Animal Cell Culture Fundamentals: A Microbiologist's Guide to Mammalian Systems
This article provides microbiologists with a comprehensive guide to the principles and practices of animal cell culture.
Animal Cell Culture Fundamentals: A Microbiologist's Guide to Mammalian Systems
Abstract
This article provides microbiologists with a comprehensive guide to the principles and practices of animal cell culture. It bridges the knowledge gap from microbial systems by detailing the unique requirements of mammalian cells, including complex media, stringent aseptic techniques, and specialized equipment. The scope covers foundational concepts like primary cultures and cell lines, core methodologies for maintenance and cryopreservation, essential troubleshooting for contamination and culture health, and the critical importance of validation through cell line authentication and quality control. This serves as an essential primer for applying these techniques in biomedical research and drug development.
From Microbes to Mammalian Cells: Mastering Foundational Concepts
Defining Animal Cell Culture and Its Core Applications in Research and Bioproduction
Animal cell culture, a cornerstone technique in modern life sciences, involves the propagation of animal cells in a controlled artificial environment. This in-depth technical guide delineates the fundamental principles, methodologies, and quantitative landscape of animal cell culture, contextualized for microbiologists and drug development professionals. We detail core protocols for maintaining cell integrity from thawing to cryopreservation, summarize key market metrics and growth conditions in structured tables, and visualize critical workflows. Furthermore, we explicate the indispensable applications of this technology in biopharmaceutical manufacturing, vaccine production, and advanced research models, underscoring its pivotal role in translating basic biological insights into therapeutic and commercial outcomes.
Animal cell culture is defined as the process by which human, animal, or insect cells are grown in a favorable artificial environment outside their natural biological context [1]. This technology, which became a common laboratory technique in the mid-1900s, has evolved from a simple tool for maintaining live cell lines into a major platform driving innovation in life sciences and commercial biotechnology [1]. The foundational principle hinges on recreating in vivo conditions in vitro, providing a controlled system to study cell biology, disease mechanisms, and production of complex biological products [2] [3].
The historical development of animal cell culture dates back to the early 20th century. Key milestones include Ross Granville Harrison's 1907-1910 experiments demonstrating nerve fiber growth from frog embryonic tissue in clotted lymph, which established the basic methodology [1] [4]. The period between the 1940s and 1960s marked a significant acceleration, driven largely by the demand for viral vaccines. The development of the polio vaccine by Jonas Salk, enabled by the viral culture techniques of Enders, Weller, and Robbins, stands as a testament to this progress [1]. Today, mammalian cell culture is an indispensable prerequisite for manufacturing a wide array of biological therapeutics, including monoclonal antibodies, hormones, interferons, clotting factors, and vaccines [1].
For microbiologists, transitioning to animal cell culture requires a paradigm shift in aseptic technique and medium complexity. While microbial cultures often utilize simple, defined media, animal cell culture media are complex concoctions requiring a precise balance of amino acids, vitamins, salts, glucose, and growth factors, typically supplemented with serum or defined replacements to support cell survival and proliferation [2] [4]. The core challenge lies in maintaining a sterile, physiologically stable environment (typically 37°C, 5% CO2, and 95% relative humidity) for cells that are far more fastidious than most microorganisms [4] [5].
Technical Breakdown: Cell Types, Culture Models, and Workflows
Classification of Cell Cultures and Cell Lines
Cultures initiated directly from animal tissues are termed primary cultures. These are heterogeneous, slow-growing, and retain the characteristic number of chromosomes of the source tissue, but have a finite lifespan [2]. Primary cultures can be further classified as:
- Anchorage-dependent/Adherent cells: Require a solid, non-toxic surface for attachment and growth (e.g., kidney cells, fibroblast cells) [2].
- Anchorage-independent/Suspension cells: Can grow freely floating in the culture medium (e.g., hematopoietic cells, hybridomas) [2].
When a primary culture is subcultured (passaged), it becomes a cell line [6]. Cell lines are categorized based on their growth potential:
- Finite Cell Lines: Cells divide a limited number of times (typically 20-100 population doublings) before undergoing senescence [2]. An example is human fibroblast cultures like WI-38 [1].
- Continuous Cell Lines: These have acquired the ability to proliferate indefinitely (immortalization) either through random mutation or deliberate genetic modification [2]. They often emerge from tumor tissues or via transformation by chemicals or viruses. Examples include HeLa (human cervical carcinoma) and CHO (Chinese Hamster Ovary) cells [1] [2].
Essential Experimental Workflows
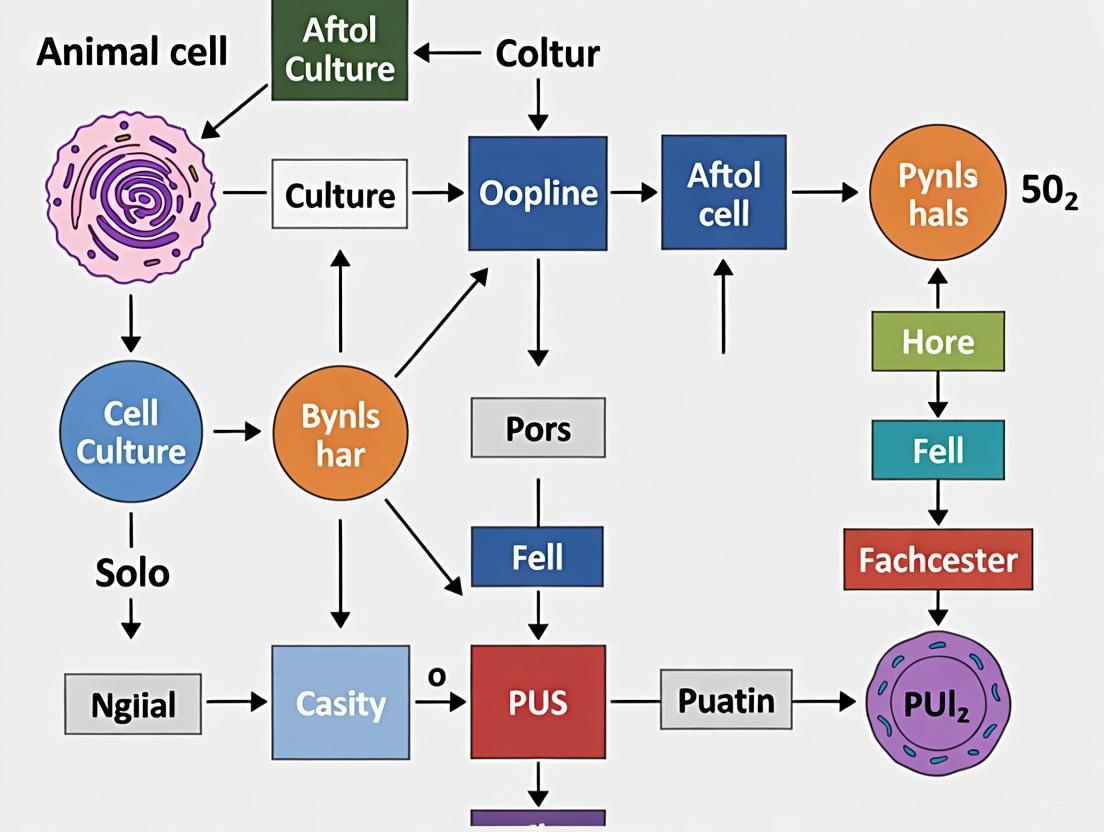
Mastering fundamental techniques is critical for cell culture integrity. The workflow below outlines the core process for handling adherent mammalian cells.
Workflow Diagram 1: Core adherent cell culture process.
Protocol: Thawing Cryopreserved Cells
Rapid thawing and removal of cryoprotectant are vital for cell viability [6].
- Preparation: Warm complete growth medium in a 37°C water bath. Prepare a culture vessel with the recommended volume of pre-equilibrated medium [5].
- Thawing: Remove vial from liquid nitrogen storage and immediately place in a 37°C water bath with gentle agitation. Thaw rapidly (~2 minutes) until only a small ice crystal remains [6].
- Decontamination: Spray or dip the vial in 70% ethanol and transfer to a biosafety cabinet [6].
- Dilution and Centrifugation: Transfer the cell suspension to a sterile centrifuge tube containing 9 mL of warm medium. Gently pipette to mix. Centrifuge at approximately 125 × g for 5-10 minutes to pellet cells and remove the cryoprotectant (DMSO) [6].
- Resuspension and Seeding: Discard the supernatant. Gently resuspend the cell pellet in 1-2 mL of fresh complete growth medium. Transfer the cell suspension to the prepared culture vessel and mix by gentle rocking [6] [5].
- Incubation: Place the culture vessel in a 37°C incubator with a humidified atmosphere of 5% CO2. Examine the cells after 24 hours and change the medium if necessary [6].
Protocol: Subculturing Adherent Cells (Passaging)
This process, also known as trypsinization, is used to split cells into new vessels before they reach 100% confluency to maintain exponential growth [6] [5].
- Remove Medium: Aspirate and discard the spent culture medium from the flask.
- Rinse: Wash the cell monolayer with a pre-warmed, sterile phosphate-buffered saline (PBS) to remove residual serum and calcium, which inhibit trypsin.
- Add Dissociation Reagent: Add enough pre-warmed trypsin-EDTA solution to cover the cell monolayer (e.g., 2-3 mL for a T-75 flask) [2].
- Incubate: Place the flask in a 37°C CO2 incubator for 1-3 minutes. Observe cells under a microscope until they round up and detach. Firmly tap the side of the flask to dislodge any remaining adherent cells [2].
- Neutralize: Add a volume of complete growth medium containing serum (which inhibits trypsin) that is at least double the volume of trypsin used. Pipette the solution across the surface to collect all cells and break up clumps.
- Count and Seed: Perform a cell count using a hemocytometer or automated cell counter. Seed an appropriate aliquot of the cell suspension into new culture vessels containing fresh, pre-warmed medium [5].
The Scientist's Toolkit: Essential Research Reagents
The following table catalogs fundamental reagents required for successful animal cell culture.
Table 1: Essential Reagents for Animal Cell Culture
| Reagent/Chemical | Core Function | Technical Notes |
|---|---|---|
| Basal Medium (e.g., DMEM, RPMI-1640) | Provides essential nutrients: amino acids, vitamins, carbohydrates, inorganic salts [4]. | Formulation must be selected based on cell type requirements. |
| Serum (e.g., Fetal Bovine Serum - FBS) | A complex, undefined supplement providing growth factors, hormones, and adhesion factors [4]. | Subject to batch-to-batch variability; potential source of contaminants. |
| Serum-Free & Chemically Defined Media | Eliminates variability of serum; supports specific cell types in a controlled environment [7] [8]. | Crucial for biomanufacturing consistency and specific applications like stem cell culture. |
| Trypsin/EDTA | Proteolytic enzyme (trypsin) disaggregates adherent cells; EDTA chelates calcium to enhance trypsin activity [2] [5]. | Exposure time must be optimized to avoid cellular damage. |
| Cryoprotectant (DMSO) | Prevents intracellular ice crystal formation during the freezing process, protecting cell viability [6]. | Must be removed promptly after thawing. |
| Antibiotics/Antimycotics | Used to prevent bacterial and fungal contamination in culture [2]. | Not a substitute for aseptic technique; can mask low-level contamination. |
| PBS (Phosphate Buffered Saline) | An isotonic salt solution used for washing cells and diluting reagents without causing osmotic shock. | Lacking calcium and magnesium, it is ideal for rinsing before trypsinization. |
| pH Indicator (Phenol Red) | Visual indicator of culture medium pH (yellow: acidic; red: normal; purple: basic) [4]. | A color change can indicate microbial contamination or metabolic stress. |
Quantitative Data and Market Landscape
The animal cell culture market is a multi-billion dollar industry, characterized by robust growth and significant commercial investment. The following tables summarize key quantitative data.
Table 2: Animal Cell Culture Market Metrics and Forecasts
| Metric | Value/Range | Context & Timeframe |
|---|---|---|
| Global Market Value (Est.) | ~USD 15 Billion [8] | Base Year 2023 |
| Projected CAGR | 8% - 11.3% [7] [8] | Forecast Period 2025-2032 |
| North America Market Share | ~40% [7] | Largest regional market, driven by strong biopharma R&D. |
| Biopharmaceutical Manufacturing Segment Share | ~65% [8] | Largest application segment (therapeutic proteins, mAbs, vaccines). |
| Leading Company Market Concentration | ~60% shared by Life Technologies, Thermo Fisher, Merck Millipore, Corning [8] | Reflects an oligopolistic market structure. |
Table 3: Standard Mammalian Cell Culture Conditions and Parameters
| Parameter | Typical Setting | Notes |
|---|---|---|
| Temperature | 37°C [4] | Mimics core body temperature for human and many mammalian cells. |
| CO2 Concentration | 5% [4] | Works with bicarbonate buffer in media to maintain physiological pH (~7.4). |
| Relative Humidity | 95% [4] | Preents evaporation of culture medium. |
| Growth Medium pH | 7.2 - 7.4 [4] | Critical for enzyme function and cell health; monitored via phenol red. |
Core Applications in Research and Bioproduction
Biopharmaceutical Manufacturing
Animal cell culture is indispensable for producing complex, glycosylated therapeutic proteins that cannot be synthesized in microbial systems like E. coli [1] [3]. Chinese Hamster Ovary (CHO) cells are the predominant industrial workhorse due to their robustness in suspension culture and ability to perform human-compatible post-translational modifications [3]. Key product classes include:
- Monoclonal Antibodies (mAbs): Used for treating cancer, autoimmune diseases, and infectious diseases [1] [3]. Industrial antibody titers can now exceed 5 g/L in optimized processes [1].
- Hormones and Enzymes: Examples include recombinant insulin for diabetes and erythropoietin (EPO) for anemia [1] [3].
- Other Therapeutic Proteins: Including clotting factors for hemophilia, interferons, and interleukins [1] [2].
Vaccine Production
The technique is fundamental to modern virology and vaccine development. Cell-based methods have largely replaced egg-based production for many viruses, offering faster scalability and reduced risk of allergic reactions [1] [3]. Viral vaccines for diseases such as chicken pox, polio, rabies, hepatitis B, and measles are produced using mass culturing of animal cell lines [1]. The recent COVID-19 pandemic underscored the value of cell culture platforms for rapid pandemic response.
Basic and Translational Research
Cell cultures provide a simplified, controlled model system for a wide range of research applications:
- Cancer Research: Cultures are used to characterize cancer cells and study the role of chemicals, viruses, and radiation in carcinogenesis [1] [2].
- Drug Screening and Toxicity Testing: Cell-based assays are used to study the effects and toxicity of new drug candidates, providing a bridge between in vitro biochemical assays and complex in vivo models [1] [3].
- Gene Therapy: Animal cell cultures are used for the development and testing of gene-modifying techniques, where cells with defective genes are replaced with functional ones [1] [2].
- Model Systems: They are vital for studying basic cell biology, cell cycle mechanisms, specialized cell function, and cell-cell interactions [1].
Emerging Trends and Future Perspectives
The field of animal cell culture is dynamic, with several advanced technologies shaping its future:
- 3D Cell Culture and Organ-on-a-Chip (OOC): These technologies aim to better mimic the in vivo microenvironment by growing cells in three-dimensional structures, often under perfusion. A 2023 meta-analysis concluded that while gains from perfusion in standard 2D cultures are modest, 3D cultures show a slight but significant improvement under flow, suggesting that high-density cultures benefit from enhanced mass transport [9]. OOCs are used to model organs like the intestine, liver, and lung for more physiologically relevant drug screening and disease modeling [9].
- Advanced Media Formulations: The shift towards serum-free and chemically defined media continues, driven by the need for consistency, reduced contamination risk, and compliance with regulatory requirements [8].
- Automation and High-Throughput Processing: Integration of automation, single-use bioreactor technologies, and artificial intelligence (AI) for process optimization is enhancing efficiency, scalability, and reproducibility in both research and bioproduction settings [7] [8].
- Cell and Gene Therapies: The rise of advanced therapeutic medicinal products (ATMPs), including CAR-T cells and other genetically modified cell therapies, is creating new demands and driving innovation in cell culture scale-up and manufacturing processes [8].
The foundation of modern microbiological and biomedical research rests heavily on the ability to culture and study animal cells in vitro. For researchers and drug development professionals, the choice of cellular model is a critical first step that directly influences the physiological relevance, reproducibility, and translational potential of experimental data. This decision most frequently centers on selecting between two fundamental systems: primary cell cultures and immortalized cell lines [10]. Primary cells are isolated directly from human or animal tissues and undergo minimal manipulation, preserving the original characteristics and functions of the tissue of origin [11] [12]. In contrast, immortalized cell lines are populations of cells that have acquired the ability to proliferate indefinitely, either through intentional genetic modification or as a result of spontaneous mutation in cancer-derived cells [11] [13]. The core distinction of "finite vs. infinite growth" underpins every aspect of their use, from experimental design to data interpretation. This guide provides an in-depth technical comparison of these systems, framing them within the broader context of animal cell culture basics for microbiological research.
Core Principles and Fundamental Differences
Defining the Cellular Models
Primary Cell Cultures are initiated directly from tissue obtained from a human donor or animal. The isolation process involves mechanical or enzymatic dissociation of the tissue into a single-cell suspension, which is then placed in a culture vessel with a suitable growth medium [10] [12]. These cultures are considered primary from the point of isolation until their first subculture. Once passaged, they become a cell line [10]. Primary cells are finite; they undergo a limited number of population doublings (typically up to 10) before entering a state of senescence, where they remain metabolically active but cease to divide [10] [12]. Their key advantage is the retention of genetic and phenotypic stability and a close match to in vivo function, making them highly physiologically relevant [11] [14].
Immortalized Cell Lines are derived from primary cultures that have undergone a transformative genetic event, allowing them to escape senescence and proliferate indefinitely [12]. This transformation can occur spontaneously, often in cultures derived from tumor tissue (e.g., HeLa cells from cervical cancer), or be induced deliberately via viral genes or the introduction of oncogenes [11] [13]. These infinite cells are the workhorses of many laboratories due to their robustness, ease of culture, and ability to be expanded without limitation [15] [16]. However, this very transformation means they may lack key functions or characteristics of normal cells and often shift their cellular resources towards proliferation, which can compromise their biological relevance [11] [16].
The following table summarizes the critical differences between primary cells and immortalized cell lines, providing a clear, quantitative comparison for researchers.
Table 1: Comprehensive Comparison of Primary Cells and Immortalized Cell Lines
| Feature | Primary Cells | Immortalized Cell Lines |
|---|---|---|
| Origin & Definition | Isolated directly from donor tissue [11] | Derived from tumors or intentionally immortalized [11] |
| Lifespan | Finite (limited population doublings) [11] [12] | Infinite (can proliferate indefinitely) [11] |
| Physiological Relevance | High; closely resembles in vivo cell function [11] [14] | Low to moderate; may lack key functions, often cancer-derived [11] [15] |
| Genetic & Phenotypic Stability | High genomic stability, but can drift with passaging [14] [10] | Subject to genetic drift and proteomic changes with continuous culture [14] [16] |
| Donor Characteristics | Retained (e.g., HLA type, CMV status, disease state) [11] [14] | Not available [11] |
| Reproducibility & Variability | High donor-to-donor variability [15] | Highly reproducible, but prone to cross-contamination and misidentification [14] |
| Maintenance Difficulty | High; require optimized conditions, more fastidious [10] [12] | Low; robust, easy to culture and maintain [10] [15] |
| Cost & Scalability | High cost, limited scalability [15] | Low cost, highly scalable for high-throughput studies [15] |
| Typical Applications | Disease modeling, drug toxicity testing, immunology, metabolic studies [11] [12] | High-throughput screening, functional genomics, basic mechanistic studies, vaccine production [11] [15] [16] |
The choice between these systems involves a direct trade-off. Primary cells offer biological fidelity at the expense of practicality and scalability, while immortalized cell lines offer practical convenience at the expense of physiological relevance [15]. This trade-off is visually summarized in the following decision-making workflow.
Detailed Methodologies and Experimental Protocols
Establishing and Maintaining Primary Cultures
The process of creating a primary cell culture is technically demanding and requires meticulous attention to detail to preserve cell viability and function.
A. Isolation and Initial Culture: The foundational step is the dissociation of tissue. The digestion method uses proteolytic enzymes like trypsin or collagenase to break down the extracellular matrix, creating a single-cell suspension [10]. The tissue explant method involves mincing tissue into small fragments and allowing cells to migrate out from these fragments onto the culture vessel surface, which is often pre-coated with collagen to enhance attachment [10]. For inherently non-adherent cells like those from blood or bone marrow, suspension culture is used, typically involving density gradient centrifugation for separation [10]. Upon isolation, cells are resuspended in a specialized growth medium. This medium is typically supplemented with serum (e.g., Fetal Bovine Serum) to provide growth factors and other essential components, and often includes antibiotics like penicillin/streptomycin initially to prevent contamination from the host tissue [12]. The culture is incubated at 37°C in a humidified atmosphere with 5% CO₂ to maintain physiological pH [13] [12].
B. Maintenance and Passaging: Primary cells are typically passaged when they reach 80-90% confluency, before they contact-inhibit and potentially differentiate [12]. The process for adherent cells involves:
- Washing with a balanced salt solution to remove serum residues.
- Digestion using a low concentration of trypsin/EDTA to disrupt cell-cell and cell-substrate bonds. The trypsinization process is temperature-sensitive and must be carefully monitored to avoid over-digestion, which can damage cell surface receptors [10].
- Neutralization of the trypsin using serum-containing medium.
- Centrifugation and resuspension in fresh medium for seeding into new culture vessels at an appropriate density [12].
C. Cryopreservation and Recovery: For long-term storage, primary cells are cryopreserved using a controlled-rate freezer. The standard cryopreservation medium consists of a mixture of 80% complete growth medium, 10% FBS, and 10% DMSO as a cryoprotectant [12]. Cells are frozen at a slow rate of -1°C per minute to minimize the formation of lethal intracellular ice crystals and stored in liquid nitrogen or its vapor phase [12]. Upon thawing, a rapid process in a 37°C water bath is critical. It is recommended to seed the cells immediately after thawing and replace the medium containing DMSO within 24 hours, as DMSO can be toxic to primary cells upon prolonged exposure [12].
Characterizing Immortalized Cell Lines
While immortalized cells are easier to maintain, their identity and stability must be actively managed to ensure experimental integrity.
A. Authentication and Contamination Control: A significant risk with continuous cell lines is misidentification and cross-contamination [14]. A prominent example is the widespread contamination of various cell lines with HeLa cells [14]. To combat this, guidelines, including those from leading journals, now recommend Short Tandem Repeat (STR) profiling as a genetic fingerprint to authenticate cell lines [14] [10]. Furthermore, routine screening for mycoplasma and other microbial contaminants is essential, as studies have found a significant portion of cell lines to be contaminated, which can drastically alter cell physiology and experimental outcomes [14].
B. Assessing Functional Phenotype: Given their adapted nature, it is crucial to understand how an immortalized cell line differs functionally from its primary counterpart. Quantitative proteomic techniques, such as SILAC (Stable Isotope Labeling by Amino acids in Cell culture), can be employed to compare the proteomes of cell lines and primary cells [16]. This methodology allows for the identification of specific functional deficits. For instance, a comparative study of the Hepa1-6 hepatoma cell line and primary hepatocytes revealed that the cell line had a deficiency in mitochondrial proteins, a drastic up-regulation of cell cycle functions, and a shutdown of key liver-specific drug-metabolizing enzymes [16]. This kind of analysis provides a rational basis for determining if a cell line is suitable for a particular research question.
The Scientist's Toolkit: Essential Research Reagents
Successful cell culture, whether primary or immortalized, relies on a suite of essential reagents and materials. The following table details key components of a researcher's toolkit.
Table 2: Key Reagents and Materials for Cell Culture Research
| Reagent/Material | Function/Purpose | Technical Notes |
|---|---|---|
| Culture Vessels (flasks, plates) | Provide a sterile, biocompatible surface for cell growth. | Treated plastic for adherent cells; specialized low-attachment plates for suspension or 3D cultures [13]. |
| Basal Medium (e.g., DMEM, RPMI-1640) | Provides essential nutrients, salts, and energy sources (glucose). | The foundation to which supplements are added [13] [12]. |
| Serum (e.g., Fetal Bovine Serum - FBS) | Source of growth factors, hormones, lipids, and attachment factors. | Introduces variability; defined serum-free media are preferred for consistent results [13] [12]. |
| Antibiotics/Antimycotics (e.g., Penicillin/Streptomycin) | Prevent bacterial and fungal contamination. | Use is recommended for primary isolation but can be avoided in established, sterile cultures to avoid masking low-level contamination [12]. |
| Dissociation Agents (e.g., Trypsin, Collagenase) | Enzymatically digest extracellular matrix to dissociate tissues or detach adherent cells for passaging. | Concentration and incubation time must be optimized to prevent cell damage [10] [12]. |
| Cryoprotectant (e.g., DMSO) | Prevents intracellular ice crystal formation during freezing. | Must be removed promptly after thawing due to potential cytotoxicity [12]. |
| Extracellular Matrix (ECM) Coatings (e.g., Collagen, Matrigel) | Mimics the natural cellular environment, enhancing attachment, proliferation, and differentiation. | Crucial for culturing sensitive primary cells and for 3D culture models like organoids [10] [13]. |
| Buffering Systems (e.g., HEPES) | Maintains physiological pH (approx. 7.4) in the culture medium. | HEPES is useful for procedures outside a CO₂ incubator, while the CO₂/bicarbonate system is standard within an incubator [13] [12]. |
Application Scenarios and Decision Framework
The strengths and weaknesses of primary cells and cell lines make them suited for different stages and types of research. The following diagram maps their application across the drug discovery and development pipeline, illustrating how they can be used complementarily.
Primary Cells are indispensable in applications where physiological relevance is paramount. They are the gold standard for:
- Drug Screening and Toxicity Testing: Evaluating the efficacy and safety of new drug candidates in a system that closely mimics the human in vivo response [14] [12].
- Disease Modeling: Studying the pathophysiology of diseases using cells derived from patients, allowing for the investigation of specific genetic backgrounds and disease mechanisms [12].
- Immunology and Vaccine Development: Investigating immune cell function, signaling, and response to pathogens or vaccines, as they retain their native receptors and functions [11].
- Advanced 3D Models: Serving as the building blocks for more complex ex vivo systems like organoids and organs-on-chips, which better recapitulate tissue structure and function [13].
Immortalized Cell Lines excel in projects that require scale, consistency, and genetic tractability:
- Large-Scale Functional Genomics: Genome-wide siRNA or CRISPR screens to identify gene functions, where millions of identical cells are required [15] [16].
- Biomolecule Production: Large-scale production of proteins, antibodies, and vaccines (e.g., polio, rabies) due to their infinite expandability [12].
- Basic Mechanistic Studies: Investigating fundamental cellular processes like the cell cycle, where their robustness and reproducibility are advantageous [16].
The dichotomy between finite primary cells and infinite immortalized lines represents a fundamental compromise in biological research: fidelity versus convenience. While primary cells provide a window into native human (or animal) biology, their practical limitations are significant. Conversely, the robustness and scalability of immortalized cell lines are offset by their often poor predictive power for human physiology, contributing to high failure rates in drug development, particularly in complex areas like central nervous system diseases [15].
The future of in vitro modeling is being shaped by technologies that aim to bridge this gap. Human-induced pluripotent stem cells (iPSCs) represent a powerful alternative, as they can be renewed indefinitely like cell lines and differentiated into human-specific somatic cells [13] [15]. Furthermore, deterministic reprogramming technologies, such as the opti-ox platform, are emerging to address the batch-to-batch variability and lengthy differentiation processes associated with traditional iPSC workflows. These systems can generate consistent, scalable, and functionally validated human cells (ioCells) designed to combine the physiological relevance of primary cells with the reproducibility and ease of use of cell lines [15]. As regulatory bodies like the FDA begin to endorse such New Approach Methodologies (NAMs), the field is moving toward a future where researchers will no longer have to choose between biological relevance and practical utility, thereby accelerating the translation of basic research into effective clinical applications [15].
The foundation of many advances in biologics, gene therapy, and drug discovery rests upon the robust cultivation of animal cells. For microbiologists transitioning into mammalian cell culture systems, understanding the fundamental distinction between adherent and suspension cultures is paramount. These are not merely different technical approaches but represent distinct biological states that profoundly impact cellular morphology, function, and experimental outcomes. Adherent cell cultures proliferate by attaching to a solid, growth-promoting substrate, a property known as "anchorage dependence" [17]. In contrast, suspension cell cultures reproduce freely while suspended in the culture medium, without attachment to any surface [18]. This dichotomy in growth requirement dictates every subsequent aspect of experimental design, from vessel selection and medium formulation to passaging protocols and scaling potential. The choice between these systems is often dictated by the cell line's innate characteristics, the required yield, and the final application, whether for basic research, viral vector production, or therapeutic protein manufacturing [19] [20].
Core Principles and Morphological Characteristics
Defining Adherent Cell Culture
Adherent cells require a solid, biologically compatible surface for attachment and proliferation. This anchorage dependence is a characteristic of many primary cells and cell lines derived from tissues that naturally function in a stationary, structured environment in vivo, such as fibroblasts and epithelial cells [6]. The attachment process is mediated by cell surface receptors that interact with specific proteins on the substrate, leading to cytoskeletal reorganization and the characteristic spread morphology of adherent cells. A key feature of adherent culture is contact inhibition; once the cells have proliferated to cover the entire available surface (reached confluency), they cease dividing [6]. This necessitates a subculturing process, known as passaging, to detach a portion of cells and seed them into a new vessel to maintain exponential growth.
Defining Suspension Cell Culture
Suspension cells grow and multiply freely floating in the culture medium. This growth mode is typical of cells derived from blood, such as lymphocytes, and certain immortalized cell lines (e.g., HL-60, WEHI-231) that have lost their anchorage requirement [18]. Because they are not limited by surface area, suspension cultures can achieve much higher cell densities in a given volume compared to adherent systems. They are maintained by diluting the culture with fresh medium once the cell concentration reaches a predetermined maximum, a process simpler than the enzymatic detachment required for adherent cells [18]. This makes them inherently more scalable, which is a critical advantage for industrial bioprocessing.
Comparative Analysis: Morphology and Growth Dynamics
The physical growth requirements directly translate to distinct morphological and behavioral characteristics, summarized in the table below.
Table 1: Core Characteristics of Adherent vs. Suspension Cultures
| Feature | Adherent Culture | Suspension Culture |
|---|---|---|
| Growth Requirement | Requires attachment to a solid substrate (anchorage-dependent) [17]. | Grows freely floating in the medium (anchorage-independent) [18]. |
| Cell Morphology | Spread, flattened, and elongated shapes; strong cell-surface and cell-cell interactions [21]. | Typically spherical or rounded morphology; growth as single cells or small aggregates [18]. |
| Growth Surface | Requires tissue-culture (TC) treated vessels (e.g., red-coded standard or yellow-coded Cell⁺ surfaces) [22]. | Uses non-TC-treated, hydrophobic vessels (e.g., green-coded surfaces) to prevent attachment [22]. |
| Passaging Method | Enzymatic (e.g., trypsin) or non-enzymatic dissociation reagent required for detachment [17]. | Simple dilution of the cell suspension into fresh medium; no detachment needed [18]. |
| Confluence Check | Microscopic observation of monolayer coverage [17]. | Medium appears turbid (cloudy) when the culture flask is swirled [18]. |
| Scalability | Scaled out by increasing surface area (e.g., more flasks, multi-layered vessels) [19]. | Scaled up by increasing culture volume (e.g., larger bioreactors) [19]. |
| Typical Applications | Primary cells, cell lines for viral plaque assays, epithelial and fibroblast studies [21]. | Production of recombinant proteins, antibodies, and viral vectors; hematopoetic cell studies [19]. |
Experimental Protocols for Culture Maintenance
Subculturing Adherent Cells
The passaging of adherent cells is a critical skill for maintaining healthy, proliferative cultures. The following protocol details the standard procedure using a dissociation reagent like trypsin [17].
Table 2: Materials for Adherent Cell Passaging
| Material/Reagent | Function |
|---|---|
| Complete Growth Medium | Provides nutrients, growth factors, and serum to support cell growth. Pre-warmed to 37°C. |
| Balanced Salt Solution (without Ca2+/Mg2+) | Washes away residual serum and divalent cations that inhibit trypsin. |
| Dissociation Reagent (e.g., Trypsin) | Proteolytic enzyme that digests adhesion proteins, detaching cells from the surface. |
| Trypan Blue Stain | Dye used with a hemocytometer or automated cell counter to determine cell viability and count. |
Step-by-Step Protocol [17]:
- Confirm Cell Confluency: Visually inspect cells under a microscope. Passage when they are 80-90% confluent and in the log phase of growth, with viability >90%.
- Remove Spent Medium: Aspirate and discard the used culture medium from the vessel.
