Guidance Documents | Provide standardized protocols and consensus guidelines for evaluation (e.g., EP12, M52, MM03) [4]. |
| Individualized Quality Control Plan (IQCP) Tools | Framework for developing a customized quality control plan based on a risk assessment of the testing process [4]. |
The integrity of a microbiological method verification study is fundamentally dependent on a well-considered strategy for sample selection and sizing. Adherence to the minimum sample requirements for accuracy, precision, reportable range, and reference range provides a regulatory-compliant foundation. However, true success is achieved when these samples are clinically relevant isolates that accurately reflect the laboratory's patient population and testing demands. By rigorously applying the principles and protocols outlined in this guide—from sourcing appropriate materials to justifying selections based on local epidemiology—laboratories can ensure their verification studies are robust, defensible, and ultimately guarantee the delivery of reliable patient results.
In the field of clinical and pharmaceutical microbiology, the reliability of a testing method is paramount. Before a new microbiological method can be routinely deployed to inform critical decisions on product safety or patient care, its performance must be rigorously demonstrated within the specific laboratory environment where it will be used [28]. This process, central to a broader thesis on fundamentals of microbiological method verification study design research, ensures that results are consistently accurate, precise, and dependable. Method verification is a standard practice required by regulations such as the Clinical Laboratory Improvement Amendments (CLIA) for non-waived systems before patient results can be reported [4]. The core of this demonstration lies in a robust experimental design, which meticulously defines the number of replicates, the involvement of different operators, and the testing duration. These three elements collectively provide evidence that the method is under statistical control and is suitable for its intended purpose, forming the bedrock of data integrity in drug development and diagnostic research [25].
It is crucial to distinguish between the terms "validation" and "verification," as they are often used interchangeably but represent different processes. A validation is a more extensive process meant to establish that a novel or modified assay works as intended; this applies to laboratory-developed tests (LDTs) or modified FDA-approved tests [4] [29]. Conversely, a verification is a one-time study for unmodified, FDA-approved or cleared tests, meant to demonstrate that the test performs in line with the manufacturer's established performance characteristics in the user's specific environment [4] [17]. International standards, such as the ISO 16140 series for the food and feed chain, further formalize these processes, outlining distinct stages for both the initial validation of alternative methods and their subsequent verification in a single laboratory [17]. This guide focuses on the practical experimental design parameters required for a successful verification study.
Core Principles of Verification Study Design
Key Parameters and Their Definitions
The design of a verification study is built upon evaluating specific performance characteristics. The essential parameters, along with their definitions and the role of replicates, operators, and duration in their assessment, are summarized in the table below.
Table 1: Key Performance Characteristics in Method Verification
| Parameter | Definition | Role of Replicates, Operators, & Duration |
|---|---|---|
| Accuracy | The closeness of agreement between a measured value and the true or expected value [25]. | Established by testing a sufficient number of samples in agreement with a reference method. |
| Precision | The closeness of agreement between a series of measurements from multiple sampling of the same homogeneous sample [25]. | Directly assessed via multiple replicates, multiple operators, and testing over multiple days to capture different sources of variation. |
| Reportable Range | The interval between the upper and lower levels of analyte (including concentrations) that the method can quantitatively measure with acceptable accuracy and precision [4]. | Verified by testing samples at the upper and lower ends of the range, often in replicates. |
| Analytical Sensitivity (Limit of Detection) | The lowest number of microorganisms that can be detected by the method under stated conditions [25]. | Determined by testing low-level challenges in multiple replicates over time to establish a detection limit with statistical confidence. |
The Interplay of Replicates, Operators, and Duration
The three core elements of this discussion are not independent; they work in concert to challenge the method under various conditions and provide a comprehensive picture of its robustness.
- Replicates are repeated measurements of the same sample. They are primarily used to evaluate repeatability (within-run precision), which is the variation observed when the same technician performs the test repeatedly in a short time frame using the same reagents and equipment [25]. A minimum of three replicates is often required for this assessment [25].
- Operators refer to different technicians performing the test. Involving multiple operators is key to evaluating intermediate precision (also known as between-run precision or ruggedness). This measures the method's reproducibility across different people, different reagent lots, and potentially different equipment, reflecting the typical variation encountered in daily laboratory practice [4] [25].
- Testing Duration refers to conducting the verification study over multiple days or runs. Extending the study over time, typically 3 to 5 days or more, is critical for capturing day-to-day variations and is an integral part of establishing both precision and the limit of detection [4] [29].
Quantitative Guidance for Experimental Design
The required scale of a verification study varies depending on whether the assay is qualitative or quantitative and whether it is an FDA-approved test being verified or a laboratory-developed test (LDT) being validated. The following table consolidates quantitative recommendations from regulatory guidelines and authoritative sources.
Table 2: Quantitative Experimental Design Recommendations
| Characteristic | Assay Type | Recommended Minimum Design (Replicates, Operators, Duration) | Sample Source & Notes |
|---|---|---|---|
| Precision [4] | Qualitative / Semi-Quantitative | 2 positive and 2 negative samples, tested in triplicate for 5 days by 2 operators. If fully automated, operator variance is not needed. | Controls or de-identified clinical samples. |
| Precision [29] | Quantitative (FDA-verified) | 2 samples at each of 2 concentrations, plus one control, tested over 20 days; or 2 concentrations in triplicate over 5 days. | Patient specimens or reference materials. |
| Precision [29] | Quantitative (LDT-validated) | Minimum of 3 concentrations (high, low, LOD), tested in duplicate 1-2 times/day over 20 days. | |
| Accuracy [4] | Qualitative / Semi-Quantitative | Minimum of 20 clinically relevant isolates (combination of positive and negative). | Standards, controls, reference materials, proficiency tests, or de-identified clinical samples. |
| Accuracy [29] | Quantitative (FDA-verified) | 20 patient specimens within the measuring interval. | |
| Limit of Detection [29] | Quantitative (LDT-validated) | 60 data points (e.g., 12 replicates from 5 samples near the detection limit) conducted over 5 days. | Samples should be in the appropriate matrix. Probit regression analysis is often used. |
| Reportable Range [4] | Qualitative / Semi-Quantitative | Minimum of 3 samples (e.g., known positives or samples near cutoff values). |
Detailed Experimental Protocols
Protocol for Precision Studies
A well-designed precision study captures the total variability of the method.
- Sample Preparation: Select a minimum of two positive and two negative samples for qualitative assays, or samples with high and low values for quantitative/semi-quantitative assays [4]. These can be controls, reference materials, or de-identified clinical samples.
- Study Execution: Test each sample in triplicate (three repeated measurements per run) over five separate days. The testing should be performed by two different qualified operators to introduce user variability [4].
- Data Analysis: Calculate the percentage of results in agreement for qualitative assays. For quantitative assays, calculate the standard deviation and coefficient of variation (relative standard deviation) for within-run, between-run, and total variation [25]. The results should meet the performance claims of the manufacturer or criteria set by the laboratory director.
Protocol for Limit of Detection (LOD) Studies
Establishing the LOD for a laboratory-developed molecular assay requires a statistically significant number of data points.
- Sample Preparation: Prepare samples at concentrations around the expected detection limit. It is critical that these samples are prepared in the appropriate clinical matrix (e.g., sputum, serum) to account for any interfering substances [29].
- Study Execution: Test a series of these low-concentration samples extensively. A common approach is to collect 60 data points, for example, by testing 12 replicates from each of 5 different samples, with the study conducted over five days to incorporate day-to-day variability [29].
- Data Analysis: The data are analyzed using statistical methods such as probit regression to determine the analyte concentration at which a detection rate of 95% is achieved [29].
Visualization of Verification Workflows
The following diagram illustrates the high-level workflow for planning and executing a microbiological method verification study, integrating the core elements of replicates, operators, and duration.
Precision Study Design
This diagram details the specific experimental design for a precision study, highlighting the integration of replicates, operators, and testing duration.
The Scientist's Toolkit: Essential Research Reagent Solutions
The execution of a verification study relies on well-characterized and reliable materials. The following table lists key reagent solutions and their critical functions in ensuring the validity of the study.
Table 3: Essential Research Reagent Solutions for Verification Studies
| Reagent Solution | Function in Verification | Specific Examples & Notes |
|---|---|---|
| Quality Control (QC) Organisms | To validate testing methodologies and monitor instrument, operator, and reagent quality. These are well-characterized microorganisms with defined profiles and predictable reactions [22]. | Obtained from type culture collections (e.g., ATCC) or as commercial controls from providers like Microbiologics [22]. |
| Reference Materials & Standards | To establish accuracy and the reportable range by providing a known value against which the method's output is compared [4]. | Can include standards, controls, proficiency test samples, or previously characterized clinical samples [4]. |
| In-House Microbial Isolates | To demonstrate that the method is appropriate for detecting organisms relevant to the laboratory's specific environment and patient population [22] [30]. | Environmental isolates from the manufacturing facility or clinical isolates from the patient population. Services like BIOBALL Custom Services can help preserve these in ready-to-use formats [22]. |
| Culture Media | To support the growth of microorganisms recovered during testing. Its suitability is foundational to any growth-based method [30]. | Must be validated for its ability to support the growth of a range of indicator organisms, including aerobic and anaerobic bacteria, yeasts, and molds [30]. |
A meticulously designed experimental approach that rigorously defines the number of replicates, incorporates multiple operators, and extends the testing over an adequate duration is non-negotiable for a successful microbiological method verification. This structured approach provides the empirical evidence needed to satisfy regulatory requirements and, more importantly, to instill confidence that the method will perform reliably in its intended setting. As the regulatory landscape evolves, with the implementation of standards like ISO 15189:2022 and the European In Vitro Diagnostic Regulation (IVDR), the principles outlined in this guide will continue to form the foundation of quality and reliability in pharmaceutical development and clinical diagnostics [28]. By adhering to these fundamentals, researchers and scientists ensure that the data guiding critical decisions in drug development and patient care is generated with the highest degree of integrity and scientific rigor.
Within the fundamental research on microbiological method verification study design, the calculation of performance metrics is a critical pillar. Percentage agreement serves as a fundamental statistical measure for assessing the reliability of qualitative and semi-quantitative assays, which are prevalent in clinical microbiology [4]. This measure provides a straightforward, interpretable metric for confirming that a new, unmodified FDA-cleared test performs in accordance with its established performance characteristics in the user's specific environment [4]. Verification studies are a mandatory requirement under the Clinical Laboratory Improvement Amendments (CLIA) for non-waived testing systems before patient results can be reported, ensuring that assays of moderate or high complexity perform reliably in the operator's unique setting [4]. This guide details the experimental protocols and calculations for determining percentage agreement and establishing scientifically sound acceptance criteria, forming the cornerstone of a robust verification study.
Core Concepts and Definitions
Verification Versus Validation
A critical first step is distinguishing between method verification and method validation, as the required rigor and extent of performance assessment differ significantly [4].
- Verification: A one-time study performed for unmodified, FDA-approved or cleared tests. Its purpose is to demonstrate that the test's established performance characteristics are met when the test is used as intended by the manufacturer in the specific laboratory environment [4].
- Validation: A more extensive process performed for laboratory-developed tests (LDTs) or modified FDA-approved tests. It aims to establish that a novel or altered assay works as intended for its specific claim [4].
Assay Result Types
The approach to calculating percentage agreement is influenced by the type of result the assay produces [4]:
- Qualitative Assays: Provide a binary result, such as "detected" or "not detected."
- Semi-Quantitative Assays: May use a numerical value (e.g., a cycle threshold (Ct) in PCR) to determine an acceptable cutoff but ultimately report a qualitative result.
- Quantitative Assays: Provide a numerical value. While percentage agreement can be adapted for quantitative data (e.g., within a certain percentage of a reference value), other statistical measures like correlation and bias are more commonly employed.
Experimental Protocols for Key Verification Studies
The following section outlines detailed methodologies for conducting the core experiments necessary for a verification study, focusing on the parameters most relevant for qualitative and semi-quantitative microbiological assays.
Protocol for Accuracy Assessment
Accuracy verification confirms the acceptable agreement of results between the new method and a comparative method [4].
- Objective: To demonstrate that the new test's results show a high level of concordance with those from a previously validated method.
- Sample Requirements: A minimum of 20 clinically relevant isolates or samples should be used [4]. These should include a combination of positive and negative samples for qualitative assays, or a range of samples with high to low values for semi-quantitative assays.
- Sample Sources: Acceptable specimens can be obtained from:
- Reference standards or control materials.
- Proficiency test samples.
- De-identified clinical samples that have been previously tested or are tested in parallel with a validated method [4].
- Experimental Procedure:
- Test all selected samples using the new method (the test under verification).
- For each sample, compare the result from the new method to the result from the comparative (reference) method.
- Record the number of results that are in agreement between the two methods.
- Data Analysis: Calculate the percentage agreement using the formula:
- Percentage Agreement (%) = (Number of Results in Agreement / Total Number of Results) × 100 [4].
Protocol for Precision Assessment
Precision verification confirms acceptable variance within a run (repeatability), between runs, and between different operators [4].
- Objective: To ensure the test produces consistent and reproducible results over time and across normal laboratory variations.
- Sample Requirements: A minimum of 2 positive and 2 negative samples, tested in triplicate, over 5 days, by 2 different operators [4]. If the system is fully automated, testing for user variance may not be required.
- Sample Sources: Controls or de-identified clinical samples are appropriate [4].
- Experimental Procedure:
- For each sample type (positive and negative), aliquot samples for testing.
- Two different operators should each test the full set of samples in triplicate per day.
- This process is repeated for five separate days to capture between-run variability.
- Data Analysis: Calculate the percentage agreement for each sample type across all replicates, days, and operators.
- Precision Agreement (%) = (Number of Concordant Results / Total Number of Results) × 100 [4].
Establishing Reportable and Reference Ranges
While not directly calculated via percentage agreement, these parameters are essential for defining the test's operational limits.
- Reportable Range Verification: Confirm the upper and lower limits of what the test system can report. For a qualitative PCR assay, this would be verifying that results are correctly reported as "Detected," "Not Detected," or "Invalid" as defined by the manufacturer. Testing a minimum of 3 known positive samples is recommended [4].
- Reference Range Verification: Confirm the expected normal result for the tested patient population. This is often verified using a minimum of 20 isolates, such as samples negative for the target analyte (e.g., MRSA-negative samples for a MRSA detection assay) [4]. If the laboratory's patient population is not well-represented by the manufacturer's reference range, additional testing and re-definition of the range may be necessary [4].
The workflow for planning and executing a verification study, from definition to final report, is summarized in the following diagram.
Data Analysis and Calculation Methods
Calculating Percentage Agreement
Percentage agreement is the primary metric for evaluating qualitative and semi-quantitative assay performance during verification [4]. The calculation is performed as follows:
- Tally Agreements and Disagreements: For each sample tested, record whether the result from the new method agrees with the result from the reference method.
- Apply the Formula:
- Percentage Agreement (%) = (Number of Agreeing Results / Total Number of Results) × 100
Example Calculation: An accuracy study uses 20 samples. The new method's result agrees with the reference method for 19 of these samples.
- Percentage Agreement = (19 / 20) × 100 = 95%
The following tables summarize the key experimental parameters and performance targets derived from established guidelines [4].
Table 1: Experimental Design Parameters for Verification Studies
| Performance Characteristic | Minimum Sample Number | Sample Type | Replication |
|---|---|---|---|
| Accuracy | 20 isolates | Combination of positive and negative samples, or a range of values | Single test per sample |
| Precision | 2 positive & 2 negative | Controls or de-identified clinical samples | Triplicate, over 5 days, by 2 operators |
| Reportable Range | 3 samples | Known positives near cutoff values | As required to define limits |
| Reference Range | 20 isolates | Samples representing "normal" condition | Single test per sample |
Table 2: Core Calculations and Acceptance Criteria
| Performance Characteristic | Calculation Method | Typical Acceptance Criteria |
|---|---|---|
| Accuracy | (Agreements / Total Samples) × 100 | Meets or exceeds manufacturer's stated claims or lab-defined criteria (e.g., ≥95%) |
| Precision | (Concordant Results / Total Replicates) × 100 | Meets or exceeds manufacturer's stated claims or lab-defined criteria (e.g., ≥95%) |
| Reportable Range | Verification that results are reportable as defined | All tested samples report within the defined range |
| Reference Range | Verification that "normal" results are correct | ≥95% of samples yield the expected normal result |
Defining Acceptance Criteria
Acceptance criteria are the predefined benchmarks that determine the success or failure of the verification study. The laboratory director is ultimately responsible for setting and approving these criteria [4].
- Primary Basis: The manufacturer's stated performance claims for the assay are the primary source for setting acceptance criteria. The verification study must demonstrate that the assay performs as well as, or better than, these claims in your laboratory's hands [4].
