A Practical Guide to Sample Size Calculation for Microbiological Method Verification
This article provides a comprehensive guide for researchers and drug development professionals on determining appropriate sample sizes for the verification of microbiological methods.
A Practical Guide to Sample Size Calculation for Microbiological Method Verification
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on determining appropriate sample sizes for the verification of microbiological methods. Aligning with international standards like the ISO 16140 series, it bridges the gap between statistical principles and practical laboratory application. The content covers foundational concepts, step-by-step methodologies, strategies for troubleshooting common issues, and the final steps for validation and comparative analysis, empowering scientists to design robust and defensible verification studies.
Why Sample Size Matters: Foundational Concepts for Robust Method Verification
Distinguishing Method Validation from Verification in Microbiology
In clinical, pharmaceutical, and food safety microbiology laboratories, demonstrating the reliability of analytical methods is a fundamental requirement for regulatory compliance and data integrity. The terms "method validation" and "method verification" are often used interchangeably, but they describe distinct processes with different objectives, scopes, and applications. Understanding this distinction is critical for selecting the correct approach when implementing new microbiological tests and for ensuring that the data generated is scientifically sound and defensible.
Method validation is the comprehensive process of proving that an analytical procedure is fit for its intended purpose. It is an in-depth investigation conducted to establish the performance characteristics and limitations of a new method, typically during its development or when significantly modifying an existing one. In contrast, method verification is the process of providing objective evidence that a previously validated method performs as expected within a specific laboratory's environment, using its operators and equipment. Essentially, validation asks, "Does this method work in principle?" while verification asks, "Can our laboratory perform this method correctly?"
Core Conceptual Differences
The fundamental differences between method validation and verification can be understood through their definitions, objectives, and the contexts in which they are applied.
What is Method Validation?
Method validation is a documented process that proves an analytical method is acceptable for its intended use [1]. It is a rigorous exercise performed to demonstrate that the method is capable of delivering results at the required performance level for specific applications [2]. Validation is typically required in the following scenarios:
- Development of a new analytical method (a Laboratory Developed Test or LDT).
- When an existing FDA-cleared or approved method is modified in a way not specified as acceptable by the manufacturer (e.g., using different specimen types or altering test parameters like incubation times) [3].
- Transfer of a method between laboratories or instruments where its performance must be re-established [1].
What is Method Verification?
Method verification is the process of confirming that a previously validated method performs as expected under a specific laboratory's conditions [1]. It is a one-time study meant to demonstrate that a test performs in line with previously established performance characteristics when used exactly as intended by the manufacturer for unmodified FDA-approved or cleared tests [3]. Laboratories perform verification anytime they start using a new, standardized method to demonstrate they can achieve the performance characteristics claimed during the validation process [4] [5].
Table 1: High-Level Comparison of Validation and Verification
| Aspect | Method Validation | Method Verification |
|---|---|---|
| Core Question | Does this method work for its intended purpose? | Can our lab perform this validated method correctly? |
| Context | New methods, lab-developed tests, modified methods | Adopting unmodified, commercially available methods |
| Scope | Comprehensive assessment of all performance parameters | Limited assessment of key performance parameters |
| Performed By | Method developer (often a third party) [4] | End-user laboratory |
| Regulatory Focus | Establishes performance claims [1] | Demonstrates laboratory competency [1] |
Performance Parameters and Experimental Design
The experimental designs for validation and verification differ significantly in breadth and depth. Validation requires a full characterization of the method, while verification focuses on confirming a subset of key parameters in the user's specific environment.
Parameters for Method Validation
A complete method validation characterizes a wide array of performance metrics [2] [6]:
- Accuracy: Closeness of agreement between a measured value and the true value.
- Precision: The degree of agreement among individual test results when the procedure is applied repeatedly to multiple samplings (includes within-run, between-run, and operator variance) [3].
- Specificity: Ability to assess the analyte unequivocally in the presence of expected interferences like impurities or other matrix components.
- Detection Limit (LOD): The lowest amount of analyte that can be detected.
- Quantitation Limit (LOQ): The lowest amount of analyte that can be quantified with acceptable precision and accuracy.
- Linearity: The ability to obtain results directly proportional to analyte concentration.
- Range: The interval between upper and lower analyte levels where suitable precision, accuracy, and linearity are demonstrated.
- Robustness: Capacity to remain unaffected by small, deliberate variations in procedural parameters.
Parameters for Method Verification
For verification of unmodified FDA-approved tests, laboratories are required to verify a more focused set of characteristics [3]:
- Accuracy: To confirm acceptable agreement of results between the new method and a comparative method.
- Precision: To confirm acceptable within-run, between-run, and operator variance.
- Reportable Range: To confirm the acceptable upper and lower limits of the test system.
- Reference Range: To confirm the normal result for the tested patient population.
Application Notes and Protocols
This section provides detailed, practical guidance for designing and executing method verification studies in a microbiological context, with a specific focus on sample size considerations.
Sample Size Determination for Verification Studies
The following table summarizes the typical sample size requirements for verifying key parameters of qualitative and semi-quantitative microbiological assays, as derived from CLIA standards and best practices [3].
Table 2: Sample Size Guidance for Verification of Qualitative/Semi-Quantitative Assays
| Performance Characteristic | Minimum Sample Number | Sample Type and Distribution | Statistical Analysis |
|---|---|---|---|
| Accuracy | 20 isolates | Combination of positive and negative samples for qualitative assays; range from high to low values for semi-quantitative assays [3]. | (Number of results in agreement / Total number of results) × 100 |
| Precision | 2 positive and 2 negative, tested in triplicate for 5 days by 2 operators [3] | Controls or de-identified clinical samples. If system is fully automated, user variance testing may not be needed. | (Number of results in agreement / Total number of results) × 100 |
| Reportable Range | 3 samples | Known positive samples for qualitative assays; samples near upper and lower cutoff values for semi-quantitative assays [3]. | Verification that results fall within the established reportable range. |
| Reference Range | 20 isolates | De-identified clinical or reference samples representing the laboratory's typical patient population [3]. | Verification that results align with the expected reference range. |
Experimental Protocol for a Microbiological Method Verification
This protocol outlines the steps for verifying a qualitative microbiological test, such as a PCR assay for a specific pathogen.
Objective: To verify that the laboratory can successfully implement a commercial, FDA-cleared PCR test for Listeria monocytogenes in environmental samples, achieving performance metrics consistent with the manufacturer's claims.
Scope: Applicable to the verification of accuracy, precision, reportable range, and reference range prior to the implementation of the new test for routine use.
Materials and Reagents:
- Commercial Test Kit: Includes all necessary reagents, primers, probes, and controls.
- Reference Materials: Known positive and negative control strains from a recognized culture collection (e.g., ATCC).
- Clinical Samples: De-identified residual environmental sponge samples, previously characterized using a validated method.
- Equipment: Real-time PCR instrument, DNA extraction system, microbiological incubator, and biosafety cabinet.
- Culture Media: Appropriate enrichment and plating media as specified by the test method.
Procedure:
- Verification of Accuracy:
- Obtain 20 well-characterized isolates or samples. This should include 10 positive samples (various Listeria species and other relevant bacteria to challenge specificity) and 10 negative samples.
- Test all samples using the new PCR method according to the manufacturer's instructions.
- Compare the results to those obtained from the reference method or known characterization.
- Calculate the percent agreement. The result must meet or exceed the manufacturer's stated claims or a laboratory-defined minimum (e.g., ≥95%).
Verification of Precision:
- Select 2 positive and 2 negative samples (e.g., control strains or spiked samples).
- Two trained analysts will each test these samples in triplicate, over three non-consecutive days (total of 36 data points).
- Ensure runs include all required quality controls.
- Calculate the percent agreement for within-run, between-run, and between-analyst comparisons. Results should meet pre-defined acceptance criteria for consistency.
Verification of Reportable Range:
- Test a minimum of 3 samples with known concentrations near the assay's limit of detection to confirm the lower reportable limit.
- For the upper limit, test a high-titer positive sample to ensure the result is correctly reported as "detected" without inhibition.
- All results should fall within the "Detected" or "Not detected" parameters as expected.
Verification of Reference Range:
- Test 20 samples that are known to be negative for Listeria monocytogenes from the laboratory's typical environmental monitoring program.
- All 20 samples should be reported as "Not detected," confirming the manufacturer's stated reference range is applicable to the laboratory's patient (or sample) population.
Acceptance Criteria: All calculated performance characteristics (accuracy, precision) must meet or exceed the specifications provided in the test kit's package insert or the laboratory's pre-defined acceptance criteria based on CLIA director approval [3].
Workflow and Decision Pathways
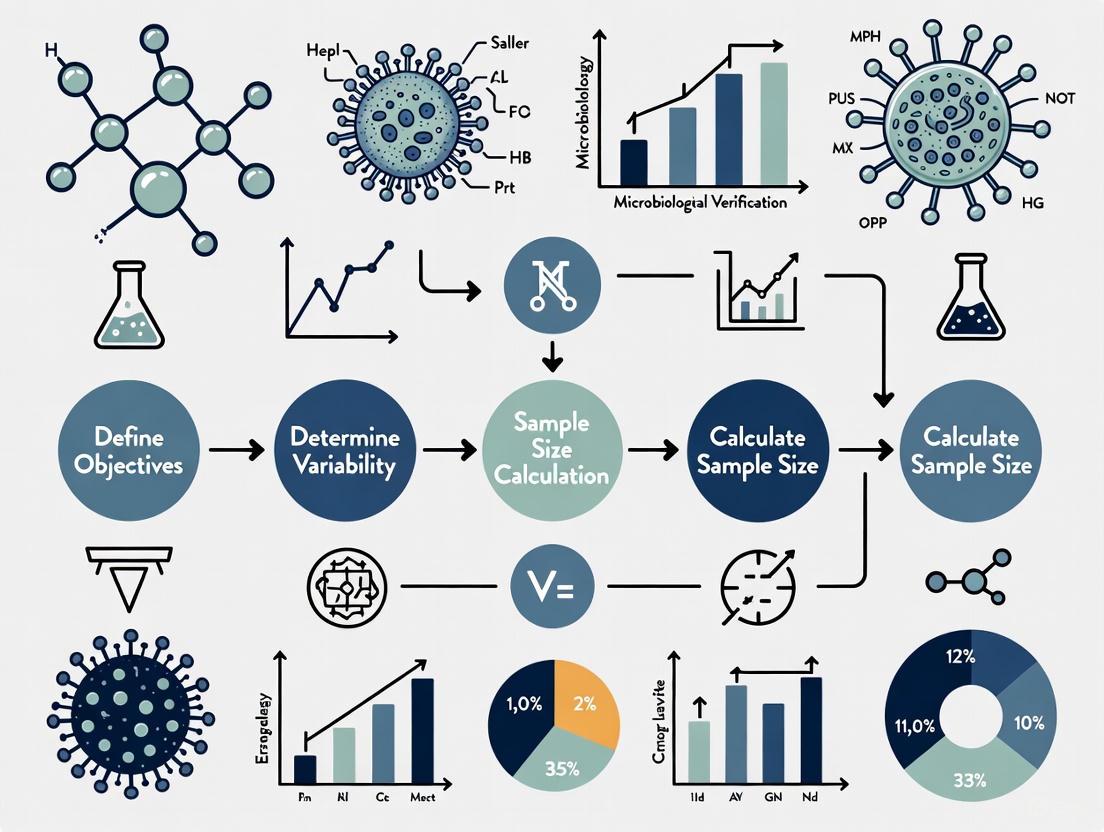
The following diagram illustrates the logical decision process for determining whether a method requires validation or verification, and the key steps involved in the verification workflow.
The Scientist's Toolkit: Research Reagent Solutions
Successful execution of method verification studies relies on high-quality, traceable materials. The following table lists essential reagents and their critical functions.
Table 3: Essential Reagents for Microbiological Method Verification
| Reagent/Material | Function and Importance |
|---|---|
| Certified Reference Strains | Well-characterized microbial strains from collections like ATCC or NCTC. Used as positive controls and for spiking experiments to establish accuracy and precision. |
| Molecular Grade Water | Ultra-pure, nuclease-free water used in molecular assays (e.g., PCR) to prevent inhibition or degradation of sensitive reactions, ensuring robust and reproducible results. |
| Quality Control (QC) Strains | Strains with known reactivity patterns used in daily QC to monitor the consistent performance of the test system post-implementation. |
| Inhibitor Controls | Specifically designed controls (e.g., internal amplification controls in PCR) to detect the presence of substances in a sample that may interfere with the test, ensuring result validity. |
| Selective and Non-Selective Enrichment Media | Broths and agars used to cultivate target microorganisms from samples. Critical for ensuring the method's ability to recover stressed or low-level contaminants. |
In microbiological method verification research, robust statistical planning is the cornerstone of generating reliable, defensible, and scientifically valid data. Calculating an appropriate sample size is not merely a procedural step; it is a critical methodological decision that protects against both false positives and false negatives, ensuring efficient use of resources and upholding ethical standards in scientific research [7]. An underpowered study, due to an insufficient sample size, risks failing to detect true effects of a new microbiological method, potentially causing valuable innovations to be abandoned. Conversely, an excessively large sample size wastes resources, can cause ethical problems by involving more test materials than necessary, and delays the completion of research activities [7] [8].
This Application Note demystifies the triad of statistical concepts—Power, Confidence, and Effect Size—that govern sample size calculation. We frame these concepts specifically within the context of microbiological method verification and validation, guided by standards such as the ISO 16140 series [9]. The protocols and tools provided herein will enable researchers, scientists, and drug development professionals to build statistically sound sampling plans that meet rigorous scientific and regulatory expectations.
Theoretical Foundations
Interrelated Concepts in Sample Size Estimation
The determination of sample size is governed by the interplay between several key statistical parameters. Understanding these relationships is crucial for designing a valid verification study. The core concepts include:
Type I Error (α) and Confidence Level: A Type I error (or false positive) occurs when the null hypothesis (H₀) is incorrectly rejected, meaning one concludes there is an effect or difference when none exists in the population [7] [8]. The probability of committing a Type I error is denoted by alpha (α). The Confidence Level, defined as (1-α), expresses the degree of certainty that the true population parameter lies within the calculated confidence interval. A standard α of 0.05 corresponds to a 95% confidence level, indicating a 5% risk of a false positive [7] [8].
Type II Error (β) and Statistical Power: A Type II error (or false negative) occurs when the null hypothesis is incorrectly retained, meaning a true effect or difference is missed [7] [8]. The probability of this error is beta (β). Statistical Power, defined as (1-β), is the probability that the test will correctly reject a false null hypothesis—that is, detect a true effect. The ideal power for a study is conventionally set at 0.8 (or 80%), meaning the study has an 80% chance of detecting an effect of a specified size if it truly exists [7] [8]. There is a delicate balance to be maintained between the risks of Type I and Type II errors.
Effect Size (ES): The Effect Size is a quantitative measure of the magnitude of a phenomenon or the strength of the relationship between two variables. In method verification, this could represent the minimum difference in detection capability between a new method and a reference method that is considered scientifically or clinically important [7]. Unlike the P-value, the ES is independent of sample size and provides a more practical indication of a finding's real-world significance. Larger effect sizes are easier to detect with smaller samples, while detecting small effect sizes requires larger sample sizes [7] [8].
P-Value: The P value is the obtained statistical probability of incorrectly accepting the alternate hypothesis. It is compared against the pre-defined alpha level to determine statistical significance. If the P value is at or lower than alpha, the alternative hypothesis (H₁) is accepted [7] [8].
The logical and mathematical relationships between these concepts, leading to sample size calculation, are visualized in the following workflow:
Error Types and Their Consequences in Microbiology
The concepts of Type I and Type II errors have direct, practical implications in a microbiology quality control setting. The following table summarizes these errors, their probabilities, and their real-world impact:
Table 1: Types of Statistical Errors in Microbiological Method Assessment
| Error Type | Statistical Description | Probability | Consequence in Microbiological Context | Example in Method Verification |
|---|---|---|---|---|
| Type I Error (False Positive) | Incorrectly rejecting a true null hypothesis (H₀) [7] [8] | α (Typically 0.05) [7] [8] | Concluding a new method is different from or superior to a reference method when it is not. | Adopting an alternative method that appears more sensitive but is not, leading to unnecessary cost and potential false failure rates. |
| Type II Error (False Negative) | Incorrectly failing to reject a false null hypothesis (H₀) [7] [8] | β (Often 0.20) [7] [8] | Concluding a new method is equivalent to a reference method when it is truly different or inferior. | Failing to identify a loss of detection capability in a new rapid method, potentially allowing contaminated products to be released. |
Practical Application & Experimental Protocols
Sample Size Calculation Formulas for Common Scenarios
The formulas for calculating sample size vary depending on the study design and the nature of the data. The table below summarizes key formulas relevant to microbiological method verification and related research.
Table 2: Sample Size Calculation Formulas for Common Research Methods [7] [8]
| Study Type | Formula | Variable Explanations |
|---|---|---|
| Comparison of Two Proportions (e.g., detection rates) | n = [p(1-p)(Z₁₋α/₂ + Z₁₋β)²] / (p₁ - p₂)² where p = (p₁ + p₂)/2 |
p₁, p₂: proportion of event of interest (e.g., detection) for group I and group II.Z₁₋α/₂: 1.96 for alpha 0.05.Z₁₋β: 0.84 for power 0.80. |
| Comparison of Two Means (e.g., colony counts) | n = [2σ² (Z₁₋α/₂ + Z₁₋β)²] / d² |
σ: pooled standard deviation from previous studies.d: clinically or technically meaningful difference between the means of 2 groups.Z values as above. |
| Validation of Sensitivity/Specificity | n = [Z₁₋α/₂² * P(1-P)] / d² |
P: expected sensitivity or specificity.d: allowable error (precision) for the estimate. |
For non-parametric tests or complex risk-based scenarios, such as those used in medical device packaging validation, a binomial reliability approach is often used. This method is suitable for qualitative (pass/fail) data and incorporates confidence and reliability levels derived from a risk assessment [10].
Table 3: Minimum Sample Sizes for Zero-Failure Binomial Reliability Testing [10]
| Confidence Level | Reliability Level | Minimum Sample Size (0 failures allowed) |
|---|---|---|
| 95% | 90% | 29 |
| 95% | 95% | 59 |
| 95% | 99% | 299 |
| 90% | 95% | 45 |
| 99% | 95% | 90 |
Protocol for Sample Size Determination in Method Verification
This protocol outlines the steps for determining a statistically justified sample size for the verification of a microbiological method, aligned with the principles of ISO 16140 [9].
Protocol Title: Sample Size Determination for Microbiological Method Verification Objective: To establish a statistically sound sample size plan that provides sufficient power to demonstrate the performance of a method relative to its validation claims or a reference method. Scope: Applicable to the verification of quantitative and qualitative microbiological methods in a single laboratory.
Materials and Reagents:
- Statistical Software: Tools such as G-Power, R, or other dedicated sample size calculators [7] [8].
- Pilot Data or Literature: Historical data, method validation reports, or published literature to inform variability (standard deviation) and expected effect size.
- Risk Assessment Matrix: A tool for assigning severity, occurrence, and detection ratings to justify confidence and reliability levels [10].
Procedure:
Define the Hypothesis and Objective:
- Clearly state the null hypothesis (H₀), e.g., "There is no difference in the detection rate between the new method and the reference method."
- State the alternative hypothesis (H₁), e.g., "The new method has a detection rate that is non-inferior to the reference method."
Select Statistical Parameters:
- Set the Significance Level (α): Typically 0.05 for a 95% confidence level [7] [8].
- Set the Statistical Power (1-β): Typically 0.80 or 80% [7] [8]. For higher-stakes verifications, a power of 0.90 may be chosen.
- Determine the Effect Size (ES): This is the most critical and often challenging step.
- For quantitative data (e.g., mean colony counts), the ES is the smallest difference (d) you need to detect, relative to the expected variability (σ). Use pilot data or a literature review to estimate σ.
- For qualitative data (e.g., presence/absence), the ES is the minimum difference in proportions (e.g., detection rates) that is considered microbiologically significant.
- If no prior data exists, use a conservative (larger) estimate for variability or consult a statistician.
Choose the Appropriate Statistical Test:
- Based on your objective and data type, select the test (e.g., comparison of two proportions, comparison of two means, reliability demonstration). Refer to Table 2 for corresponding formulas.
Calculate the Sample Size:
- Use the formula from Table 2 corresponding to your chosen test, inputting your selected α, power, and effect size.
- Alternatively, use statistical software, which often provides a more user-friendly interface for these calculations. For risk-based attribute data, use the zero-failure binomial sample sizes in Table 3 as a starting point, justified by a Risk Priority Number (RPN) [10].
Document and Justify:
- The final sample size and the complete rationale behind the chosen parameters (α, power, ES, and the source of variability estimates) must be documented in the study protocol.
The Scientist's Toolkit: Essential Reagents and Materials
Table 4: Key Research Reagent Solutions for Microbiological Method Verification
| Item | Function/Application in Verification Studies |
|---|---|
| Reference Strains | Well-characterized microorganisms from culture collections (e.g., ATCC) used as positive controls to ensure method performance and reproducibility [11]. |
| Facility Isolates | Environmental or process isolates representative of the actual microbial population in the production facility; used to challenge the method with relevant strains [11]. |
| Selective and Non-Selective Media | Used for the recovery and enumeration of challenge microorganisms; recovery must be demonstrated for the specific product category [11]. |
| Neutralizing Agents | Inactivates antimicrobial properties of the product or method to ensure accurate microbial recovery and prevent false negatives. |
| Statistically Justified Sample Size | The foundational "reagent" determined by this protocol; ensures the experimental data generated is reliable, reproducible, and scientifically defensible [7] [10]. |
Concluding Remarks
The rigorous application of statistical power, confidence, and effect size principles is non-negotiable in modern microbiological research and drug development. Moving beyond the arbitrary selection of sample sizes to a calculated, justified approach strengthens the validity of your method verification data, ensures regulatory compliance, and makes efficient use of valuable resources. By integrating these statistical tools into the experimental planning phase, as outlined in this document, scientists and researchers can produce higher-quality, more reliable data that truly demonstrates the fitness-for-purpose of their microbiological methods.
In microbiological research and drug development, the validity of any study hinges on the integrity of its sample size calculation. An incorrectly sized sample—whether too small or excessively large—undermines the entire scientific process, leading to either undetected hazards (false negatives) or significant resource waste. Within the framework of method verification and validation, establishing a sample plan is a foundational step that determines the power of a study to detect true effects and the reliability of its conclusions [12].
The core challenge lies in balancing vigilance with practicality. Inadequate sample sizes fail to capture the true microbial profile of a batch, allowing contaminated products to go undetected and posing serious risks to public health [12]. Conversely, excessively large samples strain time, personnel, and financial resources without a commensurate improvement in detection probability, making quality control processes unsustainable [12]. This application note details the consequences of incorrect sample sizing and provides structured protocols to empower researchers in designing defensible, efficient microbiological studies.