- Wash Cell Layer: Gently add a balanced salt solution (without calcium and magnesium) to the side of the vessel opposite the cell layer. Rock the vessel to wash the cells, then aspirate and discard the solution. This step removes serum that would inhibit trypsin.
- Add Dissociation Reagent: Add pre-warmed dissociation reagent (e.g., trypsin) to cover the cell layer. Gently rock the vessel for complete coverage.
- Incubate: Incubate the vessel at room temperature for approximately 2 minutes (time varies by cell line).
- Check for Detachment: Observe under a microscope. If less than 90% of cells are detached (rounded and floating), tap the vessel gently and continue incubation, checking every 30 seconds.
- Neutralize Reaction: When most cells are detached, add a volume of complete growth medium that is at least double the volume of trypsin used. Pipette the medium over the cell layer surface to dislodge any remaining cells and neutralize the enzyme.
- Centrifuge: Transfer the cell suspension to a centrifuge tube and spin at approximately 200 x g for 5-10 minutes.
- Resuspend and Count: Discard the supernatant and resuspend the cell pellet in a small volume of fresh medium. Take a sample to count cells and assess viability using trypan blue.
- Seed New Flasks: Dilute the cell suspension to the recommended seeding density and pipette into new culture vessels. Return the vessels to the incubator.
Subculturing Suspension Cells
Maintaining suspension cells is generally less labor-intensive, as it does not require a detachment step. The protocol focuses on controlling cell density to keep cells in the exponential growth phase [18].
Step-by-Step Protocol [18]:
- Assess Culture Density: Check the culture for turbidity (cloudiness) and the presence of cell clumps. If cells have settled, swirl the flask to resuspend them evenly.
- Sample and Count: Aseptically remove a small sample of the cell suspension. Determine the total cell count and percent viability using an automated cell counter or hemocytometer with trypan blue.
- Calculate Dilution: Calculate the volume of fresh, pre-warmed growth medium needed to dilute the culture down to the recommended seeding density for the cell line.
- Passage the Culture: Aseptically add the required volume of fresh medium into the culture flask. Alternatively, you can centrifuge the culture (e.g., 10 minutes at 800 x g) to remove the spent medium and metabolic waste, then resuspend the cell pellet in a fresh, appropriate volume of medium [18].
- Maintain Gas Exchange: For shaker flasks, loosen the caps one full turn. For spinner flasks, loosen the side arm caps to allow for proper gas exchange before returning them to the incubator or shaker.
The workflow for handling both culture types is fundamentally different, as illustrated below.
The Scientist's Toolkit: Essential Reagents and Materials
Successful cell culture relies on a suite of specialized reagents and materials. The selection is often specific to the culture type.
Table 3: Essential Research Reagent Solutions for Cell Culture
| Item | Function | Adherent Culture | Suspension Culture |
|---|---|---|---|
| Culture Vessels | Provides the environment for cell growth. | TC-treated flasks/dishes/plates (Red: Standard; Yellow: Cell⁺ for sensitive cells) [22]. | Non-TC-treated, hydrophobic flasks (Green-coded); spinner or shaker flasks [18] [22]. |
| Complete Growth Medium | Provides nutrients, energy, and essential growth factors. | Formulated with serum or defined supplements; often contains calcium to promote adhesion. | Serum-free or serum-containing; may lack calcium to minimize aggregation; may contain surfactants (e.g., Pluronic F-68) to reduce shear [18]. |
| Dissociation Reagent | Detaches adherent cells for subculturing. | Essential (e.g., trypsin, TrypLE) [17]. | Not required for routine passaging. |
| Cell Counter & Viability Stain | Determines cell concentration and health. | Essential for determining seeding density (e.g., hemocytometer, automated counter with Trypan Blue) [17]. | Essential for determining dilution ratio (e.g., hemocytometer, automated counter with Trypan Blue) [18]. |
| Centrifuge | Pellet cells for medium change or after detachment. | Used after trypsinization to remove the dissociation reagent [17]. | Used periodically to remove waste products and refresh medium [18]. |
Scaling and Industrial Applications: A Case-Based Analysis
The choice between adherent and suspension systems becomes critically strategic when moving from laboratory research to industrial-scale manufacturing, particularly in the field of viral vector production for gene therapies.
Scale-Up Philosophies and Economic Drivers
The scalability of a process is a major determinant of its commercial viability. Adherent cultures are typically scaled out by increasing the available surface area, for instance, by using more roller bottles, multi-layered stacks (e.g., Cell Factories), or fixed-bed bioreactors (e.g., iCELLis) [19]. While this is effective, it can become labor-intensive, space-consuming, and challenging for ensuring batch-to-batch consistency at very large scales. In contrast, suspension cultures are scaled up by simply increasing the volume in stirred-tank bioreactors (STRs), a well-established and highly efficient method in traditional biologics [19]. This allows for a much higher volumetric cell density and is generally more amenable to process automation and monitoring.
Case Studies in Viral Vector Manufacturing
The industry currently employs both platforms, with the choice often dictated by the specific product and stage of development.
Adherent Platform Success:
- Zolgensma (Novartis): This AAV9-based gene therapy for spinal muscular atrophy is manufactured using an adherent HEK293 process in an iCELLis fixed-bed bioreactor. This platform was deemed a commercially viable solution, demonstrating that adherent processes can be successfully scaled [19].
- Luxturna (Spark Therapeutics/Roche): This AAV2-based therapy also uses an adherent HEK293 process in roller bottles, a classic scale-out approach suitable for its required dosage and patient population size [19].
Suspension Platform Adoption:
- Glybera (UniQure): This was the first Western-approved gene therapy to use a suspension-based process. The switch from an initial adherent process to suspension HEK293 cells was driven by the need for higher vector quantities [19].
- Industry Trend: Many companies, including pioneers like Bluebird Bio, have explicitly stated intentions to adapt their manufacturing processes from adherent to suspension platforms for certain products to achieve better scalability and cost-effectiveness [19].
Molecular Insights from HEK293 Adaptation
The transition of cell lines like HEK293 from adherent to suspension growth is not merely a change in protocol but involves underlying molecular adaptations. Genomic and transcriptomic analyses of various HEK293 derivatives have revealed significant changes in gene expression associated with cellular component organization, cell motility, and cell adhesion between adherent and suspension subtypes [20]. Furthermore, specific metabolic pathway switching, such as in cholesterol biosynthesis, and the differential expression of key genes (including RARG, ID1, and ZIC1), have been identified as hallmarks of the suspension-adapted phenotype [20]. This molecular understanding is crucial for rationally designing and optimizing cell lines for large-scale bioproduction.
The decision to utilize an adherent or suspension culture system is a foundational one that resonates through every aspect of a research or production workflow. Adherent cultures, with their anchorage-dependent growth and characteristic spread morphology, are indispensable for studying many primary cells and tissue-specific functions. Suspension cultures, characterized by their anchorage-independent, free-floating growth, offer unparalleled advantages in scalability and ease of handling for industrial bioprocessing. As the field of biologics and gene therapy advances, the ability to adapt processes to suspension-based platforms is increasingly viewed as critical for commercial success. However, as evidenced by current marketed products, well-optimized adherent processes remain viable and important. A deep understanding of the morphological, procedural, and molecular distinctions between these two systems empowers scientists to make informed decisions, optimize culture conditions, and robustly scale their processes to meet the demands of modern biotechnology.
For microbiologists venturing into the realm of animal cell culture, the familiar principles of microbiology serve as a foundation, but the specific requirements diverge significantly. The core challenge lies in the fundamental biological differences: microbial cells are often prokaryotic, self-sufficient, and robust, whereas mammalian cells are eukaryotic, fastidious, and require a highly complex and controlled environment to mimic their natural in vivo conditions [23]. This guide provides a detailed, technical comparison of the nutrient, environmental, and equipment needs for these two distinct cell culture systems, framing the information within the context of adapting a microbiologist's existing knowledge and skills. Understanding these contrasts is crucial for successful experimental outcomes in fields like drug development, biopharmaceutical production, and basic biological research.
Core Differences in Culture Media and Nutrients
The composition of culture media is the most pronounced difference between these two systems, directly reflecting the differing metabolic and biosynthetic capabilities of the cells.
Media Composition: A Side-by-Side Comparison
The table below summarizes the key compositional differences in media designed for microbial versus mammalian cell culture.
Table 1: Core Compositional Differences in Culture Media
| Component | Microbial Culture Media [24] [25] | Mammalian Cell Culture Media [26] [25] |
|---|---|---|
| Carbon Source | Often simple sugars (e.g., glucose) for energy. | Glucose, but also other carbon sources; part of a complex energy matrix. |
| Nitrogen Source | Inorganic (e.g., ammonium salts, nitrates) or simple organic sources. | Primarily organic, from amino acids and complex protein hydrolysates. |
| Growth Factors | Generally not required; cells synthesize their own. | Essential. Provided by serum (e.g., FBS) or defined additives like specific hormones and growth factors. |
| Buffering System | Often relies on salts within the medium. | CO₂-bicarbonate system is common, requiring a controlled CO₂ atmosphere (typically 5-10%) in incubators [27]. |
| pH Indicator | May be present. | Commonly uses phenol red, which transitions from yellow (acidic) to red (basic) over pH 6.2–8.2 [25]. |
| Additional Components | Selective agents (antibiotics, dyes) for isolating specific microbes. | Antibiotics (e.g., Penicillin-Streptomycin) to prevent bacterial contamination [25]. Attachment factors (e.g., collagen) for adherent cells. |
Media Formulation and Selection
The historical development and philosophy behind media formulation also differ. Microbial media can range from defined minimal media, containing only the bare essentials for growth, to complex media containing poorly defined mixtures like yeast or meat extracts, which support a wide variety of microbes [24] [25]. The choice depends on whether the goal is to select for specific microbes or to promote broad growth.
In contrast, mammalian cell culture media are inherently complex. The field has evolved from using natural media (e.g., plasma, tissue extracts) to a variety of synthetic media formulations [26]. These are categorized based on the presence of undefined components:
- Serum-Containing Media: Supplemented with animal serum (e.g., Fetal Bovine Serum, FBS), which provides a wide range of growth factors, hormones, and attachment factors. While highly effective for many cell types, it introduces batch-to-batch variability and undefined conditions [26].
- Serum-Free Media (SFM): Formulated with defined supplements (e.g., bovine serum albumin, growth factors) to replace serum, improving reproducibility and facilitating downstream processing.
- Chemically Defined Media: Contain only highly purified ingredients and recombinant proteins, offering the highest level of reproducibility and control, which is critical for biopharmaceutical manufacturing [26].
For a microbiologist, this shift means moving from media that controls which cells grow to media that meticulously supports the survival of a single, specific cell type.
Environmental and Physical Conditions
The physical environment required for cultivation is another area of stark contrast, driven by the different origins of the cells.
Key Environmental Parameters
Table 2: Comparison of Critical Environmental Conditions
| Parameter | Microbial Culture | Mammalian Cell Culture |
|---|---|---|
| Temperature | Variable, often 25°C - 37°C, depending on the microbe's natural habitat. | Strictly 36°C - 37°C for most mammalian cells to mimic core body temperature [27]. |
| pH | Can tolerate a broader range, often optimized for specific organisms. | Narrow range, typically pH 7.2 - 7.4, tightly regulated by a CO₂-bicarbonate buffer system [27] [25]. |
| Osmotic Pressure | Controlled by salts in the medium. | Critical and sensitive; requires a carefully balanced isotonic solution. |
| Oxygen Requirements | Varies greatly (aerobic, anaerobic, facultative). Can often tolerate higher dissolved oxygen tensions. | Most are aerobic, but require precise dissolved oxygen control; high shear stress from sparging can damage cells [28]. |
Growth Dynamics and Observation
Microbial growth in liquid media often leads to visible turbidity, which can be quantified with a spectrophotometer. On solid media, they form distinct, macroscopic colonies.
Mammalian cells, however, require microscopic observation. Their growth phases—lag, log (exponential), stationary, and decline—are analogous to microbial growth curves but are tracked differently [6]. Adherent cells must be observed under an inverted microscope to assess confluency (the percentage of the growth surface covered by cells), which determines when they need to be subcultured [6]. Suspension cells are monitored for cell concentration and viability using dyes like Trypan Blue and counted with a hemocytometer or automated cell counter [29] [30].
Diagram: Mammalian cell growth requires passaging to maintain health.
Essential Laboratory Equipment and Setup
While a microbiologist's lab will have familiar equipment, the emphasis and specific types of tools required for mammalian cell culture are distinct and non-negotiable for maintaining aseptic and controlled conditions.
Equipment Comparison and Purpose
Table 3: Contrasting Key Laboratory Equipment
| Equipment | Role in Microbiology | Role in Mammalian Cell Culture |
|---|---|---|
| Containment Cabinet | A laminar flow hood may be used for sterility, but its primary purpose is to protect the sample from contaminants [31]. | A Biosafety Cabinet (BSC Class II) is essential. It protects the sample from contamination and protects the user from biohazards using HEPA-filtered exhaust air [31] [29]. |
| Incubator | Often a simple dry-heat incubator set to a specific temperature. | A humidified CO₂ incubator is mandatory to precisely control temperature, CO₂ (for pH balance), and high humidity (to prevent evaporation) [27] [29]. |
| Microscope | Standard compound microscope for viewing stained slides. | An inverted microscope is standard for viewing adherent cells in flasks and plates without disturbing them [30]. |
| Preservation | Short-term refrigeration or freezing; long-term at -80°C or freeze-drying. | Cryopreservation in liquid nitrogen (-130°C to -196°C) is essential for long-term storage of most cell lines to maintain genetic and phenotypic stability [29] [6]. |
| Cell Counter | Spectrophotometer for measuring turbidity (optical density). | Hemacytometer or automated cell counter is used to count cells and assess viability (live/dead ratio) before experiments [29] [30]. |
The Aseptic Workflow and Contamination Control
The consequence of contamination is far more catastrophic in mammalian cell culture. Whereas a bacterial culture might overcome a minor fungal spore contamination, the same contaminant will typically obliterate a mammalian cell culture. Furthermore, mammalian cells can be infected by mycoplasma, a type of bacteria that does not cause turbidity and is invisible under a standard microscope, requiring specialized PCR or staining techniques for detection [6].
This necessitates rigorous aseptic technique, which goes beyond standard microbiological practice. Key measures include:
- Working exclusively within a BSC that has been properly sterilized with ethanol before and after use.
- Using antibiotic-containing media judiciously (as a backup, not a substitute for aseptic technique).
- Routinely checking cells for contamination (bacterial, fungal, and mycoplasma).
- Creating master and working cell banks to preserve low-passage cells [6].
Diagram: The core mammalian cell culture workflow relies on specialized equipment.
Strategic Applications in Bioprocessing
The choice between microbial and mammalian systems is strategic, driven by the nature of the desired biologic product.
- Microbial Fermentation is favored for producing smaller, non-glycosylated molecules such as peptides, cytokines, growth factors, plasmid DNA (pDNA), and antibody fragments. Its advantages include shorter process times, higher production yields, and lower costs [23]. Organisms like E. coli and S. cerevisiae are well-established workhorses.
- Mammalian Cell Culture is the dominant platform for producing large, complex proteins that require specific post-translational modifications, most notably glycosylation. This includes monoclonal antibodies (mAbs), recombinant hormones, and many viral vaccines. Chinese Hamster Ovary (CHO) cells are the most commonly used mammalian host [23]. While more expensive and time-consuming, they are often the only system that can produce a functionally active product.
The Scientist's Toolkit: Essential Reagents and Materials
For the microbiologist transitioning to mammalian cell culture, familiarity with the following core reagents is critical.
Table 4: Essential Reagent Toolkit for Mammalian Cell Culture
| Reagent/Material | Function | Notes for Microbiologists |
|---|---|---|
| Basal Medium (e.g., DMEM, RPMI-1640) [26] | Provides essential salts, vitamins, and amino acids. | Far more complex than LB broth; often requires supplementation to be complete. |
| Fetal Bovine Serum (FBS) [26] | Provides a source of growth factors, hormones, and attachment factors. | A major source of variability and cost. The drive is towards serum-free media. |
| Trypsin/EDTA [6] | Enzyme solution used to dissociate adherent cells from the culture surface for subculturing. | Analogous to the function of lysozyme for breaking down bacterial cell walls, but used gently on living cells. |
| Dimethyl Sulfoxide (DMSO) [29] | A cryoprotectant added to freezing media to prevent ice crystal formation and cell lysis during cryopreservation. | Not typically used in standard microbial culture preservation. |
| Penicillin-Streptomycin (Pen-Strep) [25] | Antibiotic mixture added to media to prevent bacterial contamination. | Use is ubiquitous in research, but is avoided in biomanufacturing to ensure aseptic technique is paramount. |
| HEPES Buffer [27] | An organic chemical buffer that provides additional pH stability outside a CO₂ environment. | Useful for procedures that require extended time outside the incubator. |
For the microbiologist, mastering mammalian cell culture requires a paradigm shift from cultivating robust, independent prokaryotes to nurturing fragile, dependent eukaryotes. The key differences lie in the complexity of the nutrient media, the precision and constancy of the physical environment, and the specialized equipment required to maintain this environment. Success hinges on understanding that mammalian cells are not just "large microbes"; they require a simulated in vivo environment to survive and function. By appreciating these core differences and applying the rigorous, tailored techniques outlined in this guide, researchers can effectively leverage both microbial and mammalian systems to advance their scientific and biotechnological goals.
The foundation of modern microbiological and biomedical research rests significantly on the use of immortalized cell lines, which provide a consistent, renewable, and ethically preferable platform for experimentation. These cell lines, derived from various tissues and often from pathological conditions, allow researchers to dissect complex biological processes, model human diseases, and screen potential therapeutic compounds in a controlled in vitro environment. For microbiologists venturing into cell culture, understanding the origin, characteristics, and specific applications of these cellular tools is paramount to designing robust and reproducible experiments. This guide provides an in-depth technical examination of three cornerstone biological reagents: the ubiquitous HeLa cell line, the hormone-responsive MCF-7 breast cancer model, and the antibody-producing hybridomas.
The selection of an appropriate cell line is a critical first step in any research program, as each possesses a unique set of genetic, phenotypic, and functional attributes that determine its suitability for specific investigations. These attributes include, but are not limited to, morphology, growth kinetics, expression of specific receptors, genetic stability, and functional outputs. Misapplication or a lack of understanding of a cell line's specific properties can lead to erroneous conclusions, a problem compounded by the fact that cell lines can evolve and diverge when maintained in different laboratories. This guide aims to equip researchers with the necessary knowledge to navigate these common cell lines effectively, ensuring that their experimental models are aligned with their scientific questions.
HeLa Cell Line: The Immortal Workhorse
Origin and Historical Context
The HeLa cell line, the first immortal human cell line to be successfully maintained in continuous culture, was derived from a cervical adenocarcinoma of a 31-year-old African American patient, Henrietta Lacks, in 1951 [32] [33] [34]. The cells were taken without her knowledge or consent, a common practice at the time that has since sparked significant ethical discourse and led to major reforms in informed consent and patient rights in research [33] [34]. Named using the first two letters of her first and last name, HeLa cells exhibited an unprecedented ability to proliferate relentlessly in culture, doubling every 20-24 hours [33] [34]. This robustness, coupled with their easy cultivability and susceptibility to numerous viruses, quickly made them a fundamental resource for scientists worldwide, contributing to countless medical breakthroughs.
Key Characteristics and Technical Data
HeLa cells are characterized by their epithelial-like morphology and a set of unique biological properties that underpin their "immortality" and utility. They possess an active form of the enzyme telomerase, which prevents the telomere shortening that normally leads to cellular senescence, allowing them to bypass the Hayflick limit [33]. Genetically, HeLa cells are hypertriploid, with an average of 82 chromosomes (range 70-164) instead of the normal human diploid number of 46 [33]. This complex karyotype, featuring a high degree of aneuploidy and structural rearrangements (including "HeLa signature chromosomes"), is a result of their cancerous origin and transformation by Human Papillomavirus 18 (HPV18) [33] [34]. The initial biopsy contained HPV-18, the integration of which into the human genome was a key event in driving the cancer, a discovery that later contributed to the development of HPV vaccines [34].
Table 1: Key Characteristics of the HeLa Cell Line
| Parameter | Description |
|---|---|
| Origin | Cervical adenocarcinoma; 31-year-old female [33] [34] |
| Morphology | Epithelial-like [33] |
| Growth Properties | Immortalized; doubles every 20-24 hours; bypasses Hayflick Limit [33] |
| Karyotype | Hypertriploid, aneuploid; 70-164 chromosomes (avg. 82) [33] |
| Key Genetic Feature | Transformed by HPV-18; active telomerase [33] [34] |
| Susceptibility | High susceptibility to various viruses (e.g., Polio, Adenovirus) [33] |
Primary Research Applications
The applications of HeLa cells in research are vast and have been instrumental in numerous scientific milestones. Their use is documented in over 60,000 scientific articles, a number that continues to grow [34].
- Virology and Vaccine Development: HeLa cells were crucial for testing the first polio vaccine by Jonas Salk due to their high susceptibility to poliovirus [32] [33] [34]. They have since been used to study a wide array of viruses, including HIV, Zika, mumps, and measles, and were pivotal in research linking HPV to cervical cancer [33] [34].
- Cancer Biology: HeLa cells serve as a model for studying cancer mechanisms, testing chemotherapeutic agents like camptothecin, and investigating the effects of hormones and other compounds on cell proliferation [33].
- Genetics and Cell Biology: They were the first human cells to be successfully cloned and were used to create the first human-animal hybrid, facilitating early gene mapping efforts [34]. Research on HeLa cells has also contributed to our understanding of cellular aging and the effects of radiation and toxins [33] [34].
- Space Biology: In the 1960s, HeLa cells were sent into space to study the effects of zero gravity on human cells, where they were found to divide even more rapidly [34].
MCF-7 Cell Line: A Model for Hormone-Responsive Breast Cancer
Origin and Historical Context
The MCF-7 cell line is one of the most widely studied models of human breast cancer. It was established from a pleural effusion (a complication where cancer cells are found in fluid around the lungs) of a 69-year-old female patient with a metastatic breast adenocarcinoma [35]. The line is named after the Michigan Cancer Foundation, where it was developed. Unlike many other cancer cell lines, MCF-7 cells retain several characteristics of the original mammary epithelium, making them a valuable tool for investigating the biology of breast cancer and its response to therapeutic agents [35].
Key Characteristics and Technical Data
A defining feature of MCF-7 cells is their expression of the oestrogen receptor alpha (ER-α), which makes them a premier model for studying hormone-responsive (luminal A subtype) breast cancer [35]. They also express androgen, progesterone, and glucocorticoid receptors [35]. Morphologically, they exhibit an epithelial-like appearance and form characteristic dome structures in monolayer cultures due to fluid accumulation between the cell layer and the culture dish [35]. A critical consideration for researchers is the well-documented genetic and phenotypic instability of MCF-7 cells. Subpopulations and variants have emerged in different laboratories, leading to significant biological differences between MCF-7 lines obtained from different sources [35] [36]. These differences can include variations in chromosome makeup, growth rate, hormone receptor content, and tumorigenicity in mouse models [36]. For instance, one study found that different MCF-7 lines had varying growth rates and responses to estrogen and antiestrogen treatments, with one line (MCF-7 (ATCC)) being entirely unresponsive to such treatments despite having receptors [36].
Table 2: Key Characteristics of the MCF-7 Cell Line
| Parameter | Description |
|---|---|
| Origin | Pleural effusion of breast adenocarcinoma; 69-year-old female [35] |
| Morphology | Epithelial-like; forms dome structures [35] |
| Key Feature | Expresses oestrogen receptor alpha (ER-α) and other hormone receptors [35] |
| Genetic Stability | Genetically unstable; subpopulations and variants exist [35] |
| Research Caveat | Biological behavior can vary significantly between labs; source documentation is critical [36] |
Primary Research Applications
MCF-7 cells are primarily used as an in vitro model to study breast cancer biology, particularly the role of estrogen signaling in cancer proliferation and survival.
- Hormone Response Studies: Treatment with estrogen has an anti-apoptotic, growth-promoting effect on MCF-7 cells, while anti-estrogen drugs like tamoxifen inhibit proliferation and induce apoptosis [35]. This makes them an excellent model for screening and developing endocrine therapies.
- Drug Resistance Research: Numerous drug-resistant variants of MCF-7 have been intentionally developed, such as lines resistant to tamoxifen (MCF7/TAMR-7), fulvestrant (MCF7/182R-6), and aromatase inhibitors (MCF7/LetR-1) [35]. These sublines are invaluable for understanding the mechanisms of acquired resistance in breast cancer.
- General Cancer Biology: The line is used to study cancer cell invasion, metastasis, and the effects of various chemotherapeutic agents and natural compounds on cancer cell proliferation [35].
Hybridoma Cell Lines: Engines of Monoclonal Antibody Production
Hybridoma technology is a seminal method for producing monoclonal antibodies (mAbs). Invented by Köhler and Milstein in 1975 (for which they received a Nobel Prize in 1984), this technique involves the somatic fusion of antibody-producing B lymphocytes from an immunized animal (typically a mouse) with immortal myeloma cells (cancerous B-cells) [37] [38]. The resulting hybrid cells, termed hybridomas, combine the desired traits of both parents: the ability to produce a single, specific antibody from the B cell, and the capacity for indefinite growth ("immortality") from the myeloma cell [37] [38] [39]. This allows for the limitless production of homogeneous, clonally identical antibodies that recognize a single epitope on an antigen, providing unparalleled specificity compared to polyclonal antibody sera [37].
The Hybridoma Generation Workflow
The production of monoclonal antibodies via hybridoma technology is a multi-step process that requires careful execution at each stage. The following diagram and accompanying description outline the key procedural stages.
Diagram 1: Hybridoma generation and monoclonal antibody production workflow.
- Immunization: A laboratory animal (e.g., mouse) is injected with the antigen of interest over several weeks to stimulate a robust immune response and the production of antigen-specific B cells [37] [38].
- Cell Isolation & Preparation: Activated, antibody-producing B lymphocytes are isolated from the spleen of the immunized animal. In parallel, immortal myeloma cells are prepared; these are selected to be deficient in the hypoxanthine-guanine phosphoribosyltransferase (HGPRT) enzyme, making them sensitive to HAT selection medium [37] [38].
- Cell Fusion: The B cells and myeloma cells are fused together using a fusogen like polyethylene glycol (PEG) or by electrofusion, creating a heterogenous mixture that includes the desired B cell-myeloma hybrids (heterokaryons) [37] [38].
- Hybridoma Selection: The cell mixture is cultured in HAT (hypoxanthine-aminopterin-thymidine) selection medium. Aminopterin blocks the de novo nucleotide synthesis pathway. Unfused B cells have a short natural lifespan and die off. Unfused HGPRT-negative myeloma cells cannot use the salvage pathway and perish. Only the fused hybridomas, which possess the HGPRT enzyme from the B cell and immortality from the myeloma cell, survive and proliferate in HAT medium [37] [38].
- Screening & Cloning: The surviving hybridomas are screened (typically via ELISA) to identify clones that produce the desired antibody [37] [38]. Positive clones are then isolated and cloned, often by limiting dilution, to ensure that the resulting hybridoma line is derived from a single progenitor cell and is truly monoclonal [37] [38].
- Propagation & Production: The stable monoclonal hybridoma cell line can be propagated in vitro (in culture flasks) or in vivo (as ascites in mice) for continuous antibody production [37]. The cells can also be cryopreserved for long-term storage [37].
Primary Research and Clinical Applications
Monoclonal antibodies produced via hybridoma technology have revolutionized biomedical research, diagnostics, and therapeutics.
- Research and Diagnostics: mAbs are indispensable tools for identifying and characterizing cellular markers (e.g., the cluster of differentiation (CD) markers), distinguishing between morphologically similar diseases in histopathology, and detecting occult metastases [38]. They are also used in techniques like ELISA, flow cytometry, western blotting, and immunoaffinity purification [37] [38] [39].
- Therapeutics: Monoclonal antibodies are used to treat a wide range of conditions, including cancer, autoimmune diseases, and infectious diseases [37] [39]. Early murine mAbs posed a risk of eliciting a human anti-mouse antibody (HAMA) response, which led to the development of chimeric, humanized, and fully human antibodies to reduce immunogenicity [40] [39].
Comparative Analysis and Selection Guide
Choosing the correct cell line is a strategic decision based on the research question. The table below provides a direct comparison of the three cell lines to aid in this selection.
Table 3: Comparative Guide to HeLa, MCF-7, and Hybridoma Cell Lines
| Feature | HeLa | MCF-7 | Hybridoma |
|---|---|---|---|
| Primary Research Use | Virology, general cell biology, cancer biology, toxicology | Hormone-responsive breast cancer biology, drug resistance | Monoclonal antibody production, immunology |
| Defining Functional Output | N/A (General model system) | Hormone-induced signaling and proliferation | Secretion of a specific, homogeneous antibody |
| Key Receptors/Markers | Susceptibility to virus receptors (e.g., CD4 for HIV) | Oestrogen receptor alpha (ER-α), Progesterone receptor | Surface immunoglobulins (parental B cell) |
| Growth Considerations | Very rapid, adherent, highly robust | Slower, adherent, hormone-sensitive for proliferation | Can be adherent or suspension; requires screening |
| Major Technical Caveats | Notorious for contaminating other cell cultures | High variability between lab stocks; requires defined frozen stock | Time-consuming initial development; potential for murine immunogenicity |
Essential Reagents and Protocols
The Scientist's Toolkit: Key Research Reagent Solutions
Successful cell culture requires a suite of reliable reagents. Below is a list of essential materials for working with these cell lines.
Table 4: Essential Research Reagents for Featured Cell Lines
| Reagent / Material | Function / Application |
|---|---|
| HAT Media (Hypoxanthine-Aminopterin-Thymidine) | Selective media for killing unfused myeloma cells and allowing only hybridomas to grow after cell fusion [37] [38]. |
| Polyethylene Glycol (PEG) | A fusion-promoting agent used to fuse the plasma membranes of B lymphocytes and myeloma cells to create hybridomas [37] [38]. |
| Myeloma Fusion Partner Cell Lines | Immortal, HGPRT-negative cells (e.g., SP2/0, NS0) designed for efficient fusion and hybridoma formation [40] [39]. |
| Phenol-Red-Free Media | Essential for hormone-related studies on MCF-7 cells, as phenol red is a weak estrogen and can interfere with experimental results [35]. |
| Estradiol / Tamoxifen | Estradiol is used to stimulate proliferation of MCF-7 cells via ER-α; Tamoxifen (an anti-estrogen) is used to inhibit growth and induce apoptosis [35]. |
| Fetal Bovine Serum (FBS) | A standard supplement for cell culture media, providing growth factors, hormones, and lipids. Charcoal-stripped FBS may be used for hormone studies to remove steroids [35]. |
| Cryopreservation Media | A solution containing a cryoprotectant like DMSO, used for the long-term storage of stable cell lines and hybridomas in liquid nitrogen [37]. |
After hybridoma selection in HAT medium, screening for antigen-specific antibody production is critical. ELISA is a common primary screening method.
- Coating: A 96-well plate is coated with the target antigen diluted in a coating buffer and incubated overnight.
- Blocking: The plate is washed and then blocked with a protein solution (e.g., BSA) to prevent non-specific binding of antibodies.
- Primary Incubation: Hybridoma culture supernatant is added to the wells and incubated, allowing any specific antibodies to bind to the immobilized antigen.
- Secondary Incubation: A secondary antibody (e.g., enzyme-labeled anti-mouse immunoglobulin) is added, which binds to the primary antibody from the hybridoma.
- Detection: A chromogenic substrate for the enzyme is added. The formation of a colored product indicates the presence of an antigen-specific hybridoma in the well [38].
HeLa, MCF-7, and hybridoma cell lines represent powerful and versatile tools in the microbiologist's and biomedical researcher's arsenal. Each serves a distinct purpose: HeLa as a robust general model, MCF-7 as a specific model for hormone-responsive cancers, and hybridomas as biological factories for precise immunological reagents. A deep understanding of their origins, characteristics, and inherent limitations—such as the genetic drift in MCF-7 lines or the immunogenicity of murine antibodies—is fundamental to their effective and responsible application. By selecting the appropriate cell line and applying rigorous culture and experimental protocols, researchers can continue to leverage these invaluable resources to drive scientific discovery and therapeutic innovation forward.
Essential Methods and Industrial Applications from Lab to Production
The maintenance of healthy and proliferative cell cultures is a cornerstone of biomedical research and drug development. For adherent cell lines, regular passaging, also known as subculturing or splitting, is an indispensable technique. This process involves the detachment of cells from the culture vessel surface and the transfer of a small fraction to a new vessel containing fresh growth medium [41]. The primary purpose is to enable continued propagation by providing ample space and nutrients, thereby maintaining cells in their exponential growth phase (log phase) and preventing the stress and decline associated with over-confluency [6] [41]. Mastering this technique is essential for ensuring experimental reproducibility, maintaining genetic and phenotypic stability, and generating reliable data in cellular and molecular biology studies [42]. This guide provides a detailed, step-by-step protocol for the trypsin-based passaging of adherent cells, framed within the essential practices of animal cell culture.
