Biochemical Tests for Microbial Identification: Methods, Applications, and Best Practices for Biomedical Research
This article provides a comprehensive examination of microbial identification through biochemical profiling, tailored for researchers, scientists, and drug development professionals.
Biochemical Tests for Microbial Identification: Methods, Applications, and Best Practices for Biomedical Research
Abstract
This article provides a comprehensive examination of microbial identification through biochemical profiling, tailored for researchers, scientists, and drug development professionals. It explores the foundational principles of enzymatic and metabolic characterization, details traditional and modern automated methodologies, and offers practical guidance for troubleshooting common issues. The scope extends to method validation according to regulatory standards and a comparative analysis with genotypic and proteomic techniques, delivering a complete resource for the accurate application of these tests in pharmaceutical, clinical, and biomedical research settings.
The Science of Biochemical Profiling: Core Principles for Microbial Identification
The rapid and accurate identification of bacterial pathogens is a cornerstone of clinical microbiology, infectious disease treatment, and pharmaceutical development [1]. For nearly 150 years, microbial identification has relied on biochemical characterization through phenotypic methods [1]. While techniques such as MALDI-TOF MS and molecular assays have accelerated this process, they often lack the functional insights provided by enzymatic activity profiling [2] [1].
The emerging approach of using enzymatic profiles as bacterial fingerprints leverages the fundamental principle that each bacterial species possesses a unique enzymatic profile that drives its specific metabolic needs and capabilities [3]. This application note explores how profiling these enzymatic activities provides not only identification but also functional characterization of bacterial isolates, offering a powerful tool for researchers and drug development professionals working within the broader context of microbial identification using biochemical tests.
Background: The Evolution of Bacterial Identification
The journey of microbial identification began with traditional biochemical methods that relied on Gram staining, microscopic morphology, and biochemical characterization, requiring 2-5 days for completion [1]. The late 1960s saw the introduction of miniaturized identification systems like the API system, which preselected biochemical tests for different organism groups [1]. Subsequent automation through systems such as VITEK 2, BD Phoenix, and MicroScan further reduced identification times to under 24 hours for common pathogens [1].
Modern methodologies have since evolved to include:
- MALDI-TOF MS: Provides identification within minutes by analyzing protein profiles from pure colonies [1]
- Molecular assays: Detect genetic components directly from patient samples in approximately 1 hour [1]
- NMR metabolomics: Investigates metabolic responses to antibiotic treatments [4]
Despite these advances, there remains a critical need for methods that provide functional insights into bacterial metabolism while maintaining rapid turnaround times [2]. Enzymatic activity profiling addresses this gap by combining the speed of modern techniques with the metabolic relevance of traditional biochemical approaches.
Enzymatic Profiling: Principles and Applications
Fundamental Biochemical Principles
Bacterial identification through enzymatic profiling is predicated on the fact that bacteria produce large volumes of enzymes, and each species has a distinct enzymatic profile that can be used for classification [3]. These enzymes catalyze specific biochemical reactions that fulfill the unique metabolic requirements of different bacterial species [3].
The presence or absence of specific enzymes such as catalase, gelatinase, oxidase, and urease serves as a taxonomic fingerprint for bacterial identification [3]. For instance, catalase testing distinguishes Staphylococci (catalase-positive) from Streptococcus (catalase-negative), while oxidase testing identifies bacteria with cytochrome c oxidase activity [3].
Analytical Approaches
Recent advances have introduced innovative methods for enzymatic activity profiling:
Chemiluminescent Probe Arrays
Ultrasensitive arrays of chemiluminescent probes represent a breakthrough in enzymatic profiling technology [2]. This approach utilizes highly sensitive and enzyme-selective chemiluminescent probes designed to rapidly detect various bacterial enzymatic activities under physiological conditions [2]. The technology can deliver results within 90 minutes and includes specialized probes for detecting resistance to β-lactam antibiotics [2].
NMR Metabolomics
Nuclear Magnetic Resonance (NMR) spectroscopy provides complementary information through intracellular fingerprint and extracellular footprint analysis [4]. This method can distinguish antibiotics with different mechanisms of action based on their distinct metabolic profiles and has been successfully used to predict the mode of action of unknown antibiotics [4].
Table 1: Comparison of Bacterial Identification Methods
| Method | Time Required | Key Principle | Advantages | Limitations |
|---|---|---|---|---|
| Traditional Biochemical Tests | 2-5 days [1] | Enzyme detection via substrate utilization [3] | Low cost; well-established | Slow; limited to common pathogens |
| Automated Biochemical Systems | 4-24 hours [1] | Multi-test biochemical reaction panels [1] | High throughput; simultaneous ID & AST | Database-dependent; difficulty with unusual organisms |
| MALDI-TOF MS | Minutes [1] | Protein profile analysis [1] | Extremely fast; low per-test cost | Requires pure culture; limited strain typing |
| Molecular Methods | ~1 hour [1] | Genetic target detection [1] | Direct from samples; high sensitivity | Limited functional information |
| Enzymatic Profiling (Chemiluminescent) | 90 minutes [2] | Enzyme activity via chemiluminescent probes [2] | Functional insight; detects resistance mechanisms | Emerging technology; limited clinical validation |
| NMR Metabolomics | Hours [4] | Metabolic fingerprint/footprint analysis [4] | Mechanism of action prediction; comprehensive profiling | Specialized equipment needed; complex data analysis |
Experimental Protocols
Protocol 1: Enzymatic Profiling Using Chemiluminescent Probe Arrays
Principle
This method utilizes an array of enzyme-selective chemiluminescent probes that emit light under physiological conditions when reacted with specific bacterial enzymes, creating unique enzymatic fingerprints for bacterial classification [2].
Materials
- Bacterial isolates (pure cultures)
- Array of chemiluminescent probes (enzyme-selective)
- Luminometer or chemiluminescence detection system
- Physiological buffer (pH 7.0-7.4)
- Sterile tubes or microplates
- Incubator (35-37°C)
Procedure
- Sample Preparation: Grow bacterial isolates to mid-log phase (approximately 10^8 CFU/mL) in appropriate medium.
- Probe Preparation: Prepare fresh working solutions of chemiluminescent probes according to manufacturer specifications.
- Reaction Setup: Aliquot 100 μL of bacterial suspension into reaction wells. Add 50 μL of each chemiluminescent probe to separate wells. Include appropriate controls (negative control: no bacteria; positive control: known reference strain).
- Incubation: Incubate the reaction mixture at 35-37°C for 60-75 minutes.
- Signal Detection: Measure chemiluminescence using a luminometer or appropriate detection system.
- Data Analysis: Compile luminescence values across all probes to generate enzymatic activity profiles. Compare profiles to reference database for identification.
Technical Notes
- Optimal bacterial concentration is critical: too dilute may yield weak signals; too concentrated may cause probe saturation.
- Include β-lactamase activity probes to simultaneously assess antibiotic resistance profiles [2].
- The complete process from sample preparation to identification requires approximately 90 minutes [2].
Protocol 2: NMR-Based Metabolic Fingerprinting
Principle
This approach uses quantitative 1H NMR spectroscopy to study the metabolic response of bacterial cultures to different conditions, providing both intracellular metabolic fingerprints and extracellular metabolic footprints [4].
Materials
- Bacterial cultures in defined minimal medium
- NMR spectrometer (400 MHz or higher)
- D2O for field frequency locking
- NMR buffer (e.g., phosphate buffer in D2O, pH 7.4)
- 5-mm NMR tubes
- Centrifuge and filtration devices for sample preparation
Procedure
- Culture Conditions: Grow Escherichia coli or other target bacteria to OD600 of 0.6 in defined minimal medium.
- Antibiotic Exposure: Treat cultures with antibiotics (100 μM concentration) or solvents as controls for 30 minutes [4].
- Sample Preparation:
- Intracellular Fingerprints: Harvest cells by rapid centrifugation. Extract metabolites using appropriate extraction solvent (e.g., methanol:water:chloroform). Concentrate and resuspend in NMR buffer.
- Extracellular Footprints: Filter culture medium through appropriate molecular weight cut-off filters. Mix supernatant with NMR buffer.
- NMR Analysis: Transfer samples to NMR tubes. Acquire 1H NMR spectra using appropriate parameters (water suppression, sufficient scans for signal-to-noise).
- Data Processing: Process spectra (Fourier transformation, phasing, baseline correction). Segment spectra into bins for multivariate analysis.
- Pattern Recognition: Use Partial Least Squares Discriminant Analysis (PLS-DA) or similar multivariate statistical methods to identify metabolic patterns characteristic of different antibiotic classes or bacterial strains [4].
Technical Notes
- Defined minimal medium is essential to limit overlapping signals in NMR spectra [4].
- DMSO as a solvent should be avoided as it significantly alters metabolic profiles even at 1% concentration [4].
- This method can correctly predict the mode of action of antibiotics based on metabolic fingerprints [4].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagent Solutions for Enzymatic Profiling
| Reagent/Equipment | Function | Application Notes |
|---|---|---|
| Chemiluminescent Probe Array | Detection of specific enzymatic activities [2] | Includes probes for β-lactamase activity; highly sensitive under physiological conditions |
| Defined Minimal Medium | Support bacterial growth without interfering with analysis [4] | Essential for NMR metabolomics to limit overlapping signals in spectra |
| Luminometer/Chemiluminescence Detector | Measurement of light emission from enzymatic reactions [2] | Requires sensitivity for low-light detection; plate readers enable high-throughput |
| NMR Spectrometer | Quantitative analysis of metabolic profiles [4] | 400 MHz or higher recommended for sufficient resolution in complex mixtures |
| Matrix for MALDI-TOF MS | Protein ionization and analysis [1] | α-cyano-4-hydroxycinnamic acid commonly used for microbial identification |
| API Biochemical Test Strips | Multi-test biochemical identification [1] | Traditional method; useful for validation and smaller laboratories |
| Chromogenic Enzyme Substrates | Visual detection of specific enzyme activities [3] | Provide colorimetric alternatives to chemiluminescent detection |
Workflow and Data Interpretation
Experimental Workflow
The following diagram illustrates the integrated workflow for bacterial identification through enzymatic and metabolic profiling:
Data Analysis and Interpretation
The analysis of enzymatic profiling data involves both quantitative assessment of individual enzyme activities and pattern recognition across multiple enzymatic activities:
Chemiluminescent Data Analysis:
- Normalize raw luminescence values against positive and negative controls
- Create enzymatic activity heat maps for visual comparison
- Apply multivariate statistical analysis (PCA, PLS-DA) to identify clustering patterns
- Compare unknown profiles to reference databases for identification
NMR Metabolomic Data Analysis:
- Identify and quantify metabolites through spectral analysis
- Analyze both intracellular fingerprints and extracellular footprints
- Use statistical models to predict antibiotic mechanism of action
- Validate models through cross-validation and independent test sets
Enzymatic profiling represents a powerful approach to bacterial identification that links metabolic function to microbial identity. The methods described herein—from traditional biochemical tests to innovative chemiluminescent arrays and NMR metabolomics—provide researchers with a diverse toolkit for comprehensive bacterial characterization.
These approaches offer significant advantages over identification-only methods by providing functional insights into bacterial metabolism, detecting antibiotic resistance mechanisms, and enabling prediction of antibiotic mode of action. As the field advances, integration of these enzymatic profiling techniques with established identification methods will enhance our ability to rapidly characterize bacterial pathogens in clinical, industrial, and research settings.
For researchers engaged in microbial identification and drug development, enzymatic activity profiling provides a critical bridge between genotypic identification and phenotypic characterization, ultimately supporting more informed decisions in both therapeutic intervention and antibiotic discovery.
The identification of microorganisms through their biochemical characteristics has been a cornerstone of microbiology for over a century. This field has undergone a profound evolution, moving from the use of simple agar-based media in Petri dishes to sophisticated, miniaturized kits that provide rapid, accurate identification. This progression has been driven by the dual needs to increase efficiency in clinical diagnostics and to cater to the specificity required for the growth of fastidious microorganisms. The journey began with foundational developments in solid culture media by Fannie Hesse and Richard Petri in the 1880s, which allowed for the isolation of pure cultures and the systematic study of microbial physiology [1]. For decades, identification relied on laborious tube-based biochemical tests and macroscopic colony characterization [5] [1]. A significant leap forward occurred in the late 1960s with the introduction of miniaturized, multi-test identification kits, which represented a paradigm shift towards standardization and efficiency [1]. This evolution has culminated in today's fully automated systems that integrate identification and antimicrobial susceptibility testing, fundamentally shaping the workflows of clinical microbiology laboratories and drug development research [1].
The Era of Agar-Based Media and Fundamental Biochemical Tests
The initial phase of microbial identification was wholly dependent on the cultivation of microbes on various agar media, a technique made possible by the pioneering work of Angelina Hesse [5]. The physical appearance of microbial colonies—their color, texture, and morphology—provided the first clues to their identity [5].
Selective and Differential Media
The development of selective and differential media was a critical innovation that allowed microbiologists to begin distinguishing between bacterial species based on their metabolic capabilities and resistances.
- Selective Media contain substances that inhibit the growth of certain organisms while permitting the growth of others. A classic example is Mannitol Salt Agar (MSA), whose high salt concentration selects for Staphylococcus species while inhibiting most other bacteria [5].
- Differential Media allow multiple bacterial species to grow but contain indicators that reveal differences in their metabolism. Blood Agar is a widely used differential medium that distinguishes between Streptococcus species based on their type of hemolysis (alpha, beta, or gamma) [5].
- Combination Media integrate both principles. MacConkey Agar, for instance, is both selective (containing bile salts and crystal violet to inhibit Gram-positive bacteria) and differential (containing neutral red to differentiate lactose fermenters from non-fermenters) [5].
Table 1: Key Historical Agar Media for Microbial Identification
| Media Name | Type | Key Components | Primary Function in Identification |
|---|---|---|---|
| Mannitol Salt Agar (MSA) | Selective & Differential | High Salt, Mannitol, Phenol Red | Selects for Staphylococcus; differentiates S. aureus (mannitol fermenter) from S. epidermidis (non-fermenter) [5]. |
| Blood Agar | Differential | Sheep or Horse Blood | Differentiates species based on hemolysis patterns (e.g., S. pyogenes shows beta-hemolysis) [5]. |
| MacConkey Agar | Selective & Differential | Bile Salts, Crystal Violet, Lactose, Neutral Red | Selects for Gram-negative enteric bacteria; differentiates lactose fermenters (pink colonies) from non-fermenters [5]. |
Key Biochemical Tests and the Dichotomous Key
The macroscopic observation of growth on agar media was supplemented by simple, rapid biochemical tests performed on pure cultures. These tests provided definitive data for microbial identification and were often arranged into dichotomous keys to guide microbiologists [1].
- Catalase Test: This test distinguishes between catalase-positive Staphylococci (bubbles form) and catalase-negative Streptococci (no bubbles) when hydrogen peroxide is added to a bacterial smear [5] [1].
- Coagulase Test: Used to differentiate the pathogenic Staphylococcus aureus (coagulase-positive) from other, typically non-pathogenic, staphylococci [1].
- Oxidase Test: Identifies bacteria that produce cytochrome c oxidase, a key test for distinguishing Pseudomonas (positive) from members of the Enterobacteriaceae family (negative) [1].
- Indole Test: Detects the ability of a bacterium to produce indole from tryptophan, a critical test for identifying Escherichia coli (positive) [1].
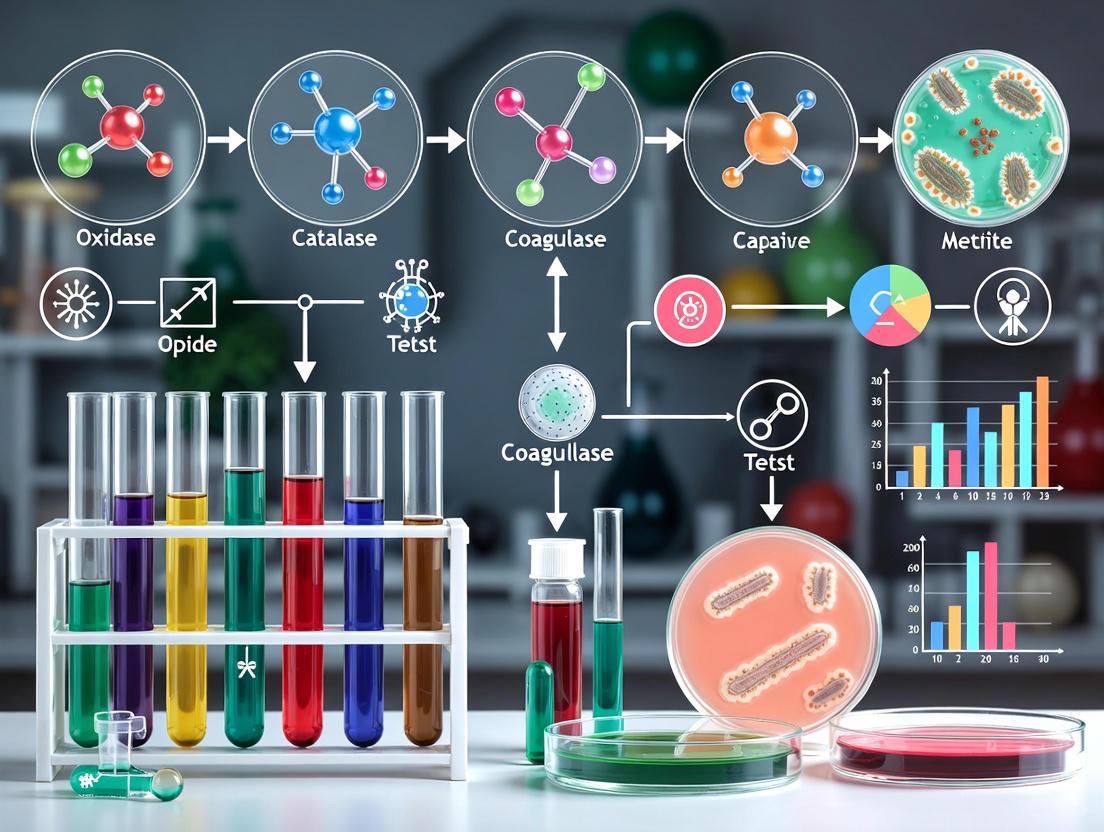
The following workflow illustrates the traditional, agar-based identification pathway for a common clinical sample, relying on sequential biochemical testing.
Traditional Biochemical Identification Workflow
The Revolution of Miniaturization and Automation
The limitations of the traditional approach—being labor-intensive, time-consuming, and requiring large amounts of space and media—drove the development of miniaturized and automated systems.
The Advent of Miniaturized Kits
The first major step towards miniaturization was the introduction of commercial kits like the API (Analytical Profile Index) system by bioMérieux [1]. These systems featured plastic strips with multiple micro-wells, each containing lyophilized substrates for different biochemical tests. A single bacterial colony could be suspended in a saline solution and used to inoculate all wells simultaneously, drastically reducing the time and materials required for setup [1]. This innovation allowed laboratories to generate a biochemical profile of an unknown organism quickly, which could then be referenced against a database for identification.
Fully Automated Identification Systems
The next evolutionary step was the integration of these miniaturized kits with automation and sophisticated data analysis software. Systems such as the VITEK 2 (bioMérieux), BD Phoenix, and Beckman Coulter MicroScan became the new standards in clinical laboratories [1]. These platforms use identification cards or panels with a comprehensive battery of biochemical substrates. The entire process—inoculation, incubation, and periodic reading of reactions—is automated. Advanced algorithms interpret the reaction patterns, often providing a species-level identification in as little as 4 to 18 hours, a significant improvement over the 2-5 days required by traditional methods [1].
Table 2: Evolution from Traditional to Automated Biochemical Identification
| Parameter | Traditional Tube-Based Methods | Miniaturized Kits (e.g., API) | Automated Systems (e.g., VITEK 2) |
|---|---|---|---|
| Time to Identification | 2–5 days [1] | 18–48 hours | 4–18 hours [1] |
| Throughput | Low | Medium | High [1] |
| Degree of Automation | Fully manual | Manual inoculation, manual/visual interpretation | Fully automated (inoculation, incubation, reading) [1] |
| Data Integration | Manual interpretation and recording | Manual code entry into database | Automated analysis and database matching [1] |
| Key Advantage | Low cost per test; fundamental for teaching | Standardization; wide database of profiles | Speed, high throughput, reproducibility, simultaneous ID & AST [1] |
Experimental Protocols
Protocol: Biochemical Identification Using a Miniaturized Kit (API 20E Example)
The following protocol outlines the standard procedure for identifying members of the Enterobacteriaceae family using a classic miniaturized kit.
I. Principle: The API 20E strip consists of 20 microtubes containing dehydrated biochemical substrates. When a bacterial suspension is added, the metabolites produced during incubation alter the medium, causing color changes that are either spontaneous or revealed by the addition of reagents. The combination of reactions generates a numerical profile used for database identification [1].
II. Materials:
- API 20E test strip and incubation box.
- Bacterial colony from a pure, 18-24 hour culture.
- Sterile saline solution (0.85% NaCl).
- McFarland standard (0.5) or turbidity meter.
- Pipettes and sterile tips.
- Reagents for test development (e.g., Kovac's for Indole, Barritt's for Voges-Proskauer).
III. Procedure:
- Preparation of Inoculum: Emulsify isolated bacterial colonies in 5 mL of sterile saline to achieve a turbidity equivalent to a 0.5 McFarland standard.
- Inoculation of Strip:
- Use a pipette to fill the microtubes with the bacterial suspension. For the CIT, VP, and GEL tubes, fill both the tube and the cupule.
- Create an anaerobic environment in the ADH, LDC, ODC, H2S, and URE tubes by overlaying with mineral oil after inoculation.
- Incubation: Close the incubation box with a lid and incubate at 35°C for 18-24 hours.
- Reading and Interpretation:
- After incubation, record spontaneous reactions (e.g., fermentation, decarboxylation).
- Add the required reagents to specific tests (e.g., Kovac's to IND, Barritt's A & B to VP).
- Refer to the interpretation manual to score each test as positive or negative.
- Convert the pattern of positives and negatives into a 7- or 8-digit numerical profile.