Quantitative Impact of Sample Size on Sampling Plan Performance
The performance of a microbiological sampling plan is mathematically described by its Operating Characteristic (OC) curve, which plots the probability of accepting a batch against the true proportion of defective samples [13]. The shape and accuracy of this curve are profoundly influenced by the chosen sample size.
The False Negative Problem: Undetected Contamination
A sampling plan with an insufficient sample size will have an OC curve shifted to the right, meaning the probability of accepting a batch remains high even when the contamination level is unacceptable [13]. This occurs because a small sample has a low probability of including contaminated units, especially when contamination is heterogeneous.
For example, if 1% of units in a batch are contaminated, a sample size of 299 units is required to have 95% confidence ((Prej = 0.95)) in detecting the problem [13]. A smaller sample size drastically reduces this detection probability. Furthermore, the sensitivity of the test method itself—the probability of correctly identifying a contaminated sample—exacerbates this issue. Low sensitivity increases false negatives, further shifting the OC curve to the right and reducing the probability of batch rejection [13].
Table 1: Sample Sizes Needed for 95% Confidence in Detecting Contamination
| Contamination Rate (Pdef) | Required Sample Size (n) | Calculation (Approx. 3/Pdef) |
|---|---|---|
| 1% (1 in 100) | 299 | 300 |
| 5% (1 in 20) | 59 | 60 |
| 10% (1 in 10) | 29 | 30 |
The Resource Waste Problem: False Positives and Economic Cost
While less dangerous than false negatives, false positives generated by poor sampling plans lead to significant resource waste. A low specificity (the probability of correctly identifying a non-contaminated sample) means actual negative samples are tested positive [13]. This moves the OC curve to the left, increasing the rejection rate of batches that are, in fact, acceptable [13].
The economic impact is multifaceted:
- Wasted Product: Rejection of safe batches results in direct financial loss.
- Unnecessary Labor: Time and effort are invested in follow-up testing, root-cause analysis, and disposal procedures.
- Operational Disruption: Production schedules are halted unnecessarily.
The effect of specificity is particularly severe in sampling plans with larger sample sizes, where it "should be much larger than 0.99 to have a reasonable performance" [13]. This highlights the critical interplay between statistical power and analytical method quality.
Consequences of Incorrect Sample Sizes
Scientific and Safety Consequences
- Inaccurate Method Validation: Method verification and validation require a clear understanding of a method's performance characteristics (specificity, sensitivity, reproducibility) [14] [9]. An incorrect sample size during validation jeopardizes this understanding, leading to the implementation of a method whose true limitations are unknown.
- Undetected Microbial Hazards: As shown in Table 1, small samples cannot reliably detect low-prevalence pathogens. This is catastrophic in drug development and food safety, where virulent pathogens pose a direct threat to consumer health [12] [13].
- Erosion of Scientific Credibility: Results from an underpowered study are not defensible to the scientific, regulatory, or legal communities [14]. In microbial forensics, this can "seriously impact the course or focus of an investigation, thus affecting the liberties of individuals" [14].
Operational and Resource Consequences
- Inefficient Resource Allocation: Oversampling consumes materials, reagents, and analyst time that could be deployed more effectively elsewhere in the R&D pipeline [12].
- Increased Cost of Quality Control: The direct costs of consumables and indirect costs of personnel time skyrocket with excessively large routine sampling plans, making the quality control process inefficient and unsustainable [12].
Protocols for Determining Sample Size in Method Verification
A robust, risk-based approach is essential for determining the correct sample size. The following protocol aligns with principles from international standards [9] and applied microbiology [12].
Protocol 1: Risk-Based Sample Plan Development
Objective: To establish a sampling plan frequency and size based on a scientific assessment of risk. Applications: Environmental monitoring, raw material testing, finished product release testing.
Conduct a Risk Assessment:
- Identify critical control points and potential microbial hazards in the process [12].
- Consider factors such as the susceptibility of ingredients to contamination, complexity of processing steps, and historical data from past contamination incidents [12].
- Example: In a vegetable factory, leafy greens are higher risk due to raw consumption and exposure to soil, warranting a more intensive sample plan [12].
Define the Scope and Objectives:
- Clearly state the purpose of testing (e.g., detection of a specific pathogen, enumeration of a spoilage organism).
- Define the statistical confidence required (e.g., 95% confidence) and the level of contamination that must be detected [13].
Determine Sampling Frequency and Size:
- Use the risk assessment to set frequencies. High-risk areas (e.g., raw material intake) require more frequent sampling than lower-risk areas (e.g., finished product storage) [12].
- Employ statistical techniques (e.g., random sampling, stratified sampling) to determine a sample size that accurately represents the batch and can detect the target contamination level with the required confidence [12]. Refer to formulas such as ( n = \frac{log(0.05)}{log(1-Pdef)} ) for qualitative testing [13].
Select and Validate Methodology:
The following workflow visualizes this risk-based protocol:
Protocol 2: Verification of Sample Plan Effectiveness
Objective: To verify that an implemented sampling plan performs as expected, particularly concerning the impact of method sensitivity and specificity. Applications: Verification of any new or revised sampling plan before full implementation.
Model the OC Curve:
- Using the formula ( P{accept} = (1 - P{def})^n ) for perfect tests, model the ideal OC curve for your sample size (n) and a range of defect rates (Pdef) [13].
- This represents the best-case performance.
Adjust for Method Imperfection:
- Calculate the practical probability of detection ((P{det})) that accounts for test method performance: ( P{det} = sens \times P{def} + (1 - spec) \times (1 - P{def}) ) [13], where
sensis sensitivity andspecis specificity. - Model the actual OC curve using this adjusted (P_{det}) value.
- Calculate the practical probability of detection ((P{det})) that accounts for test method performance: ( P{det} = sens \times P{def} + (1 - spec) \times (1 - P{def}) ) [13], where
Compare and Interpret Curves:
- A significant left-shift in the OC curve (lower acceptance) indicates false positives are likely due to low specificity, which will waste resources [13].
- A significant right-shift (higher acceptance) indicates false negatives are likely due to low sensitivity, which creates safety risks [13].
- Use this analysis to refine the sample size or select a more accurate test method.
The Scientist's Toolkit: Essential Reagents and Materials
The following reagents and materials are fundamental for executing microbiological sampling and analysis as part of a verified method.
Table 2: Key Research Reagent Solutions for Microbiological Sampling
| Item | Function | Key Consideration |
|---|---|---|
| Selective & Non-selective Media | Supports the growth of target microorganisms while inhibiting non-targets. Essential for detection and enumeration. | Must be validated for the specific food matrix and target microbe to ensure recovery [12]. |
| Enrichment Broths | Amplifies low numbers of target pathogens to detectable levels. | Composition and incubation conditions are critical for sensitivity and must be optimized [15]. |
| Molecular Detection Reagents (e.g., PCR mixes, primers, probes) | Provides high specificity and sensitivity for confirming the identity of microorganisms [9]. | Requires rigorous validation of inclusivity and exclusivity to avoid false positives/negatives [9]. |
| Sample Diluents & Neutralizers | Prepares the sample for analysis and neutralizes residual antimicrobial agents or inhibitors present in the sample matrix. | Vital for obtaining representative and reliable results by ensuring microbial recovery is not biased [12]. |
| Reference Strains & Controls | Serves as positive and negative controls for validating method performance (specificity, sensitivity) during verification [14] [9]. | Use of certified reference materials is necessary for defensible and accurate verification. |
Determining the correct sample size is a critical, non-negotiable component of microbiological method verification. It is a balancing act that demands a scientific, risk-based approach. Under-sizing samples leads to a dangerous inability to detect contaminants, compromising product safety and public health. Over-sizing leads to unsustainable inefficiencies and wasted resources without a meaningful improvement in safety. By employing the structured protocols and understanding the quantitative relationships outlined in this document, researchers and drug development professionals can design defensible sampling plans that are both effective and efficient, thereby ensuring the reliability of their methods and the safety of their products.
The ISO 16140 series of International Standards provides standardized protocols for the validation and verification of microbiological methods in the food and feed chain. This series is essential for testing laboratories, test kit manufacturers, competent authorities, and food business operators to ensure that the methods they implement are fit for purpose and reliably performed within their facilities [9]. Understanding this framework is particularly crucial for research on sample size calculation, as the series defines specific requirements for the number of samples, food categories, and replicates needed for statistically sound method verification and validation studies.
The series has been developed to address the need for a common validation protocol for alternative (often proprietary) methods, providing a basis for their certification and enabling informed choices about their implementation [9]. The standards under the ISO 16140 umbrella each address distinct aspects of the method approval process, creating a comprehensive ecosystem for assuring microbiological data quality.
The ISO 16140 series is structured into several parts, each focusing on a specific validation or verification scenario. Table 1 summarizes the scope and application of each part.
Table 1: Parts of the ISO 16140 Series on Microbiology of the Food Chain - Method Validation
| Standard Part | Title | Scope and Primary Application |
|---|---|---|
| ISO 16140-1 | Vocabulary | Defines terms used throughout the series [9]. |
| ISO 16140-2 | Protocol for the validation of alternative (proprietary) methods against a reference method | The base standard for validating alternative methods, involving a method comparison study and an interlaboratory study [9]. |
| ISO 16140-3 | Protocol for the verification of reference methods and validated alternative methods in a single laboratory | Describes how a laboratory demonstrates its competence in performing a previously validated method [9] [16]. |
| ISO 16140-4 | Protocol for method validation in a single laboratory | Addresses validation studies conducted within a single lab, the results of which are not transferred to other labs [9]. |
| ISO 16140-5 | Protocol for factorial interlaboratory validation for non-proprietary methods | Used for non-proprietary methods requiring rapid validation or when a full interlaboratory study isn't feasible [9]. |
| ISO 16140-6 | Protocol for the validation of alternative (proprietary) methods for microbiological confirmation and typing procedures | Validates methods for confirming presumptive results or for typing strains (e.g., serotyping) [9]. |
| ISO 16140-7 | Protocol for the validation of identification methods of microorganisms | Validates methods for identifying microorganisms (e.g., using PCR or mass spectrometry) where no reference method exists [9]. |
The relationships between these standards, especially when moving from method validation to routine laboratory use, can be visualized in the following workflow. This is critical for understanding where sample size calculations apply in the method lifecycle.
Distinction Between Method Validation and Verification
A fundamental concept within the ISO 16140 framework is the clear distinction between method validation and method verification. These are two sequential stages required before a method can be used routinely in a laboratory [9].
Method Validation is the first stage, which proves that a method is fit for its intended purpose. It characterizes the method's performance against defined criteria, such as its detection limit, accuracy, and specificity. As shown in the diagram, validation can follow different pathways (e.g., ISO 16140-2, -4, -5, -7) depending on the method type and scope of application. For instance, ISO 16140-2 involves an extensive interlaboratory study to generate performance data that is recognized broadly [9]. This stage is typically conducted by method developers or independent validation bodies.
Method Verification is the second stage, where a laboratory demonstrates that it can competently perform a method that has already been validated. It answers the question: "Can we achieve the performance characteristics claimed in the validation study in our lab, with our personnel and equipment?" [9] [16]. This process, detailed in ISO 16140-3, is a requirement for laboratories accredited to ISO/IEC 17025 and is considered a best practice for all testing facilities [16].
Detailed Experimental Protocols for Method Verification (ISO 16140-3)
For researchers designing verification studies, ISO 16140-3:2021 outlines a structured two-stage process for laboratories to verify a method they intend to implement.
Two-Stage Verification Process
The verification process under ISO 16140-3 is divided into two distinct stages:
Implementation Verification: The purpose is to demonstrate that the user laboratory can perform the method correctly. This is achieved by testing a food item that was already used in the original validation study and showing that the laboratory can obtain comparable results. This confirms that the laboratory's execution of the method is fundamentally sound [9].
Food Item Verification: The purpose is to demonstrate that the method performs satisfactorily for the specific, and potentially challenging, food items that the laboratory tests routinely. This is done by testing several such food items and confirming that the method's performance meets defined characteristics for them [9].
Sample and Food Category Considerations
A critical aspect of designing a verification study is the selection of food categories and items, which directly impacts sample size calculations. The validation of a method often covers a defined scope of food categories.
ISO 16140-2 defines a list of food categories (e.g., heat-processed milk and dairy products). A method validated using a minimum of five different food categories is considered validated for a "broad range of foods," which covers 15 defined categories [9]. This concept is vital for scoping verification work. When a laboratory conducts a verification study, it must select food items that fall within the method's validated scope and are also relevant to the laboratory's own testing needs [9].
Table 2: Key Concepts for Sample Planning in Verification and Validation
| Concept | Description | Implication for Sample Size |
|---|---|---|
| Food Category | A group of sample types of the same origin (e.g., heat-processed milk and dairy products) [9]. | Validation studies often use 5 categories to represent a "broad range" of foods [9]. |
| Food Item | A specific product within a food category (e.g., UHT milk within the "heat-processed milk" category). | Verification requires testing specific items relevant to the lab's scope [9]. |
| Implementation Verification | Testing a food item used in the original validation study [9]. | Requires at least one food item. |
| Food Item Verification | Testing challenging food items from the lab's own scope [9]. | Requires several food items; specific numbers are defined in the standard. |
| Inoculum Level | The number of microorganisms introduced into a test sample. | Low-level inoculation (e.g., near the method's detection limit) is often used to challenge the method [11]. |
Regarding low-level inocula, it is important to note that microbial distribution at low concentrations follows a Poisson distribution rather than a normal distribution. This means that with a target of, for example, 10 CFU, there is a significant probability that an individual aliquot may contain more or fewer cells than intended. This variability must be accounted for in the experimental design, potentially by increasing replicate numbers [11] [17].
The Scientist's Toolkit: Key Reagents and Materials
The successful execution of methods under the ISO 16140 framework requires specific, high-quality reagents and materials. The following table details essential components for microbiological method verification and validation studies.
Table 3: Key Research Reagent Solutions for Microbiological Method Testing
| Reagent / Material | Function and Importance in Validation/Verification |
|---|---|
| Reference Method Materials | Materials specified by the standardized reference method (e.g., ISO 6579-1 for Salmonella). Serves as the benchmark against which an alternative method is validated [18]. |
| Alternative Method Kits | Proprietary test kits (e.g., iQ-Check EB, Petrifilm BC Count Plate). The object of the validation study to prove performance equivalence or superiority [18]. |
| Culture Media | Used for cultivation of microorganisms. Must be validated to support growth of fastidious organisms; factors like pH, ionic strength, and nutrient composition are critical. Handling (e.g., reheating) must be standardized [17]. |
| Reference Strains | Well-characterized strains from culture collections (e.g., ATCC). Used as indicator organisms to demonstrate a medium's ability to support growth and to challenge the method's detection capability [11] [17]. |
| Facility Isolates | Microbial strains isolated from the local manufacturing or testing environment. Should be included in verification studies to ensure the method detects relevant contaminants [17]. |
| Selective Agars | Agar media used for the isolation and confirmation of specific microorganisms. Validation of confirmation methods (ISO 16140-6) is tied to the specific agars used in the study [9]. |
| Inactivation Agents | Used to neutralize inhibitory substances in a sample (e.g., antimicrobial residues). Their performance must be validated to ensure they do not harm target microorganisms and effectively neutralize inhibitors [17]. |
Defining the scope of a microbiological method verification study is a critical first step that directly influences the experimental design, sample size calculations, and ultimate validity of the research findings. This document establishes frameworks for selecting appropriate food categories and target microorganisms, ensuring verification studies are conducted with scientific rigor and regulatory compliance. The principles outlined here are framed within the context of microbiological method verification as defined in the ISO 16140 series, which provides standardized protocols for laboratories validating alternative methods against reference methods [9].
The scope of validation directly informs verification activities in a laboratory. When a method has been validated for a "broad range of foods" (typically across 15 defined food categories using a minimum of 5 categories during validation), it is expected to perform reliably across all similar matrices within those categories [9]. Understanding this relationship between validation scope and verification requirements is essential for designing efficient yet comprehensive verification studies with appropriate sample sizes.
Food Categorization Framework
ISO 16140 Food Categories
The ISO 16140-2 standard defines 15 primary categories of food and feed samples that form the basis for validation and verification studies [9]. These categories group sample types of similar origin and characteristics, providing a systematic framework for method evaluation. When a method is validated using a minimum of 5 different food categories, it is considered validated for a "broad range of foods" encompassing all 15 categories [9].
Table 1: ISO 16140 Food Categories for Method Validation and Verification
| Category Number | Description | Example Matrices |
|---|---|---|
| 1 | Meat and meat products | Raw meats, cured meats, paté |
| 2 | Fish and fish products | Fresh fish, shellfish, smoked fish |
| 3 | Fruits and vegetables | Fresh produce, salads, juices |
| 4 | Egg and egg products | Whole eggs, powdered eggs, egg-based products |
| 5 | Milk and milk products | Raw milk, cheese, yogurt, butter |
| 6 | Cereals and cereal products | Flour, bread, pasta, breakfast cereals |
| 7 | Confectionery | Chocolate, candies, chewing gum |
| 8 | Nuts, nut products, and seeds | Whole nuts, nut butters, sunflower seeds |
| 9 | Sugars and sugar products | Honey, syrups, molasses |
| 10 | Fermented foods and beverages | Beer, wine, sauerkraut, tempeh |
| 11 | Spices and seasonings | Dried herbs, spice blends, condiments |
| 12 | Food supplements | Probiotic supplements, vitamin formulations |
| 13 | Water | Bottled water, process water |
| 14 | Other foods | Prepared meals, composite dishes |
| 15 | Animal feed | Pet food, livestock feed, ingredients |
Additional Category Considerations
Beyond the 15 primary food categories, validation and verification studies may incorporate supplementary categories including pet food and animal feed, environmental samples from food or feed production environments, and primary production samples [9]. The overlap between validation scope, method scope, and laboratory application scope must be carefully considered when designing verification studies, as illustrated in ISO 16140-3, Figure 3 [9].
Target Microorganisms Selection
Microorganisms of Public Health Significance
Selection of target microorganisms should be driven by the method's intended application and regulatory requirements. Pathogens of concern vary by food category and may include Salmonella spp., Listeria monocytogenes, Escherichia coli O157:H7, and Cronobacter species, particularly in infant formula products [18].
Indicator Organisms and Spoilage Microorganisms
Beyond pathogens, verification studies often include indicator organisms that signal potential contamination or assess general microbiological quality. Recent method certifications have focused on microorganisms such as:
- Enterobacteriaceae: Detection methods validated for infant formula, infant cereals, and related ingredients [18]
- Total Bacterial Count: Quantitative methods for raw milk testing [18]
- Bacillus cereus: Enumeration methods in various food matrices [18]
- Yeast and Mold: Enumeration methods for various food products [18]
Experimental Design and Protocols
Two-Stage Verification Protocol
ISO 16140-3 specifies two distinct stages for verification of validated methods [9]:
Stage 1: Implementation Verification
- Purpose: Demonstrate that the user laboratory can perform the method correctly
- Protocol: Test one of the same food items evaluated in the validation study
- Acceptance Criteria: Obtain results similar to those from the validation study
Stage 2: Food Item Verification
- Purpose: Demonstrate that the user laboratory is capable of testing challenging food items within the laboratory's scope of accreditation
- Protocol: Test several challenging food items using defined performance characteristics
- Acceptance Criteria: Confirm the method performs well for these food items
Sample Size Considerations
The appropriate sample size for verification studies depends on several factors:
- Scope of Validation: Methods validated for a "broad range" (5+ categories) may require fewer samples per category
- Laboratory Scope: The specific food matrices routinely tested by the laboratory
- Statistical Power: The desired confidence level for detecting significant differences between methods
- Regulatory Requirements: Specific sample size mandates for certain food-pathogen combinations
Table 2: Method Verification Examples and Characteristics
| Validated Method | Target Microorganism | Food Categories | Test Portion | Reference Method |
|---|---|---|---|---|
| iQ-Check EB | Enterobacteriaceae | Infant formula, infant cereals | Up to 375g | ISO 21528-2 |
| Petrifilm Bacillus cereus | Bacillus cereus | Various food categories | Standard method | ISO 7932:2004 |
| One Plate Yeast & Mould | Yeasts and moulds | Various food categories | Standard method | ISO 21527:2008 |
| InviScreen Salmonella | Salmonella spp. | Various food categories | Standard method | ISO 6579-1:2017 |
| Autof ms1000 | Confirmation of bacteria, yeasts, molds | Various agar media | Isolated colonies | Reference identification methods |
Research Reagent Solutions
Table 3: Essential Research Reagents for Microbiological Method Verification
| Reagent Category | Specific Examples | Function in Verification Studies |
|---|---|---|
| Alternative proprietary methods | iQ-Check EB, Petrifilm plates, Soleris NF-TVC | Demonstrate comparable performance to reference methods |
| Reference culture strains | ATCC strains, NCTC strains | Provide known positive controls for target microorganisms |
| Selective agar media | XLD Agar, Chromogenic media | Isolate and identify target microorganisms from food matrices |
| Molecular detection kits | foodproof Salmonella Detection Kit, InviScreen Salmonella spp. Detection Kit | Detect target pathogens using DNA-based methods |
| Sample preparation reagents | foodproof StarPrep One Kit, foodproof Magnetic Preparation Kit | Extract and purify microbial DNA from food samples |
| Confirmation systems | Autof ms1000 (MALDI-TOF) | Confirm identity of isolated colonies using mass spectrometry |
Workflow Visualization
From Theory to Practice: A Step-by-Step Guide to Sample Size Calculation
In microbiological method verification, the foundation of a robust experimental design is the precise definition of the primary outcome and the establishment of a statistically justified level of precision. This initial step determines the validity, reproducibility, and regulatory acceptance of the method. A clearly articulated outcome, coupled with a pre-specified precision threshold, directly informs the sample size calculation, ensuring the study is sufficiently powered to detect meaningful effects or demonstrate equivalence. This protocol provides a structured framework for researchers and scientists in drug development to execute this critical first step.
Core Concepts and Definitions
Primary Outcome
The primary outcome is the single most important variable, or endpoint, that the method verification study is designed to assess. It must be a specific, measurable, and unambiguous characteristic that directly reflects the method's performance.
Characteristics of a Well-Defined Primary Outcome:
- Specific: Precisely defined, leaving no room for interpretation.
- Measurable: Quantifiable using a reliable and validated technique.
- Relevant: Directly related to the objective of the microbiological method.
- Pre-specified: Defined before any data collection commences to avoid bias.
Acceptable Precision (Margin of Error)
The acceptable precision, often expressed as the margin of error (E), is the maximum tolerable difference between the point estimate derived from your sample data and the true population parameter. It represents the clinical or practical significance threshold. In method verification, this is the pre-defined limit within which the method's results are considered acceptable for their intended purpose. A smaller margin of error requires a larger sample size to achieve greater certainty.