Understanding Cell Growth and When to Subculture
The Growth Phases of Cultured Cells
Adherent cells in culture follow a characteristic growth pattern composed of four distinct phases, as illustrated in the growth curve below [6] [41]. To ensure viability and genetic stability, cell lines must be maintained in the exponential growth phase and subcultured before they enter the stationary phase [6].
The log phase is the optimal window for subculturing. Passaging cells before they reach 100% confluence is critical because normal cells exhibit contact inhibition, ceasing growth when the surface is covered [41]. Allowing cells to become overly confluent can lead to prolonged recovery times, reduced viability, and in some cases, irreversible senescence [43].
Key Indicators for Subculturing
Regular microscopic observation is required to determine the optimal time for passaging. Key indicators include [41] [44]:
- Confluency: Most adherent cell lines should be passaged when they reach 70-90% confluency.
- Medium Color: A rapid yellowing (acidification) of the medium, caused by increased metabolic waste (e.g., lactic acid), indicates a high cell density and the need for a medium change or subculture.
- Growth Phase: Cells should be subcultured while they are in the mid to late log phase of growth.
Materials and Reagents
The following table summarizes the essential materials and reagents required for the trypsinization and subculturing process [41] [44] [45].
Table 1: Essential Reagents and Materials for Passaging Adherent Cells
| Item | Function / Purpose |
|---|---|
| Cell Culture Vessels (e.g., T-flasks, dishes) | Surface for cell attachment and growth. |
| Complete Growth Medium | Provides nutrients, growth factors, and serum for cell proliferation. |
| Balanced Salt Solution (BSS)(e.g., PBS without Ca²⁺/Mg²⁺, HBSS) | Washes cells to remove residual serum and ions that inhibit trypsin. |
| Trypsin-EDTA Solution(e.g., 0.05%–0.25% trypsin) | Proteolytic enzyme detaches cells by digesting adhesion proteins. EDTA chelates calcium and magnesium to enhance cell detachment. |
| Trypan Blue Solution | Vital dye used to distinguish live (unstained) from dead (blue) cells during counting. |
| Hemocytometer or Automated Cell Counter | Device for determining cell concentration and viability. |
| Serum-containing Medium or Trypsin Inhibitor | Inactivates trypsin to prevent over-digestion and cell surface damage. |
| Centrifuge Tubes | For collecting and centrifuging cell suspensions. |
Step-by-Step Passaging Protocol
The following workflow outlines the complete process for passaging adherent cells, from preparation to seeding of the new culture.
Pre-Procedure Preparation
- Warm Reagents: Thaw and warm all reagents, including trypsin-EDTA, balanced salt solution (BSS), and complete growth medium, in a 37°C water bath for approximately 30 minutes. Avoid prolonged exposure of reagents to high temperatures [44].
- Label Vessels: Pre-label new culture vessels with the cell line, passage number, date, and your initials.
- Aseptic Setup: Wipe the interior of the biosafety cabinet and all reagent bottles with 70% ethanol. Ensure all necessary equipment is inside the cabinet before starting work to maintain sterility [6] [43].
Trypsinization and Detachment
- Aspirate Medium: Remove the spent culture medium from the adherent cell monolayer using a sterile vacuum aspirator or pipette [44] [45].
- Wash Monolayer: Add a sufficient volume of pre-warmed, calcium- and magnesium-free BSS (e.g., PBS) to cover the cell layer. Gently swirl the flask and then aspirate the BSS. This step is critical for removing any trace of serum, which would otherwise inhibit the activity of trypsin [44] [45].
- Add Trypsin-EDTA: Add enough pre-warmed trypsin-EDTA solution to just cover the cell monolayer. Typical volumes are 2-3 mL for a T-75 flask and 1 mL for a T-25 flask. Gently rock the vessel to ensure even coverage [45] [43].
- Incubate: Place the culture vessel in a 37°C CO₂ incubator for 1-2 minutes. The incubation time is cell line-dependent and must be determined empirically [44] [45].
- Check for Detachment: Periodically view the cells under an inverted microscope. Cells should retract, become rounded, and begin to detach. Gently tap the side of the flask to facilitate the release of remaining cells. Do not leave cells in trypsin for longer than necessary, as over-exposure can damage cell surface proteins and reduce viability [44] [45].
Trypsin Inactivation and Cell Collection
- Resuspend Cells: Once the majority of cells are detached, promptly add a volume of pre-warmed complete growth medium that is at least two times the volume of trypsin used. The serum in the medium acts as a trypsin inhibitor, halting the proteolytic activity [44] [45].
- Create Homogeneous Suspension: Gently pipette the cell suspension up and down across the growth surface and within a pipette to ensure a single-cell suspension and break up any cell clumps. Avoid creating foam, as this can damage cells [44].
Cell Counting and Seeding Density Calculation
- Count Cells: Mix a small sample of the cell suspension with an equal volume of trypan blue (e.g., 20 µL cells + 20 µL trypan blue). Load the mixture into a hemocytometer and count the cells. Live cells will exclude the dye, while dead cells will appear blue [41] [43].
- Calculate Seeding Volume: Determine the required volume of cell suspension to seed at the desired density using the formula below. Optimal seeding density is cell line-specific and can be found on the product sheet from the supplier (e.g., ATCC) [41].
Formula: Volume of Cell Suspension (mL) = (Desired Seeding Density × Culture Vessel Surface Area) / Cell Concentration (cells/mL)
Table 2: Example Seeding Densities for Common Culture Vessels
| Culture Vessel | Approximate Growth Area (cm²) | Typical Seeding Density Range (cells/cm²) | Recommended Medium Volume (mL) |
|---|---|---|---|
| 96-well plate | 0.3 | 2,000 - 10,000 | 0.1 - 0.2 |
| 24-well plate | 2 | 10,000 - 50,000 | 0.5 - 1.0 |
| T-25 flask | 25 | 25,000 - 250,000 | 5 - 7 |
| T-75 flask | 75 | 75,000 - 750,000 | 15 - 20 |
| T-175 flask | 175 | 175,000 - 1,750,000 | 35 - 50 |
Seeding the New Culture
- Transfer Cell Suspension: Pipette the calculated volume of cell suspension into a new culture vessel containing the pre-warmed complete growth medium. If preparing multiple vessels, ensure the cell suspension is mixed frequently to maintain a uniform distribution of cells [41] [45].
- Distribute Cells: Gently rock the new vessel in several directions (forward-backward, side-to-side) to evenly distribute the cells across the growth surface.
- Incubate: Place the newly seeded culture vessel into the 37°C, 5% CO₂ incubator.
- Inspect: Check the cells under a microscope after 24 hours to confirm attachment and assess morphology and confluency [6].
Troubleshooting Common Issues
Even with careful technique, challenges can arise. The following table addresses common problems and their solutions.
Table 3: Troubleshooting Guide for Cell Passaging
| Problem | Possible Cause | Suggested Solution |
|---|---|---|
| Cells detach slowly or incompletely | Insufficient trypsin activity; over-confluent culture; incorrect trypsin concentration. | Pre-warm trypsin fully; ensure BSS wash is thorough; subculture before 100% confluency; optimize trypsin concentration and incubation time. |
| Low cell viability after passaging | Over-exposure to trypsin; harsh pipetting; inadequate trypsin inactivation. | Monitor detachment closely and inactivate trypsin immediately; pipette gently; ensure sufficient serum is added for inactivation. |
| Cells clump excessively | Incomplete trypsinization; over-confluent harvest; inadequate pipetting. | Ensure a single-cell suspension is achieved during resuspension; pipette more thoroughly to dissociate clumps. |
| Cells do not re-attach after passaging | Over-trypsinization; contaminated trypsin; incorrect seeding density. | Reduce trypsin exposure time; aliquot trypsin to avoid contamination; verify and optimize the seeding density for your cell line. |
Mastering the protocol for passaging adherent cells with trypsin is a fundamental skill that ensures the health and reliability of your cell cultures. Consistent and careful technique, combined with regular monitoring and detailed record-keeping, forms the foundation of successful cell culture work. By understanding the principles behind each step—from the removal of inhibitory serum to the precise inactivation of trypsin—researchers can maintain robust, contaminant-free cultures that are essential for generating valid and reproducible scientific data in microbiology research and drug development.
Cryopreservation is a vital technique in biological research that enables the long-term storage of living cells and tissues at extremely low temperatures, effectively suspending their cellular metabolism [46] [47]. For microbiologists and cell culture researchers, mastering cryopreservation is essential for maintaining valuable cell lines, ensuring experimental reproducibility, and securing backup stocks. The process involves cooling cells to temperatures between -80°C and -196°C, which dramatically reduces kinetic and molecular activity, thereby preserving cellular structure and function indefinitely [46].
The fundamental challenge in cryopreservation lies in managing the lethal effects of ice crystal formation, which can mechanically disrupt cellular membranes and cause deadly increases in solute concentration as water freezes [48]. Dimethyl sulfoxide (DMSO) has emerged as the cryoprotectant of choice for most mammalian cell culture applications, functioning by depressing the freezing point of water, slowing the cooling rate, and facilitating vitrification—the formation of an amorphous, non-crystalline solid state that prevents ice crystal damage [46] [48]. This technical guide provides an in-depth examination of DMSO-based cryopreservation methodologies, optimized protocols, and recent advancements relevant to research scientists and drug development professionals.
Fundamental Principles of Cryoprotection
Mechanisms of Action of DMSO
DMSO (dimethyl sulfoxide) is a permeating cryoprotective agent (CPA) that protects cells through multiple mechanisms during the freeze-thaw cycle. Its relatively small molecular size (less than 100 daltons) and amphiphilic nature allow it to easily penetrate cell membranes [48]. Once intracellular, DMSO exerts its protective effects primarily through:
- Hydrogen bonding with water molecules: This interaction depresses the freezing point of water and reduces the availability of water molecules to form critical nucleation sites required for ice crystal formation [48].
- Membrane permeability modulation: At concentrations around 10%, DMSO induces transient pore formation in biological membranes, facilitating water exchange during temperature changes [48].
- Vitrification enhancement: By increasing intracellular solute concentration, DMSO promotes the vitrification of water at low temperatures, forming an amorphous glassy state rather than destructive ice crystals [48] [49].
It is crucial to recognize that DMSO concentration significantly influences its efficacy and toxicity. At low concentrations (approximately 5%), evidence suggests DMSO decreases membrane thickness and increases membrane permeability. At standard cryopreservation concentrations (10%), it induces water pore formation beneficial for cryoprotection, while at higher concentrations (40%), lipid bilayers begin to disintegrate, leading to cellular toxicity [48].
Thermal Dynamics in Cryopreservation
Understanding the thermal transitions during freezing is essential for protocol optimization. Differential scanning calorimetry studies have characterized key thermodynamic parameters for freezing medium containing DMSO, including a glass transition temperature (Tg') of approximately -120°C, crystallization temperature (Tc) around -20°C when cooling at 2.5°C/min, and melting temperature (Tm) of approximately -4°C [50]. These parameters inform the development of optimized freezing and thawing protocols that minimize cellular damage.
The cooling rate profoundly impacts cell survival. Slow cooling at approximately 1°C/minute allows for controlled dehydration of cells, preventing intracellular ice formation which is invariably lethal [46] [48] [47]. This controlled rate freezing can be achieved through specialized equipment or passive cooling devices like isopropanol chambers.
Pre-Freezing Considerations and Preparations
Cell Preparation and Assessment
Successful cryopreservation begins with proper cell preparation. Cells should be harvested during their logarithmic growth phase when they exhibit maximum growth and viability, typically at greater than 80% confluency for adherent cells [46] [47]. Prior to freezing, cells should be characterized and checked for microbial contamination, including mycoplasma testing [46] [47]. Key preparatory steps include:
- Quality assessment: Ensure cells are healthy and free from contamination, with at least 90% viability before freezing [46].
- Passage number consideration: Use cells at as low a passage number as possible to maintain genetic stability and maximize post-thaw recovery [46].
- Cell concentration optimization: Target a general range of 1×10^3 to 1×10^6 cells/mL, adjusting for specific cell type requirements [47].
Cryopreservation Media Formulations
The composition of cryopreservation media significantly impacts cell recovery. While traditional laboratory-made formulations often consist of culture medium with fetal bovine serum (FBS) and 10% DMSO, commercially available, defined formulations offer greater consistency and reduced risk of contamination [47].
Table 1: Cryopreservation Media Formulations
| Medium Type | Composition | Applications | Advantages/Limitations |
|---|---|---|---|
| Serum-containing | Complete medium with 10% DMSO or 10% glycerol; OR 50% cell-conditioned medium + 50% fresh medium with 10% DMSO/glycerol | General cell culture applications | Established protocol; contains undefined components with lot-to-lot variability [46] |
| Serum-free | 50% cell-conditioned serum-free medium + 50% fresh serum-free medium with 7.5% DMSO; OR fresh serum-free medium with 7.5% DMSO and 10% BSA | Stem cells, primary cells, clinical applications | Defined components; reduces infection risk [46] |
| Commercial defined formulations (e.g., CryoStor, Synth-a-Freeze) | Optimized ratios of cryoprotectants, proteins, and supplements | Stem cells, sensitive primary cells, regulated applications | Consistent performance, cGMP options available [46] [47] |
Freezing Protocols: Methodologies and Optimization
Standard Freezing Protocol for Adherent and Suspension Cells
The following generalized protocol for cryopreserving cultured cells can be adapted for specific cell types based on manufacturer recommendations [46]:
- Preparation: Prepare freezing medium and store at 2° to 8°C until use. For adherent cells, gently detach cells from the tissue culture vessel using appropriate dissociation reagents [46].
- Harvesting: Resuspend detached cells in complete growth medium. Determine total cell number and percent viability using a hemocytometer or automated cell counter with Trypan Blue exclusion [46].
- Centrifugation: Centrifuge the cell suspension at approximately 100-400 × g for 5 to 10 minutes (speed varies by cell type). Aseptically remove the supernatant without disturbing the cell pellet [46].
- Resuspension: Resuspend the cell pellet in cold freezing medium at the recommended viable cell density for the specific cell type [46].
- Aliquoting: Dispense aliquots of the cell suspension into sterile cryogenic vials, mixing gently but frequently to maintain a homogeneous cell suspension [46].
- Controlled-rate freezing: Freeze cells slowly at approximately 1°C per minute using a controlled-rate cryo-freezer or isopropanol freezing container placed at -80°C overnight [46] [47].
- Long-term storage: Transfer frozen cells to liquid nitrogen storage in the gas phase below -135°C [46].
Diagram 1: Cell Freezing Workflow (46 characters)
Optimized Freezing Parameters from Recent Research
Recent research has refined freezing protocols based on thermophysical characterization. For ovarian tissue cryopreservation, an optimized freezing curve established through differential scanning calorimetry includes [50]:
- 5 minutes at 4°C
- 1°C/min to -7°C
- Seeding at 60°C/min to -32°C
- 10°C/min to -15°C
- 0.3°C/min to -40°C
- 10°C/min to -140°C
While this specific protocol was developed for ovarian tissue, it demonstrates the precision possible in optimizing thermal profiles for different cell types.
Thawing Protocols and Post-Thaw Processing
Standard Thawing Procedure
The thawing process is particularly stressful to frozen cells, and proper technique is critical for maximizing cell recovery. The general principle of "slow freeze, fast thaw" should be followed [51] [47]:
- Preparation: Pre-warm complete growth medium to 37°C and prepare appropriate culture vessels [51].
- Rapid thawing: Remove the cryovial from liquid nitrogen storage and immediately place it in a 37°C water bath with gentle swirling until only a small ice crystal remains (approximately 1 minute) [51].
- Decontamination: Transfer the vial to a laminar flow hood and wipe the outside with 70% ethanol before opening [51].
- Dilution: Transfer the thawed cells dropwise into a centrifuge tube containing pre-warmed complete growth medium [51].
- Centrifugation: Centrifuge the cell suspension at approximately 200 × g for 5-10 minutes to remove DMSO [51].
- Reseeding: Resuspend the cell pellet in fresh complete growth medium and transfer to an appropriate culture vessel, plating at high density to optimize recovery [51].
DMSO Reduction Strategies Post-Thaw
For clinical applications or DMSO-sensitive cells, post-thaw processing to reduce DMSO concentration may be necessary. Recent comparative studies have evaluated two main approaches [52]:
- Washing method: Centrifugation and resuspension in DMSO-free medium
- Dilution method: Direct dilution to reduce DMSO concentration to 5% or lower
Notably, a 2025 study on mesenchymal stromal cells (MSCs) found that the dilution method resulted in significantly higher cell recovery with similar viability compared to washed cells, with fewer early apoptotic cells observed after 24 hours [52]. This suggests that for some applications, complete DMSO removal may be more detrimental than maintaining reduced concentrations.
Quantitative Analysis of DMSO Concentration Effects
Impact on Cell Viability and Recovery
Recent meta-analyses and comparative studies have provided quantitative evidence for optimizing DMSO concentrations in cryopreservation protocols. A systematic review of autologous hematopoietic stem cell transplantation studies found that reducing DMSO concentration from 10% to 5% improved post-thaw CD34+ cell viability [49]. Similarly, a 2025 toxicology study on MSCs demonstrated that cryopreserved cells with 5% DMSO showed no impairment in animal models and were well-tolerated [52].
Table 2: Comparative Analysis of DMSO Concentration Effects
| Parameter | 5% DMSO | 10% DMSO | Research Context |
|---|---|---|---|
| CD34+ cell viability | Improved | Standard | Autologous hematopoietic stem cell transplantation [49] |
| Cell recovery post-thaw | 95% of pre-freeze count | 55% of pre-freeze count | MSC cryopreservation with washing vs. dilution [52] |
| Early apoptotic cells (24h post-thaw) | Significantly lower | Significantly higher | MSC flow cytometry analysis [52] |
| Adverse effects in patients | Reduced frequency | More frequent | Clinical transplantation studies [49] |
| Engraftment rate | Minimal impact | Minimal impact | Hematopoietic stem cell transplantation [49] |
Functional Outcomes Across Cell Types
Different cell types exhibit varying sensitivities to DMSO and cryopreservation conditions. While standard protocols often utilize 10% DMSO, evidence suggests that many primary cells and stem cells may benefit from modified approaches:
- Hematopoietic stem cells: 5% DMSO shows improved viability with equivalent engraftment potential [49]
- Mesenchymal stromal cells: Maintain functionality and potency with 5% DMSO when using dilution method [52]
- Ovarian tissue: Optimized protocols use Leibovitz L-15 medium with 1.5M DMSO and 0.1M sucrose [50]
The Scientist's Toolkit: Essential Materials and Reagents
Table 3: Research Reagent Solutions for DMSO Cryopreservation
| Item | Function | Examples/Specifications |
|---|---|---|
| Cryoprotective agent | Prevents ice crystal formation, enables vitrification | DMSO (cell culture grade), glycerol, commercial cryopreservation media [46] |
| Base medium | Provides nutritional support during freeze-thaw transition | Leibovitz L-15, complete growth medium appropriate for cell type [46] [50] |
| Protein source | Protects against membrane damage during freezing | Fetal bovine serum (FBS), human serum albumin (HSA), bovine serum albumin (BSA) [46] [50] |
| Non-permeating agents | Provide extracellular protection, osmotic stabilization | Sucrose, trehalose, raffinose (typically 0.1-0.2M) [50] [48] |
| Controlled-rate freezing device | Ensures optimal cooling rate (~1°C/min) | Isopropanol chambers (e.g., "Mr. Frosty"), programmable freezers [46] [47] |
| Cryogenic storage vials | Secure containment for low-temperature storage | Sterile, internal-threaded vials resistant to liquid nitrogen [46] [47] |
| Viability assessment tools | Quantifies pre-freeze and post-thaw cell quality | Automated cell counters, hemocytometers, Trypan Blue [46] |
Troubleshooting and Quality Control
Common Issues and Solutions
Even with optimized protocols, researchers may encounter challenges with cryopreservation. Key troubleshooting strategies include:
- Poor post-thaw viability: Ensure cells are in log phase before freezing, use proper freezing rate (~1°C/min), and verify DMSO concentration [51] [47]
- Contamination: Implement strict aseptic technique, use antibiotics in freezing media when appropriate, and regularly test for mycoplasma [47] [6]
- Low cell recovery: Freeze at appropriate cell density, avoid excessive centrifugation forces, and plate thawed cells at high density [51]
- DMSO toxicity: Consider reducing DMSO concentration to 5% for sensitive cells, use step-wise addition, or explore less toxic cryoprotectants [52] [49]
Safety Considerations
DMSO presents specific safety considerations that researchers must address:
- Enhanced chemical permeability: DMSO facilitates transdermal absorption of organic molecules, requiring appropriate personal protective equipment and careful handling [46]
- Storage conditions: Cryovials stored in liquid phase present an explosion risk; storage in vapor phase nitrogen is recommended [46] [51]
- Clinical applications: For cell-based therapies, DMSO dosage should be minimized, with recent evidence supporting the safety of products containing 5% DMSO in critically ill patients [52] [53]
Diagram 2: Cryopreservation Troubleshooting (34 characters)
Mastering DMSO-based cryopreservation requires meticulous attention to protocol details, from cell preparation through to long-term storage and thawing. The established standard of 10% DMSO with controlled-rate freezing at approximately 1°C/minute remains effective for many applications, but emerging evidence supports considering lower DMSO concentrations (5%) for improved viability and reduced toxicity in sensitive cell types and clinical applications [52] [49].
Future directions in cryopreservation research include the development of defined, serum-free formulations for regulatory compliance, optimization of cell-type specific protocols through thermophysical characterization [50], and exploration of DMSO-free alternatives for clinical therapies [53]. As cryopreservation methodologies continue to evolve, researchers should maintain awareness of both fundamental principles and emerging evidence to ensure the highest quality cell banking for their specific applications.
For microbiologists and cell culture specialists, proficiency in these techniques is not merely a technical skill but a fundamental competency that ensures the integrity, reproducibility, and long-term success of research programs dependent on stable cellular models.
For microbiologists venturing into animal cell culture, establishing a laboratory that is both functionally effective and compliant with Biosafety Level 2 (BSL-2) standards is a critical first step. BSL-2 containment is required for work involving agents that pose a moderate hazard to personnel and the environment, such as indigenous human pathogens that can cause disease through accidental ingestion, mucous membrane exposure, or skin punctures [54] [55] [56]. This guide provides an in-depth technical overview of the essential equipment and aseptic techniques necessary to set up a BSL-2 compliant cell culture laboratory, ensuring both the integrity of your research and the safety of laboratory personnel.
Understanding Biosafety Level 2 (BSL-2) Fundamentals
BSL-2 builds upon the foundation of BSL-1 by introducing enhanced controls for handling moderate-risk biological agents. The core differentiators of a BSL-2 lab include:
- Restricted Access: Laboratory access is limited and controlled, especially when work is being conducted [54] [56].
- Enhanced Personnel Training: Laboratory personnel must have specific training in handling pathogenic agents and are supervised by scientists competent in handling infectious agents [54].
- Primary Barriers: All procedures that can create infectious aerosols or splashes must be conducted within a Biological Safety Cabinet (BSC) or other physical containment equipment [54] [55] [56].
- Safety Equipment and Facility Design: Labs must be equipped with eye washing stations, self-closing doors, and have an autoclave or other decontamination method available for waste processing [55] [56].
- Personal Protective Equipment (PPE): Appropriate PPE, including laboratory coats, gloves, and eye protection, must be worn at all times [54] [56].
A proper risk assessment, considering the infectious agent, procedures performed, and available countermeasures, is mandatory before project initiation [54] [56].
Essential Equipment for a BSL-2 Cell Culture Lab
The equipment in a BSL-2 lab must facilitate aseptic work while protecting the researcher and the environment. The following table summarizes the core equipment and its specific role in ensuring BSL-2 compliance and culture success.
Table 1: Essential Equipment for a BSL-2 Cell Culture Laboratory
| Equipment Category | Specific Examples | Function in Cell Culture | BSL-2 Compliance & Safety Consideration |
|---|---|---|---|
| Primary Containment | Class II Biological Safety Cabinet (BSC) | Provides an aseptic work area for cell culture procedures; protects the user and environment from aerosols [57] [29]. | Absolute requirement for all procedures that may create aerosols or splashes (e.g., pipetting, sonication) [55] [56]. |
| Incubation | Humid CO₂ Incubator | Maintains optimal temperature (37°C), high humidity, and controlled CO₂ (e.g., 5%) to support cell growth and medium pH [58] [29]. | Frequent cleaning and decontamination are essential to prevent microbial contamination and biofilm formation, which are safety risks [57] [29]. |
| Storage & Preservation | Laboratory Refrigerator & Freezer (-20°C); Ultra-low Temperature Freezer (-80°C); Liquid Nitrogen Cryostorage Container | Stores media, reagents, and cells at specified temperatures [58] [29]. Cryopreservation in vapor-phase liquid nitrogen is used for long-term storage of valuable cell stocks [29]. | Prevents genetic drift and cross-contamination. Vapor-phase systems are required for biohazardous materials to minimize explosion risks [29]. |
| Sample Preparation | Cooling Centrifuge; Water Bath | Separates cells from media; gently thaws frozen cells and warms media [58] [29]. | Sealed rotors or safety cups contain aerosols during centrifugation. "Dry bath" alternatives (e.g., metal beads) reduce contamination risk from standing water [29]. |
| Analysis & Quality Control | Inverted Microscope; Automated Cell Counter / Hemacytometer | Allows daily observation of cell morphology, confluency, and detection of contamination [58] [29]. Enumerates cell concentration and viability [29]. | Critical for monitoring culture health and identifying potential biological hazards early. |
| Decontamination | Autoclave | Sterilizes media, reagents, and decontaminates biohazardous waste before disposal [55] [56]. | Absolute requirement for proper disposal of all BSL-2 biological waste [55] [56]. |
Workflow for Aseptic Start-Up and Equipment Placement
The physical setup of your equipment directly impacts the effectiveness of your aseptic technique and containment. The following diagram illustrates the logical workflow and spatial considerations for establishing a sterile work area.
Mastering Aseptic Technique in a BSL-2 Setting
Aseptic technique is a set of procedures designed to create a barrier between microorganisms in the environment and the sterile cell culture [57]. In a BSL-2 context, these techniques are not only for protecting your culture from contamination but are also fundamental for containing your potentially hazardous biological agents.
Core Aseptic Practices and BSL-2 Enhancements
- Sterile Work Area: The BSC is the cornerstone of your sterile work area. It must be in a low-traffic area, free from drafts, and its surface must be decontaminated with 70% ethanol before and after work, and after any spill [57]. Ultraviolet (UV) light can be used to sterilize the interior between uses, but it is not a substitute for chemical decontamination and should not be used when the cabinet is occupied [57].
- Personal Hygiene and PPE: Hand washing before and after work, and after any potential contamination is mandatory [54] [57]. In a BSL-2 lab, PPE is non-negotiable. This includes a lab coat or gown, gloves, and safety goggles or a face shield, especially for procedures with splash risk [54] [57] [56]. Gloves should be changed frequently and never worn outside the laboratory [54].
- Sterile Reagents and Media: All media, reagents, and solutions must be sterilized, typically by filtration through a 0.2 µm membrane, before use [57]. The outside of all bottles, flasks, and plates should be wiped with 70% ethanol before being introduced into the BSC [57].
- Sterile Handling: Work should be performed slowly and deliberately to minimize the creation of aerosols and turbulence within the BSC [57]. Key practices include:
- Using sterile plastic or glass pipettes only once to avoid cross-contamination [57] [59].
- Never placing caps or pipettes directly on the non-sterile surface; instead, hold them in your hand or place them on a sterile surface with the opening facing down [57].
- Avoiding talking or singing while performing sterile procedures [57].
- Not pouring from bottles or flasks; instead, use pipettes to transfer liquids [57].
Aseptic Technique Workflow Checklist
The following checklist provides a step-by-step guide for maintaining asepsis during cell culture procedures. Adhering to this checklist is critical for both experimental success and BSL-2 safety.
BSL-2 Specific Safety Protocols and Waste Management
Beyond aseptic technique, specific safety practices are mandated for BSL-2 compliance.
- Sharps Management: Policies for the safe handling of sharps must be strictly implemented. This includes limiting the use of needles and syringes to situations where there is no alternative, using safety-engineered devices, and never recapping, bending, or breaking needles by hand [54]. Used disposable sharps must be placed in puncture-resistant containers immediately after use [54] [57].
- Waste Decontamination: All cultures, stocks, and other potentially infectious materials must be decontaminated before disposal, most commonly by autoclaving [54] [56]. Liquid biological waste can be treated with bleach or other validated disinfectants before disposal, following institutional and environmental regulations [60].
- Signage and Access Control: A sign must be posted at the laboratory entrance indicating the Biosafety Level, the infectious agents in use, the supervisor's contact information, and any specific entry requirements (e.g., PPE) [54].
- Emergency Procedures: Laboratories must have posted protocols for handling spills, exposures, and other emergencies. Staff must be properly trained and equipped to decontaminate spills involving infectious materials [54] [57].
Essential Research Reagent Solutions
Table 2: Key Reagents and Materials for Animal Cell Culture
| Reagent/Material | Function | BSL-2 Consideration |
|---|---|---|
| Cell Culture Media (e.g., DMEM, RPMI-1640) | Provides essential nutrients (carbohydrates, amino acids, vitamins, inorganic salts) to support cell growth and proliferation [42]. | All media waste must be decontaminated. Serum-supplemented media can support microbial growth, increasing potential biohazard. |
| Serum (e.g., Fetal Bovine Serum - FBS) | A complex mix of proteins, growth factors, and other components that provides essential factors for the growth of many cell types. | Sourced from animals, posing a potential risk of viral or mycoplasma contamination; requires careful sourcing and testing. |
| Antibiotics & Antimycotics (e.g., Penicillin-Streptomycin) | Added to culture media to prevent bacterial and fungal contamination. | Not a substitute for aseptic technique. Overuse can mask low-level contamination and lead to antibiotic-resistant organisms. |
| Trypsin/EDTA | A proteolytic enzyme solution used to dissociate adherent cells from their substrate for subculturing (passaging) [42]. | Neutralized with complete media after dissociation. All waste containing trypsin must be decontaminated. |
| Cryoprotectant (e.g., DMSO) | Added to cells before freezing to reduce ice crystal formation and protect cell viability during cryopreservation [29]. | Handle with appropriate PPE as DMSO can rapidly penetrate skin and carry other chemicals with it. |
| Phosphate Buffered Saline (PBS) | A balanced salt solution used for washing cells and diluting reagents. | All waste PBS must be treated as potential biological waste and decontaminated. |
Establishing a BSL-2 compliant cell culture laboratory is a deliberate process that integrates specific engineering controls, safety equipment, and rigorously adhered-to practices. The essential equipment, centered around the biological safety cabinet, creates the physical containment necessary for moderate-risk work. However, the true backbone of safety and experimental success is the researcher's unwavering commitment to aseptic technique. By understanding the principles outlined in this guide—from equipment selection and setup to the meticulous execution of sterile procedures and waste management—microbiologists can build a foundation for robust, reproducible, and safe animal cell culture research.
Animal cell culture has evolved from a basic research tool into a cornerstone of modern biotechnology, enabling the production of complex biologics that are impossible to synthesize by conventional chemical means. For microbiologists transitioning into biopharmaceutical development, understanding these advanced applications is crucial for innovating in vaccine development, therapeutic protein production, and gene-based therapies. This whitepaper provides a comprehensive technical guide to these applications, emphasizing the critical role of optimized cell culture systems in achieving high-yield, consistent, and safe biological products. The convergence of novel vector systems, advanced media optimization strategies, and quality-by-design principles has transformed biomanufacturing, allowing researchers to address previously untreatable diseases through sophisticated cell culture platforms.
Core Applications in Biomanufacturing
Vaccine Production Technologies
The COVID-19 pandemic catalyzed unprecedented innovation in vaccine technology, particularly in gene-based vaccination platforms that leverage viral vectors and lipid nanoparticles (LNPs) to deliver genetic material encoding pathogen-derived immunogens.
Table 1: Advanced Vaccine Production Platforms
| Platform Type | Key Components | Production System | Advantages | Examples |
|---|---|---|---|---|
| mRNA Vaccines | Lipid nanoparticles (LNPs), modified nucleotides, 5' cap, UTRs | In vitro transcription, HEK293 cells for validation | Rapid development, scalable production, non-integrating | Pfizer/BioNTech (BNT162b2), Moderna (mRNA-1273) [61] |
| Viral Vectors | Recombinant adenovirus (rAd), deleted E1/E3 regions, transgene | HEK293 cell line (complements E1 deletion), bioreactor cultivation | Built-in adjuvant properties, efficient cell targeting, proven history | Johnson & Johnson (Ad26.COV2.S), AstraZeneca (ChAdOx1 nCoV-19) [61] |
| Virus-Like Particles (VLPs) | Structural viral proteins, self-assembling particles | Nicotiana benthamiana (plant-based), mammalian cells | Non-infectious, highly immunogenic, native conformation | Medicago Covifenz (SARS-CoV-2 VLP) [62] |
| Self-amplifying RNA (saRNA) | Alphavirus replicase, subgenomic promoter, LNP delivery | In vitro transcription, purification | Lower dose requirements, prolonged antigen expression | ARCT-154 (approved in Japan for COVID-19) [61] |
These platforms represent a shift from traditional attenuated or inactivated whole-pathogen vaccines toward precisely engineered modalities that stimulate robust immune responses while maintaining favorable safety profiles. Gene-based vaccines specifically are designed to encode immunogens without mutating host DNA, balancing effective antigen presentation with controlled activation of innate immune responses through pattern recognition receptors like TLR3, TLR7, and TLR9 [61].