- Consult the API database (manual or software) to match the profile to a species.
Protocol: Operation of an Automated System (VITEK 2)
I. Principle: A bacterial suspension is prepared and loaded into a specialized plastic test card containing multiple biochemical wells. The card is sealed and inserted into an incubator/reader module. Optical measurements are taken periodically, and the system's software compares the kinetic reaction data to a curated database for identification [1].
II. Materials:
- VITEK 2 instrument.
- VITEK 2 ID-specific test card (e.g., GN for Gram-negative rods).
- Bacterial colony from a pure culture.
- Sterile saline tubes.
- Turbidity meter (DensiChek).
- Cassette and sealing device.
III. Procedure:
- Suspension Preparation: Select several colonies and suspend in saline. Adjust the turbidity to the manufacturer's specified McFarland index using the turbidity meter.
- Card Inoculation: Transfer the suspension tube to a cassette and attach the test card. The system automatically fills the card with the suspension via vacuum pressure.
- Loading: Place the cassette into the filling module. The instrument will seal the card and transfer it to the incubator/reader.
- Analysis: The system incubates the card and reads colorimetric and turbidimetric changes every 15 minutes. Results are typically available within 4-10 hours and are automatically reported to the computer system.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Biochemical Identification
| Item | Function/Application |
|---|---|
| Nutrient Agar & Blood Agar | General-purpose and enriched media for obtaining pure cultures from clinical samples [5]. |
| Selective Media (e.g., MacConkey, MSA) | For selective isolation of specific bacterial groups (e.g., enterics, staphylococci) from mixed samples [5]. |
| API / VITEK 2 Identification Kits | Miniaturized test panels for standardized, high-throughput biochemical profiling of bacteria and yeasts [1]. |
| Sterile Saline (0.85% NaCl) | For preparing standardized bacterial suspensions for inoculating miniaturized kits and automated systems. |
| Catalase (3% H₂O₂) & Oxidase Reagents | Rapid, single-step tests for preliminary grouping of Gram-positive cocci and Gram-negative rods [5] [1]. |
| McFarland Standards / Turbidity Meter | Essential for standardizing the density of bacterial suspensions to ensure accurate and reproducible inoculation [1]. |
The journey from agar-based media to miniaturized kits represents a monumental shift in microbial identification, characterized by a relentless drive for greater speed, accuracy, and efficiency. While traditional methods established the fundamental principles of microbial biochemistry, their limitations in speed and throughput became a bottleneck in clinical and research settings. The innovation of miniaturized kits like the API system introduced a new era of standardization and multi-parameter analysis. This evolution reached its current zenith with fully automated systems that integrate identification with antimicrobial susceptibility testing, providing a comprehensive diagnostic solution in a fraction of the time. Despite the advent of even newer technologies like MALDI-TOF MS and genomic sequencing, automated biochemical systems remain vital in many laboratories, particularly where simultaneous susceptibility testing is required or as a backup confirmatory method [1]. This historical progression underscores the dynamic nature of microbiology, where technological advancement continuously refines our ability to understand and identify the microbial world.
Within the framework of microbial identification, the characterization of key metabolic reactions provides critical data for differentiating and identifying bacterial species. Among these, carbohydrate fermentation, enzyme production, and specific substrate utilization stand as cornerstone biochemical tests. These tests exploit the fundamental truth that different bacterial groups possess distinct enzyme systems and metabolic pathways, leading to unique patterns of substrate use and end-product formation [6]. The ability to accurately profile these reactions in a laboratory setting is therefore indispensable for researchers, clinical scientists, and professionals in drug development who require precise microbial identification for diagnostics, epidemiological studies, and therapeutic discovery. This document outlines detailed application notes and protocols for investigating these critical metabolic activities.
Core Principles and Biochemical Basis
Carbohydrate Fermentation in Microbial Metabolism
Carbohydrate fermentation is a type of anaerobic metabolism where microorganisms derive energy by catabolizing organic compounds, such as sugars, without using oxygen as a terminal electron acceptor [7] [8]. In this process, the carbohydrate molecules are broken down, and the electrons are transferred to organic molecules, leading to the production of ATP and a variety of organic end products [7]. The specific pathways and end products vary by microbial species, providing a basis for differentiation.
During fermentation, carbohydrates like glucose are first broken down to pyruvate via pathways like glycolysis. The subsequent fate of pyruvate differs among organisms, yielding various end products such as lactic acid, acetic acid, ethanol, carbon dioxide, and hydrogen [6] [9]. The production of acid during fermentation lowers the pH of the surrounding medium, a key detectable outcome. Furthermore, some organisms release gaseous by-products like CO₂ or H₂ alongside acids [6].
Enzyme Production and Catalytic Efficiency
Microbial enzymes are the catalytic workhorses that drive these metabolic reactions. The evolutionary pressure on microorganisms often drives enzymes toward optimal catalytic efficiency to make the best use of cellular resources [10]. This efficiency is not a random outcome but is shaped by natural selection to maximize the ratio of metabolic flux to enzyme concentration (v_net/E_tot) under physiological conditions, constrained by biophysical limits such as diffusion rates and molecular vibration frequencies [10]. Understanding the kinetics and operational modes of these enzymes—such as Michaelis-Menten or random-ordered mechanisms—is crucial for interpreting metabolic capabilities and for applications in biotechnology and industrial processes [11] [10].
The Scientist's Toolkit: Essential Research Reagents
The following table catalogues the fundamental materials and reagents required for conducting carbohydrate fermentation tests, a foundational procedure in metabolic profiling.
Table 1: Key Research Reagent Solutions for Carbohydrate Fermentation Tests
| Reagent/Material | Function and Application |
|---|---|
| Carbohydrate Broth Base | A basal medium providing essential nutrients (peptones, salts) for microbial growth [6] [9]. |
| Specific Carbohydrates (e.g., Glucose, Lactose, Sucrose, Mannitol) | The test substrates whose fermentation ability is being assessed. They are added to the basal medium [6] [9]. |
| pH Indicators (Phenol Red, Bromocresol Purple, Andrade's) | Detects acid production by changing color as the medium's pH drops [6] [9] [12]. |
| Durham Tubes | Small, inverted tubes placed within the broth medium to capture and visualize gas produced as a by-product of fermentation [6] [9]. |
| Selective & Differential Media (e.g., MacConkey Agar, Blood Agar) | Agar-based media that inhibit certain microbes while allowing others to grow, and contain indicators to differentiate them based on metabolic reactions [5]. |
Experimental Protocol: Carbohydrate Fermentation Test
This protocol provides a step-by-step methodology for determining a microorganism's ability to ferment a specific carbohydrate, with observations for acid and gas production [6] [9] [12].
The following diagram illustrates the logical workflow and decision process for the carbohydrate fermentation test, from preparation to final interpretation of results.
Detailed Methodology
A. Preparation of Media [6] [9]
- Dissolve Components: Weigh and dissolve the components of a carbohydrate broth base (e.g., 10g proteose peptone, 5g sodium chloride, 1g beef extract) in 990 mL of distilled water.
- Add Carbohydrate and Indicator: Add 10g of the specific carbohydrate under investigation (e.g., glucose, lactose) and the pH indicator (e.g., 0.018g phenol red). Heat gently if needed for complete dissolution.
- Dispense and Tube: Dispense 5-7 mL of the broth into test tubes. Carefully place a small, inverted Durham tube into each test tube, ensuring it is completely submerged and free of air bubbles.
- Sterilize: Loosely cap the tubes and autoclave at 121°C and 15 psi pressure for 15 minutes. (Note: Some heat-sensitive carbohydrates require filter sterilization and aseptic addition to sterile, cooled broth base).
B. Inoculation and Incubation [6] [12]
- Using a sterile inoculating loop, pick up a well-isolated colony from a fresh (18-24 hour) pure culture of the test organism.
- Inoculate the broth medium by swirling the loop. Avoid touching the Durham tube.
- Incubate the inoculated tubes aerobically at 35±2°C for 18-24 hours. If no change is observed, re-incubate for up to 5 days to confirm a negative result.
C. Interpretation of Results [6] [9] [12] After incubation, observe the tubes for a color change and for the presence of a gas bubble in the Durham tube.
- Acid Production (Positive): The medium changes from red (phenol red at neutral pH) to a bright yellow color, indicating sufficient acid production has lowered the pH.
- Gas Production (Positive): A visible air bubble is trapped in the inverted Durham tube.
- No Fermentation (Negative): The medium remains red (or turns a darker purple if alkaline by-products are formed from peptone metabolism).
Table 2: Interpretation of Carbohydrate Fermentation Test Results
| Observation | Result | Interpretation |
|---|---|---|
| Yellow color change | Acid production | The organism ferments the carbohydrate and produces organic acids. |
| Yellow color change + Gas bubble | Acid and Gas production | The organism ferments the carbohydrate, producing both acid and gas. |
| No color change (remains red) | No fermentation | The organism cannot ferment the specific carbohydrate provided. |
Data Presentation and Microbial Differentiation
The patterns of carbohydrate fermentation are highly useful for differentiating between bacterial groups and species. The table below summarizes the fermentation profiles of some common bacteria, illustrating how these patterns serve as identification signatures.
Table 3: Carbohydrate Fermentation Patterns of Common Bacteria [6]
| Bacterial Species | Glucose | Lactose | Sucrose | Mannitol | Gas Production |
|---|---|---|---|---|---|
| Escherichia coli | + | + | V | + | + |
| Klebsiella pneumoniae | + | + | + | + | + |
| Proteus mirabilis | + | - | - | - | + |
| Pseudomonas aeruginosa | + | - | - | + | - |
| Salmonella Typhi | + | - | - | + | - |
| Shigella flexneri | + | - | - | + | + |
| Legend: + = Positive; - = Negative; V = Variable |
Advanced Applications and Integration in Microbial Identification
While carbohydrate fermentation is a classic tool, microbial identification has evolved to include a suite of methods. Biochemical tests like catalase, oxidase, and indole are often used in tandem with fermentation tests to create a definitive identification profile [5] [1]. For instance, a Gram-negative rod that is oxidase-negative and ferments lactose with acid and gas production is highly indicative of E. coli [1].
Modern clinical and research laboratories increasingly integrate these traditional methods with advanced technologies for greater speed and accuracy.
- Automated Biochemical Systems: Systems like API strips, VITEK 2, and BD Phoenix use miniaturized biochemical wells, including carbohydrate fermentation substrates, to generate identification profiles rapidly [1].
- Mass Spectrometry: Matrix-Assisted Laser Desorption/Ionization Time-of-Flight (MALDI-TOF MS) identifies microbes by analyzing their unique protein profiles directly from colonies, often in minutes, and has become a primary tool in many labs [1].
- Genomic Sequencing: 16S rRNA gene sequencing and whole-genome sequencing provide the most precise identification, especially for unculturable or novel organisms, by comparing genetic sequences [5].
The following diagram illustrates how the carbohydrate fermentation test fits into a broader, integrated strategy for microbial identification.
Carbohydrate fermentation testing remains a vital, robust, and accessible method for determining the metabolic capabilities of microorganisms. When performed according to the detailed protocols outlined and interpreted within the context of other biochemical and modern molecular data, it provides researchers and scientists with powerful insights for microbial differentiation and identification. The integration of these classic metabolic profiles with cutting-edge technologies like MALDI-TOF MS and genomic sequencing creates a comprehensive and definitive identification strategy, essential for advancing research, ensuring public health, and guiding drug development.
In the era of advanced microbial identification technologies, such as MALDI-TOF mass spectrometry and next-generation sequencing, traditional biochemical spot tests remain indispensable tools in both clinical and research laboratories [13]. These tests, including catalase, oxidase, coagulase, and indole, provide a rapid, cost-effective, and highly accessible means for the preliminary characterization and differentiation of microorganisms. The global microbial identification market, valued at USD 4.55 billion in 2025, continues to rely on phenotypic methods, which are anticipated to hold a dominant share of 35.2% in 2025 [13]. This enduring relevance is attributed to their ease of use, validation utility, and compatibility with existing laboratory infrastructure. Framed within a broader thesis on microbial identification, this article details the principles, protocols, and contemporary applications of these foundational tests, providing researchers and drug development professionals with essential Application Notes and Protocols for their scientific toolkit.
The Biochemical Basis of Traditional Spot Tests
Traditional spot tests are designed to detect specific enzymatic activities or biochemical products that serve as markers for microbial identification. The following section outlines the fundamental principles and significance of each test.
Principle of the Indole Test
The indole test screens for the ability of an organism to produce the enzyme tryptophanase, which degrades the amino acid tryptophan present in the medium [14] [15]. Tryptophanase catalyzes the deamination and hydrolysis of tryptophan, yielding indole, pyruvic acid, and ammonium. The detected indole combines with p-dimethylaminobenzaldehyde (DMAB) in Kovac's or Ehrlich's reagent under acidic conditions to form a red-colored quinoidal compound (rosindole) [14] [15]. This test is a critical component of the IMViC test battery, used primarily to differentiate members of the Enterobacteriaceae family.
Principle of the Catalase Test
The catalase test detects the production of the catalase enzyme, which is produced by aerobic and facultative anaerobic microorganisms to protect themselves from the toxic effects of hydrogen peroxide (H₂O₂) [16] [17]. Catalase hydrolyzes hydrogen peroxide into liquid water and oxygen gas. The rapid production of oxygen gas results in the formation of bubbles, indicating a positive test [16] [17]. This test is fundamental for differentiating catalase-positive staphylococci from catalase-negative streptococci.
Principle of the Oxidase Test
The oxidase test determines the presence of cytochrome c oxidase, the terminal enzyme in the electron transport chain of aerobic respiration [18] [19]. The colorless reagent, tetramethyl-p-phenylenediamine dihydrochloride, acts as an artificial electron donor. In oxidase-positive bacteria, the enzyme oxidizes the reagent, forming a dark purple compound, indophenol blue, within seconds [18] [19]. This test is crucial for identifying bacteria such as Pseudomonas, Neisseria, and Vibrio.
Principle of the Coagulase Test
The coagulase test identifies Staphylococcus aureus by detecting the enzyme coagulase, which is a virulence factor [20] [21]. Coagulase binds to prothrombin in plasma, converting fibrinogen to fibrin and causing plasma to clot. Two forms exist:
- Bound coagulase (clumping factor) is detected by a slide test and causes direct clumping of bacterial cells with plasma [20] [21].
- Free coagulase is detected by a tube test and forms a complex with a plasma coagulase-reacting factor, leading to the formation of a fibrin clot [20] [21].
Research Reagent Solutions: Essential Materials for Testing
The following table catalogs the key reagents and supplies required to perform these traditional spot tests, forming the core of a microbiology laboratory's toolkit.
Table 1: Essential Research Reagents and Supplies for Traditional Biochemical Tests
| Test | Key Reagents | Supplies | Function of Reagents |
|---|---|---|---|
| Indole Test [14] | Kovac’s reagent (p-dimethylaminobenzaldehyde, HCl, Amyl Alcohol) or Ehrlich’s reagent; 1% p-dimethylaminocinnamaldehyde (for spot test) | Sterile loop, filter paper (for spot test), test tubes | Kovac’s/Ehrlich’s reagent: reacts with indole to form a red complex; DMACA: reacts with indole to form a blue-green compound. |
| Catalase Test [16] [17] | 3% Hydrogen Peroxide (H₂O₂); 15% for anaerobes | Glass slide, test tubes, sterile wooden stick or platinum loop | Serves as a substrate for the catalase enzyme; breakdown leads to O₂ bubble formation. |
| Oxidase Test [18] [19] | Kovacs’ Oxidase Reagent (1% tetramethyl-p-phenylenediamine dihydrochloride) | Filter paper, platinum loop, swab, test tubes | Acts as an artificial electron acceptor for cytochrome c oxidase, forming a purple indophenol dye. |
| Coagulase Test [20] [21] | EDTA-treated Rabbit Plasma (preferred), 5% CaCl₂ (optional) | Glass slides, test tubes, loops, sterile sticks | Provides fibrinogen and coagulase-reacting factor (CRF) essential for clot formation. |
Application Notes and Experimental Protocols
This section provides detailed, step-by-step protocols for each test, including precise result interpretation to ensure reliable and reproducible outcomes.
Protocol 1: Indole Test
Application Note: This test is primarily used to differentiate within the Enterobacteriaceae family, notably distinguishing indole-positive E. coli from indole-negative Klebsiella and Enterobacter species, and Proteus mirabilis (indole-negative) from other Proteus species (indole-positive) [14].
Procedure:
- Rapid Spot Test:
- Moisten a piece of filter paper with a small amount of 1% p-dimethylaminocinnamaldehyde reagent [14].
- Using a sterile loop, pick a well-isolated colony from an 18-24 hour culture and rub it onto the moistened filter paper.
- Observation: Observe for an immediate color change. A blue color developing within 20 seconds indicates a positive test [14].
- Tube Test:
- Inoculate a tube of tryptophan broth (e.g., 1% tryptone) with the test organism and incubate at 37°C for 24-48 hours [14].
- For Kovac's method, add 5 drops of Kovac's reagent down the side of the tube. Gently tap the tube to mix.
- Observation: The appearance of a pink to cherry-red ring at the top of the medium indicates a positive test. The absence of color (yellow reagent layer) is a negative result [14].
Limitations: Do not use media containing dyes (e.g., MAC, EMB) or Mueller-Hinton agar, as tryptophan is destroyed during its preparation. A negative spot test should be confirmed with the more sensitive tube test [14].
Protocol 2: Catalase Test
Application Note: This rapid test is essential for differentiating genera, such as catalase-positive Staphylococcus and Bacillus from catalase-negative Streptococcus and Clostridium [16] [17].
Procedure (Slide Method):
- Place a clean glass slide inside a petri dish (to contain aerosols).
- Using a sterile wooden stick or platinum loop, transfer a small amount of a young (18-24 hour) colony onto the slide. Avoid picking up any agar, especially from blood agar, as blood cells are catalase-positive and can cause false positives [16] [17].
- Immediately place a drop of 3% H₂O₂ onto the bacterial smear.
- Observation: The immediate evolution of bubbles (O₂) constitutes a positive test. The absence of bubbling is negative [16] [17].
Limitations: Do not use colonies from media containing blood. Iron-containing loops (e.g., nichrome) can yield false-positive results; use platinum loops or wooden applicators. Only use fresh cultures (18-24 hours old), as older cultures may give false-negative results [16].
Protocol 3: Oxidase Test
Application Note: The oxidase test is pivotal for identifying Pseudomonas, Neisseria, Vibrio, and Campylobacter species, and for differentiating them from oxidase-negative Enterobacteriaceae [18] [19].
Procedure (Filter Paper Method):
- Place a strip of Whatman No. 1 filter paper in a sterile petri dish.
- Add 2-3 drops of 1% Kovacs oxidase reagent to moisten the paper.
- Using a platinum loop or glass rod (nichrome loops can cause false positives), pick a portion of a fresh, well-isolated colony and smear it onto the moistened filter paper.
- Observation: Observe for a color change. The development of a dark purple-blue color within 5-10 seconds is a positive result. No color change or a change after 60 seconds is considered negative [18] [19].
Limitations: Use fresh reagents (not older than one week). Test only colonies from media without high glucose content or dyes. The reagent kills the bacteria, so subculturing must be done prior to testing [18] [19].
Protocol 4: Coagulase Test
Application Note: This is the definitive test for differentiating the major pathogen Staphylococcus aureus (usually positive) from other coagulase-negative staphylococci (CoNS) like S. epidermidis and S. saprophyticus [20] [21].
Procedure:
- Slide Test (Detects Bound Coagulase):
- Emulsify several colonies in a drop of saline on each of two spots on a slide to create a dense, smooth suspension.
- Add a drop of EDTA-treated rabbit plasma to one suspension and mix gently. Leave the other as a control for auto-agglutination.
- Observation: Clumping of the bacterial cells within 10 seconds with no clumping in the control is a positive test [20] [21].
- Tube Test (Detects Free Coagulase):
- Dilute rabbit plasma 1:10 in physiological saline.
- In a small test tube, mix 0.5 mL of diluted plasma with 5 drops (approx. 0.1 mL) of a broth culture or heavy bacterial suspension from an agar plate.
- Incubate the tube at 35-37°C and examine for clot formation every 30 minutes for up to 4 hours. If no clot forms, re-examine after 24 hours.
- Observation: The formation of any degree of clot is a positive test. A negative test shows no clot formation [20] [21].
Limitations: Methicillin-resistant S. aureus (MRSA) strains may be deficient in bound coagulase, yielding a negative slide test but a positive tube test. Therefore, a negative slide test must always be confirmed with a tube test [20].
Data Presentation and Interpretation
The following tables summarize the expected results for key microorganisms, providing a quick reference for interpretation.
Table 2: Biochemical Test Results for Gram-Positive Cocci
| Microorganism | Catalase Test | Coagulase Test |
|---|---|---|
| Staphylococcus aureus | Positive [16] [17] | Positive [20] [21] |
| Staphylococcus epidermidis | Positive [16] | Negative [20] [21] |
| Streptococcus pyogenes | Negative [16] [17] | Negative |
| Enterococcus faecalis | Negative | Negative |
Table 3: Biochemical Test Results for Gram-Negative Bacilli
| Microorganism | Oxidase Test | Indole Test |
|---|---|---|
| Escherichia coli | Negative [18] [19] | Positive [14] |
| Klebsiella pneumoniae | Negative [14] | Negative [14] |
| Pseudomonas aeruginosa | Positive [18] [19] | Negative |
| Proteus mirabilis | Negative | Negative [14] |
| Proteus vulgaris | Negative | Positive [14] |
| Salmonella enterica | Negative | Negative |
Visualizing Workflows and Biochemical Pathways
The diagrams below outline the logical workflow for microbial identification using these tests and the biochemical pathways involved.
Figure 1: A decision tree outlining the use of traditional spot tests in the preliminary identification of bacteria based on Gram stain morphology.
Figure 2: The core biochemical reactions catalyzed in each of the four traditional spot tests, showing substrate, enzyme, and visual endpoint.