Experimental Protocol: Defining Parameters for Sample Size Calculation
Purpose and Scope
This protocol outlines the procedure for formally defining the primary outcome and acceptable precision for a microbiological method verification study, which are critical inputs for subsequent sample size calculations.
Materials and Equipment
- Study protocol document
- Statistical software (e.g., R, SAS, PASS, nQuery)
- Relevant regulatory guidance documents (e.g., USP, ICH, CLSI)
Procedure
Step 1: Identify and Justify the Primary Outcome 1.1. Based on the method's objective (e.g., quantifying bacterial load, identifying specific pathogens, determining antimicrobial susceptibility), list all potential measurable outcomes. 1.2. Consult existing literature, regulatory guidelines, and internal stakeholder input to select the single most critical outcome. 1.3. Document a complete operational definition for the outcome, including the specific units of measurement, the measurement technology, and the sampling procedure.
Step 2: Determine the Acceptable Precision (Margin of Error, E) 2.1. Establish the margin of error based on one of the following, listed in order of preference: * Regulatory Standards: Use predefined limits from pharmacopeial standards (e.g., USP) or other regulatory guidance. * Clinical or Practical Significance: Define the smallest change or difference in the outcome that would be meaningful in a real-world application. * Historical Data: Analyze data from previous, similar studies or from a pilot study to estimate variability and inform a reasonable margin. 2.2. Justify the chosen value with a clear scientific or regulatory rationale and document it in the study protocol.
Step 3: Specify the Statistical Confidence Level 3.1. Select the confidence level (1 - α) for the study. A 95% confidence level (α = 0.05) is most common in scientific research. 3.2. Document this value, as it is a key component for sample size calculation.
Step 4: Document all Parameters for Sample Size Calculation 4.1. Compile the finalized parameters into a structured table within the study protocol to ensure clarity and transparency for all team members and reviewers.
Data Analysis and Interpretation
The parameters defined in this protocol are not for immediate statistical analysis but are inputs for the sample size calculation. The subsequent statistical analysis plan will detail how the primary outcome, once measured, will be analyzed against these pre-defined precision goals.
Table 1: Defined Parameters for Sample Size Calculation in a Microbiological Method Verification Study
| Parameter | Description | Example: Bacterial Load Enumeration | Justification & Notes |
|---|---|---|---|
| Primary Outcome | The key variable being measured. | Mean log10 Colony Forming Units (CFU) per mL. | Directly measures the quantitative performance of the enumeration method. |
| Acceptable Precision (E) | The maximum tolerable margin of error. | ± 0.5 log10 CFU/mL. | Based on clinical relevance where a 0.5 log change is considered significant. |
| Confidence Level (1-α) | The probability that the confidence interval contains the true parameter. | 95% (α = 0.05). | Standard for scientific research to control Type I error. |
| Expected Standard Deviation (σ) | The anticipated variability in the data (estimated). | 0.8 log10 CFU/mL. | Estimated from a pilot study or previous similar experiments. |
Visualization of the Workflow
The following diagram illustrates the logical sequence and decision points for defining the primary outcome and establishing precision.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for Microbiological Method Verification
| Item | Function / Application |
|---|---|
| Reference Standard Strains | Certified microbial strains (e.g., from ATCC) used as positive controls to ensure method accuracy and reproducibility. |
| Culture Media | Prepared and sterilized growth substrates (e.g., Tryptic Soy Agar, Mueller-Hinton Broth) for the propagation and enumeration of microorganisms. |
| Diluents and Buffers | Sterile solutions (e.g., Phosphate Buffered Saline, Saline) used for serial dilutions of microbial suspensions to achieve countable colony ranges. |
| Antimicrobial Agents | Standard powders or disks for susceptibility testing methods, requiring precise reconstitution and storage. |
| Neutralizing Agents | Components added to dilution blanks or media to inactivate residual antimicrobial or disinfectant effects in the sample. |
| Quality Control Organisms | Specific strains used to verify the performance and sterility of each batch of culture media and reagents. |
In microbiological method verification research, establishing a statistically significant result is only the first step. Determining the practical significance of that result through effect size is what translates a finding from a mere numerical difference into a meaningful scientific conclusion. While a P-value can indicate whether an observed effect is likely real (e.g., a difference between two microbial quantification methods), it does not convey the magnitude or importance of that effect [7] [19]. Effect size quantifies this magnitude, providing a scale-independent measure of the strength of a phenomenon [19].
The accurate determination of effect size is a critical prerequisite for a robust sample size calculation. It creates a direct bridge between statistical analysis and practical application, ensuring that a study is designed to be sensitive enough to detect differences that are not only statistically real but also scientifically or clinically relevant [20]. This step is therefore foundational for avoiding both wasted resources on overpowered studies and the ethical dilemma of underpowered studies that fail to detect meaningful effects [7].
Quantifying Effect Size: Key Measures and Calculations
The choice of effect size measure depends on the type of data and the study design. The following table summarizes common effect size measures used in biomedical and microbiological research.
Table 1: Common Effect Size Measures and Their Applications
| Effect Size Measure | Data Type | Formula | Interpretation (Cohen's Guidelines) | Common Use in Microbiology |
|---|---|---|---|---|
| Cohen's d [19] | Continuous (Comparing two means) | ( d = \frac{M1 - M2}{SD_{pooled}} ) | Small: 0.2, Medium: 0.5, Large: 0.8 | Comparing mean microbial counts (e.g., CFU/mL) between a new and a reference method. |
| Pearson's r [19] | Continuous (Correlation) | - | Small: 0.1, Medium: 0.3, Large: 0.5 | Assessing the strength of a linear relationship between two quantitative measurements (e.g., optical density and cell concentration). |
| Odds Ratio (OR) [7] | Binary / Categorical | - | - | Comparing the odds of an event (e.g., detection of a pathogen) between two groups. |
| Cohen's f [21] [22] | Continuous (Comparing >2 means - ANOVA) | ( f = \sqrt{ \frac{\sum{i=1}^G \frac{Ni}{N} (\mui - \bar{\mu})^2}{\sigma{pooled}^2} } ) | - | Comparing alpha diversity metrics (e.g., Shannon entropy) across multiple sample groups or treatment conditions. |
For Cohen's d, the calculation involves the difference between two group means divided by the pooled standard deviation [19]. A d of 1 indicates the groups differ by 1 standard deviation. The formulas for comparing two means or two proportions, integral to these calculations, are well-established [7].
Determining Effect Size for Study Planning
Selecting an appropriate effect size for a sample size calculation is a critical decision. Two primary approaches guide this selection, each with distinct advantages.
Table 2: Methods for Determining Effect Size in Study Planning
| Method | Description | Application in Method Verification | Considerations |
|---|---|---|---|
| Minimum Clinically Important Difference (MCID) [20] | The smallest effect that is considered scientifically or clinically meaningful. | Defining the smallest difference in analytical performance (e.g., sensitivity, precision) that would impact the method's utility. | Anchors the study in practical significance; requires expert input and consensus. |
| Conventional Method [20] | Based on effect sizes observed in previous similar studies, pilot data, or meta-analyses. | Using data from a preliminary pilot study or published validation studies of similar methods to estimate a realistic effect. | Provides a data-driven estimate; may not reflect the specific context of the new method. |
Addressing Uncertainty in Effect Size Estimation
Effect size is rarely known with absolute certainty before a study is conducted. To manage this uncertainty, researchers should [20]:
- Perform Sensitivity Analysis: Calculate sample sizes and power for a range of plausible effect sizes (e.g., the estimated MCID, and slightly larger and smaller values) to understand how the required sample size changes.
- Consider Bayesian Assurance: This method incorporates prior knowledge and uncertainty about the effect size into the sample size calculation, leading to more robust study designs.
Experimental Protocol: Determining Effect Size for a Microbiological Study
This protocol outlines a step-by-step process for determining the effect size to be used in power analysis for a study comparing two microbiome analysis methods.
Research Reagent Solutions and Essential Materials
Table 3: Key Materials for Effect Size Determination in Microbiome Studies
| Item | Function |
|---|---|
| Large Microbiome Database (e.g., American Gut Project, FINRISK) [21] [22] | Provides a large, population-level dataset for robust effect size calculation for various metadata variables. |
| Effect Size Analysis Software (e.g., Evident, G-Power, R, Python) [8] [21] [22] | Tools to compute effect sizes (e.g., Cohen's d, f) from pilot data or large databases and to perform subsequent power analysis. |
| Pilot Study Data [7] [20] | A small-scale preliminary dataset used to estimate means, standard deviations, and prevalence for the outcomes of interest. |
Step-by-Step Workflow
The following diagram illustrates the logical workflow for determining effect size, integrating both pilot data and large public databases.
Detailed Methodology
The protocol below is adapted from the Evident workflow for power analysis in microbiome studies [21] [22].
Objective: To derive an effect size for comparing the mean α-diversity (Shannon entropy) between two independent groups (e.g., two sample types or two DNA extraction methods).
Materials and Software:
- A large microbiome dataset (e.g., from the American Gut Project) OR a pilot dataset from your specific experiment.
- Statistical software (e.g., Evident, R, Python, G*Power).
Procedure:
- Define Population and Parameter: Clearly identify the population and the key outcome variable (e.g., Shannon entropy).
- Compute Population Parameters:
- If using a large database (like AGP), calculate the average Shannon entropy (( \mui )) and the population variance (( \sigmai^2 )) for each group. With large sample sizes (( N_i )), these are considered robust estimates of the true population parameters [22].
- If using a pilot study, calculate the mean (( Mi )) and standard deviation (( SDi )) for each group from your pilot data.
- Calculate Pooled Variance: Under the assumption of homoscedasticity, compute the pooled variance (( \sigma{pooled}^2 )) by averaging the empirical variances from each group, weighted by their sample sizes [22]: ( \sigma{pooled}^2 = \frac{\sum{i=1}^G Ni \sigmai^2}{\sum{i=1}^G N_i} )
- Compute Effect Size:
- Use Effect Size in Power Analysis: Input the calculated effect size (d), along with the desired significance level (α, typically 0.05) and power (1-β, typically 0.8), into statistical software to determine the required sample size for your main study [7].
Determining the effect size is not a mere statistical formality but a fundamental exercise in scientific reasoning. By rigorously quantifying the magnitude of the effect a study is designed to detect—through either the MCID or evidence-based conventional methods—researchers ensure that their microbiological method verification is both statistically sound and practically relevant. This step guarantees that valuable resources are invested in studies capable of detecting meaningful differences, thereby strengthening the validity and impact of research outcomes in drug development and public health.
In the context of microbiological method verification, establishing acceptable error rates is a fundamental step in the sample size calculation process. This step ensures that the study is designed with a pre-defined tolerance for risk, balancing the chance of false positives against the risk of false negatives. A well-considered balance between Type I (α) and Type II (β) errors is critical for developing a robust, reliable, and scientifically defensible method. Setting these parameters is not an arbitrary exercise but a strategic decision that directly impacts the credibility of the research and the efficacy of the resulting microbiological method [7].
Defining Type I (Alpha) and Type II (Beta) Errors
Statistical hypothesis testing in method verification involves a null hypothesis (H₀), which typically states that there is no effect or no difference, and an alternative hypothesis (H₁) that states there is a meaningful effect [7].
- Type I Error (Alpha - α): A Type I error occurs when the null hypothesis (H₀) is incorrectly rejected. In practical terms, it is the probability of concluding that a new method is different or superior when, in fact, it is not. This is known as a false-positive finding [7]. The alpha level (α) is the threshold set by the researcher for accepting this risk. An α of 0.05 implies a 5% risk of a false positive.
- Type II Error (Beta - β): A Type II error occurs when the null hypothesis is incorrectly retained. This represents the failure to detect a true effect, resulting in a false-negative conclusion. In method verification, this would mean failing to identify a true, practically significant difference between methods [7]. The probability of correctly rejecting a false null hypothesis is the statistical power of the test, calculated as 1-β [23] [7].
The following table summarizes these core concepts:
Table 1: Definitions of Key Statistical Error Parameters
| Parameter | Symbol | Common Value | Definition | Consequence in Method Verification |
|---|---|---|---|---|
| Type I Error Rate | α | 0.05 | Probability of a false positive; rejecting H₀ when it is true. | Concluding a new method is different when it is not. |
| Confidence Level | 1-α | 0.95 (95%) | Probability of correctly not rejecting a true H₀. | Confidence that a "significant" finding is real. |
| Type II Error Rate | β | 0.20 | Probability of a false negative; failing to reject H₀ when it is false. | Failing to detect a true, meaningful difference between methods. |
| Statistical Power | 1-β | 0.80 (80%) | Probability of correctly rejecting a false H₀. | The ability of the study to detect a true effect if it exists. |
The Interrelationship of Alpha, Beta, Effect Size, and Sample Size
The parameters α, β, effect size, and sample size are intrinsically linked. A change in one necessitates an adjustment in at least one of the others to maintain the same statistical properties [7].
- Effect Size: This is the magnitude of the difference or effect that the study is designed to detect. It is a measure of practical significance [23]. In microbiome studies, for example, the choice of diversity metric (e.g., Bray-Curtis vs. Jaccard) can profoundly influence the observed effect size and, consequently, the required sample size [24].
- Sample Size: For a given effect size, alpha, and power, a specific sample size is required. A smaller effect size, a lower alpha (stricter false-positive control), or a higher power (lower false-negative risk) will all increase the required sample size [23] [7].
Diagram 1: Relationship between key parameters in sample size calculation
Experimental Protocol for Establishing Alpha and Beta
Protocol: A Risk-Based Approach to Setting Error Rates
This protocol provides a step-by-step guide for determining the appropriate alpha and beta levels for a microbiological method verification study.
4.1.1 Objective To define the Type I (α) and Type II (β) error rates for a study, ensuring the sample size calculation is aligned with the clinical, regulatory, and practical consequences of false-positive and false-negative outcomes.
4.1.2 Materials and Reagents
- Historical data from pilot studies or previous similar methods.
- Statistical software (e.g., G*Power, R) or online calculators (e.g., OpenEpi).
- Risk assessment documentation (e.g., FMEA output).
4.1.3 Procedure
- Define the Primary Hypothesis: Clearly state the null and alternative hypotheses for the method verification. For example, H₀: "There is no difference in the recovery rate between the new method and the standard reference method."
- Conduct a Risk Assessment: Use a structured risk assessment tool, such as Failure Mode and Effects Analysis (FMEA), to evaluate the impact of both Type I and Type II errors [25]. Categorize the overall risk of the method as low, medium, or high based on factors like patient safety, product quality, and decision impact.
- Set the Alpha (α) Level:
- The standard value is α = 0.05 [7].
- For high-risk scenarios where a false positive could have severe consequences (e.g., releasing a contaminated product), a more stringent alpha (e.g., 0.01 or 0.001) should be used [7].
- For exploratory or pilot studies, a less conservative alpha (e.g., 0.10) may be acceptable [7].
- Set the Beta (β) Level and Calculate Power:
- Determine the Minimally Important Effect Size:
- This is the smallest difference from the null hypothesis that is considered practically or clinically significant [23].
- Use data from pilot studies, published literature, or subject matter expertise to define this value [23]. For instance, a 10% difference in microbial recovery might be deemed the minimum important effect.
- In microbiome studies, note that the choice of alpha and beta diversity metrics (e.g., Bray-Curtis, UniFrac) can influence the observed effect size and must be selected a priori to avoid p-hacking [24].
- Calculate the Sample Size: Input the defined α, β (power), and effect size into an appropriate statistical formula or software to determine the required sample size [23] [7].
4.1.4 Data Analysis and Interpretation The final output of this protocol is a justified set of parameters for sample size calculation. The chosen alpha and beta should be documented in the study protocol, along with the rationale based on the risk assessment.
Table 2: Example Risk-Based Selection of Alpha and Beta [7] [25]
| Risk Level | Example Context | Recommended α (Type I) | Recommended Power (1-β) | Recommended β (Type II) |
|---|---|---|---|---|
| Low Risk | Exploratory research, preliminary method feasibility. | 0.10 | 0.80 | 0.20 |
| Medium Risk | Standard method verification, comparative studies. | 0.05 | 0.80 - 0.90 | 0.20 - 0.10 |
| High Risk | Final validation for product release, safety-critical methods. | 0.01 - 0.001 | 0.90 - 0.95 | 0.10 - 0.05 |
The Scientist's Toolkit
Table 3: Research Reagent Solutions for Experimental Power Analysis
| Item | Function in Error Rate & Sample Size Context |
|---|---|
| Statistical Software (G*Power, R, PS Power) | Used to perform the sample size calculation after alpha, beta, and effect size have been defined. These tools implement the complex statistical formulas required for different study designs [23]. |
| Pilot Study Data | Provides a preliminary estimate of key parameters like variance and baseline rates, which are necessary for calculating the effect size for the main study [23]. |
| Online Calculators (OpenEpi) | Provides a free and accessible interface for performing basic sample size and power calculations for common study designs [23]. |
| Standard Operating Procedure (SOP) for Validation | A pre-defined SOP ensures that the rationale for choosing alpha, beta, and the resulting sample size is documented, consistent, and defensible during audits [26] [25]. |
| Risk Assessment Matrix | A formal tool (e.g., FMEA) used to objectively categorize the risk level of the method, which directly informs the stringency of the chosen alpha and beta levels [25]. |
Calculating the appropriate sample size is a fundamental step in designing a scientifically sound study for the verification of microbiological methods. An inadequate sample size can lead to Type I errors (false positives) or Type II errors (false negatives), compromising the reliability of the verification study and the validity of its conclusions [7]. The choice of sample size is intrinsically linked to the nature of the method being verified—whether it is qualitative (detecting the presence or absence of a microorganism) or quantitative (enumerating the number of microorganisms). This article provides detailed protocols for determining sample sizes for both method types within the context of microbiological method verification research for drug development.
Fundamental Distinctions Between Qualitative and Quantitative Methods
In microbiology, qualitative methods are used to detect the presence or absence of specific microorganisms, such as pathogens like Listeria monocytogenes, Salmonella, and Escherichia coli O157:H7. These methods are highly sensitive, with a limit of detection (LOD) that can be as low as 1 colony forming unit (CFU) per test portion, and results are typically reported as Positive/Negative or Detected/Not Detected [27]. In contrast, quantitative methods measure the numerical population of specified microorganisms, reported as CFU per unit weight or volume (e.g., CFU/g). These methods, such as aerobic plate counts, have a higher LOD, often 10 or 100 CFU/g, and require a series of dilutions to achieve a countable range of colonies on an agar plate [27].
The following table summarizes the core differences that influence sample size strategy:
Table 1: Core Differences Between Qualitative and Quantitative Microbiological Methods
| Parameter | Qualitative Methods | Quantitative Methods |
|---|---|---|
| Objective | Detection and identification [27] | Enumeration and quantification [27] |
| Reported Result | Presence/Absence (e.g., Detected/25g) [27] | Numerical count (e.g., 10⁵ CFU/g) [27] |
| Limit of Detection (LOD) | Very low (theoretically 1 CFU/test portion) [27] | Higher (e.g., 10 CFU/g for plate counts) [27] |
| Key Performance Parameters | Sensitivity, Specificity [28] [29] | Accuracy, Precision, Linearity [29] |
Sample Size Calculation for Qualitative Method Verification
For qualitative methods, the primary goal is to statistically demonstrate that the method can reliably detect the target microorganism when it is present (sensitivity) and correctly yield a negative result when it is absent (specificity).
Statistical Foundation and Parameters
The sample size calculation for a qualitative method verification study is often based on estimating a proportion (prevalence) or ensuring a certain probability of detection. The key parameters are:
- Prevalence (P): The expected or acceptable proportion of positive samples in the population.
- Margin of Error (E) or Precision: The acceptable deviation from the true prevalence value.
- Confidence Level (Zα/2): The probability that the true value lies within the margin of error (typically 95%, for which Zα/2 is 1.96) [30].
The formula for calculating the sample size (N) for a prevalence study is: N = (Zα/2² × P × (1 - P)) / E² [30]
This formula is applied when the objective is to estimate the prevalence of a characteristic, such as the rate of contamination in a lot.
Experimental Protocol for Qualitative Method Verification
Objective: To verify that a qualitative method (e.g., a PCR assay for Salmonella) meets predefined performance criteria (sensitivity and specificity) in a single laboratory, as per guidelines such as ISO 16140-3 [9].
Materials:
- Reference Material: Certified reference strains of target microorganisms (e.g., Salmonella enterica subsp. enterica ATCC 14028) [29].
- Test Samples: A panel of samples representing a defined category (e.g., dairy, meat) that includes both artificially contaminated and known negative samples [9].
- Culture Media: Non-selective and selective enrichment broths, and differential agar plates as required by the method [27] [9].
- Equipment: PCR thermocycler and detection system, microbiological incubators, biosafety cabinet.
Procedure:
- Define Scope and Criteria: Determine the target microorganism, the food categories to be verified, and the acceptance criteria for sensitivity and specificity (e.g., ≥95% agreement with the reference method) [9] [29].
- Calculate Sample Size: Using the formula above, for an expected prevalence of detection (sensitivity) of 50% and a margin of error of 10% at a 95% confidence level, the calculation is:
N = (1.96² × 0.5 × 0.5) / 0.1² = 96.04 → 97 samples. A minimum of 97 samples per food category would be required to estimate the detection rate. In practice, for initial verification, a minimum of 5-10 positive and 5-10 negative samples per food category is often used [31]. - Prepare Sample Panel: Artificially inoculate a portion of the test samples with a low level (e.g., <100 CFU) of the target microorganism. The remaining samples are left uninoculated as negative controls [29].
- Perform Testing: Test all samples in parallel using the new qualitative method and a validated reference method [9] [31].
- Analyze Results: Construct a 2x2 contingency table to compare results. Calculate sensitivity, specificity, and overall percent agreement against the reference method [31] [29].
Sample Size Calculation for Quantitative Method Verification
For quantitative methods, the goal is to precisely and accurately measure the concentration of microorganisms. Sample size determination therefore focuses on the variability of measurements and the desired precision of the estimate.
Statistical Foundation and Parameters
The sample size for a quantitative method is typically calculated to compare means (e.g., the mean count from the new method versus the reference method). The key parameters are:
- Standard Deviation (s): The expected variability in the microbial counts, obtained from a pilot study or previous data.
- Effect Size (d) or Precision: The smallest difference in means that is of practical importance or the desired accuracy of the estimate.
- Significance Level (α): The risk of a Type I error (usually 0.05).
- Power (1-β): The probability of correctly rejecting a false null hypothesis (typically 80% or 90%) [7] [30].
The formula for calculating sample size (N) per group for a comparison of two means is: N = 2 × ( (Zα/2 + Z1-β) × s / d )² [30] Where Z1-β is 0.84 for 80% power and 1.28 for 90% power.
Experimental Protocol for Quantitative Method Verification
Objective: To verify that a quantitative method (e.g., spiral plating for aerobic plate count) provides results equivalent to a reference method (e.g., pour plate method) in terms of accuracy and precision [9] [29].