- Laboratory-Defined Criteria: In some cases, the laboratory director may establish more stringent criteria based on clinical needs, the specific patient population, or published standards from organizations like the Clinical and Laboratory Standards Institute (CLSI) [4].
- Regulatory Compliance: All criteria must ensure compliance with relevant regulatory standards, such as CLIA regulations [4].
The decision-making process for final implementation, based on the calculated agreement and acceptance criteria, is logically represented below.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of a verification study requires careful selection and use of high-quality materials. The following table details key reagents and their functions.
Table 3: Essential Materials for Microbiological Method Verification
| Item | Function & Importance |
|---|---|
| Clinical Isolates | Well-characterized bacterial or fungal strains used as positive and negative controls to challenge the assay's accuracy and specificity. |
| Reference Materials & Standards | Substances with one or more specified properties that are used to calibrate a measurement system or to assess a method's accuracy [4]. |
| Proficiency Test (PT) Samples | Blinded samples obtained from an external provider used to objectively assess the laboratory's testing performance and compare it to peer laboratories [4]. |
| De-identified Clinical Samples | Residual patient samples that have been anonymized. Provide a realistic matrix for verifying performance in the intended clinical setting [4]. |
| Quality Controls (QC) | Materials run alongside patient samples to ensure the test is performing correctly on a daily basis. Verification confirms that QC expectations are met [4]. |
The rigorous determination of percentage agreement and the establishment of scientifically sound acceptance criteria are fundamental to the verification of microbiological methods. By adhering to the structured experimental protocols outlined in this guide—encompassing accuracy, precision, reportable range, and reference range—researchers and drug development professionals can generate robust, defensible data. This process, framed within a comprehensive verification plan, ensures that laboratory tests are reliable, compliant with regulatory standards, and ultimately fit for their intended purpose in supporting patient diagnosis and public health.
Creating an Audit-Ready Verification Report
In the context of microbiological method verification, an audit-ready verification report serves as the definitive record of a study's design, execution, and outcomes. This document provides transparent evidence that the method is fit for its intended purpose and meets all predefined acceptance criteria. For researchers, scientists, and drug development professionals, a well-structured report demonstrates scientific rigor and regulatory compliance, enabling inspectors to easily verify the validity of the verification process. The core principle involves integrating quantitative data (the "what") with qualitative analysis (the "why" and "how") to present a cohesive narrative that withstands regulatory scrutiny [31].
Core Components of an Audit-Ready Report
A comprehensive verification report must contain several essential elements that together provide a complete picture of the verification study.
- Executive Summary: A high-level overview of the verification study, its objectives, and a conclusive statement on the method's performance against all acceptance criteria.
- Methodology and Experimental Design: A detailed description of the microbiological method, including organisms, matrices, and the specific experimental protocols followed.
- Results and Data Analysis: A complete presentation of all quantitative data, supported by statistical analysis and qualitative interpretation.
- Conclusion and Recommendation: A definitive statement on the method's suitability, including any limitations or specific conditions for use.
Presenting both quantitative and qualitative data together is crucial; quantitative data alone can leave the audience bogged down in metrics, while qualitative data alone lacks supporting proof. When combined, they provide greater meaning and rationale for strategic decision-making [31].
Data Presentation Standards for Verification Reports
Effective data presentation is fundamental to creating an audit-ready report. Data must be organized to facilitate easy review and comparison while maintaining scientific accuracy.
Presentation of Quantitative Data
Quantitative data, comprising numerical measurements and statistical analyses, should be presented in clearly structured tables. For discrete numerical variables, such as colony counts, frequency distributions provide a comprehensive view of the data [32].
Table 1: Sample Quantitative Data Presentation - Colony Count Verification
| Test Organism | Theoretical Count (CFU/mL) | Mean Observed Count (CFU/mL) | Standard Deviation | Percent Recovery (%) | Acceptance Criteria Met? |
|---|---|---|---|---|---|
| E. coli ATCC 8739 | 1.0 × 10⁶ | 9.8 × 10⁵ | 0.12 × 10⁵ | 98.0% | Yes (85-115%) |
| S. aureus ATCC 6538 | 1.0 × 10⁶ | 1.1 × 10⁶ | 0.15 × 10⁶ | 110.0% | Yes (85-115%) |
| P. aeruginosa ATCC 9027 | 1.0 × 10⁶ | 9.5 × 10⁵ | 0.09 × 10⁵ | 95.0% | Yes (85-115%) |
| C. albicans ATCC 10231 | 1.0 × 10⁵ | 9.2 × 10⁴ | 0.08 × 10⁴ | 92.0% | Yes (85-115%) |
For continuous variables, such as inhibition zone measurements, data should be categorized with consistent intervals to display frequency distributions effectively. The process involves: (1) subtracting the lowest value from the highest value, (2) dividing this result by the number of categories to create, and (3) defining category intervals based on this calculation [32].
Table 2: Specificity Testing Against Non-Target Organisms
| Non-Target Organism | Growth in Presence of Inhibitor | Zone of Inhibition (mm) | Cross-Reactivity Assessment |
|---|---|---|---|
| Lactobacillus acidophilus | No growth | Not applicable | No interference |
| Bacillus subtilis | Reduced growth (30% of control) | 2.5 | Minimal interference |
| Enterococcus faecalis | No growth | Not applicable | No interference |
| Aspergillus brasiliensis | No growth | Not applicable | No interference |
Presentation of Qualitative Data
Qualitative data provides context and rationale for quantitative findings, explaining anomalies, describing observations, and documenting deviations from protocol. This subjective information is critical for interpreting the numerical results and demonstrating scientific judgment [31].
Table 3: Qualitative Observations and Interpretations
| Test Component | Observation | Interpretation | Impact Assessment |
|---|---|---|---|
| Culture purity | Subculture showed morphological variation on Day 3 | Possible contamination introduced during handling | Repeat test performed; original data excluded from final analysis |
| Medium performance | Slight color change in broth media after 48 hours | Indicator system functioning as expected | No impact on results; documented for future reference |
| Equipment performance | Incubator temperature fluctuation ±0.7°C on Day 2 | Within validated operating parameters | No impact on results; monitored throughout study |
Integrated Data Presentation
The most effective verification reports present quantitative and qualitative data side-by-side, creating a comprehensive narrative that tells the complete story of the verification process. This integrated approach allows auditors to understand not just the results, but the scientific reasoning behind them [31].
Experimental Protocols and Methodologies
Detailed methodologies are essential for audit-ready reports, enabling reproducibility and demonstrating scientific rigor.
Sample Preparation Protocol
The sample preparation methodology must be documented with sufficient detail to allow exact replication:
- Materials and Reagents: Specify all materials, including sources, lot numbers, and preparation methods.
- Inoculum Preparation: Describe the process for preparing standardized inoculum, including culture media, incubation conditions, and standardization method.
- Sample Processing: Detail all steps involved in sample processing, including volumes, temperatures, time points, and equipment used.
- Quality Controls: Document all quality controls performed throughout sample preparation.
Accuracy and Precision Assessment
Accuracy and precision must be evaluated using predetermined protocols with clear acceptance criteria:
- Accuracy Protocol: Comparison of results from the new method with those from a reference method using known positive samples.
- Precision Protocol: Multiple analyses of homogeneous samples by different analysts on different days to determine inter-assay and intra-assay variability.
- Linearity Protocol: Analysis of samples across the claimed analytical measurement range of the method.
Specificity and Limit of Detection Studies
Specificity and detection capability studies validate the method's ability to correctly identify target organisms:
- Specificity Testing: Evaluation against a panel of related organisms, normal flora, and common contaminants.
- Limit of Detection: Determination of the lowest number of microorganisms that can be reliably detected by the method.
Visualization of Experimental Workflows
Visual representations of experimental workflows and decision trees enhance understanding of complex processes and logical relationships in verification studies.
Method Verification Workflow
Method Verification Workflow Diagram
Data Analysis Decision Pathway
Data Analysis Decision Pathway
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and reagents used in microbiological method verification studies, with specifications critical for audit-ready documentation.
Table 4: Essential Research Reagents for Microbiological Method Verification
| Reagent/Material | Function in Verification | Specification Requirements | Quality Control Documentation |
|---|---|---|---|
| Reference Strains (ATCC) | Positive controls for accuracy, specificity, and limit of detection studies | Source, strain number, passage history, purity confirmation | Certificate of Analysis, purity records, subculture documentation |
| Culture Media | Supports growth and differentiation of target organisms | Formulation, pH, sterility, growth promotion testing | Quality control certificates, growth promotion test results, expiration dating |
| Selective Supplements | Inhibits non-target organisms in specificity testing | Concentration, sterility, compatibility with base media | Preparation records, filtration documentation, storage conditions |
| Staining Reagents | Facilitates morphological confirmation of microorganisms | Staining intensity, clarity, specificity | Staining quality control records, comparison to reference images |
| Antimicrobial Agents | Used in specificity and interference testing | Potency, solubility, stability in test system | Certificate of Analysis, preparation records, storage conditions |
| Sample Matrices | Represents actual test conditions for real-world validation | Source, processing method, storage conditions | Donor/source information, processing records, compatibility testing |
Assembly and Quality Control of the Final Report
The final verification report must be assembled with meticulous attention to detail, ensuring all components are present, accurate, and consistent.
Report Quality Assessment Checklist
- Completeness Verification: Confirm all planned experiments are documented and all data points are included.
- Cross-Reference Validation: Ensure all sections, tables, and figures are properly referenced in the text.
- Version Control: Implement strict version control with document history tracking.
- Approval Signatures: Include dated signatures from all responsible personnel (study director, quality assurance, department head).
Audit Preparation Protocol
Preparation for regulatory audit involves additional verification steps:
- Raw Data Reconciliation: Ensure all raw data matches summarized results in the report.
- Deviation Documentation: Verify all protocol deviations are properly documented with impact assessments.
- Training Records: Confirm personnel training records are available and current for all techniques used.
- Instrument Calibration: Document calibration status of all equipment used in the verification study.
By adhering to these structured approaches for data presentation, protocol documentation, visualization, and reagent specification, microbiological researchers can create verification reports that not only withstand regulatory scrutiny but also serve as comprehensive references for future method applications and troubleshooting.
Identifying and Resolving Common Verification Challenges and Errors
In the field of pharmaceutical drug development, the reliability of microbiological data is paramount. Common laboratory errors—specifically contamination, incubation issues, and enumeration mistakes—represent a significant threat to data integrity, product safety, and regulatory compliance. These errors can compromise the entire method verification process, leading to inaccurate conclusions about a method's suitability for its intended purpose. Method verification provides assurance that a test performs in line with established performance characteristics when used as intended, a requirement for non-waived systems under the Clinical Laboratory Improvement Amendments (CLIA) [4]. Similarly, validation establishes that non-FDA cleared or modified tests work as intended [4]. This guide examines these pervasive errors within the framework of microbiological method verification, providing researchers and scientists with detailed protocols and mitigation strategies to ensure the generation of reliable, defensible data.
Understanding and Quantifying Common Laboratory Errors
A thorough understanding of common errors is the first step in developing robust verification studies and quality control (QC) protocols. The table below summarizes the primary errors, their causes, and their impact on microbiological testing.
Table 1: Common Microbiological Laboratory Errors and Their Impacts
| Error Category | Specific Error | Primary Causes | Impact on Testing and Verification |
|---|---|---|---|
| Contamination | External/Cross-Contamination [33] | Improper aseptic technique, inadequate sterilization, poor workflow [34] [35] | False positives, unnecessary and costly investigations, compromised cell lines and reagents [33] [35] |
| Sample Contamination [35] | Dirty glassware, non-sterile consumables, airborne contaminants [35] | Skewed results, wasted reagents, misleading conclusions during method validation [35] | |
| Incubation Issues | Incorrect Temperature [34] | Improper calibrator setting, faulty equipment, frequent door openings [34] | Disrupted or halted microbial growth, failure to detect target organisms [34] |
| Inadequate Atmosphere [30] | Failure to provide anaerobic conditions or required CO₂ levels [30] | Failure to grow fastidious anaerobes or tissue cultures, leading to false negatives [30] | |
| Serial Incubation Problems [33] | Missed transfer to a second temperature [33] | Inaccurate results, need for retesting, delays in verification timelines [33] | |
| Enumeration & Data Errors | Colony Counting Errors [33] | Merged colonies, subjective "naked eye" counting, fast-growing organisms [33] | Inaccurate bioburden counts, incorrect potency assays, flawed equivalence data during method comparison [33] |
| Inaccurate Data Recording [33] | Manual transcription errors, miskeying into LIMS [33] | Incorrect patient results, flawed validation data, misrepresentation of product quality [33] | |
| Improper Sampling [36] | Non-representative sampling, contaminated equipment, insufficient sample size [36] | Biased or incorrect results that undermine the entire analytical process [36] |
Experimental Protocols for Investigating and Mitigating Errors
To systematically control for these errors within a verification study, specific experimental protocols must be employed. The following sections provide detailed methodologies for key investigations.
Protocol for Assessing Media Suitability and Contamination Control
The suitability of the growth medium is fundamental to any microbiological test and must be verified as part of the method.
- Objective: To validate that the prepared media adequately supports the growth of a range of representative and environmental microorganisms and remains free from contamination under specified storage conditions.
- Materials:
- Prepared culture media (e.g., Tryptic Soy Agar, Sabouraud Dextrose Agar)
- Indicator organisms: Typically, 5 or more strains including aerobic bacteria (e.g., Staphylococcus aureus, Pseudomonas aeruginosa), anaerobic bacteria (e.g., Clostridium sporogenes), yeasts (e.g., Candida albicans), and molds (e.g., Aspergillus brasiliensis) [30].
- Environmental isolates: Microbes isolated from the laboratory's own manufacturing and testing environments.
- Sterile saline or buffer for dilution.
- Methodology:
- Prepare suspensions of each test organism, calibrated to a low inoculum size (e.g., less than 100 CFU).
- Inoculate the test media in triplicate with each organism.
- Incubate at the specified temperatures and atmospheric conditions for the prescribed time.
- For media storage validation, sterilize and prepare media as per the standard procedure, including any secondary heating steps (e.g., microwave melting of stored agar). Then, inoculate with test organisms.
- Include uninoculated controls to check for sterility.
- Acceptance Criteria: Recovery of the test organisms should be at least 80% compared to a control. Recovery of less than 50% is generally unacceptable and indicates the presence of inhibitory substances or nutrient degradation [30].
Protocol for Verifying Incubator Performance and Conditions
The incubation environment must be rigorously controlled and monitored.
- Objective: To qualify the incubator's ability to maintain a uniform and stable temperature and, if applicable, atmospheric conditions throughout the chamber.
- Materials:
- Calibrated temperature data loggers or precision thermometers (minimum of 5, placed at various locations inside the incubator).
- Data loggers for humidity and CO₂, if required.
- Methodology:
- Place the data loggers throughout the incubator, ensuring coverage of corners, center, and near the door.
- Set the incubator to the required temperature (e.g., 32.5°C ± 1.0°C for bacterial enumeration).
- Record the temperature continuously for a minimum of 24-48 hours without opening the door to establish a baseline.
- Introduce a routine door-opening simulation (e.g., 3-5 brief openings per 8-hour period) and continue monitoring for another 24 hours to assess recovery time and fluctuation.
- Acceptance Criteria: The temperature must remain within the specified range (e.g., ±1.0°C or tighter if required) at all monitored locations, with recovery to the set point within a defined time after door openings [34].
Protocol for Evaluating Enumeration Method Accuracy and Precision
Demonstrating equivalence in enumeration is critical when verifying an alternative method against a compendial method.
- Objective: To compare the accuracy and precision of a new enumeration method (e.g., an automated colony counter) against the traditional manual counting method.
- Materials:
- Low-inoculum samples of a stable microorganism (e.g., Staphylococcus epidermidis or Bacillus atrophaeus).
- Standard culture media plates.
- Both the new and compendial counting systems.
- Methodology:
- Prepare a microbial suspension and perform a series of dilutions to obtain plates with a countable range of colonies (e.g., 25-250 CFU for spread plates).
- For accuracy, test a minimum of 20 samples across the reportable range, analyzed by both the new and reference methods. Calculate the percentage agreement [4].
- For precision, test a minimum of 2 positive and 2 negative samples in triplicate over 5 days by 2 different operators. Calculate the percentage of results in agreement [4].
- Acceptance Criteria: The alternative method should demonstrate non-inferiority or equivalence to the compendial method. The acceptance criteria, such as a defined percentage agreement or a statistical confidence interval, should be pre-established based on the manufacturer's claims and user requirements [4] [37].
Visualization of Error Pathways and Mitigation Workflows
The following diagrams map the relationship between common errors and their root causes, and outline a systematic workflow for method verification that incorporates error mitigation.