Despite the rapid advancement and adoption of molecular and proteomic technologies, traditional biochemical spot tests retain a vital role in microbial identification. Their speed, low cost, and simplicity make them invaluable for initial screening, teaching foundational microbiological principles, and validating results from automated systems. As the microbial identification market grows, with phenotypic methods maintaining a significant share, the catalase, oxidase, coagulase, and indole tests will continue to be essential components of the researcher's and clinical microbiologist's arsenal. Their judicious application, following standardized protocols and acknowledging limitations, ensures their continued contribution to accurate microbial characterization in both diagnostic and drug development contexts.
From Manual Kits to Automation: A Practical Guide to Biochemical Identification Workflows
In the landscape of microbial identification, phenotypic methods based on biochemical reactions remain a cornerstone for characterizing microorganisms. Among these, the Analytical Profile Index (API) system, pioneered by bioMérieux, represents a well-established, manual method often regarded as a gold standard technique for identification to the species level [22] [23]. This system provides a standardized, miniaturized version of conventional biochemical tests, which were historically complicated to perform and interpret [24]. The API platform is designed for the identification of a broad spectrum of microorganisms, including Gram-positive bacteria, Gram-negative bacteria, and yeasts, making it an indispensable tool in clinical, industrial, and research laboratories [22].
The global microbial identification market, where phenotypic methods like API strips hold a dominant share, is witnessing significant growth driven by the need for accurate and rapid diagnostics [13]. Despite the advent of advanced technologies like MALDI-TOF mass spectrometry and next-generation sequencing, biochemical identification systems remain favored for their cost-effectiveness, accessibility, and utility in validating genotypic findings [13]. The API system, with its extensive and robust database encompassing over 600 species, provides a reliable and accessible means of microbial identification, solidifying its role in comprehensive microbial characterization [23].
The API product line comprises specialized test strips, each configured for identifying specific groups of microorganisms. These kits consist of plastic strips with multiple (up to 20) miniature test chambers containing dehydrated substrates [22] [24]. The following table summarizes the primary API strip types and their designated uses:
Table 1: API Strip Selection for Microbial Identification
| Strip Name | Target Microorganisms | Incubation Time | Key Applications |
|---|---|---|---|
| API 20E [22] | Enterobacteriaceae & other non-fastidious Gram-negative rods | 18-24 hours [22] | Infectious disease diagnosis; industrial microbe ID [24] |
| API Rapid 20E [22] | Enterobacteriaceae | 4 hours [22] | Rapid clinical diagnosis |
| API 20NE [22] | Non-Enterobacteriaceae Gram-negative rods | 24-48 hours [22] | Identification of Pseudomonas [23] |
| API Staph [22] | Staphylococci & Micrococci | Overnight [22] | ID of Staphylococcus aureus [23] |
| API 20 Strep [22] | Streptococci & Enterococci | 4 or 24 hours [22] | ID of Enterococcus [23] |
| API Coryne [22] | Corynebacteria & similar organisms | 24 hours [22] | - |
| API Listeria [22] | Listeria species | 24 hours [22] | ID of Listeria monocytogenes [23] |
| API 20C AUX [22] | Yeasts | 48-72 hours [22] | Yeast identification |
| API 20A [22] | Anaerobes | 24 hours [22] | ID of Clostridium perfringens [23] |
Principles of the API 20E System
The API 20E strip is a quintessential model for understanding the system's operation, specifically designed for the identification of Enterobacteriaceae and other non-fastidious Gram-negative bacilli [22] [24]. Its principle relies on detecting specific enzymatic activities and metabolic capabilities of the inoculated bacterium [24].
Each of the 20 microtubes on the strip contains dehydrated substrates for a distinct biochemical test. When a bacterial suspension is used to rehydrate these wells, microbial metabolism during incubation leads to visible color changes. These changes result from pH variations or the production of specific metabolites, which are either spontaneous or revealed by the addition of reagents post-incubation [24] [25]. The pattern of positive and negative reactions is used to determine the identity of the organism.
Experimental Protocol: API 20E Test Procedure
Materials and Reagent Setup
Table 2: Essential Research Reagent Solutions for API 20E
| Item | Function/Description |
|---|---|
| API 20E Strip [25] | Plastic strip with 20 dehydrated biochemical test chambers. |
| 0.85% Saline Solution [25] | Isotonic solution for creating a homogeneous bacterial suspension. |
| Sterile Mineral Oil [25] | Creates an anaerobic environment for specific tests (ADH, LDC, ODC, H2S, URE). |
| Incubation Chamber [25] | Plastic tray with lid; a humidified environment is created by adding water to the bottom. |
| Kovac's Reagent [24] | Detects indole production (IND test) from tryptophan metabolism. |
| Barritt's Reagents A & B [25] | Detect acetoin (VP test) in the Voges-Proskauer reaction. |
| 10% Ferric Chloride (FeCl₃) [25] | Detects phenylpyruvic acid production (TDA test) by tryptophan deaminase. |
| APIWEB Database / Codebook [22] [24] | Software or manual reference for converting reaction profiles into species identification. |
Workflow Diagram
Step-by-Step Methodology
- Bacterial Suspension Preparation: Using a pure culture (18-24 hours old), emulsify a single isolated colony (2-3 mm diameter) in 5 mL of 0.85% sodium chloride solution to create a homogeneous, turbid suspension [25].
- Strip Inoculation:
- Hold the API 20E strip at a slight angle.
- Using a sterile Pasteur pipette, fill each test well (cupule) with the bacterial suspension. Use capillary action by touching the pipette tip to the side of the cupule's neck to draw fluid in, avoiding bubble formation [25].
- Completely fill the CIT, VP, and GEL wells to the top. For the ADH, LDC, ODC, H2S, and URE wells, which require an anaerobic environment, subsequently overlay the inoculated media with sterile mineral oil to fill them completely [24] [25].
- Incubation:
Interpretation of Results and Data Analysis
Post-Incubation Reagent Addition and Reading
After the incubation period, specific reagents must be added to particular wells to reveal test results [24] [25]:
- TDA (Tryptophan Deaminase): Add 1 drop of 10% Ferric Chloride. A dark brown color indicates a positive reaction.
- IND (Indole): Add 1 drop of Kovac's reagent. A red or pink ring forms atop the medium if positive.
- VP (Voges-Proskauer): Add 1 drop of VP reagent A (α-naphthol) and 1 drop of VP reagent B (40% KOH). A red color developing within 10 minutes indicates a positive reaction.
The remaining tests are read based on spontaneous color changes according to the provided color chart [24]. The results are recorded as positive or negative for each of the 20 tests.
Profile Number Generation and Identification
The interpretation process involves converting the pattern of biochemical reactions into a numerical profile for database matching.
The 20 tests on the strip are divided into groups of three, with each test in a triplet assigned a value of 1, 2, or 4. The values for the positive tests within each triplet are summed to create a single digit. This process is repeated for all groups, generating a 7-digit profile number [24]. For example, if in the first triplet (ONPG, ADH, LDC) both ADH and LDC are positive, the calculation is 0 (for ONPG) + 2 (for ADH) + 4 (for LDC) = 6. This number is then referenced in the API codebook or entered into the APIWEB software to obtain the species identification, often with a confidence percentage [22] [24].
Table 3: Example Biochemical Tests in API 20E and Their Significance
| Test Code | Full Name | Biochemical Principle | Positive Result Indication |
|---|---|---|---|
| ONPG [24] | o-Nitrophenyl-β-D-galactopyranoside | Tests for β-galactosidase enzyme | Ability to ferment lactose |
| CIT [24] | Citrate Utilization | Uses citrate as sole carbon source | Can grow on citrate medium |
| LDC [24] | Lysine Decarboxylase | Decarboxylation of lysine | Specific metabolic pathway present |
| URE [24] | Urease | Production of urease enzyme | Hydrolyzes urea to ammonia & CO₂ |
| IND [24] | Indole Production | Production of indole from tryptophan | Presence of tryptophanase enzyme |
| VP [24] | Voges-Proskauer | Detection of acetoin | Use of butylene glycol pathway |
API strips represent a critical nexus between traditional microbiology and modern diagnostic needs. Their standardization, cost-effectiveness, and extensive validation make them a trusted method for microbial identification in diverse settings worldwide [24] [13]. As confirmed by market analysis, phenotypic methods, including automated versions of biochemical tests, are anticipated to maintain a dominant market share, underscoring their continued relevance [13]. For researchers and drug development professionals, the API system provides a robust, gold-standard technique that is particularly valuable for validating newer genomic identifications, troubleshooting discrepant results, and conducting studies in resource-limited settings. Its simplicity, combined with the powerful, database-driven interpretation, ensures that manual multitest systems will remain a vital component of the scientist's toolkit for comprehensive microbial characterization.
Automated high-throughput platforms have revolutionized microbial identification and antimicrobial susceptibility testing (AST) in clinical and research settings. These systems provide rapid, accurate results that are essential for effective patient care, drug development, and antimicrobial stewardship programs. Within the broader context of biochemical test-based microbial identification research, this application note details the technical specifications, performance characteristics, and implementation protocols for three major automated platforms: VITEK 2 (bioMérieux), BD Phoenix (BD Diagnostic Systems), and MicroScan (Siemens Healthcare Diagnostics). Each system employs distinct technological approaches to biochemical substrate utilization analysis and growth detection, enabling comprehensive microbial characterization with minimal manual intervention [26]. The integration of these systems into laboratory workflows has significantly reduced turnaround times while maintaining high accuracy standards compared to conventional methods [27] [28].
The VITEK 2, BD Phoenix, and MicroScan systems represent evolving generations of automation in microbiological diagnostics. Each platform offers unique advantages in testing capacity, technological approach, and application flexibility. Understanding their core specifications enables laboratories to select the most appropriate system for their specific research or clinical needs.
Table 1: Technical Specifications of Automated Microbiology Platforms
| Parameter | VITEK 2 Compact | BD Phoenix M50 | MicroScan MICroSTREP |
|---|---|---|---|
| Identification Technology | Biochemical substrate utilization with colorimetric/fluorimetric detection | Modified conventional, fluorogenic, and chromogenic substrates | Conventional biochemical reactions with photometric interpretation |
| AST Technology | Kinetic growth measurement in antibiotic-containing wells | Redox indicator with turbidity measurement | Broth microdilution with visual or automated reading |
| Testing Capacity | Variable by model (30-240 tests) | Up to 100 ID/AST combination panels simultaneously | Batch processing of panels |
| Identification Time | 2-18 hours (organism-dependent) | 2-12 hours (organism-dependent) | 18-24 hours (standard incubation) |
| AST Time | 4-18 hours | 6-16 hours | 18-24 hours |
| Database Coverage | Gram-negative, Gram-positive, anaerobes, yeasts, coryneforms | Gram-negative, Gram-positive, yeasts | Primarily Gram-positive bacteria (Streptococcus pneumoniae in studied format) |
| Panel Types | Disposable, barcoded test cards | ID-only, AST-only, and combination panels | Specialized panels for specific organism groups |
| Software Features | 21 CFR Part 11 compliant, expert system, one-click validation | Data management, expert system, EpiCenter connectivity | Conventional interpretation |
The technological diversity among these platforms reflects their development across different generations of automation. The VITEK 2 system employs sealed, disposable test cards with miniaturized wells containing biochemical substrates, which are read every 15 minutes to generate kinetic growth curves [29]. The BD Phoenix system utilizes a combination of traditional and novel substrates with both colorimetric and fluorogenic endpoints, reading panels every 20 minutes during incubation [30]. The MicroScan system, while offering automated reading capabilities, often requires longer incubation times comparable to manual methods but provides excellent reproducibility [27].
Performance Comparison and Validation Data
Rigorous comparative studies have established the performance characteristics of these automated systems against reference methods and one another. The essential agreement (EA - MIC within one doubling dilution of reference) and categorical agreement (CA - identical susceptibility categorization) provide standardized metrics for evaluating system reliability.
Table 2: Performance Comparison for Streptococcus pneumoniae Testing (n=311 isolates)
| Platform | Essential Agreement (%) | Categorical Agreement (%) | Very Major Errors | Minor Errors | Average Time to Result (hours) |
|---|---|---|---|---|---|
| BD Phoenix | 90.4-100% (by antibiotic) | 99.3% | 1 | 29 | 12.1 |
| VITEK 2 | >95% (overall) | 98.8% | 7 | 28 | 9.8 |
| MicroScan MICroSTREP | >95% (overall) | 99.5% | 0 | 19 | 24 |
| Etest (reference) | >95% (overall) | 99.5% | 0 | 13 | 24 |
For S. pneumoniae susceptibility testing, the BD Phoenix system demonstrated the highest overall categorical agreement (99.3%) with fewer very major errors (false susceptible results) compared to VITEK 2 [27] [28]. Both automated systems provided results in approximately half the time required by manual methods, offering significant advantages for clinical decision-making. The Phoenix system showed excellent essential agreement (90.4-100%) across individual antimicrobial agents, with perfect performance (100%) observed for vancomycin and gatifloxacin [27].
In a separate evaluation focusing on staphylococci and enterococci, the BD Phoenix system correctly identified 99.7% of isolates to genus level and 99.3% to species level, with all S. aureus isolates and enterococci being accurately identified [30]. For antimicrobial susceptibility testing of these gram-positive organisms, the system demonstrated categorical agreement of 98.2% for S. aureus and 100% for enterococci, successfully detecting all 36 vancomycin-resistant enterococci included in the study [30].
Resistance Detection Capabilities
Modern automated platforms incorporate specialized algorithms and test configurations to detect emerging antimicrobial resistance patterns, which is crucial for both clinical management and epidemiological surveillance.
Table 3: Resistance Marker Detection Capabilities
| Resistance Mechanism | BD Phoenix | VITEK 2 | MicroScan |
|---|---|---|---|
| Methicillin (MRSA) | mecA detection | Oxacillin interpretation | Oxacillin interpretation |
| Vancomycin (VRE/VRSA) | Yes | Interpretation-based | Interpretation-based |
| ESBL Production | Yes, with confirmation | Yes, with confirmation | Variable |
| Carbapenemase (CPO) | Detection with Ambler classification | Not specified | Not specified |
| Inducible Clindamycin (iMLSb) | Yes | Not specified | Not specified |
| High-Level Aminoglycoside (HLAR) | Yes | Not specified | Not specified |
The BD Phoenix system offers particularly comprehensive resistance detection, including the CPO Detect test that provides Ambler classification (A, B, or D) for carbapenemase-producing organisms directly from the susceptibility panel [31]. This phenotypic classification occurs within 6-11 hours on average and represents a significant advantage for guiding targeted therapeutic interventions [31]. Both VITEK 2 and BD Phoenix systems incorporate expert systems that flag unusual resistance patterns and suggest confirmatory testing when needed.
Detailed Experimental Protocols
VITEK 2 Identification Protocol
The VITEK 2 system employs standardized inoculation procedures with subsequent automated incubation, reading, and interpretation. The following protocol details microbial identification using ATCC Minis as quality control strains, adaptable for clinical or research isolates [32].
Materials Required:
- VITEK 2 Compact or equivalent system
- Appropriate identification card (GN, GP, YST, NH, ANC, CBC, BCL)
- ATCC Minis or pure subcultured isolates
- Recommended agar media for each organism
- Saline solution (0.45-0.50%)
- DensiCHECK Plus or equivalent nephelometer
- Polystyrene tubes (12 × 75 mm)
- Sterile cotton swabs
- Incubation equipment appropriate for each organism
Procedure:
- Culture Preparation: Thaw frozen ATCC Minis or select isolated colonies from fresh subculture (18-24 hours growth). Culture purity is essential for accurate identification.
- Inoculum Preparation: Using a sterile swab, transfer colonies to 3.0 mL saline solution in a polystyrene tube. Vortex thoroughly to create a homogeneous suspension.
- Standardization: Adjust turbidity to the appropriate McFarland standard using a calibrated densitometer:
- Gram-negative bacteria: 0.50-0.63 McFarland
- Gram-positive bacteria: 0.50-0.63 McFarland
- Yeasts: 1.8-2.2 McFarland
- Fastidious organisms: As recommended for specific card type
- Card Inoculation: Place the standardized suspension and selected identification card into a cassette. The system automatically fills cards through vacuum injection.
- Loading and Incubation: Insert cassettes into the instrument within 30 minutes of inoculation. Cards are incubated at 35±2°C with continuous kinetic monitoring.
- Data Interpretation: The system compares biochemical reaction patterns to its database, generating a bionumber and percent probability of identification. Results are typically available within 2-18 hours, depending on the card type and organism [29].
Quality Control:
- Perform QC with recommended strains (e.g., ATCC quality control strains)
- Monitor McFarland standardization regularly
- Maintain appropriate environmental conditions for incubation
BD Phoenix Antimicrobial Susceptibility Testing Protocol
This protocol details AST performance using the BD Phoenix system, adaptable for both clinical isolates and challenge strains in research settings [30].
Materials Required:
- BD Phoenix M50 System
- Phoenix combination or AST-only panels
- CrystalSpec nephelometer or equivalent
- Phoenix AST broth
- Phoenix ID broth (for combination panels)
- Redox indicator (AST indicator)
- Sterile saline (0.45-0.50%)
- Incubation equipment
Procedure:
- Inoculum Preparation: Select 3-5 well-isolated colonies from fresh culture (18-24 hours). Prepare suspension in saline to achieve 0.5 McFarland standard.
- AST Inoculation: Transfer 25μL of standardized suspension to AST broth tube containing one drop of redox indicator. Mix thoroughly.
- ID Inoculation (combination panels): Pour remaining suspension into the ID side of the combination panel.
- Panel Loading: Pour AST broth into the AST side of the panel. Load panels into the instrument within 30 minutes of inoculation.
- Incubation and Reading: Panels are incubated at 35±2°C with readings every 20 minutes. The system employs dual technology (redox indicator and turbidity) for growth detection.
- Result Interpretation: The system determines MICs based on growth patterns and applies expert rules for interpretation. Results are typically available within 6-16 hours.
Quality Control:
- Test control strains with each new lot number and periodically as recommended
- Verify inoculum density regularly
- Monitor instrument function and temperature stability
MicroScan Susceptibility Testing Protocol
The MicroScan system provides reliable susceptibility testing with conventional incubation times but automated reading capabilities [27].
Materials Required:
- MicroScan MICroSTREP plus panels
- Renok hydrator/inoculator system
- Mueller-Hinton broth with lysed horse blood (2-5%)
- Saline solution (0.45-0.50%)
- Densitometer
- Incubation equipment (ambient air, 35±2°C)
Procedure:
- Inoculum Preparation: Create bacterial suspension in saline adjusted to 0.5 McFarland standard.
- Panel Inoculation: Using the Renok system, deliver 115μL of inoculated Mueller-Hinton broth with lysed horse blood to each well of the microdilution panel.
- Incubation: Incubate panels at 35°C in ambient air for 20-24 hours.
- Reading: Read panels visually or with automated reading equipment. Determine MICs based on well growth patterns.
- Interpretation: Apply CLSI guidelines for categorical interpretation of MIC results.
Workflow Integration and Automation
Modern microbiology laboratories increasingly implement integrated automation systems that streamline the entire testing process from specimen processing to result reporting. Automated inoculation and streaking systems represent the initial phase of this integration, handling repetitive tasks with greater consistency and efficiency [33].
Automated Microbiology Testing Workflow
This workflow diagram illustrates the integrated process from specimen receipt through final reporting. Automated systems handle barcoding, inoculum preparation, and often interpretation through sophisticated algorithms. The integration of digital imaging and artificial intelligence enables automated plate reading and sorting, significantly reducing hands-on technologist time [33]. Middleware connectivity allows bidirectional communication with laboratory information systems, facilitating automated result entry and alert notifications for critical results.
Research Reagent Solutions
Successful implementation of automated microbiology platforms requires standardized reagents and quality control materials to ensure reproducible, accurate results across experiments and between laboratories.
Table 4: Essential Research Reagents for Automated Microbiology
| Reagent/Material | Function | Application Examples |
|---|---|---|
| ATCC Minis | Ready-to-use quality control strains in glycerol stock | VITEK 2 QC testing for ANC, BCL, CBC, GP, GN, NH, YST cards [32] |
| Identification Cards/Panels | Contain biochemical substrates for organism identification | VITEK 2 ANC, GN, GP cards; BD Phoenix ID panels |
| Susceptibility Panels | Contain antimicrobial dilutions for MIC determination | BD Phoenix SMIC/ID-100; MicroScan MICroSTREP plus |
| Standardized Inoculum Broths | Provide optimal nutrient base for microbial growth during testing | Phoenix AST broth; VITEK 2 saline suspension medium |
| McFarland Standards | Calibrate bacterial suspension density for proper inoculation | DensiCHECK; CrystalSpec nephelometer |
| Quality Control Strains | Verify system performance and reagent functionality | S. pneumoniae ATCC 49619; S. agalactiae ATCC 13813 [27] |
The ATCC Minis format provides particular advantages for automated systems, offering single-use, quality-controlled strains that eliminate the need for subculturing from lyophilized stocks. Studies have demonstrated 91-99% identification probability across various VITEK 2 card types when using these standardized strains [32]. The frozen glycerol stock format maintains biochemical characteristics identical to lyophilized counterparts while simplifying workflow integration.
Automated high-throughput platforms represent the convergence of microbiology, robotics, and informatics to address the growing demands for rapid, accurate microbial characterization. The VITEK 2, BD Phoenix, and MicroScan systems each offer distinct advantages in testing capabilities, workflow integration, and resistance detection. Performance validation demonstrates excellent agreement with reference methods while significantly reducing time-to-result compared to manual techniques. As antimicrobial resistance continues to evolve, these automated systems provide essential tools for both clinical management and research applications, particularly when implemented with standardized reagents and quality control protocols. The integration of artificial intelligence and enhanced data management in next-generation systems will further transform microbial identification and susceptibility testing in research and diagnostic contexts.
Microbial identification remains a cornerstone of microbiological research, clinical diagnostics, and pharmaceutical development. The Gram stain, developed by Hans Christian Gram in 1882, serves as the foundational first step in this process, providing immediate categorization of bacteria based on cell wall structure [34] [35]. This initial phenotypic characterization guides subsequent analytical choices, creating an integrated workflow that progresses from basic staining to sophisticated molecular and mass spectrometry-based identification methods. Within the expanding global microbial identification market—projected to grow from USD 4.55 billion in 2025 to USD 10.01 billion by 2032—the integration of traditional techniques with advanced technologies like MALDI-TOF mass spectrometry and next-generation sequencing represents a critical paradigm for research efficiency and diagnostic accuracy [13].