Materials:
- Test Microorganism: A stable, non-pathogenic strain suitable for quantitative studies (e.g., Escherichia coli ATCC 8739).
- Test Sample: A homogeneous slurry or product suspension with a known microbial load.
- Diluents and Media: Buffered peptone water, phosphate buffered saline, Plate Count Agar.
- Equipment: Spiral plater, automated colony counter, incubator.
Procedure:
- Define Parameters and Criteria: Define the acceptable difference between methods (d), and the required power (80%) and significance (α=0.05). Establish acceptance for accuracy (e.g., mean recovery of 50-200%) and precision (e.g., CV < 10%) [29].
- Perform a Pilot Study: Conduct a small-scale experiment (e.g., n=5) with both methods to estimate the standard deviation (s) of the differences in log-transformed counts.
- Calculate Sample Size: If the pilot study shows a standard deviation of 0.3 log10 CFU/g, and the critical difference to detect (d) is 0.5 log10 CFU/g, with 80% power and α=0.05:
N = 2 × ( (1.96 + 0.84) × 0.3 / 0.5 )² = 2 × (2.8 × 0.6)² ≈ 2 × (1.68)² ≈ 5.64. A minimum of 6 samples per method would be required. To account for potential drop-outs and ensure robustness, increasing this number to 10-15 is advisable. - Execute Full Verification Study: Test the calculated number of sample replicates using both the new method and the reference method.
- Analyze Results: Perform a statistical analysis (e.g., Student's t-test on log-transformed data, calculation of mean difference, and coefficient of variation) to confirm that the methods do not differ by more than the predefined acceptable limit and that precision meets the criteria [29].
Integrated Workflow for Sample Size Determination
The following diagram illustrates the decision-making process for selecting the appropriate sample size calculation strategy based on the method type and study objective.
The Scientist's Toolkit: Essential Reagents and Materials
Successful execution of method verification studies relies on specific, high-quality reagents and materials. The following table details key components.
Table 2: Essential Research Reagents and Materials for Microbiological Method Verification
| Reagent/Material | Function/Application | Example |
|---|---|---|
| Certified Reference Strains | Provide a traceable and characterized inoculum for accuracy, specificity, and LOD studies [29]. | Staphylococcus aureus ATCC 6538 |
| Selective & Differential Media | Allow isolation and preliminary identification of target microorganisms by inhibiting non-target flora and displaying characteristic reactions [27] [9]. | Modified Semi-solid Rappaport-Vassiliadis (MSRV) medium for Salmonella [28] |
| Culture Enrichment Broths | Amplify low numbers of target pathogens to detectable levels, a critical step in qualitative methods [27]. | Buffered Peptone Water, Fraser Broth |
| Standardized Diluents | Ensure accurate serial dilution for quantitative counts without causing microbial stress or death [27] [29]. | Buffered Peptone Water, Phosphate Buffered Saline |
| Enzymes & Molecular Reagents | Essential for rapid methods (e.g., PCR); enzymes like DNA polymerase amplify target sequences for detection [27]. | Taq Polymerase, primers, probes |
A rigorous and statistically justified approach to sample size calculation is non-negotiable for the verification of microbiological methods in drug development. The fundamental distinction between qualitative and quantitative objectives dictates the statistical parameters and formulas used. By applying the specific protocols, formulas, and workflows outlined in this article, researchers and scientists can design efficient and defensible verification studies. This ensures that new methods are proven to be fit-for-purpose, generating reliable data that underpins product quality and patient safety.
Utilizing Statistical Software and Online Calculators (e.g., G*Power)
In microbiological method verification research, such as studies validating a new microbial identification technique or a pathogen detection assay, calculating an appropriate sample size is not merely a statistical formality; it is a fundamental component of research integrity. An inadequate sample size can lead to false negatives (Type II errors), where a truly effective method is deemed ineffective, or false positives (Type I errors), where an ineffective method appears successful, potentially compromising drug development quality and safety [7]. This document provides detailed application notes and protocols for utilizing statistical software and online calculators to determine sample sizes, framed within the context of a rigorous microbiological research thesis.
Core Statistical Concepts for Sample Size Determination
Before employing any software, a clear understanding of the key statistical parameters is essential. These parameters are interlinked, and researchers must define them based on their specific research context.
- Power (1-β): The probability that the study will correctly reject the null hypothesis when the alternative hypothesis is true. It is the likelihood of detecting an effect if it truly exists. A power of 0.8 (or 80%) is conventionally considered the minimum acceptable level [7].
- Significance Level (α): The probability of rejecting the null hypothesis when it is actually true (Type I error). It is typically set at 0.05 (5%) but can be set lower (e.g., 0.01) in studies where the consequences of a false positive are severe [7].
- Effect Size (ES): The magnitude of the difference or relationship that the study aims to detect. It represents the practical or clinical significance, not just statistical significance. Determining the ES is often the most challenging step [23].
- Sample Size (N): The number of independent observations or samples (e.g., individual microbial cultures, clinical isolates) required to achieve the desired power and significance level for a given effect size.
The relationship between these elements is such that for a given effect size, a higher power or a more stringent significance level will require a larger sample size. Conversely, for a fixed sample size, a smaller effect size becomes harder to detect with high power [7].
Determining Effect Size in Microbiological Research
The effect size must be determined based on what is considered a clinically or practically significant difference in the specific research context [23]. For instance:
- When verifying a new quantitative method against a standard, the effect size could be the minimum difference in colony-forming units (CFU) per milliliter that is considered biologically meaningful.
- For a qualitative method (e.g., presence/absence of a pathogen), the effect size might be the minimum acceptable difference in detection rates.
If prior knowledge is unavailable, researchers can use standardized effect sizes (small, medium, large) as proposed by Cohen, though these are arbitrary and must be applied with caution [23]. For a comparison of two means (e.g., mean log reduction using two disinfectants), a standardized effect size of 0.2 is considered small, 0.5 medium, and 0.8 large. Conducting a pilot study is a highly recommended approach to obtain preliminary data for estimating the effect size and standard deviation for the main study [23].
A range of tools is available to simplify sample size calculation, from comprehensive statistical packages to specialized freeware and web applications. Table 1 summarizes key tools relevant to health and microbiological research.
Table 1: Key Software and Online Calculators for Sample Size Determination
| Tool Name | Type/Availability | Primary Use Case | Key Features |
|---|---|---|---|
| G*Power [23] | Free Statistical Software | A priori, post hoc, and compromise power analysis for a wide range of tests. | Extensive set of statistical tests (t-tests, F-tests, χ² tests, etc.). Allows plotting of power curves. |
| OpenEpi [23] | Open-Source Online Calculator | Sample size and power for common study designs in epidemiology. | Accessible via web browser; includes calculations for cross-sectional, cohort, and case-control studies. |
| PS Power and Sample Size Calculation [23] | Free Software Application | Power and sample size for studies with dichotomous, continuous, or survival outcomes. | Practical tool for common study designs in medical research. |
| GraphPad QuickCalcs [32] | Suite of Online Calculators | Quick statistical analyses including t-tests, confidence intervals, and P values. | User-friendly interface for common, straightforward calculations. |
| Other Online Calculators [33] | Various Web Tools | Intuitive tests of significance, correlation, and confidence intervals. | Useful for quick, simple checks and for researchers less familiar with statistical software. |
Detailed Experimental Protocols for Sample Size Calculation
The following protocols outline the step-by-step process for determining sample size using different tools, contextualized for microbiological method verification.
Protocol 1: A Priori Power Analysis for a Comparative Study Using G*Power
Aim: To determine the sample size required to detect a significant difference between the means of two independent groups (e.g., comparing the accuracy of a novel microbial identification method versus a reference method).
Research Reagent Solutions:
- Statistical Software: G*Power software package [23].
- Preliminary Data: Estimates of mean values and standard deviations from prior literature or a pilot study.
- Defined Parameters: Justified values for alpha (α), power (1-β), and the effect size of practical significance.
Methodology:
- Launch G*Power and select the test family. For comparing two independent means, navigate to
Tests > Means > Two independent groups. - Select the statistical test. Choose the appropriate test, such as the
t-testfor independent groups. - Choose the type of power analysis. Select
A priori: Compute required sample size – given α, power, and effect size. - Input the parameters:
- Tail(s): Specify whether the hypothesis is one-tailed or two-tailed. A two-tailed test is standard unless there is a strong directional prediction.
- Effect size d: Click "Determine" to open a calculator. Input the estimated means and standard deviations for both groups from your pilot data or literature. G*Power will compute Cohen's d. Alternatively, input d directly (e.g., 0.2 for small, 0.5 for medium, 0.8 for large).
- α err prob: Set the significance level, typically 0.05.
- Power (1-β err prob): Set the desired power, typically 0.80 or 0.90.
- Allocation ratio N2/N1: Set to 1 for equal group sizes.
- Click "Calculate." GPower will output the total sample size (N) and the required sample size per group (N1 and N2). *Figure 1 illustrates the logical workflow of this power analysis.
Figure 1: Workflow for a priori sample size calculation using GPower.*
Protocol 2: Sample Size for a Descriptive (Prevalence) Study Using OpenEpi
Aim: To determine the sample size required to estimate a population proportion (e.g., the prevalence of a specific antibiotic-resistant strain in a bacterial population) with a specified precision.
Research Reagent Solutions:
- Online Calculator: OpenEpi [23].
- Prevalence Estimate (P): An initial estimate of the proportion from previous studies or literature. If unknown, use 0.5 for a conservative (maximum) sample size.
- Precision (Margin of Error, E): The acceptable absolute deviation from the true proportion (e.g., ±5% or 0.05).
Methodology:
- Access the OpenEpi website and navigate to the "Sample Size" calculator for descriptive studies.
- Select the calculation for proportion.
- Input the parameters:
- Population size (if known): For large or unknown populations, this can be left blank (infinite).
- Expected frequency (p): Enter the estimated proportion (e.g., 0.15 for 15% prevalence).
- Confidence level (CI): Typically set to 95%.
- Design effect (DEFF): Set to 1 for simple random sampling. Use a higher value (e.g., 1.5-2) for complex designs like cluster sampling.
- Precision / Margin of error: Enter the desired precision (e.g., 0.05).
- Click "Calculate." The calculator will output the required sample size. Figure 2 shows the decision pathway for calculating sample sizes for different study types.
Figure 2: Decision pathway for selecting the appropriate sample size calculation method based on study design.
Presentation and Interpretation of Results
Once the sample size is calculated, it must be clearly reported and critically evaluated within the research context.
Structured Presentation of Calculations
Presenting the parameters and results in a structured format, as shown in Table 2, enhances transparency and reproducibility.
Table 2: Example Sample Size Calculation for a Method Comparison Study
| Parameter | Symbol | Value | Justification |
|---|---|---|---|
| Statistical Test | - | Two-independent samples t-test | Comparison of mean log reduction between new and standard disinfectant. |
| Effect Size | d | 0.8 (Large) | A large difference (0.8 SD) is considered the minimum practically important difference in log reduction. |
| Significance Level | α | 0.05 | Conventional threshold for Type I error. |
| Power | 1-β | 0.90 | High power selected to minimize risk of missing a true effect (Type II error). |
| Allocation Ratio | N2/N1 | 1 | Equal sample sizes in both test groups. |
| Calculated Sample Size per Group | N1, N2 | 29 | Output from G*Power. Total N = 58. |
Critical Considerations and Ethical Implications
Simply calculating a sample size is insufficient. Researchers must engage in a realistic dialog about its feasibility [23]. In microbiological and drug development contexts, this involves:
- Ethics: Using more samples than necessary exposes biological resources and, in pre-clinical studies, animals, to unnecessary use. An underpowered study is also unethical as it cannot yield reliable conclusions, wasting resources and potentially misleading future research [7].
- Feasibility: The calculated sample size must be achievable within the constraints of time, budget, and available microbial isolates or clinical samples.
- Reporting: The sample size calculation, including all parameters and the software tool used, must be explicitly detailed in the methods section of the final thesis or publication [23].
Troubleshooting Common Issues
- Unrealistically Large Sample Size: If the calculated sample size is too large to be feasible, consider whether the effect size is too small or the power too high. Re-evaluate the clinically meaningful effect size or explore alternative study designs with greater efficiency [23].
- Unknown Effect Size or Variance: When prior information is completely absent, a pilot study is strongly recommended. Using standardized effect sizes (small, medium, large) is a common but less ideal alternative, as it divorces the calculation from the specific research context [23].
- Complex Study Designs: For multifactorial experiments (e.g., those with multiple treatments or time points), standard calculators may be insufficient. Consultation with a biostatistician is advised to use specialized software or custom simulation-based power analysis.
Bayesian microbial subtyping attribution models represent a significant advancement in the field of microbial source tracking and outbreak investigation. These models are essential for conceiving, prioritizing, and assessing the impact of public health policy measures by attributing foodborne illnesses to specific food sources [34]. The Bayesian framework provides a powerful approach for analyzing sporadic cases of foodborne illness by incorporating both prior scientific knowledge and observed microbiological data. This methodology allows researchers to account for critical factors such as the level of exposure to different contamination sources and genetic differences between bacterial types and sources, enabling more accurate attribution estimates than previously possible with deterministic models [34].
The fundamental strength of Bayesian approaches lies in their ability to handle complex, multi-parameter problems inherent in microbiological studies while formally accounting for uncertainty in parameter estimates. Unlike traditional frequentist methods that often rely on point estimates, Bayesian models generate posterior probability distributions that provide a more comprehensive understanding of parameter uncertainty [35]. This is particularly valuable in microbial subtyping, where sample sizes may be limited and prior information from previous studies or expert opinion can significantly improve model precision and robustness. Recent advancements in computational capabilities and sampling algorithms have made these methods increasingly accessible for routine public health and food safety applications.
Theoretical Framework and Key Bayesian Models
Bayesian Microbial Subtyping Attribution Model
The foundational Bayesian microbial subtyping attribution model introduced by Hald et al. represents one of the most sophisticated approaches for attributing sporadic foodborne illness cases to their sources. This model incorporates two critical dimensions: the level of exposure to potential contamination sources and the differences between bacterial subtypes across these sources [34]. The model structure accounts for the fact that different bacterial subtypes may have varying affinities for different food sources, and that exposure patterns significantly influence attribution probabilities.
However, this advanced modeling approach introduces challenges with parameterization, as it requires estimating numerous type- and source-dependent parameters. Initial implementations addressed this overparameterization by setting certain parameters to constant values based on arbitrary assignments or the most frequent types [34]. Research has demonstrated that the model exhibits high sensitivity to these parameterization choices, potentially affecting the robustness of attribution estimates. Modified approaches have proposed using bacterial types specific to unique sources rather than the most frequent ones and employing data-based values instead of arbitrary assignments, which has been shown to enhance model convergence and improve the adequacy of estimates [34].
Bayesian Sample Size Determination Model
For microbiological surveys, determining appropriate sample sizes presents a significant challenge. Insufficient sampling leads to biased inferences, while excessive sampling wastes valuable laboratory resources [36]. A Bayesian statistical model addresses this challenge by combining prior knowledge with observed data to estimate the sample size needed for accurate identification of bacterial subtypes in a specimen.
This model utilizes the Dirichlet distribution to express prior scientific knowledge about the distribution of bacterial subtypes, which allows probabilities to be assigned to quantities within a specified range while obeying the condition that their sum remains fixed [36]. The model incorporates two key inputs: (1) a prespecified prior distribution statement based on available scientific knowledge provided by informed microbiologists, and (2) observed data from microbiological surveys indicating the number of strains per specimen. Through Markov chain Monte Carlo simulation with the Metropolis-Hastings algorithm, the model generates posterior probability estimates of the number of bacterial subtypes present, enabling researchers to determine the probability of observing all strains based on the number of colonies sampled [36].
BIRDMAn Framework for Differential Abundance Analysis
BIRDMAn (Bayesian Inferential Regression for Differential Microbiome Analysis) represents a flexible computational framework for hierarchical Bayesian modeling of microbiome data that simultaneously accounts for its characteristic high sparsity, high-dimensionality, and compositionality [35]. Implemented within the Stan probabilistic programming language, which utilizes Hamiltonian Monte Carlo sampling, BIRDMAn enables parameter estimation of all biological variables and non-biological covariates while providing uncertainty estimates for these parameters.
This framework offers specific advantages for analyzing microbiome data, including the ability to model complex experimental designs such as longitudinal studies with repeated measures, account for batch effects and technical variability, and handle the compositional nature of microbiome data without requiring rarefaction [35]. Simulations have demonstrated that BIRDMAn models are robust to uneven sequencing depth and provide substantial improvements in statistical power over existing differential abundance methods, with more than a 20-fold improvement reported in some scenarios [35].
Table 1: Comparison of Key Bayesian Models for Microbial Subtyping
| Model Name | Primary Application | Key Features | Advantages |
|---|---|---|---|
| Bayesian Attribution Model [34] | Source attribution of foodborne illnesses | Incorporates exposure levels and subtype differences | Handles complex multi-parameter problems; accounts for source exposure |
| Bayesian Sample Size Model [36] | Determining colony sample size for subtype identification | Uses Dirichlet distribution for prior knowledge | Prevents both under-sampling and over-sampling; incorporates expert knowledge |
| BIRDMAn Framework [35] | Differential abundance analysis in microbiome studies | Hierarchical Bayesian modeling with Hamiltonian Monte Carlo | Handles compositionality and sparsity; improves statistical power >20-fold |
Experimental Protocols
Protocol for Implementing Bayesian Sample Size Determination
Principle: This protocol enables estimation of the optimal number of bacterial colonies that should be sampled to correctly identify all bacterial subtypes present in a specimen with a specified probability [36].
Materials:
- Microbial isolates from primary specimens
- Standardized subtyping method (e.g., AFLP, phage typing, FTIR spectroscopy)
- Statistical software with Bayesian modeling capabilities (e.g., Stan, PyMC3)
- Prior knowledge of expected strain distribution from literature or expert opinion
Procedure:
- Define Prior Distribution: Specify a prior distribution statement for the number of strains per specimen based on available scientific knowledge. This can be a uniform distribution across a plausible range or a distribution with peaks at more likely values [36].
Assign Prior Weight: Determine the weight (prior sample size) to assign to the prior distribution, reflecting the certainty of this belief. A lower weight (e.g., equivalent to 1 specimen) indicates higher uncertainty, while a greater weight (e.g., equivalent to 32 specimens) reflects stronger belief in the prior distribution [36].
Collect Observed Data: Perform initial subtyping on a sample of bacterial colonies from multiple specimens. The number of colonies examined per specimen should be sufficient to potentially capture the diversity present (e.g., 48 colonies per carcass in the Campylobacter example) [36].
Model Fitting: Input the prior distribution and observed data into the Bayesian model using Markov chain Monte Carlo simulation with the Metropolis-Hastings algorithm to generate posterior probability distributions of the number of subtypes per specimen [36].
Sample Size Estimation: Use the posterior distribution to estimate the probability of correctly identifying all subtypes based on different numbers of sampled colonies. Determine the minimum sample size that achieves an acceptable probability threshold (typically ≥80%) [36].
Application Example - Campylobacter jejuni AFLP Typing:
- Prior Distribution: Two alternative priors were specified: (1) uniform distribution between 9-24 AFLP types per carcass with low weight, and (2) normal-like distribution peaked at 16-17 types with higher weight [36].
- Observed Data: 48 colonies examined from each of 20 broiler carcasses, with AFLP typing revealing 9-19 types per carcass [36].
- Outcome: Model generated posterior probabilities enabling estimation of sample size needed to detect all AFLP types with specified confidence.
Protocol for FTIR Spectroscopy-Based Strain Typing
Principle: Fourier-transform infrared (FTIR) spectroscopy distinguishes microbial strains by quantifying the absorption of infrared light by biochemical components within bacterial cells, producing highly specific metabolic fingerprint-like signatures [37].
Materials:
- IR Biotyper system (Bruker Daltonics) or equivalent FTIR spectrometer
- Appropriate culture media (e.g., BHI agar, TSA, blood agar)
- Cryo stocks of microbial strains
- Silicon sample plate for IR Biotyper
Procedure:
- Culture Preparation:
- Resuscitate strains from cryo stocks by plating on appropriate media and incubating under specified conditions (e.g., 24h at 37°C for L. monocytogenes on BHI agar) [37].
- For FTIR analysis, select pure single colonies for subculture on standardized media. Avoid blood agar and chromogenic agar, as they can introduce additional variance or colorize biomass, altering infrared absorbance characteristics [37].
- Incubate for standardized time and temperature according to the target organism (see Table 2 for specific conditions).
Sample Preparation:
- Harvest bacterial biomass from agar plates using a sterile loop.
- Resuspend biomass in 100 μL of HPLC-grade water and vortex thoroughly to create a homogeneous suspension [37].
- Centrifuge if necessary to remove large particles, then transfer supernatant to a new tube.
- Adjust concentration to an optical density (OD) appropriate for the instrumentation.
Spectra Acquisition:
- Apply 2-35 μL of bacterial suspension to a silicon sample plate and dry at low temperature (e.g., 30°C) to form a homogeneous film [37].
- Load the sample plate into the IR Biotyper instrument.
- Acquire spectra in the mid-infrared range (typically 4000-500 cm⁻¹) with appropriate resolution and number of scans per spectrum [37].
- Include quality control samples to ensure instrument performance and reproducibility.
Data Analysis:
- Preprocess spectra (vector normalization, derivation) to reduce technical variance.
- Analyze spectral data using multivariate statistical methods (principal component analysis, hierarchical clustering).
- Compare unknown strains against reference spectral libraries for identification and subtyping.
Table 2: Standardized Culture Conditions for FTIR Spectroscopy of Common Foodborne Pathogens [37]
| Organism | Media | Temperature | Time | Atmosphere |
|---|---|---|---|---|
| L. monocytogenes | BHI, TSA | 37°C | 24 ± 0.5 h | Aerobic |
| S. pneumonia | Blood agar | 37°C | 24 ± 0.5 h | Microaerophilic, capnophilic |
| S. enterica | TSA | 37°C | 24 ± 0.5 h | Aerobic |
| L. pneumophila | BCYE | 37°C | 48 ± 1 h | Microaerophilic, humid |
Protocol for Bayesian Attribution Modeling
Principle: This protocol outlines the steps for implementing a Bayesian microbial subtyping attribution model to estimate the proportion of human cases of foodborne illness attributable to different food sources [34].
Materials:
- Human case isolates with subtype information
- Food source isolates with subtype information
- Food consumption data (exposure information)
- Computational resources for Bayesian analysis
Procedure:
- Data Collection:
- Compile microbial subtyping data from human clinical cases.
- Collect subtyping data from potential food sources.
- Obtain food exposure data representing population-level consumption patterns.
Model Parameterization:
- Define the statistical model relating human cases to food sources through subtype-specific parameters.
- Use specific types associated with unique sources rather than the most frequent types to enhance model robustness [34].