Error Cause-and-Effect Diagram
Method Verification and Error Control Workflow
The Scientist's Toolkit: Essential Reagents and Materials
The selection of appropriate reagents and materials is critical for minimizing variability and preventing errors in microbiological testing and method verification.
Table 2: Essential Research Reagent Solutions for Microbiological Testing
| Item | Function/Application | Key Considerations for Error Prevention |
|---|---|---|
| Culture Media (e.g., TSA, SDA) [30] | Supports growth and enumeration of bacteria, yeasts, and molds. | Must be validated for growth promotion of indicator and environmental organisms. pH, ionic strength, and osmolality must be controlled. Handling (e.g., autoclaving, reheating) must be standardized and validated [30]. |
| Indicator Organisms [30] | Used for media suitability testing and method validation. | Set should include aerobic and anaerobic bacteria, yeasts, and molds. Should be representative of potential contaminants. Recovery should be ≥80% of inoculum [30]. |
| Sterile Consumables (pipette tips, microplates) [35] | Acts as a barrier to contaminants during sample handling and analysis. | Use of pre-sterilized, single-use items eliminates variability from in-house cleaning and reduces contamination risk [35]. |
| Data Loggers [34] | Monitors temperature, humidity, and CO₂ in incubators and storage units. | Regular calibration is essential. Used to verify equipment performance and identify fluctuations that could impact microbial growth [34]. |
| Antimicrobial Inactivators (e.g., neutralizers) [30] | Inactivates antimicrobial properties in product samples during bioburden or sterility testing. | Critical for accurate microbial recovery. The effectiveness of the inactivator must be validated as part of the method suitability test [30]. |
| Automated Enumeration System [33] [37] | Provides objective, rapid colony counting or microbial detection. | Reduces subjectivity and enumeration errors associated with manual counting. Requires validation against the compendial method to demonstrate equivalency in accuracy and precision [33] [37]. |
Integrating Error Control into the Microbiological Method Verification Framework
A successful method verification study is not merely a technical exercise; it is a comprehensive quality assurance process. Controlling for contamination, incubation, and enumeration errors is fundamental to this process. Following a structured framework, such as that outlined in USP <1223> for alternative microbiological methods, ensures that all critical performance characteristics are evaluated while minimizing the influence of adventitious errors [37]. This includes establishing and adhering to pre-defined acceptance criteria for accuracy, precision, and specificity before commencing the study to prevent "specification creep" [30]. Furthermore, proper documentation of every aspect of the verification—including sample handling, equipment calibration, and raw data—is essential for audit trails and regulatory compliance [4] [37]. Ultimately, viewing error control not as a separate activity but as an integral component of method verification and routine laboratory practice is the key to generating reliable, high-quality microbiological data that ensures product safety and efficacy.
Microbiological method verification is a critical requirement in drug development, ensuring that analytical procedures consistently produce reliable and meaningful data about microbial identity, purity, and potency. Within this framework, database adequacy and taxonomic changes represent two fundamental yet often underestimated limitations that can compromise study validity and regulatory compliance. These constraints are particularly acute for methods relying on reference-dependent classification, such as 16S and 18S rRNA gene sequencing, where the quality of reference databases and stability of taxonomic nomenclature directly impact method performance [38].
The regulatory landscape recognizes these challenges. ICH Q2(R2) guidelines emphasize consideration of validation elements for analytical procedures, including those used for biological/biotechnological drug substances and products [39]. Similarly, the FDA acknowledges the importance of microbial data for verification within quality systems, though specific guidance on navigating database limitations remains an area of ongoing development [40]. This paper examines these limitations within a comprehensive verification framework, providing technical guidance for researchers designing robust microbiological method verification studies.
Critical Challenges in Microbiological Method Verification
Database Adequacy and Coverage Limitations
Taxonomic assignment methods fundamentally depend on comprehensive reference databases, which often suffer from significant structural and coverage limitations that directly impact method verification outcomes.
Database Imbalances: Common 16S and 18S rRNA databases exhibit extreme taxonomic imbalance, where a few taxa contain disproportionately high sequence counts while many others are severely underrepresented. Analysis reveals that in standard databases, approximately 80% of sequences often originate from only 20% of taxonomic groups [38]. This skew creates an accuracy paradox where methods appear to perform well in verification studies (e.g., showing 90% accuracy) while actually only recognizing patterns from high-frequency taxa effectively.
Coverage Gaps: Microbial marker genes correspond to only a small fraction of species' taxonomic names and known sequences [38]. This inherent coverage gap means taxonomic assignment methods cannot learn patterns from unseen taxa regardless of their algorithmic sophistication, creating fundamental limitations in method capabilities, particularly for novel or rare microorganisms.
Table 1: Database Limitations Impacting Method Verification
| Limitation Type | Impact on Method Verification | Potential Consequence |
|---|---|---|
| Taxonomic Imbalance | Biased performance evaluation favoring high-frequency taxa | Overestimation of method capability for rare organisms |
| Reference Database Coverage Gaps | Inability to classify novel or underrepresented species | False negatives or misclassification in environmental samples |
| Cross-Database Inconsistencies | Non-comparable results when using different reference databases | Verification results that cannot be replicated across laboratories |
Taxonomic Nomenclature Instability
The dynamic nature of microbial taxonomy introduces additional complexity to method verification, as taxonomic names and relationships continually evolve based on new scientific evidence.
Nomenclature Changes: Taxonomic names are regularly updated, added, or reclassified as new microorganisms are identified and phylogenetic relationships are refined [38]. This creates significant challenges for method verification, as a procedure validated against one taxonomic framework may become partially obsolete with nomenclature updates.
Database Choice Effects: Classification results using different taxonomic databases (e.g., Bergey's, NCBI) cannot be directly compared, as they employ different reference sequences and nomenclatures [38]. This variability complicates cross-study comparisons and method transfer between laboratories utilizing different reference standards.
Performance Metrics: Addressing Current Limitations
Weaknesses in Conventional Metrics
Traditional performance metrics used in method verification suffer from critical weaknesses that can mask true method capabilities and limitations.
Sequence Count Based Metrics: Conventional metrics like accuracy, precision, and recall are typically calculated as fractions based on prediction counts (e.g., Accuracy = N~correct~/N~total~) [38]. When applied to imbalanced databases, these metrics primarily measure performance on high-frequency taxa rather than a method's ability to recognize all taxa equally. This creates optimistically biased verification results that do not reflect real-world performance across diverse microbial communities.
Binary Error Measurement: Most conventional approaches measure prediction error in binary form (1 for incorrect, 0 for correct) without considering taxonomic relationships [38]. This approach treats all misclassifications as equally erroneous, despite the reality that misclassifications between closely related taxa are less severe than those between distantly related organisms. This results in information loss about error severity and fails to distinguish between method stability and catastrophic classification failures.
Advanced Metrics for Robust Verification
To address these limitations, researchers should incorporate more sophisticated metrics that better reflect methodological performance across the taxonomic spectrum.
Taxonomy Distance (TD): This metric quantifies the dissimilarity between predicted and actual taxonomic labels based on their positions in the taxonomic hierarchy [38]. TD is calculated as:
TD = Number of ranks in difference / Number of unique ranks in two taxa
This approach provides a graded assessment of classification errors rather than a simple binary right/wrong evaluation, enabling verification studies to distinguish between minor and major misclassifications.
Average Taxonomy Distance (ATD): By calculating the average TD across all evaluations, verification studies can obtain a more robust measure of overall method performance [38]. ATD can be further broken down by taxonomic groups (ATDbyTaxa) to identify method strengths and weaknesses across different microbial lineages.
Table 2: Comparison of Performance Metrics for Method Verification
| Metric | Calculation | Advantages | Limitations |
|---|---|---|---|
| Traditional Accuracy | N~correct~/N~total~ | Simple to calculate and interpret | Highly biased toward frequent taxa; misleading for imbalanced databases |
| Taxonomy Distance (TD) | Number of rank differences / Total unique ranks | Measures error severity; works with hierarchical taxonomy | More complex to implement; requires complete taxonomic tree |
| Average Taxonomy Distance (ATD) | ΣTD~i~/N | Robust overall performance measure; facilitates method comparison | May obscure performance patterns for specific taxonomic groups |
Experimental Approaches for Comprehensive Verification
Framework for Database Evaluation
Verification studies must include systematic assessment of database-related limitations through structured experimental protocols.
Database Characterization Protocol:
- Taxonomic Distribution Analysis: Quantify the distribution of sequences across taxonomic groups in reference databases using cumulative sequence fraction plots [38]
- Coverage Assessment: Evaluate database coverage against relevant target organisms, calculating the percentage of expected taxa represented with adequate sequence data
- Cross-Database Comparison: Compare classification results across multiple reference databases (e.g., RDP, Greengenes, SILVA) to quantify database-specific effects [38]
Representative Sample Selection: Instead of pruning large taxa to balance databases (which reduces sequence diversity), verification studies should implement stratified sampling approaches that maintain natural distributions while ensuring all taxonomic groups are represented in evaluation datasets [38].
Protocol for Assessing Taxonomic Change Robustness
Verification studies must evaluate method resilience to taxonomic nomenclature updates through specific experimental designs.
Nomenclature Stability Assessment:
- Longitudinal Database Analysis: Compare taxonomic assignments using different versions of the same reference database to quantify classification consistency across nomenclature updates
- Cross-Nomenclature Comparison: Process identical sample sets through different taxonomic frameworks (e.g., Bergey's vs. NCBI) to measure nomenclature-dependent effects [38]
- Method Stability Index: Develop a quantitative measure of method performance consistency across taxonomic database versions
Taxonomic Nomenclature Stability Assessment Workflow
Emerging Solutions and Advanced Approaches
Conformal Prediction Frameworks
Recent advances in semi-automated validation frameworks offer promising approaches to address database and taxonomic limitations. Conformal prediction combines deep learning classifiers with statistical reasoning to generate sets of plausible taxonomic labels at multiple ranks while providing rigorous control over prediction confidence [41].
This approach is particularly valuable for managing taxonomic uncertainty, as it:
- Produces singleton prediction sets that can be automatically accepted when confidence is high
- Provides statistical guarantees for prediction reliability across hierarchical taxonomic ranks
- Offers scalable validation solutions for large-volume data typical in microbiome studies [41]
Hierarchical Classification Methods
Rather than treating taxonomic assignment as a flat classification problem, hierarchical classification approaches explicitly incorporate taxonomic tree structure into the classification process [38]. These methods:
- Respect natural biological relationships between taxonomic groups
- Enable meaningful partial classifications when precise species-level assignment is uncertain
- Provide more biologically plausible error patterns than flat classification systems
Hierarchical Taxonomic Classification Structure
Data-Centric Architecture for Verification
Modern data-centric architectures create unified, accurate datasets as foundations for analytical applications, making data quality the cornerstone of robust verification systems [42]. These approaches emphasize:
- Metadata management for contextual information about data provenance and lineage
- AI-powered data quality tools for automated cleaning and validation processes
- Robust data governance policies ensuring accountability across the data lifecycle [43]
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Resources for Method Verification
| Reagent/Resource | Function in Verification Studies | Application Notes |
|---|---|---|
| RDP Naive Bayesian Classifier | Taxonomic assignment using 16S rRNA gene sequences | Requires verification against current database versions; compare with alternative methods [38] |
| SILVA Database | Comprehensive quality-checked ribosomal RNA database | Use specific versioning to maintain verification consistency; monitor for nomenclature updates [38] |
| Greengenes Database | 16S rRNA gene reference database with taxonomic naming | Compare performance against SILVA to assess database-specific effects [38] |
| Conformal Prediction Framework | Statistical calibration for classification confidence | Provides confidence measures for taxonomic assignments; implements cross-rank validation [41] |
| CAMI Benchmark Data Sets | Specially-generated data for method benchmarking | Provides standardized evaluation datasets across different microbial contexts [38] |
Database adequacy and taxonomic changes represent persistent yet manageable challenges in microbiological method verification. By implementing robust evaluation metrics like Taxonomy Distance, employing stratified sampling approaches, and adopting emerging frameworks like conformal prediction, researchers can design verification studies that more accurately reflect true method capabilities and limitations. As regulatory expectations evolve and microbial databases continue to expand, proactive management of these fundamental limitations will remain essential for generating reliable, reproducible microbiological data in drug development contexts. The experimental protocols and analytical frameworks presented here provide a pathway toward more comprehensive verification approaches that acknowledge and address these core methodological constraints.
In the rigorous framework of microbiological method verification, the emergence of discrepant results—unexpected or conflicting data points—is not a sign of failure but a critical opportunity for scientific problem-solving. Method verification is a mandatory process under regulations like the Clinical Laboratory Improvement Amendments (CLIA), required for unmodified FDA-approved tests before patient results can be reported [4]. It establishes that a test's performance characteristics—accuracy, precision, reportable range, and reference range—perform as intended in the user's specific operational environment [4].
When discrepant results occur during these studies, they indicate a potential disconnect between the assay's established performance and its application in a new context. A systematic approach to investigating these discrepancies is fundamental, as it ensures the reliability of the laboratory data that underpins drug development and patient care. This guide provides a structured strategy for researchers and scientists to diagnose, investigate, and resolve these challenges.
A Systematic Framework for Investigating Discrepancies
A structured investigation is paramount to efficiently and effectively identifying the root cause of discrepant results. The following workflow provides a logical sequence for troubleshooting. The diagram below outlines the core investigative process, from initial discovery to final resolution.
Phase 1: Confirmation and Documentation
The initial step is to confirm the discrepancy. This involves repeating the analysis of the affected sample, if possible, to rule out a simple transient error. Concurrently, initiate a documentation trail that captures all available metadata: sample identifier, analyst, instrument, reagent lots, date and time of analysis, and the original raw data. This information is crucial for spotting patterns or temporal associations.
Phase 2: Categorical Investigation
The investigation should systematically examine each stage of the testing process. The following table summarizes the key questions and potential causes to consider at each phase.
Table: Troubleshooting Discrepant Results Across Testing Phases
| Phase | Investigation Focus | Common Causes of Discrepancy |
|---|---|---|
| Pre-Analytical | Sample integrity, handling, and selection | Incorrect sample matrix; improper storage conditions; sample degradation; presence of interfering substances; selection of non-representative isolates [44]. |
| Analytical | Reagents, instrumentation, and operator | Expired or compromised reagents; equipment malfunction or improper calibration (e.g., detector wavelength accuracy, pipette volume); deviations from the verified method by the operator [4] [45]. |
| Post-Analytical | Data processing and reporting | Data transcription errors; incorrect application of the reference range; software miscalculation or misconfiguration of the reportable range [4]. |
Phase 3: Root Cause Analysis and Corrective Action
Once the most likely category is identified, a deeper root cause analysis is performed using tools like the "5 Whys." The outcome dictates the corrective action, which may include steps like requalifying an instrument, retraining staff, revising the procedure, or repeating part of the verification study. All findings and actions must be thoroughly documented to demonstrate due diligence and to inform future verification efforts [45].
Experimental Protocols for Root-Cause Analysis
When a categorical investigation points to a potential analytical issue, targeted experimental protocols are required to confirm the root cause. The following experiments are foundational to a method verification study and can be leveraged to pinpoint the source of a discrepancy.
Protocol for Assessing Accuracy
Accuracy confirms the acceptable agreement between the new method and a comparative method [4].
- Methodology: Test a minimum of 20 clinically relevant isolates, comprising a combination of positive and negative samples, in parallel with a validated comparative method [4].
- Data Analysis: Calculate the percentage agreement: (Number of results in agreement / Total number of results) × 100. The result must meet the manufacturer's stated claims or criteria determined by the laboratory director [4].
Protocol for Assessing Precision
Precision confirms acceptable variance within a run, between runs, and between operators [4].
- Methodology: Test a minimum of 2 positive and 2 negative samples (or samples with high-to-low values for semi-quantitative assays) in triplicate over 5 days by 2 different operators. For fully automated systems, operator variance may not be needed [4].
- Data Analysis: Calculate the percentage of agreement as with accuracy. This evaluates the reproducibility of the method under normal operating conditions [4].
The quantitative data from accuracy and precision experiments are often best summarized in a table for clear comparison and to highlight outliers.
Table: Key Performance Characteristics for Method Verification
| Performance Characteristic | Minimum Sample Requirement | Acceptance Criteria | Primary Function in Investigation |
|---|---|---|---|
| Accuracy | 20 positive and negative isolates [4] | Meet manufacturer's claims or lab-director defined criteria [4] | Identifies systematic error or bias in the method. |
| Precision | 2 positive & 2 negative, in triplicate, over 5 days, by 2 operators [4] | Meet manufacturer's claims or lab-director defined criteria [4] | Identifies random error and instability in the testing system. |
| Reportable Range | 3 known positive samples [4] | Results fall within established upper and lower limits [4] | Confirms the method provides a valid result for samples at the assay's limits. |
| Reference Range | 20 isolates representative of the patient population [4] | Matches the established "normal" result for the population [4] | Ensures the method is correctly calibrated for the intended patient base. |
The Scientist's Toolkit: Essential Research Reagent Solutions
A successful investigation relies on high-quality, traceable materials. The following table details essential reagents and materials used in method verification studies.