Recombinant Protein Synthesis
Recombinant proteins constitute the largest segment of biopharmaceuticals, with monoclonal antibodies (mAbs) dominating the therapeutic landscape. These complex molecules require sophisticated cell culture systems to ensure proper folding, post-translational modifications, and functional activity.
Chinese hamster ovary (CHO) cells remain the predominant production host due to their robustness in suspension culture, high volumetric productivity (>5 g/L for mAbs), and human-like glycosylation patterns. However, controlling critical quality attributes (CQAs) such as charge heterogeneity presents substantial challenges. Charge variants arise from post-translational modifications including deamidation, sialylation, and oxidation, which can impact stability, bioactivity, and pharmacokinetics [63].
Table 2: Recombinant Protein Production Systems
| Production Host | Typical Applications | Key Advantages | Productivity Range | Notable Challenges |
|---|---|---|---|---|
| CHO Cells | Monoclonal antibodies, Fc-fusion proteins, recombinant hormones | Human-like glycosylation, scalability, regulatory familiarity | 3-10 g/L for mAbs | Charge heterogeneity, host cell protein contamination, apoptosis control |
| HEK293 Cells | Viral vectors, complex proteins requiring specific processing | High transfection efficiency, suspension adaptation | 0.5-3 g/L for proteins | Lower volumetric yield compared to CHO, scalability limitations |
| Komagataella phaffii (Yeast) | Enzymes, albumin, some vaccine antigens | Defined media requirements, secretory production, no endotoxins | 1-15 g/L depending on protein | Hyperglycosylation, intracellular retention for some proteins [64] |
| Plant-Based Systems | VLPs, therapeutic enzymes, antibodies | Scalable agriculture, low human pathogen risk, cost-effective | Varies by protein and expression strategy | Different glycosylation patterns, extraction requirements [62] |
Process intensification strategies including perfusion culture and concentrated fed-batch have pushed product titers to unprecedented levels, subsequently creating downstream processing challenges, particularly for harvest clarification where traditional depth filtration faces limitations with high cell density cultures [65].
Gene Therapy Manufacturing
Gene therapies represent the frontier of biopharmaceutical innovation, offering potential cures for genetic disorders through direct genetic modification. Both viral and non-viral delivery systems are employed, each with distinct manufacturing considerations.
Adenoviral (Ad) vectors, first isolated in 1953, are non-enveloped viruses with icosahedral capsids containing double-stranded DNA genomes. Recombinant Ads used for therapy and vaccination are typically rendered replication-defective by removing essential replication genes (e.g., E1) and replacing them with therapeutic transgenes. Their inherent ability to target antigen-presenting cells and engage TLR9 to activate type I interferon responses contributes to efficient T cell priming [61].
Emerging non-viral approaches utilize CRISPR-based therapies delivered via lipid nanoparticles formulated with sgRNA and mRNA, enabling in vivo gene editing for conditions like transthyretin amyloidosis (NCT06539208) and hereditary angioedema (NCT05120830) [61]. The manufacturing workflow for gene therapies requires rigorous monitoring of product-related impurities and thorough viral clearance validation to ensure patient safety.
Advanced Methodologies and Protocols
Media Optimization Using Machine Learning
Optimizing cell culture media remains a significant challenge due to the complex interactions between numerous components and their effects on cellular metabolism and product quality. Traditional approaches like one-factor-at-a-time (OFAT) and Design of Experiments (DoE) are inefficient for capturing nonlinear relationships in high-dimensional spaces [64] [63].
Bayesian Optimization (BO) has emerged as a powerful machine learning framework for media development, combining probabilistic modeling with an exploration-exploitation trade-off to identify optimal conditions with minimal experimentation. The BO-based iterative experimental design has demonstrated 3-30 times greater efficiency than standard DoE approaches [64].
Experimental Protocol: Bayesian Optimization for Media Development
Define Design Space: Identify continuous variables (e.g., component concentrations), categorical variables (e.g., carbon source type), and constraints (e.g., total concentration limits).
Initialize with Diverse Experiments: Select an initial set of 8-12 media formulations spanning the design space using Latin Hypercube Sampling to ensure broad coverage.
Establish Assessment Metrics: Define quantitative objectives such as cell viability, titer, product quality attributes (e.g., charge variant distribution), or specific productivity.
Implement Iterative Cycle:
- Train Gaussian Process (GP) surrogate model on all accumulated data
- Use acquisition function (e.g., Expected Improvement) to identify the most promising conditions for subsequent experimentation
- Execute new experiments predicted to balance exploration of uncertain regions and exploitation of promising areas
- Incorporate results into dataset and update GP model
Validate Optimal Formulation: Confirm performance of identified optimum in triplicate bioreactor runs to ensure robustness [64].
This approach successfully identified media compositions that maintained peripheral blood mononuclear cell (PBMC) viability above 70% for 72 hours using only 24 total experiments, and optimized recombinant protein production in Komagataella phaffii with significantly reduced experimental burden [64].
Charge Variant Control in mAb Production
Controlling charge heterogeneity is critical for monoclonal antibody therapeutics, as variants can impact stability, bioactivity, and immunogenicity. Machine learning approaches enable prediction and control of charge variants by modeling complex relationships between process parameters and product quality attributes.
Experimental Protocol: ML-Driven Charge Variant Control
Dataset Generation:
- Cultivate CHO cells producing mAbs under varied process conditions (pH, temperature, dissolved oxygen, feed strategy)
- Analyze charge variants using cation exchange chromatography (CEX) or capillary isoelectric focusing (cIEF)
- Measure critical process parameters and medium components
Feature Engineering:
- Normalize all process variables and quality attributes
- Calculate derived features (e.g., metabolic rates, cumulative nutrient consumption)
- Handle categorical variables (e.g., basal medium type) through one-hot encoding
Model Training:
- Employ ensemble methods (Random Forest, Gradient Boosting) or neural networks for nonlinear regression
- Train separate models for acidic and basic variant prediction
- Use cross-validation to prevent overfitting and assess generalizability
Process Optimization:
- Identify optimal process parameter combinations that minimize undesirable charge variants while maintaining high titer
- Validate model predictions through controlled bioreactor runs
- Implement control strategies for critical parameters (e.g., tight pH control at 6.9-7.1, lower temperature shift timing) [63]
This data-driven approach has successfully reduced problematic charge variants by 15-40% in industrial mAb production processes while maintaining product titers [63].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Advanced Cell Culture Applications
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Basal Media | DMEM, RPMI-1640, IMDM, Ham's F12 | Nutrient foundation | Historically designed for non-human cells; increasing shift to human plasma-like media (HPLM, Plasmax) for physiological relevance [66] |
| Growth Factors | FGF-2, TGF-β, EGF, VEGF, PDGF | Stimulate proliferation and maintain phenotype | Recombinant human forms preferred for clinical applications; concentrations typically 1-100 ng/mL depending on cell type [67] |
| Serum Alternatives | Human Platelet Lysate (hPL), Serum-Free Media (SFM) | Provide growth factors and attachment factors | hPL shows superior cost-performance balance for MSC expansion; SFM essential for regulatory compliance but higher cost [68] |
| Lipid Nanoparticles | Ionizable lipids, PEG-lipids, phospholipids, cholesterol | Nucleic acid delivery and protection | Critical for mRNA vaccine and gene editing therapeutic efficacy; composition affects tropism and endosomal escape [61] |
| Cell-Specific Supplements | IL-2, IL-7, IL-15 (T cells), BMP-4, Wnt3a (stem cells) | Direct differentiation and functional maintenance | CAR-T cell expansion and persistence enhanced with cytokine optimization; concentration timing critical for fate determination [64] [66] |
| Chemically Defined Supplements | Insulin, transferrin, selenium, ethanolamine | Replace serum components | Essential for regulatory compliance; reduce batch-to-batch variability in biomanufacturing [66] |
Future Perspectives and Emerging Trends
The field of animal cell culture continues to evolve rapidly, driven by several transformative trends. Personalized medicine approaches are creating demand for patient-specific media formulations optimized for autologous cell therapies [66]. Artificial intelligence and machine learning are becoming indispensable tools for media optimization and process control, moving beyond traditional statistical approaches to capture complex nonlinear relationships in biological systems [64] [63]. Sustainable biomanufacturing initiatives are promoting the development of serum-free and animal component-free media that reduce ethical concerns and improve lot-to-lot consistency [68] [66].
Advanced production technologies like molecular farming in plants offer promising alternatives for scalable production of recombinant proteins and virus-like particles, as demonstrated by Medicago's plant-derived COVID-19 vaccine [62]. Continuous bioprocessing and process intensification strategies are gaining traction to improve manufacturing efficiency and reduce facility footprints. As these innovations mature, they will further expand the applications of animal cell culture in addressing unmet medical needs through advanced biologics.
For microbiologists entering this field, understanding these advanced applications provides a foundation for contributing to the next generation of biopharmaceutical innovations, where interdisciplinary approaches combining microbiology, cell biology, data science, and engineering will drive future breakthroughs.
The transition to animal-free cell culture systems represents a paradigm shift in biomedical research and biopharmaceutical manufacturing. These systems, which include chemically defined media (CDM) and recombinant reagents, eliminate components derived directly from animal tissues or body fluids. This shift is driven by the critical need for greater process consistency, reduced contamination risk, and improved regulatory compliance in both research and therapeutic applications [69] [70]. For microbiologists venturing into mammalian cell culture, understanding these systems is essential, as they offer control and reproducibility analogous to defined bacterial culture media, but with additional complexity required to support mammalian cell metabolism and signaling pathways.
Traditional cell culture methodologies relying on fetal bovine serum (FBS) present significant challenges, including undefined composition, substantial batch-to-batch variability, and potential contamination with animal viruses or prions [70]. Serum-free media (SFM) marked an initial improvement but may still contain animal-derived components such as hormones, attachment factors, or proteins isolated from blood. True animal-free systems advance this further by utilizing exclusively recombinant proteins and synthetic components manufactured without animal-derived materials at any production stage [71] [72]. The implementation of these systems requires careful consideration of definitions, component selection, and adaptation protocols to maintain cell health, productivity, and experimental reproducibility.
Definitions and Key Concepts
Navigating the terminology of animal-free cell culture is essential for proper implementation. Various suppliers may use similar terms with nuanced differences in meaning, making careful examination of product specifications crucial.
Chemically Defined Media (CDM) consist exclusively of ingredients with known chemical structures and concentrations, including salts, amino acids, vitamins, and other small molecules. These media contain no proteins, hydrolysates, or other complex raw materials with undefined composition [71]. The definition extends to the manufacturing process, where no animal-derived materials are used in any synthetic steps or as process raw materials [69]. This complete definition ensures full traceability and eliminates lot-to-lot variability associated with biological components.
Animal Component-Free (ACF) products contain no primary raw materials derived directly from animal tissue or body fluid. However, they may contain recombinant proteins produced in animal cell lines or through fermentation processes, and secondary/tertiary raw materials may be of animal origin [71]. This classification is distinct from Animal Origin-Free (AOF), where neither primary nor secondary raw materials are derived from animals, though tertiary materials from animal sources may be used [71]. Xeno-Free (XF) formulations exclude materials from non-human animals but may incorporate components of human origin, such as human serum or recombinant proteins produced in human cell lines [71].
Table 1: Classification of Animal-Free Culture Media
| Classification | Key Characteristics | Typical Applications |
|---|---|---|
| Chemically Defined | All components known chemical structures; no proteins or complex biologics; no animal-derived materials in manufacturing | Biopharmaceutical production; clinical/therapeutic applications; fundamental research requiring high reproducibility |
| Animal Component-Free (ACF) | No direct animal tissue/fluid components; may contain recombinant animal proteins or use animal-derived secondary materials | Research applications transitioning from serum-containing systems; industrial bioprocessing |
| Animal Origin-Free (AOF) | No animal-derived primary or secondary raw materials; tertiary materials may have animal origin | Preclinical therapeutic development; applications requiring reduced animal component risk |
| Xeno-Free (XF) | No non-human animal materials; may contain human-derived components (serum, recombinant proteins) | Cell therapy manufacturing; clinical applications with human implantation |
The terminology extends to specific reagent categories. Recombinant reagents are produced through genetic engineering in microbial, insect, or mammalian expression systems, ensuring consistency and eliminating animal sourcing [69] [70]. These include growth factors, cytokines, hormones, and attachment factors essential for cell proliferation and function. Understanding these distinctions enables researchers to select appropriate systems based on their specific application requirements, particularly considering regulatory needs for therapeutic development [71].
Market Context and Growth Drivers
The global cell culture media market is experiencing significant transformation, with animal-free and chemically defined systems representing a rapidly expanding segment. Market analyses project the overall cell culture media market to reach USD 12.80 billion by 2033, registering a compound annual growth rate (CAGR) of 13.20% from 2025 to 2033 [73]. This robust growth is partly driven by the accelerating adoption of defined media systems across research and industrial applications.
Several key factors are propelling the shift toward animal-free systems. The biopharmaceutical production segment led the market in 2024 with a 47.79% revenue share, creating substantial demand for reproducible, defined media to support expanding production and minimize contamination risks in downstream processes [73]. Similarly, the bacterial cell culture market (encompassing microbiology applications) is projected to grow from USD 3.66 billion in 2025 to USD 6.56 billion by 2034 at a 6.7% CAGR [74], with increasing demand for standardized microbial detection and diagnostic tools.
Table 2: Market Outlook for Cell Culture Media Segments
| Market Segment | 2024-2025 Market Size | Projected 2034 Market Size | CAGR | Key Drivers |
|---|---|---|---|---|
| Overall Cell Culture Media | USD 3.66B (2025) [74] | USD 12.80B by 2033 [73] | 13.20% [73] | Biopharmaceutical production, cell-based vaccines, therapeutic development |
| Bacterial Culture Media | USD 3.66B (2025) [74] | USD 6.56B by 2034 [74] | 6.7% [74] | Infectious disease diagnostics, food safety testing, antibiotic development |
| Microbiology & Bacterial Culture Media | USD 6.03B (2025) [75] | USD 13.22B by 2034 [75] | 9.11% [75] | Clinical diagnostics, pharmaceutical safety testing, regulatory requirements |
Regulatory considerations significantly influence this market transition. Cell-based vaccines have become critical components of global immunization strategies, with regulatory approvals for cell-based candidate vaccine viruses streamlining development of more consistent and potentially effective vaccines [73]. The 2024 FDA approval of Ryoncil (remestemcel-L), the first mesenchymal stromal cell therapy approved in the U.S., further demonstrates the regulatory acceptance of cell therapies manufactured under defined conditions [73]. These developments create a favorable environment for implementing animal-free systems in therapeutic applications.
Implementation Strategies and Methodologies
System Design and Component Selection
Successful implementation of animal-free systems requires systematic approach to media formulation and component selection. A complete chemically defined medium typically contains several essential component categories: inorganic salts and buffers (e.g., CaCl₂, KCl, MgSO₄, NaHCO₃, NaCl, NaH₂PO₄) to maintain osmotic balance and pH; amino acids (both essential and non-essential) as protein building blocks; vitamins as enzyme cofactors; energy sources such as glucose; nucleosides or nucleotide precursors; lipids and lipid precursors including fatty acids and cholesterol; and recombinant proteins replacing traditional serum components [42].
Key recombinant reagents include insulin or insulin-like growth factors for metabolic regulation; transferrin for iron transport; albumin as a carrier protein and antioxidant; selenium as an antioxidant cofactor; and specific growth factors and cytokines tailored to the cell type being cultured [69] [72]. Formulations such as ITSE Animal-Free (containing recombinant insulin, transferrin, selenium, and ethanolamine) provide essential components typically required for optimal cell growth in serum-free or reduced serum media [72].
Cell Adaptation Protocols
Transitioning cells from serum-containing to animal-free systems requires careful adaptation to prevent culture shock and maintain cell viability. The following stepwise protocol provides a generalized approach that can be customized for specific cell types:
Pre-adaptation Assessment: Begin with healthy, exponentially growing cells in serum-containing media. Confirm absence of microbial contamination (bacteria, fungi, mycoplasma) and determine baseline growth characteristics including population doubling time, maximum cell density, and morphology [6].
Gradual Serum Reduction:
- Stage 1 (Days 1-3): Prepare a mixture containing 75% original serum-containing media and 25% target animal-free media. Monitor cell morphology, viability, and growth rate daily.
- Stage 2 (Days 4-7): Transition to 50:50 mixture of original and target media if cells appear healthy and maintain >85% viability.
- Stage 3 (Days 8-14): Transition to 25% original media and 75% target animal-free media.
- Stage 4 (Days 15+): Transition to 100% target animal-free media [6].
Culture Optimization: During adaptation, cells may require adjustments to seeding density, typically 25-50% higher than in serum-containing conditions. Supplementation with additional recombinant growth factors or extracellular matrix components may be necessary for fastidious cell types [70] [72].
Performance Validation: After stable growth is established in 100% animal-free media, validate system performance by assessing key parameters including:
- Population doubling time during exponential growth phase
- Maximum cell density at confluence
- Specific productivity (for protein-producing cells)
- Plating efficiency and colony-forming ability
- Maintenance of cell-specific markers and functionality [6]
For suspension cells, the adaptation process follows similar media mixing ratios but may require additional attention to agitation rates and gas exchange parameters. Some cell lines may require intermediate adaptation to serum-free media before transitioning to fully animal-free systems.
Research Reagent Solutions for Animal-Free Systems
Implementing animal-free cell culture requires replacing traditional serum-derived components with defined recombinant alternatives. The following table summarizes essential reagent categories and their functions in supporting cell growth and functionality:
Table 3: Essential Research Reagents for Animal-Free Cell Culture Systems
| Reagent Category | Specific Examples | Function in Culture System | Application Notes |
|---|---|---|---|
| Basal Media | DMEM, RPMI-1640, Ham's F-12 modifications | Provide essential nutrients, salts, vitamins, energy sources | Select formulations optimized for specific cell types (e.g., HEK293, CHO, stem cells) [72] |
| Recombinant Growth Factor Supplements | ITSE Animal-Free (insulin, transferrin, selenium, ethanolamine) | Insulin: metabolic regulation; Transferrin: iron transport; Selenium: antioxidant | Universal supplement for many cell types in serum-free conditions [72] |
| Cell-Specific Media | SMM 293-CD1, MCHOSI, Stem Cell Media | Formulations optimized for specific cell lineages with tailored nutrient composition | HEK293 media for transient protein expression; CHO media for stable protein production [72] |
| Attachment Factors | Recombinant laminin, fibronectin fragments | Replace serum-derived attachment proteins for adherent cells | Crucial for primary cells and sensitive adherent lines; concentration optimization required |
| Specialized Growth Factors | Recombinant FGF, EGF, TGF-β families | Signal-specific proliferation, differentiation, or maintenance | Preclinical and GMP grades available; species-specific variants (human, mouse, rat) [69] [70] |
| Cryopreservation Media | Animal-free cryoprotectant formulations | Maintain cell viability during freeze-thaw cycles without animal components | Enable complete animal-free workflow from culture to storage [69] |
Specialized media formulations exist for specific research applications. Stem cell research has particularly advanced in animal-free systems, with multiple commercial options available for human ES/iPS cells, neural stem cells (NSCs), mesenchymal stem cells (MSCs), and hematopoietic stem cells (HSCs) [69]. These formulations often incorporate small molecule cocktails such as the CEPT combination (Chroman 1, Emricasan, Polyamine Supplement, Trans-ISRIB) to enhance viability during passaging, single-cell cloning, and cryopreservation [70].
For biopharmaceutical production, specialized media support high-density culture and recombinant protein production. HEK293 systems benefit from media optimized for transient protein expression and lentiviral packaging, while CHO cell media are designed for stable protein expression in DHFR or GS selection systems [72]. Supplementation with specific expression enhancers (e.g., SMS 293-SUPI, SMS CHO-S-SUPI) added post-transfection can significantly increase product yields [72].
Technological Advancements and Future Directions
The field of animal-free cell culture continues to evolve rapidly, driven by technological innovations that enhance system performance and applicability. Several key trends are shaping the future landscape of defined culture systems:
Process Intensification techniques including perfusion culture and continuous processing are transforming upstream biomanufacturing by enhancing efficiency, reproducibility, and product quality [76]. These approaches maintain optimal cell growth by continuously removing waste products and adding fresh nutrients, allowing higher cell densities and productivity without scale increases. The integration of advanced process analytical technology (PAT) enables real-time monitoring of critical parameters including pH, dissolved oxygen, glucose, lactate, and cell density, facilitating immediate adjustments to maintain optimal culture conditions [76].
Cell Line Engineering advancements are creating hosts specifically optimized for performance in defined systems. Multiplexed CRISPR editing enables simultaneous modifications across multiple genes to optimize cellular metabolism, reduce metabolic waste, and enhance productivity [76]. Targeted integration methods allow precise insertion of expression constructs, significantly reducing clone screening efforts while improving stability and productivity [76]. These engineered cell lines demonstrate improved performance in chemically defined media, supporting more consistent manufacturing processes.
Artificial Intelligence and Automation are increasingly applied to optimize culture systems and improve reproducibility. AI algorithms analyze sensor data to identify subtle changes in cell behavior, enabling real-time adjustments to culture conditions [74]. Automated systems for medium preparation, sample handling, and monitoring reduce variability while increasing throughput [74] [76]. These technologies are particularly valuable for design of experiments approaches to optimize complex media formulations for specific applications.
The convergence of these technologies supports the development of increasingly sophisticated animal-free systems capable of supporting diverse applications from basic research to clinical manufacturing. As these systems mature, they promise to further enhance reproducibility, reduce costs, and accelerate development timelines across the biotechnology sector.
The comprehensive implementation of chemically defined media and recombinant reagents represents a fundamental advancement in cell culture technology. For microbiologists expanding into mammalian systems, these defined approaches offer familiar principles of controlled, reproducible culture conditions while addressing the complex nutritional requirements of mammalian cells. The strategic transition to animal-free systems requires careful planning, systematic adaptation, and thorough validation, but delivers significant benefits through enhanced experimental reproducibility, reduced contamination risk, and improved regulatory compliance.
As the field continues to evolve, technological innovations in process monitoring, cell engineering, and data analytics will further enhance the capabilities and applications of defined culture systems. The ongoing shift toward animal-free platforms reflects both ethical progression in research practices and technical advancement in our ability to precisely control the cellular microenvironment, ultimately supporting more reliable research outcomes and safer therapeutic products.
Solving Common Problems and Optimizing Culture Health
In the field of animal cell culture, microbial contamination represents one of the most significant challenges compromising research integrity and biomanufacturing quality. Unlike chemically synthesized medicines, biopharmaceuticals derived from dynamic biological systems exhibit "unique vulnerability to contamination" due to their biological inputs and growth conditions [77]. Contaminants including bacteria, mycoplasma, and viruses can ingress at any process point from cell-line development through fill–finish, potentially compromising product quality, efficacy, and patient safety [77]. For microbiologists and drug development professionals, implementing a comprehensive, proactive contamination control strategy is essential—moving beyond traditional reactive testing toward layered, risk-based approaches that prevent microbial intrusion throughout the manufacturing process.
The insidious nature of contamination is particularly problematic for cell therapies, which cannot undergo purification steps like chromatography that purify protein drugs, making microbial contamination especially risky for patients [77]. This technical guide provides an in-depth examination of major contamination types—bacterial, mycoplasma, and viral—with detailed methodologies for their identification, eradication, and prevention within the context of animal cell culture systems.
Contamination Profiles: Characteristics, Impacts, and Detection
Understanding the distinct profiles of various contaminants is fundamental to developing effective control strategies. The table below summarizes the key characteristics, impacts, and detection methods for bacterial, mycoplasma, and viral contaminants in cell culture systems.
Table 1: Comparative Profiles of Major Cell Culture Contaminants
| Contaminant Type | Size Range | Primary Characteristics | Impact on Cell Culture | Detection Window |
|---|---|---|---|---|
| Bacteria | 0.5-5 μm | Prokaryotic with cell walls; visible pH change/turbidity | Metabolic competition; altered gene expression; cell death | 1-3 days (traditional methods) [77] |
| Mycoplasma | 0.3-0.8 μm | Smallest prokaryotes; lack cell wall; filter-penetrating | Altered metabolism, proliferation, gene expression; chromosomal aberrations [78] | Weeks (culture); 3-4 hours (PCR) [78] |
| Viruses (e.g., LCMV) | 110-130 nm | RNA viruses; pleiomorphic; sand-like granularities | Species-dependent; can persist silently or cause cytopathic effects | Variable (PCR, serology, viral culture) [79] |
| Bacterial Endotoxins | ~10 kDa (aggregates to 1000 kDa) | Heat-stable LPS from gram-negative bacterial membranes | Induces inflammation; affects cell growth/function; confounds research [80] | Immediate (LAL assay) [81] [80] |
Bacterial Contamination and Endotoxins
Bacterial contamination typically manifests through visible turbidity, pH changes, or rapid culture deterioration. However, the associated endotoxins (lipopolysaccharides/LPS from gram-negative bacterial cell walls) present a more insidious challenge. These heat-stable molecules can significantly impact cell biology even in the absence of viable bacteria, affecting cell growth, function, and research outcomes [80]. Endotoxins are detected using the Limulus Amebocyte Lysate (LAL) test, which can identify levels as low as 0.01-0.03 Endotoxin Units (EU)/mL through gel-clot, turbidimetric, or chromogenic methods [81] [80]. The U.S. Food and Drug Administration (FDA) has established endotoxin limits for pharmaceuticals, typically using the formula K/M, where K=5.0 EU/kg (human threshold pyrogen dose) and M=maximum human dose per kg administered in a single hour [81].
Mycoplasma Contamination
Mycoplasma species represent a particularly challenging contaminant due to their small size (0.3-0.8 μm), which allows them to penetrate standard 0.22 μm sterilization filters [78]. Lacking cell walls, they are resistant to antibiotics like penicillin and streptomycin and can persist asymptomatically in culture while significantly altering host cell biology [78]. Studies suggest 5-35% of bioproduction cell lines harbor mycoplasma contamination, which can affect cell proliferation, metabolism, and cause chromosomal aberrations without causing cell death [77] [78]. Mycoplasma contamination has been shown to interfere with genomic studies, dysregulate hundreds of host genes, and compromise the interpretation of gene expression studies and epigenetic analyses like ATAC-seq [78].
Viral Contaminants
Viral contaminants such as Lymphocytic Choriomeningitis Virus (LCMV) present unique challenges. LCMV, an arenavirus with pleiomorphic structure and 110-130nm diameter, can infect laboratory cell cultures through contaminated rodent populations or their secretions [79]. While often asymptomatic in immunocompetent hosts, certain strains can cause serious disease, particularly in transplacental transmission where it may cause spontaneous abortion, microcephaly, or neurological deficits [79]. Viral contaminants are particularly concerning because they may persist silently in cell cultures without obvious cytopathic effects, only to be discovered when they compromise experimental results or biological products.
Detection Methodologies and Experimental Protocols
Traditional versus Rapid Microbial Methods
Traditional microbiological testing methods include compendial tests for bioburden, such as sterility testing that requires up to 14 days for contamination detection [82]. For water-soluble products, this typically involves passing samples through 0.45-μm filters, placing them in culture medium, and observing for microbial growth over several days to two weeks [77]. While effective, these extended timeframes are problematic for cell therapies where patients may need immediate treatment [82].
Rapid microbiological methods (RMMs) can reduce testing periods to approximately seven days but still require complex processes including cell extraction and growth enrichment mediums, along with significant technical expertise [82]. Novel approaches are emerging that combine ultraviolet light absorbance spectroscopy with machine learning to provide contamination detection within 30 minutes, offering a preliminary screening method that enables earlier corrective actions [82].
PCR-Based Mycoplasma Detection Protocol
Polymerase chain reaction (PCR) provides extremely sensitive, specific, and rapid detection of mycoplasma contamination, allowing researchers to respond quickly when contamination is detected [78]. The following protocol outlines a standardized procedure for mycoplasma diagnosis:
Table 2: Key Reagents for Mycoplasma Detection via PCR
| Reagent/Equipment | Function | Example Specification |
|---|---|---|
| Cell Culture Supernatant | Sample source for mycoplasma detection | After ≥12 hours of cell culture |
| PCR Primers | Amplify mycoplasma-specific DNA sequences | Mycoplasma-F: GGGAGCAAACAGGATTAGTATCCCT; Mycoplasma-R: TGCACCATCTGTCACTCTGTTAACCTC [78] |
| Taq Plus Master Mix | DNA amplification with high fidelity | 2× concentration with dye for visualization |
| Thermal Cycler | Programmable temperature control for PCR | Standard PCR cycling capabilities |
| Agarose Gel Electrophoresis | Separation and visualization of PCR products | 1.5% agarose-TAE gel containing 1× Gel stain |
Procedure (TIMING: 3-4 hours):
- Collect 200 μL of cell culture supernatant after at least 12 hours of cell culture.
- Transfer to a sterile 1.5-mL safe lock tube and incubate at 95°C for 5 minutes.
- Prepare PCR reaction mix according to manufacturer specifications, including appropriate positive and negative controls.
- Add 1 μL of prepared sample to the PCR mix.
- Run PCR with appropriate cycling conditions for the selected primers.
- Analyze PCR products using gel electrophoresis (1.5% agarose) with transillumination to visualize amplified bands.
- Interpret results: A positive band at the expected size indicates mycoplasma contamination.
Critical Notes: Primers should be stored at -20°C in small aliquots to avoid multiple freeze-thaw cycles. Processed samples can be stored at 2-8°C for up to one week or at -20°C for several months [78].
LAL Endotoxin Testing Methodologies
The Limulus Amebocyte Lysate (LAL) test is the standard for endotoxin detection, with four FDA-approved methods available [81]:
- Gel-clot method: Qualitative assessment based on gel formation
- Turbidimetric method: Spectrophotometric measurement of turbidity development
- Chromogenic assay: Colorimetric measurement of chromophore release
- Colorimetric method: Based on Lowry protein detection
All LAL reagents must be obtained from FDA-licensed manufacturers and validated for each specific product due to potential interference issues. Certain products may inhibit the LAL reaction through chemical means (EDTA, fluorescein, extreme pH) or physical means (adsorption, viscosity) [81]. Most interference can be overcome through sample dilution, though validation with low-level endotoxin spikes is essential to demonstrate recovery efficiency [81].
Comprehensive Prevention and Control Strategies
Proactive Contamination Control Framework
Effective contamination control requires a proactive, layered approach addressing multiple potential contamination sources throughout the bioprocess. Key elements include:
Diagram 1: Comprehensive Contamination Control Framework
Aseptic Technique and Laboratory Practices
Proper aseptic technique forms the foundation of contamination prevention. Essential practices include [78] [83]:
- Wearing appropriate personal protective equipment (PPE) including gloves and clean lab coats (changed weekly)
- Maintaining clean, organized cell culture hoods with unobstructed airflow
- Spraying all items with 75% alcohol before placement in the hood
- Keeping plates and bottles properly covered
- Avoiding hands and arms moving over open dishes and flasks
- Promptly cleaning spills and maintaining clean incubators
- Isolating new or untested cell lines in designated incubators until confirmed contamination-free
Additional sterilization techniques include using antibiotics/antimycotic supplements in culture media, disinfecting surfaces with 10% bleach solutions, and ensuring proper disposal of cell-containing containers in biohazard bins after treatment with bleach [83].
HEPA Filtration and Environmental Control
High-Efficiency Particulate Air (HEPA) filtration represents a critical component in maintaining controlled environments. HEPA filters can theoretically remove at least 99.97% of dust, pollen, mold, bacteria, and airborne particles sized 0.3 microns, with higher efficiency for larger and smaller particles [84]. Studies indicate approximately 10% of process contamination originates from airflow in cleanrooms, making proper HEPA system function essential [77].
HEPA filter classification varies by region, with North America typically using IEST-RP-CC001, while other regions employ ISO29463 or EN1822 standards [85]. These filters are constructed from randomly arranged glass microfibers creating tortuous paths for particle capture, housed in robust frames with proper sealing systems to prevent bypass leakage [85]. Regular testing and validation according to ISO 14644-3 standards are essential for maintaining controlled environments in pharmaceutical manufacturing, healthcare, and research laboratories [85].