- Employ data-based values instead of arbitrary values for parameter settings to improve convergence and adequacy of estimates [34].
Prior Specification:
- Specify prior distributions for all model parameters based on previous studies or expert knowledge when available.
- Use weakly informative priors when prior information is limited to avoid introducing strong biases.
Model Fitting:
- Implement the model using Bayesian computational methods such as Markov Chain Monte Carlo (MCMC).
- Run multiple chains to assess convergence using diagnostic statistics (Gelman-Rubin statistic, trace plots).
Model Validation:
- Compare results with alternative models (e.g., Mullner's modified Hald model, simple deterministic models) to assess consistency [34].
- Perform sensitivity analyses to evaluate the impact of prior choices and parameterization decisions on attribution estimates.
Interpretation:
- Extract posterior distributions of attribution proportions for each food source.
- Report credible intervals to communicate uncertainty in estimates.
- Translate results into public health recommendations for intervention strategies.
Integration with Sample Size Calculation in Method Verification
The implementation of Bayesian approaches for microbial subtyping must be framed within the broader context of sample size calculation for microbiological method verification research. Appropriate sample size determination is fundamental for designing studies that yield generalizable results while efficiently allocating laboratory resources [38]. Bayesian methods offer unique advantages in this domain by formally incorporating uncertainty and prior information into sample size calculations.
For cross-sectional studies investigating microbial prevalence, the sample size can be calculated using the formula [38]:
n = (Z₁₋α/₂)² × p(1-p) / d²
Where:
- Z₁₋α/₂ = critical value (1.96 for 95% confidence)
- p = expected prevalence
- d = margin of error
However, this frequentist approach does not incorporate prior knowledge and treats parameters as fixed values. Bayesian assurance methods address this limitation by assigning prior distributions to uncertain parameters (e.g., treatment effect size, standard deviation) and calculating the unconditional probability of trial success [39]. This provides a more accurate representation of the true probability of success by formally accounting for parameter uncertainty.
In the context of method verification according to ISO 16140 standards, two stages are required before a method can be used in a laboratory: method validation (proving the method is fit for purpose) and method verification (demonstrating the laboratory can properly perform the method) [9]. Bayesian sample size determination can optimize both stages by ensuring sufficient sampling to demonstrate method performance characteristics while avoiding excessive resource expenditure.
The Bayesian framework is particularly valuable for determining the number of colonies that need to be subtyped to identify all strains present in a specimen with a specified probability. This approach combines prior knowledge about the expected distribution of strains with observed data from initial sampling to generate progressively more precise sample size estimates as additional data becomes available [36].
Visualization of Workflows
Diagram 1: Integrated Bayesian Workflow for Microbial Subtyping and Sample Size Determination
Diagram 2: Bayesian Sample Size Determination Process
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for Bayesian Microbial Subtyping Studies
| Reagent/Material | Function/Application | Specification Considerations |
|---|---|---|
| Culture Media | Supports growth and maintenance of microbial strains | Standardized formulations (BHI, TSA, BCYE); avoid blood/chromogenic agars for FTIR [37] |
| FTIR Spectroscopy System | Rapid strain typing via metabolic fingerprinting | IR Biotyper system; silicon sample plates; HPLC-grade water for suspensions [37] |
| DNA Extraction Kits | Nucleic acid isolation for molecular subtyping | High-quality kits suitable for downstream applications (WGS, MLST, AFLP) |
| Bayesian Statistical Software | Implementation of Bayesian models for attribution and sample size | Stan, PyMC3, JAGS, or specialized packages with MCMC capability [36] [35] |
| Reference Strains | Quality control and method validation | Well-characterized strains for system calibration and comparison |
| Cryopreservation Supplies | Long-term strain storage | Cryovials, appropriate cryoprotectants (e.g., glycerol), controlled-rate freezing equipment |
Bayesian approaches for microbial subtyping provide powerful tools for addressing complex challenges in food safety and public health. The integration of Bayesian attribution models, sample size determination frameworks, and modern typing technologies like FTIR spectroscopy creates a robust methodology for source tracking and outbreak investigation. These approaches enable researchers to formally incorporate prior knowledge while accounting for uncertainty in parameters, leading to more reliable and interpretable results. When implemented within the context of appropriate sample size calculations and method verification protocols, Bayesian microbial subtyping methods significantly enhance our ability to protect public health through evidence-based interventions.
Navigating Common Pitfalls and Optimizing Your Verification Study
Addressing Challenges with Rare Microorganisms or Low Contamination Levels
Detecting rare microorganisms or low-level contamination is a critical challenge in pharmaceutical development and quality control. The reliability of microbiological methods at the limits of detection is paramount for ensuring drug safety, particularly for sterile products and cell therapies. The effectiveness of these methods is not solely dependent on analytical procedures but is fundamentally influenced by the initial study design, specifically statistically sound sample size calculation [38]. An underpowered study, with an insufficient number of samples, risks failing to detect a contaminant, potentially leading to serious public health consequences. This application note details protocols for method verification and validation, focusing on experimental design and execution to confidently address these analytical challenges.
Theoretical Foundations: Sample Size Calculation
A robust experimental design begins with calculating the minimum sample size required to draw reliable and generalizable conclusions. The following formulas and considerations are central to this process.
Key Statistical Concepts for Sample Size Calculation [38]:
- Null Hypothesis (H₀): The assumption that there is no effect or no difference (e.g., the new method does not improve detection).
- Alternative Hypothesis (H₁): The hypothesis that contradicts the null hypothesis (e.g., the new method does improve detection).
- Significance Level (α): The probability of rejecting the null hypothesis when it is true (Type I error). Commonly set at 0.05.
- Study Power (1-β): The probability of correctly rejecting the null hypothesis when it is false. A power of 0.8 (80%) is typically considered optimal.
- Effect Size: A quantitative measure of the magnitude of a phenomenon. For prevalence, this is the expected proportion or rate.
- Margin of Error (d): The acceptable range of error in the estimation of a parameter.
For a cross-sectional study aiming to estimate a prevalence rate, such as a contamination rate, the sample size can be calculated as:
Sample size (n) = (Z₁₋α/₂)² × p × (1-p) / d²
Where:
- Z₁₋α/₂ is the Z-value for the desired confidence level (1.96 for 95% CI)
- p is the estimated prevalence or proportion (from previous studies)
- d is the margin of error [38]
Example Calculation: If the literature suggests a contamination prevalence of 9% (0.09) in a process, and a researcher wants to estimate the true prevalence with a 95% confidence level and a margin of error of 5%, the calculation is: n = (1.96)² × 0.09 × (1-0.09) / (0.05)² n = (3.8416 × 0.09 × 0.91) / 0.0025 ≈ 126 samples [38]
Quantitative Data for Experimental Design
Regulatory guidelines provide minimum sample requirements for various types of method performance studies. The following tables summarize these key quantitative benchmarks.
Table 1: Sample Size Requirements for Method Verification Studies (Qualitative/Semi-Quantitative Assays) [3]
| Performance Characteristic | Minimum Sample Number | Sample Details | Replication |
|---|---|---|---|
| Accuracy | 20 | Clinically relevant isolates; combination of positive and negative samples | Single test per sample |
| Precision | 2 positive + 2 negative | Samples with high to low values | Triplicate for 5 days by 2 operators |
| Reportable Range | 3 | Known positive samples near upper/lower cutoff values | Single test per sample |
| Reference Range | 20 | De-identified clinical samples representing the patient population | Single test per sample |
Table 2: Sample Requirements for Method Detection Limit (MDL) Studies [40]
| Study Type | Sample Matrix | Minimum Number | Frequency & Duration |
|---|---|---|---|
| Initial MDL | Spiked Samples | 7 | Analyzed over at least 3 batches |
| Ongoing MDL | Spiked Samples | 8 per year (2 per quarter) | Analyzed with routine batches |
| Ongoing MDL | Method Blanks | Use routine blanks | Use blanks from every batch |
Experimental Protocols
Protocol for Determining Method Detection Limit (MDL)
This protocol follows the principles of EPA Revision 2, which defines the MDL as "the minimum measured concentration of a substance that can be reported with 99% confidence that the measured concentration is distinguishable from method blank results" [40].
1. Principle: The MDL procedure uses a combination of spiked samples and routine method blanks to establish a detection limit that accounts for both instrumental sensitivity and background laboratory contamination [40].
2. Materials:
- Clean reference matrix (e.g., reagent water)
- Analyte of interest at high purity
- All standard laboratory equipment and reagents for the method
3. Procedure:
- Spiked Samples (MDLₛ):
- Prepare a minimum of 7 spiked samples at a concentration 1-5 times the estimated detection limit.
- Analyze these samples in at least 3 separate analytical batches over time to capture routine laboratory variation (e.g., different days, different analysts).
- For ongoing verification, analyze two low-level spiked samples per quarter in separate batches [40].
- Method Blanks (MDLբ):
- Collect data from routine method blanks analyzed with every batch of samples over a one-to-two-year period.
- A laboratory may use the last six months of data or the fifty most recent blanks, whichever is greater, to minimize computational burden [40].
- Calculation:
- Calculate the standard deviation (SDₛ) from the results of the spiked samples.
- Calculate the standard deviation (SDբ) from the results of the method blanks.
- The MDL is the higher of the two values: either MDLₛ = t × SDₛ or MDLբ = t × SDբ, where 't' is the appropriate one-tailed Student's t-value for a 99% confidence level [40].
Protocol for Verification of a Qualitative Microbiological Method
This protocol outlines the verification process for an unmodified, FDA-cleared qualitative method in a single laboratory, as required by CLIA regulations [3].
1. Principle: Before implementing a new method, a laboratory must verify predefined performance characteristics to demonstrate it can perform the test as well as the manufacturer and that it is suitable for the laboratory's patient population [3] [9].
2. Materials:
- A minimum of 20 clinically relevant isolates (see Table 1 for breakdown by characteristic) [3].
- Reference materials, proficiency test samples, or de-identified clinical samples.
- The new instrument/kit and all necessary reagents.
3. Procedure:
- Accuracy Verification:
- Test a panel of 20 samples with known status (positive/negative).
- Analyze results using a comparative method (e.g., the reference method or a previously validated method).
- Calculate percent agreement: (Number of results in agreement / Total number of results) × 100. The result must meet the manufacturer's stated claims or criteria set by the laboratory director [3].
- Precision Verification:
- Select a minimum of 2 positive and 2 negative samples.
- Analyze each sample in triplicate over the course of 5 days by 2 different operators.
- Calculate the percent agreement for all replicates. The results should meet predefined acceptance criteria [3].
- Reportable Range:
- Test a minimum of 3 samples with known analyte concentrations near the upper and lower cutoffs of the test.
- Verify that the method correctly reports results as "Detected" or "Not detected" based on these cutoffs [3].
- Reference Range:
- Test a minimum of 20 samples that are known to be negative for the analyte.
- Verify that at least 95% of these samples report the expected negative result, confirming the manufacturer's reference range is appropriate for the laboratory's patient population [3].
Workflow Visualization
The following diagram illustrates the logical progression and decision points in the method validation and verification process for microbiological methods, based on the ISO 16140 series [9].
Method Validation and Verification Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
The table below lists essential materials and their functions for conducting the experiments described in this application note.
Table 3: Essential Materials for Microbiological Method Verification
| Reagent/Material | Function/Application | Protocol Reference |
|---|---|---|
| Clean Reference Matrix | A material free of the target analyte, used for preparing spiked samples for MDL studies. | Method Detection Limit (MDL) |
| Clinical Isolates & Reference Strains | Well-characterized microorganisms used to verify method accuracy, specificity, and precision. | Qualitative Method Verification |
| Certified Reference Materials | Materials with certified properties (e.g., endotoxin concentration) used for calibrating instruments and validating methods. | LAL Test Validation [41] |
| Limulus Amebocyte Lysate (LAL) | Aqueous extract from horseshoe crab blood cells; used in a kinetic chromogenic test for quantifying bacterial endotoxins. | LAL Test Validation [41] |
| Monoclonal Antibodies for Immunophenotyping | Fluorescently-labeled antibodies that bind to specific cell surface antigens, used for identity testing of cell therapy products. | Immunophenotype Validation [41] |
In microbiological method verification research, determining an appropriate sample size for a definitive study is a common challenge when prior data is unavailable. Traditional sample size calculations require accurate estimates of variability, effect sizes, and baseline parameters—information often lacking for novel methods or organisms. Pilot studies provide a practical solution to this dilemma, offering a systematic approach to gather preliminary data and assess feasibility before committing extensive resources to larger trials [42]. Within the framework of microbiological research, where methods range from quantitative bioburden tests to qualitative presence/absence assays, these small-scale studies are particularly valuable for informing sample size decisions while avoiding the pitfalls of miscalculation [17] [43].
This application note provides structured protocols for employing pilot studies to plan sample sizes for microbiological method verification, ensuring subsequent studies are sufficiently powered to detect clinically or analytically meaningful differences.
The Role of Pilot Studies in Microbiological Research
Pilot studies are formally defined as "small-scale tests of methods and procedures to assess the feasibility/acceptability of an approach to be used in a larger-scale study" [42]. In microbiological contexts, their primary purpose shifts from estimating efficacy to evaluating logistical feasibility and generating reliable parameters for sample size calculation.
Key objectives for pilot studies in method verification include:
- Assessing Feasibility: Testing data collection protocols, intervention fidelity, and participant or sample adherence [42].
- Informing Sample Size: Providing estimates of variability, minimally important differences, and baseline event rates for formal power calculations [42] [44].
- Evaluating Methods: Testing the appropriateness and psychometric adequacy of measures in the target population, which is crucial when adapting methods for diverse microbial groups or new matrices [42].
Critically, pilot studies should not be used for definitive assessments of intervention safety, efficacy, or for performing underpowered hypothesis testing [42].
Conceptual Framework for Pilot Studies
The following workflow outlines the strategic position of a pilot study within the broader scope of microbiological method verification research.
Quantitative Parameters for Sample Size Calculation from Pilot Data
The parameters required for sample size calculation depend on the type of microbiological method being verified (e.g., quantitative vs. qualitative) and the study design. The table below summarizes key parameters derived from pilot studies.
Table 1: Key Quantitative Parameters from Pilot Studies for Sample Size Calculation
| Parameter Type | Description | Application in Sample Size Calculation |
|---|---|---|
| Standard Deviation (SD) | Measure of variability in quantitative data (e.g., CFU counts, viral titers) [45]. | Used in calculations for comparing means (e.g., t-tests, ANOVA). A larger SD necessitates a larger sample size. |
| Event Rate/Proportion | Observed proportion of a binary outcome in the pilot sample (e.g., % positive cultures, test failure rate) [43]. | Informs calculations for comparing proportions (e.g., chi-square tests). Rates close to 0% or 100% require smaller sample sizes. |
| Minimally Important Difference (MID) | The smallest difference in a parameter (e.g., mean count, proportion) that is clinically or analytically meaningful [42]. | The primary input for most sample size formulas. A smaller MID requires a larger sample size. |
| Design Effect (Deff) | A factor that inflates sample size to account for non-independent data (e.g., clustering, repeated measures) [42]. | Critical for complex designs. Calculated as 1 + (m - 1)*ICC, where m is cluster size and ICC is intraclass correlation. |
| Attrition/Drop-out Rate | The proportion of pilot study samples or data points that are lost to follow-up or deemed unusable [42]. | The main study sample size is inflated by 1 / (1 - attrition rate) to ensure adequate final power. |
Confidence Intervals for Pilot Study Estimates
Due to small sample sizes, point estimates from pilot studies (like SD or proportion) are imprecise. Using confidence intervals (CIs) around these estimates is a recommended strategy to plan for a plausible range of scenarios in the main study [42]. The table below illustrates the wide CIs around a standard deviation estimate from a small pilot study, demonstrating the need for conservative planning.
Table 2: Confidence Intervals for Standard Deviation from a Pilot Study Assumes a pilot study with n=20 samples finds a standard deviation (SD) of 10.0 CFU. The 95% CI for the true SD is calculated using a Chi-square distribution.
| Pilot Sample Size (n) | Observed Standard Deviation | Lower 95% CI for SD | Upper 95% CI for SD |
|---|---|---|---|
| 20 | 10.0 CFU | 7.7 CFU | 14.2 CFU |
Interpretation: A main study designed based on the point estimate of 10.0 CFU might be underpowered if the true population SD is closer to the upper confidence limit of 14.2 CFU. A conservative approach is to use the upper confidence limit for sample size calculation [42].
Experimental Protocols for Microbiological Pilot Studies
Protocol 1: Pilot Study for a Quantitative Microbiological Method
This protocol is designed for methods yielding continuous data, such as bioburden determination, viral titer assays, or quantitative PCR.
1. Objective: To estimate the variability (standard deviation) of measurements and assess the feasibility of the experimental protocol for a subsequent method comparison study.
2. Experimental Design:
- A minimum of n=20 replicates is recommended for estimating variability with a reasonable degree of precision [42].
- The replicates should cover a range of expected values (e.g., low, medium, and high bioburden levels) relevant to the method's application.
- If comparing to a reference method, test all replicates with both methods in a randomized sequence to minimize bias.
3. Workflow: The following diagram outlines the key steps in executing a pilot study for a quantitative method.
4. Data Analysis:
- Calculate Descriptive Statistics: Compute the mean, standard deviation (SD), and range of the measurements.
- Assess Distribution: Plot the data using a histogram or box plot to check for normality and identify potential outliers [45].
- Determine Confidence Interval for SD: Calculate the 95% CI for the standard deviation (as in Table 2) to understand the precision of your variability estimate.
5. Sample Size Calculation for Main Study:
Use the estimated parameters in a formal sample size formula. For comparing the means of two methods (two-sample t-test):
Sample Size per Group = f(α, β) * (2 * SD²) / (MID)²
Where:
f(α, β)is a constant based on chosen significance level (α, typically 0.05) and power (β, typically 0.8 or 0.9).SDis the standard deviation from the pilot (using the upper confidence limit is conservative).MIDis the minimally important difference to detect.
Protocol 2: Pilot Study for a Qualitative Microbiological Method
This protocol applies to tests with binary outcomes (e.g., positive/negative), such as sterility testing, presence of objectionable organisms, or PCR-based detection assays [17] [43].
1. Objective: To estimate the positive and negative agreement rates between a new and a reference method and to identify issues with test interpretation, contamination, or protocol adherence.
2. Experimental Design:
- Select a panel of 30-50 samples that are enriched for positives to ensure a sufficient number of positive results for analysis [43].
- Include samples with known status (confirmed positives and negatives) if possible.
- All samples are tested using both the new and the reference method by operators blinded to the results.
3. Workflow: The key steps for a qualitative method pilot study are shown below.
4. Data Analysis:
- Construct a 2x2 Table: Cross-tabulate the results from the new method against the reference method.
- Calculate Agreement Metrics:
- Positive Percent Agreement (PPA):
a / (a+c)(sensitivity) - Negative Percent Agreement (NPA):
d / (b+d)(specificity) - Overall Percent Agreement:
(a+d) / (a+b+c+d)
- Positive Percent Agreement (PPA):
- Report Feasibility: Document rates of invalid results, ambiguous interpretations, and protocol deviations.
5. Sample Size Calculation for Main Study:
Use the estimated PPA and NPA in a sample size formula for proportions. For example, to test whether PPA is above a performance goal (e.g., 95%):
Sample Size (for positives) = f(α, β) * [PPA*(1-PPA)] / (PPA - Performance Goal)²
A similar calculation is done for the negative group using the NPA. The pilot study provides the PPA/NPA estimates and informs the required number of positive and negative samples for the main study [43].
The Scientist's Toolkit: Essential Reagents and Materials
Successful execution of a pilot study for microbiological method verification relies on carefully selected reagents and materials. The following table details key solutions and their critical functions.
Table 3: Research Reagent Solutions for Microbiological Pilot Studies
| Reagent/Material | Function in Pilot Study | Key Considerations |
|---|---|---|
| Qualified Growth Media | Supports the growth and detection of microorganisms from test samples [17]. | Validate for pH, ionic strength, and osmolality. Must support growth of fastidious, aerobic, anaerobic organisms, yeasts, and molds relevant to the sample matrix [17]. |
| Indicator Organisms | Demonstrate medium suitability and method capability to detect target microbes [17]. | Include standard strains (e.g., from ATCC) and, critically, environmental isolates from the manufacturing facility to ensure ecological relevance [17]. |
| Neutralizing Agents | Inactivate antimicrobial properties of the product being tested to ensure accurate microbial recovery [17]. | Must be validated for efficacy against the specific product and confirmed to be non-toxic to the target microorganisms. |
| Reference Materials | Provide a known positive and negative control for qualitative tests, or a standardized value for quantitative assays [43]. | Essential for establishing the accuracy and reliability of the new method. Sourced from certified providers or well-characterized in-house stocks. |
| Data Collection Software | Manages and validates data collected during the pilot study [43]. | Ranges from Microsoft Excel with statistical functions to specialized packages (e.g., JMP, EP Evaluator). Automated transfer reduces human error [43]. |
Pilot studies are an indispensable strategic tool for planning rigorous and efficient microbiological method verification studies when prior data is limited. By focusing on feasibility assessment and estimating key parameters like variability and agreement rates, these small-scale investigations provide the empirical foundation for robust sample size calculations. Adopting the protocols outlined in this application note—using confidence intervals to account for estimate imprecision and systematically evaluating all aspects of the experimental workflow—enables researchers to design definitive studies that are adequately powered, logistically sound, and capable of yielding valid, generalizable conclusions. This approach ultimately enhances research quality and contributes to the reliable assurance of microbiological product quality and patient safety.
Method verification is the process whereby a laboratory demonstrates that it can satisfactorily perform a validated method [9]. In the context of microbiological methods, this is a critical requirement for laboratories in the food and feed testing and pharmaceutical sectors. Verification provides confidence that a method is executed correctly within a specific laboratory's environment and with its personnel. A core component of this process is the statistical justification for the sample size used during verification studies. A sample size that is too small may lead to inconclusive or erroneous conclusions about the method's performance, while an excessively large sample size wastes precious laboratory resources, time, and materials. This application note provides a structured framework for balancing the statistical rigor required for defensible data with the practical realities of resource constraints during microbiological method verification.
Theoretical Foundations: Validation and Verification
Distinguishing Between Validation and Verification
Understanding the distinction between method validation and method verification is fundamental. Method validation is the primary process of proving that a procedure is fit for its intended purpose. This is typically conducted through interlaboratory studies as detailed in standards like the ISO 16140 series [9]. In contrast, method verification is the subsequent act, described in ISO 16140-3, where a user laboratory demonstrates that it can properly perform a method that has already been validated [9]. The performance data generated during the validation phase provides the benchmark against which the laboratory's verification results are compared.
Key Performance Parameters
The validation and verification of microbiological methods focus on a set of key performance parameters, which differ between qualitative and quantitative methods. The table below summarizes these parameters based on pharmacopoeial requirements [46].