Gram Stain: Principles and Protocol
Theoretical Basis
The Gram stain technique differentiates bacteria based on fundamental differences in cell wall architecture. Gram-positive bacteria possess thick peptidoglycan layers (approximately 90% of cell wall content) that retain the crystal violet-iodine complex after decolorization, appearing purple-blue under microscopy [34] [35]. In contrast, gram-negative bacteria have thin peptidoglycan layers (approximately 10% of cell wall content) with high lipid content, allowing decolorizer to remove the primary stain; they subsequently take up the counterstain and appear pink-red [34] [35]. This differential staining provides immediate morphological information about bacterial shape (cocci or bacilli) and arrangement (clusters, chains, or pairs), offering preliminary data that directs downstream identification strategies [35].
Detailed Staining Protocol
Specimen Preparation
- Collection: Obtain specimens using aseptic technique based on infection site: sterile body fluids (blood, CSF, synovial fluid), respiratory samples (sputum from deep cough), urine (midstream clean-catch), or swabs (throat, wound, genital) [34] [35].
- Smear Preparation: Transfer small amount of specimen to clean glass slide using sterile loop. For solid media, emulsify colony in sterile water or saline. Spread evenly to form thin film approximately 15mm in diameter [34].
- Fixation: Air dry completely, then heat-fix by passing slide gently through Bunsen burner flame 2-3 times. Avoid overheating which may distort cellular morphology [34] [36].
Staining Procedure
- Apply Crystal Violet: Flood smear with crystal violet solution for 10-60 seconds. Pour off excess and rinse gently with distilled or tap water [34] [36].
- Apply Gram's Iodine: Cover smear with iodine solution (mordant) for 10-60 seconds. The iodine forms insoluble complex with crystal violet within bacterial cells. Rinse with water [34] [36].
- Decolorization: Tilt slide at angle and apply decolorizer (acetone/ethanol mixture, 50:50 v/v) dropwise for 1-5 seconds until runoff becomes clear. This is the most critical step; over-decolorization may render gram-positive bacteria appearing gram-negative, while under-decolorization may leave gram-negative bacteria appearing gram-positive [34] [36].
- Counterstaining: Flood smear with safranin or basic fuchsin solution for 30-60 seconds. Rinse gently with water and blot dry with bibulous paper or air dry [34] [36].
Microscopic Examination
- Examine using light microscope with oil immersion at 100x objective.
- Systematically scan multiple fields, particularly areas where smear is one cell thick.
- Record gram reaction (positive: purple-blue; negative: pink-red), morphology (cocci, bacilli, coccobacilli), arrangement (clusters, chains, pairs, tetrads), and presence of host cells [34] [35].
Table 1: Interpretation of Gram Stain Findings
| Appearance | Interpretation | Common Examples |
|---|---|---|
| Gram-positive cocci in clusters | Staphylococcus species | S. aureus |
| Gram-positive cocci in chains | Streptococcus species | S. pneumoniae |
| Gram-positive bacilli, thick | Clostridium species | C. perfringens |
| Gram-positive bacilli, thin | Listeria species | L. monocytogenes |
| Gram-negative diplococci | Neisseria species | N. meningitidis |
| Gram-negative bacilli, thin | Enterobacteriaceae | E. coli, Klebsiella |
| Gram-negative coccobacilli | Haemophilus species | H. influenzae |
| Gram-variable, branched | Actinomyces, Nocardia species | A. israelii |
Integrated Identification Workflow
The Gram stain represents merely the initial step in a comprehensive microbial identification pipeline. Contemporary laboratory practice integrates this classical technique with modern technological platforms to achieve accurate species-level identification, which is essential for both research characterization and clinical decision-making.
Diagram: Microbial identification workflow integrating Gram stain with modern methods.
Phenotypic Identification Methods
Following Gram stain characterization, phenotypic methods leverage microbial metabolism and growth characteristics for identification. These approaches remain widely utilized, accounting for an estimated 35.2% of the microbial identification market in 2025 [13].
Biochemical Test Systems
- Manual Test Strips: Systems like API (Analytical Profile Index) utilize microcupules containing dehydrated substrates to test carbohydrate fermentation, enzyme activity, and metabolic byproducts [13].
- Automated Platforms: Instruments including VITEK 2, VITEK COMPACT PRO, and BD Phoenix systems automate inoculation, incubation, and interpretation, significantly reducing processing time [13].
Advantages and Limitations Phenotypic methods offer cost-effectiveness, established protocols, and validation utility, particularly in resource-constrained settings [13]. However, they typically require 24-48 hours for pure culture growth and sufficient metabolic activity, and may lack discrimination for closely related species or atypical strains.
Genotypic Identification Methods
Molecular techniques provide species-level identification by analyzing genetic targets, offering superior specificity and reduced turnaround time compared to phenotypic methods.
PCR-Based Methods
- Conventional and Real-Time PCR: Amplify species-specific gene targets for detection and identification. Real-time PCR additionally enables quantification of microbial load [13].
- Broad-Range PCR: Amplify conserved regions (e.g., 16S rRNA gene for bacteria, ITS for fungi) followed by sequencing for definitive identification, particularly valuable for fastidious or uncultivable organisms [13].
Next-Generation Sequencing (NGS) Comprehensive genomic analysis through platforms like Charles River Laboratories' Accugenix NGS Services enables high-resolution strain typing, virulence factor detection, and resistance gene identification, supporting pharmaceutical manufacturing quality control and outbreak investigation [13].
Mass Spectrometry-Based Identification
Matrix-assisted laser desorption/ionization time-of-flight (MALDI-TOF) mass spectrometry has revolutionized routine microbial identification by analyzing unique protein profiles, primarily highly abundant ribosomal proteins.
Methodology
- Create thin smear of pure colony on target plate.
- Overlay with matrix solution (e.g., α-cyano-4-hydroxycinnamic acid).
- Ionize sample with laser and measure time-of-flight of ions.
- Compare resulting mass spectrum against reference database [13].
Performance Characteristics MALDI-TOF systems identify most common bacterial and yeast isolates within minutes directly from colonies, with reported species identification rates exceeding 90% for most clinical isolates [13]. Implementation has demonstrated 30% reduction in time-to-report for blood culture pathogens in clinical settings like University Hospital Heidelberg [13].
Table 2: Comparison of Microbial Identification Technologies
| Technology | Time to Result | Approximate Cost | Discriminatory Power | Key Applications |
|---|---|---|---|---|
| Gram Stain | 10-30 minutes | Low | Low to Moderate | Initial categorization, morphology |
| Biochemical Panels | 24-48 hours | Low to Moderate | Moderate | Species identification, metabolic profiling |
| Automated Phenotypic Systems | 4-18 hours | Moderate | Moderate to High | Routine clinical identification, AST |
| MALDI-TOF MS | 10-30 minutes | Moderate | High | Routine high-throughput identification |
| 16S rRNA Sequencing | 6-24 hours | High | High | Difficult-to-identify organisms, research |
| NGS | 1-5 days | Very High | Very High | Outbreak investigation, research, strain typing |
Research Reagent Solutions
Table 3: Essential Reagents and Materials for Gram Stain and Identification Workflow
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Crystal Violet (Primary Stain) | Stains all bacterial cells purple | Critical for initial staining; 0.5-1% aqueous solution typically used [34] |
| Gram's Iodine (Mordant) | Forms crystal violet-iodine complex | Fixes primary stain within gram-positive cell walls [34] |
| Acetone/Ethanol Decolorizer | Removes primary stain from gram-negative bacteria | Most critical step; timing varies with smear thickness [34] [36] |
| Safranin/Basic Fuchsin (Counterstain) | Stains decolorized gram-negative bacteria | Basic fuchsin provides more intense staining than safranin for some organisms [34] |
| MALDI-TOF Matrix Solution | Enables laser desorption/ionization | Typically α-cyano-4-hydroxycinnamic acid in organic solvent [13] |
| PCR Master Mixes | Amplification of target DNA sequences | Include DNA polymerase, dNTPs, buffers for specific gene targets [13] |
| Biochemical Test Strips/Kits | Metabolic profiling | API, VITEK, or similar systems with dehydrated substrates [13] |
| Selective Culture Media | Supports growth of target organisms | Chromogenic media enhance differentiation of species [34] |
Technical Considerations and Troubleshooting
Gram Stain Optimization
Several factors impact Gram stain reliability and must be carefully controlled:
- Culture Age: Older cultures may lose peptidoglycan integrity, causing gram-positive organisms to appear gram-negative [34].
- Smear Thickness: Excessively thick smears prevent proper decolorization, while very thin smears may yield insufficient material for interpretation [34].
- Decolorization Time: Insufficient decolorization may leave gram-negative organisms appearing gram-positive; excessive decolorization may remove stain from gram-positive organisms [34] [36].
- Stain Freshness: Deteriorated stains, particularly crystal violet and decolorizer, produce unreliable results [34].
Method Selection Framework
Choosing appropriate identification strategies depends on multiple factors:
- Urgency: MALDI-TOF provides fastest turnaround (minutes); phenotypic methods require longer incubation [13].
- Resources: MALDI-TOF instrumentation represents significant capital investment; PCR and biochemical methods have lower initial costs [13].
- Discriminatory Needs: Epidemiological studies require high-resolution methods (NGS, MLST); routine identification may suffice with phenotypic methods or MALDI-TOF [13].
- Sample Quality: Direct specimen testing requires molecular methods; culture-based methods necessitate viable organisms [34] [13].
The integration of Gram staining within a comprehensive identification workflow represents a powerful paradigm for microbial characterization. This hierarchical approach leverages the rapid, cost-effective nature of phenotypic staining to inform subsequent methodological selections, whether phenotypic, genotypic, or mass spectrometry-based. As the microbial identification market evolves with technological advancements, the fundamental role of Gram staining as an initial categorization tool remains unchallenged. For researchers and laboratory professionals, understanding the capabilities, limitations, and appropriate application contexts for each identification method ensures optimal resource utilization and diagnostic accuracy in both research and clinical settings. The continued integration of classical techniques with emerging technologies will further enhance our ability to rapidly and accurately characterize microorganisms, advancing both basic research and applied diagnostic science.
In the field of pharmaceutical development and manufacturing, ensuring product safety is paramount. Microbial contamination poses a significant risk, capable of compromising drug efficacy and patient safety. The systematic approach to contamination control rests on three fundamental pillars: robust environmental monitoring for early detection, precise tracking to identify contamination sources, and thorough root cause analysis to prevent recurrence. Within this framework, microbial identification serves as the critical first step, enabling all subsequent investigative and corrective actions [1].
The evolution of microbial identification technologies has progressively enhanced our ability to respond to contamination events. While traditional biochemical methods remain relevant for characterizing microorganisms, modern approaches like MALDI-TOF MS can provide identifications from pure colonies in minutes rather than days, dramatically accelerating the investigation process [1]. This application note details integrated methodologies for implementing these principles within drug manufacturing environments, with specific focus on technical protocols suitable for researchers, scientists, and development professionals.
Environmental Monitoring Program (EMP) Design
Core Principles and Objectives
An Environmental Monitoring Program (EMP) is a systematic, scientific approach to validating the effectiveness of preventive controls within a controlled environment [37]. For pharmaceutical manufacturers, the primary objectives mirror those in food safety but are adapted for cleanroom and manufacturing settings [37]:
- Primary Objective: To detect pathogens or indicator organisms in the environment before they contaminate pharmaceutical products.
- Secondary Objective: To identify microorganisms that could cause product spoilage or degradation.
- Tertiary Objective: To assess and verify the effectiveness of cleaning, sanitation, and hygiene practices.
The data generated by an EMP serves as crucial evidence for both internal quality control and regulatory compliance, demonstrating that manufacturing environments remain in a validated state of control [38].
The Zone Concept for Risk-Based Sampling
A risk-based sampling strategy is fundamental to an effective EMP. The "Zone Concept" provides a structured framework for classifying areas based on their proximity to the product and potential impact on product sterility. This hierarchical approach enables efficient resource allocation.
Table: Environmental Monitoring Zones and Sampling Specifications
| Zone | Description | Target Microorganisms | Testing Frequency | Sampling Tools |
|---|---|---|---|---|
| Zone 1 | Direct product contact surfaces (e.g., vessels, filling needles, utensils) | Indicator organisms (e.g., Aerobic Plate Count, Yeast/Mold); pathogen testing as risk-assessed | Daily or per batch campaign [37] | Sterile swabs, contact plates |
| Zone 2 | Non-product contact surfaces close to Zone 1 (e.g., equipment frames, adjacent walls) | Indicator organisms (APC, Y/M); environmental monitoring for objectionable organisms | Weekly | Swabs, sponges |
| Zone 3 | Non-product contact surfaces further from Zone 1 (e.g., floors, ceilings, drains) | Indicator organisms; heightened focus on drains for Gram-negative bacteria | Weekly | Swabs, sponges |
| Zone 4 | Support areas outside processing rooms (e.g., hallways, change rooms) | Indicator organisms to monitor general facility hygiene | Monthly | Swabs, settle plates |
Establishing Sampling Sites and Frequency
The identification of specific sampling locations should be science-based and documented in a facility map and sampling plan [38]. Key considerations include:
- Historical Data: Use historical environmental monitoring data to identify potential problem areas.
- Risk Assessment: Employ tools like FMEA or HACCP to identify contamination points, including hard-to-clean areas, high-traffic zones, and material transfer points [38].
- Sampling During Operations: Monitoring should occur during active manufacturing to accurately assess environmental control under dynamic conditions.
Microbial Identification Methods for Contamination Investigation
When a contamination event occurs or an action level is exceeded, accurate microbial identification becomes critical for the subsequent investigation. The following table compares the primary identification methodologies used in clinical and pharmaceutical microbiology.
Table: Comparison of Microbial Identification Methodologies
| Method | Principle | Time to Identification | Advantages | Limitations |
|---|---|---|---|---|
| Traditional Biochemical Tests | Metabolic profiling using carbohydrate utilization, enzyme production [1] | 2-5 days [1] | Low cost; well-established databases; easy to perform | Slow; limited accuracy for unusual or closely related species |
| Automated Biochemical Systems | Miniaturized biochemical panels read by automated instruments [1] | 4-24 hours [1] | High throughput; minimal hands-on time; integrated susceptibility testing | Difficulty with inert or fastidious organisms; database limitations |
| MALDI-TOF MS | Analysis of highly abundant protein profiles (mass/charge ratio) [1] | Minutes from pure colony [1] | Extremely fast; low cost per sample; extensive database | Requires pure culture; limited direct sample application |
| Molecular Methods | Detection of genetic components (DNA/RNA) [1] | <1 hour (direct from sample) [1] | High sensitivity and specificity; can detect non-culturable organisms | Higher cost; requires technical expertise; may detect non-viable organisms |
Application in Contamination Investigation
The choice of identification method depends on the investigation's urgency and required precision. For example:
- Routine Environmental Monitoring: MALDI-TOF MS provides rapid identification of isolates from environmental plates, enabling same-day assessment of contamination significance.
- Sterility Failure Investigation: A combination of methods may be employed, with molecular techniques providing rapid detection and biochemical methods confirming viable organisms.
- Trend Analysis: Automated biochemical systems can provide consistent, reproducible identifications for tracking microbial populations over time.
Experimental Protocols
Protocol: Environmental Sample Collection and Processing
Principle: To aseptically collect environmental samples from predetermined sites and process them for microbial recovery and identification.
Materials:
- Sterile swabs or sponges with neutralizing buffer (e.g., D/E Neutralizing Broth, Letheen Broth) [37]
- Appropriate transport containers
- Culture media: Tryptic Soy Agar (TSA), Sabouraud Dextrose Agar (SDA)
- Incubators (20-25°C and 30-35°C)
Procedure:
- Sample Collection:
- Using sterile technique, remove swab or sponge from transport medium.
- For surfaces, swab a defined area (e.g., 10x10 cm) using a consistent pattern.
- For air monitoring, use settle plates or active air samplers for specified duration.
- Return sample to transport container and maintain chilled (2-8°C) during transport to laboratory.
Sample Processing:
- Aseptically express fluid from sponge or swab into sterile container.
- Inoculate appropriate media:
- TSA for bacterial enumeration (incubate at 30-35°C for 3-5 days)
- SDA for fungal enumeration (incubate at 20-25°C for 5-7 days)
- For pathogen detection, use selective enrichment and isolation procedures.
Interpretation:
- Count colonies and calculate CFU/sample area or volume.
- Compare to established alert and action levels.
- Proceed to identification for action level excursions or objectionable organisms.
Protocol: Microbial Identification via Biochemical Profiling
Principle: To identify microbial isolates based on their metabolic characteristics using conventional or automated biochemical tests.
Materials:
- Pure culture of isolate
- API Identification Strips (bioMérieux) or equivalent
- VITEK 2, Phoenix, or MicroScan automated system
- Incubator (35±2°C)
- Saline solution (0.85% NaCl)
Procedure:
- Isolate Preparation:
- Obtain pure culture by subculturing on non-selective media.
- Prepare suspension in saline to appropriate turbidity standard (e.g., 0.5 McFarland).
Inoculation and Incubation:
- For manual systems: Inoculate each cupule of API strip with bacterial suspension.
- For automated systems: Fill identification card or panel according to manufacturer instructions.
- Incubate at 35±2°C for specified time (4-24 hours depending on system).
Interpretation:
- For manual systems: Add reagents as required and interpret color changes.
- For automated systems: Instrument automatically reads and interprets reactions.
- Compare biochemical profile to database for species identification.
Root Cause Analysis Framework for Contamination Events
When contamination is detected, a structured root cause analysis (RCA) is essential to identify underlying issues and prevent recurrence. The following diagram illustrates the comprehensive workflow for investigating a contamination event, from detection to implementation of preventive measures.
The "5 Whys" Methodology for Root Cause Investigation
The "5 Whys" technique provides a structured approach to drill down from the apparent problem to the fundamental root cause. This iterative questioning process continues until the underlying process or system failure is identified.
Example Application: Repeated Microbial Contamination in Zone 1
1st Why: Why was Staphylococcus epidermidis detected on the filling needle?
- Answer: The aseptic process was compromised during operator intervention.
2nd Why: Why was the aseptic technique compromised?
- Answer: The operator's glove tore during manipulation of the stopper.
3rd Why: Why did the glove tear?
- Answer: The operator's ring punctured the glove material.
4th Why: Why was the operator wearing jewelry in the aseptic area?
- Answer: The gowning procedure and verification process failed to detect the jewelry.
5th Why: Why did the gowning procedure fail?
- Answer: Gowning qualification occurs only annually, and the current procedure lacks a jewelry verification step before entry.
Root Cause: Inadequate gowning procedure and verification process. Winning Solution: Revise gowning procedure to include mandatory jewelry check and implement pre-entry verification by a second qualified individual.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of contamination control strategies requires specific reagents and materials. The following table details essential components for environmental monitoring and microbial identification.
Table: Essential Research Reagents and Materials for Contamination Investigation
| Category | Item | Function/Application | Key Considerations |
|---|---|---|---|
| Sampling Tools | Sterile swabs with neutralizing buffer | Sample collection from small or difficult-to-reach surfaces | Neutralizes common sanitizers; preserves microorganism viability [37] |
| Sterile sponges with handles | Large surface area sampling | Covers approximately 100-1000 cm²; appropriate for floors and walls | |
| Contact plates (RODAC) | Flat surface sampling | Contains appropriate culture media; used for flat, regular surfaces | |
| Culture Media | Tryptic Soy Agar (TSA) | General bacterial enumeration | Supports growth of wide range of bacteria; standard for aerobic plate count |
| Sabouraud Dextrose Agar (SDA) | Fungal enumeration and isolation | Low pH selects for fungi; inhibits bacterial growth | |
| Selective media (MacConkey, MSA) | Isolation of specific microbial groups | Differentiates based on metabolic characteristics; used for screening | |
| Identification Systems | API Biochemical Strips | Manual biochemical identification | Profile-based identification; extensive databases for clinical isolates [1] |
| VITEK 2 / Phoenix / MicroScan | Automated identification and susceptibility | Rapid results (4-24h); high throughput; standardized interpretation [1] | |
| MALDI-TOF MS target plates | Protein profiling for mass spectrometry | Requires pure isolates; extremely rapid identification (minutes) [1] | |
| Molecular Reagents | DNA extraction kits | Nucleic acid purification for molecular methods | Critical for PCR-based identification; removes inhibitors |
| PCR master mixes | Amplification of target genes | Contains enzymes, nucleotides, buffers; standardized for reproducibility | |
| Species-specific primers and probes | Detection and differentiation of target organisms | Designed for conserved gene regions (16S rRNA, gyrB, rpoB) |
Data Analysis and Trending
The ultimate value of an environmental monitoring program is realized through systematic data analysis and trending. The following diagram illustrates the continuous improvement cycle that transforms raw monitoring data into enhanced contamination control.
Key Performance Indicators and Trend Analysis
Effective monitoring programs track specific metrics to assess program effectiveness and identify emerging issues:
- Microbial Recovery Rates: Trend counts by location, zone, and time to establish baselines.
- Identification Profiles: Monitor shifts in microbial flora that may indicate changes in environmental conditions or cleaning effectiveness.
- Alert and Action Level Excursions: Track frequency and patterns to identify deteriorating conditions before they impact product quality.
- Corrective Action Effectiveness: Measure reduction in excursions following implementation of corrective measures.
Contamination control in pharmaceutical manufacturing requires an integrated approach combining systematic environmental monitoring, rapid microbial identification, and structured root cause analysis. The methodologies presented provide a science-based framework for detecting, investigating, and preventing contamination events.
The continuing evolution of microbial identification technologies, particularly the advent of MALDI-TOF MS and molecular methods, has dramatically enhanced our ability to rapidly identify contamination sources and implement targeted corrective actions [1]. When coupled with robust environmental monitoring design and structured investigation protocols, these techniques form a comprehensive contamination control strategy essential for ensuring drug safety and maintaining regulatory compliance.