Table: Essential Research Reagent Solutions for Verification Studies
| Item | Function in Verification & Investigation |
|---|---|
| Reference Standards & Controls | Commercially available materials with defined analyte concentrations; used as benchmarks for assessing accuracy, precision, and for daily quality control to detect instrument or reagent drift [4]. |
| Proficiency Testing (PT) Samples | External, blinded samples of known value; used to objectively assess the laboratory's testing performance and identify potential biases compared to peer laboratories [4]. |
| De-identified Clinical Samples | Well-characterized residual patient samples; used to verify the reference range and assess method performance against real-world specimens, which is critical for confirming a discrepancy [4]. |
| CLSI Document Guidelines | Framework documents (e.g., EP12-A2, M52, MM03-A2) providing standardized protocols and acceptance criteria for evaluating method performance, ensuring investigations are aligned with industry best practices [4]. |
In microbiological research and drug development, the integrity of data is paramount. Discrepant results, when approached with a structured and rigorous problem-solving strategy, are not merely obstacles. They are integral to the method verification process, providing the evidence needed to ensure that an analytical method is robust, reliable, and fit for its intended purpose in the complex landscape of patient care. Mastering the interpretation of these discrepancies solidifies the scientific foundation upon which safe and effective therapeutics are built.
Corrective and Preventive Actions (CAPA) for Verification Failures
In the tightly regulated environments of pharmaceutical, medical device, and clinical laboratories, method verification is a mandatory process to demonstrate that a validated test performs as intended when installed in a user's laboratory [4]. A verification failure is not merely a procedural setback; it represents a significant quality event indicating that a laboratory cannot reliably reproduce a method's established performance characteristics. Addressing such failures through a robust Corrective and Preventive Action (CAPA) system is fundamental to ensuring the integrity of microbiological data, patient safety, and regulatory compliance.
The purpose of this guide is to provide researchers and drug development professionals with a systematic framework for investigating, correcting, and preventing verification failures, thereby strengthening the overall foundation of microbiological research and quality control. Effective CAPA processes transform isolated failures into opportunities for systemic improvement, embedding corrective actions to address existing problems and preventive actions to mitigate future risks within the context of microbiological method verification [46] [47].
Understanding Verification Failures in Microbiological Context
Verification vs. Validation: A Critical Distinction
A clear understanding of terminology is essential for proper failure investigation. In a laboratory context, verification and validation are distinct processes with different implications for CAPA [4]:
- Verification: A one-time study for unmodified U.S. Food and Drug Administration (FDA)-approved or cleared tests. It demonstrates that the test performs in line with the manufacturer's previously established performance characteristics when used as intended in the user's laboratory environment [4].
- Validation: A process to establish that an assay works as intended. This is required for non-FDA cleared tests (e.g., laboratory-developed methods) and modified FDA-approved tests [4].
This distinction is critical because the scope of a CAPA investigation will differ significantly depending on whether the failure occurred during verification of a standard method or validation of a modified or novel method.
Key Performance Characteristics in Verification
Method verification studies for non-waived systems (tests of moderate or high complexity) under the Clinical Laboratory Improvement Amendments (CLIA) must verify several key performance characteristics before reporting patient results [4]. Failures can occur in one or more of these areas:
- Accuracy: The agreement of results between the new method and a comparative method.
- Precision: The consistency of results, including within-run, between-run, and operator variance.
- Reportable Range: The upper and lower limits of detection that the test system can reliably report.
- Reference Range: The normal expected result for the tested patient population.
The CAPA Lifecycle for Verification Failures
A structured CAPA process ensures that verification failures are resolved systematically and permanently. The lifecycle can be visualized as a continuous improvement cycle, adapted for the technical specifics of method verification.
CAPA Workflow for Verification Failures
The diagram below outlines the sequential workflow for managing a verification failure through the CAPA lifecycle, from initial detection to closure and effectiveness monitoring.
Phase 1: Identification and Immediate Response
The initial response to a verification failure focuses on containment and problem definition.
3.2.1 Failure Detection and Documentation: A verification failure may be detected through various means, including falling outside acceptance criteria for accuracy, precision, reportable range, or reference range studies [4]. Immediately document all relevant details: the specific test parameters that failed, date and time, personnel involved, instrument identifiers, reagent lot numbers, and environmental conditions.
3.2.2 Immediate Containment Actions: Implement corrections to prevent further impact. This may include [47]:
- Quarantining affected samples or reagents
- Halting verification activities until the situation is stabilized
- Notifying relevant stakeholders (quality unit, laboratory director)
- Preserving all relevant data, including raw instrument outputs and control results
3.2.3 Problem Statement Formulation: Develop a clear, concise problem statement that is specific, measurable, and bounded. A well-defined problem statement might be: "The verification study for the Vitek 2 AST-GN80 card failed accuracy testing for amikacin, with only 85% essential agreement (20/24 isolates) compared to the broth microdilution reference method, falling below the required 90% acceptance criterion."
Phase 2: Investigation and Root Cause Analysis
The investigation phase aims to determine the fundamental reason for the verification failure, moving beyond symptoms to address underlying causes.
Root Cause Analysis Techniques
Several structured methods can be applied to investigate verification failures:
5 Whys Technique: A simple method of repeatedly asking "why" to drill down from the symptom to the root cause. For a verification failure, this might reveal that what initially appeared to be a reagent issue actually stems from inadequate training or procedural deficiencies [47] [48].
Fishbone Diagram (Ishikawa): A visual technique that categorizes potential causes to explore all possibilities. For microbiological verification failures, categories might include: Methods, Materials, Equipment, Environment, People, and Measurements [47] [48].
The following diagram illustrates how these elements come together in a structured analysis of a verification failure.
Investigation Methodology
A thorough investigation should include both technical and procedural elements:
Technical Assessment: Review all verification data against acceptance criteria. Examine accuracy, precision, reportable range, and reference range results systematically [4]. Compare actual performance with manufacturer claims and regulatory requirements.
Process Analysis: Evaluate whether the verification study was designed and executed correctly. This includes assessing:
- Sample selection and preparation methods
- Quality control procedures
- Instrument maintenance and calibration records
- Technician competency and training records
- Environmental monitoring data
Comparative Testing: Where appropriate, conduct parallel testing with a reference method or previously verified system to isolate the source of discrepancy [4].
Phase 3: Action Planning and Implementation
Based on the confirmed root cause, develop a comprehensive action plan that addresses both immediate correction and long-term prevention.
Developing the CAPA Plan
The action plan should clearly distinguish between corrective and preventive actions:
Corrective Actions: Address the specific verification failure and its root cause. Examples include [47]:
- Recalibrating or repairing faulty equipment
- Retraining staff on specific techniques
- Replacing compromised reagents or quality control materials
- Repeating all or part of the verification study
Preventive Actions: Address systemic issues to prevent recurrence. Examples include [47]:
- Revising standard operating procedures (SOPs) to clarify ambiguous steps
- Enhancing training programs based on identified knowledge gaps
- Implementing additional quality controls or verification checkpoints
- Improving documentation templates to reduce errors
Action Plan Implementation
Successful implementation requires clear assignment of responsibility, realistic timelines, and appropriate resource allocation:
- Assign each action item to specific personnel with the necessary expertise
- Establish definitive due dates based on priority and complexity
- Allocate necessary resources (financial, personnel, equipment)
- Document all implementation activities with appropriate evidence
Phase 4: Effectiveness Verification and Closure
The final phase ensures that the implemented actions have successfully resolved the issue and will prevent recurrence.
3.5.1 Verification of Corrective Actions: Confirm that the specific verification failure has been resolved. This typically involves repeating the failed portion of the verification study and demonstrating that results now meet all acceptance criteria [4] [47].
3.5.2 Effectiveness Monitoring: Implement a plan to monitor the long-term effectiveness of preventive actions. This might include [47] [48]:
- Tracking similar metrics over subsequent verification studies
- Monitoring related quality indicators (e.g., proficiency testing performance)
- Conducting periodic audits of the revised processes
- Verifying that recurrence rates for similar issues have decreased
3.5.3 CAPA Closure: Formal closure occurs only after [47]:
- All planned actions have been completed
- Effectiveness checks demonstrate successful resolution
- All documentation is complete and accurate
- The CAPA has been reviewed and approved by designated quality personnel
Quantitative Framework for Verification Failure Investigation
Method verification requires testing against specific numerical acceptance criteria. The table below outlines standard verification requirements for qualitative and semi-quantitative microbiological methods, which can serve as a framework for investigating failures.
Table 1: Verification Requirements for Microbiological Methods [4]
| Performance Characteristic | Minimum Sample Requirements | Acceptance Criteria | Common Failure Points |
|---|---|---|---|
| Accuracy | 20 clinically relevant isolates (combination of positive and negative) | Meet manufacturer's stated claims or laboratory-defined criteria | Insufficient essential agreement with reference method; inappropriate sample selection |
| Precision | 2 positive + 2 negative samples tested in triplicate for 5 days by 2 operators | Meet manufacturer's stated claims or laboratory-defined criteria | Excessive within-run, between-run, or operator variability; inconsistent results over time |
| Reportable Range | Minimum 3 samples (known positives for detected analyte) | Results fall within manufacturer-established reportable range | Failure to detect near cutoff values; limited linearity or dynamic range |
| Reference Range | Minimum 20 isolates representative of patient population | Matches manufacturer's range or laboratory's established normal values | Does not represent laboratory's typical patient population; incorrect normal values established |
Successful investigation and resolution of verification failures requires specific tools and resources. The following table outlines essential components of a CAPA toolkit for microbiological laboratories.
Table 2: Essential Research Reagent Solutions and Resources for CAPA Investigations
| Tool/Resource | Function in CAPA | Application Example |
|---|---|---|
| Reference Strains & QC Organisms | Well-characterized microorganisms with defined profiles for verifying test validity [22] | Investigating accuracy failures by testing with known positive and negative controls |
| ISO 16140 Series | International standards for method validation and verification protocols [17] | Designing verification studies and troubleshooting failures according to standardized approaches |
| Statistical Analysis Software | Data analysis tool for evaluating precision, accuracy, and other performance characteristics | Identifying trends and significant deviations in verification data |
| Root Cause Analysis Templates | Structured forms for 5 Whys, Fishbone diagrams, and other RCA tools [48] | Systematically investigating failures beyond superficial causes |
| Electronic Quality Management System (eQMS) | Digital platform for tracking CAPA activities, deadlines, and effectiveness checks [49] | Managing the entire CAPA lifecycle with proper documentation and audit trails |
| CLSI Standards (e.g., EP12, M52) | Guidelines for evaluating qualitative test performance and verifying commercial microbial systems [4] | Establishing appropriate acceptance criteria and verification protocols |
Integration with Broader Quality Systems
CAPA for verification failures should not operate in isolation but must be integrated into the broader quality management system.
6.1 Regulatory Framework: CAPA procedures must comply with relevant regulations, including FDA 21 CFR 820 for medical devices, EU GMP Annex 15, and CLIA requirements for laboratory testing [50] [48]. The FDA emphasizes that CAPA documentation demonstrates whether a quality system is effective and enables identification and resolution of problems [46].
6.2 Management Review: Information about verification failures and resulting CAPAs should be disseminated for management review [50]. This ensures visibility of systemic issues and appropriate resource allocation for quality improvements.
6.3 Continuous Improvement: A well-functioning CAPA system contributes to continuous improvement by identifying patterns across multiple verification failures. Trending of CAPA data can reveal underlying systemic issues that require higher-level intervention [46] [47].
Verification failures in microbiological testing represent critical decision points for quality systems. A robust, well-documented CAPA process transforms these failures from compliance liabilities into opportunities for meaningful improvement. By implementing the structured approach outlined in this guide—with its emphasis on thorough investigation, evidence-based actions, and systematic effectiveness verification—researchers and quality professionals can ensure that their laboratories produce reliable, defensible microbiological data. Ultimately, excellence in managing verification failures through CAPA reinforces the scientific integrity of the entire drug development and manufacturing process, protecting both patient safety and product quality.
Method verification is a foundational requirement in microbiology laboratories, mandated by standards such as the Clinical Laboratory Improvement Amendments (CLIA) for non-waived systems before patient results can be reported [4]. This process confirms that a validated method performs according to established performance characteristics in the user's environment. Traditional verification workflows, however, are inherently manual, complex, and vulnerable to human error. These errors can trigger a cascade of commercial and legal issues, leading to poor decisions that impact product safety, patient care, and business sustainability [22].
The integration of automation technologies presents a transformative opportunity to streamline these workflows, enhance data integrity, and fundamentally reduce the risk of human error. This guide examines the core principles and practical applications of automation in microbiological method verification, providing researchers and drug development professionals with a framework for designing robust, efficient, and error-resistant verification studies.
Foundational Concepts: Verification, Validation, and Automation
Distinguishing Verification from Validation
A critical first step in optimizing workflows is understanding the distinction between method validation and method verification, two terms often used interchangeably but with different meanings [4] [17].
- Method Validation establishes that an assay works as intended. This process is required for non-FDA cleared tests, such as laboratory-developed methods (LDMs) or modified FDA-approved tests [4]. Per the ISO 16140 series, validation is the initial stage to prove a method is "fit for purpose," often involving a method comparison study and an interlaboratory study [17].
- Method Verification is a one-time study demonstrating that an unmodified, FDA-approved or cleared test performs in line with its previously established performance characteristics when used as intended by the manufacturer in a specific laboratory [4]. It is the process whereby a laboratory demonstrates that it can satisfactorily perform a validated method [17].
The Scope of Automatable Tasks
Automation in pharma validation refers to the integration of automated technologies and systems to validate pharmaceutical manufacturing equipment, processes, or systems with minimal human intervention [51]. In the context of method verification, automation can be applied to several key areas:
- Equipment Qualification: Automated tools can monitor and document Installation, Operational, and Performance Qualifications (IQ/OQ/PQ) [51].
- Data Collection and Processing: Automated systems can collect, transcribe, and calculate results, minimizing manual data entry errors [52].
- Execution of Repetitive Tasks: Automated systems can perform high-volume, repetitive testing with consistent precision, such as serial dilutions or plate inoculations [51].
The choice between human-in-the-loop automation and fully autonomous workflow automation depends on a risk-based assessment. A human-in-the-loop approach keeps human control for validation, quality control, or complex decision-making, which is vital for regulated industries. In contrast, fully autonomous workflow automation leverages advanced AI to operate with minimal to zero human intervention, ideal for high-volume, repetitive processes [53].
A Framework for Automated Verification
Core Verification Characteristics and Automated Assessment
For an unmodified FDA-approved test, laboratories must verify specific performance characteristics. The table below summarizes the CLIA requirements and suggests how automation can be integrated into the assessment of each characteristic [4].
Table 1: Core Verification Characteristics and Automation Applications
| Characteristic | Traditional Verification Approach | Automation Application & Benefit |
|---|---|---|
| Accuracy | Test a minimum of 20 clinically relevant isolates with a combination of positive and negative samples [4]. | Automated image recognition systems can classify medications with >95% accuracy, reducing manual interpretation errors [52]. Intelligent Document Processing (IDP) can automate data comparison. |
| Precision | Test a minimum of 2 positive and 2 negative samples in triplicate for 5 days by 2 operators [4]. | Automated liquid handlers and plate readers can execute and read replicates with unwavering consistency, eliminating operator-induced variance. |
| Reportable Range | Verify using a minimum of 3 known positive samples [4]. | Automated systems can systematically test samples across the entire claimed range (e.g., high, mid, and low concentrations) and auto-flag results falling outside verifiable limits. |
| Reference Range | Verify using a minimum of 20 isolates representative of the laboratory's patient population [4]. | Digital workflows can automatically collate results from verified samples to establish and statistically confirm the reference range, ensuring a traceable and auditable process. |
Quantitative Performance of Automated Systems
Recent studies demonstrate the efficacy of automation in reducing error. The following table summarizes key performance metrics from an automated verification system.
Table 2: Quantitative Performance Data of an Automated Medication Verification System (AMVS)
| Performance Metric | Result | Context / Significance |
|---|---|---|
| Overall Accuracy | > 95% | Identification of drug types and segmentation analysis [52]. |
| Accuracy (Fewer than 10 drug types) | ~ 96% | High accuracy for smaller, complex mixtures [52]. |
| Accuracy (Ten drug types) | ~ 93% | Slight decrease with complexity, yet remains highly effective [52]. |
| Key Innovation | Fusion of edge detection and Convolutional Neural Networks (CNNs) | Enables accurate drug segmentation without manual labeling during model construction [52]. |
Experimental Protocols for Automated Verification
Protocol: Automated Image-Based Verification for Solid Dosage Forms
This protocol is adapted from a study on an Automated Medication Verification System (AMVS), which can be modeled for verifying microbiological specimens or solid dosage forms [52].