Table 1: Essential Validation Parameters for Microbiological Methods
| Validation Parameter | Qualitative Tests | Quantitative Tests | Identification Tests |
|---|---|---|---|
| Trueness | - (or used instead of LOD) | + | + |
| Precision | - | + | - |
| Specificity | + | + | + |
| Limit of Detection (LOD) | + | - (may be required) | - |
| Limit of Quantification (LOQ) | - | + | - |
| Linearity | - | + | - |
| Range | - | + | - |
| Robustness | + | + | + |
| Equivalence | + | + | - |
The Concept of "Right-Fit Rigor"
A "right-fit" approach to methodological rigor is essential for efficient and effective verification. The core principle is that the level of statistical rigor employed should be directly responsive to the level of certainty about the method's performance [47]. This certainty can be assessed along four dimensions:
- Context: How well is the testing environment and sample matrix understood?
- Maturity: How established is the method? Is it a well-known compendial method or a novel alternative?
- Precision: What level of accuracy and precision is required for the intended use of the results?
- Urgency: What are the time constraints for completing the verification?
This framework suggests that with less certainty, a lower level of rigor may be initially sufficient, focusing on rapid feedback. As certainty increases, for instance when verifying a method for a high-stakes product release, a higher level of rigor with more robust sample sizes is justified [47].
A Practical Framework for Sample Size Calculation
Determining an appropriate sample size is a critical step that balances statistical power with practical feasibility. The following workflow provides a logical path for making this determination.
Sample Size Scenarios and Recommendations
Based on the framework above, sample size decisions can be guided by the specific verification activity and the chosen standard.
Table 2: Sample Size Scenarios for Method Verification
| Scenario | Basis for Sample Size | Recommended n | Statistical Rationale | Resource Implication |
|---|---|---|---|---|
| Implementation Verification | ISO 16140-3 [9] | 1 food item (from validation study) | Demonstrate technical competence by replicating a known result. | Low |
| Food Item Verification | ISO 16140-3 [9] | Several challenging food items | Demonstrate method robustness across relevant, difficult matrices. | Medium |
| Qualitative Method (e.g., Sterility Test) | Pilot study & statistical modeling | 20-50 positive identifications [46] | Achieve a 90% confidence level in identification accuracy (e.g., for USP <1113>). | High (requires many samples) |
| Quantitative Method (e.g., Enumeration) | Power analysis for precision (e.g., CI width) | 5-15 replicates per matrix | Obtain a confidence interval for the mean count that is acceptably narrow for the intended purpose. | Medium to High |
Protocol for Resource-Aware Sample Size Calculation
This protocol provides a step-by-step guide for determining a feasible yet statistically sound sample size for a quantitative microbial enumeration test.
1. Define the Acceptance Criterion:
- Determine the maximum acceptable width of the confidence interval (CI) for the mean count. For example, you may require that the 95% CI of the mean count falls within ±0.5 log10 of the true mean.
2. Conduct a Pilot Study:
- Perform the enumeration test on a small, feasible number of replicates (e.g., n=5-7) from a homogeneous sample.
3. Estimate Variability:
- Calculate the standard deviation (SD) from the pilot study results.
4. Calculate the Required Sample Size:
- Use the formula for the confidence interval margin of error: ( ME = t * \frac{SD}{\sqrt{n}} )
- Rearrange to solve for ( n ): ( n = (t * \frac{SD}{ME})^2 )
- Where:
- ( n ) = required sample size
- ( t ) = t-statistic for the desired confidence level (e.g., ~2 for 95% CI with small n)
- ( SD ) = standard deviation from pilot study
- ( ME ) = desired margin of error
5. Iterate Based on Resources:
- If the calculated ( n ) is prohibitively high, consider:
- Re-evaluating the required margin of error (ME).
- Investigating sources of high variability that could be controlled.
- Justifying a larger, yet still acceptable, ME based on the method's intended use.
The Scientist's Toolkit: Research Reagent Solutions
The following reagents and materials are essential for successfully executing microbiological method verification protocols.
Table 3: Essential Reagents and Materials for Verification Studies
| Item | Function / Application | Key Considerations |
|---|---|---|
| Reference Microorganisms | Used for trueness, precision, LOD, and specificity studies. | Strains must be traceable to recognized culture collections. Selected based on the method's claimed scope [46]. |
| Compendial Nutrient Media | Serves as the reference method or control in equivalence testing. | Must be prepared and sterilized according to pharmacopoeial specifications (e.g., USP, Ph. Eur.) [46]. |
| Alternative (Proprietary) Media | The subject of the verification study. | Performance is compared against the compendial medium for equivalence [9]. |
| Neutralizing Agents | Critical for testing antimicrobial products; neutralizes the product's effect to allow microbial recovery. | Must be validated to show it inhibits antimicrobial effect without being toxic to microorganisms [46]. |
| Specified Sample Items | Representative samples (e.g., food categories, pharmaceutical products) used for verification. | For ISO 16140-3, includes one item from the validation study and several challenging items from the lab's scope [9]. |
Experimental Protocol: Verification of a Qualitative Method
This detailed protocol outlines the verification of a qualitative microbiological method, such as a pathogen detection assay, with a focus on a resource-conscious approach to sample size.
1. Objective: To verify the laboratory's competence in performing a validated qualitative method for the detection of Salmonella in a specific food matrix.
2. Scope and Applicability: This protocol is applicable to the verification of alternative (proprietary) methods that have been previously validated through an interlaboratory study as per ISO 16140-2 [9].
3. Materials and Reagents:
- See Table 3 for essential items.
- The validated alternative method kit (e.g., PCR-based, immunoassay).
- Reference method materials as defined in the method's validation document.
4. Experimental Workflow:
5. Sample Size Justification and Procedure:
- Sample Items: Select a minimum of 5 representative and challenging sample items from the laboratory's scope of testing. One item should be the same as that used in the original validation study (Implementation Verification) [9].
- Inoculation: Artificially inoculate samples with low levels (near the method's LOD) of the target microorganism (Salmonella) and also include uninoculated controls.
- Testing: Analyze all samples using both the alternative method being verified and the reference method concurrently.
- Replicates: For a qualitative method, the focus is on the number of independent samples rather than analytical replicates. A minimum of 20-50 data points (inclusive of positive and negative results) may be needed to reliably assess accuracy parameters like specificity and sensitivity [46].
6. Data Analysis and Acceptance Criteria:
- Construct a 2x2 contingency table to compare results from the alternative method against the reference method.
- Calculate performance metrics:
- Relative Accuracy: (Number of correct results / Total number of tests) * 100%. Must be statistically equivalent to the validation data.
- Specificity: (True Negatives / (True Negatives + False Positives)) * 100%. Must meet or exceed the validated threshold.
- Sensitivity: (True Positives / (True Positives + False Negatives)) * 100%. Must meet or exceed the validated threshold.
- The method is considered verified in the laboratory if all calculated metrics fall within the confidence intervals or meet the minimum performance criteria established in the validation study.
The Role of Inoculum Control and Handling Unexpected Counts
In microbiological method verification, the reliability of data is paramount. Achieving this reliability hinges on two fundamental, interconnected practices: meticulous inoculum control and robust procedures for handling unexpected microbial counts. The precision of inoculum preparation directly influences the outcome of quantitative tests such as bioburden and viral titer assays [17]. Consequently, any inconsistency in the starting material can lead to significant variability in final results, undermining the validity of the entire method.
Furthermore, the very nature of microbiological tests, where low counts follow a Poisson distribution rather than a linear one, makes understanding and controlling the inoculum even more critical [17]. When counts are low, random distribution can lead to substantial variations between aliquots, making it difficult to distinguish between a true process variation and an artifact of sampling. This technical note details standardized protocols for inoculum preparation and provides a logical framework for investigating out-of-specification (OOS) counts, thereby strengthening the scientific and regulatory standing of microbiological method verification studies.
Experimental Protocols
Key Research Reagent Solutions
The following reagents are essential for the execution of the protocols described in this document.
Table 1: Essential Research Reagents for Microbiological Method Verification
| Reagent Type | Function & Importance in Verification |
|---|---|
| Validated Growth Media | Supports growth of fastidious organisms; pH (e.g., 6.0-8.0) and osmolality must be validated as they can select for different microbial populations [17]. |
| Indicator Organisms (Aerobic & Anaerobic Bacteria, Yeasts, Molds) | Demonstrates medium's ability to support growth. Should be supplemented with environmental isolates from the specific manufacturing facility [17]. |
| Neutralizing/Inactivating Agents | Validated to inactivate antimicrobial properties of the product being tested, ensuring accurate recovery of low-level inoculums [17]. |
| Standardized Reference Strains | Provides a known, quantified inoculum for establishing accuracy and linearity of quantitative methods. |
Protocol 1: Standardized Inoculum Preparation for Quantitative Methods
This protocol ensures a consistent and known starting population of microorganisms for quantitative assays like bioburden and viral titer tests.
1. Principle To generate a homogenous microbial suspension of known concentration, which is critical for determining the accuracy, precision, and linearity of a quantitative microbiological method [17].
2. Materials
- Freshly subcultured reference strains (e.g., from ATCC) and relevant environmental isolates.
- Appropriate liquid growth medium (e.g., TSB).
- Sterile saline or phosphate-buffered saline (PBS) with diluents.
- McFarland standards or a calibrated spectrophotometer.
- Vortex mixer and sterile pipettes.
3. Procedure 1. Revival and Subculture: Revive frozen or lyophilized cultures and subculture onto appropriate solid media to obtain fresh, growing colonies (18-24 hours old). 2. Suspension Preparation: Harvest colonies and suspend in a sterile diluent to achieve a turbidity equivalent to a 0.5 McFarland standard (approximately 1-2 x 10^8 CFU/mL for bacteria). 3. Quantification and Dilution: - Perform serial dilutions in a validated diluent to achieve the target inoculum level for the specific assay. - Confirm the concentration of the final working inoculum by plate count or another validated method. - Critical Step: Mix the suspension thoroughly before each aliquot withdrawal to ensure an even, random distribution of organisms [17]. 4. Utilization: Use the prepared inoculum within a validated time frame to prevent significant changes in viability.
Protocol 2: Investigation of Unexpected Microbial Counts
This protocol provides a systematic workflow for responding to and investigating OOS microbial count results.
1. Principle To determine the root cause of an unexpected count—whether it is a true process deviation or an artifact of laboratory error—through a structured investigation process [17].
2. Materials
- Retained samples from the original test.
- Original and fresh batches of culture media and diluents.
- Records of incubator temperature charts and equipment calibration.
3. Procedure 1. Initial Assessment & Documentation: Immediately document the result and quarantine the sample. Review the analyst's raw data and calculation sheets for transcription errors. 2. Laboratory Investigation Phase: - Media Quality: Check the growth promotion records of the media batch used. Re-test with indicator organisms to confirm fertility. - Equipment & Environment: Verify calibration records for pipettes, incubators, and analytical balances. Review environmental monitoring data for the testing area for any excursions. - Technique Review: Interview the analyst to confirm adherence to the approved procedure, especially regarding mixing steps and incubation conditions. 3. Sample & Testing Re-evaluation: - If no lab error is found, prepare and test retained samples. The investigation should consider the possibility of Poisson distribution effects at low counts, where a 0.1 mL aliquot from a sample with 10 CFU/mL has a ~37% chance of containing no organisms [17]. - Test the product with and without a neutralizer to rule out inhibitory substances that may have been carried over. 4. Root Cause Determination & Reporting: Correlate all findings to assign a definitive root cause. Document the entire investigation in a formal report.
Diagram 1: Investigation workflow for unexpected counts
Integrating Sample Size Calculation in Method Verification
A critical, yet often overlooked, aspect of microbiological method verification is the justification of sample size. An underpowered verification study may fail to detect a true problem with the method, while an oversized study wastes resources and time, raising ethical concerns about resource allocation [48] [7] [49].
Key Components for Sample Size Calculation
When planning a verification study, researchers must define the following statistical parameters to determine the appropriate sample size:
Table 2: Key Components for Sample Size Calculation in Method Verification
| Component | Description | Consideration in Microbiological Context |
|---|---|---|
| Type I Error (Alpha, α) | Probability of a false positive (rejecting H₀ when true). Typically set at 0.05 [48] [7]. | The acceptable risk of concluding a method is unsuitable when it is actually suitable. |
| Type II Error (Beta, β) | Probability of a false negative (failing to reject H₀ when false). Power = 1-β [48] [7]. | The risk of incorrectly validating an unsuitable method. Power of 80% (β=0.2) is conventional [48]. |
| Effect Size (ES) | The minimal difference or effect the study needs to detect [48] [7]. | In recovery studies, this is the minimal acceptable recovery rate (e.g., 70% vs. 50%). For a comparison of means, it could be the expected difference in log counts. |
| Variability (Standard Deviation) | The inherent variance in the data [48]. | Estimated from pilot studies or historical data. High variability in microbial counts requires a larger sample size. |
| Dropout Rate | Anticipated rate of unusable data points [48] [49]. | Accounts for contaminated plates or invalid test runs. Final sample size = n / (1 - dropout rate). |
The fundamental relationship is that sample size increases with desired power, lower alpha (significance) levels, and smaller effect sizes to be detected, but decreases with larger effect sizes [7]. For quantitative methods like bioburden testing, where results are continuous (e.g., CFU/sample), a two-sample t-test comparison against a reference method is often appropriate. The formula for the sample size per group (n) is complex, but relies on the components in Table 2 [48] [7].
Diagram 2: Factors affecting required sample size
Impact of Poisson Distribution on Low Counts
For tests with low expected microbial counts, standard sample size calculations based on normal distribution may be inadequate. At low densities (e.g., <100 CFU/mL), microbial distribution in a liquid follows a Poisson distribution [17].
Table 3: Impact of Poisson Distribution on Aliquot Sampling
| True Concentration (CFU/mL) | Probability a 0.1 mL Aliquot Contains Zero CFU | Apparent Concentration (if 0/0.1 mL result) |
|---|---|---|
| 10 | exp(-10*0.1) = 36.8% | 0 CFU/mL (a 100% deviation) |
| 100 | exp(-100*0.1) = 0.0045% | ~100 CFU/mL (a negligible deviation) |
This non-linear behavior means that verification studies for methods expecting low counts must account for higher inherent variance or use larger sample volumes/aliquots to mitigate the Poisson effect and ensure the study is sufficiently powered [17].
Robust microbiological data requires an integrated approach that marries sound statistical planning with meticulous laboratory technique. Inoculum control is the foundational practice that ensures the reliability of quantitative results, while a structured investigation process for unexpected counts safeguards data integrity. By incorporating formal sample size calculations into the verification study design, researchers can produce scientifically defensible and statistically sound evidence that their microbiological methods are fit for purpose, ultimately supporting the development of safe and effective drug products.
Optimizing Sample Size for Multi-factorial or Complex Study Designs
Determining an appropriate sample size is a fundamental requirement in scientific research, ensuring studies are powered to detect effects of interest while using resources efficiently. For multi-factorial or complex study designs—increasingly common in microbiological method verification, behavioral intervention research, and clinical trials—traditional sample size calculation methods are insufficient. This application note provides researchers, scientists, and drug development professionals with advanced methodologies and practical protocols for sample size optimization in complex experimental designs, including full factorial experiments, Sequential Multiple Assignment Randomized Trials (SMART), and the Multiphase Optimization Strategy (MOST). By integrating rigorous statistical principles with domain-specific requirements, these protocols support the development of robust, efficient, and ethically sound study designs.
In microbiological method verification and drug development, research questions often extend beyond simple group comparisons to investigate multiple factors, sequential decision rules, or intervention components simultaneously [9] [31]. Traditional randomized controlled trials (RCTs) evaluate interventions as complete packages, which limits their ability to isolate the effects of individual components or understand their interactions [50]. This insufficiency has driven the adoption of complex designs that can efficiently address multifaceted research questions.
The Multiphase Optimization Strategy (MOST) is an engineering-inspired framework for developing and optimizing behavioral interventions by testing individual components [50] [51]. Sequential Multiple Assignment Randomized Trials (SMART) represent another complex design used to build adaptive interventions where treatment sequences are individualized based on participant response [52]. In microbiology, the ISO 16140 series provides standardized approaches for method validation and verification, often requiring multi-factorial experimental designs to establish method performance across different food categories, sample matrices, and microbial strains [9] [11].
Each complex design presents unique sample size challenges. This application note addresses optimization strategies for these designs within the context of microbiological method verification and broader drug development research.
Foundational Principles of Sample Size Calculation
Core Statistical Relationships
Statistical power analysis balances four interrelated elements: significance level (α), statistical power (1-β), effect size (ES), and sample size (N). Understanding their relationships is prerequisite to optimizing complex designs [7].
- Significance Level (α): The probability of rejecting a true null hypothesis (Type I error). Typically set at 0.05, but may be lowered (e.g., 0.01) when false positives have severe consequences, or raised (e.g., 0.10-0.20) in pilot studies [7].
- Statistical Power (1-β): The probability of correctly rejecting a false null hypothesis. A power of 0.80 is conventionally considered adequate, indicating an 80% chance of detecting a specified effect if it truly exists [7].
- Effect Size (ES): The magnitude of the phenomenon under investigation. This must be defined as a scientifically meaningful difference, often derived from pilot data, previous literature, or theoretical considerations [53] [7].
- Sample Size (N): The number of experimental units required to achieve the desired power for detecting the specified effect size at the chosen significance level [7].
Any change to one element necessitates adjustments to at least one other to maintain the same statistical properties. For example, detecting a smaller effect size requires a larger sample size to maintain constant power and alpha.
Power Analysis for Complex Mediational Models
Mediation analysis examines the mechanism—through a mediator variable—by which an independent variable affects a dependent variable. Power analysis for such models requires specialized approaches beyond basic formulas [53].
The Satorra and Saris (1985) method estimates power in Structural Equation Models (SEM), including mediational models, through these steps:
- Define all parameters in the population model based on theory or pilot data.
- Generate a covariance matrix from these parameters.
- Analyze this matrix under a constrained model where parameters of interest are fixed (e.g., to zero).
- Use the resulting likelihood ratio statistic as a non-centrality parameter (λ) to compute power [53].
Power is the probability that a test statistic from a non-central χ² distribution exceeds the critical value from a central χ² distribution. Monte Carlo simulation provides a more flexible, modern approach for estimating power in complex models, including those with multiple mediators, latent variables, or categorical outcomes [53].
Sample Size Optimization for Specific Complex Designs
Full Factorial Designs
Full factorial designs investigate multiple factors (independent variables) simultaneously, each at two or more levels, by including all possible factor-level combinations. This enables estimation of both main effects and interaction effects [54].
Table 1: Types of Full Factorial Designs
| Design Type | Factor Levels | Key Application | Advantages | Sample Size Consideration |
|---|---|---|---|---|
| 2-Level Full Factorial | Two levels per factor (e.g., High/Low) | Screening experiments to identify active factors | Efficiently identifies significant main effects; assumes linearity | Number of runs = Lᴷ (K factors, L=2 levels) |
| 3-Level Full Factorial | Three levels per factor (e.g., Low/Medium/High) | Response surface modeling | Detects curvature (quadratic effects) in responses | Number of runs = Lᴷ (K factors, L=3 levels); grows rapidly |
| Mixed-Level Full Factorial | Different factors at different levels | Real-world scenarios with mixed categorical/continuous factors | Accommodates both numerical and categorical factors | Number of runs = (L₁ × L₂ × ... × Lᴷ); can be resource-intensive |
The total number of experimental runs required for a full factorial design is the product of the levels of all factors. For example, a 2⁴ design (4 factors at 2 levels each) requires 16 unique experimental runs. Replication (multiple runs under identical conditions) is necessary to estimate experimental error and enhance the reliability of effect detection [54]. The required sample size is the total number of runs multiplied by the number of replicates per run.
The Multiphase Optimization Strategy (MOST)
MOST is a framework for optimizing multicomponent interventions through three phases: Preparation, Optimization, and Evaluation [50] [51]. The Optimization phase typically employs a factorial design to screen and refine intervention components efficiently.
In a factorial experiment within MOST, multiple intervention components are randomized simultaneously. This design allows researchers to test the main effect of each component and interaction effects between components using a smaller sample size than required by a series of traditional RCTs [50] [51]. The sample size for the factorial experiment in the Optimization phase must be powered to detect the smallest effect size of clinical or practical importance for the main effects of the individual components.
Sequential Multiple Assignment Randomized Trials (SMART)
SMART designs are used to develop adaptive interventions (AIs), where a sequence of treatment decisions is tailored to the individual patient based on evolving needs and response [52].
Table 2: Key Considerations for SMART Design Sample Size
| Aspect | Description | Impact on Sample Size |
|---|---|---|
| Primary Research Question | Often a comparison between two or more embedded Adaptive Interventions (AIs) | Power calculation should be based on this primary comparison. |
| Response Rates | Proportion of participants re-randomized at each stage (e.g., non-responders to first-stage treatment) | Lower response rates may require a larger initial sample to ensure adequate power for second-stage comparisons. |
| Multiple Comparisons | Several AIs can be embedded and compared within a single SMART. | May require adjustment of alpha levels or use of multiple-objective optimal design strategies [52]. |
| Optimal Allocation | Unequal randomization probabilities may be more efficient or ethical than equal allocation. | Can maximize power for a fixed sample size or minimize sample size for a fixed power [52] [55]. |
In a prototypical SMART with two stages, participants are first randomized to an initial treatment. Responders continue their treatment, while non-responders are re-randomized to a subsequent treatment option. The sample size must ensure sufficient non-responders are available for meaningful second-stage randomization and analysis [52]. Optimal allocation methodologies can be applied to determine the most statistically efficient or ethically favorable randomization proportions across stages, rather than defaulting to equal allocation [52] [55].
Experimental Protocols for Microbiological Method Verification
The following protocols integrate principles of complex design and sample size optimization into microbiological method verification, guided by standards such as the ISO 16140 series [9].
Protocol 1: Verification of a Compendial Alternative Method
Objective: To verify that a rapid microbiological method (RMM) performs equivalently to a compendial reference method for a specific product or material, as per requirements in USP General Notices 6.30 [11].
Key Materials: Table 3: Research Reagent Solutions for Microbiological Verification
| Reagent/Material | Function/Description | Example/Standard |
|---|---|---|
| Reference Strains | Well-characterized microorganisms used to challenge the method. | ATCC or NCTC strains relevant to the product bioburden. |
| In-House Isolates | Environmental or product isolates representing the actual microbial population in the facility. | Should be justified if used instead of reference strains [11]. |
| Culture Media | Supports the growth and recovery of challenge microorganisms. | Fluid thioglycollate or other media per method requirement; recovery must be demonstrated [11]. |
| Neutralizing Agents | Inactivates antimicrobial properties of the product being tested. | Specific to the product formulation; effectiveness must be validated. |
Procedure:
- Define Scope and Acceptance Criteria: Specify the products/matrices covered and predefined acceptance criteria for agreement with the reference method (e.g., percentage concordance).