Eradication Protocols and Specialized Procedures
Mycoplasma Eradication
When mycoplasma contamination is detected, several eradication approaches may be employed:
- Antibiotic Treatments: Specific anti-mycoplasma agents can be effective, though resistance is a concern
- Reagent Passage: Some protocols involve passage through 0.1μm filters, though this is not completely effective
- Temperature Manipulation: Heat treatment at 41°C for several hours has shown efficacy for some species
- Macrophage Co-culture: Utilizing primary macrophages to phagocytose mycoplasma contaminants
However, many experts recommend discarding contaminated cultures whenever possible, as eradication attempts may select for resistant variants or create persistent subpopulations that evade treatment [78].
Endotoxin Removal
Endotoxin removal presents special challenges due to their heat stability and adhesive properties. Removal strategies include:
- Using Triton X-114: Leveraging its micellar properties to separate LPS endotoxins from samples
- Depyrogenation: High-temperature treatment (e.g., 250°C for 45 minutes) to destroy pyrogenic activity
- Ultrafiltration: Size-based separation methods
- Chromatography: Adsorption techniques using activated charcoal or specialized resins
Prevention through use of endotoxin-tested reagents and proper aseptic technique remains the most effective strategy [80].
The Researcher's Toolkit: Essential Reagents and Materials
Table 3: Essential Research Reagents and Materials for Contamination Control
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Ready-to-Use Cell Culture Media | Pre-formulated media solutions | Reduces preparation variability and contamination risk; optimized for specific cell types [86] |
| LAL Reagents | Endotoxin detection | Must be from FDA-licensed manufacturers; validate for each product [81] |
| PCR Master Mix & Primers | Mycoplasma detection | Specific primers for conserved mycoplasma regions; aliquot to avoid freeze-thaw cycles [78] |
| HEPA Filtration Systems | Airborne contamination control | Validate per ISO 14644-3; monitor pressure drop for replacement timing [85] |
| Antibiotic/Antimycotic Supplements | Prevent bacterial/fungal growth | Incorporated into culture media; does not replace aseptic technique [83] |
| Sterile Single-Use Systems | Disposable equipment | Reduce cross-contamination risks; validate vendor sterility assurance [77] |
| Validated Reference Materials | Quality control standardization | USP microbiological standards for method validation [77] |
| Decontamination Solutions | Surface sterilization | 75% ethanol for hood surfaces; 10% bleach for biohazard disposal [78] [83] |
Emerging Technologies and Future Directions
The field of contamination control continues to evolve with several promising developments:
- Machine Learning-Enhanced Detection: UV absorbance spectroscopy combined with machine learning algorithms can provide rapid (30-minute) contamination screening with simple workflows [82]
- Advanced HEPA Technologies: Ongoing development of HEPA filters with reduced airflow resistance while maintaining efficiency, along with smart monitoring integration for predictive maintenance [85]
- Cryopreserved Reference Materials: Development of standardized reference materials to improve testing validation and reliability [77]
- Automated Monitoring Systems: Integration of real-time sensors and automated sampling to reduce operator variability and enable continuous culture monitoring [82]
These advancements support the industry shift toward proactive, risk-based quality assurance frameworks that emphasize prevention throughout the manufacturing process rather than relying solely on end-product testing [77].
Effective contamination control in animal cell culture requires a comprehensive, multifaceted strategy addressing bacterial, mycoplasma, and viral contaminants through rigorous prevention, detection, and eradication protocols. By implementing robust aseptic techniques, environmental controls, validated testing methodologies, and emerging technologies, researchers and biomanufacturers can significantly reduce contamination risks, ensuring research integrity and product safety. The field continues to advance toward more rapid, automated systems that provide earlier detection and intervention, ultimately supporting the production of safer biologics and more reliable research outcomes.
For microbiologists venturing into the world of animal cell culture, quantitative morphological analysis represents a powerful bridge between established microbiological principles and advanced cellular biotechnology. This discipline involves extracting numerical data from cell microscopy images to generate quantitative profiles that portray key information about cell structure and bioprocesses [87]. In the context of a broader thesis on animal cell culture basics, understanding cell morphology is paramount as it offers a means of identification and classification of key morphological parameters linked to cell bioactivity and cell health, which is of great interest to both academic and industrial research sectors [87]. Unlike alternative analysis methods such as plate-based viability assays or cytometry-based expression assays, morphological analysis can discriminate subtle morphological variations that other techniques might miss [87].
The application of this approach is particularly valuable in drug development processes due to its high-throughput potential to assess large datasets and improve analysis efficiency [87]. Furthermore, morphological profiling provides complementary data to existing biological techniques such as molecular profiling, protein biomarker detection, and plate-based assays, thus establishing a crucial link across multiple analysis methodologies [87]. As the field progresses, researchers are focusing on identifying a minimal set of morphological measurands, often termed critical quality attributes (CQAs), which are traceable to standardized (SI) units of measurement to improve data comparability across studies and laboratories [87].
Foundational Concepts in Quantitative Morphology
Principles of Quantitative Morphological Phenotyping
Quantitative morphological phenotyping (QMP) is an image-based method used to capture morphological features at both the cellular and population level [88]. This interdisciplinary methodology spans from data collection to result analysis and interpretation, and can leverage subtle cellular morphological changes to achieve high analytical specificity [88]. The process typically involves the analysis of key morphological features of differing cell populations and organelles, which generally consists of analyzing fluorescent intensity, shape features, and co-localization of signals [87].
The analytical process requires sophisticated approaches that can be challenging for those new to the field. A systematic workflow typically includes several key steps: sample preparation, image acquisition, image processing, feature extraction, and data analysis [88]. In each step, researchers must choose from various available methods, each with specific applications, advantages, and disadvantages that can significantly impact the final results [88].
Key Cellular Structures and Their Morphological Indicators
The interpretation of cell morphology typically focuses on specific cellular components that serve as indicators of cellular state. Since cell imaging concentrates on morphological features such as cell nuclei, actin cytoskeletons, mitochondria networks, and cell membranes, these represent the primary cellular components considered in morphological analysis [87]. Each of these structures exhibits characteristic changes in response to stress, senescence, or compromised health:
- Nucleus: Often shows changes in size, shape, chromatin organization, and membrane integrity in stressed or senescent cells.
- Actin Cytoskeleton: Undergoes reorganization in response to various stressors, which can be quantified through morphological analysis.
- Mitochondria: Exhibits fragmentation, swelling, or changes in network complexity under stress conditions.
- Cell Membrane: Shows alterations in integrity, blebbing, or changes in membrane potential during stress or senescence.
Quantitative Parameters for Assessing Cellular States
Core Morphological Parameters and Their Interpretation
The tables below summarize key quantitative parameters used in morphological analysis and how they relate to cellular states of stress, senescence, and poor health.
Table 1: Key Quantitative Morphological Parameters for Cell Health Assessment
| Cellular Structure | Morphological Parameter | Normal/Healthy State | Stress/Senescence Indicators |
|---|---|---|---|
| Nucleus | Nuclear Area | Consistent size within cell type | Significant increase or decrease |
| Nuclear Shape (Circularity, Irregularity) | Regular, defined shape | Increased irregularity, blebbing | |
| Chromatin Texture | Homogeneous distribution | Condensation, fragmentation | |
| Actin Cytoskeleton | Filamentous Actin Organization | Well-organized stress fibers | Disrupted, fragmented organization |
| Cytoplasmic Spreading | Consistent spread area | Reduced spreading area | |
| F-actin Intensity | Consistent intensity | Significant increase or decrease | |
| Mitochondria | Network Branching | Interconnected tubular network | Fragmented, punctate morphology |
| Mitochondrial Length | Elongated tubules | Shortened, rounded morphology | |
| Membrane Potential | High, stable potential | Depolarized, heterogeneous | |
| Cell Membrane | Membrane Integrity | Intact, continuous | Blebbing, perforations |
| Cell Area/Volume | Consistent within population | Abnormal shrinkage or swelling | |
| Membrane Ruffling | Controlled, dynamic | Excessive or absent ruffling |
Table 2: Advanced Morphological Features in Senescence and Stress
| Feature Category | Specific Measurand | Technical Measurement Approach | Association with Cellular State |
|---|---|---|---|
| Senescence-Associated | SA-β-gal Activity | Fluorescence intensity quantification | Increased in senescent cells |
| Lipofuscin Accumulation | Autofluorescence detection | Accumulates in aged/stressed cells | |
| Senescence-Associated Heterochromatin Foci | Chromatin texture analysis | Increased nuclear foci | |
| Stress Response | ROS Accumulation | Fluorescent probe intensity | Elevated in oxidative stress |
| Oxidative Stress Markers | Immunofluorescence quantification | Increased with stress severity | |
| HSP Expression & Localization | Fluorescence co-localization analysis | Altered expression and localization | |
| Cell Cycle & Death | Mitotic Index | Cell counting with specific markers | Decreased in senescence/stress |
| Apoptotic Morphology | Membrane blebbing, chromatin condensation | Increased in late-stage stress | |
| Sub-G1 Population | DNA content quantification via flow cytometry | Increased in apoptosis |
Analytical Techniques and Measurement Tools
The field of quantitative morphology employs various sophisticated methods to generate reliable numbers that describe the nervous system in terms of the volumes, surfaces, lengths, and numbers of its components [89]. These methods, collectively known as design-based stereology, are firmly based in mathematics and provide unbiased estimation of morphological parameters [89]. Importantly, understanding their mathematical background is not necessary for their informed and productive application, making them accessible to microbiologists expanding into animal cell culture [89].
Common stereological approaches include:
- Point probes for estimating volume (Area Fraction Fractionator)
- Line probes for estimating surface area (vertical sections design)
- Area probes for estimating length (Spaceball probe)
- Volume probes for estimating number (Disector) [89]
These methods solve problems associated with other quantitative approaches by providing mathematically proven techniques that yield accurate estimates without the need for exhaustive counting of all elements in a sample [89].
Methodological Framework: From Image Acquisition to Analysis
Systematic Data Analysis Pipeline
A systematic data analysis pipeline is essential for robust quantitative morphological phenotyping [88]. The workflow typically involves multiple stages from experimental design to final interpretation, with each step requiring careful consideration of available methods and their implications for the final results.
Experimental Protocols for Key Assessments
Protocol 1: Assessment of Hyperglycemic-Induced Oxidative Stress and Senescence Based on research using human corneal epithelial (HCE-T) cells [90]
Cell Culture and Treatment:
- Culture HCE-T cells in medium containing 17.5 mM glucose (normal) or elevated glucose concentrations (25-50 mM) to induce hyperglycemic stress.
- For interventional studies, treat cells with glucosamine (GlcN) at concentrations ranging from 0-10 mM for 24 hours.
Cell Viability Assessment (MTT Assay):
- Plate cells at appropriate density in 96-well plates and allow to adhere overnight.
- Apply experimental treatments for designated time periods.
- Add MTT reagent (0.5 mg/mL final concentration) and incubate for 2-4 hours at 37°C.
- Dissolve formed formazan crystals with DMSO or isopropanol.
- Measure absorbance at 570 nm with reference wavelength at 630-650 nm.
Cell Cycle Analysis via Flow Cytometry:
- Harvest cells by trypsinization and wash with PBS.
- Fix cells in 70% ethanol at -20°C for at least 2 hours.
- Wash cells and resuspend in PBS containing RNase A (100 µg/mL).
- Add propidium iodide (50 µg/mL) and incubate for 30 minutes at room temperature in the dark.
- Analyze DNA content using flow cytometry to determine cell cycle distribution (sub-G1, G1, S, G2/M phases).
Reactive Oxygen Species (ROS) Detection:
- Load cells with CM-H2DCFDA (5 µM) in serum-free medium for 30 minutes at 37°C.
- Wash cells with PBS and apply experimental treatments if required.
- Measure fluorescence intensity using microplate reader (excitation 485 nm, emission 535 nm) or analyze via fluorescence microscopy.
Protein Expression Analysis (Western Blotting):
- Lyse cells in RIPA buffer containing protease and phosphatase inhibitors.
- Separate proteins by SDS-PAGE and transfer to PVDF membranes.
- Block membranes and probe with primary antibodies against SIRT1, KLF4, fibronectin, claudin-1, and loading control (e.g., β-actin).
- Incubate with HRP-conjugated secondary antibodies and detect using chemiluminescence.
Protocol 2: Morphological Analysis of Fixed Cells
Cell Staining for Key Structures:
- Fix cells with 4% paraformaldehyde for 15 minutes at room temperature.
- Permeabilize with 0.1% Triton X-100 in PBS for 10 minutes if intracellular staining is required.
- Block with 1-5% BSA in PBS for 30-60 minutes.
- Incubate with primary antibodies or specific stains for:
- Nuclei: DAPI (300 nM) or Hoechst 33342 (1-5 µg/mL)
- Actin cytoskeleton: Phalloidin conjugates (e.g., Alexa Fluor 488-phalloidin, 1:200-1:500)
- Mitochondria: MitoTracker dyes (50-200 nM) or antibodies against mitochondrial proteins
- Cell membrane: Wheat Germ Agglutinin (WGA) conjugates (1-5 µg/mL)
Image Acquisition:
- Acquire images using confocal or widefield fluorescence microscopy.
- For confocal microscopy, capture Z-stacks at appropriate intervals to create 3D representations.
- Maintain consistent acquisition settings (exposure time, gain, laser power) across experimental conditions.
Image Analysis:
- Use automated image analysis tools (e.g., CellProfiler, ImageJ/FIJI with appropriate plugins) for segmentation and feature extraction.
- Segment individual cells and cellular compartments based on staining patterns.
- Extract morphological parameters including area, perimeter, circularity, intensity, and texture features.
Signaling Pathways in Cellular Stress Responses
Understanding the molecular pathways underlying morphological changes is crucial for interpreting cell health status. The diagram below illustrates the SIRT1 pathway, which plays a key role in cellular responses to oxidative stress and senescence, as identified in studies on hyperglycemic stress [90].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Morphological Analysis of Cellular Stress
| Reagent/Material | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| Cell Viability Assays | MTT, MTS, WST-1 | Measures metabolic activity as indicator of cell viability and cytotoxicity | MTT produces formazan crystals requiring solubilization before reading [90] |
| ROS Detection Probes | CM-H2DCFDA, Dihydroethidium | Detection and quantification of reactive oxygen species in live cells | CM-H2DCFDA is cell-permeable and becomes fluorescent upon oxidation [90] |
| Senescence-Associated Markers | SA-β-gal Staining, Lipofuscin Autofluorescence | Histochemical detection of senescent cells in culture | SA-β-gal activity detected at pH 6.0 using X-gal substrate [90] |
| Cytoskeletal Stains | Phalloidin conjugates, Anti-tubulin antibodies | Visualization of actin cytoskeleton and microtubule network | Phalloidin binds F-actin with high specificity; various fluorophore conjugates available |
| Nuclear Stains | DAPI, Hoechst 33342, Propidium Iodide | DNA staining for nuclear visualization, cell cycle analysis, and viability assessment | Propidium iodide only penetrates cells with compromised membranes (dead cells) [90] |
| Pathway Inhibitors/Activators | EX-527, INZ (SIRT1 inhibitors) | Functional validation of specific pathway involvement in morphological responses | EX-527 is a specific SIRT1 inhibitor used to confirm SIRT1 pathway role [90] |
| Fixation/Permeabilization Reagents | Paraformaldehyde, Triton X-100, Methanol | Cell preservation and membrane permeabilization for intracellular staining | Paraformaldehyde (4%) commonly used for morphology preservation; concentration and time vary by cell type |
The interpretation of cell morphology through quantitative approaches provides microbiologists with powerful tools for assessing cellular health in animal cell culture systems. By recognizing the distinctive morphological signatures of stress, senescence, and poor health, researchers can gain deep insights into cellular status and response to experimental manipulations. The integration of systematic morphological analysis with molecular pathway investigation creates a comprehensive framework for understanding cellular behavior, which is essential for applications ranging from basic research to drug development and biomanufacturing. As standardization efforts progress through the identification of critical quality attributes and the development of validated methods, morphological analysis will continue to grow in importance as a key technique in the biotechnology and pharmaceutical sectors.
The reproducibility and success of animal cell culture, a cornerstone technique in life sciences research and biopharmaceutical development, hinge on the precise control of the physicochemical environment. This whitepaper provides an in-depth technical guide for researchers on optimizing four critical parameters: pH, CO2 concentration, temperature, and cell confluency. Framed within the context of animal cell culture basics for microbiologists, we synthesize current evidence-based guidelines, present quantitative data in structured tables, and detail advanced experimental protocols. By integrating foundational principles with advanced optimization methodologies like Bayesian optimization and Response Surface Methodology, this guide aims to empower scientists and drug development professionals to enhance cell health, experimental consistency, and recombinant protein yields.
Animal cell culture is an indispensable tool for studying cellular and disease biology, producing therapeutic proteins, and developing novel drugs. Unlike microbial cultures, mammalian cells are exquisitely sensitive to their physicochemical surroundings, as they have evolved to function within the tightly regulated milieu of a larger organism. The culture environment must therefore mimic in vivo conditions to support cell growth, maintain viability, and ensure the consistent production of biologically relevant data and products. For microbiologists transitioning to mammalian cell systems, this represents a paradigm shift from managing the environment for optimal population expansion to maintaining the homeostasis of individual, complex eukaryotic cells.
This guide focuses on four interdependent pillars of the culture environment: pH, CO2, temperature, and confluency. Inadequate control of any single parameter can induce cellular stress, alter metabolic pathways, compromise membrane integrity, and ultimately lead to experimental failure and poor reproducibility. Subsequent sections will dissect each parameter, providing foundational theory, evidence-based optimization strategies, detailed protocols for monitoring and control, and an overview of advanced, resource-efficient experimental design methods for systematic media and environment optimization.
The Critical Role of pH and Buffering Systems
Fundamentals of pH in Cell Culture
Extracellular pH is a fundamental variable that influences virtually every cellular process, including metabolism, proliferation, and membrane potential. Most normal mammalian cell lines grow optimally at a pH of 7.4, though some transformed lines may prefer a slightly more acidic environment (pH 7.0–7.4), and some normal fibroblast lines thrive in slightly more basic conditions (pH 7.4–7.7) [27]. The intracellular pH is typically maintained at a slightly lower level, around 7.2 [91]. Organelles such as mitochondria also maintain distinct pH levels, and significant deviations can disrupt their critical functions.
Buffering Systems in Culture Media
Buffers are mixtures of weak acids and their conjugate bases (or vice versa) that resist changes in pH by neutralizing added H+ or OH- ions. The effectiveness of a buffer is greatest when the pH of the solution is close to its acid dissociation constant (pKa) [92]. The relationship is described by the Henderson-Hasselbalch equation:
pH = pKa + log10([A-]/[HA])
where [A-] is the concentration of the base form and [HA] is the concentration of the acid form. The buffering capacity is the amount of acid or base that can be added before the pH changes significantly, and it is maximal at the buffer's pKa [91]. The following diagram illustrates the dynamic equilibrium of the primary buffering system used in cell culture.
The two primary buffering systems are:
CO2/Bicarbonate (HCO3-) Buffer: This is the most physiologically relevant system. Sodium bicarbonate (NaHCO3) is added to the medium, and it interacts with CO2 from the incubator atmosphere as shown in the equilibrium above [93]. A common misconception is that buffers set the pH to a predefined level; in reality, the pH is determined by the specific concentrations of HCO3- and CO2. The required [HCO3-] to achieve a target pH can be calculated, accounting for intrinsic buffering from serum components, using the formula [92]:
[HCO3-] = [CO2] x 10^(pH_target - 6.15) + β_intrinsic x (pH_target - 7.4)Non-Volatile Buffers (e.g., HEPES): Organic buffers like HEPES (pKa ≈ 7.3 at 37°C) are often used to augment buffering capacity, especially in open culture systems like dishes or when working outside a CO2 incubator [92] [91]. HEPES is a zwitterionic buffer effective in the pH range of 6.8-8.2.
Quantitative Guidelines for pH Control
The following table summarizes the relationship between CO2 concentration and bicarbonate levels required to achieve target pH values, which is critical for media formulation and incubator setup.
Table 1: CO2 and Bicarbonate Requirements for Target pH in Cell Culture Media at 37°C
| Target pH | Theoretical [CO2] Requirement | Recommended [NaHCO3] (mM) | Suitable for Media |
|---|---|---|---|
| ~7.4 (Physiological) | 4.5% - 6.5% | 26 mM | EMEM + Earle's Salts [93] |
| ~7.4 (Physiological) | 7.5% - 11% | 44 mM | DMEM [93] |
| ~7.0 (Slightly Acidic) | ~3% (Est.) | ~15-20 mM (Est.) | For some transformed lines [27] |
| ~7.7 (Slightly Basic) | ~8% (Est.) | ~30-35 mM (Est.) | For some fibroblast lines [27] |
Note: These values are theoretical and based on the Henderson-Hasselbalch equation. Direct pH measurement is always recommended for critical applications. Using DMEM (44mM NaHCO3) in a standard 5% CO2 environment will result in a pH of ~7.5-7.6, which may be corrected by metabolic activity in dense, healthy cultures [93].
Experimental Protocol: Preparing and Validating Media pH
Aim: To prepare culture medium buffered with CO2/HCO3- and validate its pH under incubation conditions.
Materials:
- Basal medium powder (e.g., DMEM, RPMI)
- Sodium bicarbonate (NaHCO3)
- HCl or NaOH for titration
- pH meter
- Sterile purified water
- CO2 incubator (calibrated to desired %CO2)
- Phenol Red-containing medium (for colorimetric assessment)
Method:
- Medium Preparation: Dissolve basal medium powder and the required amount of NaHCO3 (see Table 1) in sterile purified water. If the medium contains components like lactic acid in its acid form (not a salt), be aware that it will react with HCO3-, consuming the base and resulting in a lower-than-predicted pH; using salts like Na-lactate avoids this [92].
- Titration: Titrate the medium to the desired pH using sterile HCl or NaOH. It is critical that this is performed while the medium is equilibrated with the intended CO2 concentration. This often requires performing the titration in a container inside the incubator or while gently bubbling the medium with the correct CO2/air mixture.
- Sterile Filtration: Filter-sterilize the medium using a 0.22 μm membrane.
- Validation:
- Quantitative (Plate Reader): For precise measurement, use Phenol Red-containing medium. Prepare calibration standards of known pH in a CO2-free atmosphere. In a plate reader with an incubator function, measure the absorbance of your medium at 560 nm and 430 nm. The ratio (A560/A430) can be converted to pH using the standard curve [92].
- Qualitative (Visual): Phenol Red imparts an orange-red color at pH ~7.4. A yellow hue indicates acidic conditions (pH <7.0), while a purple/red hue indicates alkaline conditions (pH >7.8) [93].
CO2 Incubation and Temperature Control
The Symbiotic Relationship of CO2 and Temperature
CO2 concentration and temperature are not independent variables; they are functionally linked through the CO2/HCO3- buffering system and their collective impact on cellular metabolism. The solubility of CO2 in aqueous medium is temperature-dependent, and the pKa of the carbonic acid/bicarbonate equilibrium also shifts with temperature. Consequently, a buffer that is optimal at room temperature may not perform as expected at 37°C [91]. For instance, the neutral pH of water decreases as temperature rises, a phenomenon that also affects buffering solutions.
Optimal Parameters for Different Cell Lines
While standard conditions for many mammalian cells are 37°C and 5% CO2, the optimal settings are ultimately determined by the cell line's origin and the medium formulation.
Table 2: Optimal Temperature and CO2 Conditions for Various Cell Types
| Cell Type / Line | Optimal Temperature | Recommended CO2 | Notes |
|---|---|---|---|
| Human & Mammalian | 36°C – 37°C [27] | 5% (for 26mM HCO3- media) [27] [93] | Overheating is more serious than underheating [27]. |
| Avian Cell Lines | 38.5°C [27] | 5% (Typical) | Can be maintained at 37°C, but growth is slower. |
| Insect Cells (Sf9, Sf21) | 27°C [27] | Not strictly required | Media is typically more acidic (pH 6.2); pH rises with cell growth. |
| Cold-blooded Animals | 15°C – 26°C [27] | Varies with medium | Tolerate a wide temperature range. |
Advanced Optimization: Temperature Shift for Recombinant Protein Production
A powerful strategy to enhance recombinant protein yields in mammalian cells like CHO and HEK293 is a hypothermic shift. Standard cultivation begins at 37°C for robust cell growth. After 48 hours post-inoculation, the temperature is shifted down to 30-35°C. This arrest of the cell cycle extends culture longevity and diverts cellular resources from proliferation to protein production, often increasing specific productivity by at least 2-fold [94].
Incubator Setup, Calibration, and Maintenance Protocol
Proper installation and maintenance are crucial for reliable environmental control.
Aim: To ensure a CO2 incubator is correctly installed, calibrated, and maintained for optimal performance and contamination control.
Materials:
- CO2 incubator
- Two-stage CO2 regulator
- Source of CO2 and N2 (for tri-gas models)
- Certified CO2 calibration gas
- Certified reference thermometer
- Distilled water
- 70% isopropyl alcohol or other recommended disinfectant
- Personal Protective Equipment (PPE)
- Installation: Place the incubator on a stable, level surface away from heating/cooling vents, heat-producing equipment (e.g., autoclaves), and direct air currents. Connect to a dedicated power source with protective grounding. Install a two-stage regulator on the CO2 tank to prevent over-pressurization.
- Initial Cleaning: Before first use, clean the entire chamber and all removable parts (shelves, plenums, humidity pan) with 70% isopropyl alcohol. Avoid chlorine-based disinfectants as they can damage stainless steel.
- Calibration:
- Temperature: Using a certified reference thermometer, compare the actual chamber temperature to the display and calibrate the sensor if necessary. This should be performed quarterly.
- CO2 Sensor: Calibrate the infrared CO2 sensor using certified calibration gas. This is typically done by qualified technicians or trained lab personnel.
- Humidification: Fill the humidity pan with sterile distilled water only. Tap water contains chlorine and minerals that cause corrosion and scale buildup. Check the water level weekly and refill as needed.
- Routine Maintenance:
- Daily: Check CO2 tank pressure.
- Weekly: Check water level in humidity pan; inspect cultures for contamination.
- Quarterly/Annually: Calibrate sensors; change HEPA/ULPA filters (if applicable); perform a high-temperature decontamination cycle (e.g., 145°C) with an empty chamber.
Monitoring and Optimizing Cell Confluency
The Importance of Cell Density and Confluency
Cell confluency refers to the percentage of the culture surface area covered by adherent cells. Maintaining appropriate cell density is critical, as both too few and too many cells can stress the culture and alter its behavior [97]. Seeding density needs to be optimized for each cell type and experimental purpose. Some cells require close contact to thrive, while others prefer lower densities. Furthermore, primary cells and immortalized cell lines often have different density requirements and passaging schedules.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Culture Optimization
| Reagent / Material | Function | Application Example |
|---|---|---|
| HEPES Buffer | Non-volatile buffer augmenting CO2/HCO3- system. | Maintaining pH during manipulation outside incubator [92] [91]. |
| Sodium Bicarbonate | Conjugate base for the physiologically relevant CO2 buffering system. | Formulating media to work with specific CO2 tensions [93]. |
| Phenol Red | pH indicator dye. | Visual and spectrophotometric monitoring of medium pH [92] [93]. |
| Recombinant IGF-I | Growth factor supplement. | Replacing serum; can double cell viability over insulin in extended cultures [94]. |
| Poly-D-Lysine / Collagen | Extracellular matrix coating. | Promoting adhesion of sensitive cells to culture surfaces [97]. |
| Histone Deacetylase Inhibitors | Additive for transcriptional enhancement. | Boosting recombinant protein yields (e.g., sodium butyrate) [94]. |
| 0.1 μm Membrane Filters | Sterile filtration. | Removing mycoplasma contamination from media and reagents [97]. |
Advanced Experimental Design for Systematic Optimization
Traditional One-Factor-at-a-Time (OFAT) approaches are inefficient and fail to capture interacting effects between multiple culture parameters. Advanced statistical methods offer a more powerful alternative.
Response Surface Methodology (RSM): RSM is a set of statistical techniques for modeling and analyzing problems where several independent variables influence a dependent response. Using a Design of Experiments (DOE) approach, such as a d-optimal design, researchers can efficiently explore the effects of factors like seeding density, culture duration, and substrate patterning on outcomes like confluence and cell alignment [98]. This method can identify optimal conditions with fewer experiments than OFAT.
Bayesian Optimization (BO): For even more complex optimization tasks (e.g., involving 10s of media components), BO-based iterative design is a powerful resource-efficient framework. BO uses a probabilistic surrogate model (often a Gaussian Process) to represent the relationship between design factors (e.g., media component concentrations) and the target objective (e.g., cell viability, protein titer). It then strategically plans the next experiments by balancing the exploration of uncertain regions of the design space with the exploitation of known promising regions. This approach has been shown to identify improved cell culture media compositions using 3–30 times fewer experiments than standard DOE methods, even when dealing with complex constraints and categorical variables (e.g., different carbon sources) [64].
The workflow for applying Bayesian optimization to a problem like media development is summarized below.
Mastery over the cell culture environment is not a mundane task but a critical determinant of experimental success and bioprocess productivity. As this guide has detailed, precise and interdependent control of pH, CO2, temperature, and confluency is non-negotiable for maintaining healthy, reproducible mammalian cell cultures. Moving beyond basic maintenance, researchers can leverage advanced strategies like temperature shifting and sophisticated statistical optimization frameworks—including Response Surface Methodology and Bayesian Optimization—to systematically push the boundaries of cell culture performance, such as achieving high-yield recombinant protein production. By integrating these foundational principles and advanced methodologies, microbiologists and drug development professionals can ensure their in vitro models are robust, reliable, and truly reflective of the biological systems they seek to understand and exploit.
For researchers in microbiology and drug development, the successful culture of animal cells is a foundational technique for modeling biological systems, testing therapeutic compounds, and producing biological products. Within this context, cell health is paramount, and its failure often manifests through three core issues: slow growth, low viability, and a failure of adherent cells to attach. These problems not only hinder experimental progress but can also compromise the validity of downstream data. This guide provides an in-depth, technical troubleshooting framework, equipping scientists to diagnose and resolve these common yet critical challenges. A systematic approach to these issues is essential, as they often share underlying causes, such as suboptimal culture conditions or microbial contamination [99].
The growth and proliferation of cells in culture follow a characteristic sigmoidal pattern, comprising distinct phases: the Lag phase (acclimation), the Log or Exponential phase (active division), the Stationary phase (growth plateaus), and the Decline phase (cell death predominates) [100] [6]. Data collection and cell passaging are most effective during the logarithmic phase, before overcrowding induces stress [100]. Optimal cell health requires maintaining cells in this exponential phase through regular subculturing, thereby ensuring viability, genetic stability, and phenotypic stability [6]. When cells deviate from this expected growth pattern, a structured investigation into their environment and handling is required.
Diagnosing Slow Growth and Low Viability
Slow growth and low viability are often interconnected symptoms of a stressed cell population. A definitive diagnosis requires a methodical assessment of potential culprits, from culture conditions to the cells themselves.
Root Causes and Investigative Steps
The following table summarizes the primary causes and corresponding diagnostic actions for slow growth and low viability.
Table 1: Troubleshooting Slow Growth and Low Viability
| Category | Specific Cause | Diagnostic & Corrective Actions |
|---|---|---|
| Culture Environment | Incorrect incubator temperature or CO₂ [101] | Calibrate and continuously monitor incubator settings. |
| Nutrient insufficiency or improper pH [102] | Check medium formulation, prepare fresh medium, and ensure proper CO₂ equilibration. | |
| Reagents and Media | Poor-quality or incompatible serum [99] [102] | Test growth with a new lot of qualified, application-appropriate serum. |
| Improper storage or expired media [102] | Strictly adhere to storage conditions and expiration dates. | |
| Cell Stock and Handling | Low seeding density [102] | Adjust seeding concentration based on the cell line's specific requirements. |
| Over-passaging or high passage number [100] | Return to a low-passage stock vial and monitor characteristics. | |
| Inaccurate cell counting [99] | Employ automated cell counters for superior precision [100]. | |
| Contamination | Microbial (e.g., bacteria, fungus) [102] | Regularly inspect cultures for turbidity and pH shifts; practice sterile technique. |
| Mycoplasma contamination [99] | Implement a routine PCR-based testing schedule. |
Record Keeping and a Systematic Approach
A critical first step in troubleshooting is realizing a problem exists, as many growth issues can be subtle [100]. Meticulous record-keeping is indispensable for isolating variables. Essential information to document includes:
- Cell Stock Details: Source, passage number, seeding density, and freezing protocol [100].
- Reagent Information: Lot numbers, dates of first use, and concentrations for all media, sera, and buffers [100].
- Equipment & Environment: Records of incubator servicing, CO₂ tank replacement, and mycoplasma screening [100].
Sometimes, the most efficient path is not to isolate the single culprit but to "cut your losses" and initiate a fresh start with a new stock vial of cells and all new media, sera, and buffers [100]. This approach can save significant time and resources compared to testing each variable individually.