1. Hypothesis: An automated system combining edge detection and a pre-trained classification model can verify medication types with >95% accuracy, reducing manual error.
2. Materials and Reagents:
- Drug Verification Box: A sealed, light-tight enclosure to minimize optical variations [52].
- Single-Board Computer: Raspberry Pi 4B or similar for portability [52].
- Camera Module: Fixed at a specified distance from the sample tray (e.g., 70mm) [52].
- Consistent LED Lighting: To ensure stable image capture [52].
- 3D-Printed Sample Tray: With angled walls to prevent contact between items and simplify segmentation [52].
3. Methodology:
- Dataset Collection: Capture images of individual reference items (e.g., 30 images each for 10 drug categories) to build a classification model [52].
- Edge Detection: Use the
findContoursfunction in OpenCV, preceded by thresholding or the Canny edge detection method, to delineate object boundaries within an image containing multiple items [52]. - Image Classification: Feed each segmented image region into a pre-trained classification model (e.g., ResNet) to predict the item type. This eliminates the need for manual annotation of medication regions [52].
- Verification: The system's prediction is compared against the expected result for verification.
4. Data Analysis:
- Calculate the percentage of correct identifications over the total number of tests.
- Report accuracy separately for different complexity levels (e.g., number of items per image) [52].
Protocol: Automated Data Integrity Checks for Quantitative Assays
1. Hypothesis: An Intelligent Document Processing (IDP) solution can automate the transcription of data from instrument reports into Laboratory Information Management Systems (LIMS), reducing transcription errors to less than 1%.
2. Materials and Reagents:
- IDP Software Solution: A tool with high-accuracy Optical Character Recognition (OCR) capable of integrating with existing lab systems [54].
- Data Source: Digital output files or scanned images of instrument reports.
3. Methodology:
- System Integration: Configure the IDP tool to seamlessly integrate with the lab's LIMS and data sources [54].
- Template Setup: Define templates for different report types to instruct the IDP on where to find specific data points (e.g., sample ID, absorbance value, calculated concentration).
- Automated Extraction and Validation: The IDP tool automatically extracts data, cross-references it with pre-defined acceptance criteria (e.g., reference range), and flags outliers or mismatches for human review [54].
- Secure Data Transfer: Validated data is automatically transcribed into the appropriate fields in the LIMS, with a full audit trail.
4. Data Analysis:
- Monitor the rate of exceptions flagged by the system that require human intervention.
- Periodically audit a subset of automated transcriptions against source documents to confirm error rates meet the sub-1% target.
The Researcher's Toolkit: Essential Solutions for Automated Verification
Table 3: Research Reagent Solutions for Automated Verification Workflows
| Solution / Material | Function in Verification | Specific Application Example |
|---|---|---|
| Quality Control (QC) Organisms | Well-characterized microorganisms with defined profiles serve as verified standards for validating testing methodologies and monitoring test performance [22]. | Used in accuracy and precision studies to ensure the automated method correctly identifies and enumerates target microbes. |
| Reference Materials & Proficiency Test Standards | Commercially available standards quantitatively certified for use in method verification and proficiency testing to ensure data accuracy and support accreditation [22]. | Serves as the known "truth set" for verifying the reportable range and accuracy of an automated method. |
| Pre-Trained Classification Models (e.g., ResNet) | Allows for rapid fine-tuning and optimization of image-based classification tasks without the need for extensive data or training from scratch [52]. | Can be adapted for automated colony counting or morphological analysis in microbial enumeration tests [52]. |
| Intelligent Document Processing (IDP) | Automates the extraction, validation, and routing of data from documents, improving speed and accuracy while ensuring compliance [54]. | Automates the transcription of data from instrument reports into LIMS for precision and reportable range studies. |
| Automated Microbial Controls | Ready-to-use microbial controls in user-friendly formats simplify compliance and streamline QC testing in automated workflows [22]. | Provides a consistent and standardized inoculum for precision studies run on automated plating or enumeration systems. |
Workflow Visualization
Automated Method Verification Workflow
The following diagram illustrates the streamlined, error-resistant process for conducting a method verification study using automation.
Human-in-the-Loop Decision Model
Automation in regulated environments often requires strategic human oversight. This diagram outlines a risk-based decision model for determining the appropriate level of automation.
Regulatory and Strategic Considerations
Implementing automation in a GxP environment requires careful planning and adherence to regulatory guidelines. The FDA recognizes the increased use of AI and automation throughout the drug product lifecycle and is developing a risk-based regulatory framework to promote innovation while protecting patient safety [55]. Key considerations include:
- Computer System Validation (CSV): Automated verification tools are subject to CSV, a regulatory requirement focusing on validating systems used in drug manufacturing and clinical trials to ensure data integrity and patient safety [51].
- Data Integrity: Automated systems must comply with ALCOA+ principles, ensuring data is Attributable, Legible, Contemporaneous, Original, Accurate, and Complete [51].
- Lifecycle Approach: Validation activities should be incorporated from system design to decommissioning, leveraging automation to streamline each phase [51].
- Leveraging Harmonized Standards: Always consult and verify against current pharmacopoeial standards, such as the harmonized USP general chapter <61> Microbial Enumeration Tests, which becomes official on May 1, 2025 [56].
The optimization of verification workflows through automation is no longer a futuristic concept but a present-day imperative for enhancing quality and efficiency in microbiological and pharmaceutical research. By strategically integrating technologies such as automated sample processors, IDP, and AI-driven image classification, laboratories can significantly reduce the human error inherent in manual processes. A hybrid model, which applies full automation for low-risk, repetitive tasks while retaining human oversight for complex, high-risk decisions, offers a practical and compliant path forward. As regulatory bodies like the FDA continue to formalize guidelines for AI and automation, embracing these technologies will be fundamental for any research organization aiming to ensure data integrity, accelerate development, and uphold the highest standards of patient safety.
Advanced Validation Protocols and Comparative Method Assessment
In clinical microbiology and drug development, the reliability of test results is paramount. The processes of method verification and method validation are foundational to ensuring that diagnostic tests and microbial assays perform as intended. However, these terms are not interchangeable; they apply to distinct scenarios governed by different regulatory and scientific requirements. A verification is a one-time study demonstrating that an unmodified, FDA-cleared or -approved test performs in line with established manufacturer claims in the user's environment [4]. In contrast, a validation is a more extensive process meant to establish that an assay works as intended when it is a laboratory-developed test (LDT) or a modified FDA-approved test [4]. This distinction is critical for researchers and developers, as the choice between a commercial test and a custom-developed method can significantly impact development timelines, regulatory pathways, and the ultimate defensibility of generated data.
The recent regulatory shift concerning Laboratory Developed Tests (LDTs) underscores the importance of rigorous method establishment. While a federal district court vacated the FDA's May 2024 final rule in March 2025, which had explicitly added LDTs to the definition of in vitro diagnostic products, the landscape remains dynamic [57] [58]. This guide focuses on the fundamental scientific principles of when validation is required, providing a stable technical framework for researchers irrespective of ongoing regulatory updates.
Core Definitions: Verification vs. Validation
Understanding the precise meaning of key terms is the first step in determining the correct methodological approach.
- Verification: The process of confirming that an unmodified, FDA-cleared or approved test performs according to the manufacturer's stated performance characteristics when implemented in a specific laboratory [4]. It is a one-time study to confirm established claims.
- Validation: The process of establishing through extensive testing that a laboratory-developed test (LDT) or a modified FDA-approved test performs reliably for its intended purpose [4]. Validation defines the performance characteristics, limitations, and appropriate operating conditions of a new or altered method [59].
- Laboratory Developed Test (LDT): An in vitro diagnostic test that is developed, validated, and performed within a single laboratory [57].
- Modified Method: An FDA-approved test that has been altered in a way not specified as acceptable by the manufacturer. This can include changes to specimen types, sample dilutions, or test parameters like incubation times [4].
The following workflow diagram (Figure 1) provides a decision pathway for determining whether a method requires verification or full validation.
Figure 1. Decision Workflow for Method Verification vs. Validation.
When is Full Validation Required?
Full method validation is a rigorous, resource-intensive process. It is mandated in the following specific scenarios, which are common in research and development of novel microbiological assays.
Laboratory Developed Tests (LDTs)
An LDT is any test developed and performed within a single laboratory [4]. LDTs are essential for addressing complex or highly specialized diagnostic needs not met by commercially available products [60]. Since these tests are created in-house, no prior performance characteristics exist, necessitating a full validation to establish:
- Analytical Specificity and Sensitivity: The ability of the test to correctly identify the target analyte (e.g., a specific microbial gene or antigen) and not react with non-target materials [59].
- Reproducibility and Precision: The consistency of results when the test is performed multiple times on the same sample, including within-run, between-run, and between-operator variance [4] [61].
- Reportable Range: The span of results, from low to high, that the test can reliably measure [4].
- Limit of Detection (LoD): The lowest amount of the target analyte (e.g., microbial load) that can be reliably detected [61].
- Robustness: The test's reliability when minor, deliberate changes are made to operational parameters, such as incubation temperature or reagent volume [59].
Modified Commercially Available Tests
Any modification to an FDA-cleared or approved test that falls outside the manufacturer's acceptable parameters requires a full validation of the modified aspect of the test [4]. Common modifications that trigger validation include:
- Changes in Specimen Type: Using a sample type (e.g., saliva) not validated by the manufacturer for a test approved for swab samples.
- Alterations to Test Parameters: Changing incubation times, temperatures, or sample dilution procedures.
- Use of Non-Approved Components: Substituting a key reagent, buffer, or piece of equipment not specified by the manufacturer.
The CLSI and EUCAST strongly caution developers that unnecessary deviations from reference methods, such as the standard broth microdilution for antimicrobial susceptibility testing, can lead to increased costs, regulatory hurdles, and delays in test availability [62]. Modifications aimed solely at producing more favorable results, such as lower minimal inhibitory concentration (MIC) values, are not scientifically valid and are strongly discouraged [62].
Tests for Microbial Forensics and Biodefense
In the field of microbial forensics, where results can have severe legal and national security consequences, the validation requirements are exceptionally stringent. A multi-tiered validation framework is used to ensure results are both reliable and legally defensible [59]:
- Developmental Validation: The initial acquisition of test data to determine the conditions and limitations of a newly developed method [59].
- Internal Validation: The accumulation of test data within an operational laboratory to demonstrate that staff can successfully perform the established methods and obtain reliable results [59].
- Preliminary Validation: An expedited evaluation of a method used to investigate a biocrime or bioterrorism event when no fully validated method is available. This is conducted with the understanding that the method's limitations are documented and considered in the interpretation of results [59].
Table 1: Scenarios Requiring Full Method Validation
| Scenario | Description | Primary Goal | Common Examples |
|---|---|---|---|
| LDT Implementation | A test is developed from scratch within a single laboratory. | Establish all performance characteristics and limitations. | Quantitative PCR for a novel viral target, custom microbial identification array. |
| Test Modification | An FDA-approved test is altered in a way not specified by the manufacturer. | Validate the performance and impact of the specific modification. | Using a different specimen type, changing incubation time or reagent. |
| Microbial Forensics | A method whose results may be used in legal or attribution proceedings. | Ensure data is scientifically robust and legally defensible. | Strain typing for attribution, toxin detection in a biocrime. |
Experimental Design for Validation Studies
A successful validation study begins with a carefully constructed validation plan, which should be reviewed and approved by the laboratory director or principal investigator [4] [59]. The plan outlines the study's purpose, design, acceptance criteria, and resource requirements.
Core Performance Characteristics and Testing Protocols
For a comprehensive validation, the following performance characteristics must be assessed. The experimental design varies based on whether the assay is qualitative, semi-quantitative, or fully quantitative.
Table 2: Experimental Design for Key Validation Parameters
| Parameter | Definition | Qualitative/Semi-Quantitative Assay Protocol | Quantitative Assay Protocol |
|---|---|---|---|
| Accuracy | Agreement between the test result and the true value. | Samples: Min. 20 relevant isolates (positive & negative).Calculation: % Agreement = (Agreeing Results / Total Results) × 100 [4]. | Samples: Test against a reference standard or method.Calculation: Linear regression and Bland-Altman analysis to assess bias [61]. |
| Precision | Closeness of agreement between repeated measurements. | Samples: Min. 2 positive & 2 negative, tested in triplicate for 5 days by 2 operators.Calculation: % Agreement across all replicates [4]. | Samples: Test multiple controls across the reportable range over 20 days.Calculation: Standard Deviation (SD) and % Coefficient of Variation (%CV) at different concentrations [61]. |
| Reportable Range | The span of reliable results the test can produce. | Samples: Min. 3 known positive samples.Evaluation: Verify that results are correctly reported as "Detected" or "Not Detected" against established cutoffs [4]. | Samples: A dilution series of a known concentration, spanning the expected range.Evaluation: Establish the range where the method shows a linear response (e.g., R² > 0.98) [61]. |
| Analytical Sensitivity (LoD) | The lowest amount of analyte reliably detected. | Samples: Serial dilutions of a known positive sample or control.Evaluation: The lowest concentration where ≥95% of replicates test positive [4]. | Samples: Serial dilutions of a calibrated standard.Evaluation: The lowest concentration where the result is both detectable and within the stated imprecision limit (e.g., CV < 20%) [61]. |
| Analytical Specificity | The ability to detect the target without cross-reactivity. | Samples: Test against a panel of near-neighbor organisms and common interfering substances (e.g., blood, mucus).Evaluation: No false-positive results should occur [59]. | (Protocol is similar to qualitative assays) |
Special Considerations for Quantitative Assays
Quantitative molecular methods, such as Q-PCR and QRT-PCR used for viral load testing, require additional statistical rigor [61]. Key considerations include:
- Standard Curves and Calibrators: A calibration curve is created by testing a dilution series of a known standard (e.g., copies/mL) in parallel with patient samples. The slope and efficiency of this curve are critical for accurate quantification [61].
- Understanding Variability: Assay variability, or "noise," is inherent. For viral loads, this is often expressed in log10 units. The Medical Decision Interval (MDI) is the clinically significant change in microbial replication and is calculated as the sum of the biological variation and the intra-assay imprecision. For example, the MDI for HIV-1 is 0.5 log10 units [61].
- Statistical Analysis: Precision should be assessed using standard deviation in log10 units rather than solely relying on %CV, as %CV can be misleading across a wide quantitative range [61].
The following workflow (Figure 2) outlines the key stages in executing a validation study, from planning to implementation.
Figure 2. Key Stages of a Method Validation Study Workflow.
The Scientist's Toolkit: Essential Reagents and Materials
A successful validation study relies on high-quality, well-characterized reagents and controls. The following table details essential research reagent solutions and their critical functions in method validation.
Table 3: Essential Research Reagent Solutions for Validation Studies
| Reagent / Material | Function in Validation | Key Considerations |
|---|---|---|
| Reference Standards | Calibrators with a known concentration of the target analyte (e.g., CFU/mL, copies/mL) used to create a standard curve for quantitative assays [61]. | Traceability to an international standard is critical for comparability between labs. Purity and stability must be verified. |
| Quality Controls (Positive & Negative) | Materials used to monitor the daily performance of the assay. Positive controls ensure detection capability, while negative controls monitor for contamination [4]. | Should be independent of the calibration material. Matrix should mimic patient samples as closely as possible. |
| Clinically Relevant Isolates | A well-characterized panel of microbial strains used to establish accuracy, analytical specificity, and reportable range [4]. | Must include target organisms, near-neighbor species (for specificity), and a range of concentrations. |
| Interference Substances | Substances like blood, mucus, or common medications used to challenge the assay and evaluate analytical specificity under realistic conditions [59]. | Tested at clinically relevant concentrations to ensure they do not cause false positives or negatives. |
| Characterized Clinical Samples | De-identified residual patient samples that have been tested by a reference method. Used for method comparison and accuracy studies [4]. | Provides the most realistic assessment of test performance but requires ethical approval and privacy protections. |
Within the framework of microbiological method verification study design, demonstrating that a method is "fit-for-purpose" is a fundamental regulatory and scientific requirement. This evaluation ensures that an analytical method consistently produces reliable results for its specific intended use. Two of the most critical and complex components of this process are matrix extension (applying a validated method to new sample types) and scope determination (defining the exact boundaries of the method's application) [17]. For researchers and drug development professionals, a structured approach to these tasks is not optional but is mandated by standards such as the ISO 16140 series for food and feed chains and CLIA regulations for clinical microbiology [4] [17]. This guide provides an in-depth technical examination of the experimental protocols and decision-making frameworks required to robustly establish and document the fitness-for-purpose of microbiological methods.