- Select Microorganisms: Include a panel of representative strains, including specified reference strains and, if justified, in-house isolates or slow-growing microorganisms relevant to the product risk assessment [11].
- Determine Sample Size: For a qualitative method verification, a minimum sample size per microorganism is required. A minimum of 3 replicates per organism is common, but more replicates may be needed to achieve a statistically sound design or if variability in inoculum control is high [11].
- Inoculation and Testing: Artificially contaminate the product with a low level (typically not more than 10 CFU) of each challenge microorganism. Test the inoculated samples in parallel using the alternative method and the reference method.
- Data Analysis: Compare results from both methods. Calculate the percentage agreement (or discrepancy rates). Performance must meet or exceed the pre-defined acceptance criteria.
Protocol 2: Multi-factorial Validation of a Microbiological Method for a Broad Range of Foods
Objective: To validate an alternative microbiological method for a "broad range of foods" according to ISO 16140-2, which requires testing a minimum of five different food categories out of fifteen defined categories [9].
Key Materials:
- Food samples spanning at least 5 different categories (e.g., heat-processed milk products, raw poultry, ready-to-eat vegetables).
- Challenge microorganisms relevant to each food category.
- Reference method as defined in the standard.
Procedure:
- Experimental Design: This is an inherent multi-factorial design with factors being Food Category (at least 5 levels) and Microorganism (multiple levels). The design must account for potential interactions between food matrix and microbial recovery.
- Sample Size and Replication: The validation includes testing a sufficient number of naturally contaminated or artificially inoculated samples per food category-microorganism combination. The ISO 16140-2 protocol specifies the exact number of replicates and samples required for the statistical comparison (e.g., for qualitative methods, 20 negative and 20 positive samples per food category might be tested against the reference method) [9].
- Execution: For each food category and microorganism combination, perform testing with both the alternative and reference methods according to the prescribed protocol.
- Statistical Analysis: Analyze data for each food category separately and collectively. Performance characteristics like relative accuracy, relative detection level, and inclusivity/exclusivity are calculated. Successful validation across the five categories allows the method's scope to be extended to the entire "broad range of foods" [9].
Optimizing sample size in multi-factorial and complex study designs is a critical step that balances statistical rigor with practical feasibility. Moving beyond one-size-fits-all formulas requires a deep understanding of the specific design architecture—whether it be a factorial experiment in a MOST framework, a SMART for building adaptive interventions, or a multi-factorial validation study in microbiology. By applying the protocols and principles outlined in this document, researchers in microbiology and drug development can design more efficient, informative, and powerful studies, ultimately accelerating the development and verification of robust scientific methods and interventions.
Ensuring Compliance: Validation Against Standards and Comparative Analysis
Aligning with Regulatory and Compendial Requirements (USP, ISO)
Microbiological method verification is a critical laboratory process that demonstrates a testing facility can competently perform a previously validated method and achieve the stated performance characteristics [9]. In the regulated pharmaceutical environment, this practice is not merely a formality but a mandatory requirement to ensure the reliability, accuracy, and reproducibility of test results used for product quality assessment and release. The process provides documented evidence that a method is suitable for its intended purpose within the specific laboratory environment [17].
The current regulatory landscape for microbiological methods is defined primarily by two key compendial frameworks: the International Organization for Standardization (ISO) 16140 series and the United States Pharmacopeia (USP). The ISO 16140 series provides a structured protocol for the validation and verification of microbiological methods in the food and feed chain, with principles that are widely applicable to pharmaceutical contexts [9]. Concurrently, the USP continually updates general chapters such as 〈1113〉, 〈1117〉, and 〈1223〉 to address microbial identification, best laboratory practices, and validation of alternative microbiological methods specifically for pharmaceutical quality control [56].
For researchers designing studies on sample size calculation, understanding the nuanced requirements of these frameworks is essential. This document provides detailed application notes and experimental protocols to guide the design and execution of microbiological method verification studies that align with compendial requirements, with particular emphasis on statistically sound sample size determination.
Regulatory and Compendial Frameworks
ISO 16140 Series Framework
The ISO 16140 series, titled "Microbiology of the food chain - Method validation," has evolved into a multi-part standard that comprehensively addresses method validation and verification. The series' structure and its relevance to verification studies are outlined in Table 1 [9].
Table 1: Parts of the ISO 16140 Series Relevant to Method Verification
| Part | Title | Scope and Application |
|---|---|---|
| ISO 16140-2 | Protocol for the validation of alternative (proprietary) methods against a reference method | Base standard for alternative methods validation; includes method comparison and interlaboratory study protocols for qualitative and quantitative methods [9]. |
| ISO 16140-3 | Protocol for the verification of reference methods and validated alternative methods in a single laboratory | Defines the two-stage verification process: implementation verification and item verification [9]. |
| ISO 16140-4 | Protocol for method validation in a single laboratory | Applicable when validation is conducted within one laboratory without an interlaboratory study; verification per ISO 16140-3 is not applicable in this case [9]. |
A critical distinction within the ISO framework is the clear separation between method validation and method verification. Validation is the primary process of proving a method is fit for its purpose, typically involving a method comparison study and an interlaboratory study [9]. In contrast, verification is the subsequent process where a laboratory demonstrates it can satisfactorily perform a method that has already been validated [9]. The ISO 16140-3 standard specifically outlines a two-stage verification process:
- Implementation Verification: The laboratory demonstrates it can correctly perform the method by testing one of the same items used in the original validation study.
- Item Verification: The laboratory demonstrates its capability to test challenging food items within its specific scope of application [9].
United States Pharmacopeia (USP) Framework
The USP provides continuously updated standards for pharmaceutical microbiology. Recent revisions reflect a shift toward risk-based approaches, modern technologies, and clearer data integrity expectations.
Table 2: Key USP General Chapters Governing Microbiological Methods
| USP Chapter | Title | Key Focus Areas in Recent Revisions |
|---|---|---|
| 〈1113〉 | Microbial Identification, Characterization, and Strain Typing | Modernization of identification strategies; incorporation of MALDI-TOF MS and Whole Genome Sequencing; replacement of "verification" with "qualification" for methods [56]. |
| 〈1117〉 | Microbiological Best Laboratory Practices | Enhanced details on media QC, equipment calibration, data integrity (ALCOA principles), and risk assessments for investigations [56]. |
| 〈1223〉 | Validation of Alternative Microbiological Methods | Guidance for validating rapid microbiological methods (RMM); harmonized with PDA Technical Report 33 [57]. |
A significant terminological update in USP 〈1113〉 is the replacement of "verification" with "qualification" when referring to microbial identification methods. This "Qualification" emphasizes accuracy, reproducibility, specificity, and database validation, often achieved through parallel testing, stock culture challenges, and reference laboratory comparisons [56]. Furthermore, USP revisions increasingly emphasize the application of ALCOA principles (Attributable, Legible, Contemporaneous, Original, Accurate) to microbiological data, recognizing the challenges of manual methods and the role of validated automated systems [56].
Sample Size Considerations for Verification Studies
Determining an appropriate sample size is a critical statistical component of method verification study design. The sample size must provide sufficient statistical power to demonstrate method performance with confidence while remaining practically feasible.
Quantitative Method Sample Size
For quantitative methods, sample size directly impacts the confidence in the estimated mean and the ability to detect differences relative to a reference method. The statistical basis accounts for expected variability and desired precision. The Poisson distribution becomes particularly important at low microbial counts, where random distribution effects are more pronounced [17]. When microbial concentrations are high, linear averaging is effective. However, with low counts (e.g., <100 CFU/mL), the Poisson distribution dictates that a 0.1 mL aliquot from a 10 CFU/mL sample has a significant probability (approximately one-third) of containing zero organisms, fundamentally influencing count accuracy and required replication [17].
Qualitative Method Sample Size
For qualitative (presence/absence) methods, sample sizes are often based on demonstrating a specific level of detection or probability of detection. Regulatory guidelines frequently provide minimum sample numbers for verification. The ISO 16140-2 standard, for instance, specifies that validating a method for a "broad range of foods" requires testing a minimum of 5 out of 15 defined food categories [9]. This principle is directly transferable to pharmaceutical verification when dealing with different product matrices.
Experimental Protocols for Method Verification
Protocol 1: Verification of a Quantitative Bioburden Method
1.0 Objective: To verify a laboratory's ability to accurately recover and enumerate microorganisms using a validated quantitative bioburden method on a specific product type.
2.0 Scope: Applicable to the membrane filtration method for determining Total Aerobic Microbial Count (TAMC) and Total Yeast and Mold Count (TYMC) on a new parenteral drug solution.
3.0 Materials and Reagents:
- Soybean-Casein Digest Agar (SCDA) plates
- Sabouraud Dextrose Agar (SDA) plates
- Sterile membrane filtration units (0.45µm pore size)
- Sterile dilution fluid (e.g., Buffered Sodium Chloride-Peptone Solution)
- Reference strains: Staphylococcus aureus (ATCC 6538), Pseudomonas aeruginosa (ATCC 9027), Bacillus subtilis (ATCC 6633), Candida albicans (ATCC 10231), Aspergillus brasiliensis (ATCC 16404)
4.0 Experimental Design and Sample Size:
- A minimum of 3 independent batches of the product will be tested.
- For each batch, prepare 5 replicates per dilution for the test method.
- Include method suitability controls as per USP 〈61〉 using the listed reference strains at a target inoculum of <100 CFU.
- The sample size justification is based on capturing product batch-to-batch variability with triplicate batches and providing sufficient data points for a preliminary statistical analysis of variance with 5 replicates per batch.
5.0 Procedure:
- Sample Preparation: Aseptically combine the contents of multiple product vials to create a homogeneous pool for each batch.
- Inoculation: For each batch, inoculate separate product aliquots with a low level (approximately 50-100 CFU) of each reference strain individually.
- Filtration and Analysis: Process each inoculated aliquot per the validated membrane filtration method. Filter the product, rinse the membrane, and transfer it to SCDA (for bacteria) and SDA (for yeasts and molds) plates.
- Incubation: Incubate SCDA plates at 30-35°C for 3-5 days and SDA plates at 20-25°C for 5-7 days.
- Enumeration: Count CFUs on all plates after incubation.
6.0 Acceptance Criteria:
- The method is considered verified if the average recovery of each reference strain from the product is ≥ 70% of the average recovery from the control (dilution fluid without product) [17].
- The Coefficient of Variation (CV) between replicates should not exceed 15% for homogeneous suspensions.
Protocol 2: Verification of a Qualitative Sterility Test Method (Rapid Method)
1.0 Objective: To verify a laboratory's performance of a validated rapid microbiological method (RMM) for sterility testing against the compendial membrane filtration method.
2.0 Scope: Applicable to an ATP-bioluminescence-based RMM for detecting microbial contamination in a sterile injectable product.
3.0 Materials and Reagents:
- Growth Direct System or equivalent RMM [57]
- Fluid D and Fluid A as per USP 〈71〉
- Sterile membrane filtration units
- Reference strains: Staphylococcus aureus (ATCC 6538), Pseudomonas aeruginosa (ATCC 9027), Bacillus subtilis (ATCC 6633), Clostridium sporogenes (ATCC 19404), Candida albicans (ATCC 10231), Aspergillus brasiliensis (ATCC 16404)
4.0 Experimental Design and Sample Size:
- Test a panel of 6 representative objectionable microorganisms.
- For each microorganism, test 5 replicates at a low inoculum level (approximately 10-100 CFU).
- Include 5 negative controls (uninoculated product) for each method.
- This sample size (N=5 per organism) provides a >99% probability of detecting a positive result if the method is working, assuming a Poisson distribution for low-level inoculates [17].
5.0 Procedure:
- Sample Preparation: Aseptically pool sterile product.
- Inoculation: Inoculate separate product units with a low level of each challenge organism.
- Parallel Testing: Process each inoculated unit and negative control in parallel using both the RMM and the compendial method.
- Incubation/Analysis: Follow the manufacturer's instructions for the RMM (e.g., incubation and autofluorescence detection). For the compendial method, incubate for 14 days as per USP 〈71〉.
- Result Comparison: Record positive/negative results for both methods at the RMM's time-to-result and at the 14-day compendial method endpoint.
6.0 Acceptance Criteria:
- The RMM must demonstrate 100% detection of all challenge organisms inoculated into the product (no false negatives).
- The RMM must demonstrate 100% negative agreement with the compendial method for the uninoculated controls (no false positives).
- The RMM's time-to-result must be at least 50% faster than the conventional method [57] [58].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of verification protocols requires carefully selected and qualified materials. The following table details key reagents and their critical functions.
Table 3: Essential Research Reagents for Microbiological Method Verification
| Reagent/Material | Function in Verification | Key Quality Attributes & Considerations |
|---|---|---|
| Reference Microorganism Strains | Challenge organisms used to demonstrate recovery and detection capability of the method. | Use ATCC or equivalent traceable strains. Maintain proper viability and avoid excessive subculturing to prevent genetic drift [17]. |
| Culture Media (Agar & Broths) | Supports the growth and recovery of microorganisms from the test product. | Must be qualified to support growth of appropriate indicators. pH, osmolality, and presence of selective agents can drastically impact recovery [17]. |
| Neutralizing/Inactivating Agents | Inactivates antimicrobial properties of the product (preservatives, antibiotics) that may inhibit microbial growth. | The choice of agent (e.g., lecithin, polysorbate) depends on the product's antimicrobial properties. Must be validated for effectiveness and non-toxicity to microbes [17]. |
| Standardized Diluents | Used for serial dilution of samples and preparation of inoculum suspensions. | Must be sterile and not support or inhibit microbial growth (e.g., Buffered Sodium Chloride-Peptone Solution). Ionic strength and pH can affect microbial stability [17]. |
| Validated Rapid Method Kits/Cartridges | Pre-configured components for RMMs like endotoxin testing or nucleic acid amplification. | Must be stored and handled per manufacturer's specifications. Lot-to-lot consistency is critical. Requires initial qualification upon adoption [57]. |
Aligning microbiological method verification with compendial requirements from USP and ISO is a foundational activity in pharmaceutical quality control. A scientifically rigorous approach, grounded in a thorough understanding of these frameworks, ensures that generated data is reliable and defensible. The experimental protocols and sample size justifications provided herein offer a practical roadmap for researchers and scientists. Particular attention must be paid to the distinct definitions of validation, verification, and qualification within the relevant standards, as well as the critical role of sample size in achieving statistically meaningful results. As regulatory expectations continue to evolve—increasingly favoring risk-based approaches, modernized technologies, and robust data integrity—the principles outlined in this document will support the development of compliant, efficient, and scientifically sound verification protocols.
Method verification is a critical process in the microbiological laboratory, ensuring that testing methods are fit for their intended purpose and that the laboratory can perform them competently. Within the framework of the ISO 16140 series, verification is defined as the process a laboratory uses to demonstrate it can satisfactorily perform a validated method [9]. This is distinct from method validation, which is the initial process of proving a method is fit-for-purpose. For researchers designing studies on sample size calculation, understanding this two-stage verification process—comprising Implementation Verification and Item Verification—is fundamental to generating reliable and defensible data.
This document outlines detailed application notes and protocols for this two-stage process, providing a structured approach for researchers, scientists, and drug development professionals.
The Two-Stage Verification Framework
The ISO 16140-3 standard formalizes a two-stage approach for the verification of validated microbiological methods in a single laboratory [9]. This structured process ensures that a laboratory not only can execute the method technically but also that the method performs adequately for the specific sample types (items) the laboratory tests.
Stages of Method Verification:
| Stage | Primary Objective | Key Requirement |
|---|---|---|
| Stage 1: Implementation Verification | To demonstrate the user laboratory can perform the method correctly by replicating the conditions and outcomes of the original validation study [9]. | Testing one or more of the exact same food items that were evaluated in the initial validation study [9]. |
| Stage 2: Item Verification | To demonstrate the laboratory can accurately test the challenging food items within its own specific scope of testing [9]. | Testing several food items that are representative of the laboratory's routine testing scope, using defined performance characteristics [9]. |
The following workflow diagram illustrates the logical sequence and decision points within this two-stage verification process.
Stage 1: Implementation Verification
Objective and Rationale
The purpose of Implementation Verification is to provide a direct comparison between the performance of the user laboratory and the performance data generated during the original validation study. By testing the same food items, the laboratory can confirm that its analysts, equipment, and environment are capable of producing results consistent with the method's validated performance criteria [9]. This step is crucial for establishing a baseline of competence before applying the method to a wider range of samples.
Experimental Protocol
1. Scope Definition:
- Identify the specific method to be verified, including its unique identifier and version.
- Obtain a sample of one or more food items that were explicitly used in the method's validation study. The choice of item should challenge the method's critical steps [9].
2. Sample Preparation:
- Follow the sample preparation procedure as defined in the method's standard operating procedure (SOP).
- If the validation study used artificially contaminated samples, replicate the inoculum level, strain(s), and conditioning time as closely as possible.
3. Testing and Data Generation:
- Perform the entire method a minimum of n=5 times for quantitative methods or test a minimum of n=20 replicates for qualitative methods on the selected food item. These sample sizes provide a reasonable degree of confidence for comparing results.
- All testing must be performed by the analysts who will routinely use the method, under standard laboratory conditions.
4. Data Analysis and Acceptance Criteria:
- For quantitative methods (e.g., colony counts), calculate the mean and standard deviation. The mean result should fall within the confidence intervals of the validation data or meet pre-defined accuracy and precision targets (e.g., ±0.5 log from the reference value).
- For qualitative methods (e.g., presence/absence), the results must demonstrate 100% concordance with the expected outcomes (positive or negative) established in the validation study.
Stage 2: Item Verification
Objective and Rationale
Item Verification ensures the method is robust enough to handle the specific, and often challenging, sample matrices within the laboratory's scope of accreditation or routine testing [9]. This stage is critical because a method validated on a broad range of foods (e.g., 5 out of 15 defined food categories) may behave differently with a specific, untested matrix due to factors like fat content, pH, or natural microbiota.
Experimental Protocol and Sample Size Calculation
1. Item Selection Strategy:
- Select a representative set of food items from the different categories and sub-categories the laboratory tests. The selection should be risk-based, prioritizing items that are most challenging, most frequently tested, or most critical to patient safety and product quality [59].
- The following table provides a guideline for the minimum number of items to test based on the scope of the laboratory's application.
Table 1: Item Verification Sample Size Guidelines
| Scope of Laboratory Testing | Minimum Number of Items to Verify | Key Considerations |
|---|---|---|
| A single food category (e.g., dairy products) | 3-5 items | Select items that represent the diversity within the category (e.g., liquid milk, cheese, powdered milk). |
| A broad range of food categories (e.g., "broad range of foods" per ISO 16140-2) | 5-8 items | Select at least one item from 5 different high-level food categories (e.g., meat, produce, dairy, ready-to-eat, spices). |
| A specific, challenging matrix (e.g., probiotic supplements) | 1-2 items, with increased replication | Focus on demonstrating consistency in a high-interference environment. Higher replication (n≥10) may be necessary. |
2. Testing and Data Generation:
- For each selected item, perform the method a minimum of n=3 times for quantitative methods or n=5 times for qualitative methods. This replication accounts for the inherent variability in microbiological testing [59].
- The samples can be tested at a single contamination level (near the specification or action limit) or at multiple levels to assess linearity and limit of detection.
3. Performance Characteristics and Acceptance Criteria:
- Define the performance characteristics to be verified. These typically include:
- Accuracy/Precision: For quantitative methods, the relative standard deviation (RSD) of replicates should be within acceptable limits for the method type.
- Specificity/Selectivity: The method should correctly identify target organisms without significant interference from the sample matrix.
- Limit of Detection (LOD): For qualitative methods, the method should reliably detect the target microorganism at the claimed LOD.
The following diagram outlines the decision-making process for determining when second analyst verification, a key quality measure, is necessary during routine testing after method verification is complete.
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful execution of a verification study relies on high-quality, standardized materials. The following table details key reagents and their functions.
Table 2: Essential Materials for Microbiological Method Verification
| Item | Function & Importance in Verification |
|---|---|
| Reference Strains | Well-characterized microbial strains (e.g., from ATCC, NCTC) used to spike samples. They are critical for determining accuracy, precision, and Limit of Detection (LOD) in both verification stages [9]. |
| Validated Food Items | Food samples that were part of the method's original validation study. They are essential for the Implementation Verification stage to benchmark laboratory performance against validation data [9]. |
| Challenging Lab-Specific Items | Representative and difficult sample matrices from the laboratory's own scope of testing. They are the focus of Item Verification to demonstrate method robustness under real-world conditions [9]. |
| Selective and Non-Selective Media | Culture media used for growth, isolation, and enumeration. Performance is verified by assessing recovery rates, selectivity, and the characteristic appearance of colonies [59]. |
| Gram Stain Reagents | Key reagents for microbial identification. Verification of a Gram stain method requires demonstrating accurate staining reactions and cellular morphology identification, often requiring a second analyst verification to prevent misidentification [59]. |
| Automated Colony Counters / Quebec Counters | Tools to aid in the accuracy and precision of quantitative results. Their use is a supplementary control to minimize human counting error during verification studies [59]. |
The two-stage verification process of Implementation and Item Verification provides a rigorous, scientifically sound framework for introducing microbiological methods into a laboratory. For researchers focused on sample size calculation, this protocol emphasizes that sample size is not a single number but is determined by the verification stage (implementation vs. item), the type of method (quantitative vs. qualitative), and the required confidence level. By adhering to this structured approach and utilizing the provided protocols, tables, and decision aids, professionals in drug development and research can ensure the integrity of their microbiological data, ultimately supporting product quality and patient safety.
Demonstrating the equivalence of a new or alternative microbiological method to a recognized reference method is a critical requirement in pharmaceutical development, clinical diagnostics, and food safety monitoring [60] [61]. This process ensures that test results are reliable, accurate, and fit for their intended purpose, thereby supporting safety-critical decisions [60]. Within a broader thesis on sample size calculation for microbiological method verification, this analysis provides detailed application notes and protocols, framing the entire process within the context of appropriate statistical power and sample size determination to ensure scientifically sound and defensible outcomes.
The fundamental framework for these activities is established by international standards, primarily the ISO 16140 series, which delineates protocols for both method validation (proving a method is fit-for-purpose) and method verification (proving a laboratory can correctly perform a validated method) [9] [61]. Adherence to these standards is often mandated by regulations, such as the European Regulation (EC) 2073/2005 for food safety and the Clinical Laboratory Improvement Amendments (CLIA) for clinical diagnostics in the United States [3] [61].
Key Concepts and Regulatory Framework
Distinguishing Between Validation and Verification
A clear understanding of the distinction between validation and verification is essential for planning and executing comparative studies.
- Method Validation is the comprehensive process of establishing, through extensive laboratory studies, that the performance characteristics of a new alternative method are equivalent to a reference method. This is required for laboratory-developed tests or modified FDA-approved tests and typically involves a method comparison study followed by an interlaboratory study to generate performance data [3] [9] [31]. Validation demonstrates that the method itself is scientifically sound.