Resolving Failure of Adherent Cells to Attach
For adherent cell phenotypes, attachment is the first critical step for survival and proliferation. Failure to attach indicates significant stress, often stemming from the culture environment or physical handling.
Primary Causes of Poor Attachment
The most common causes of attachment failure are related to environmental stress and suboptimal culture conditions [101]. Key factors include:
- Environmental Stress: Fluctuations in incubator temperature, an inappropriate gas mixture, or chemical contamination can prevent successful attachment [101].
- Inadequate Culture Surface: The cultureware may lack the necessary surface treatment or coating of extracellular matrix (ECM) proteins (e.g., collagen, fibronectin) required by certain cell types for attachment and spreading [101].
- Over-trypsinization: Excessive duration or concentration of enzymatic dissociation can damage adhesion proteins on the cell membrane, impairing the cells' ability to re-attach after passaging [102]. This is a common issue with cells like 293Ts [102].
- Improper Seeding Concentration: A seeding concentration that is too low can result in insufficient cell-cell interaction, which is sometimes necessary to form effective adhesions [102].
Troubleshooting Attachment Problems
When faced with attachment failure, systematically assess and correct the following:
- Verify Culture Conditions: Confirm incubator temperature and CO₂ levels are stable and optimal for your cell line [101].
- Coating Optimization: For fastidious cell types, coat culture vessels with ECM proteins. For example, fetal lung fibroblasts (MRC-5 cells) show dramatically improved attachment and expansion on ECM-coated surfaces [101].
- Optimize Dissociation: Strictly control trypsinization time and concentration. To minimize damage, pre-rinse the flask with PBS or pre-warm trypsin to 37°C to reduce the required digestion time [102].
- Adjust Seeding Density: Adhere to the cell line's recommended seeding density to ensure sufficient concentration for attachment without causing resource competition [102].
Essential Experimental Protocols for Assessment
Rigorous, standardized protocols are the backbone of effective troubleshooting. The following methods are critical for quantifying and monitoring cell health.
Accurate Cell Counting and Passaging
Faulty cell counts can lead to mistaken conclusions about cell health and improper seeding densities [100] [99].
Protocol: Enzymatic Dissociation of Adherent Cells [103]
- Aspirate and Wash: Remove and discard spent media. Wash the cell monolayer with a balanced salt solution without calcium and magnesium to remove residual divalent cations.
- Add Dissociation Reagent: Add a pre-warmed dissociation solution (e.g., 0.25% trypsin, TrypLE Express) to the flask, ensuring it covers the cell sheet. Incubate at 37°C.
- Monitor Detachment: Gently rock the flask and monitor under a microscope. The process typically takes 5-15 minutes. Tap the flask gently if needed to expedite removal of strongly adherent cells.
- Neutralize and Harvest: When cells are detached, add complete growth medium to neutralize the enzyme. Pipette the suspension to disperse cells.
- Centrifuge and Resuspend: Transfer the suspension to a conical tube and centrifuge at 100–200 × g for 5–10 minutes. Discard the supernatant and resuspend the cell pellet in fresh, pre-warmed complete medium.
- Count and Seed: Determine viable cell density and percent viability using an automated cell counter or hemocytometer. Seed new flasks at the recommended density.
Cell Viability Assays
Viability assays measure an aspect of general metabolism or an enzymatic activity as a marker of viable cells [104].
Protocol: MTT Tetrazolium Reduction Assay [104]
- Prepare MTT Solution: Dissolve MTT in DPBS to a concentration of 5 mg/mL. Filter-sterilize and store protected from light at 4°C.
- Add to Cells: After treatment, add the MTT solution to cells in culture to a final concentration of 0.2–0.5 mg/mL. Incubate for 1–4 hours at 37°C.
- Solubilize Formazan: Viable cells with active metabolism will convert the yellow MTT to a purple formazan precipitate. After incubation, carefully remove the medium and add a solubilization solution (e.g., 40% DMF, 2% glacial acetic acid, 16% SDS, pH 4.7).
- Measure Absorbance: Once the formazan crystals are fully dissolved, transfer the solution to a microplate and record the absorbance at 570 nm using a plate-reading spectrophotometer. The amount of formazan product is proportional to the number of metabolically active viable cells.
Diagram 1: MTT assay workflow.
The Scientist's Toolkit: Key Reagents and Materials
Successful cell culture relies on a suite of high-quality, purpose-fit reagents. The following table details essential materials for troubleshooting and routine culture.
Table 2: Essential Research Reagent Solutions for Cell Culture
| Reagent Category | Specific Examples | Function & Application |
|---|---|---|
| Cell Culture Media | DMEM, RPMI-1640, Opt-MEM [99] | Provides essential nutrients, pH buffer, and energy sources to support cell growth and proliferation. |
| Serum & Supplements | Fetal Bovine Serum (FBS) [99] | Rich source of growth factors, hormones, and attachment factors that promote cell viability and division. |
| Dissociation Reagents | Trypsin, TrypLE Express, Collagenase, Dispase, Cell Dissociation Buffer [103] | Enzymatic or non-enzymatic solutions for detaching adherent cells for subculturing. Selection depends on cell type and sensitivity. |
| Extracellular Matrix (ECM) Proteins | Collagen, Fibronectin, Laminin [101] | Coating for culture vessels to enhance cell attachment and spreading, particularly for sensitive or primary cells. |
| Antibiotics | Penicillin-Streptomycin, Amphotericin B [99] | Used to prevent bacterial and fungal contamination in cell cultures, though their routine use in the absence of contamination is debated. |
| Cryopreservation Agents | Dimethyl Sulfoxide (DMSO) [6] | Permeates cells to prevent ice crystal formation, thereby protecting cell viability during the freezing process. |
Effective troubleshooting requires a holistic view of the cell culture ecosystem. The following diagram synthesizes the key steps for diagnosing and remedying slow growth, low viability, and attachment failure into a single, logical workflow.
Diagram 2: Integrated troubleshooting workflow.
In conclusion, navigating the challenges of slow growth, low viability, and attachment failure demands a disciplined, systematic approach grounded in a thorough understanding of cell biology. Success hinges on meticulous observation, precise record-keeping, and the consistent use of high-quality reagents [100] [6]. By adhering to the structured diagnostic frameworks, standardized protocols, and integrated workflow outlined in this guide, researchers and drug development professionals can effectively safeguard their cell cultures. This not only ensures the reliability of experimental data but also enhances the efficiency and reproducibility of research within the critical field of animal cell culture.
Best Practices for Media Selection, Serum Use, and Routine Culture Maintenance
Animal cell culture is a versatile tool indispensable in basic biomedical research, drug discovery, and biopharmaceutical production. For microbiologists transitioning into mammalian cell systems, understanding the core principles of maintaining cells in an artificial environment is critical. The growth and viability of mammalian cells in vitro depend heavily on three interconnected pillars: the selection of appropriate culture media, the rational use of serum, and the implementation of consistent maintenance protocols. Unlike microbial cultures, mammalian cells require more complex nutrient mixtures and are significantly more susceptible to environmental fluctuations and contamination.
This guide provides an in-depth technical framework for establishing robust mammalian cell culture practices, contextualized within modern trends toward defined, serum-free systems and supported by data-driven optimization methodologies.
Culture Media Selection and Optimization
Cell culture medium is a complex mixture of nutrients, growth factors, and buffers that provides the physical and chemical environment essential for cell survival and proliferation. Its composition must be carefully matched to the specific requirements of the cell type and application.
Types of Cell Culture Media
- Classical Media: Basal formulations like Dulbecco's Modified Eagle Medium (DMEM) and Roswell Park Memorial Institute (RPMI) medium contain carbohydrates, amino acids, vitamins, salts, and a pH buffer system [42]. These require supplementation with serum to provide growth factors and other undefined components.
- Serum-Free Media (SFM): Formulations that eliminate serum by incorporating specific growth factors, lipids, and hormones in a defined composition. SFM reduces batch-to-batch variability, lowers contamination risk, and simplifies downstream purification [105].
- Chemically Defined Media: A subtype of SFM where all components are known and their concentrations specified, providing maximum consistency and regulatory compliance [106].
- Animal-Origin-Free Media: Formulations entirely free of components derived from animals, mitigating the risk of prion, viral, and zoonotic contamination, which is crucial for therapeutic product manufacturing [106].
Key Media Components and Functions
Table 1: Essential Components of Cell Culture Media
| Component Category | Key Examples | Primary Function |
|---|---|---|
| Inorganic Salts & Buffers | NaCl, KCl, NaHCO₃, CaCl₂ | Maintain osmotic balance, regulate membrane potential, serve as enzyme cofactors |
| Amino Acids | L-Glutamine, L-Arginine, L-Isoleucine | Building blocks for protein synthesis; some act as energy sources |
| Vitamins | B-group vitamins | Serve as coenzymes for cellular metabolism and proliferation |
| Carbohydrates | Glucose | Primary energy source via glycolysis and oxidative phosphorylation |
| Serum Supplements | Insulin, Transferrin, Selenium | Stimulate growth, facilitate iron transport, provide antioxidant defense |
| Trace Elements | Iron, Zinc, Copper | Act as cofactors for metalloenzymes and electron transport chain proteins |
Modern Media Optimization Strategies
Traditional one-factor-at-a-time (OFAT) optimization approaches are inefficient for complex media due to the high dimensionality and component interactions. Modern strategies employ statistical and computational methods:
- Response Surface Methodology (RSM): A statistical technique used to model and optimize multiple medium components simultaneously. For instance, one study optimized insulin, transferrin, selenium, and glucose concentrations to maximize recombinant human GM-CSF production in CHO cells, determining ideal concentrations of 1.1 g/L, 0.545 g/L, 0.000724 g/L, and 1.4 g/L, respectively [105].
- Machine Learning (ML) and Active Learning: These advanced computational approaches build predictive models from experimental data to identify optimal medium compositions more efficiently than traditional methods. One study using gradient-boosting decision tree algorithms successfully fine-tuned 29 medium components for HeLa-S3 cell culture, significantly improving cellular NAD(P)H levels—an indicator of metabolic activity—while reducing fetal bovine serum requirements [107].
- Design of Experiments (DOE): Systematic approaches like Plackett-Burman designs enable efficient screening of multiple factors to identify critical components. This method was successfully applied to optimize iron, magnesium, calcium, zinc, and EDTA concentrations for HEK293 serum-free suspension culture development [108].
Figure 1: Workflow for Systematic Media Optimization. The process integrates statistical design with machine learning to efficiently identify optimal medium compositions.
Serum Applications and Transition Strategies
Fetal bovine serum (FBS) has been a standard medium supplement due to its rich mixture of growth factors, hormones, and attachment factors. However, its undefined nature, batch-to-batch variability, ethical concerns, and high cost have driven the development of serum-free alternatives.
Key Serum Components and Replacement Strategies
Table 2: Essential Serum Components and Their Defined Replacements
| Serum Component | Function in Culture | Serum-Free Replacement | Typical Concentration Range |
|---|---|---|---|
| Albumin | Lipid carrier, antioxidant, detoxifier | Recombinant albumin, rapeseed protein isolates | 1-5 g/L |
| Insulin | Growth promoter, metabolic regulator | Recombinant insulin | 0.5-2 g/L [105] |
| Transferrin | Iron transport | Recombinant transferrin, iron complexes | 0.5-1 g/L [105] |
| Selenium | Antioxidant defense | Sodium selenite | 0.0005-0.001 g/L [105] |
| Growth Factors | Cell proliferation & differentiation | Recombinant EGF, FGF, PDGF | Cell type-specific |
Systematic Adaptation to Serum-Free Conditions
Abrupt transition to serum-free media typically causes significant cellular stress. A graduated, stepwise adaptation protocol yields better outcomes:
- Initiate Adaptation: Begin by culturing cells in a 50:50 mixture of original serum-containing medium and target serum-free formulation [105] [108].
- Monitor Key Parameters: Assess viability, doubling time, and morphology at each passage. Only proceed when viability exceeds 90% and cells demonstrate stable growth [105].
- Gradually Increase SFM Ratio: Progress to 75:25 SFM-to-serum medium, then to 100% SFM over multiple passages [105].
- Address Cell-Specific Needs: Some cell lines may require additional matrix coatings or specific growth factor supplements during adaptation.
- Cryopreserve Adapted Cells: Once stable growth in SFM is established, cryopreserve multiple vials to create a master cell bank [6].
For suspension adaptation, gradually reduce serum concentration while simultaneously introducing suspension culture conditions. One successful protocol for HEK293 cells reduced FBS in steps from 10% to 2.5%, noting that some cells began growing in suspension at the 2.5% FBS stage with a doubling time of 59.31 hours before eventually recovering faster growth in full SFM [108].
Routine Culture Maintenance Protocols
Consistent maintenance practices are essential for preserving cell line authenticity, genetic stability, and experimental reproducibility.
Subculturing and Growth Phase Monitoring
Mammalian cells typically follow a characteristic growth pattern with four distinct phases:
- Lag Phase: Period of cellular recovery after subculturing with slow growth [6].
- Log (Exponential) Phase: Period of rapid, exponential growth where cells should be maintained for optimal health and consistency [6].
- Stationary Phase: Growth plateaus as nutrients diminish and waste products accumulate [6].
- Decline Phase: Cell viability decreases due to nutrient depletion and toxic metabolite accumulation [6].
To maintain genetic and phenotypic stability, subculture cells during the mid-exponential phase, before reaching 100% confluency (for adherent cells) or maximum recommended density (for suspension cultures) [6]. The American Type Culture Collection (ATCC) recommends limiting passages to no more than five from the original reference stock to minimize genetic drift [109].
Cryopreservation and Cell Banking
Proper cryopreservation creates a secure inventory of low-passage cells:
- Cryoprotectant Solution: Use culture medium supplemented with 10% DMSO and 10-20% serum or serum replacements [6].
- Controlled Freezing: Implement a gradual cooling rate of approximately -1°C per minute using isopropanol chambers or controlled-rate freezers [6].
- Storage Conditions: Maintain frozen cells below -130°C, preferably in liquid nitrogen vapor phase, for long-term stability [6].
- Quality Control: Document passage number, viability, and storage location for all cryopreserved vials.
Contamination Control and Aseptic Technique
Maintaining sterile conditions is paramount, as mammalian cells lack the defensive capabilities of microorganisms:
- Biosafety Cabinet Usage: Perform all open-container manipulations within a certified Class II biosafety cabinet with proper UV decontamination and airflow [110].
- Antibiotic Use: Limit routine antibiotic use to facilitate detection of contamination; reserve for primary cultures or when absolutely necessary [42].
- Routine Monitoring: Regularly check cultures for microscopic signs of contamination (mycoplasma, bacteria, fungi) and morphological changes indicative of stress or differentiation [6].
- Authentication: Periodically verify cell line identity through STR profiling to guard against misidentification and cross-contamination, particularly problematic with an estimated 16.1% of published papers using problematic cell lines [42].
Figure 2: Essential Components of Routine Culture Maintenance. Regular monitoring of key parameters preserves cell line integrity over time.
Essential Research Reagents and Materials
Table 3: Key Reagents for Mammalian Cell Culture
| Reagent/Category | Specific Examples | Function & Application |
|---|---|---|
| Basal Media | DMEM, RPMI-1640, EMEM | Provide fundamental nutritional support for cell growth and maintenance |
| Serum & Alternatives | Fetal Bovine Serum (FBS), KnockOut Serum Replacement | Supply growth factors, hormones, and carriers in classical or transitioning cultures |
| Dissociation Agents | Trypsin-EDTA, Accutase, Accumax | Detach adherent cells for subculturing while preserving viability and surface markers |
| Cryoprotectants | DMSO, Glycerol | Protect cells from ice crystal formation damage during freezing and thawing processes |
| Growth Factors & Supplements | Recombinant Insulin, Transferrin, Selenium Solutions | Replace specific serum functions in defined media formulations |
| Detection Assays | CCK-8, Trypan Blue Exclusion | Assess cell viability, proliferation rates, and metabolic activity |
The field of animal cell culture is progressively moving toward fully defined, serum-free systems that enhance reproducibility, safety, and regulatory compliance. Successful implementation requires understanding cellular requirements, systematically optimizing culture components using statistical and computational approaches, and maintaining scrupulous aseptic technique. By applying the best practices outlined in this guide—rational media selection, controlled serum transition, and consistent maintenance protocols—researchers can establish robust, reliable mammalian cell culture systems that support reproducible scientific discovery and biopharmaceutical development.
Ensuring Reproducibility with Quality Control and Model Validation
Cell lines are indispensable tools in biomedical research and drug discovery, serving as in vitro models that substitute for tissues or organs of origin [111] [112]. However, these critical biological reagents harbor a pervasive and often invisible problem: misidentification and cross-contamination. Frequent misidentification poses major quality control challenges, leading to unreliable data, hindering scientific progress, and impacting clinical translation [111] [113]. Even properly authenticated cell lines may undergo genetic and phenotypic changes over time, further compromising experimental outcomes [111] [112].
The scale of this problem is staggering. The International Cell Line Authentication Committee (ICLAC) registry currently lists nearly 600 misidentified or contaminated cell lines [113]. A conservative estimate suggests that 32,755 articles report research with misidentified cells, which in turn have been cited by approximately half a million other papers, creating a ripple effect of wasted resources and misleading conclusions [114]. This contamination of the scientific literature does not appear to be decreasing over time and is not restricted to countries in the periphery of global science [114].
Table 1: Commonly Misidentified Cell Lines in Research (Selected Examples)
| Cell Line | Claimed Identity | Actual Identity | Contaminating Cell Line |
|---|---|---|---|
| L-02 | Human liver, normal hepatic cells | Human cervical adenocarcinoma | HeLa [113] |
| BEL-7402 | Human liver, hepatocellular carcinoma | Human cervical adenocarcinoma/colon carcinoma | HeLa/HCT 8 [113] |
| QGY-7703 | Human liver, hepatocellular carcinoma | Human cervical adenocarcinoma | HeLa [113] |
| WRL 68 | Human embryonic liver cells | Human cervical adenocarcinoma | HeLa [113] |
| BGC-823 | Human gastric carcinoma | Human cervical adenocarcinoma | HeLa [113] |
| Chang Liver | Human liver, normal hepatic cells | Human cervical adenocarcinoma | HeLa [113] |
For microbiologists transitioning to mammalian cell culture systems, understanding and implementing cell line authentication is particularly crucial. The challenges of contamination control in cell culture parallel those in microbiology, but with the added complexity that cellular cross-contamination is not visually detectable through routine microscopy and can persist undetected through numerous passages.
The Scope and Consequences of Cell Line Misidentification
Origins and Mechanisms of Misidentification
Cell line misidentification typically occurs through several mechanisms:
- Cross-contamination during routine culture: The most common source, where rapidly growing cell lines (notably HeLa) overwhelm other cultures in the same laboratory space [113] [114].
- Mislabeling and technical errors: Simple mistakes in labeling or handling multiple cell lines simultaneously.
- Inadequate authentication protocols: Failure to verify cell line identity upon receipt, during banking, and at regular intervals during research.
- Genetic drift: Even authenticated cell lines may undergo phenotypic and genotypic changes when maintained in culture for extended periods through excessive subculturing [115] [112].
The problem is perpetuated when misidentified cells are shared between laboratories, distributed through informal channels, or even obtained from repositories that lack comprehensive authentication protocols. Once introduced into a laboratory, misidentified cell lines can compromise years of research and development efforts.
Impact on Research Reproducibility and Drug Development
The consequences of using misidentified cell lines are far-reaching and severe:
- Irreproducible results: Experiments produce unreliable data that cannot be replicated, undermining the scientific foundation for further research [111] [113].
- Wasted resources: One analysis suggests that the use of misidentified cell lines wastes an estimated $3.5 billion annually in the United States alone in research funding [113].
- Compromised drug discovery: Preclinical studies using misidentified cells may yield misleading results about compound efficacy and toxicity, potentially directing clinical development down unproductive pathways [116].
- Literature contamination: The persistent circulation of papers reporting on wrong cells without warning or correction creates a foundation of questionable knowledge that subsequent research builds upon [114].
The problem extends beyond scientific circles to affect public trust in research and the efficient allocation of research funding. In the context of drug development, the use of misidentified cell lines can delay the availability of new therapies and increase development costs.
Core Authentication Methods and Technologies
Short Tandem Repeat (STR) Profiling: The Gold Standard
Short tandem repeat (STR) profiling stands as the internationally recognized gold standard for human cell line authentication [117] [112]. This technique examines highly polymorphic regions of the genome containing short, repetitive DNA sequences (typically 2-6 base pairs in length) that vary in the number of repeats between individuals [116].
The process involves:
- DNA extraction from the cell line in question
- Multiplex PCR amplification of multiple STR loci simultaneously
- Capillary electrophoresis to separate amplified fragments by size
- Analysis of fragment sizes to determine the number of repeats at each locus
- Comparison with reference databases to verify identity
STR profiling generates a unique genetic fingerprint for each cell line with extremely high discrimination power. The probability of two unrelated individuals sharing identical STR profiles across multiple loci can be as low as 1 in 1 × 10¹⁸ [116].
Table 2: Comparison of Cell Line Authentication Methods
| Method | Principle | Applications | Strengths | Limitations |
|---|---|---|---|---|
| STR Profiling | Analysis of polymorphic short tandem repeat loci | Human cell line authentication; gold standard | High discrimination power; standardized; cost-effective | Primarily for human cells; requires reference data |
| Isoenzyme Analysis | Electrophoretic separation of species-specific enzyme variants | Species verification | Detects interspecies contamination; relatively simple | Limited discrimination within species |
| Karyotyping | Chromosomal analysis of number and structure | Genomic stability assessment | Identifies major chromosomal abnormalities | Low resolution; labor-intensive |
| Mycoplasma Testing | PCR, DNA staining, or culture-based detection | Microbial contamination screening | Critical for culture health; multiple format options | Does not address cell line identity |
| Optical Genome Mapping (OGM-ID) | Analysis of genome-wide insertions/deletions using long DNA molecules | Simultaneous authentication and karyotype assessment | Detects intraspecies and interspecies contamination; provides karyotype information | Emerging technology; complex data analysis |
International standards, such as the ANSI/ATCC ASN-0002-2022 guidelines, recommend profiling a core set of STR loci plus a sex-determining marker [117]. However, many service providers now offer expanded panels analyzing 21-24 loci to provide superior discrimination and lower the probability of identity [117].
Emerging and Complementary Technologies
While STR profiling remains the cornerstone of cell line authentication, several complementary and emerging technologies offer additional capabilities:
Optical Genome Mapping (OGM-ID): This novel approach utilizes the same data collected for karyotype assessment to authenticate cell lines based on genome-wide large (>500 bp) insertions and deletions. OGM-ID can determine both interspecies and intraspecies contamination while simultaneously providing karyotypic information, making it particularly valuable for cell therapy development [118].
Morphology checks: Regular microscopic examination of cellular morphology provides the simplest and most direct method for monitoring cell state. While not definitive for authentication, morphological changes can signal potential problems with culture health or identity [115].
Growth curve analysis: Establishing baseline proliferation characteristics helps monitor culture consistency and can reveal deviations suggestive of contamination or genetic drift [115].
Mycoplasma detection: While not an identity verification method, routine screening for mycoplasma and other adventitious agents is essential for maintaining culture health and preventing confounding experimental results [111] [115]. Multiple detection methods are available, including PCR, DNA staining with fluorochromes like Hoechst 33258, and microbiological culture [115] [116].
Authentication Workflow: A decision pathway for implementing cell line authentication in research settings.
Implementing Authentication in Research Practice
Strategic Timing for Authentication
Effective cell line quality control requires authentication at multiple critical points throughout the research lifecycle:
- Upon acquisition of a new cell line: Authentication should occur before the cell line is introduced into ongoing research programs [117] [116].
- When creating new cell lines: Establish baseline authentication data for novel cell lines before distribution or publication [117].
- Before freezing down working stocks: Verify identity before creating cell banks to ensure the preservation of authentic material [117] [116].
- At regular intervals during culture: Authentication every 10 passages helps monitor genetic stability and detect potential cross-contamination [117].
- Before key experiments: Particularly for long-term studies, verify identity immediately prior to critical experiments [116].
- When observing inconsistent results: Unexplained variations in experimental outcomes may indicate identity issues [117].
- Prior to manuscript submission: Most journals now require authentication certificates for publication [111] [117].
- When submitting grant applications: Funding agencies increasingly require authentication data as part of application packages [117].
Maintaining detailed records of authentication results, including STR profiles, dates of testing, and passage numbers, is essential for demonstrating research integrity and supporting publication claims.
Comprehensive Quality Control Program
Beyond identity verification, a robust cell culture quality control program includes several complementary components:
- Mycoplasma testing: Conducted regularly (e.g., every few weeks) using validated methods, as mycoplasma contamination can significantly alter cell behavior and metabolism without visible signs under routine microscopy [115] [116].
- Passage number monitoring: Recording and controlling passage numbers helps prevent phenotypic and genotypic changes associated with excessive subculturing [115].
- Morphological documentation: Regular photographic records of cell morphology at various densities provide valuable baseline data for detecting changes over time [115].
- Culture practice standardization: Using consistent media formulations, serum lots, and culture conditions minimizes unnecessary phenotypic variation [116].
Table 3: The Researcher's Authentication Toolkit
| Tool/Resource | Category | Primary Function | Key Features |
|---|---|---|---|
| STR Profiling Services | Service Provider | Human cell line authentication | CLIA-certified labs; ISO standards; 21+ marker panels |
| ICLAC Register | Database | List of known misidentified lines | 593+ misidentified lines; searchable database |
| Cellosaurus | Database | Cell line knowledge resource | RRID integration; extensive cross-references |
| Mycoplasma Detection Kits | Reagent | Microbial contamination screening | PCR, enzymatic, or staining-based formats |
| ATCC Guidelines | Reference | Authentication standards | STR methodology; quality control protocols |
| PowerPlex 18D System | Reagent | STR multiplex PCR | 17 STR loci + amelogenin; optimized chemistry |
Journal Policies and Authentication Standards
Evolving Publication Requirements
In response to the recognized prevalence of cell line misidentification, major scientific publishers and journals have implemented increasingly stringent authentication requirements:
- American Association for Cancer Research (AACR) publishers: Require cell line authentication for all cell lines used in submitted studies [117].
- Nature Publishing Group: Strongly recommends authentication and encourages authors to submit certificates of authentication with submissions [117].
- Journal of Cell Communication and Signaling (JCCS): Requires comprehensive cell line details including species, sex, tissue origin, name, Research Resource Identifier (RRID), source, acquisition date, and authentication methods [111] [112].
- International Journal of Cancer: Reports rejecting approximately 4% of considered manuscripts due to severe cell line issues [117].
These policies generally align with guidelines from funding agencies such as the National Institutes of Health (NIH), which requires authentication of cell lines in grant applications [117] [112].
Documentation and Reporting Standards
When submitting manuscripts for publication, researchers should be prepared to provide:
- Official cell line name and Research Resource Identifier (RRID)
- Species, sex, and tissue of origin
- Source or supplier and date of acquisition
- Authentication method used (e.g., STR profiling) and date performed
- Mycoplasma testing method and results
- Passage number range used in experiments
The RRID system has been particularly valuable for consistently tracking reagents throughout the scientific literature, helping to prevent inadvertent use of misidentified lines and improving reproducibility [112].
Problem to Solution: The scientific community's evolving response to cell line misidentification.
Cell line authentication represents a critical foundation for reproducible biomedical research. While the problems of misidentification and cross-contamination are long-standing and pervasive, the research community has developed effective tools and standards to address these challenges. STR profiling provides a robust, standardized method for identity verification, while emerging technologies like optical genome mapping offer complementary capabilities.
For microbiologists and other researchers working with animal cell cultures, implementing regular authentication checkpoints throughout the research lifecycle is no longer optional—it is an essential component of responsible science. By normalizing these practices and adhering to journal and funding agency requirements, the research community can reduce the circulation of erroneous findings, enhance reproducibility, and accelerate the translation of basic research into clinical advances for human health [111].
The future of biological research demands rigorous quality control, with cell line authentication serving as a cornerstone of research integrity. As authentication technologies continue to evolve and awareness grows, researchers have an unprecedented opportunity to rebuild trust in cell-based research and ensure that limited research resources are invested in generating reliable, reproducible data.
In the field of animal cell culture, maintaining the integrity and authenticity of cellular substrates is paramount for ensuring the reliability of research data, the safety of manufactured biologics, and the success of drug development projects. Quality control (QC) monitoring is critical for the reproducibility of data in translational science research [119]. Among the myriad of potential pitfalls, three core QC checks form the first line of defense: mycoplasma testing, karyotyping, and isoenzyme analysis. These methods collectively address the major risks of microbial contamination, genetic instability, and interspecies cross-contamination that can compromise cell cultures. For microbiologists and researchers engaged in cell-based research and product development, implementing a rigorous, routine schedule of these tests is not optional but fundamental to scientific integrity. This guide provides an in-depth technical examination of these essential QC checks, providing methodologies, data interpretation, and integration strategies tailored for professionals in research and drug development.
Mycoplasma Testing
The Stealth Contaminant in Cell Cultures
Mycoplasma species are among the smallest self-replicating bacteria, lacking a rigid cell wall. This structural simplicity enables them to pass through standard sterilizing filters (0.2 µm) that would typically prevent bacterial contamination [120] [121]. Their size and plasticity also mean they often evade visual detection under routine microscopic examination, as contamination does not cause the turbidity typically associated with bacterial infections [121]. Over 190 species of mycoplasmas have been identified, with approximately 20 species—originating from humans, cattle, and pigs—found contaminating laboratory cell cultures [121].
The consequences of undetected mycoplasma contamination are profound. These organisms can silently alter cellular parameters, including: suppressing cell growth and altering metabolism; skewing gene expression and protein production; compromising experimental reproducibility and regulatory compliance; and leading to substantial financial losses in biotech workflows due to invalidated experiments or production runs [120]. Contamination typically occurs through cross-contamination from infected, untested cell cultures, often via microscopic airborne droplets generated during pipetting or media transfers [121]. The risk is heightened when multiple cell lines are handled in the same biosafety cabinet or share the same bottle of medium [121].
Detection Methodologies
Several testing methods are available, each with distinct advantages and limitations. The most reliable laboratories often implement a combination of these tests to ensure accuracy [120].
PCR-Based Detection: This molecular method is fast and highly sensitive, making it ideal for screening multiple cell lines. Modern real-time PCR assays can detect less than 10 colony forming units (CFU) of Mycoplasma, dramatically reducing turnaround times to under 24 hours compared with traditional 28-day culture protocols [122]. PCR is particularly valuable in settings where rapid results are critical, such as in clinical cell therapy products where expeditious screening is essential for both regulatory compliance and patient safety [122].
Culture-Based Assays: This traditional approach allows viable mycoplasma to grow in specialized media, providing definitive confirmation of contamination. While considered the gold standard for its ability to detect a broad range of viable mycoplasma species, culture-based techniques are time-consuming (requiring up to 28 days) and labor-intensive [122]. They remain essential for regulatory submissions and definitive confirmation.
DNA Staining: This technique uses fluorochrome dyes to identify characteristic mycoplasma DNA in contaminated cells. While less sensitive than PCR or culture methods, it provides a cost-effective screening option that can be implemented in most laboratory settings [120].
Table 1: Comparison of Major Mycoplasma Detection Methods
| Method | Principle | Time Required | Sensitivity | Key Advantage |
|---|---|---|---|---|
| PCR-Based | Amplification of mycoplasma-specific DNA sequences | <24 hours | High (<10 CFU) [122] | Speed and sensitivity |
| Culture-Based | Growth in specialized media | Up to 28 days [122] | High (detects viable organisms) | Gold standard, definitive |
| DNA Staining | Fluorochrome staining of mycoplasma DNA | 1-2 days | Moderate | Cost-effective, simple |
Experimental Protocol: PCR-Based Mycoplasma Detection
Sample Preparation: Collect supernatant from test cell cultures after 48-72 hours of growth without antibiotics. Centrifuge at 300 × g for 10 minutes to remove cellular debris. Use the resulting supernatant for DNA extraction.
DNA Extraction: Extract nucleic acids from 200 µL of supernatant using a commercial DNA extraction kit according to manufacturer's instructions. Include both positive (known mycoplasma DNA) and negative (sterile water) extraction controls.
PCR Amplification: Prepare reaction mixtures containing:
- 10 µL of PCR master mix
- 2 µL of mycoplasma-specific primers (targeting 16S rRNA genes)
- 3 µL of template DNA
- 5 µL of nuclease-free water
Thermal Cycling Conditions:
- Initial denaturation: 95°C for 5 minutes
- 35 cycles of: 95°C for 30 seconds, 55°C for 30 seconds, 72°C for 45 seconds
- Final extension: 72°C for 7 minutes
Analysis: Separate PCR products by agarose gel electrophoresis (1.5%) and visualize under UV light. The presence of specific amplification bands (approximately 500 bp) indicates mycoplasma contamination.