Core Concepts and Regulatory Framework
Distinguishing Between Verification and Validation
A foundational step in planning a fitness-for-purpose evaluation is understanding the distinction between method validation and method verification, terms often used interchangeably but with distinct meanings.
- Method Validation is the primary process of establishing that an assay works as intended. It is required for non-FDA-cleared tests, such as laboratory-developed tests (LDTs), or for modified FDA-approved methods. Any change to the manufacturer's instructions, such as using different specimen types or altering test parameters, constitutes a modification that requires validation [4].
- Method Verification is a one-time study performed for unmodified, FDA-approved or cleared tests. It demonstrates that the test performs in line with the manufacturer's established performance characteristics within the user's specific laboratory environment [4]. The process of matrix extension often blurs this line, as applying a verified method to a new sample matrix may be considered a modification, thereby requiring a more rigorous, validation-like approach.
The Principle of Fitness-for-Purpose
At its core, fitness-for-purpose means that the performance characteristics of a method are appropriate for the context in which the results will be used. In pharmaceutical microbiology, inaccurate results can lead to batch failure, regulatory penalties, and patient harm, underscoring the critical nature of this principle [63]. The evaluation must be based on objective evidence that the method consistently meets pre-determined specifications for its intended application, a expectation central to FDA regulations [64].
Scope Determination: Defining the Boundaries of Method Application
Scope determination involves defining the exact sample types, analytes, and conditions for which the method is suitable. The international standard ISO 16140 provides a structured model for understanding the different facets of scope [17].
The Interplay of Scopes in Method Verification
The relationship between the different scopes is hierarchical and logical, as visualized below:
Diagram 1: The relationship between validation and laboratory application scopes, adapting the model from ISO 16140-3 [17].
- Scope of Validation: This is the broad claim of a method's applicability, often defined by categories (e.g., "dairy products," "environmental samples"). A method validated for a "broad range of foods" based on testing in 5 of 15 defined food categories is expected to work for any sample within those 15 categories [17].
- Scope of the Method: This refers to the specific sample items (e.g., "whole milk," "hard cheese") that were actually tested during the validation study [17].
- Scope of Laboratory Application: This is the set of sample types that a specific laboratory needs to test routinely. The fitness-for-purpose evaluation must confirm that the method performs adequately for all items within this laboratory-defined scope [17].
The Concept of "Categories in the Food Chain"
ISO 16140-2 introduces a structured system of categories to manage scope. It defines a "category" as a group of sample types of the same origin (e.g., heat-processed milk and dairy products) [17]. This categorization is pivotal for scope determination because:
- Validation Efficiency: It is not feasible to test every possible sample type. Validation across a minimum of five different food categories allows a method to be considered validated for a "broad range of foods" [17].
- Informed Extrapolation: It provides a scientifically-grounded framework for laboratories to justify the extension of a method's application to a new sample type within a previously validated category, potentially reducing verification burdens.
Matrix Extension: Protocols for Incorporating New Sample Types
Matrix extension is the practical process of adding a new sample type to the method's scope. This requires experimental verification to demonstrate that the new matrix does not interfere with the method's performance.
Experimental Design for Matrix Extension
The verification study for a new matrix must evaluate the key analytical performance characteristics. The following table summarizes the experimental parameters for qualitative and semi-quantitative assays, drawing from CLIA guidelines and ISO standards [4].
Table 1: Experimental Design for Verifying Matrix Extension in Qualitative/Semi-Quantitative Assays
| Performance Characteristic | Minimum Sample Number & Type | Experimental Procedure & Calculations | Acceptance Criteria |
|---|---|---|---|
| Accuracy [4] | Minimum of 20 samples. Use a combination of positive and negative samples (for qualitative) or a range from high to low values (for semi-quantitative). | Test samples with the new method and a comparative method. Calculate as: (Number of results in agreement / Total number of results) × 100. | Meets manufacturer's stated claims or laboratory-defined criteria set by the Lab Director. |
| Precision [4] | Minimum of 2 positive and 2 negative samples tested in triplicate for 5 days by 2 operators. | Calculate the percentage of agreement between replicates across different runs, days, and operators. | Meets manufacturer's stated claims or laboratory-defined criteria set by the Lab Director. |
| Reportable Range [4] | Minimum of 3 samples. Use known positives or samples near the upper/lower cutoff values. | Verify that the results (e.g., "Detected," "Not detected," Ct value) fall within the established reportable range. | The laboratory confirms the result is reportable as defined in its procedures. |
| Reference Range [4] | Minimum of 20 isolates. Use de-identified clinical samples or reference materials representative of the new matrix. | Confirm the normal expected result for the patient population associated with the new matrix. | The expected result for a typical sample is confirmed. If the population differs, the reference range may need re-definition. |
Two-Stage Verification Process for Validated Methods
ISO 16140-3 formalizes the process for implementing a validated method in a new laboratory, which directly applies to matrix extension. This process occurs in two distinct stages [17]:
- Implementation Verification: The purpose is to demonstrate that the user laboratory can perform the method correctly. This is achieved by testing one of the exact same items (e.g., a specific sample type) that was evaluated in the original validation study. Successful replication of the expected result affirms the laboratory's technical competency with the method.
- Item Verification: This stage demonstrates that the method performs reliably for the specific, and potentially challenging, sample items that fall within the laboratory's own scope of application. This is where matrix extension is formally tested. The laboratory must test several of these new items and use defined performance characteristics to confirm the method's fitness-for-purpose for these new matrices [17].
The Scientist's Toolkit: Essential Reagents and Materials
A robust fitness-for-purpose evaluation relies on well-characterized and traceable materials. The following reagents and controls are non-negotiable for generating reliable data.
Table 2: Essential Research Reagent Solutions for Verification Studies
| Reagent / Material | Function in Fitness-for-Purpose Evaluation | Key Considerations |
|---|---|---|
| Quality Control (QC) Organisms [22] | To validate testing methodologies and monitor the ongoing performance of instruments, operators, and reagents. | Must be well-characterized microorganisms with defined profiles from recognized culture collections (e.g., ATCC). |
| Reference Materials [65] | To provide a traceable standard for ensuring the accuracy and precision of measurements, crucial for method comparison during matrix extension. | Includes materials like dehydrated pellets with known CFU counts for growth promotion testing or quantitative assays. |
| Pharmaceutical Grade Water [63] | As a solvent, diluent, and reagent in microbial testing procedures. | Must be of pharmaceutical grade and regularly tested for microbial contamination to prevent interference with results. |
| Validated Disinfectants [63] | To maintain a contamination-free environment during testing, which is critical for the integrity of results, especially in sterility testing and low-bioburden analyses. | A rotation of at least three disinfectants is recommended to prevent microbial resistance. Efficacy must be validated. |
Integrated Workflow for Evaluation
The entire process of fitness-for-purpose evaluation, from planning to final implementation, can be summarized in the following comprehensive workflow. This integrates the concepts of scope determination and matrix extension into a practical, step-by-step process.
Diagram 2: A unified workflow for conducting a fitness-for-purpose evaluation through matrix extension and scope determination.
Fitness-for-purpose evaluation is a systematic and evidence-driven discipline central to quality assurance in pharmaceutical and clinical microbiology. The processes of matrix extension and scope determination are not one-time events but are integral to the lifecycle of a method. By adhering to structured protocols from standards like ISO 16140, leveraging well-characterized reagents, and implementing a rigorous experimental design, laboratories can build a compelling, defensible case for the reliability of their methods. This ensures not only regulatory compliance but also the ultimate goal: the delivery of safe, high-quality products and accurate diagnostic information to protect patient health.
Within the framework of microbiological method verification study design, comparative method studies serve as the cornerstone for establishing the reliability and accuracy of new analytical procedures. These studies are designed to determine whether a new or alternative method (test method) produces results equivalent to those obtained by an established reference standard. The fundamental clinical question is one of substitution: can one measure a given analyte with either method and obtain the same results? [66] The resolution of discrepancies between methods and the selection of appropriate reference standards present significant methodological challenges that researchers must address through rigorous experimental design and statistical analysis.
In microbiology, this process is formally standardized in protocols such as the ISO 16140 series, which provides specific guidance for method validation and verification. [17] These standards acknowledge that before a method can be used in a laboratory, two stages are required: first, proving the method is fit for purpose (validation), and second, demonstrating the laboratory can properly perform the method (verification). [17] This technical guide examines the critical components of comparative method studies within this context, with particular emphasis on reference standard selection and discrepancy resolution protocols.
Reference Standard Selection and Categorization
The analytical method used for comparison must be carefully selected because the interpretation of experimental results depends on assumptions about the correctness of the comparative method. [67] Reference standards exist in a hierarchy of accuracy and establishment, each with distinct implications for study design and result interpretation.
Table 1: Categories of Reference Standards in Comparative Studies
| Category | Definition | Technical Requirements | Interpretation of Discrepancies |
|---|---|---|---|
| Definitive Method | A method that can determine the true value of a measurand with the highest accuracy possible [67] | Highest specificity; minimal systematic error; often based on fundamental physical/chemical principles | All differences attributed to the test method |
| Reference Method | A thoroughly investigated method showing consistently reliable results in comparison with definitive methods [67] | High quality documented through comparative studies with definitive methods and traceable reference materials | Differences typically attributed to the test method |
| Comparative Method | A method in routine use whose correctness has not been fully documented [67] | Standard laboratory procedures without established traceability | Differences must be carefully interpreted; source of error must be identified |
| Imperfect Reference Standard | A reference method with known, quantified error rates [68] | Known sensitivity and specificity determined through previous validation | Requires statistical correction methods; may produce biased estimates |
The choice of reference standard directly impacts how discrepancies are resolved. When a validated reference method is used, any differences observed are typically attributed to the test method. [67] However, when the comparative method is a routine laboratory method without established traceability, large and medically unacceptable differences require identification of which method is inaccurate. [67] In microbiology, the ISO 16140 series specifically addresses the validation of alternative (mostly proprietary) methods against reference methods, with the reference method serving as the benchmark for comparison. [17]
A particular challenge arises when dealing with imperfect reference standards, where neither method is error-free. In these cases, statistical correction methods such as those proposed by Staquet et al. and Brenner may be employed, though each has limitations under certain conditions. [68]
Experimental Design Considerations
Fundamental Design Parameters
Proper experimental design is essential for generating meaningful comparison data. Several critical parameters must be addressed to ensure the validity of the study conclusions.
Table 2: Key Experimental Design Parameters for Comparative Studies
| Parameter | Considerations | Recommendations |
|---|---|---|
| Sample Number | Precision of results; detection of clinically important differences | Minimum 40 patient specimens [67]; 20 clinically relevant isolates for microbiology verification [4] |
| Sample Selection | Representation of real-world conditions; analytical range | Cover entire working range of method; represent spectrum of diseases [67]; include 5+ food categories in microbiology [17] |
| Measurement Timing | Physiological changes in measurand; methodological interference | Simultaneous sampling where possible [66]; randomize order if sequential [66] |
| Replication | Identification of outliers; assessment of repeatability | Single measurements common; duplicates recommended for outlier detection [67] |
| Time Period | Incorporation of routine laboratory variability | Multiple runs over different days (minimum 5 days) [67] |
| Specimen Stability | Pre-analytical variables affecting results | Analyze within 2 hours of each other unless stability known [67] |
Specific Microbiology Considerations
In microbiological applications, comparative studies must account for matrix effects and category representation. The ISO 16140-2 standard defines 15 food categories, and validation of a method using 5 different categories qualifies it as validated for a "broad range of foods." [17] This principle of categorical representation extends to other microbiological matrices, including environmental samples, feed, and primary production samples. [17]
The design should also incorporate two stages of verification for validated methods: implementation verification (demonstrating the user laboratory can correctly perform the method) and item verification (demonstrating capability with challenging items within the laboratory's scope). [17]
Discrepancy Resolution Protocols
Data Analysis and Visualization Techniques
The initial phase of discrepancy resolution involves comprehensive data visualization to identify patterns and outliers. The most fundamental technique is graphical inspection of data, which should be performed as data is collected to identify discrepant results requiring immediate reanalysis. [67]
Bland-Altman Plot: This visualization method plots the difference between paired measurements (test method minus reference method) against the average of the two measurements. [66] The plot includes horizontal lines representing the mean difference (bias) and limits of agreement (mean difference ± 1.96 standard deviations of the differences). [66] This approach allows visual assessment of the relationship between the measurement magnitude and disagreement, helping identify systematic biases and outliers.
Comparison Plot: For methods not expected to show one-to-one agreement, a comparison plot with test results on the y-axis and reference results on the x-axis is more appropriate. [67] This visualization helps assess analytical range, linearity of response, and the general relationship between methods.
The following workflow diagram illustrates the systematic approach to discrepancy resolution in comparative method studies:
Statistical Approaches to Discrepancy Resolution
When discrepancies are identified, statistical methods provide objective criteria for resolution:
Bias and Precision Statistics: The mean difference between methods (bias) quantifies how much higher or lower values are with the test method compared to the reference. [66] The standard deviation of the differences measures variability, from which limits of agreement are determined (mean difference ± 1.96 SD). [66] These statistics help determine whether observed differences fall within clinically acceptable boundaries.
Linear Regression Analysis: For data covering a wide analytical range, linear regression statistics (slope, y-intercept, and standard error of the estimate) allow estimation of systematic error at multiple decision concentrations. [67] The systematic error at a given medical decision concentration (Xc) is calculated as SE = Yc - Xc, where Yc is the value predicted from the regression equation Y = a + bX. [67]
Correction Methods for Imperfect Reference Standards: When the reference standard has known error rates (sensitivity and specificity), correction methods can adjust for reference standard imperfection. The Staquet et al. method generally outperforms the Brenner method when the index test and reference standard are conditionally independent, though it may produce illogical results with very high or low disease prevalence. [68]
Method Verification in Microbiology
Verification of Validated Methods
Once a method has been validated through comparative studies, laboratories must still verify their ability to perform the method successfully. For microbiological methods, this process follows specific protocols outlined in standards such as ISO 16140-3. [17] Method verification demonstrates that a laboratory can satisfactorily perform a validated method before implementing it for routine testing. [4]
The verification process for unmodified FDA-approved tests in clinical microbiology laboratories requires assessment of accuracy, precision, reportable range, and reference range. [4] For qualitative assays in microbiology, accuracy verification typically involves testing a minimum of 20 clinically relevant isolates with a combination of positive and negative samples. [4]
Two-Stage Verification Protocol
The ISO 16140-3 standard specifies two distinct stages for verification of validated methods: [17]
Implementation Verification: The purpose is to demonstrate that the user laboratory can correctly perform the method. This is achieved by testing one of the same items evaluated in the validation study to confirm that the laboratory can obtain similar results.
Item Verification: This stage demonstrates that the user laboratory is capable of testing challenging items generally tested within the laboratory's scope. This involves testing several such items and using defined performance characteristics to confirm the method performs adequately.
The following diagram illustrates the relationship between different methodological assessments in the method evaluation lifecycle:
Essential Research Reagents and Materials
Table 3: Essential Research Reagent Solutions for Comparative Studies
| Reagent/Material | Function in Comparative Studies | Technical Specifications |
|---|---|---|
| Reference Strains | Quantification of method accuracy and specificity | Well-characterized strains from recognized collections (ATCC, NCTC) |
| Clinical Isolates | Assessment of method performance with diverse specimens | Minimum 20 isolates representing target organisms [4] |
| Selective Media | Method specificity confirmation and contamination control | Agar types specified in validation protocol [17] |
| Quality Controls | Monitoring of assay precision and reproducibility | Positive/negative controls for qualitative methods [4] |
| Proficiency Samples | Interlaboratory comparison and competency assessment | Blinded samples with established reference values |
| Buffer Systems | Maintenance of optimal physiological conditions | pH, concentration, and composition specified in method [69] |
Comparative method studies with robust discrepancy resolution protocols form an essential component of microbiological method verification frameworks. The selection of an appropriate reference standard—whether a definitive method, reference method, routine comparative method, or imperfect reference standard with known error characteristics—directly influences study design and the interpretation of discrepancies. Through systematic experimental design, appropriate statistical analysis, and adherence to established verification protocols, researchers can generate reliable evidence regarding method equivalence and implementation readiness. The ongoing development of standardized approaches, such as those in the ISO 16140 series, provides a critical foundation for ensuring the reliability of microbiological testing across laboratory settings.
Within microbiological method verification study design research, validation is a mandatory process that establishes the performance characteristics and reliability of an analytical method. This guide details the three core validation categories—Developmental, Internal, and Preliminary Validation—providing a structured framework for researchers, scientists, and drug development professionals. The objective is to deliver detailed experimental protocols and data presentation standards to ensure that methods are scientifically sound, fit for their intended purpose, and meet regulatory requirements.