As manufacturing technologies advance and regulatory expectations evolve, the principles of thorough environmental monitoring, precise contamination tracking, and rigorous root cause analysis remain fundamental to pharmaceutical quality systems. The protocols and frameworks detailed in this application note provide actionable guidance for implementation in research and development environments, manufacturing facilities, and quality control laboratories.
Solving Common Challenges: Ensuring Accuracy in Biochemical Identification
Addressing Database Limitations and Taxonomic Changes
In the field of microbial identification, database limitations and frequent taxonomic changes represent significant obstacles to accurate and reproducible research. The rapid evolution of microbial classification, driven by advanced genomic sequencing, often renders existing databases incomplete or outdated. This is particularly problematic in applied settings such as pharmaceutical development, clinical diagnostics, and food safety testing, where misidentification can lead to severe consequences including treatment failures and product recalls.
The scale of taxonomic reorganization is substantial. Recent updates ratified in 2025 introduced 1 new phylum, 1 class, 4 orders, 33 families, 14 subfamilies, 194 genera, and 995 species of bacterial viruses alone [39]. This dynamic landscape necessitates robust protocols to maintain identification accuracy despite evolving classifications. Furthermore, biochemical testing methods face intrinsic technological limitations including insufficient sensitivity, cross-reactivity issues, and delayed results that complicate their application in modern precision medicine [40].
Quantitative Assessment of Current Limitations
Database Completeness and Classification Accuracy
Recent studies have quantitatively evaluated the performance of various classification methods when handling complex microbial communities. The following table summarizes key performance metrics across different classification approaches:
Table 1: Performance Comparison of Classification Methods for Microbial Identification
| Classification Method | Classification Principle | Reads Classified | Misclassification Rate | RAM Requirements | Key Limitations |
|---|---|---|---|---|---|
| Kaiju | Translation to amino acid sequences with protein-level matching | 76-94% (depending on settings) | ~25% | >200 GB | Database-dependent, high memory requirements |
| Kraken2 | k-mer frequency analysis | 5-51% (depending on confidence thresholds) | ~25% (varies with confidence levels) | >200 GB | Performance highly dependent on confidence thresholds |
| RiboFrame | 16S extraction with Bayesian classification | 3,000-70,000 paired reads | Lowest after MAGs | ~20 GB | Limited to 16S regions, lower classification volume |
| kMetaShot (on MAGs) | k-mer-based classification of assembled genomes | Nearly all MAGs (no threshold) | 0% (at genus level) | 24 GB per thread | Requires quality MAGs, computationally intensive |
Notably, classification accuracy varies dramatically based on the specific methodology and parameters used. Kaiju demonstrates the highest classification rates but still misidentifies approximately 25% of taxa at standard settings. Kraken2 shows extreme sensitivity to confidence thresholds, with classification rates dropping from 51% to 5% as confidence requirements increase [41]. Most significantly, only kMetaShot applied to Metagenome-Assembled Genomes (MAGs) achieved zero misclassification at the genus level, though this approach requires substantial computational resources and quality assemblies [41].
Impact of Database Selection
The choice of reference database profoundly influences identification outcomes:
Table 2: Database Selection Impact on Classification Performance
| Database | Classifier | Classification Rate | Key Issues |
|---|---|---|---|
| nt_core | Kraken2 | 5-51% (depending on confidence) | Moderate classification with significant misidentification |
| SILVA | Kraken2 | <2% of reads | Extremely low classification rates |
| SILVA | RiboFrame | 3,000-70,000 paired reads | Effective for 16S but limited scope |
| nreuk/nreuk+ | Kaiju | 76-94% | Best overall coverage but still has gaps |
Kraken2's performance with the SILVA database exemplifies how database-classifier compatibility dramatically affects outcomes, with classification rates plummeting to less than 2% despite using the same underlying data that RiboFrame successfully utilizes [41]. This highlights the necessity of validating both classifier and database combinations for specific applications.
Experimental Protocols for Validation and Enhancement
Protocol 1: Taxonomic Classification Benchmarking
Purpose: To evaluate and compare the performance of different taxonomic classifiers against a validated mock community.
Materials and Reagents:
- In silico Mock Community: Designed to represent key taxa relevant to your research domain
- Reference Databases: NCBI nt, SILVA, Greengenes, and specialized databases
- Computational Resources: High-performance computing cluster with minimum 200GB RAM
- Classification Software: Kaiju, Kraken2, RiboFrame, and kMetaShot
Methodology:
- Mock Community Design: Create an in silico mock community containing known proportions of target microorganisms, including representation from commonly problematic taxa (e.g., closely related species)
- Sequence Simulation: Generate synthetic sequencing reads (150bp paired-end) mimicking your standard sequencing platform output
- Multi-Tool Classification:
- Process reads through each classifier using standardized parameters
- For Kaiju: Use default parameters with E-value 0.01 and minimal alignment length 11-42
- For Kraken2: Test confidence thresholds from 0.05 to 0.99
- For RiboFrame: Apply both V3-V4 and full-length 16S modes
- MAG-based Classification:
- Assemble reads using MetaBat2 with custom, default, and "metalarge" settings
- Classify resulting MAGs using kMetaShot with confidence thresholds 0, 0.2, and 0.4
- Performance Metrics Calculation:
- Calculate precision, recall, and F1-score for each classifier
- Quantify misclassification rates at genus and species levels
- Identify systematic errors and database gaps
Expected Outcomes: This protocol will identify the optimal classifier-database combination for your specific research context and establish baseline performance metrics for ongoing quality control [41].
Protocol 2: Database Enhancement and Customization
Purpose: To create and validate custom reference databases that address taxonomic gaps and limitations.
Materials and Reagents:
- Reference Genomes: Curated high-quality genomes from NCBI RefSeq and specialized collections
- Sequence Data: Isolate genomes and metagenomes from your target environment
- Bioinformatics Tools: Prokka, CheckM, GTDB-Tk, and custom scripting environments
- Computational Resources: Storage capacity for expanded databases (500GB+)
Methodology:
- Taxonomic Gap Analysis:
- Identify frequently unclassified or misclassified taxa from Protocol 1 results
- Cross-reference with recent taxonomic publications (e.g., ICTV updates [39])
- Reference Sequence Curation:
- Download complete genomes for target taxa from RefSeq and specialized repositories
- Quality filter using CheckM (>90% completeness, <5% contamination)
- Annotate using Prokka with standardized parameters
- Custom Database Construction:
- For protein-based classifiers: Extract protein sequences from annotated genomes
- For k-mer-based classifiers: Build custom k-mer indices incorporating new references
- For 16S-based methods: Extract 16S sequences from quality-filtered genomes
- Validation and Integration:
- Test custom database performance against mock communities
- Compare with standard databases using statistical measures
- Implement version control for database tracking and updates
Expected Outcomes: A customized reference database with improved coverage of taxa relevant to your research focus, resulting in enhanced classification accuracy for target microorganisms [41] [42].
Visualization of Taxonomic Classification Workflow
Figure 1: Comprehensive Workflow for Addressing Database Limitations in Microbial Identification
Table 3: Key Research Reagent Solutions for Microbial Identification and Database Enhancement
| Reagent/Resource | Function | Application Notes |
|---|---|---|
| Mock Community Standards | Validation and benchmarking of classification methods | Should include taxa relevant to research focus; can be commercial or custom-designed |
| Reference Databases | Taxonomic classification reference | NCBI nt, SILVA, Greengenes; requires regular updating and version control |
| Quality Control Tools | Assessment of sequence and assembly quality | CheckM for MAG quality; FastQC for sequence quality; QUAST for assembly evaluation |
| Bioinformatics Pipelines | Automated classification and analysis | QIIME 2 for 16S data; custom workflows for WGS; standardized parameters essential |
| Computational Resources | High-performance computing infrastructure | 200GB+ RAM for classification; large storage for databases; version control systems |
| Taxonomic Update Services | Tracking nomenclatural changes | Subscription to ICTV updates; GTDB monitoring; automated alert systems |
| Custom Database Tools | Specialized reference construction | Prokka for annotation; Kraken2-build for custom indices; manual curation interfaces |
Implementation Framework for Pharmaceutical Applications
For drug development professionals, implementing a systematic approach to addressing taxonomic challenges is critical for regulatory compliance and research reproducibility. We recommend:
1. Database Management Protocol:
- Maintain version-controlled reference databases with documented update schedules
- Implement quarterly reviews of taxonomic updates from authoritative sources
- Establish custom database curation for pathogen-specific research programs
2. Quality Assurance Framework:
- Regular benchmarking using mock communities relevant to your research focus
- Cross-validation of identification results across multiple classification methods
- Documentation of classifier parameters and performance metrics for regulatory submissions
3. Technology Integration Strategy:
- Leverage emerging technologies like machine learning approaches that show promise for rapid identification [43]
- Implement complementary methods (e.g., MALDI-TOF confirmation of genomic identifications)
- Develop standardized operating procedures that accommodate taxonomic changes without protocol revisions
The integration of these approaches creates a robust foundation for microbial identification that remains accurate despite the evolving taxonomic landscape, ensuring reliable results throughout the drug development pipeline from discovery through quality control.
Accurate microbial identification is a cornerstone of diagnostic microbiology, infectious disease control, and drug development. However, distinguishing between closely related species remains a significant challenge, as they often exhibit minimal phenotypic differences while potentially possessing critical variations in pathogenicity, virulence, and antifungal susceptibility [44]. Traditional methods relying solely on morphological or biochemical characteristics frequently fail to resolve these complex taxonomic relationships. The polyphasic approach addresses these limitations by integrating data from multiple methodologies—genotypic, phylogenetic, and phenotypic—into a consensus classification system, thereby providing a more robust and accurate identification framework [45]. This holistic strategy is particularly vital in clinical and pharmaceutical settings, where misidentification can directly impact patient outcomes and drug development pipelines.
Core Methodologies in the Polyphasic Approach
The strength of the polyphasic approach lies in the synergistic use of diverse techniques. The following section details the core methodologies, providing a foundational understanding for researchers.
Phenotypic and Biochemical Analyses
Phenotypic characterization forms the traditional basis of microbial identification and remains a valuable first step in the polyphasic workflow.
- Morphological Characteristics: Colony morphology (texture, color, growth rate) and microscopic features (spore-forming structures, hyphal appearance) are examined. Standardized culture conditions on media like Sabouraud dextrose agar or Harold's agar are crucial for consistency, as these traits can be influenced by environmental factors [44] [45]. Staining techniques, such as Gram stain or differential interference contrast microscopy, are used to enhance structural visualization without killing cells [5] [45].
- Biochemical and Physiological Profiling: These tests analyze the metabolic capabilities of a microbe, which are dictated by its unique enzymatic profile [3]. Simple, rapid tests can yield presumptive identification:
- Catalase Test: Distinguishes catalase-positive bacteria (e.g., Staphylococci, E. coli) from catalase-negative ones (e.g., Streptococcus) by detecting bubble formation upon addition of hydrogen peroxide [5] [3].
- Oxidase Test: Identifies bacteria with cytochrome c oxidase activity (e.g., Pseudomonas) through a color change of the reagent to purple [3].
- Substrate Utilization Tests: Commercial panels containing various carbon or nitrogen sources are inoculated with the unknown microbe. Identification is based on unique patterns of color changes induced in the separate panels, indicating substrate use [5] [3].
Molecular and Chemotaxonomic Analyses
Molecular and chemotaxonomic techniques provide a higher resolution for differentiating genetically close species.
- Genetic Markers and Multilocus Sequence Analysis (MLSA): DNA sequencing has revolutionized fungal taxonomy. The Internal Transcribed Spacer (ITS) region is the primary barcode for fungi, while protein-coding genes like beta-tubulin (BT) offer additional resolution for complex clades [44] [45]. Multilocus Sequence Analysis (MLSA), which uses multiple genetic loci, is a practical and powerful method for phylogenetic analysis and clarifying species boundaries [44] [45].
- Mass Spectrometry for Protein Profiling: Matrix-Assisted Laser Desorption/Ionization Time-of-Flight (MALDI-TOF) Mass Spectrometry is a reliable, high-throughput alternative to DNA-based methods. It generates unique protein spectral fingerprints, primarily from ribosomal proteins in the 2–20 kDa range, which serve as biotaxonomic markers [44] [45]. This technique has demonstrated high accuracy in identifying yeasts (e.g., Candida, Cryptococcus) and, with robust databases, is increasingly effective for molds and dermatophytes [45].
Table 1: Key Methodologies in a Polyphasic Identification Workflow
| Method Category | Specific Technique | Primary Application/Principle | Key Advantage |
|---|---|---|---|
| Morphological | Macroscopic colony observation | Analysis of color, texture, and growth on specific media [44] | Low cost; provides initial diagnostic clues |
| Microscopic examination (e.g., light microscopy) | Analysis of cellular and spore structures [45] | Reveals structural characteristics | |
| Biochemical | Catalase Test | Detects catalase enzyme activity [5] [3] | Rapid, simple test for Gram-positive cocci differentiation |
| Oxidase Test | Detects cytochrome c oxidase enzyme [3] | Differentiates between bacterial groups (e.g., Pseudomonas vs. Enterobacteriaceae) | |
| Substrate Utilization Assays | Profiles metabolic capabilities using diverse substrates [5] | Provides a broad phenotypic profile | |
| Molecular | ITS Sequencing | Primary DNA barcode for fungal identification [44] [45] | Highly versatile; extensive reference databases |
| Beta-tubulin (BT) Gene Sequencing | Secondary marker for higher resolution in complexes [44] | Helps resolve closely related species | |
| Chemotaxonomic | MALDI-TOF Mass Spectrometry | Generates species-specific protein fingerprints [44] [45] | High-throughput and rapid identification |
Experimental Protocol: A Practical Workflow for Fungal Species Complex Delineation
This protocol outlines a structured, polyphasic strategy for differentiating closely related fungal species, using the Trichophyton benhamiae complex as a model [44].
Sample Preparation and Morphological Analysis
- Strain Cultivation: Inoculate test strains onto diluted Sabouraud dextrose agar (S10) and Harold's agar (M40Y). Incubate at 25°C for 7–21 days to ensure adequate growth [44].
- Macroscopic Analysis: Document colony characteristics, including pigmentation (e.g., "white" vs. "yellow" morphotypes), texture, and growth rate.
- Microscopic Analysis: Using light microscopy, examine the microscopic morphology, such as hyphal structures, conidia production, and other reproductive features.
DNA Extraction and Multi-Gene Phylogenetic Analysis
- DNA Extraction: Harvest mycelia from cultures grown in Sabouraud dextrose broth. Perform genomic DNA extraction using a commercial kit, incorporating a lyophilization and bead-beating step for efficient cell wall disruption. Extend the lysis time to >2 hours to ensure yield [44].
- PCR Amplification: Amplify target genetic loci using polymerase chain reaction (PCR).
- Sequencing and Phylogeny: Purify PCR amplicons and perform Sanger sequencing. Assemble consensus sequences and align them with reference sequences using software like MAFFT. Construct a Maximum Likelihood (ML) phylogeny using a tool like IQ-TREE, with branch support calculated from 1000 bootstrap replicates. The dataset should be partitioned (e.g., ITS1+ITS2, 5.8S+28S, BT introns, BT exons) with the best-fit model for each partition [44].
Chemotaxonomic Identification via MALDI-TOF MS
- Protein Extraction: Culture strains on agar plates for 3-5 days. Subject a bacterial scraping to a protein extraction protocol involving ethanol precipitation and formic acid/acetonitrile extraction [44].
- Spectral Acquisition: Analyze the protein extract using a MALDI-TOF mass spectrometer (e.g., Microflex LT, Bruker Daltonics) with default settings to acquire mass spectra [44].
- Database Matching and Analysis: Compare the resulting main spectrum profile (MSP) against a commercial or in-house reference database for identification. Closely related sister clades may exhibit similar spectra and require phylogenetic data for definitive resolution [44].
Data Integration and Interpretation
Correlate the results from all three methodologies. The phylogenetic analysis will define monophyletic clades, while MALDI-TOF and morphological data will provide distinguishing characteristics. For example, genetically distinct clades may be confirmed as separate species if supported by spectral or phenotypic differences, whereas morphotypes without genetic divergence (e.g., T. benhamiae "white" and "yellow") are consolidated into a single species [44].
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of the polyphasic approach relies on specific reagents, kits, and instrumentation. The following table details key solutions for the protocols described.
Table 2: Essential Research Reagents and Kits for Polyphasic Identification
| Item | Function/Application | Specific Example/Note |
|---|---|---|
| Selective & Differential Media | Supports growth of target organisms while inhibiting others; allows visual differentiation based on metabolic traits [5]. | Sabouraud Dextrose Agar (fungi), Mannitol Salt Agar (Staphylococci), MacConkey Agar (enteric bacteria) [5]. |
| DNA Extraction Kit | Purifies high-quality genomic DNA from microbial cultures for subsequent PCR and sequencing. | Kits with bead-beating step and extended lysis for robust fungal cell wall disruption (e.g., Invisorb Spin Plant Mini Kit) [44]. |
| PCR Reagent Master Mix | Amplifies target genetic loci (e.g., ITS, beta-tubulin) for phylogenetic analysis. | Requires primers specific to the microbial group (e.g., ITS5/ITS4 for fungi) [44]. |
| Sanger Sequencing Kit | Determines the nucleotide sequence of PCR amplicons. | Essential for generating data for multilocus sequence analysis (MLSA). |
| MALDI-TOF MS System | Generates protein spectral fingerprints for rapid identification by matching against a reference database [44] [45]. | Commercial systems like MALDI Biotyper (Bruker), VITEK MS (bioMérieux) [45]. |
| MALDI Matrix Solution | A chemical compound (e.g., α-cyano-4-hydroxycinnamic acid) that enables soft ionization of protein samples for TOF analysis. | Critical component for preparing samples for MALDI-TOF MS. |
| Protein Extraction Reagents | Chemicals used to isolate and purify proteins from microbial cells for mass spectrometry. | Typically involves ethanol, formic acid, and acetonitrile [44]. |
The polyphasic approach, integrating genotypic, phenotypic, and chemotaxonomic data, is the definitive standard for differentiating closely related microbial species. This comprehensive framework overcomes the limitations of any single method, providing the resolution needed to clarify species boundaries in complex groups, as demonstrated with the T. benhamiae complex. For researchers and drug development professionals, adopting this multifaceted strategy is critical for accurate pathogen identification, which in turn informs epidemiological tracking, antifungal stewardship, and the development of targeted therapeutics. As technology advances, the continued refinement and integration of these techniques will further solidify the polyphasic approach as the cornerstone of modern microbial systematics and diagnostics.
Within microbial identification, fastidious bacteria and weak reactors present a significant challenge to researchers and drug development professionals. Fastidious organisms possess complex nutritional requirements and often exhibit slow growth, failing to prosper in standard laboratory media [46]. Similarly, weak reactors yield subdued or ambiguous results in conventional biochemical tests, complicating definitive identification. These challenges directly impact the accuracy and efficiency of microbial research and diagnostic outcomes.
The increasing global infectious disease burden, including pathogens like Haemophilus influenzae and Neisseria meningitidis, underscores the need for precise identification methods [47] [48]. This document provides detailed application notes and protocols to advance research on these complex microorganisms within the broader context of biochemical test-based microbial identification.
Core Challenges and Key Organisms
Fastidious bacteria require specific growth factors or conditions not present in basic media. Legionella pneumophila, for instance, needs cysteine and iron, while Haemophilus species require X (hemin) and V (NAD) factors [46] [48]. Weak reactors, such as some Neisseria species, produce minimal acidic products in fermentation tests, leading to faint color changes that are easily misinterpreted [48].
The table below summarizes common fastidious bacteria and their specific growth requirements which are frequently implicated in human disease.
Table 1: Fastidious Bacteria of Clinical and Research Importance
| Bacterium | Growth Requirements / Fastidious Nature | Associated Diseases | Identification Challenges |
|---|---|---|---|
| Haemophilus influenzae | Requires both X factor (hemin) and V factor (NAD) [48]. | Meningitis, pneumonia, epiglottitis [46]. | Differentiation from other Haemophilus spp. based on factor requirements [48]. |
| Legionella pneumophila | Requires cysteine and iron; does not grow on common media [46]. | Legionnaires' disease, Pontiac fever [46]. | Demanding culture conditions; often requires molecular methods or biosensors for detection [46]. |
| Neisseria gonorrhoeae | Capnophile, requires chocolate agar or supplemented media [48]. | Gonorrhea, pelvic inflammatory disease [48]. | Weak carbohydrate fermentation reactions; requires pure culture and specific tests (CTA) [48]. |
| Brucella species | Slow growth (2-4 weeks), requires CO~2~ [49] [46]. | Brucellosis, undulant fever [49]. | High-risk aerosol potential; culture is "logistically demanding" and lacking timeliness [49]. |
| Helicobacter pylori | Microaerophilic, requires rich media and long incubation [46]. | Peptic ulcers, gastric cancer [46]. | Difficult to culture from clinical specimens; often diagnosed via non-culture methods (e.g., urea breath test) [46]. |
| Mycobacterium tuberculosis | Slow growth (3-8 weeks on Löwenstein-Jensen media) [46]. | Tuberculosis [46] [47]. | Extremely slow doubling time; requires biosafety level 3 facilities [46]. |
Experimental Protocols for Biochemical Identification
X and V Factor Test forHaemophilusSpecies
Principle: This test differentiates Haemophilus species based on their specific requirement for hemin (X factor) and/or nicotinamide adenine dinucleotide (V factor) for growth [48].
Materials:
- Pure culture of the isolate (e.g., on chocolate agar).
- Trypticase soy agar or Mueller-Hinton agar plates.
- Sterile filter paper disks impregnated with X factor, V factor, and a combined XV factor.
- Sterile forceps.
- Incubator (35–37°C, 5–10% CO~2~).
Procedure:
- Using a sterile loop, create a lawn of the test organism on a trypticase soy agar plate.
- Aseptically place the X, V, and XV factor disks on the inoculated surface, spaced adequately apart.