Karyotyping
Monitoring Genomic Integrity
Karyotype analysis is the study of metaphase chromosomes to assess genomic integrity. It involves analyzing, comparing, classifying, and numbering chromosomes according to their length, the location of centromeres, arm ratio, and banding patterns [123]. This technique provides critical information about chromosome number and structural variations, offering an important basis for cytogenetic classification and identifying genetic abnormalities that may arise during cell culture.
The importance of karyotyping is particularly evident when working with human pluripotent stem cells (hPSCs) for regenerative medicine, disease modeling, and drug screening. Although hPSCs are mostly diploid when first derived, they can acquire different types of genetic alterations during prolonged culture passages [124]. These include recurrent genomic abnormalities such as chromosome 1 or 1q amplification, trisomy 12 or 12p amplification, trisomy X (in female cell lines), trisomy 17 or 17q amplification, and 20q11.21 amplification [124]. Many of these recurrent mutations provide selective growth advantages in culture and can alter hPSC functional characteristics, including decreased differentiation potential, increased self-renewal capacity, and a shift towards malignant properties [124].
Detection Capabilities and Methodologies
Karyotyping is currently considered the most sensitive method for identification of intraspecies contamination, with an experienced cytogeneticist potentially detecting contamination levels as low as 1% [125]. The method's versatility extends beyond simple authentication to comprehensive characterization of a cell line's genomic status [125].
The standard G-banding technique provides a detailed chromosomal map that allows identification of individual chromosomes and detection of structural abnormalities. High-resolution banding techniques can accurately identify chromosomes and determine whether the karyotype is normal [123]. More advanced techniques like array-based Comparative Genomic Hybridization (aCGH) can detect subtle subchromosomal aberrations that may be missed by standard G-banding [124].
Table 2: Chromosomal Abnormalities Commonly Detected in Cell Cultures
| Abnormality Type | Examples | Functional Impact | Detection Method |
|---|---|---|---|
| Whole chromosome aneuploidy | Trisomy 12, Trisomy X | Altered differentiation propensity, increased self-renewal | G-banding karyotype [124] |
| Subchromosomal amplification | 20q11.21 amplification, 1q amplification | Selective growth advantage, potential malignant shift | aCGH, high-resolution banding [124] |
| Subchromosomal deletions | 18q loss, 10p loss | Altered gene expression profiles | aCGH [124] |
Experimental Protocol: Karyotype Analysis with G-Banding
Cell Preparation and Colchicine Treatment:
- Culture cells until they are growing vigorously at approximately 70-80% confluence.
- Add colchicine to the medium to a final concentration of 0.2 μg/mL 2.5 hours before harvesting [123].
- Digest and collect cells by routine trypsinization into 15 mL centrifuge tubes.
Hypotonic Treatment:
- Centrifuge cells, remove supernatant, and retain cell precipitate.
- Add 8 mL of pre-warmed (37°C) 0.075 mol/L KCl hypotonic solution and mix thoroughly by pipetting.
- Incubate in a 37°C water bath for 15 minutes [123].
- Centrifuge and remove supernatant, leaving approximately 0.5 mL of residual fluid to avoid cell loss.
Fixation:
- Resuspend swollen cell sediment by gentle shaking.
- Perform pre-fixation by adding freshly prepared fixative (methanol:acetic acid, 3:1) dropwise along the tube wall, followed by gentle shaking and fixation for 5 minutes.
- Centrifuge for 10 minutes, discard supernatant.
- Perform first fixation with 5 mL fixative, gently pipetting several times, then cover and leave at room temperature for 30 minutes.
- Repeat centrifugation and perform second fixation following the same procedure [123].
Slide Preparation and Staining:
- Use alcohol-cleaned slides with frosted front side.
- Aspirate 100 μL of cell suspension and drop onto slide from a height of 30-40 cm.
- Quickly pass the slide several times through an alcohol lamp flame for over-fixing.
- For G-banding, treat slides with 2.5% trypsin solution (adjusted to pH 6.8-7.2) for 20-25 seconds at 37°C with continuous gentle shaking.
- Rinse in pre-warmed saline and stain in Giemsa staining solution at 37°C for 10 minutes [123].
- Rinse with pure water and dry with cold airflow.
Analysis:
- Locate metaphase spreads under low magnification (100×).
- Select intact, independent metaphases with good chromosome dispersion and clear banding patterns.
- Switch to high magnification and oil immersion for detailed analysis.
- Count chromosome numbers and record karyotype abnormalities according to International System for Human Cytogenetic Nomenclature (ISCN) guidelines.
Isoenzyme Analysis
Authenticating Species Origin
Isoenzyme analysis serves as a traditional method for cell line authentication, specifically for determining species of origin and detecting interspecies cross-contamination. The technique takes advantage of the different banding patterns and relative migration distances for individual isoforms of intracellular enzymes with similar substrate specificity but different molecular structures [125]. These differences arise from species-specific variations in enzyme structure and can be visualized through electrophoretic separation.
The method is technically simple, robust, and rapid, requiring only a few hours for an investigator to confirm a cell line's purity and species of origin [126]. This makes it particularly valuable for quality control in settings where multiple cell lines are manipulated in the same facility, introducing the possibility of cross-contamination [126]. Different cell lines may proliferate with varying growth rates such that a single cell from a rapidly growing line can overtake a culture of slower growing cells in just a few passages [126].
Detection Capabilities and Methodologies
Isoenzyme analysis can detect interspecies contamination when the contaminating cells represent at least 10% of the total cell population [125]. Some studies have demonstrated detection when contaminating cells represent about 10% of the total population [126], though others found that mixtures containing only 1% of contaminating cells could not routinely be detected using this method [125].
The technique typically evaluates several intracellular enzymes, including: nucleoside phosphorylase (NP), malate dehydrogenase (MD), glucose-6-phosphate dehydrogenase (G6PD), lactate dehydrogenase (LD), peptidase B (PepB), aspartate amino transferase (AST), and mannose 6-phosphate isomerase (MPI) [126]. The specific enzymes selected for evaluation depend on the animal species of origin of the cell line being characterized and the potential species representing the greatest risk of contamination [126].
Table 3: Key Enzymes for Detecting Specific Cross-Contaminations
| Enzyme | Optimal for Detecting | Notes on Resolution |
|---|---|---|
| PepB | Chinese hamster vs. mouse | Definitive differentiation between these species [126] |
| AST | Human vs. cercopithecus monkey | Especially useful for this combination [126] |
| LD | Multiple species | May display single or multiple bands depending on cell line |
| MD | Human vs. cercopithecus monkey | Shows doublet mitochondrial band in mixed cultures [126] |
Experimental Protocol: Isoenzyme Analysis via Electrophoresis
Cell Extract Preparation:
- Harvest cells in mid-log phase growth.
- Wash cell pellet with phosphate-buffered saline.
- Lysc cells using freeze-thaw cycling or detergent-based extraction.
- Clarify extract by centrifugation at 10,000 × g for 10 minutes.
- Retain supernatant for analysis.
Gel Electrophoresis:
- Prepare agarose gels according to commercial kit specifications (e.g., AuthentiKit system).
- Load 5-10 µL of sample extracts into gel wells.
- Include system suitability controls: murine L929 cell extract as standard and human HeLa extract as control [126].
- Run electrophoresis at constant voltage (100-150 V) for approximately 45-60 minutes until adequate separation is achieved.
Enzyme-Specific Staining:
- Prepare specific substrate solutions for each enzyme (NP, MD, G6PD, LD, PepB, AST, MPI).
- Incubate gels in substrate solutions at 37°C with monitoring of color development.
- Stop reaction when bands achieve sufficient intensity but before excessive background develops.
Analysis:
- Measure migration distances of sample bands from origin.
- Calculate correction factor based on observed and expected migration distances for standard reagent.
- Multiply test sample migration distances by correction factor for day-to-day standardization.
- Compare corrected migration distances with standardized charts for species assignment.
The Integrated Quality Control Strategy
Implementing a Comprehensive QC Framework
While each QC method addresses specific risks, their true power emerges when integrated into a systematic quality management approach. Implementation of a Quality Management System (QMS) such as ISO9001:2015 to ensure reproducible and standardized cell culture conditions and genomic screening strategies can significantly decrease the prevalence of genomic alterations affecting hPSCs used for research applications [124]. A retrospective analysis of cytogenetic data over a 5-year span demonstrated that adaptation of hPSC lines to standardized cell culture conditions under a QMS leads to a striking improvement of genomic stability in vitro, as evidenced by a reduced probability of potentially pathogenic chromosomal aberrations and subchromosomal genomic alterations [124].
The development and use of Standard Operating Procedures (SOPs) for cell culture protocols and procedures for genome integrity assessment are an integral part of a successful QMS [124]. These written instructions provide individuals with the information to perform jobs properly in the most detailed possible fashion, thus minimizing variation and promoting quality through consistent implementation of all processes within the organization [124].
Workflow Integration and Testing Frequency
For optimal protection of cell line integrity, these QC methods should be implemented at specific points in the cell culture lifecycle:
- Upon receipt of new cell lines: Perform full authentication (isoenzyme analysis or STR profiling) and mycoplasma testing before introducing into main culture facility.
- At cell banking: Conduct comprehensive testing including karyotyping on master and working cell banks.
- During routine culture: Implement periodic mycoplasma testing (e.g., monthly) and morphological assessment.
- Before critical experiments: Verify absence of mycoplasma and confirm cell line authenticity.
- At end-of-production: Test cells used for product manufacturing to ensure quality until completion.
Data collected over three years since implementation of systematic testing demonstrates the importance of continual vigilance for rapid identification of "problem" cell lines to ensure reproducible data in translational science research [119]. Initial testing at one collaborative research institute identified a >10% mycoplasma contamination rate, underscoring the persistent nature of this challenge despite modern laboratory practices [119].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for Cell Culture Quality Control
| Reagent / Kit | Primary Function | Application Notes |
|---|---|---|
| PCR Mycoplasma Detection Kit | Amplification of mycoplasma-specific DNA sequences | Provides primers for 16S rRNA targets; includes positive and negative controls [122] |
| AuthentiKit System | Speciation via isoenzyme electrophoresis | Contains reagents for NP, MD, G6PD, LD, PepB, AST, MPI enzymes [126] |
| Colchicine Solution | Arrests cells in metaphase | Used at 0.2 μg/mL for 2.5 hours before karyotype harvesting [123] |
| Hypotonic Solution (0.075M KCl) | Swells cells for chromosome spreading | Must be pre-warmed to 37°C; 15-minute incubation [123] |
| Methanol:Acetic Acid Fixative | Preserves chromosome morphology | Freshly prepared in 3:1 ratio; used for multiple fixation steps [123] |
| Giemsa Staining Solution | Creates G-banding pattern on chromosomes | Requires trypsin pre-treatment for banding patterns [123] |
| Agarose Gels | Matrix for electrophoretic separation | Used in isoenzyme analysis for species identification [126] |
Workflow Diagrams
Integrated Quality Control Workflow
Mycoplasma Detection Decision Pathway
Routine quality control checks comprising mycoplasma testing, karyotyping, and isoenzyme analysis form the essential triad for maintaining cell culture integrity in research and drug development settings. Each method addresses distinct but complementary aspects of quality control: mycoplasma testing safeguards against microbial contamination, karyotyping monitors genetic stability, and isoenzyme analysis authenticates species origin. Implementation of these methods within a structured Quality Management System with defined Standard Operating Procedures significantly enhances detection and prevention of culture abnormalities. For microbiologists and cell culture researchers, adherence to this comprehensive QC framework is not merely good laboratory practice but a fundamental requirement for generating reliable, reproducible scientific data and ensuring the safety of biologically-derived products.
Growth curve analysis provides critical insights into cellular health and proliferation kinetics, serving as a cornerstone technique in animal cell culture. This technical guide details the methodologies for constructing accurate growth curves, calculating population doubling time (PDT), and determining optimal seeding densities—fundamental parameters for ensuring experimental reproducibility and valid research outcomes. Framed within the broader context of animal cell culture basics for microbiologists, this whitepaper synthesizes established protocols with advanced computational approaches to equip researchers and drug development professionals with the tools necessary for robust cell culture management. The precise determination of these metrics is paramount for applications ranging from basic biological research to biomanufacturing and therapeutic development, where consistent cell behavior directly impacts product quality and data integrity.
In vitro cell culture is a fundamental tool in life sciences and biotechnology, used to study disease mechanisms, produce recombinant proteins, and develop cell-based therapies [64]. Unlike microbial systems, animal cells exhibit complex growth kinetics influenced by a myriad of factors including nutrient availability, cell density, and environmental conditions. Quantitative analysis of these kinetics through growth curves provides researchers with a dynamic view of population dynamics, enabling informed decisions about culture management and experimental timing.
The population doubling time (PDT) represents the time required for a cell population to double in number during the exponential growth phase and serves as a key indicator of metabolic activity and culture health [127]. Closely related is the concept of optimal seeding density—the number of cells initially plated per unit area that promotes efficient attachment, minimizes lag phase duration, and supports robust exponential growth without prematurely inducing contact inhibition or nutrient depletion [128] [129]. Together, these parameters form the foundation of reproducible cell culture practices, allowing researchers to standardize processes across experiments and laboratories, a critical consideration for drug development professionals requiring stringent quality control.
Theoretical Framework: The Cell Growth Curve
Phases of the Growth Curve
Animal cell populations typically progress through four distinct phases of growth, each characterized by specific physiological states [128] [6]:
Lag Phase: Immediately following subculturing, cells adapt to their new environment, recovering from passaging stress and synthesizing proteins and metabolites necessary for division. While little cell division occurs, this period is metabolically active as cells prepare for proliferation. The duration of this phase is influenced by factors such as cell type, seeding density, and the handling methods used during subculturing [128].
Log (Exponential) Phase: With environmental conditions optimized, cells divide at a constant, maximal rate, resulting in exponential population growth. The growth rate and PDT remain constant during this period, making it the most critical phase for calculating doubling times and studying cell physiology. Cells are typically at their most uniform and healthy state during log phase, making this the optimal window for most experimental interventions, including drug treatments and transfections [128] [127].
Stationary Phase: As nutrients become depleted and metabolic wastes accumulate, the rate of cell division slows until it balances with the rate of cell death. The viable cell count stabilizes, and metabolism shifts as cells enter a state of reduced proliferation. For adherent cells, contact inhibition often contributes to this growth arrest when confluency is reached [128] [6].
Death Phase: The population experiences a net decline as cell death exceeds division, typically due to severe nutrient depletion and toxic metabolite accumulation. Apoptosis and necrosis become predominant, and viability decreases steadily until the culture is lost if not replenished with fresh medium or passaged [128].
Table 1: Characteristics of Growth Curve Phases
| Phase | Cell Activity | Key Processes | Duration | Recommendations |
|---|---|---|---|---|
| Lag Phase | Adaptation to new environment | Gene regulation, enzyme synthesis, recovery from passaging | 24-48 hours | Ideal for genetic manipulation; avoid experimental treatments |
| Log Phase | Exponential division | Constant doubling time, active metabolism, high viability | Varies by cell line | Optimal time for subculturing, assays, and drug treatments |
| Stationary Phase | Balanced division and death | Nutrient depletion, waste accumulation, contact inhibition | Several days | Harvest products; passage immediately to maintain health |
| Death Phase | Net population decline | Apoptosis, necrosis, significantly reduced viability | Variable | Avoid this phase; culture health is severely compromised |
Key Kinetic Parameters
Population Doubling Time (PDT) is mathematically defined as the time required for the cell population to double during the exponential growth phase. It is calculated using the formula [128] [127] [130]: [ Td = \frac{(t2 - t1) \times \ln(2)}{\ln(N2 / N_1)} ] Where:
- ( T_d ) = Doubling time
- ( t2 - t1 ) = Time interval between measurements
- ( N_1 ) = Initial cell number
- ( N_2 ) = Final cell number
- ( \ln(2) ≈ 0.693 )
Population Doubling Level (PDL) represents the cumulative number of times the cell population has doubled since its isolation, providing a more accurate measure of cellular "age" than passage number alone, as it accounts for actual replication events rather than just subculture events [127]. The PDL is calculated for each passage using: [ \text{PDL} = 3.32 \times \log{10}(N2 / N_1) ] The cumulative PDL is the sum of PDLs across all passages.
Growth Rate (μ), the fractional increase in cell number per unit time, is reciprocally related to doubling time [128]: [ \mu = \frac{\ln(2)}{T_d} ]
Experimental Methodology
Workflow for Growth Curve Analysis
The following diagram illustrates the comprehensive workflow for conducting growth curve analysis, from experimental setup through data interpretation:
Determining Optimal Seeding Density
Seeding density significantly impacts growth kinetics and experimental outcomes. Too low density can delay entry into log phase or prevent growth altogether due to insufficient cell-to-cell signaling, while excessive density may shorten the exponential phase and accelerate nutrient depletion [128] [129].
Experimental Approach:
- Preliminary Range-Finding: Plate cells at varying densities spanning two orders of magnitude (e.g., 1,000, 5,000, 10,000, 50,000 cells/cm²) based on literature values for your cell type.
- Systematic Testing: For heterogeneous cultures like mesenchymal stem cells (MSCs), test densities of 20, 200, and 2000 cells/cm² to identify optimal proliferation conditions [129].
- Growth Monitoring: Track cell counts daily for each density condition until all cultures reach stationary phase.
- Analysis: Identify the density that produces the shortest lag phase, robust exponential growth, and appropriate time to confluency.
Research indicates that optimal growth often occurs at intermediate seeding densities. For instance, in rat bone marrow stromal cells, a plating density of 200 cells/cm² yielded superior growth compared to both sparser (20 cells/cm²) and denser (2000 cells/cm²) conditions [129]. The optimal density minimizes the lag phase duration while allowing sufficient expansion before reaching confluency.
Data Collection for Growth Curves
Sampling Protocol:
- Interval: Sample every 12-24 hours for most mammalian cells; more frequently (e.g., every 6-8 hours) for fast-growing lines [128].
- Consistency: Maintain consistent sampling times and conditions across replicates.
- Duration: Continue until clear stationary phase is observed, typically 7-10 days.
- Replicates: Sample in duplicate or triplicate at each time point.
Cell Counting Methods:
- Manual Counting: Using hemocytometer with trypan blue exclusion to distinguish viable cells [45] [130].
- Automated Counters: Systems like the LUNA-FX7 provide consistent, reproducible counts and can automatically calculate growth parameters [128].
- Non-Destructive Methods: Live-cell imaging systems that estimate confluency or cell counts without trypsinization, particularly valuable for precious primary cultures [127].
Data Recording: Record for each time point:
- Total cell count and concentration
- Viable cell count and viability percentage
- Time since seeding
- Observable morphological changes
Table 2: Research Reagent Solutions for Growth Curve Analysis
| Reagent/Equipment | Function | Application Notes |
|---|---|---|
| Complete Growth Medium | Provides nutrients, growth factors, and hormones for cell proliferation | Composition should be consistent; serum batches should be standardized |
| Trypsin-EDTA Solution | Detaches adherent cells for counting and passaging | Typically 0.05% trypsin with 0.53 mM EDTA; concentration may vary by cell line [45] |
| Hemocytometer | Manual cell counting chamber | Enables viable cell counting with trypan blue exclusion; requires expertise for consistency [130] |
| Automated Cell Counter | Automated cell counting and viability assessment | Improves reproducibility and efficiency; e.g., LUNA-FX7 with Bioprocess function [128] |
| PBS or HBSS | Salt solution for washing cells | Calcium- and magnesium-free for use before trypsinization [45] |
| Trypan Blue | Dye exclusion test for viability assessment | Stains non-viable cells blue; viable cells exclude dye |
Data Analysis and Calculation
Plotting the Growth Curve
Plot time on the x-axis and log of viable cell concentration on the y-axis. The exponential phase appears as a straight line on this semi-log plot, confirming constant growth rate during this period [128].
Calculating Population Doubling Time
Select two time points (t₁, t₂) within the exponential phase where the growth is linear on the semi-log plot, and their corresponding cell counts (N₁, N₂). Apply the doubling time formula [127] [130]:
Example Calculation: If cells grow from ( 1.0 \times 10^5 ) to ( 8.0 \times 10^5 ) in 48 hours: [ T_d = \frac{48 \times \ln(2)}{\ln(8.0 \times 10^5 / 1.0 \times 10^5)} = \frac{48 \times 0.693}{\ln(8)} = \frac{33.26}{2.08} = 16 \text{ hours} ]
Modern automated systems can calculate doubling time continuously throughout the culture period, providing more dynamic information about growth kinetics [128].
Advanced Analysis Methods
For more sophisticated applications, particularly when tracking adaptive processes or investigating subtle growth variations, advanced computational methods can be employed:
Time-Dependent Growth Rate Modeling: For cultures undergoing adaptation (e.g., developing drug resistance), growth rates may change over time. specialized software can infer time-dependent growth rates from cell count data using logistic growth models with time-varying parameters [131]: [ \frac{dN}{dt} = r(t)N - r(t)\frac{N^2}{K} ] Where r(t) is the time-dependent growth rate and K is the carrying capacity.
Bayesian Optimization for Media Development: Machine learning approaches like Bayesian Optimization can efficiently identify optimal culture conditions by balancing exploration of new parameter combinations with exploitation of known favorable conditions, significantly reducing the experimental burden for complex optimizations such as media formulation [132] [64].
Technical Considerations and Troubleshooting
Standardization for Reproducibility
- Consistent Seeding: Use standardized protocols for cell detachment and counting to ensure consistent seeding densities.
- Environmental Control: Maintain stable temperature, CO₂ concentration, and humidity throughout the experiment [128].
- Media Consistency: Use the same batch of media and serum throughout a single experiment to minimize variability.
- Passage Practice: For ongoing cultures, standardize passage procedures using consistent split ratios and confluency levels at passage [127].
Common Issues and Solutions
- Increasing Doubling Time: May indicate declining cell health, nutrient depletion, or suboptimal culture conditions. Review media replacement schedules and check incubator stability [128].
- Extended Lag Phase: Often results from excessively low seeding density, poor cell viability after passaging, or suboptimal culture conditions.
- Poor Growth Curve Reproducibility: Frequently stems from inconsistent sampling times, variable counting techniques, or changes in reagent batches.
- Cell Line Drift: Monitor doubling time as a sensitive indicator of phenotypic changes; significant deviations (>20-30%) from baseline may indicate genetic drift or contamination [127].
Documentation and Tracking
Maintain detailed records of:
- Seeding density and passage number at experiment initiation
- Population Doubling Level (PDL) for primary cells and finite lines
- Media formulations and serum lots
- Environmental parameters (temperature, CO₂)
- Morphological observations
In regulated environments, both passage number and PDL should be documented for critical applications [127].
Applications in Research and Development
Basic Research Applications
- Cell Physiology Studies: Doubling time serves as a sensitive indicator of cellular response to genetic manipulations, environmental stressors, or pharmacological treatments.
- Senescence Studies: Progressive increase in doubling time can indicate cellular aging, particularly in primary cultures.
- Toxicology: Changes in growth kinetics provide quantitative measures of compound cytotoxicity.
Bioprocess and Biomanufacturing
In biomanufacturing, understanding growth kinetics is essential for process scale-up and optimization. As processes move from laboratory to production scale, maintaining consistent doubling times and growth characteristics becomes challenging due to changes in mixing times, oxygen transfer rates, and shear forces [133]. Growth curve analysis at small scale provides baseline data for scale-up exercises, where parameters like power input per unit volume (P/V) or impeller tip speed are adjusted to maintain similar physiological states across scales [133].
Therapeutic Development
For cell-based therapies, tracking population doubling levels is critical for ensuring product safety and potency. Regulatory agencies require strict documentation of cellular replicative history, as excessive doublings can lead to genetic instability or functional alterations [127]. Growth curve analysis helps establish validated expansion protocols that generate sufficient cell numbers while maintaining therapeutic properties.
Growth curve analysis remains an essential technique for characterizing cell populations in culture, providing fundamental data on population doubling time and optimal seeding density that informs both routine culture maintenance and experimental design. The methodology outlined in this guide—from careful experimental setup through appropriate data analysis—enables researchers to obtain reliable, reproducible growth kinetics for their specific cell systems.
As cell culture applications continue to expand in complexity and scale, from personalized cell therapies to large-scale biomanufacturing, the principles of growth curve analysis provide a foundation for quality control and process optimization. By integrating traditional approaches with emerging technologies like automated monitoring systems and machine learning-driven optimization, researchers can extract maximum information from growth kinetics while minimizing experimental burden. Ultimately, rigorous attention to these fundamental parameters ensures that cell-based research and production builds upon a foundation of quantitatively understood cellular behavior, enhancing both scientific validity and technological application.
The landscape of preclinical biomedical research is undergoing a fundamental transformation, driven by a convergence of regulatory guidance, scientific advancement, and ethical considerations. Recent initiatives from the U.S. Food and Drug Administration (FDA) and the National Institutes of Health (NIH) are actively prioritizing the development and use of innovative, human-based research technologies while reducing reliance on animal models [134] [135]. This shift is rooted in a critical scientific challenge: many animal models do not translate well to human diseases, limiting researchers' abilities to develop effective interventions [134]. For microbiologists and cell culture specialists, this evolving paradigm places a premium on the ability to rigorously validate in vitro model systems to ensure they possess the physiological relevance necessary to yield replicable, translatable results.
The NIH's new initiative aligns with the FDA's roadmap to reduce animal testing, emphasizing the use of New Approach Methodologies (NAMs) as alternatives to traditional animal models [136]. A cornerstone of this initiative is the planned establishment of the Office of Research Innovation, Validation and Application (ORIVA) within the NIH’s Office of the Director. This office will coordinate NIH-wide efforts to develop, validate, and scale the use of non-animal approaches [134]. This guide provides a technical framework for validating model systems, with a focus on ensuring physiological relevance within this new research context.
The Driving Forces Behind the Shift to Human-Based Models
Regulatory and Policy Changes
Two landmark decisions in 2025 have accelerated the move toward human-relevant models. First, the FDA announced plans to phase out the requirement for animal testing of certain classes of new drugs—notably monoclonal antibody (mAb) therapies—in favor of "more effective, human-relevant methods" [135] [137]. Shortly thereafter, on April 29th, the NIH announced its initiative to prioritize human-based technologies and reduce animal use in testing [137]. These policies follow the track of the FDA Modernization Act 2.0 signed in late 2022, aiming to improve the predictive accuracy of preclinical research while addressing ethical and cost concerns associated with animal testing [135].
Scientific Limitations of Traditional Models
The scientific impetus for this shift stems from recognized limitations in existing models. Animal models often cannot replicate or predict human outcomes due to physiological, genetic, and functional differences [136]. Many therapeutics with proven safety and efficacy in animal models fail to demonstrate similar profiles in humans [136]. This translation gap is particularly pronounced in studies involving human conditions such as Alzheimer's, cancer, and inflammatory diseases [136]. Furthermore, traditional two-dimensional (2D) cell cultures fall short as they lack the three-dimensional interactions present in real tissues, which can lead to misleading results; for example, drug responses in 2D cultures often poorly predict outcomes in patients [135] [137].
Key Technologies in Human-Based Research
Emerging technologies now allow researchers to study health and disease using human-derived information, making them alternative avenues for yielding replicable and translatable results [134]. The NIH specifically highlights several key technologies:
- Organoids, tissue chips, and other in vitro systems that allow scientists to model human disease and capture human variability and patient-specific characteristics [134].
- Computational models which simulate complex biological human systems, disease pathways, and drug interactions [134].
- Real-world data that allow scientists to study health outcomes in humans at community and population levels [134].
Among these, 3D cell culture systems like organoids and spheroids have emerged as particularly promising human-relevant models [135] [137]. These constructs mimic aspects of human tissue architecture and function, offering a more physiologically relevant platform for disease modeling and drug screening.
Advanced 3D Culture Systems: Clinostat-Based Bioreactors
Not all 3D culture methods are equivalent. While static 3D cultures (e.g., those embedded in hydrogels) often suffer from diffusion limitations, and dynamic systems (e.g., spinning flasks) can introduce high shear forces, clinostat-based bioreactors represent an advanced technological solution [135] [137]. These systems, exemplified by CelVivo's ClinoStar and ClinoReactor, leverage clinostat principles—slow rotation to neutralize gravitational sedimentation—to cultivate 3D organoids in a suspension culture [135] [137]. This approach offers significant advantages:
- Low-shear, stress-free conditions that foster native-like cell polarity, functionality, and cell–cell communication [137].
- Development of natural oxygen, nutrient, and metabolite gradients, including hypoxic cores similar to those in tumors and intact organs [137].
- Enhanced reproducibility with studies demonstrating size coefficients of variation below 10%, enabling consistent responses to drug exposure across replicates [137].
A Framework for Validating Model System Physiology
Key Validation Parameters
Validating a model system requires assessing multiple parameters that collectively determine its physiological relevance. The table below summarizes the core parameters, their significance, and common assessment methodologies.
Table 1: Key Parameters for Validating Model System Physiology
| Validation Parameter | Physiological Significance | Recommended Assessment Methods |
|---|---|---|
| Morphological Architecture | Recapitulation of native tissue 3D structure; enables proper cell-cell and cell-matrix interactions. | Histology (H&E), immunohistochemistry, confocal microscopy, electron microscopy. |
| Cell Composition & Purity | Presence of relevant cell types in appropriate proportions; absence of contaminating lineages. | Flow cytometry, single-cell RNA sequencing, immunostaining for lineage markers. |
| Functional Capacity | Execution of specialized tasks performed by the native tissue/organ (e.g., secretion, contraction, barrier function). | ELISA/Western Blot for secreted products, transepithelial electrical resistance (TEER), metabolic assays. |
| Gene & Protein Expression | Expression of key markers, receptors, and enzymes characteristic of the native human tissue. | RNA sequencing, RT-qPCR, Western Blot, mass spectrometry-based proteomics. |
| Biomarker Production | Synthesis and release of tissue-specific functional biomarkers. | Mass spectrometry, immunoassays, functional enzymatic assays. |
| Metabolic Activity | Appropriate nutrient consumption, waste production, and energy utilization patterns. | Seahorse Analyzer, LC-MS for metabolomics, glucose/lactate assays. |
| Drug/Toxin Response | Pharmacological relevance and predictive value for human clinical outcomes. | Dose-response curves (IC50/EC50), high-content imaging, comparison to clinical data. |
| Long-Term Stability | Maintenance of phenotypic and functional characteristics over a relevant timeframe. | Longitudinal assessment of key parameters (above) over days/weeks in culture. |
Case Study: Validating a Neuroblastoma Model for Toxin Testing
A research team at the University of Sheffield developed a cell-based assay to replace animal testing for the safety assessment of clostridial toxin-based medicines (e.g., Botox, tetanus vaccine) [138]. Their validation approach provides an exemplary model:
- Challenge: Most neuron-like cell lines are not sensitive to tetanus or botulinum toxins as they lack sufficient surface proteins for toxin binding [138].
- Solution: The team engineered human neuroblastoma cell lines to express the necessary proteins for efficient toxin uptake and replication of the entire intoxication process [138].
- Validation Outcome: The cell-based system proved ten times more sensitive to botulinum B toxins than traditional animal testing methods [138]. For tetanus, iterative refinement improved sensitivity to the needed physiologically relevant concentrations [138].
- Regulatory Path: Ten global tetanus vaccine manufacturers are now participating in studies to optimize and demonstrate the fitness-for-purpose of these assays under Good Manufacturing Practice (GMP) regulations, with the objective of completely replacing animal safety tests [138].
Quantitative Benchmarks for Validation
Establishing quantitative benchmarks is crucial for objective assessment of model quality. The following table compiles key metrics from recent literature for evaluating advanced 3D model systems.
Table 2: Quantitative Benchmarks for Model System Validation
| Metric | Target Benchmark | Reported Example | Significance |
|---|---|---|---|
| Size Uniformity (Coefficient of Variation) | < 10% | Spheroids in clinostat systems showed CV < 10% [137]. | Indicates high reproducibility, essential for screening. |
| Functional Sensitivity | Equal to or greater than animal model | Botulinum B assay: 10x more sensitive than mouse test [138]. | Demonstrates superior predictive power. |
| Structural Integrity (Long-Term Culture) | Stable for > 30 days | Lung organoids maintained uniform structure for extended periods [137]. | Enables chronic toxicity studies & long-term experiments. |
| Marker Expression (vs. Native Tissue) | > 70% correlation to human transcriptome | N/A (Best practice target) | Confirms molecular fidelity. |
| Barrier Function (TEER values) | Within range of native tissue | N/A (Tissue-specific) | Validates integrity of epithelial/endothelial layers. |
Experimental Protocols for Core Validation Activities
Protocol 1: Assessing Morphological Fidelity via Histology and Imaging
This protocol is fundamental for confirming that a 3D model recapitulates basic tissue architecture.
- Fixation: Immerse organoids/spheroids in 4% paraformaldehyde for 24-48 hours at 4°C to ensure complete penetration.