Core Validation Categories
Developmental Validation
Developmental validation constitutes the initial, in-house assessment of a method's performance characteristics before it is deployed for routine use. It focuses on establishing foundational performance parameters.
- Objective: To thoroughly characterize the analytical method's performance under controlled, "in-house" conditions.
- Primary Focus: To demonstrate that the method is robust, reliable, and capable of producing accurate and precise results before it undergoes more extensive interlaboratory testing.
- Key Parameters: The process involves a rigorous assessment of specificity/selectivity, accuracy, precision, linearity, range, and robustness. The specific parameters validated depend on whether the method is qualitative or quantitative.
Table 1: Core Performance Parameters in Developmental Validation
| Parameter | Qualitative Method Focus | Quantitative Method Focus |
|---|---|---|
| Specificity/Selectivity | Ability to correctly identify target microorganisms in the presence of background flora. | Assurance that the signal measured is specific to the analyte and free from interference. |
| Accuracy | Agreement with a reference method for known positive/negative samples; reported as percent correct identification. | Closeness of agreement between the measured value and the true value; often assessed via spike-recovery studies. |
| Precision | Degree of agreement among repeated analyses from the same homogeneous sample under stipulated conditions. | Expressed as repeatability (within-lab, same day) and intermediate precision (within-lab, different days, analysts, equipment). |
| Linearity & Range | Not typically applicable. | The ability to obtain results directly proportional to analyte concentration within a given range. |
| Limit of Detection (LOD) | The lowest number of microorganisms that can be reliably detected. | The lowest amount of analyte that can be detected, but not necessarily quantified. |
| Limit of Quantification (LOQ) | Not applicable. | The lowest amount of analyte that can be quantitatively determined with acceptable precision and accuracy. |
| Robustness | Capacity to remain unaffected by small, deliberate variations in method parameters (e.g., incubation temperature, time). | Same as for qualitative methods. |
Internal Validation
Internal validation, also known as verification, is the process a laboratory undertakes to confirm that it can successfully implement a previously validated method within its own environment, using its own personnel and equipment.
- Objective: To verify that a method validated elsewhere (e.g., through a collaborative study) performs as expected in the user's specific laboratory.
- Primary Focus: To ensure the laboratory's competence and the reproducibility of the method locally, without the need for a full collaborative study.
- Key Activities: This includes testing a subset of the method's performance characteristics, such as accuracy and precision on known reference materials, confirming the LOD, and demonstrating specificity with typical sample matrices encountered by the laboratory. The International Standard ISO 16140-3:2021 provides a specific "Protocol for the verification of reference methods and validated alternative methods in a single laboratory" [70]. Similarly, NordVal International offers protocols for validating alternative microbiological methods that harmonize with the ISO 16140 series [71].
Preliminary Validation
Preliminary validation is a limited-scale study that provides initial, "proof-of-concept" data for a new method or a significant modification of an existing method. It is often a precursor to a full developmental validation.
- Objective: To gather initial evidence that a method is feasible and possesses the basic analytical characteristics worthy of a full developmental validation.
- Primary Focus: To assess the method's potential and identify any major shortcomings before committing extensive resources.
- Key Activities: This phase typically involves a smaller sample size, a narrower range of matrices, and a limited number of replicates. It may focus on key parameters like specificity against a small panel of target and non-target microorganisms, or initial estimates of LOD and accuracy.
Integrated Experimental Protocols
Protocol for a Quantitative Method Accuracy and Precision Study
This protocol outlines a methodology to generate data for the creation of an accuracy profile, a comprehensive graphical tool for assessing the validity of a quantitative measurement procedure [71].
- Sample Preparation: Select a blank matrix representative of the intended sample types (e.g., food homogenate). Spike the matrix with the target analyte (microorganism) at a minimum of 3 concentration levels covering the quantitative range (e.g., low, medium, high). The true concentration of the spiked analyte should be known or referenceable to a standard.
- Experimental Design: For each concentration level, analyze a minimum of 3 replicates per day over 3 different days, performed by at least 2 different analysts. This design allows for the calculation of both repeatability (within-day precision) and intermediate precision (between-day, between-analyst precision).
- Data Analysis:
- Calculate the recovery (%) for each individual measurement:
(Measured Concentration / True Concentration) * 100. - For each concentration level, calculate the mean recovery (accuracy) and the standard deviation and relative standard deviation (RSD%) of the recoveries (precision).
- Calculate the recovery (%) for each individual measurement:
- Data Presentation: The results from such a study are ideally summarized in a table and visualized using an accuracy profile, which plots the recovery (%) against the concentration level, including confidence intervals for the mean.
Table 2: Example Data from a Quantitative Accuracy and Precision Study
| Spike Level | True Concentration (CFU/mL) | Mean Recovery (%) | Repeatability RSD% | Intermediate Precision RSD% |
|---|---|---|---|---|
| Low | 1.0 x 10² | 95.5 | 5.2 | 8.1 |
| Medium | 1.0 x 10⁴ | 102.3 | 3.1 | 5.7 |
| High | 1.0 x 10⁶ | 98.7 | 2.5 | 4.3 |
Protocol for a Qualitative Method Relative Accuracy Study
This protocol, aligned with international standards, is designed to estimate the sensitivity and specificity of a qualitative alternative method compared to a reference method [71] [72].
- Sample Selection and Inoculation: Select a panel of naturally contaminated or artificially inoculated samples. The panel should include samples that are expected to yield positive results and negative results for the target microorganism. The number of samples must be sufficient for a statistically sound analysis.
- Testing Procedure: Test all samples in parallel using both the alternative method (the method under validation) and the prescribed reference method. The testing should be performed under "blind" conditions to avoid bias.
- Data Analysis - Contingency Table: The results are compiled into a 2x2 contingency table to calculate the key statistical parameters.
Table 3: Contingency Table for Qualitative Method Comparison
| Reference Method Positive | Reference Method Negative | Total | |
|---|---|---|---|
| Alternative Method Positive | a (True Positive) | b (False Positive) | a + b |
| Alternative Method Negative | c (False Negative) | d (True Negative) | c + d |
| Total | a + c | b + d | N |
- Relative Sensitivity = a / (a + c) * 100%
- Relative Specificity = d / (b + d) * 100%
- False Positive Rate = b / (b + d) * 100%
- False Negative Rate = c / (a + c) * 100%
It is critical to note that the design of this validation study (e.g., whether sampling is based on the results of the imperfect method, the gold standard, or at random) directly determines which bias parameters (sensitivity/specificity or predictive values) can be validly calculated [72].
Workflow and Data Presentation
Method Validation Pathway
The following workflow outlines the logical progression through the key stages of method validation, from initial feasibility assessment to ongoing verification.
Presenting Quantitative Validation Data
Effective presentation of quantitative data is crucial for interpreting and reporting validation studies. Frequency distribution tables and histograms are fundamental tools for this purpose.
- Frequency Tables: The first step in analyzing quantitative data is often tabulation. A well-designed frequency table should be numbered, have a clear title, and its data should be organized logically (e.g., by size or chronology) [73]. For quantitative data with a wide range, grouping data into class intervals is essential [74].
- Constructing Class Intervals:
- Calculate the range (highest value - lowest value).
- Divide the range into 5-16 equal subranges (class intervals). The number of intervals is a balance between detail and conciseness [73].
- Count the number of observations (frequency) within each interval.
- Histograms: A histogram is a graphical representation of a frequency distribution for quantitative data. It consists of contiguous rectangular bars where the width represents the class interval and the area of the bar represents the frequency [73] [74]. Unlike bar charts for categorical data, the horizontal axis is a continuous number line.
Table 4: Example Frequency Table for Quantitative Data (e.g., Bacterial Counts)
| Class Interval (CFU/mL) | Frequency | Relative Frequency (%) |
|---|---|---|
| 0 - 9.9 x 10³ | 4 | 13.3% |
| 1.0 x 10⁴ - 1.9 x 10⁴ | 14 | 46.7% |
| 2.0 x 10⁴ - 2.9 x 10⁴ | 8 | 26.7% |
| 3.0 x 10⁴ - 3.9 x 10⁴ | 3 | 10.0% |
| 4.0 x 10⁴ - 4.9 x 10⁴ | 1 | 3.3% |
| Total | 30 | 100% |
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and reagents used in the validation of microbiological methods.
Table 5: Key Research Reagents for Microbiological Method Validation
| Reagent/Material | Function in Validation |
|---|---|
| Certified Reference Materials (CRMs) | Provides a matrix with a known, certified concentration of the target analyte. Serves as the gold standard for determining accuracy in quantitative recovery studies and for calibrating equipment. |
| Selective and Non-Selective Growth Media | Used in reference methods for the cultivation, isolation, and enumeration of microorganisms. Critical for specificity studies to differentiate target from non-target organisms and for determining CFU in accuracy assessments. |
| Strain Panels (Type Cultures and Wild Isolates) | A characterized collection of target and non-target microorganisms. Essential for conducting specificity/selectivity studies to confirm the method correctly identifies the target and does not cross-react with related species or background flora. |
| Inactivation Reagents or Neutralizers | Used to stop antimicrobial activity at the end of specified contact times or to neutralize disinfectants in sample diluents. Crucial for robustness studies and for ensuring accurate recovery in viability-based methods. |
| Sample Matrices (e.g., food homogenates, buffers with interfering substances) | Representative samples of the intended test materials, including challenging matrices with high background flora or inherent antimicrobial properties. Used to assess the method's practical applicability, robustness, and freedom from matrix interference. |
The adoption of modern microbial methods (MMMs) represents a paradigm shift in pharmaceutical microbiology, offering enhanced sensitivity, reduced time-to-result, and continuous monitoring capabilities. Despite regulatory encouragement and demonstrated benefits, industry adoption remains challenging. This technical guide provides a comprehensive framework for the evaluation and implementation of MMMs, aligning with the fundamental principles of microbiological method verification study design. We present a structured roadmap encompassing initial technology assessment, regulatory compliance, validation protocols, and implementation strategies to support researchers, scientists, and drug development professionals in navigating this complex landscape.
Modern microbial methods, synonymous with alternative microbial methods and rapid microbial methods, utilize advanced technologies to supplement or replace traditional culture-based approaches. Regulatory agencies worldwide have encouraged their use through guidance documents including the 2004 PAT Guidance for Industry, Annex 1, USP <1223>, Eur. Ph. Chapter 5.1.6, and PDA Technical Report No. 33 [75]. These technologies provide considerable benefits including enhanced sensitivity, cost and time savings, and continuous monitoring support [76]. Regulatory emerging-technology programs such as the U.S. FDA Emerging Technology Team have been established specifically to support implementation of these advanced methods [75].
Despite these advantages and extensive regulatory guidance, adoption of modern microbial methods has been limited in recent years [75]. Challenges often arise during the initial evaluation and implementation process, frequently stemming from insufficiently comprehensive stakeholder involvement and unfamiliarity with validation requirements [76]. This guide addresses these challenges by providing a systematic approach to technology assessment, verification study design, and implementation strategy within the context of pharmaceutical drug development.
Initial Technology Assessment Roadmap
Strategic Alignment and Application Identification
The initial technology assessment begins with determining how a new method aligns with company goals and identifies specific applications that would benefit from modern technology [75]. Key considerations include:
- Project Objectives: Define specific goals the project team aims to achieve with the new technology [75]
- Application Selection: Identify whether rapid release testing for sterility or mycoplasma, in-process testing, raw material analysis, water testing, or continuous environmental monitoring would provide maximum value [75]
- Implementation Timing: Ideally begin strategy development during clinical trials to include the alternative method in the New Drug Application or Biologics License Application [75]
For facilities implementing new technologies, MMMs can increase quality confidence, provide data from facility commissioning, and support data-driven decision-making for process optimization [75]. These methods also serve as valuable tools for non-GMP investigations and validations before final application implementation.
Technical Considerations and Risk Assessment
A comprehensive technical assessment must evaluate technology maturity, intended use parameters, and comparative performance against traditional methods [75]. Critical considerations include:
- Technology Readiness: Assess whether the technology has only basic principles reported or has been adopted in different laboratory settings, which affects verification requirements [75]
- Performance Metrics: Evaluate time to result (hours versus days saved), false-positive/false-negative risks compared to existing methods, and detection sensitivity [75]
- Detection Capabilities: Understand the reporting unit (e.g., colony-forming equivalents vs. traditional CFU) and how sensitivity compares to current methods [75]
- Interference Potential: Determine if product matrices cause interference or background noise with the technology [75]
- Investigation Support: Address how the method handles microorganism identification during out-of-specification investigations, especially if destructive to microbes [75]
A formal risk assessment should document vulnerabilities associated with traditional methods versus modern alternatives, forming the basis for method development and validation work packages [75].
Table 1: Key Technical Considerations for Modern Microbial Method Selection
| Parameter | Evaluation Questions | Impact on Implementation |
|---|---|---|
| Technology Maturity | Has the technology been adopted for this application in other labs? | Determines extent of required verification studies |
| Time to Result | Is the technology continuous monitoring or providing discrete results? | Affects process control capabilities and investigation timelines |
| Detection Limit | What is the required limit of detection for the application? | Must demonstrate equivalency or superiority to current method |
| Sample Interference | Does the technology experience interference from the product matrix? | May require additional method development or sample preparation |
| Data Output | How does the technology report results compared to CFU? | Impacts data interpretation and investigation protocols |
Regulatory and Compliance Framework
Data Integrity Requirements
For GMP use, modern microbial methods must meet stringent data integrity requirements. All new instruments should meet these minimum acceptable parameters [75]:
- Support 21 CFR Part 11 compliance
- Create uneditable data records and activity logs
- Contain alarm matrices for capturing invalid occurrences
- Interface with company active directories and electronic data management systems
- Include configurable user permissions (minimum administrator and operator levels)
- Prevent data editing or deletion without quality-event record generation
- Export data and reports in readable formats compatible with company control policies
Developing a working relationship with instrument vendors is crucial for ensuring compliance. Vendors should provide resources to support qualification and integration with existing systems [75].
Validation and Verification Principles
Understanding the distinction between validation and verification is fundamental to successful implementation. Validation establishes that an assay works as intended for laboratory-developed methods or modified FDA-approved tests [4]. Verification demonstrates that an unmodified FDA-approved or cleared test performs according to established characteristics when used as intended by the manufacturer [4]. For microbial forensics, validation provides confidence that methods generate reliable and defensible results, with potential serious consequences if improperly performed [59].
The basic categories of validation include [59]:
- Developmental Validation: Acquisition of test data and determination of conditions and limitations for a newly developed method
- Internal Validation: Accumulation of test data within an operational laboratory demonstrating established methods perform within predetermined limits
- Preliminary Validation: Early evaluation of a method used to investigate a biocrime or bioterrorism event when fully validated methods aren't available
For clinical laboratories, verification studies for qualitative or semi-quantitative assays must address accuracy, precision, reportable range, and reference range [4].
Method Verification Study Design
Verification Experimental Design
Method verification studies are required by the Clinical Laboratory Improvement Amendments (CLIA) for non-waived systems before reporting patient results [4]. The verification plan must be documented and include [4]:
- Type of verification and purpose of study
- Test purpose and method description
- Study design details (sample types, replicates, analysts, days)
- Quality assurance and quality control protocols
- Performance characteristics and acceptance criteria
- Required materials, equipment, and resources
- Safety considerations and completion timeline
For qualitative and semi-quantitative assays (common in microbiology), specific verification approaches include [4]:
- Accuracy: Minimum 20 clinically relevant isolates (positive and negative), with agreement calculated as (number in agreement/total results) × 100
- Precision: Minimum 2 positive and 2 negative samples tested in triplicate for 5 days by 2 operators (operator variance may be excluded for fully automated systems)
- Reportable Range: Minimum 3 known positive samples verifying manufacturer-determined cutoff values
- Reference Range: Minimum 20 isolates representing the laboratory's patient population
Quantitative Method Verification
For quantitative molecular methods like Q-PCR and QRT-PCR, verification requires additional statistical considerations. Assay variability typically ranges from 0.2 to 0.5 log10 units, combining with biological variation to define the medical decision interval (MDI) [61]. The MDI represents the clinically significant change in microbial replication equal to the sum of biological variation and intra-assay imprecision [61].
Quantitative verification must include [61]:
- Standard Curves: Serial dilutions of known organism density or synthetic oligonucleotides amplified parallel to samples
- Calibrators: Substances used to adjust instrument readings relative to known standards
- Controls: Materials with known characteristics analyzed alongside test samples to monitor process performance
Precision for quantitative assays should be characterized using standard deviation multiples rather than percentage coefficient of variation alone, as %CV can be misleading across different microbial densities [61].