- Gently press the disks to ensure firm contact with the agar.
- Incubate the plate at 35–37°C in 5–10% CO~2~ for 18–24 hours.
- Observe for growth around the disks.
Interpretation:
- Growth only around the XV disk: Identifies H. influenzae (requires both factors) [48].
- Growth around the V and XV disks: Identifies H. parainfluenzae (requires only V factor) [48].
- Growth around the X and XV disks: Suggests H. ducreyi (requires only X factor) [48].
- Growth around all disks is not typical for Haemophilus and may indicate a contaminant.
Troubleshooting: Ensure the use of a pure culture. If growth is confluent across the plate, the medium may be contaminated with V factor (NAD). Use a defined, unsupplemented medium base [48].
Carbohydrate Utilization Test forNeisseriaSpecies
Principle: This test differentiates Neisseria species based on their ability to ferment specific carbohydrates, producing acid. The acid production is detected by a color change in a pH indicator [48].
Materials:
- Cystine Trypticase Agar (CTA) base with carbohydrates.
- Sterile carbohydrate solutions (e.g., glucose, maltose, lactose, sucrose).
- pH indicator (e.g., phenol red).
- Sterile test tubes or slants.
- Incubator (35–37°C).
Procedure:
- Prepare CTA carbohydrate slants by adding a specific, filter-sterilized carbohydrate solution to the CTA base.
- Inoculate each slant heavily with a pure culture of the organism from an 18–24 hour culture.
- Incubate the slants at 35–37°C in ambient air for 18–24 hours. Observe for weak reactions at 48 hours.
- Observe the color of the medium. A change from red to yellow indicates acid production (positive).
Interpretation:
Troubleshooting: Use a heavy inoculum from a fresh culture (18–24 hours old). Weak or delayed reactions are common; extend incubation and compare against a control (CTA base without carbohydrate). Ensure test is performed on a pure culture [48].
Catalase Test
Principle: Tests for the presence of the catalase enzyme, which breaks down hydrogen peroxide into water and oxygen gas [50].
- Procedure:
- Place 1–2 drops of 3% hydrogen peroxide (H~2~O~2~) on a glass slide.
- Add a loopful of a single bacterial species from a fresh culture to the drop.
- Immediate and vigorous bubbling indicates a positive test [50].
Oxidase Test
Principle: Used to determine if a bacterium possesses the enzyme cytochrome c oxidase [50].
- Procedure:
- Smear bacteria from a fresh plate onto a sterile cotton swab.
- Add 1–2 drops of oxidase reagent (e.g., tetramethyl-p-phenylenediamine dihydrochloride) onto the swab.
- A color change to dark blue or purple within 10–30 seconds indicates a positive result [50].
The Scientist's Toolkit: Research Reagent Solutions
Successful identification of fastidious organisms and weak reactors depends on specific, high-quality reagents.
Table 2: Essential Research Reagents for Biochemical Identification
| Reagent / Material | Function / Principle | Example Application |
|---|---|---|
| X & V Factor Disks | Provides essential growth factors (Hemin and NAD) to support the growth of fastidious bacteria. | Differentiation of Haemophilus species (e.g., H. influenzae vs. H. parainfluenzae) [48]. |
| Cystine Trypticase Agar (CTA) | A semi-solid medium used to prepare carbohydrate utilization slants. Supports growth while allowing fermentation detection. | Carbohydrate fermentation tests for Neisseria and other fastidious genera [48]. |
| Hydrogen Peroxide (3%) | Substrate for the catalase enzyme. Breakdown produces oxygen bubbles in a positive test. | Differentiation of staphylococci (catalase-positive) from streptococci (catalase-negative) [50]. |
| Oxidase Reagent | Electron donor for cytochrome c oxidase. Oxidized form is colored (blue/purple). | Differentiation of Pseudomonas (oxidase-positive) from members of Enterobacteriaceae (oxidase-negative) [50]. |
| Selective & Enriched Media | Contains specific nutrients (e.g., blood, vitamins) and/or inhibitors to selectively isolate target organisms. | Chocolate agar for Haemophilus and Neisseria; Buffered Charcoal Yeast Extract (BCYE) agar for Legionella [46] [48]. |
Quantitative Data Analysis and Interpretation
For quantitative molecular methods like qPCR, precision is paramount. The Coefficient of Variation (CV), calculated as (Standard Deviation / Mean) × 100%, is a key metric for precision [51]. A lower CV indicates more consistent and reproducible results, which is critical for accurately discriminating small changes in gene copy numbers or pathogen load.
Table 3: Key Statistical Values for Quantitative Assay Analysis
| Statistical Term | Definition | Role in Quantitative Analysis |
|---|---|---|
| Coefficient of Variation (CV) | The ratio of the standard deviation to the mean, expressed as a percentage. | Primary measure of precision or reproducibility. A low CV is essential for reliable results [51]. |
| Standard Deviation (SD) | A measure of the amount of variation or dispersion of a set of values. | Describes the spread of replicate data points around the mean [51]. |
| Standard Error (SE) | The standard deviation of the sampling distribution of a statistic, most commonly the mean. | Provides confidence boundaries for how close the sample mean is to the true population mean [51]. |
| Technical Replicates | Multiple measurements of the same sample aliquot. | Helps estimate and reduce system-level variation (e.g., from pipetting or instrument noise) [51]. |
| Biological Replicates | Measurements from different samples within the same test group. | Accounts for the natural biological variation within a population [51]. |
Integrated Workflow for Identification
The identification of difficult organisms is a systematic process that integrates phenotypic, biochemical, and increasingly, genotypic methods. The workflow below outlines a logical pathway from initial isolation to final confirmation.
Figure 1: A stepwise workflow for identifying difficult organisms, culminating in advanced methods for definitive confirmation.
Advanced Techniques and Future Directions
When conventional biochemical tests are inconclusive, advanced technologies provide definitive species-level identification.
- MALDI-TOF Mass Spectrometry rapidly identifies microorganisms by comparing their unique protein fingerprints to a reference library. It demonstrates better accuracy for stressed environmental strains and provides consistent results that reduce operator variability compared to traditional methods [52].
- Genomic Sequencing (e.g., Whole Genome Sequencing - WGS) serves as the ultimate tool when other methods fail, providing a complete genetic profile for definitive identification [52]. Protein-coding gene sequencing can differentiate closely related species that ribosomal RNA-based methods cannot reliably separate (e.g., within the Bacillus cereus group) [52].
- Biosensors represent a cutting-edge frontier, especially for fastidious pathogens. These devices integrate a biological recognition system with a transducer to convert a biochemical signal into a measurable output. Nanomaterial-based biosensors are being developed for direct detection of pathogens like Legionella pneumophila and Mycobacterium tuberculosis, offering potential for rapid, sensitive, and point-of-care diagnostics that bypass the need for culture [46].
The World Health Organization (WHO) emphasizes the urgent need for affordable, robust, and easy-to-use diagnostic platforms, including "sample-in/result-out" systems designed for use in low-resource settings [53]. The continued development and integration of these advanced techniques are crucial for addressing the global challenges posed by antimicrobial resistance and emerging infectious diseases.
Best Practices for Sample Preparation, Inoculation, and Incubation
In the field of microbiological research, particularly within the scope of microbial identification using biochemical tests, the reliability of experimental outcomes is fundamentally dependent on the initial steps of sample preparation, inoculation, and incubation. These foundational procedures determine the viability, purity, and metabolic state of microbial cultures, which directly influences the accuracy and reproducibility of subsequent biochemical analyses [1]. This application note provides detailed, actionable protocols designed for researchers, scientists, and drug development professionals, framing these core techniques within the context of a rigorous microbial identification workflow. Adherence to these standardized practices is crucial for generating high-quality, comparable data across experiments and laboratories, thereby strengthening the validity of research findings.
Materials and Reagent Solutions
The following table catalogs the essential reagents and materials required for the procedures outlined in this document.
Table 1: Research Reagent Solutions and Essential Materials
| Item Name | Function/Application | Key Details |
|---|---|---|
| Luria-Bertani (LB) Broth/Agar | A nutrient-rich medium for the general growth and maintenance of bacteria [54]. | Typically contains tryptone, yeast extract, and NaCl. Can be used as a liquid broth or solidified with agar for plates [54]. |
| Antibiotic Stock Solutions | Selective pressure to maintain plasmids and ensure growth of only the desired microbial strain [54]. | Prepared as 1000X concentrates (e.g., 100 mg/mL ampicillin) and stored at -20°C. Working concentration for media is 1:1000 dilution [54]. |
| Hydrogen Peroxide (3%) | Substrate for the catalase test, a key biochemical assay for microbial identification [55] [3]. | Used to detect the presence of catalase enzyme. Must be fresh and stored properly to avoid decomposition and false negatives [55]. |
| Tetramethyl-p-phenylenediamine-dihydrochloride | Reagent for the oxidase test, which identifies cytochrome c oxidase activity [55] [3]. | Oxidizes to a dark purple compound in the presence of the oxidase enzyme. Solutions should be prepared fresh [55]. |
| Glycerol | Cryoprotectant for the long-term storage of bacterial strains [54]. | Used to prepare glycerol stocks for storage at -80°C, preserving strain viability. |
Protocols for Sample Preparation and Inoculation
Preparation of Culture Media
Luria-Bertani (LB) Broth Protocol:
- Weighing: For 400 mL of LB broth, weigh out 4 g of NaCl, 4 g of Tryptone, and 2 g of Yeast Extract into a 500 mL glass bottle [54].
- Dissolution: Add deionized water (dH₂O) to a total volume of 400 mL and mix until all components are fully dissolved [54].
- Sterilization: Loosely cap the bottle (do not tighten completely to prevent pressure buildup) and cover the top with aluminum foil. Sterilize by autoclaving. After autoclaving, allow the medium to cool to room temperature before tightening the cap. Sterilized LB broth can be stored at room temperature [54].
Antibiotic Supplementation: Antibiotics are heat-labile and must be added to the medium only after it has been autoclaved and has cooled to at least room temperature, preferably to around 55°C for agar plates [54].
- Procedure: Aseptically add the appropriate volume of antibiotic stock solution to achieve the desired working concentration. For example, to prepare 100 mL of LB with ampicillin, add 100 µL of a 100 mg/mL ampicillin stock solution [54].
Table 2: Common Antibiotic Working Concentrations
| Antibiotic | Typical Working Concentration |
|---|---|
| Ampicillin | 100 µg/mL |
| Kanamycin | 50 µg/mL |
| Chloramphenicol | 25 µg/mL |
| Tetracycline | 10 µg/mL |
Inoculation Techniques
Inoculating a Liquid Culture from an Agar Plate:
- Preparation: Dispense sterile liquid LB medium, supplemented with the appropriate antibiotic, into a sterile culture tube or flask [54].
- Selection: Using a sterile pipette tip or a sterile toothpick, gently touch a single, well-isolated bacterial colony from a fresh agar plate [54].
- Inoculation:
- Aeration: Loosely cover the culture vessel with a sterile cap (not airtight), sterile aluminum foil, or use a vented closure to ensure adequate aeration during incubation [54].
Incubation Conditions and Growth Analysis
Standard Incubation Parameters
- Temperature: The standard incubation temperature for many common bacteria, such as E. coli, is 37°C [54]. Some plasmids or bacterial strains may require lower temperatures (e.g., 30°C) for stable propagation, which will result in slower growth and necessitate longer incubation times [54].
- Aeration: Cultures must be incubated with vigorous shaking (150-250 rpm) in a shaking incubator to ensure proper aeration, which is critical for achieving high cell densities [54].
- Duration: Typical incubation for an overnight culture lasts 12-18 hours [54]. The optimal density is often in the stationary phase. Growth for longer periods (e.g., 18-30 hours) may be required for cultures with low copy number plasmids or those incubated at lower temperatures [54].
Assessing Culture Growth
After incubation, successful growth is indicated by a visible cloudy haze in the medium [54]. It is essential to include a negative control (e.g., LB media with antibiotic but without inoculated bacteria) which should remain clear [54]. For protocols requiring bacteria in a specific growth phase (e.g., log phase), the culture density must be measured quantitatively using a spectrophotometer to determine the Optical Density at 600 nm (OD₆₀₀) [54].
Foundational Biochemical Tests for Microbial Identification
Following successful culture, biochemical tests are employed for preliminary microbial identification. These tests leverage the unique enzymatic profiles of different bacteria [55] [3].
Catalase Test Protocol
Principle: This test identifies the presence of the catalase enzyme, which breaks down toxic hydrogen peroxide into water and oxygen. It is a key test for differentiating bacterial genera, such as Staphylococcus (catalase-positive) from Streptococcus (catalase-negative) [55] [3].
Procedure:
- Using a wooden applicator (to avoid false positives from metal loops), transfer a small amount of a microbial colony to the surface of a clean glass slide [55].
- Immediately add a few drops of 3% hydrogen peroxide to the sample on the slide and observe [55].
Analysis:
- Positive Test: The rapid evolution of oxygen gas bubbles [55] [3].
- Negative Test: An absence of, or very few, bubbles [55].
Oxidase Test Protocol
Principle: This test detects the presence of cytochrome c oxidase, an enzyme in the electron transport chain of aerobic bacteria. It helps distinguish between bacterial groups, such as Pseudomonas (oxidase-positive) and Escherichia coli (oxidase-negative) [55] [3].
Procedure (Filter Paper Method):
- Place a piece of filter paper in a sterile Petri dish and add a few drops of a fresh 1% tetramethyl-p-phenylenediamine-dihydrochloride solution to moisten it [55].
- Using a wooden applicator, smear a small amount of a young (<24 hour old) colony onto the moistened filter paper [55].
Analysis:
- Positive Test: Development of a dark purple color within 10-20 seconds [55].
- Negative Test: No color change, or a color change after 60 seconds or more [55].
Workflow Integration and Troubleshooting
The following diagram illustrates the complete integrated workflow from sample preparation to identification, highlighting the critical decision points.
Workflow for Microbial Culture and Identification
Troubleshooting Common Issues
Table 3: Troubleshooting Guide for Culture Preparation
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| No growth after overnight incubation | Incorrect antibiotic used; Old stock culture; Insufficient aeration. | Verify antibiotic resistance marker on plasmid matches the antibiotic in media [54]. Streak bacteria on a fresh agar plate before inoculating liquid culture [54]. Ensure loose covering and adequate shaking speed (can increase to 350-400 rpm for higher density) [54]. |
| Poor or slow growth | Low incubation temperature; Low copy number plasmid. | Extend incubation time, especially for cultures at 30°C [54]. For low copy number plasmids, incubate for 18-30 hours [54]. |
| Inconclusive Biochemical Test Results | Old hydrogen peroxide reagent; Use of metal loop for catalase test; Delayed reading of oxidase test. | Use a freshly prepared hydrogen peroxide solution [55]. Use wooden applicators for the catalase test [55]. Read oxidase test results within 10-20 seconds to avoid false positives [55]. |
Validation, Compliance, and the Evolving Diagnostic Landscape
The validation of alternative microbiological methods is a critical process for pharmaceutical manufacturers and researchers aiming to implement rapid, automated, and sensitive technologies. These methods, which can include molecular techniques, viability staining, and automated identification systems, offer significant advantages over traditional culture-based approaches, such as reduced time-to-result and increased accuracy [56]. The primary regulatory guidance governing this field in the United States and Europe is found in United States Pharmacopeia (USP) General Chapter <1223> and European Pharmacopoeia (Ph. Eur.) Chapter 5.1.6 [56] [57]. Both chapters provide a framework to ensure that any alternative method is validated to be at least equivalent to the compendial method it intends to replace. A thorough understanding of these frameworks is essential for successfully validating methods used in microbial identification, enumeration, and detection within pharmaceutical quality control and drug development [58] [59].
For research centered on microbial identification using biochemical tests, these guidelines ensure that new or alternative identification methods, whether based on enzymatic profiles or genotypic characteristics, are fit for their intended purpose [58]. The core principle is that an alternative method must be shown to be non-inferior to the traditional method through a structured validation process [56] [60]. It is noteworthy that recent revisions to both USP <1223> and Ph. Eur. 5.1.6 have made these chapters more flexible and aligned with modern technological capabilities, emphasizing a risk-based approach and the importance of user requirements [56] [57].
Comparative Analysis of Validation Parameters
The validation parameters required by USP <1223> and Ph. Eur. 5.1.6 vary depending on whether the alternative method is qualitative, quantitative, or used for identification. The following tables provide a structured comparison of these parameters for qualitative and quantitative tests.
Table 1: Validation Parameters for Qualitative Microbiological Tests (e.g., Sterility Test)
| Validation Parameter | USP <1223> Requirement | Ph. Eur. 5.1.6 Requirement |
|---|---|---|
| Specificity | Ability to detect a range of relevant microorganisms; assures no interference from the test article [60]. | Focuses on the method's ability to distinguish between different microorganisms, with enhanced guidance for identification methods and databases [57]. |
| Limit of Detection (LOD) | The lowest number of microorganisms that can be detected. Demonstrated by inoculating with a low number of CFU (≤5 per unit) and comparing recovery rates to the compendial method using statistical tests like Chi-square [60]. | The lowest number of microorganisms that can be detected under stated conditions. The revised chapter provides additional detail on establishing LOD for different types of tests [57]. |
| Ruggedness | Degree of reproducibility under a variety of normal conditions (e.g., different analysts, instruments). Often determined by the method supplier [60]. | Considered part of the validation to ensure reliability across different operational and environmental variables [57]. |
| Robustness | Capacity to remain unaffected by small, deliberate variations in method parameters. A measure of reliability during normal usage [60]. | A measure of the method's capacity to remain unaffected by small variations in parameters, ensuring reliability [57]. |
Table 2: Validation Parameters for Quantitative Microbiological Tests (e.g., Microbial Enumeration)
| Validation Parameter | USP <1223> Requirement | Ph. Eur. 5.1.6 Requirement |
|---|---|---|
| Accuracy | Closeness of test results to the value from the traditional method. Expressed as percentage recovery (should be ≥70%) or via statistical analysis (e.g., ANOVA on log-transformed data) [60]. | Addressed under primary validation. The method must demonstrate acceptable accuracy across its operational range [57]. |
| Precision | The degree of agreement among repeated test results across the operational range. Expressed as standard deviation or relative standard deviation [60]. | The degree of agreement among individual test results from repeated samplings. Part of primary validation for quantitative methods [57]. |
| Linearity & Range | The operational range should overlap with the traditional method. Demonstrated by testing at least 5 suspensions of microorganisms across the range (e.g., 10² to 10⁶ CFU/mL) [60]. | The method must be validated over a specified range, which is established during primary validation [57]. |
| Specificity | Ensures the method detects the target microorganism without interference from the product or other components [60]. | The method should correctly identify and/or quantify the target microorganism in the presence of other components [57]. |
| Limit of Quantification (LOQ) | The lowest number of microorganisms that can be accurately quantified [60]. | The lowest number of microorganisms that can be quantified with acceptable accuracy and precision [57]. |
A pivotal concept in USP <1223> is the critical reconsideration of the Colony-Forming Unit (CFU). The chapter notes that the CFU can underestimate the true microbial count due to factors like microbial stress states, sampling techniques, and the inability of some cells to form colonies under standard growth conditions [56]. Therefore, a higher count from an alternative method does not necessarily indicate a greater product risk, provided the method has been validated as equivalent or non-inferior to the referee method in assessing microbiological safety [56]. Ph. Eur. 5.1.6 similarly acknowledges that alternative methods, particularly genotypic ones for identification, can be more accurate and precise than traditional biochemical and phenotypic methods [57].
Experimental Protocols for Validation
Protocol 1: Equivalency Study for a Qualitative Method
This protocol outlines the procedure for validating an alternative qualitative method, such as a rapid sterility test, against the compendial method.
1. Experimental Design:
- A comparative study is designed using samples inoculated with a low level (typically not more than 5 CFU per unit) of appropriate challenge microorganisms [60].
- The panel of microorganisms should reflect the required specificity and include representative gram-positive and gram-negative bacteria, yeast, and mold, some of which may be in a stressed state [58].
- A minimum of five replicates per challenge organism is recommended to account for microbiological variability [60].
2. Sample Preparation and Inoculation:
- Prepare the product sample according to standard methodology. For a sterility test, this would involve filtering the product through a membrane filter as per compendial procedures [60].
- Inoculate the sample with a calibrated suspension of the challenge organism. The inoculation level should be adjusted so that approximately 50% of the samples tested by the compendial method show growth, ensuring a challenge near the method's detection limit [60].
3. Parallel Testing:
- Test the inoculated samples in parallel using both the compendial method (e.g., incubation in fluid thioglycollate medium and soybean-casein digest broth) and the alternative method (e.g., a rapid detection system based on autofluorescence or ATP bioluminescence) [56] [60].
- Include appropriate negative controls (non-inoculated samples) to confirm the sterility of the test materials and media.
4. Data Analysis and Equivalency Determination:
- Record the presence or absence of growth in each system.
- Analyze the data using non-parametric statistical methods, such as the Chi-square test, to compare the proportion of positive results obtained by the two methods [60].
- The alternative method is considered equivalent if there is no statistically significant difference in its ability to detect microbial presence at the defined limit of detection.
Protocol 2: Equivalency Study for a Quantitative Method
This protocol describes the process for validating an alternative quantitative method, such as a rapid enumeration system, against the traditional plate count.
1. Experimental Design and Operational Range:
- Define the operational range of the alternative method, which must overlap with that of the traditional plate count (e.g., 10² to 10⁶ CFU/mL) [60].
- Prepare a series of at least five serial dilutions of a microbial suspension across this defined range [60].
2. Parallel Testing and Replication:
- For each dilution level, analyze multiple replicates (e.g., n=3 or more) using both the alternative method and the compendial plate count method [60].
- This testing should be performed using a panel of challenge microorganisms relevant to the product and test environment.
3. Data Transformation and Statistical Analysis:
- Because microbial count data typically follow a Poisson distribution, transform the raw counts (e.g., using log₁₀ transformation or square root of (count +1)) to enable the use of parametric statistics [60].