- Processing: Dehydrate samples through a graded ethanol series, clear with xylene, and embed in paraffin blocks.
- Sectioning: Cut 5-7 µm sections using a microtome and mount on charged glass slides.
- Staining: Perform standard Hematoxylin and Eosin (H&E) staining:
- Deparaffinize and rehydrate sections.
- Stain in Hematoxylin for 5-8 minutes, differentiate in acid alcohol, and blue in Scott's tap water.
- Counterstain in Eosin for 1-3 minutes.
- Imaging: Capture high-resolution images using a brightfield microscope. For 3D reconstruction, use confocal microscopy on immunostained or fluorescently labeled whole-mount organoids.
Protocol 2: Functional Validation of Barrier Integrity
Transepithelial/Transendothelial Electrical Resistance (TEER) is a gold-standard, non-destructive functional assay for barrier-forming models.
- Preparation: Culture cells on permeable membrane supports (e.g., Transwell inserts) until confluence.
- Measurement: Use a voltohmmeter with a "chopstick" or cup electrode assembly.
- Sterilize electrodes with 70% ethanol followed by sterile buffer rinse.
- Place the ends of the electrodes in the apical and basolateral compartments.
- Calculation: Record the resistance (in Ω). Subtract the resistance of a blank insert (with media but no cells) and multiply by the membrane surface area (in cm²) to obtain TEER (Ω × cm²).
- Interpretation: Monitor TEER values over time. A steady increase followed by a plateau indicates the formation of a mature, functional barrier. Compare values to known standards for the tissue being modeled.
Visualization of the Validation Workflow
The following diagram outlines a systematic workflow for validating the physiological relevance of a model system, from initial characterization to functional assessment.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful culture and validation of advanced model systems require specific reagents and tools. The following table details key components of the research toolkit.
Table 3: Essential Research Reagents and Materials for Advanced Model Systems
| Tool/Reagent | Function/Purpose | Example Applications |
|---|---|---|
| Clinostat Bioreactor | Provides low-shear, dynamic 3D culture environment via slow rotation to neutralize gravity. | Culturing organoids with enhanced physiological relevance and reduced variability [135] [137]. |
| Extracellular Matrix (ECM) Hydrogels | Mimics the native cellular microenvironment; provides mechanical and biochemical support for 3D growth. | Embedding organoids, supporting polarized growth, and enabling morphogenesis. |
| Defined Culture Media | Serum-free formulations with specific growth factors and supplements to guide cell fate and maintain phenotype. | Long-term maintenance of stem cell-derived organoids and specialized tissue functions. |
| Cell Line Engineering Tools | Modifies cells to express or knock down genes of interest, enhancing functionality for specific assays. | Engineering neuroblastoma cells to express toxin receptors for potency assays [138]. |
| Biosensors & Reporter Assays | Enable real-time, non-invasive monitoring of cell viability, metabolism, and specific pathway activities. | Kinetic assessment of drug efficacy/toxicity; measuring intracellular calcium flux. |
| Validated Primary Cell Sources | Provide human-derived, physiologically relevant cells that retain key characteristics of their tissue of origin. | Establishing patient-specific models and ensuring genetic diversity in research. |
The validation of physiologically relevant model systems is no longer a peripheral concern but a central requirement for impactful biomedical research. As regulatory agencies like the NIH and FDA increasingly prioritize human-based technologies, the ability to rigorously demonstrate that a model faithfully recapitulates key aspects of human physiology becomes critical for both scientific credibility and regulatory acceptance [134] [136]. While challenges remain—including standardization, reproducibility, and the integration of complex systemic interactions—the scientific community is developing robust frameworks and advanced tools to address them [135] [137]. By adopting the comprehensive validation strategies outlined in this guide, microbiologists and cell culture researchers can confidently develop and utilize models that not only reduce the reliance on animal testing but also significantly improve the predictive power of preclinical research, ultimately accelerating the development of safer and more effective therapeutics.
The foundation of robust and translatable biomedical research rests on the principles of reproducible and ethical science. For microbiologists venturing into animal cell culture, adhering to established guidelines is not merely a bureaucratic exercise but a critical component of scientific integrity. The widespread use of animal-derived reagents, particularly fetal bovine serum (FBS), raises significant ethical concerns and introduces scientific limitations that can compromise data quality and reproducibility [139]. Estimates suggest millions of bovine fetuses are used annually to meet the global demand for FBS, a process with substantial animal welfare implications [139]. From a scientific perspective, FBS is an undefined and variable mixture whose composition fluctuates based on batch, season, and geographical source, directly contributing to the reproducibility crisis in biomedical research [139] [42]. This article provides a technical guide for integrating standardized, ethical practices into cell culture workflows, ensuring research is both reliable and socially responsible.
Navigating the Regulatory and Guidance Landscape
A framework of guidelines and standards has been established to govern cell culture practices. While not all are legally binding, they represent the scientific community's consensus on best practices.
2.1 Core Principles and Guidelines
- Good Cell Culture Practice (GCCP): GCCP guidelines provide comprehensive guidance on quality management, culture systems, documentation, and safety [42]. Their goal is to harmonize and standardize laboratory practices to ensure compliance with regulations and ethical principles, ultimately supporting the reproducibility of in vitro experimentation [42].
- The 3Rs (Replacement, Reduction, and Refinement): Formulated by William Russell and Rex Burch, the 3Rs are a cornerstone of ethical research. They advocate for replacing animal-based research where possible, reducing the number of animals used, and refining procedures to minimize suffering [42]. The adoption of human-relevant, animal-free cell culture methods is a direct application of the "Replacement" principle.
2.2 Key Issues Addressed by Standards
- Cell Line Misidentification and Cross-Contamination: This is a pervasive problem. The International Cell Line Authentication Committee (ICLAC) lists over 500 misidentified or cross-contaminated cell lines, which has led to a profusion of false and irreproducible results in the literature [42].
- Biosafety and Genetically Modified Cell Lines (GMCLs): Many continuous cell lines are immortalized using agents with oncogenic potential, such as the Simian virus 40 (SV40) large T-antigen, or are derived from genetically modified animals. Such cell lines often require specific safety classifications and handling procedures [42].
Table 1: Essential Standards and Committees for Cell Culture Research
| Standard/Committee | Primary Focus | Key Guidance/Risk |
|---|---|---|
| Good Cell Culture Practice (GCCP) | Quality management, standardization, and documentation of cell culture processes. | Promotes reproducibility and ethical compliance [42]. |
| International Cell Line Authentication Committee (ICLAC) | Cell line misidentification and cross-contamination. | Maintains a register of misidentified cell lines; recommends authentication [42]. |
| Biosafety Guidelines for GMCLs | Safe handling of genetically modified cell lines. | Requires risk assessment and specific containment procedures [42]. |
Implementing Ethical and Defined Reagent Systems
A primary strategy for enhancing ethical standards and reproducibility is replacing ill-defined animal-derived reagents with scientifically superior alternatives.
3.1 The FBS Challenge and Chemically Defined Media (CDM)
FBS is harvested via cardiac puncture of bovine fetuses during slaughter, a significant ethical issue [139]. Scientifically, its undefined nature and batch-to-batch variability undermine experimental consistency and the ability to precisely determine the factors influencing cellular responses [139]. Chemically Defined Media (CDMs) are the solution. These media are precisely formulated with known components such as insulin, transferrin, selenium, and essential nutrients, eliminating ethical concerns and variability [139]. Recent innovations include the development of a universal CDM capable of supporting the growth of diverse cell types, including HeLa, JIMT-1, and CaCo-2 cells [139].
3.2 Alternatives to Other Animal-Derived Reagents
A full transition to animal-free workflows requires replacing several common reagents:
- Trypsin Replacement: Recombinant proteins like TrypLE serve as effective, animal-free substitutes for porcine trypsin for cell detachment and passaging [139].
- Antibodies: Traditional antibodies are produced in animals. Recombinant antibodies, particularly those generated via phage display (a fully in vitro process), offer superior specificity, reproducibility, and an animal-free pedigree [139]. Large-scale studies have shown recombinant antibodies outperform both monoclonal and polyclonal counterparts [139].
- Basement Membrane Extracts (BMEs): Animal-derived BMEs (e.g., Matrigel) can be replaced with synthetic polymers, recombinant collagen, and hyaluronic acid-based matrices for 3D cell culture applications [139].
Table 2: Research Reagent Solutions for Animal-Free Cell Culture
| Reagent Category | Traditional Animal-Derived Reagent | Ethical & Defined Alternative | Function |
|---|---|---|---|
| Culture Medium Supplement | Fetal Bovine Serum (FBS) | Chemically Defined Media (CDM) | Provides nutrients, hormones, and growth factors for cell proliferation [139]. |
| Cell Dissociation Agent | Porcine Trypsin | Recombinant TrypLE | Enzymatically dissociates adherent cells for passaging [139]. |
| Immunodetection | Animal-derived Antibodies | Recombinant (e.g., Phage Display) Antibodies | Binds specifically to target antigens for assays like Western blotting [139]. |
| 3D Culture Scaffold | Basement Membrane Extract (BME/Matrigel) | Synthetic Polymers, Recombinant Collagen | Provides a structural scaffold for three-dimensional cell growth [139]. |
Detailed Experimental Protocol: Transitioning to an Animal-Free Workflow
The following protocol details the adaptation of HeLa cells to a CDM and their use in key molecular biology techniques, providing a replicable framework for researchers.
4.1 Cell Culture in Chemically Defined Medium
- Materials:
- HeLa cells (e.g., ACC 57, DSMZ)
- Conventional medium: Dulbecco’s Modified Eagle Medium (DMEM), low glucose, supplemented with 10% FBS, 2 mM L-glutamine, 1% non-essential amino acids (NEAA) [139].
- Chemically Defined Medium (CDM) formulation: See Table 3 for components.
- Recombinant TrypLE
- Animal-free, validated antibodies for downstream assays
- Methodology:
- Preparation: Assemble the complete CDM. The prepared medium can be stored at 4°C for at least one month [139].
- Cell Adaptation: HeLa cells can be directly adapted to CDM without a gradual FBS reduction, provided they are in a highly proliferative state before the switch. Culture the cells in CDM for at least six passages prior to experimental use to reduce the influence of residual, intracellular FBS components [139].
- Maintenance and Passaging: Maintain cells at 37°C in a humidified incubator. For passaging, use recombinant TrypLE to detach adherent cells. Routinely subculture cells before they reach 100% confluency to maintain them in the exponential growth phase [139] [6].
- Quality Control: Regularly monitor cells for signs of contamination (e.g., medium turbidity, unusual pH shifts) and morphological changes using an inverted microscope [6].
Table 3: Example Formulation of a Chemically Defined Medium for HeLa Cells [139]
| Component | Concentration | Function |
|---|---|---|
| DMEM/F-12 | 1X | Base nutrient source. |
| Non-essential amino acids | 1X | Reduces metabolic burden on cells. |
| HEPES | 15 mM | pH buffer. |
| D-glucose | 0.1% | Energy source. |
| L-glutamine | 2 mM | Essential amino acid for energy and protein synthesis. |
| Insulin-Transferrin-Selenium (ITS) | 1X | Provides essential hormones and trace elements for growth. |
| Hydrocortisone | 1 μg/mL | Growth and signaling regulator. |
| Human epidermal growth factor | 10 ng/mL | Stimulates cell growth and proliferation. |
4.2 Key Molecular Techniques in an Animal-Free System
The following techniques can be successfully performed with cells adapted to CDM and animal-free reagents [139]:
- Transfection & RNA Interference (RNAi): Introduce DNA or RNAi constructs into HeLa cells to modulate gene expression.
- Quantitative RT-PCR (qRT-PCR): Measure changes in gene expression levels.
- Dual-Luciferase Assays: Study regulatory elements of gene expression.
- Western Blotting: Detect specific proteins using validated, animal-free antibodies.
Ensuring Quality Control and Authentication
Rigorous quality control is the bedrock of reproducible science. Key practices include:
- Cell Line Authentication: Use techniques like Short Tandem Repeat (STR) profiling to confirm cell line identity and rule out cross-contamination. This is crucial, as an estimated 16.1% of published papers may have used problematic cell lines [42].
- Mycoplasma Testing: Routinely test cell cultures for mycoplasma contamination, which can alter cell behavior and physiology without causing visible turbidity [42].
- Documentation and Passage Number: Maintain meticulous records of culture history, including passage number and population doubling level, as genetic drift can occur over time [6].
Visualizing the Animal-Free Transition Workflow
The following diagram illustrates the key decision points and processes for establishing reproducible and ethical cell culture practices.
The transition to standardized, ethical, and animal-free cell culture is an achievable and necessary evolution for modern biomedical research. By integrating the guidelines, protocols, and quality control measures outlined in this technical guide, microbiologists and other researchers can significantly enhance the reproducibility, human relevance, and ethical foundation of their work. This shift, driven by education and the adoption of best practices, is essential for fostering a more reliable and responsible scientific ecosystem that accelerates the development of effective therapies [140].
Conclusion
Mastering animal cell culture requires microbiologists to adopt a new mindset, prioritizing the complex physiological needs of mammalian cells over the robustness of microbes. The key to success lies in integrating foundational knowledge with meticulous methodology, rigorous troubleshooting, and unwavering commitment to validation. As the field advances, the future points unequivocally towards standardized, chemically defined, and animal-free culture systems. These innovations are crucial for enhancing experimental reproducibility, overcoming the limitations of fetal bovine serum, and developing more human-relevant models for drug discovery and clinical translation. By embracing these practices, researchers can fully leverage the power of animal cell culture to drive breakthroughs in biomedical science.
References
- 1. Animal Cell Culture - an overview [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/animal-cell-culture]
- 2. Animal Cell Culture: Types, Cell Lines, Procedure, Uses [https://microbenotes.com/animal-cell-culture/]
- 3. The growing value of animal cells to humans [https://www.cellgs.com/blog/the-growing-value-of-animal-cells-to-humans.html]
- 4. Cell culture [https://en.wikipedia.org/wiki/Cell_culture]
- 5. Cell Culture Protocols | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/cell-culture-protocols.html]
- 6. ATCC Animal Cell Culture Guide [https://www.atcc.org/resources/culture-guides/animal-cell-culture-guide]
- 7. Insights into the Animal Cell Culture Market from 2025 to ... [https://www.linkedin.com/pulse/insights-animal-cell-culture-market-from-2025-2032-projecting-ibqmf]
- 8. Animal Cell Culture Charting Growth Trajectories: Analysis ... [https://www.archivemarketresearch.com/reports/animal-cell-culture-144770]
- 9. A quantitative meta-analysis comparing cell models in ... [https://www.nature.com/articles/s41598-023-35043-5]
- 10. 原代细胞vs 细胞系:培养差异与精准鉴定策略 [https://www.uptbio.com/news/view/1231.html]
- 11. Primary vs Immortal Cell Lines [https://www.criver.com/eureka/ask-scientist-whats-difference-between-primary-and-immortalized-cells]
- 12. 原代細胞培養基礎 [https://www.sigmaaldrich.com/TW/zh/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/primary-cell-culture/primary-cell-culture?srsltid=AfmBOooF-hOAh9zVgfdqVclnaMywc3wzUBTDF5-wL8NkCjnQvNOrSaY2]
- 13. 哺乳动物细胞培养的介绍 [https://www.leica-microsystems.com.cn/cn/science-lab/life-science/introduction-to-mammalian-cell-culture/]
- 14. Cell Lines vs. Primary Cells [https://www.stemcell.com/physiological-relevance-of-human-primary-cells-vs-cell-lines]
- 15. Primary cells vs. cell lines: Is it not time for something better? [https://www.bit.bio/blog/primary-cells-vs-cell-lines]
- 16. Comparative Proteomic Phenotyping of Cell Lines and ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2649808/]
- 17. Adherent Cell Culture Protocol [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/cell-culture-protocols/subculturing-adherent-cells.html]
- 18. Suspension Cell Culture Protocol [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/cell-culture-protocols/subculturing-suspension-cells.html]
- 19. Adherent versus suspension based platforms: what is the ... [https://www.insights.bio/cell-and-gene-therapy-insights/journal/article/2244/Adherent-versus-suspension-based-platforms-what-is-the-near-future-of-viral-vector-manufacturing]
- 20. Evolution from adherent to suspension: systems biology of ... [https://www.nature.com/articles/s41598-020-76137-8]
- 21. Cell Morphology | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/cell-analysis-learning-center/molecular-probes-school-of-fluorescence/imaging-basics/sample-considerations/cell-morphology.html]
- 22. Tip of the month: Growth surfaces for cells [https://www.sarstedt.com/en/products/new-products/tip-of-the-month-growth-surfaces-for-cells/]
- 23. Differences between microbial fermentation & mammalian ... [https://www.susupport.com/blogs/knowledge/differences-between-microbial-fermentation-mammalian-cell-culture]
- 24. Bacterial culture through selective and non ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6961714/]
- 25. A Deep Dive into Cell Culture Media [https://www.scientificbio.com/blog/deep-dive-into-cell-culture-media]
- 26. Animal‐cell culture media: History, characteristics, and current ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5661806/]
- 27. Cell Culture Environment | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/cell-culture-environment.html]
- 28. Talking about Shake Flasks and Bioreactors [https://www.eppendorf.com/us-en/lab-academy/life-science/cell-biology/it-s-not-just-about-size-talking-about-shake-flasks-and-bioreactors/]
- 29. Cell Culture Equipment | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/cell-culture-equipment.html]
- 30. Cell Culture Lab Equipment Check List and Guide [https://www.coleparmer.com/blog/cell-culture-lab-equipment-guide/]
- 31. Biological Safety Cabinet vs Laminar Flow Hood [https://www.ossila.com/pages/biological-safety-cabinets-laminar-flow-hoods]
- 32. The Importance of HeLa Cells [https://www.hopkinsmedicine.org/henrietta-lacks/importance-of-hela-cells]
- 33. HeLa Cell Line: Revolutionizing Research [https://www.cytion.com/us/Knowledge-Hub/Cell-Line-Insights/HeLa-Cell-Line-Revolutionizing-Research/]
- 34. HeLa [https://en.wikipedia.org/wiki/HeLa]
- 35. Cell line profile: MCF7 [https://www.culturecollections.org.uk/products/cell-cultures/ecacc-cell-line-profiles/mcf7/]
- 36. Biological differences among MCF-7 human breast cancer cell ... [https://pubmed.ncbi.nlm.nih.gov/3620713/]
- 37. Hybridoma technology; advancements, clinical significance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8521504/]
- 38. Hybridoma technology [https://en.wikipedia.org/wiki/Hybridoma_technology]
- 39. Hybridoma Fusion Partners Cell Lines [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/hybridoma-fusion?srsltid=AfmBOopaZgzy_mGNaj9titogFXIB7gVIVZtphdXFvXp8l5PbsvUUexld]
- 40. Hybridoma Cell Line - an overview [https://www.sciencedirect.com/topics/immunology-and-microbiology/hybridoma-cell-line]
- 41. Seeding, Subculturing, and Maintaining Cells [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/maintaining-cultured-cells.html]
- 42. A Beginner's Guide to Cell Culture: Practical Advice for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10000895/]
- 43. Maintaining Cells [https://molecular-biology.coe.hawaii.edu/lessons/maintaining-cells/]
- 44. How To Passage Cells in Culture [https://bitesizebio.com/13680/how-to-passage-cells/]
- 45. Essential protocols for animal cell culture [https://www.qiagen.com/us/knowledge-and-support/knowledge-hub/bench-guide/animal-cell-culture/essential-protocols-for-animal-cell-culture/essential-protocols-for-animal-cell-culture]
- 46. Cell Freezing Protocols | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/cell-culture-protocols/freezing-cells.html]
- 47. Protocols and Best Practices for Freezing Cells [https://www.stemcell.com/cryopreservation-basics-protocols-and-best-practices-for-freezing-cells]
- 48. Cryopreservation: An Overview of Principles and Cell- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7995302/]
- 49. Impact of lower concentrations of dimethyl sulfoxide on ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324924000537]
- 50. Optimization of freezing and thawing protocols for human ... [https://www.sciencedirect.com/science/article/pii/S0011224025000513]
- 51. Thawing Cells | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/cell-culture-protocols/thawing-cells.html]
- 52. A potency and toxicology study on tolerability of cryopreserved ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590272/]
- 53. Dimethyl sulfoxide in cryopreserved mesenchymal stromal cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12362920/]
- 54. Biological Safety Manual - Chapter 04 [https://policies.unc.edu/TDClient/2833/Portal/KB/ArticleDet?ID=131879]
- 55. CDC LC Quick Learn: Recognize the four Biosafety Levels [https://www.cdc.gov/training/quicklearns/biosafety/]
- 56. Biosafety Levels & Lab Safety Guidelines [https://aspr.hhs.gov/S3/Pages/Biosafety-Level-Requirements.aspx]
- 57. Aseptic Laboratory Techniques and Safety in Cell Culture [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/aseptic-technique.html]
- 58. Equipment's used in animal cell culture | PPTX [https://www.slideshare.net/slideshow/equipments-used-in-animal-cell-culture/85423908]
- 59. Aseptic Laboratory Techniques: Plating Methods - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4846335/]
- 60. Lab Safety - iGEM Toronto 2025 [https://2025.igem.wiki/toronto/wet-lab/safety]
- 61. Bridging gene therapy and next-generation vaccine ... [https://www.nature.com/articles/s41434-024-00502-9]
- 62. Molecular Farming for Immunization: Current Advances and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11860421/]
- 63. Machine learning-driven optimization of culture conditions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12355708/]
- 64. Accelerating cell culture media development using ... [https://www.nature.com/articles/s41467-025-61113-5]
- 65. BioProcess International March 2025 Issue 2025 - March [https://www.bioprocessintl.com/publications/bioprocess-international/march-2025]
- 66. Re-imagining human cell culture media: Challenges, ... [https://www.sciencedirect.com/science/article/abs/pii/S0734975025000503]
- 67. Growth Factors for Cell Culture 2025-2033 Trends [https://www.archivemarketresearch.com/reports/growth-factors-for-cell-culture-136602]
- 68. Comparison of culture media supplements identifies serum ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12382287/]
- 69. Animal Component Free Cell Culture Reagents [https://www.sigmaaldrich.com/US/en/products/cell-culture-and-analysis/animal-component-free-cell-culture-reagents?srsltid=AfmBOoqlCrgaRqgkh_G7WS-yUDtluAQPKDkvvve-YDUSEispQE7U_7gM]
- 70. Serum-Free and Animal-Free Cell Culture Media [https://www.bio-techne.com/reagents/cell-culture-reagents/serum-free-animal-free]
- 71. How We Define Our Culture Media and Supplements [https://www.stemcell.com/how-do-we-define-our-media.html]
- 72. Animal-Free Sera and Media - Krishgen Biosystems [https://www.krishgenbiosystems.com/cell-culture/animal-free-sera-and-media/]
- 73. Cell Culture Media Market Outlook: Strong 13.2% CAGR to ... [https://www.prnewswire.com/news-releases/cell-culture-media-market-outlook-strong-13-2-cagr-to-drive-12-8-billion-revenue-by-2033---grand-view-research-inc-302620008.html]
- 74. Bacterial Cell Culture Market 2025 Growth Accelerates ... [https://www.towardshealthcare.com/insights/bacterial-cell-culture-market-sizing]
- 75. Microbiology and Bacterial Culture Media Market Size to ... [https://www.precedenceresearch.com/microbiology-and-bacterial-culture-media-market]
- 76. Cell Culture Trends To Watch In 2025 [https://www.bioprocessonline.com/doc/cell-culture-trends-to-watch-in-0001]
- 77. Comprehensive Microbial Control Strategy [https://www.bioprocessintl.com/qa-qc/beyond-traditional-microbiology-testing-developing-a-comprehensive-strategy-for-microbial-control-and-detection]
- 78. Prevention, Diagnosis and Eradication of Mycoplasma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10668599/]
- 79. Lymphocytic Choriomeningitis Virus (LCMV) [https://www.bu.edu/research/ethics-compliance/safety/rohp/agent-information-sheets/lymphocytic-choriomeningitis-virus-lcmv/]
- 80. Cell Culture FAQs: Bacterial Endotoxin Contamination [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/microbiological-testing/pyrogen-testing/what-is-endotoxin?srsltid=AfmBOopMUxKNbVqUkQVBkLi21w0PnhCFNIXfccnHtpUF7N968J2dc8Lk]
- 81. Bacterial Endotoxins/Pyrogens [https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/inspection-technical-guides/bacterial-endotoxinspyrogens]
- 82. Novel method detects microbial contamination in cell cultures [https://news.mit.edu/2025/novel-method-detects-microbial-contamination-smart-0425]
- 83. 9 Sterilization Techniques For Cell Culture [https://visikol.com/blog/2022/11/30/9-sterilization-techniques-for-cell-culture/]
- 84. What is a HEPA filter? [https://www.epa.gov/indoor-air-quality-iaq/what-hepa-filter]
- 85. HEPA Filters: Understanding Performance Standards ... [https://cleanair.camfil.us/2025/09/22/hepa-filters-understanding-performance-standards-applications-and-selection-criteria/]
- 86. Ready-to-Use Cell Culture Media in the Real World [https://www.linkedin.com/pulse/ready-to-use-cell-culture-media-real-world-5-exvpe]
- 87. Evaluation of image analysis tools for the measurement of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12119626/]
- 88. Systematic data analysis pipeline for quantitative ... [https://www.sciencedirect.com/science/article/pii/S2001037024002460]
- 89. Basic quantitative morphological methods applied to the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7818269/]
- 90. Glucosamine mitigates hyperglycemic-induced oxidative ... [https://www.nature.com/articles/s41598-025-19766-1]
- 91. pH In Cell Culture - How Does pH Buffered Culture Media ... [https://www.scientificbio.com/blog/ph-in-cell-culture-how-does-ph-buffered-culture-media-work/]
- 92. Evidence-based guidelines for controlling pH in ... [https://www.nature.com/articles/s42003-019-0393-7]
- 93. CO2 concentration and pH control in the cell ... [https://www.culturecollections.org.uk/culture-collection-news/co2-concentration-and-ph-control-in-the-cell-culture-laboratory/]
- 94. How to Optimize Cell Culture Media for High-Yield ... [https://cellculturecompany.com/how-to-optimize-cell-culture-media-for-high-yield-recombinant-protein-production-in-mammalian-cells/]
- 95. Complete CO₂ Incubator Setup and Maintenance Guide [https://www.nuaire.com/resources/co2-incubator-setup-maintenance-guide]
- 96. How to Install & Maintain CO₂ Incubators [https://www.escolifesciences.com/news/proper-installation-and-maintenance-of-co2-incubators]
- 97. 8 Ways to Optimize Cell Cultures [https://vistalab.com/8-ways-to-optimize-cell-cultures/]
- 98. Optimization by Response Surface Methodology of Confluent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2901170/]
- 99. Cell Culture Troubleshooting [https://www.sigmaaldrich.com/US/en/applications/cell-culture-and-cell-culture-analysis/cell-culture-troubleshooting?srsltid=AfmBOoqulbFWcoJmwChzNPClnkul_JvTBhvXdlqU0ncLhlOAT-GUMNYa]
- 100. Poor Cell Growth Troubleshooting [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/poor-cell-growth?srsltid=AfmBOorCRsMm5EN0WNga07xUJgWwXlh3SSHi0_MWDM9dmZJ6WtTy-XbV]
- 101. Poor Adherent Cell Attachment Troubleshooting [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/cell-culture-and-cell-culture-analysis/mammalian-cell-culture/poor-adherent-cell-attachment-troubleshooting?srsltid=AfmBOoqtGRlx8YRzIXq7sTk4QLuMtk3tKwePJH6Hdr7V6wQ3DZF_wGUz]
- 102. Common cell culture problems and causes [https://www.bocsci.com/resources/common-cell-culture-problems-and-causes.html?srsltid=AfmBOoqHgIi51_iWEztVUilI8kOArjjzeMiyWIf6E0yZrcq9_Dna86T9]
- 103. Enzymatic and Non-Enzymatic Cell Dissociation Protocols [https://www.thermofisher.com/us/en/home/references/gibco-cell-culture-basics/cell-culture-protocols/cell-dissociation-protocol.html]
- 104. Cell Viability Assays - Assay Guidance Manual - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK144065/]
- 105. Optimization of Key Factors in Serum Free Medium for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7393043/]
- 106. Best practices for media selection for mammalian cells [https://pubmed.ncbi.nlm.nih.gov/28726187/]
- 107. Employing active learning in the optimization of culture ... [https://www.nature.com/articles/s41540-023-00284-7]
- 108. Development of Serum-Free Medium and Suspension ... [https://biomedpharmajournal.org/vol18no2/development-of-serum-free-medium-and-suspension-culture-for-hek293-cells-using-systematic-optimization-strategies/]
- 109. Stock Culture Maintenance and Storage [https://www.rapidmicrobiology.com/test-method/stock-culture-maintenance-and-storage]
- 110. Introduction to Microbiology [https://www.atcc.org/resources/culture-guides/introduction-to-microbiology]
- 111. Cell line authentication and validation is a key requirement ... [https://pubmed.ncbi.nlm.nih.gov/40547562/]
- 112. Cell line authentication and validation is a key requirement ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12181071/]
- 113. Misidentified cell lines: failures of peer review, varying journal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12247328/]
- 114. The ghosts of HeLa: How cell line misidentification ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0186281]
- 115. Cell Line Authentication Test Recommendations [https://www.atcc.org/resources/technical-documents/cell-line-authentication-test-recommendations]
- 116. Cell Culture Quality Control: The Key to Reproducibility [https://www.technologynetworks.com/cell-science/articles/cell-culture-quality-control-the-key-to-reproducibility-361872]
- 117. Why the Future of Biological Research Requires Cell Line ... [https://www.psomagen.com/blog/future-of-research-requires-cell-line-authentication]
- 118. Cell line authentication using optical genome mapping [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-025-11799-0]
- 119. Keeping It Clean: The Cell Culture Quality Control ... [https://www.sciencedirect.com/science/article/pii/S2472555222065649]
- 120. Why Mycoplasma Testing Is Critical for Mammalian Cell ... [https://cellculturecompany.com/why-mycoplasma-testing-is-critical-for-mammalian-cell-cultures/]
- 121. Mycoplasma Contamination Why It ... [https://hardydiagnostics.com/media/wysiwyg/MICRObits/Pharma/2025/06-June/microbits-pharma-june-2025-newsletter.html]
- 122. Mycoplasma Contamination in Cell Culture [https://www.nature.com/research-intelligence/nri-topic-summaries/mycoplasma-contamination-in-cell-culture-micro-1211272]
- 123. Karyotype Analysis Protocol [https://www.creative-bioarray.com/support/karyotype-analysis-protocol.htm]
- 124. Standardization of Cell Culture Conditions and Routine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9265327/]
- 125. Isoenzyme Analysis - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/isoenzyme-analysis]
- 126. Cell Line Authentication Using Isoenzyme Analysis [https://www.biopharminternational.com/view/cell-line-authentication-using-isoenzyme-analysis]
- 127. Doubling Time, Passage Number & PDL Explained [https://www.snapcyte.com/doubling-time-passage-number-pdl-everything-you-need-to-know/]
- 128. Cell Culture Growth Curves and Doubling Time with LUNA ... [https://logosbio.com/essential-metrics-in-cell-culture-understanding-growth-curves-and-doubling-time/]
- 129. EFFECTS OF PLATING DENSITY AND CULTURE TIME ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2603339/]
- 130. 3.1. Cell Doubling Time - Cellecta, Inc. [https://manuals.cellecta.com/lentiviral-construct-packaging-and-transduction/v10a/en/topic/cell-doubling-time]
- 131. Inferring time-dependent population growth rates in cell ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-020-03887-7]
- 132. Bayesian Optimization in Bioprocess Engineering—Where Do ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12067035/]
- 133. Exploring Principles of Bioreactor Scale-Up [https://www.bioprocessintl.com/bioreactors/lessons-in-bioreactor-scale-up-part-1-mdash-exploring-introductory-principles]
- 134. NIH to Prioritize Human-Based Research Technologies [https://nihrecord.nih.gov/2025/07/04/nih-prioritize-human-based-research-technologies]
- 135. Refining Biomedical Research Beyond Animal Models [https://omixys.pl/news/refining-biomedical-research-beyond-animal-models/]
- 136. NIH Research: Prioritizing Human-Based ... [https://alientt.com/nih-research-prioritizing-human-based-research-technologies/]
- 137. Blog: Refining Biomedical Research Beyond Animal Models [https://celvivo.com/blog-refining-biomedical-research-beyond-animal-models/]
- 138. Replacing animals with human cell cultures in ... [https://www.understandinganimalresearch.org.uk/news/replacing-animals-with-human-cell-cultures-in-pharmaceutical-toxin-safety-tests]
- 139. Promoting ethical and reproducible cell culture [https://pmc.ncbi.nlm.nih.gov/articles/PMC12521421/]
- 140. Promoting the adoption of best practices and standards to ... [https://www.sciencedirect.com/science/article/pii/S2213671125001353]