Table 2: Method Verification Requirements by Assay Type
| Performance Characteristic | Qualitative Assays | Quantitative Assays |
|---|---|---|
| Accuracy | 20+ clinical isolates, positive and negative | Method comparison and clinical utility studies |
| Precision | 2 positive/2 negative in triplicate over 5 days, 2 operators | Precision calculations using SD multiples, not just %CV |
| Reportable Range | 3+ known positive samples | Linear range demonstrating upper and lower quantification limits |
| Reference Range | 20+ isolates representing patient population | Established normal values for tested patient population |
| Statistical Analysis | Percentage agreement calculations | Linear regression, bias analysis, Bland-Altman plots |
Figure 1: Method Verification Study Design Workflow
Implementation Strategy and Cost Analysis
Cost of Ownership Considerations
A comprehensive cost analysis must evaluate both initial investments and long-term operational expenditures [75]. The total cost of ownership includes:
Initial (One-Time) Costs [75]:
- Instrument acquisition and supporting software/equipment
- Engineering or structural laboratory updates (HVAC, piping, construction)
- Validation packages (installation, operational, and performance qualification)
Long-Term (Recurring) Costs [75]:
- Maintenance plans with defined service levels and frequency
- System updates, upgrades, and replacement cycles
- Consumables and continued training expenses
- Regulatory submission support and license updates
Engaging procurement specialists early in the evaluation process enables competitive pricing negotiations, particularly when multiple sites are impacted [75]. Supplier agreements should demonstrate clear cost benefits as instrument and consumable volumes increase over time.
User Requirements Specification Development
A User Requirements Specification (URS) defines critical equipment-related components, variables, specifications, and options necessary to meet user needs for a specific application [77]. According to USP <1223>, a URS should include "all critical functions of the technology, critical user interface requirements, space requirements, environmental requirements, operational requirements and all other important characteristics of an alternative method for the intended use" [77].
The Modern Microbial Methods Collaboration has developed a technology-agnostic URS template that provides detailed requirement considerations while allowing customization based on end-user needs [77]. Key benefits of using a standardized URS template include [77]:
- Common language standardization for modern microbial method URS development
- Clear roles, responsibilities, and definitions
- Well-defined scope and intent to prevent scope creep
- Identification of prerequisites or stage gates
- Facilitation of new method adoption through a structured starting point
The URS should be developed in collaboration with instrument suppliers who can provide primary validation data and implementation recommendations [77].
Figure 2: Modern Microbial Methods Implementation Roadmap
Essential Research Reagents and Materials
Successful implementation of modern microbial methods requires specific reagents and materials to support validation and routine use. The selection of appropriate reagents is critical for generating reliable and reproducible results.
Table 3: Essential Research Reagent Solutions for Method Verification
| Reagent/Material | Function | Application Examples |
|---|---|---|
| Reference Strains | Verify method accuracy using well-characterized microorganisms | ATCC strains for challenge studies |
| Clinical Isolates | Assess method performance with relevant patient populations | 20+ isolates for verification studies [4] |
| Positive Controls | Monitor assay performance and detect inhibition | Known positive samples for reportable range [4] |
| Negative Controls | Establish baseline signals and specificity | Samples without target analytes [4] |
| Calibrators | Standardize instrument readings to reference values | Serial dilutions for quantitative curves [61] |
| Matrix Samples | Evaluate interference from sample components | Product-specific matrices for suitability testing |
| Culture Media | Support microbial growth for comparative studies | Traditional media for side-by-side testing [75] |
Implementing modern microbial methods requires a systematic approach from initial technology assessment through validation and routine use. The four-step evaluation roadmap—encompassing technology assessment, compliance risk evaluation, cost analysis, and overall instrument evaluation—provides a foundation for successful adoption [75]. Understanding the distinction between validation and verification is crucial, with specific study design requirements for qualitative versus quantitative methods [4].
Engaging cross-functional stakeholders early in the process, including quality assurance, regulatory, IT, and laboratory personnel, minimizes implementation challenges [75] [76]. Utilizing structured tools such as the URS template developed by the M3 Collaboration standardizes the evaluation process and ensures critical requirements are addressed [77]. As regulatory expectations evolve, particularly with the emphasis on contamination control strategies in EU GMP Annex 1, modern microbial methods offer enhanced capabilities for ensuring product safety and quality [78].
By following this comprehensive framework, researchers, scientists, and drug development professionals can successfully navigate the complexities of modern microbial method evaluation and implementation, ultimately enhancing microbiological control strategies while maintaining regulatory compliance.
Conclusion
A well-designed microbiological method verification study is fundamental to generating reliable, defensible data in both clinical and pharmaceutical settings. By mastering the distinctions between verification and validation, implementing structured protocols for core performance characteristics, and establishing robust troubleshooting protocols, laboratories can ensure regulatory compliance and test result integrity. Future directions will increasingly involve leveraging automated technologies to enhance reproducibility, navigating evolving international regulations like IVDR, and developing flexible verification strategies for novel methodologies like genomic identification and rapid microbial methods. A proactive, scientifically sound approach to verification forms the bedrock of quality in microbiological testing, ultimately supporting patient safety and product quality.
References
- 1. Method Validation vs Method Verification: Which is Better ... [https://www.labmanager.com/method-validation-vs-method-verification-which-is-better-for-use-in-laboratories-33982]
- 2. Difference Between Validation And Verification Of ... [https://gmpinsiders.com/method-validation-vs-verification/]
- 3. Q2(R2) Validation of Analytical Procedures March 2024 [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/q2r2-validation-analytical-procedures]
- 4. Planning a Method Verification Study in Clinical ... [https://asm.org/articles/2022/january/planning-a-method-verification-study-in-clinical-m]
- 5. Food Safety Testing: Understanding Microbiological ... [https://www.eurofinsus.com/food-testing/resources/food-safety-testing-understanding-microbiological-method-validation-verification-and-fitness-for-purpose/]
- 6. A rapid microbiological method case study for advanced ... [https://www.europeanpharmaceuticalreview.com/article/261548/a-rapid-microbiological-method-case-study-for-advanced-therapy-medicinal-products/]
- 7. USA CLIA Standards vs. International ISO 15189 Standards [https://www.linkedin.com/pulse/comparing-quality-management-usa-clia-standards-vs-international-yf26e]
- 8. ISO 15189: Definition, Requirements, Implementation, and ... [https://simplerqms.com/iso-15189/]
- 9. Insights on updated accreditation guidelines ISO 15189:2022 [https://diagnostics.roche.com/global/en/article-listing/lab-leaders/article/iso-15189-updated-accreditation-guidelines.html]
- 10. New Regulations - Public Health - European Commission [https://health.ec.europa.eu/medical-devices-sector/new-regulations_en]
- 11. Mastering IVDR in 2025: Challenges and Strategies Across ... [https://www.ul.com/resources/mastering-ivdr-2025-challenges-and-strategies-across-full-compliance-spectrum]
- 12. 2025 Great Global QC Survey: ISO and CLIA labs [https://www.westgard.com/qc-applications/basic-qc-practices/2025-qc-survey-iso-vs-clia.html]
- 13. 2025 CLIA Acceptance Limits for Proficiency Testing [https://www.westgard.com/clia-a-quality/quality-requirements/2024-clia-requirements.html]
- 14. CMS Enacts New CLIA Regulations Effective January 2025 [https://www.bakerdonelson.com/cms-enacts-new-clia-regulations-effective-january-2025]
- 15. Method Validation/Verification: How Important is it in Your ... [https://www.americanpharmaceuticalreview.com/Featured-Articles/597641-Method-Validation-Verification-How-Important-is-it-in-Your-QC-Microbiology-Laboratory/]
- 16. Analytical Method Validation, Verification or Qualification [https://www.lachmanconsultants.com/2022/12/analytical-method-validation-verification-or-qualification-what-to-use-and-when/]
- 17. Method validation and method verification - Introduction - ISO [https://committee.iso.org/sites/tc34sc9/home/essential-information/content-left-area/validation-of-methods/method-validation-and-method-ver.html]
- 18. Semi-quantitative procedures; half professional or ... [https://myadlm.org/science-and-research/scientific-shorts/2023/semi-quantitative-procedures-half-professional-or-half-amateur-what-is-the-other-half]
- 19. Evaluation of analytical performance of qualitative and ... [https://www.sciencedirect.com/science/article/abs/pii/S0009898119319552]
- 20. Qualitative, Semi-quantitative, and ... [https://www.genengnews.com/resources/qualitative-semi-quantitative-and-quantitative-immunodiagnostics-for-covid-19/]
- 21. Methods for Analytical Validation of Novel Digital Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12622859/]
- 22. Mastering Quality: New Method Validation, QC Standards, PT [https://www.rapidmicrobiology.com/news/mastering-quality-new-method-validation-qc-standards-and-pt-a-rapidmicrobiology-special-focus]
- 23. AOAC & MicroVal Method Validation Training [https://microval.org/2025/09/02/aoac-microval-method-validation-training-microbial-method-validation-detailed-insights/]
- 24. Planning a Method Verification Study in Clinical ... [https://asm.org/articles/2022/january/planning-a-method-verification-study-in-clinical-m?sr_id=23df675c-421d-4816-a54e-4d751ba62574&sr_pos=3]
- 25. 10 Critical Validation Parameters For Microbiological ... [https://www.outsourcedpharma.com/doc/critical-validation-parameters-for-microbiological-experiments-0001]
- 26. Navigating method evaluation in clinical laboratories [https://myadlm.org/cln/articles/2024/mayjune/navigating-method-evaluation-in-clinical-laboratories]
- 27. Practical Guidance for Clinical Microbiology Laboratories [https://pmc.ncbi.nlm.nih.gov/articles/PMC6056841/]
- 28. How to verify and validate a clinical microbiology test ... [https://www.sciencedirect.com/science/article/pii/S1198743X24003094]
- 29. Validation of Laboratory-Developed Molecular Assays for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2901657/]
- 30. Validation of Microbiological Tests [https://www.biopharminternational.com/view/validation-microbiological-tests]
- 31. How to Present Quantitative & Qualitative Data in Reports [https://www.clearpointstrategy.com/blog/qualitative-and-quantitative-data]
- 32. Presenting data in tables and charts - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4008059/]
- 33. 4 Common Errors Associated with Manual QC Testing [https://www.rapidmicrobio.com/learning-center/rapid-blog/4-common-errors-microbiologists-make-when-using-the-manual-method]
- 34. Avoid Common Bacteriological Incubators Errors [https://www.igenels.com/how-to-identify-and-avoid-common-errors-in-using-bacteriological-incubators/]
- 35. How Contamination Happens in Labs (and How to Prevent It) [https://www.msesupplies.com/blogs/news/how-contamination-happens-in-labs-and-how-to-prevent-it?srsltid=AfmBOoqBPu9cvdG4ivZ9Q6-aqds3mvRFJ4GQe704CsTJUx6kvt1bmp08]
- 36. Microbial Analysis mistakes Archives [https://metalchem.com/tag/microbial-analysis-mistakes/]
- 37. A Guide to USP <1223> and Validation of Rapid Methods [https://www.americanpharmaceuticalreview.com/Featured-Articles/613587-Validating-Alternative-Microbiological-Methods-A-Guide-to-USP-1223-and-Validation-of-Rapid-Methods/]
- 38. Taxonomy based performance metrics for evaluating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6561758/]
- 39. ICH Q2(R2) Validation of analytical procedures [https://www.ema.europa.eu/en/ich-q2r2-validation-analytical-procedures-scientific-guideline]
- 40. Use of microbial data for hazard analysis and critical ... [https://pubmed.ncbi.nlm.nih.gov/10852577/]
- 41. A semi-automated validation framework for citizen science ... [https://www.sciencedirect.com/science/article/pii/S1574954125002997]
- 42. Why Data Quality Will Be One of the Most Critical Topics ... [https://www.unicage.eu/post/why-data-quality-will-be-one-of-the-most-critical-topics-of-2025]
- 43. Data Management Trends in 2025: A Foundation for ... [https://www.dataversity.net/articles/data-management-trends-in-2025-a-foundation-for-efficiency/]
- 44. Method Validation - an overview [https://www.sciencedirect.com/topics/engineering/method-validation]
- 45. Analytical Method Validation: Back to Basics, Part I [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-i]
- 46. and Corrective (CAPA): The Definitive Guide ( Preventive ) Action 2025 [https://www.thefdagroup.com/blog/definitive-guide-to-capa]
- 47. And Corrective (CAPA) Plan In GMP | GMP Insiders Prevention Action [https://gmpinsiders.com/corrective-and-prevention-action-capa/]
- 48. Stop These Dangerous CAPA Documentation Mistakes ... [https://pharmuni.com/2025/07/16/stop-these-dangerous-capa-documentation-mistakes-now/]
- 49. CAPA Implementation Tools in the Pharma Industry (2025 ... [https://www.linkedin.com/pulse/capa-implementation-tools-pharma-industry-2025-guide-pharcell-abz2f]
- 50. Corrective and Preventive Actions (CAPA) [https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/inspection-guides/corrective-and-preventive-actions-capa]
- 51. Automation in Pharma Validation [https://zamann-pharma.com/glossary/automation-in-pharma-validation/]
- 52. Automated medication verification system (AMVS) [https://pmc.ncbi.nlm.nih.gov/articles/PMC11089321/]
- 53. Choosing Between Human-in-the-Loop and Fully ... [https://medium.com/@webelightsolutions/choosing-between-human-in-the-loop-and-fully-autonomous-workflow-automation-in-2025-d592242a7b2d]
- 54. Enterprise Workflow Automation: What It Is and Why It's ... [https://www.iotforall.com/enterprise-workflow-automation-2025]
- 55. Artificial Intelligence for Drug Development [https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/artificial-intelligence-drug-development]
- 56. <61> Microbial Enumeration Tests [https://www.usp.org/harmonization-standards/pdg/general-methods/microbial-enumeration]
- 57. Laboratory Developed Tests [https://www.fda.gov/medical-devices/in-vitro-diagnostics/laboratory-developed-tests]
- 58. FDA's Laboratory-Developed Test Rule Struck Down in ... [https://www.sidley.com/en/insights/newsupdates/2025/04/fdas-laboratory-developed-tests-ldt-rule-struck-down-in-major-test-of-loper-bright]
- 59. Criteria for Validation of Methods in Microbial Forensics [https://pmc.ncbi.nlm.nih.gov/articles/PMC2547046/]
- 60. Laboratory Developed Tests | Areas of Focus [https://clsi.org/standards-development/specialty-areas/laboratory-developed-tests/]
- 61. Statistics for Method Verification of Quantitative Assays in ... [https://www.sciencedirect.com/science/article/abs/pii/S0196439919300455]
- 62. Modification of antimicrobial susceptibility testing methods [https://pubmed.ncbi.nlm.nih.gov/40971802/]
- 63. Best Practices in Pharmaceutical Microbiology Laboratory [https://www.pharmaguideline.com/2025/04/best-practices-in-microbiology-lab.html]
- 64. All you need to know about equipment validation for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12421869/]
- 65. New USP and Growth Promotion Testing EZ-Accu Shot™ [https://www.rapidmicrobiology.com/news/navigating-the-new-usp-and-growth-promotion-testing-with-ez-accu-shot]
- 66. Design, Analysis and Interpretation of Method-Comparison ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2944826/]
- 67. The Comparison of Methods Experiment [https://www.westgard.com/lessons/basic-method-validation/lesson23.html]
- 68. Comparative diagnostic accuracy studies with an imperfect ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8040223/]
- 69. Method Validation and Robustness [https://www.chromatographyonline.com/view/method-validation-and-robustness]
- 70. of the food chain — Microbiology — Part... Method validation [https://www.iso.org/standard/88181.html]
- 71. - NMKL Validation protocols [https://www.nmkl.org/nordval-international/apply-for-certificate/nordval-validation-protocol/]
- 72. Common misconceptions about validation studies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7750925/]
- 73. Presentation of Quantitative Data [https://ihatepsm.com/blog/presentation-quantitative-data]
- 74. Presenting Quantitative Data Graphically [https://courses.lumenlearning.com/waymakermath4libarts/chapter/presenting-quantitative-data-graphically/]
- 75. Initial Evaluation Roadmap for Modern Microbial Methods [https://www.pda.org/pda-letter-portal/home/full-article/initial-evaluation-roadmap-for-modern-microbial-methods]
- 76. BioPhorum's modern microbial methods evaluation roadmap [https://www.biophorum.com/news/why-biophorums-modern-microbial-methods-evaluation-roadmap-is-a-foundation-for-success/]
- 77. Facilitating Adoption of Modern Microbial Methods [https://www.pda.org/pda-letter-portal/home/full-article/facilitating-adoption-of-modern-microbial-methods]
- 78. How modern microbial methods can support a ... [https://www.biophorum.com/news/how-modern-microbial-methods-can-support-a-contamination-control-strategy/]