- Assess accuracy by performing a statistical comparison, such as ANOVA on the log-transformed data, to show that the results from the alternative method are not less than 70% of those from the compendial method or are statistically equivalent [60].
- Evaluate precision by calculating the standard deviation or relative standard deviation (coefficient of variation) of the results from both methods across the tested range [60].
Diagram 1: USP <1223> and Ph. Eur. 5.1.6 Validation Workflow. This diagram outlines the core process for validating an alternative microbiological method, from defining user needs to final implementation.
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential reagents and materials required for conducting validation studies for alternative microbiological methods, with a focus on biochemical identification.
Table 3: Key Research Reagents for Microbial Identification & Validation
| Reagent / Material | Function in Validation & Identification |
|---|---|
| Challenge Strains | A panel of well-characterized microorganisms (e.g., Staphylococcus aureus, Pseudomonas aeruginosa, Candida albicans, Aspergillus brasiliensis) used to challenge the alternative method and demonstrate specificity, accuracy, and detection limits [60]. |
| Culture Media | Selective, enriched, and non-selective agars and broths (e.g., Tryptic Soy Agar, Sabouraud Dextrose Agar) used for the propagation of challenge strains, performance of compendial methods, and growth promotion testing [55]. |
| Biochemical Substrates | Reagents for tests such as catalase (3% hydrogen peroxide), oxidase (tetramethyl-p-phenylenediamine), and urease, which are used for phenotypic identification and can serve as a comparator for alternative identification systems [55] [3]. |
| Hydrogen Peroxide (3%) | The substrate for the catalase test, a fundamental biochemical test used to differentiate bacterial genera (e.g., Staphylococcus from Streptococcus) [55] [3]. |
| Tetramethyl-p-phenylenediamine | The reagent for the oxidase test, used to identify bacteria that produce cytochrome c oxidase, such as Pseudomonas and Neisseria species [55] [3]. |
| Viability Stains | Fluorescent dyes (e.g., those used in autofluorescence methods) that stain live and/or dead cells, enabling direct counting without the need for culture, as mentioned in USP <1223> [56]. |
Diagram 2: Quantitative Method Equivalency Testing Protocol. This workflow details the parallel testing and statistical analysis required to validate a quantitative alternative method against a compendial method like the plate count.
The regulatory frameworks provided by USP <1223> and Ph. Eur. 5.1.6 are foundational for the successful integration of alternative microbiological methods in pharmaceutical research and quality control. For scientists focused on microbial identification, adhering to these guidelines ensures that new biochemical or genotypic methods are rigorously validated and provide results that are reliable, accurate, and defensible. The key to a successful validation lies in a well-structured experimental design, a thorough understanding of the statistical tools required for data analysis, and comprehensive documentation. By following these structured protocols and utilizing the appropriate research reagents, drug development professionals can confidently implement advanced microbiological methods that enhance product safety and streamline development processes.
Within pharmaceutical microbiology and drug development, accurate microbial identification is a critical component of quality control, patient safety, and regulatory compliance. This process relies on two primary methodological approaches: compendial methods, which are standardized, officially recognized procedures found in pharmacopeias, and biochemical methods, which encompass a range of techniques based on the metabolic and enzymatic properties of microorganisms [61] [62]. A compendial method, as defined by the United States Pharmacopeia (USP), represents an enforceable public quality standard for medicines, dietary supplements, and food ingredients [62]. Biochemical identification, on the other hand, leverages the fact that bacterial species have distinct enzymatic profiles, which can be revealed through tests for catalase, oxidase, urease, and substrate utilization, among others [3].
Establishing equivalence between a newly developed or modified biochemical method and an existing compendial standard is not merely an academic exercise; it is a fundamental requirement for regulatory submissions and quality assurance in manufacturing. It provides scientific and regulatory confidence that the alternative method performs at least as well as the standard method in terms of accuracy, precision, sensitivity, and specificity [63]. This application note provides a detailed protocol for designing and executing an equivalence study, specifically framed within the context of microbial identification for pharmaceutical development.
Theoretical Foundation: Compendial and Biochemical Methods
Compendial Standards in Microbiology
Compendial methods are characterized by their pre-validated, standardized nature. They are published in official compendia such as the USP-NF, European Pharmacopoeia (EP), and Japanese Pharmacopoeia (JP) [61]. For microbial identification, these monographs may prescribe specific techniques or a general requirement for identification, often referencing established methodologies. The primary advantage of compendial methods is their immediate regulatory acceptance. They are cost-effective for routine use and ensure consistency across different laboratories and manufacturers [61]. However, a significant limitation is their lack of flexibility; they may not address novel microorganisms, specific formulation challenges, or the unique impurities that might be present in a proprietary manufacturing process [61].
Biochemical Methods for Microbial Identification
Biochemical identification methods are based on detecting the unique metabolic fingerprints of microorganisms. Each bacterial species possesses a specific repertoire of enzymes that fuel its metabolic needs, and detecting these enzymes allows for accurate classification [3]. These methods range from simple, single-test assays to complex, automated systems.
- Traditional Biochemical Tests: These include tests like catalase, which distinguishes catalase-positive Staphylococci from catalase-negative Streptococci by the production of bubbles when hydrogen peroxide is added [3] [5]. Oxidase testing detects the presence of cytochrome c oxidase, with a color change to purple indicating a positive result [3]. Substrate utilization tests use panels of carbon or nitrogen sources to create a unique color-changing profile that identifies the bacterium [5].
- Automated Biochemical Systems: Systems such as the API strip series (bioMérieux), VITEK 2 (bioMérieux), and BD Phoenix represent the evolution of traditional tests into miniaturized, automated, and high-throughput formats [1]. These systems use identification cards or plates containing multiple biochemical substrates. The instrument incubates the samples and analyzes the resulting reaction patterns against an extensive database to provide a species-level identification, often within 4 to 24 hours [1].
While biochemical methods are highly adaptable and can be tailored for specific applications, they require extensive validation when used in a non-compendial context, involving higher upfront costs and longer implementation times [61].
The Regulatory and Scientific Framework of Equivalence
The process of demonstrating equivalence aligns with the principles of method validation and method verification as defined in regulatory guidelines. Method validation is a comprehensive process that proves a method is suitable for its intended purpose and is required for new methods [63]. Method verification, in contrast, is the process of confirming that a previously validated method (such as a compendial method) performs as expected in a specific laboratory [63]. When comparing a biochemical method to a compendial standard, the study design incorporates elements of both: it validates the performance of the new method while verifying its results against a accepted standard.
The ICH M10 guideline on bioanalytical method validation underscores the necessity for well-characterized and validated methods to ensure reliable data for regulatory decisions, a principle that extends to microbiological assays [64]. Furthermore, the FDA provides guidance on harmonizing compendial standards with drug application approval, outlining processes like the USP Pending Monograph Process for updating or creating new monographs that reflect approved methods [65].
The following workflow diagram outlines the key stages in establishing method equivalence.
Experimental Protocol for Establishing Equivalence
Study Design and Strain Selection
A robust equivalence study is based on a direct, parallel comparison between the compendial method (the reference method) and the biochemical method (the alternative method).
- Principle: A panel of well-characterized microbial strains is tested simultaneously using both the reference and alternative methods. The resulting identifications are compared to determine the level of concordance.
- Scope: This protocol is designed for bacterial identification and can be adapted for yeast and fungi. It covers methods such as automated biochemical systems (e.g., VITEK 2) compared to compendial directives or established biochemical patterns.
- Key Definitions:
- Reference Method: The compendial or previously validated method against which the alternative method is compared.
- Alternative Method: The biochemical method under evaluation for equivalence.
- Concordance: The percentage of strains for which the alternative method provides an identification result that matches that of the reference method.
Strain Panel Selection: The panel must be representative of the microbial isolates likely to be encountered in the specific application (e.g., manufacturing environment, product isolates). It should include:
- American Type Culture Collection (ATCC) strains or other internationally recognized reference strains.
- A minimum of 10-15 unique bacterial species, covering both Gram-positive and Gram-negative organisms.
- Strains with known, well-documented biochemical profiles.
- Clinically or industrially relevant strains, including those listed in pharmacopeial chapters.
Materials and Reagents
The following table details the essential research reagent solutions and materials required for this study.
Table 1: Key Research Reagents and Materials for Equivalence Testing
| Item | Function/Application in the Protocol |
|---|---|
| Reference Microbial Strains (e.g., from ATCC) | Serves as the standardized, traceable test subjects for comparing the performance of both methods. |
| Compendial Media (e.g., Blood Agar, MacConkey Agar) | Used for the initial isolation and purity checks of test strains as per compendial methods [5]. |
| Selective & Differential Media (e.g., Mannitol Salt Agar, Baird-Parker Agar) | Used in the reference method for preliminary grouping and phenotypic characterization of isolates [5]. |
| Biochemical Test Reagents (e.g., Hydrogen Peroxide for Catalase, Oxidase Test Strips) | Used for traditional biochemical tests that form part of the reference method or for resolving discrepant results [3]. |
| Automated Biochemical Identification System (e.g., VITEK 2, BD Phoenix) | Represents the alternative biochemical method. Includes specific test kits, cards, and databases. |
| Sterile Swabs and Inoculation Loops | Essential for the aseptic transfer and preparation of microbial samples for both methods. |
| Quality Control Strains | Used to verify the proper functioning of both the reference and alternative methods on the day of testing. |
Detailed Stepwise Procedure
Part A: Preparation of Test Strains
- Revival: Reconstitute or streak all frozen or lyophilized reference strains onto non-selective agar plates (e.g., Tryptic Soy Agar) to ensure viability and purity.
- Purity Check: Incubate plates at the appropriate temperature and duration (typically 18-72 hours at 30-37°C). Examine colonies for consistent morphology. Perform Gram staining to confirm cellular morphology and purity.
- Subculture: Select a well-isolated colony and subculture it onto a fresh agar plate to generate a working culture for the equivalence testing.
Part B: Parallel Testing with Reference and Alternative Methods
- Inoculum Preparation: Prepare a standardized suspension of each test strain in sterile saline or the buffer specified by the alternative method's manufacturer. Adjust the turbidity to a 0.5 McFarland standard or equivalent, as required.
- Reference Method Execution:
- Inoculate the required compendial or reference media (e.g., Blood Agar for hemolysis observation, selective agars) [5].
- Perform prescribed biochemical tests (e.g., Catalase, Oxidase, Coagulase) according to standard operating procedures [3].
- Record all observations and identifications based on the defined flow charts or criteria.
- Alternative Method Execution:
- Inoculate the test card, panel, or strip for the automated biochemical system (e.g., VITEK 2 GN card for Gram-negatives) as per the manufacturer's instructions.
- Load the inoculated card into the instrument.
- Initiate the automated incubation and reading cycle.
- Incubation: Incubate all tests, both reference and alternative, under the specified conditions (temperature, atmosphere, duration).
Part C: Data Collection and Analysis
- Result Recording: For the reference method, record the final identification based on phenotypic profiles. For the alternative method, record the identification and the confidence level (e.g., percentage, "excellent," "good") provided by the system.
- Concordance Calculation: Create a comparison table for all strains tested. Calculate the overall percent concordance using the formula: Overall Concordance (%) = (Number of strains with identical identification by both methods / Total number of strains tested) x 100
- Discrepant Analysis: For any strain where the identification between the two methods does not match, initiate an investigation. This may involve a third, definitive method such as 16S rRNA gene sequencing or MALDI-TOF Mass Spectrometry to resolve the discrepancy [1] [5].
Data Analysis and Interpretation
Key Performance Metrics
The success of the equivalence study is determined by evaluating several quantitative metrics. The data from the parallel testing should be compiled into a summary table for clear comparison.
Table 2: Key Performance Metrics for Equivalence Determination
| Metric | Calculation Method | Acceptance Criterion for Equivalence |
|---|---|---|
| Overall Concordance | (Identical IDs / Total Strains) x 100 | ≥ 90% - 95% |
| Sensitivity | (True Positives / (True Positives + False Negatives)) x 100 | Method-specific; should match or exceed reference method performance. |
| Specificity | (True Negatives / (True Negatives + False Positives)) x 100 | Method-specific; should match or exceed reference method performance. |
| Time to Identification | Record start and end time for each method for every strain. | A significant reduction with the alternative method may be a key advantage. |
Statistical Analysis and Acceptance Criteria
Beyond simple concordance, statistical analysis strengthens the claim of equivalence.
- Statistical Testing: A Chi-squared test or Kappa statistic can be used to measure the level of agreement between the two methods beyond what would be expected by chance. A Kappa value above 0.8 indicates almost perfect agreement.
- Acceptance Criteria: Predefine acceptance criteria prior to the study. A common benchmark is an overall concordance of ≥90% with the reference method. For a method to be considered equivalent, the lower bound of the 95% confidence interval for the concordance rate should not fall below a pre-specified limit (e.g., 85%).
- Handling Discrepancies: Resolving discrepancies using a definitive method like genetic sequencing provides critical information. It reveals whether the alternative method is more accurate, less accurate, or simply different from the reference method. This analysis is essential for a thorough scientific justification.
The decision-making process after data collection is summarized in the following logic flow diagram.
Establishing equivalence between a biochemical method and a compendial standard is a rigorous but achievable process that demands a structured experimental design, careful execution, and robust data analysis. By following the protocol outlined in this document, researchers and drug development professionals can generate the compelling evidence needed to support the use of modern, efficient biochemical identification methods in a regulated environment.
The successful demonstration of equivalence offers significant advantages, including potentially faster time-to-results, improved automation, and the ability to identify a broader range of microorganisms [1] [3]. Ultimately, this work strengthens the overall quality control framework by ensuring that the methods used to ensure product safety are both scientifically sound and compliant with regulatory expectations. For implementation, laboratories should prepare a comprehensive report detailing the study design, raw data, analysis, and conclusions, which can be referenced in regulatory filings such as Drug Master Files (DMFs) or marketing application submissions [65] [63].
The accurate and timely identification of microorganisms is a cornerstone of microbiological science, impacting fields from clinical diagnostics to pharmaceutical quality control. For decades, the paradigm for bacterial identification relied on culture and biochemical tests (CBtest), which utilize phenotypic characteristics such as morphology, growth on selective media, and metabolic profiles [66]. While standardized and widespread, these methods are often time-consuming, requiring 24 to 48 hours or more for results, and may fail to identify fastidious, slow-growing, or uncommon organisms [66].
This Application Note frames the transition from these traditional phenotypic methods to modern genotypic and proteomic technologies within the context of a broader thesis on microbial identification. We focus on two powerful techniques: 16S ribosomal RNA (rRNA) gene sequencing and Matrix-Assisted Laser Desorption/Ionization Time-of-Flight Mass Spectrometry (MALDI-TOF MS). The adoption of these methods represents a shift towards leveraging molecular and protein "fingerprints" for identification, offering unprecedented speed, accuracy, and resolution [67] [66]. We provide a comparative evaluation of these methods, complete with performance data, detailed experimental protocols, and workflow visualizations to guide researchers and drug development professionals in selecting and implementing the appropriate identification strategy.
Comparative Performance Data
The following tables summarize the key characteristics and performance metrics of biochemical testing, 16S rRNA gene sequencing, and MALDI-TOF MS, providing a clear, data-driven comparison for method selection.
Table 1: Key Characteristics of Microbial Identification Methods
| Parameter | Biochemical Tests (CBtest) | 16S rRNA Gene Sequencing | MALDI-TOF MS |
|---|---|---|---|
| Principle | Phenotypic profiles (metabolism, morphology) | Sequence analysis of a conserved gene | Spectral analysis of ribosomal protein fingerprints |
| Time to Result | 24–48 hours [66] | 8–24 hours (sequencing dependent) [66] | Minutes to a few hours [67] |
| Cost per Sample | Low | Moderate to High [66] | Low (after initial investment) [67] |
| Species-Level Resolution | Variable, often limited | ~87.5% of species [66] | High for most common species, but database-dependent [68] [69] |
| Ability to Identify Novel Taxa | No | Yes (can suggest new species) [70] | Limited, requires database expansion [70] [71] |
| Automation Potential | Low | Moderate (increasing) [66] | High [67] |
Table 2: Reported Performance of MALDI-TOF MS vs. 16S rRNA Gene Sequencing
| Study Context | Identification Concordance (Species Level) | Key Findings |
|---|---|---|
| Clinical Anaerobes [69] | 87.3% (318/364 isolates) | MALDI-TOF MS is reliable for most anaerobic bacteria, though database updates are needed for rare species. |
| Environmental Cave Isolates [71] | 40% with updated database | 16S rRNA sequencing outperformed MALDI-TOF MS for genus-level ID of environmental isolates, but updated MS databases showed improvement. |
| Pharmaceutical Contaminants [70] | Variable; some strains not identified by either method alone | A combination of 16S rRNA sequencing and MALDI-TOF MS was often necessary for definitive identification, with some strains indicating potential new species. |
Detailed Experimental Protocols
Protocol for Bacterial Identification by MALDI-TOF MS
The following protocol is adapted from established procedures using the Bruker MALDI Biotyper system and the trifluoroacetic acid (TFA) inactivation method, which is suitable even for highly pathogenic bacteria [72].
Principle: Intact bacterial cells are irradiated with a laser, causing the desorption and ionization of predominantly ribosomal proteins. The resulting mass spectrum (2–20 kDa) serves as a unique fingerprint, which is compared against a reference database for identification [67] [72].
Procedure:
- Cultivation: Grow the bacterial isolate on a solid agar medium appropriate for the species (e.g., Tryptic Soy Agar) for 24–72 hours at the optimal growth temperature [68] [72].
- Sample Inactivation and Preparation:
- Harvest 1–4 mg of biomass (the equivalent of 1-3 1 µL loops) and suspend it in 20 µL of sterile water.
- Add 80 µL of pure TFA to the suspension and incubate for 30 minutes for complete microbial inactivation [72].
- Dilute the solution tenfold with HPLC-grade water.
- Mix 1 µL of the inactivated sample solution with 10 µL of a saturated matrix solution (e.g., α-cyano-4-hydroxycinnamic acid (HCCA) in 50% acetonitrile with 2.5% TFA).
- Spot 1 µL of this mixture onto a steel MALDI target plate and allow it to air-dry completely [72].
- Data Acquisition: Insert the target into the MALDI-TOF mass spectrometer.
- Acquire mass spectra in linear positive ion mode with a mass range of 2,000–20,000 Da.
- Calibrate the instrument using a standard bacterial test standard (e.g., E. coli extract) [68].
- Data Analysis and Identification: Compare the acquired mass spectrum against the reference spectral database (e.g., Bruker MBT database).
- Identification is based on a scoring system. A score of ≥2.000 indicates confident species-level identification, a score of 1.700–1.999 indicates confident genus-level identification, and a score of <1.700 is considered unreliable [70].
Protocol for Bacterial Identification by 16S rRNA Gene Sequencing
This protocol outlines the Sanger sequencing of the nearly full-length 16S rRNA gene, a standard method for bacterial identification and phylogenetic analysis [68] [66].
Principle: The 16S rRNA gene, which contains both highly conserved and variable regions, is amplified from bacterial genomic DNA via PCR and sequenced. The resulting sequence is compared to large public databases (e.g., EzBioCloud, RDP) to determine the closest phylogenetic relatives [66] [70].
Procedure:
- Genomic DNA Extraction: Extract genomic DNA from a pure bacterial culture using a commercial kit (e.g., from Qiagen or Mo Bio) or conventional phenol-chloroform methods. Quantify the DNA using a spectrophotometer or fluorometer [66] [73].
- PCR Amplification: Amplify the nearly complete 16S rRNA gene using universal bacterial primers.
- Common Primer Pair: 27F (5'-AGAGTTTGATCMTGGCTCAG-3') and 1492R (5'-GGTTACCTTGTTACGACTT-3') [73].
- PCR Mix: 0.15 µL AccuPrime Taq DNA Polymerase High Fidelity, 2 µL 10X PCR Buffer II, 1 µL of each primer (2 mM), 2 µL template DNA, and nuclease-free water to 20 µL.
- Cycling Conditions: Initial denaturation at 95°C for 2 min; 25 cycles of 95°C for 20 sec, 50°C for 30 sec, and 72°C for 5 min; final extension at 72°C for 10 min [73].
- PCR Purification and Sequencing: Purify the PCR amplicon using a commercial purification kit to remove excess primers and nucleotides. Submit the purified product for Sanger sequencing in both directions using the same PCR primers.
- Bioinformatic Analysis:
- Sequence Assembly and Trimming: Assemble the forward and reverse reads into a single contig and trim the ends to obtain a high-quality, nearly full-length sequence.
- Database Comparison: Use the BLAST algorithm to compare the sequence against the NCBI nucleotide database or a dedicated 16S database like EzBioCloud.
- Identification and Demarcation: A sequence similarity of ≥98.65% is commonly used as a threshold for species-level demarcation, while a similarity below this threshold may indicate a novel species or require further analysis with housekeeping genes [68] [70].
Workflow Visualization
The following diagram illustrates the key steps and comparative workflows for MALDI-TOF MS and 16S rRNA gene sequencing.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Microbial Identification
| Item | Function / Application |
|---|---|
| MALDI-TOF MS Matrix (e.g., HCCA) | Energy-absorbing compound that co-crystallizes with the sample, enabling laser desorption/ionization of bacterial proteins [67] [72]. |
| Universal 16S rRNA Primers (e.g., 27F/1492R) | Oligonucleotides that bind to conserved regions of the 16S rRNA gene to amplify the variable regions for sequencing and phylogenetic analysis [73]. |
| Commercial DNA Extraction Kits | Enable rapid, standardized, and high-quality purification of genomic DNA from bacterial cultures, critical for downstream PCR and sequencing [66]. |
| Trifluoroacetic Acid (TFA) | Used in a secure sample preparation protocol for MALDI-TOF MS that ensures complete inactivation of pathogens, including bacterial spores [72]. |
| Reference Spectral Databases (e.g., MBT, RKI Public DB) | Curated libraries of mass spectra from known microorganisms; essential for pattern matching and identification accuracy in MALDI-TOF MS [69] [72]. |
| 16S rRNA Sequence Databases (e.g., EzBioCloud, RDP) | Curated libraries of 16S rRNA gene sequences from type strains; used for taxonomic assignment via sequence similarity search (BLAST) [70] [71]. |
The accurate identification of microorganisms is a critical step in clinical diagnostics, pharmaceutical development, and public health. While a diverse array of identification technologies is available, selecting the most appropriate method presents a significant challenge for laboratories, requiring a careful balance of clinical need, analytical throughput, and cost-effectiveness. This application note provides a structured decision-making framework, centered on a weighted decision matrix, to guide researchers and scientists in evaluating and selecting microbial identification technologies. We detail specific experimental protocols for key biochemical methods and present a comparative analysis of technological platforms, including traditional biochemistry, MALDI-TOF MS, and molecular techniques, to facilitate data-driven resource allocation within the context of modern microbiological research and drug development.
The cornerstone of microbial identification has long been phenotypic methods, particularly biochemical tests, which rely on the visual detection of metabolic activities or enzymatic reactions to classify microorganisms [74] [75]. These methods, including the classic API and VITEK systems, are prized for their cost-effectiveness and well-established protocols [13] [75]. However, the landscape of microbial identification is rapidly evolving. The advent of genotypic and proteomic technologies such as Polymerase Chain Reaction (PCR), next-generation sequencing (NGS), and Matrix-Assisted Laser Desorption/Ionization Time-of-Flight (MALDI-TOF) mass spectrometry has revolutionized the field by offering superior speed, automation, and precision [13].
This proliferation of available technologies creates a pressing need for a systematic selection tool. A weighted decision matrix, also known as a prioritization matrix, provides an objective framework to evaluate multiple options against predefined, critically important criteria [76] [77]. For the research scientist, this translates to a transparent and justifiable method for selecting the optimal identification platform that aligns with specific project goals, operational constraints, and the requirements of drug development workflows.
Quantitative Comparison of Microbial Identification Technologies
To enable an informed selection, key performance metrics for major identification technologies are summarized in Table 1. The data provides a baseline for evaluation against specific laboratory needs.
Table 1: Comparative Analysis of Microbial Identification Platforms
| Technology | Approximate Cost per Sample | Time to Result | Throughput (Samples per Day) | Key Differentiating Factors |
|---|---|---|---|---|
| Phenotypic Biochemical Tests | Low | 18 - 48 hours [74] | Low to Moderate | High cost-effectiveness; well-established protocols [13] |
| PCR | Moderate | 2 - 4 hours | High | High sensitivity and specificity; detects non-viable organisms [13] |
| MALDI-TOF MS | Low [13] | < 30 minutes [13] | Very High (< 5 minutes per sample) [13] | Excellent for high-throughput routine identification [13] |
| Next-Generation Sequencing (NGS) | High | 1 - 3 days | Low to Moderate (batch processing) | Provides comprehensive genomic data; no prior knowledge of organism required |
A Decision Matrix for Technology Selection
A decision matrix ranks options by developing a set of weighted criteria and scoring each choice against them [76]. This process transforms subjective preference into a quantifiable, defensible business case.
Defining Criteria and Assigning Weights
The first step involves brainstorming and refining a list of evaluation criteria. For a microbial identification lab, these typically include:
- Clinical Need/Application: The diagnostic or research question being addressed.
- Throughput: The number of isolates processed in a given time.
- Cost per Sample: The direct cost of reagents and consumables.
- Capital Equipment Cost: The initial investment in instrumentation.
- Speed/Turnaround Time (TAT): Time from sample to result.
- Accuracy & Resolution: Ability to correctly identify to the species or strain level.
- Ease of Use & Automation: Level of technical expertise required and potential for walk-away automation.
The relative importance of each criterion is determined by the laboratory's specific context and strategic goals, which is reflected in its assigned weight. Table 2 provides a hypothetical weighting scheme for two different laboratory scenarios.
Table 2: Example Criteria Weighting for Different Laboratory Types
| Criterion | Weight: Clinical Diagnostic Lab | Weight: Research/Pharma Lab |
|---|---|---|
| Speed / TAT | 30% | 15% |
| Accuracy & Resolution | 25% | 30% |
| Throughput | 20% | 20% |
| Cost per Sample | 15% | 10% |
| Capital Cost | 10% | 15% |
| Ease of Use & Automation | 10% | 10% |
| Total | 100% | 100% |
Scoring and Evaluation
An L-shaped matrix is constructed with the criteria and their weights along one axis and the list of technology options on the other [76]. Each technology is then scored on a consistent scale (e.g., 1-5, where 5 is best) against each criterion. The score is multiplied by the criterion's weight, and the sum of these weighted scores yields a total for each technology. The option with the highest score represents the most suitable choice based on the defined priorities [76] [77].
Application Notes: Experimental Protocols for Biochemical Identification
Despite the rise of newer technologies, biochemical tests remain a vital and reliable tool, especially in resource-constrained settings or for validating genomic data. Below are detailed protocols for foundational tests used in differentiating Gram-negative bacteria, which are a common focus in clinical and industrial microbiology.
Protocol: Triple Sugar Iron (TSI) Agar Test
The TSI agar test is a differential medium used primarily to distinguish among members of the Enterobacteriaceae family and to differentiate them from other Gram-negative intestinal bacilli based on their ability to ferment carbohydrates and produce hydrogen sulfide [78].
1. Principle: TSI agar contains three sugars: glucose (0.1%), lactose (1%), and sucrose (1%), along with phenol red as a pH indicator and ferrous ammonium sulfate for detecting H₂S production. The low glucose concentration is rapidly fermented by most enteric bacteria, producing acidic byproducts that turn the entire slant and butt yellow. Once the glucose is exhausted, organisms that can ferment lactose or sucrose will continue to produce acid, maintaining a yellow slant. If lactose/sucrose fermentation does not occur, the organism will metabolize peptones, producing alkaline byproducts that turn the slant red. H₂S production, indicated by a black precipitate, occurs when the bacterium reduces sodium thiosulfate to hydrogen sulfide, which then reacts with ferrous ammonium sulfate [78].
2. Materials:
- TSI agar slants in tubes
- Inoculating needle
- Pure, 18-24 hour bacterial culture
- Incubator at 35±2°C
3. Procedure: a. Using a sterile inoculating needle, touch a well-isolated colony. b. Stab the needle deeply into the agar butt, reaching to within ~5 mm of the tube bottom. c. Withdraw the needle and streak the entire surface of the agar slant in a zig-zag pattern. d. Loosen the tube cap to allow for aerobic conditions. e. Incubate the inoculated tube at 35±2°C for 18-24 hours.
4. Interpretation of Results:
- Yellow Slant/Yellow Butt (A/A): Glucose, lactose, and/or sucrose fermentation with acid production.
- Red Slant/Yellow Butt (K/A): Glucose fermentation only. The slant reverts to alkaline (red) after glucose exhaustion.
- Red Slant/Red Butt (K/K): No carbohydrate fermentation; peptone utilization only.
- Black Precipitate: Production of hydrogen sulfide (H₂S).
- Bubbles or Cracks in Agar: Production of gas (CO₂/H₂) from fermentation.
Protocol: Sulfur, Indole, Motility (SIM) Medium Test
SIM is a multi-test differential medium used to determine sulfur reduction, indole production, and motility [78].
1. Principle: SIM medium contains peptonized iron and sodium thiosulfate as sulfur sources. Bacteria that produce the enzyme cysteine desulfurase can reduce sulfur to hydrogen sulfide (H₂S), which reacts with ferrous ammonium sulfate to form a black precipitate of ferrous sulfide. The medium also contains tryptophan. Bacteria possessing the enzyme tryptophanase can hydrolyze tryptophan to indole, pyruvic acid, and ammonia. Indole is detected by the addition of Kovac's reagent, which forms a red ring upon reaction. The semi-solid nature of the medium (low agar concentration of 0.4%) allows for the detection of motility as evidenced by diffuse growth radiating from the stab line [78].
2. Materials:
- SIM medium deeps in tubes
- Inoculating needle
- Pure bacterial culture
- Kovac's reagent
- Incubator at 35±2°C
3. Procedure: a. Using a sterile inoculating needle, touch a well-isolated colony. b. Stab the needle straight down into the center of the SIM medium to a depth of about three-fourths of the way down. c. Withdraw the needle along the same stab line. d. Incubate at 35±2°C for 18-24 hours. e. After incubation, add 5-10 drops of Kovac's reagent to the surface of the medium.
4. Interpretation of Results:
- H₂S Production: A blackening of the medium along the stab line.
- Indole Production: A red ring at the top of the medium after adding Kovac's reagent.
- Motility: Turbidity or diffuse growth spreading away from the stab line; non-motile organisms grow only along the stab line.
The Scientist's Toolkit: Key Reagents for Biochemical Identification
Table 3: Essential Reagents and Materials for Biochemical Testing
| Reagent / Material | Function / Purpose | Example in Protocol |
|---|---|---|
| Selective & Differential Media | Supports growth of target organisms while inhibiting others and differentiating based on metabolic properties. | Mannitol Salt Agar (selective for Staphylococcus), TSI Agar (differential for Enterobacteriaceae) [78]. |
| pH Indicators | Visual detection of acid production from carbohydrate fermentation. | Phenol Red (yellow below pH 6.8, red/pink at neutral pH, fuschia above 7.4) [78]. |
| Enzyme Substrates | Detects the presence of specific bacterial enzymes. | Urea in Urease test, Tryptophan in Indole test, Citrate in Citrate test [74]. |
| Chemical Reagents | Added post-incubation to reveal a specific metabolic product. | Kovac's Reagent for indole detection [78] [74]. |
| Hydrogen Peroxide (3%) | Detects the presence of catalase enzyme by the liberation of oxygen bubbles [74]. | Catalase test. |
| Tetramethyl-p-Phenylenediamine Dihydrochloride | Detects the presence of cytochrome c oxidase enzyme [74]. | Oxidase test. |
The selection of a microbial identification system is a multi-factorial decision with significant implications for laboratory efficiency, diagnostic accuracy, and research outcomes. The application of a structured decision matrix, as outlined in this document, empowers scientists and drug development professionals to move beyond anecdotal evidence and make objective, defensible choices. By clearly defining needs, weighting critical factors such as clinical application, throughput, and cost, and systematically evaluating available technologies—from foundational biochemical tests to advanced proteomic and genomic platforms—laboratories can optimize their resources and enhance their operational capabilities. This rigorous approach ensures that the selected tool is not merely the most technologically advanced, but the most strategically appropriate for its intended context.
Conclusion
Biochemical testing remains a vital, cost-effective tool for microbial identification, underpinning quality control in pharmaceutical development and infectious disease diagnosis. Its strength lies in a well-understood framework for probing microbial metabolism, though users must be cognizant of its limitations with closely related or unusual species. The future of microbial identification is undoubtedly polyphasic, integrating robust biochemical profiling with rapid confirmatory techniques like MALDI-TOF MS and genotypic analysis. For researchers and drug developers, this synergy allows for more precise microbial characterization, enhancing contamination control strategies, accelerating root cause investigations, and ultimately supporting the development of safer biomedical products.
References
- 1. Evolving strategies in microbe identification—a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11412244/]
- 2. Activity Enzymatic Using an Ultrasensitive Array of... Profiling [https://pubmed.ncbi.nlm.nih.gov/38362863/]
- 3. Biochemical Tests for Microbial Identification [https://www.news-medical.net/life-sciences/Biochemical-Tests-for-Microbial-Identification.aspx]
- 4. Characterization and prediction of the mechanism of action of... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-016-0696-5]
- 5. Bacteria Through Look, Growth, Stain and Strain Identifying [https://asm.org/articles/2020/february/identifying-bacteria-through-look,-growth,-stain]
- 6. Carbohydrate Fermentation Test (Sugar Fermentation Test) [https://microbenotes.com/carbohydrate-fermentation-test/]
- 7. Fermentation [https://en.wikipedia.org/wiki/Fermentation]
- 8. Bacterial Metabolism - Medical Microbiology - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK7919/]
- 9. Carbohydrate Fermentation Test: Uses, Principle, Procedure, Results | Microbe Online [https://microbeonline.com/carbohydrate-fermentation-test-uses-principle-procedure-results/]
- 10. Optimal enzyme utilization suggests that concentrations ... [https://www.nature.com/articles/s41467-023-38159-4]
- 11. Microbial Enzymes: Tools for Biotechnological Processes [https://pmc.ncbi.nlm.nih.gov/articles/PMC4030981/]
- 12. Fermentation Test - Principle, Procedure, Uses and Interpretation [https://microbiologyinfo.com/fermentation-test/]
- 13. Microbial Identification Market Size and Trends, 2025-2032 [https://www.coherentmarketinsights.com/industry-reports/microbial-identification-market]
- 14. Indole Test- Principle, Media, Procedure, Types, Results, ... [https://microbenotes.com/indole-test-objective-principle-media-procedure-and-results/]
- 15. Protocols Indole Test [https://asm.org/protocols/indole-test-protocol]
- 16. Catalase Test- Principle, Procedure, Types, Results, Uses [https://microbenotes.com/catalase-test-principle-procedure-and-result-interpretation/]
- 17. 1.18: Catalase Test [https://bio.libretexts.org/Bookshelves/Microbiology/Microbiology_Laboratory_Manual_(Hartline)/01%3A_Labs/1.18%3A_Catalase_Test]
- 18. Oxidase Test- Principle, Procedure, Types, Results, Uses [https://microbenotes.com/oxidase-test-principle-procedure-and-results/]
- 19. Oxidase Test- Principle, Uses, Procedure, Types, Result ... [https://microbiologyinfo.com/oxidase-test-principle-uses-procedure-types-result-interpretation-examples-and-limitations/]
- 20. Coagulase Test- Principle, Procedure, Types, Result, Uses [https://microbenotes.com/coagulase-test-principle-procedure-and-result-interpretation/]
- 21. Coagulase Test- Principle, Procedure, Types, Interpretation ... [https://microbiologyinfo.com/coagulase-test-principal-procedure-types-interpretation-and-examples/]
- 22. API® ID STRIPS | Pioneering Diagnostics - bioMerieux [https://www.biomerieux.com/us/en/our-offer/clinical-products/api.html]
- 23. API Kit微生物鑑定套組(黃金標準鑑定法), Biomerieux 梅里埃 [https://www.cmp-micro.com/ch/api-kit-biomerieux/]
- 24. API (Analytical Profile Index) 20E Test - Procedure, Uses ... [https://microbiologyinfo.com/api-20e-test/]
- 25. 43: API-20E multitest strip [https://bio.libretexts.org/Learning_Objects/Laboratory_Experiments/Microbiology_Labs/Microbiology_Labs_I/43%3A_API-20E_multitest_strip]
- 26. Automated systems for identification of microorganisms [https://pmc.ncbi.nlm.nih.gov/articles/PMC358246/]
- 27. Comparison of BD Phoenix to Vitek 2, MicroScan ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2772596/]
- 28. Comparison of BD phoenix to vitek 2, microscan ... [https://pubmed.ncbi.nlm.nih.gov/19741088/]
- 29. VITEK® 2 COMPACT | Pioneering Diagnostics - bioMerieux [https://www.biomerieux.com/us/en/our-offer/industry-products/vitek-2-compact-automated-microbial-identification.html]
- 30. Evaluation of the BD Phoenix Automated Microbiology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1489426/]
- 31. BD Phoenix™ M50 automated microbiology system [https://www.bd.com/en-us/products-and-solutions/products/product-families/bd-phoenix-m50-instrument]
- 32. ATCC Minis Support VITEK 2 Quality Control Testing [https://www.atcc.org/resources/application-notes/minis-support-vitek-testing]
- 33. Automated Microbiology Systems: Building a Business Case [https://www.rapidmicrobiology.com/test-method/automated-microbiology-systems-building-a-business-case]
- 34. Gram Staining - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK562156/]
- 35. Gram Stain: What It Is, Purpose, Procedure & Results [https://my.clevelandclinic.org/health/diagnostics/22612-gram-stain]
- 36. Gram Stain Protocol [https://www.vet.cornell.edu/animal-health-diagnostic-center/testing/testing-protocols-interpretations/gram-stain-protocol]
- 37. A Guide to Environmental Monitoring [https://www.eurofinsus.com/food-testing/resources/a-guide-to-environmental-monitoring/]
- 38. Environmental Monitoring Program (EMP) Guide for Food ... [https://fsns.com/environmental-monitoring-programs-emp-for-food-safety-your-complete-guide/]
- 39. Summary of taxonomy changes ratified by the International ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12451628/]
- 40. Advancing clinical biochemistry: addressing gaps and driving ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12011881/]
- 41. Testing the limits of short-reads metagenomic ... [https://www.nature.com/articles/s41598-025-07734-8]
- 42. Key features and guidelines for the application of microbial ... [https://www.nature.com/articles/s41598-024-77864-y]
- 43. Rapid label-free identification of seven bacterial species ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12416834/]
- 44. A Polyphasic Approach to Classification and Identification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8397008/]
- 45. Fungal identification based on the polyphasic approach [https://synapse.koreamed.org/articles/1516090082]
- 46. Advances in detection of fastidious bacteria [https://www.sciencedirect.com/science/article/abs/pii/S0165993619300081]
- 47. Microbial Identification Market Size, Share & Trends 2025- ... [https://www.futuremarketinsights.com/reports/microbial-identification-market]
- 48. Conventional Biochemical ID | MI - Microbiology [https://microbiology.mlsascp.com/conventional-biochemical-id.html]
- 49. Detection of selected fastidious bacteria [https://pubmed.ncbi.nlm.nih.gov/10619747/]
- 50. Lab 11: Biochemical Tests (Day 2) [https://bio.libretexts.org/Learning_Objects/Laboratory_Experiments/Microbiology_Labs/Book%3A_General_Microbiology_Lab_Manual_(Pakpour_and_Horgan)/Lab_11%3A_Biochemical_Tests_(Day_2)]
- 51. Quantitative PCR (qPCR) Data Analysis [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/gene-expression-analysis-real-time-pcr-information/precision-qpcr.html]
- 52. Advancing Microbial ID to Species-Level Precision [https://www.rapidmicrobiology.com/news/advancing-microbial-identification-a-rapidmicrobiology-special-focus]
- 53. WHO releases new reports on new tests and treatments in ... [https://www.who.int/news/item/02-10-2025-who-releases-new-reports-on-new-tests-and-treatments-in-development-for-bacterial-infections]
- 54. Protocols Inoculating a Liquid Bacterial Culture [https://www.addgene.org/protocols/inoculate-bacterial-culture/]
- 55. The Method and Analysis of Some Biochemical Tests ... [https://brieflands.com/journals/chbs/articles/160199]
- 56. A Fresh Look at USP <1223> Validation of Alternative ... [https://www.americanpharmaceuticalreview.com/Featured-Articles/177873-A-Fresh-Look-at-USP-1223-Validation-of-Alternative-Microbiological-Methods-and-How-the-Revised-Chapter-Compares-with-PDA-TR33-and-the-Proposed-Revision-to-Ph-Eur-5-1-6/]
- 57. A comprehensive review of the newly revised European ... [https://www.europeanpharmaceuticalreview.com/article/66402/comprehensive-review-newly-revised-european-pharmacopoeia-chapter-5-1-6/]
- 58. A Guide to USP <1223> and Validation of Rapid Methods [https://www.americanpharmaceuticalreview.com/Featured-Articles/613587-Validating-Alternative-Microbiological-Methods-A-Guide-to-USP-1223-and-Validation-of-Rapid-Methods/]
- 59. A Guide to Validating RMMs Following USP <1223> [https://www.watertechnologies.com/sievers-resource-center/guide-to-validating-rmms]
- 60. <1223> VALIDATION OF ALTERNATIVE ... [https://www.drugfuture.com/pharmacopoeia/usp32/pub/data/v32270/usp32nf27s0_c1223.html]
- 61. Compendial vs. Non-Compendial Testing: Key Differences [https://allanchem.com/compendial-vs-non-compendial-testing-key-differences/]
- 62. Compendium, compendia, compendial: Clearing up the ... [https://qualitymatters.usp.org/compendium-compendia-compendial-clearing-mystery-these-terms]
- 63. Method Validation vs Method Verification: Which is Better ... [https://www.labmanager.com/method-validation-vs-method-verification-which-is-better-for-use-in-laboratories-33982]
- 64. ICH M10 on bioanalytical method validation - Scientific guideline [https://www.ema.europa.eu/en/ich-m10-bioanalytical-method-validation-scientific-guideline]
- 65. Harmonizing Compendial Standards With Drug Application ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/harmonizing-compendial-standards-drug-application-approval-using-usp-pending-monograph-process]
- 66. Advantages and Limitations of 16S rRNA Next-Generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7602188/]
- 67. MALDI-TOF mass spectrometry: an emerging technology for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4525378/]
- 68. Whole-Cell MALDI-TOF MS Versus 16S rRNA Gene Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6018384/]
- 69. Comparative evaluation of MALDI-TOF MS and 16S rRNA ... [https://pubmed.ncbi.nlm.nih.gov/37321445/]
- 70. Characterization by MALDI-TOF MS and 16S rRNA Gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11051829/]
- 71. Comparison of MALDI-TOF mass spectrometry and 16S ... [https://link.springer.com/article/10.1007/s11356-024-32537-1]
- 72. A MALDI-ToF mass spectrometry database for identification ... [https://www.nature.com/articles/s41597-025-04504-z]
- 73. Strengths and Limitations of 16S rRNA Gene Amplicon ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0093827]
- 74. Overview on Old and New Biochemical Test for Bacterial ... [https://www.auctoresonline.org/article/overview-on-old-and-new-biochemical-test-for-bacterial-identification]
- 75. Biochemical Testing - an overview [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/biochemical-testing]
- 76. Decision Matrix | Digital Healthcare Research [https://digital.ahrq.gov/health-it-tools-and-resources/evaluation-resources/workflow-assessment-health-it-toolkit/all-workflow-tools/decision-matrix]
- 77. Decision Matrix Vs Cost-Benefit Analysis [https://www.meegle.com/en_us/topics/decision-matrix/decision-matrix-vs-cost-benefit-analysis]
- 78. Tests used to identify Gram Negative Bacteria [https://www.uwyo.edu/molb2210_lab/info/biochemical_tests.htm]