- Method Verification is a subsequent, more focused process conducted by a single laboratory to demonstrate that it can successfully implement a method that has already been validated. This applies to unmodified, FDA-approved or cleared tests and confirms that the laboratory can achieve the established performance characteristics in its own environment [3] [9]. Verification demonstrates laboratory competency.
The following workflow outlines the journey from method development to routine use, highlighting the roles of validation and verification:
The ISO 16140 Series for Method Validation and Verification
The ISO 16140 series provides the definitive international standard for the validation and verification of microbiological methods in the food chain, with principles applicable to clinical and pharmaceutical microbiology [9] [61]. The series comprises several parts, each addressing a specific aspect of the process.
Table 1: Key Parts of the ISO 16140 Series for Method Equivalence
| Standard | Title | Primary Focus | Application in Research |
|---|---|---|---|
| ISO 16140-2 [9] | Protocol for the validation of alternative (proprietary) methods against a reference method | Defines the base protocol for validating alternative methods, including a method comparison study and an interlaboratory study. | Provides the statistical and experimental framework for generating performance data (e.g., LOD50, accuracy, precision) for a new method. |
| ISO 16140-3 [9] [61] | Protocol for the verification of reference methods and validated alternative methods in a single laboratory | Provides a harmonized protocol for a user laboratory to verify its competency in performing a validated method for its specific needs. | Critical for designing a laboratory's verification study, including sample size, selection of challenging items, and acceptance criteria. |
| ISO 16140-4 [9] | Protocol for method validation in a single laboratory | Used for validation studies conducted within a single laboratory, the results of which are only valid for that lab. | Applicable for initial in-house validation of laboratory-developed tests (LDTs) before a full interlaboratory study. |
| ISO 16140-6 [9] | Protocol for the validation of alternative (proprietary) methods for microbiological confirmation and typing procedures | Addresses validation of specific methods like biochemical confirmation or serotyping. | Guides the validation of methods used to confirm the identity or type of microbial isolates obtained from primary tests. |
Statistical Foundations and Sample Size Calculation
The determination of an appropriate sample size is a fundamental prerequisite in the design of any validation or verification study. An insufficient sample size risks a underpowered study that cannot reliably demonstrate equivalence, while an excessive sample size wastes valuable resources [36] [30].
The Two One-Sided Tests (TOST) Procedure
For analytical methods where the outcome is a continuous variable, the equivalence between a test and reference method is often demonstrated using the Two One-Sided Tests (TOST) procedure [62]. This method tests the joint null hypothesis that the test method is significantly different from the reference method, against the alternative hypothesis that the difference lies within a pre-specified equivalence margin (e.g., ±Δ). The TOST procedure is the statistical foundation for bioequivalence testing and is widely used in pharmaceutical development [62] [63].
Sample size calculation for a TOST-based equivalence study depends on several factors [62]:
- Significance Level (α): Typically set at 0.05.
- Statistical Power (1-β): The probability of correctly concluding equivalence when the methods are truly equivalent; often set at 80% or 90%.
- Equivalence Margin (Δ): The acceptable difference between the test and reference method. This must be defined a priori based on scientific and clinical judgment.
- Expected Variability (σ): The expected standard deviation of the measurements, often expressed as the coefficient of variation (CV).
Specialized statistical software (e.g., R with the PowerTOST package) is recommended for calculating sample sizes using the TOST procedure, as traditional formulas can be conservative and lead to overpowered studies, thus incurring unnecessary costs [62] [63].
Sample Size Considerations for Qualitative Microbiological Methods
In microbiology, many methods are qualitative (e.g., detection of a specific pathogen). The sample size for verification studies of these methods is often based on practical guidelines and standards rather than a single power calculation.
Table 2: Sample Size Guidance for Verification Studies of Qualitative Methods
| Characteristic | Recommended Sample Size | Experimental Design Notes | Standard / Source |
|---|---|---|---|
| Accuracy | Minimum of 20 samples [3] | Use a combination of positive and negative samples. Can include controls, proficiency test samples, or de-identified clinical samples. | CLIA / Clinical Microbiology [3] |
| Precision | Minimum of 2 positive and 2 negative samples, tested in triplicate for 5 days by 2 operators [3] | Evaluates within-run, between-run, and operator variance. If the system is fully automated, operator variance may not be needed. | CLIA / Clinical Microbiology [3] |
| Limit of Detection (LOD) | Variable number of replicates at low inoculum levels to estimate the LOD₅₀ [61] | The LOD₅₀ is the level that gives 50% positive results. The verified method's estimated LOD₅₀ (eLOD₅₀) must be ≤ 4x the validated LOD₅₀. | ISO 16140-3 [61] |
A Bayesian Model for Sample Size Estimation in Microbiological Surveys
For complex scenarios, such as estimating the sample size needed to identify all bacterial subtypes in a specimen, a Bayesian statistical model can be employed [36]. This model combines two key inputs:
- A prior distribution based on available scientific knowledge (e.g., an informed microbiologist's estimate of the number of strains per specimen).
- Observed data from an ongoing microbiological survey.
The output is an updated probability distribution of strains per specimen, which can be used to estimate the probability of observing all strains present given the number of colonies sampled [36]. This approach is particularly valuable for optimizing resource allocation, preventing both under-sampling (which leads to biased inferences) and over-sampling (which wastes resources) [36].
Experimental Protocols for Method Verification
The following protocols are adapted from ISO 16140-3 and CLIA guidelines, providing a practical framework for a laboratory to verify its implementation of a validated qualitative method [3] [9] [61].
Protocol 1: Verification of Accuracy
1. Objective: To confirm acceptable agreement between the results from the new method and a comparative method. 2. Experimental Design:
- Sample Size: A minimum of 20 clinically relevant isolates or samples [3].
- Sample Type: A combination of positive and negative samples. These can be derived from reference materials, proficiency tests, or de-identified clinical samples previously characterized by a validated method.
- Testing Procedure: Test all samples in parallel using the new method and the comparative (reference) method. 3. Data Analysis:
- Calculate the percentage agreement: (Number of results in agreement / Total number of results) × 100. 4. Acceptance Criterion:
- The percentage agreement must meet or exceed the manufacturer's stated claims or a level determined by the laboratory director [3].
Protocol 2: Verification of Precision (Reproducibility)
1. Objective: To confirm acceptable within-run, between-run, and operator variance. 2. Experimental Design:
- Sample Size: A minimum of 2 positive and 2 negative samples [3].
- Testing Procedure: Test each sample in triplicate, over the course of 5 days, by two different operators. 3. Data Analysis:
- Calculate the percentage agreement for all replicates: (Number of concordant results / Total number of results) × 100. 4. Acceptance Criterion:
- The percentage agreement must meet or exceed the manufacturer's stated claims or a level determined by the laboratory director [3].
Protocol 3: Verification of the Limit of Detection (LOD) for a Qualitative Method
1. Objective: To verify that the laboratory can achieve a Limit of Detection (LOD) comparable to the validated method. 2. Experimental Design:
- Sample Preparation: Inoculate a relevant food item or matrix with a low concentration of the target microorganism. The inoculum level should be around the validated LOD₅₀ of the method.
- Replicates: Test a sufficient number of replicates (e.g., 5-20) at this low inoculum level to estimate the LOD₅₀. 3. Data Analysis:
- Calculate the estimated LOD₅₀ (eLOD₅₀) based on the proportion of positive results obtained. 4. Acceptance Criterion (per ISO 16140-3):
- The eLOD₅₀ must be equal to or less than four times the validated LOD₅₀. If no LOD₅₀ is available, the eLOD₅₀ must be ≤ 4 CFU/test portion [61].
The following diagram summarizes the logical progression and decision points within a verification study:
The Scientist's Toolkit: Essential Research Reagent Solutions
The successful execution of equivalence studies relies on a suite of well-characterized biological and chemical reagents.
Table 3: Key Research Reagent Solutions for Equivalence Studies
| Reagent / Material | Function in Equivalence Studies | Application Example |
|---|---|---|
| Certified Reference Materials (CRMs) | Provides a benchmark with defined properties to calibrate equipment and validate methods. Used as a gold standard in accuracy studies. | Using a CRM for a specific microbial strain (e.g., Listeria monocytogenes) to confirm the identification capability of a new method. |
| Characterized Clinical Isolates | A panel of well-defined microbial strains from clinical or environmental sources. Essential for assessing method inclusivity (ability to detect target strains). | A panel of 20+ Campylobacter AFLP types from broiler carcasses used to verify a new detection method's accuracy [36]. |
| Proficiency Testing (PT) Samples | Blinded samples of known composition supplied by an external provider. Used for unbiased verification of a method's performance in a laboratory. | A PT sample containing Salmonella used to test the laboratory's ability to correctly detect the pathogen using the new method. |
| Inclusivity and Exclusivity Panels | A curated collection of target (inclusivity) and non-target (exclusivity) strains. Critical for verifying a method's specificity and lack of cross-reactivity. | Testing a Salmonella detection method with 5 pure target strains (inclusivity) and 5 non-target strains (exclusivity) with an acceptance limit of 100% concordance [61]. |
| Quality Control (QC) Strains | Strains with known positive and negative reactions for a test. Used for daily or weekly monitoring of test performance to ensure ongoing reliability. | Using a Staphylococcus aureus QC strain to verify the performance of a coagulase test before running patient samples. |
A robust comparative analysis to demonstrate equivalence to a reference method is a multifaceted process that hinges on careful experimental design, grounded in international standards and sound statistical principles. The calculation of an appropriate sample size is not a mere formality but a critical step that ensures the study has the necessary statistical power to provide conclusive evidence of equivalence. By adhering to the structured protocols for verification—assessing accuracy, precision, and limit of detection—and utilizing well-characterized reagents, researchers and laboratory scientists can generate defensible data that meets regulatory requirements. This rigorous approach ultimately ensures the reliability of microbiological testing, which is fundamental to safeguarding public health in pharmaceutical development, clinical diagnostics, and food safety.
Commercial sterility testing is a critical quality control imperative within the pharmaceutical, biotechnology, and food manufacturing industries. Confirming that products are free from viable contaminating microorganisms is a non-negotiable requirement for patient safety and product efficacy [64]. The core objective of this case study is to demystify the principles and application of sample size determination specifically for the verification of a commercial sterility testing method. This work is situated within a broader thesis on sample size calculation for microbiological method verification, addressing a common challenge faced by researchers and drug development professionals: justifying a statistically sound and regulatory-compliant sample size that balances risk, resources, and scientific rigor. We will explore a risk-based methodology for sample size selection, detail the experimental protocol for method verification, and provide a practical case study applying these principles.
Theoretical Framework for Sample Size Determination
Defining Commercial Sterility
A foundational concept is that commercial sterility does not imply the absolute absence of microorganisms. Rather, it confirms the absence of organisms capable of growing in the product under defined storage conditions, thereby presenting a spoilage or health risk throughout its shelf life [65]. This distinction is crucial, as it informs the purpose of the test—to detect relevant contaminants at a level that poses a risk.
Risk-Based Sample Size Selection
For sterility testing and related quality control checks, a common and accepted approach for attribute (pass/fail) data is the use of a risk-based method leveraging confidence and reliability levels [10]. This model answers the question: "With what level of confidence can I state that the true failure rate of my batch is less than a certain percentage (reliability)?"
The sample size is derived from a non-parametric binomial reliability model. The risk priority is first determined using a Risk Priority Number (RPN) derived from factors such as:
- Severity: The potential harm of a sterility failure to a patient.
- Occurrence: The likelihood of a sterility failure occurring.
- Detection: The probability that the test method will detect a failure if present [10].
Table 1: Correlation between Risk Priority and Statistical Confidence/Reliability Levels
| Risk Priority (RPN) | Recommended Confidence Level | Recommended Reliability Level |
|---|---|---|
| High | 95% | 95% |
| Medium | 95% | 90% |
| Low | 90% | 80% |
Once the confidence and reliability levels are established, the minimum sample size with zero allowable failures can be determined from a binomial reliability table.
Table 2: Minimum Sample Sizes for Sterility Test Validation (Zero Failures Allowed)
| Confidence Level | Reliability Level | Minimum Sample Size |
|---|---|---|
| 95% | 95% | 59 |
| 95% | 90% | 29 |
| 90% | 80% | 11 |
This sample size (e.g., 59 units for 95/95) represents the number of units that must be tested and must all pass to support the conclusion that the method is suitable for its intended use with the specified confidence [10].
Experimental Protocol for Method Verification
The following protocol outlines the key experiments for verifying a commercial sterility testing method, incorporating the sample size principles detailed above.
Method Suitability (Bacteriostasis and Fungistasis Test)
Before testing product samples, it is mandatory to demonstrate that the method itself does not inhibit microbial growth. This is achieved through the Bacteriostasis and Fungistasis (B&F) Test [64].
- Objective: To validate that the test system (product + culture media + procedure) can support the growth of low levels of microorganisms.
- Procedure:
- Inoculation: A small, known number (typically 10 to 100 CFU) of a panel of USP-specified microorganisms is inoculated into containers of culture media containing the product under test. The panel should include both aerobic and anaerobic bacteria, as well as fungi (e.g., Staphylococcus aureus, Pseudomonas aeruginosa, Bacillus subtilis, Clostridium sporogenes, Candida albicans, Aspergillus brasiliensis) [64].
- Incubation: The inoculated containers are incubated according to standard sterility test conditions: Fluid Thioglycollate Medium (FTM) at 30-35°C for 14 days and Soybean-Casein Digest Medium (SCDM) at 20-25°C for 14 days [64].
- Growth Comparison: The growth of the test organisms in the product-containing media is compared against control samples that contain only culture media and the same inoculum.
- Acceptance Criteria: The test method is suitable only if the growth of the microorganisms in the test samples is comparable to the control samples within the 14-day incubation period. A failure necessitates method modification, such as increasing rinse volumes in membrane filtration or adding inactivating agents [64].
Validation of the Test Method with Challenging Microorganisms
To demonstrate the method's detection capability, a validation study using a panel of relevant microorganisms is performed.
- Objective: To determine the method's Limit of Detection (LOD95) and inclusivity by confirming its ability to detect a wide range of relevant microorganisms at low levels in the presence of the product [66].
- Sample Size and Procedure:
- A minimum of three independent replicates for each microorganism in the panel should be performed for statistical significance.
- The product is artificially contaminated with a low level (e.g., <100 CFU) of each challenge organism.
- The full sterility test procedure (either Direct Inoculation or Membrane Filtration) is executed on the contaminated samples.
- The LOD95, defined as the lowest level of microorganism that can be detected 95% of the time, is calculated [66].
- Acceptance Criteria: The method should consistently detect all challenge organisms at the target inoculation level, demonstrating a low LOD95 and robust inclusivity.
Diagram 1: Experimental Workflow for Sterility Test Method Verification
Case Study: Application to a Novel Biologic Formulation
Scenario Definition
A biopharmaceutical company is developing a new parenteral biologic drug product preserved with a broad-spectrum antimicrobial. The quality team is tasked with verifying a compendial sterility testing method suitable for this inhibitory product.
- Product: High-value, preserved biologic solution.
- Challenge: The product's inherent antimicrobial properties pose a high risk of causing false-negative results using the Direct Inoculation method.
- Selected Method: Membrane Filtration, as it is considered the "gold standard" for such products because it separates potential contaminants from the inhibitory product matrix through washing [64].
Sample Size Justification and Experimental Execution
- Risk Assessment:
- Severity: A sterility failure in an injectable product is catastrophic for patient health. Score: 10.
- Occurrence: The complex manufacturing process for biologics carries a moderate risk. Score: 6.
- Detection: The inhibitory nature of the product makes detection challenging without a robust method. Score: 8.
- RPN = 10 × 6 × 8 = 480.
- Sample Size Selection: Based on the high RPN and Table 1, a 95% confidence and 95% reliability level was selected. Referring to Table 2, the required sample size with zero allowable failures is n = 59 [10].
The experimental verification was executed as follows:
- B&F Test: The initial test failed for Staphylococcus aureus and Candida albicans due to the product's preservative. The protocol was modified by incorporating a rinse solution containing polysorbate 80 and lecithin, after which the test passed for all organisms.
- LOD95 and Inclusivity Study: The method, with the modified rinse, was challenged with a panel of 6 microorganisms. All organisms at an inoculation level of <50 CFU were detected in all three replicates, confirming a low LOD95 and satisfactory inclusivity.
- Final Method Verification: The verified membrane filtration method was executed on 59 separate, uncontaminated units of the biologic product. All 59 units tested negative for microbial growth after the 14-day incubation period.
Based on the successful completion of the B&F test, the LOD95 study, and the testing of 59 units with zero failures, the membrane filtration method was declared verified and valid for routine sterility testing of the new biologic product. This outcome provides 95% confidence that the method is capable of detecting contaminants with 95% reliability.
It is critical to note that regulatory expectations for sterility testing are stringent. Testing must be performed in an ISO Class 5 environment (laminar flow hood or isolator), and all equipment used (e.g., incubators, automated systems like BacT/ALERT) must undergo full Installation, Operational, and Performance Qualification (IOPQ) to ensure data integrity and regulatory compliance [64] [67].
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Sterility Test Validation
| Item | Function in Validation |
|---|---|
| Fluid Thioglycollate Medium (FTM) | Culture medium designed to support the growth of anaerobic and aerobic bacteria. |
| Soybean-Casein Digest Medium (SCDM) | A general-purpose culture medium designed to support the growth of aerobic bacteria and fungi. |
| USP/EP Challenge Organisms | A standardized panel of microorganisms (e.g., S. aureus, P. aeruginosa, C. albicans) used to demonstrate method inclusivity and LOD95. |
| Membrane Filtration Apparatus | System featuring a 0.45µm membrane filter to trap microorganisms while allowing the inhibitory product to be washed away. |
| Inactivating Agents (Lecithin, Polysorbate) | Components added to rinse fluids to neutralize antimicrobial properties of the product on the filter membrane. |
| Automated Rapid Microbial Detection System | Systems like BacT/ALERT use culture bottles and automated sensors to detect microbial growth, offering faster results (2-3 days) than traditional visual inspection [65]. |
Diagram 2: Membrane Filtration Test Workflow
Documenting Your Calculation and Justification for Audits
Within the framework of a broader thesis on sample size calculation for microbiological method verification research, the ability to meticulously document and justify your selected sample size is not merely a procedural step—it is a scientific and regulatory imperative. For researchers, scientists, and drug development professionals, a well-documented sample size rationale provides the foundation for the credibility of verification data, demonstrates statistical confidence to auditors, and ensures that the method is proven to be fit-for-purpose before implementation in a quality control laboratory. This document outlines the regulatory context, statistical methodologies, and practical protocols for establishing and defending your sample size decisions.
Regulatory and Scientific Framework
Method verification is the process whereby a laboratory demonstrates that a previously validated method is performing as expected within the laboratory's specific environment and with its analysts [9]. This is distinct from method validation, which proves a method is fit for its intended purpose [9] [46].
The Regulatory Landscape
Adherence to established standards is non-negotiable. The following table summarizes key guidelines relevant to microbiological method verification and sample planning.
Table 1: Key Regulatory and Guidance Documents
| Standard / Guideline | Focus Area | Relevance to Sample Size |
|---|---|---|
| ISO 16140-3 [9] | Protocol for the verification of reference and alternative methods in a single laboratory. | Provides the framework for the two-stage verification process (implementation and item verification), which directly informs the scope and scale of testing. |
| USP <1223> [46] | Validation of alternative microbiological methods. | Defines required validation parameters (e.g., specificity, accuracy) for qualitative and quantitative methods; the demonstration of equivalence influences sample size. |
| European Pharmacopoeia 5.1.6 [46] | Alternative microbiological methods. | Requires a risk-benefit analysis and outlines validation parameters for different test types (qualitative, quantitative, identification), impacting the experimental design. |
| PDA Technical Report 33 [46] | Evaluation, validation, and implementation of alternative microbiological methods. | Serves as a supplemental guide to pharmacopoeias, aiding in the design of validation studies that meet regulatory expectations. |
Linking Risk to Statistical Confidence
The sample size for a verification study is fundamentally a reflection of the risk profile of the product and test. A statistically sound approach links the Risk Priority Number (RPN) to required Confidence and Reliability levels, which in turn dictate the sample size [10].
- Risk Priority Number (RPN): A calculated value based on the assigned ratings for Severity, Occurrence, and Detection [10].
- Confidence: How certain you are that the test results represent the true performance of the method (e.g., 95% confidence) [10].
- Reliability: The proportion of units that will successfully meet the pass/fail criteria (e.g., 95% reliability) [10].
Higher risk, often driven by high Severity (e.g., a sterility test failure) or low Detection, necessitates higher confidence and reliability, which increases the required sample size.
Statistical Methodology for Sample Size Determination
For microbiological tests that generate attribute or qualitative data (e.g., growth/no growth, positive/negative), the most widely accepted approach for sample size justification is the Non-parametric Binomial Reliability Demonstration Test [10].
The Binomial Reliability Model
This model is used to demonstrate, with a specified statistical confidence, that a certain proportion of units (reliability) will meet quality standards. A common and stringent application of this model requires zero (0) test failures. The minimum sample size n is determined by solving the following equation for the desired Confidence (C) and Reliability (R):
For example, to demonstrate 95% reliability with 95% confidence and zero allowable failures, the calculation is:
0.95 = 1 - 0.05ⁿ
Solving for n gives a sample size of approximately 59 [10].
Sample Size Reference Table
The following table, based on the binomial model with zero failures, provides minimum sample sizes for common Confidence/Reliability combinations.
Table 2: Minimum Sample Size for Various Confidence/Reliability Levels (Zero Failures Allowed)
| Confidence Level | Reliability Level | Minimum Sample Size |
|---|---|---|
| 95% | 95% | 59 |
| 95% | 90% | 29 |
| 90% | 95% | 45 |
| 90% | 90% | 22 |
| 99% | 99% | 459 |
Adapted from non-parametric binomial reliability data [10].
Experimental Protocol for Sample Size Justification
This protocol provides a step-by-step methodology for establishing and documenting a sample size for a microbiological method verification study.
Workflow for Sample Size Determination
The following diagram illustrates the logical workflow from risk assessment to final documentation.
Step-by-Step Procedural Details
- Define the Method and Scope: Clearly state the method being verified (e.g., qualitative test for Salmonella, quantitative enumeration). Define the categories in the food chain or product types that fall under the laboratory's scope of application [9].
- Perform a Risk Assessment: Assemble a cross-functional team to assign numerical ratings (e.g., 1-10) for:
- Severity: The potential harm to a patient from an incorrect test result.
- Occurrence: The likelihood of a method failure or error occurring.
- Detection: The probability that the laboratory's quality control system will detect a failure before it impacts a patient.
Calculate the RPN as:
RPN = Severity × Occurrence × Detection[10].
- Map RPN to Confidence/Reliability: Based on the RPN level (Low, Medium, High), establish the required statistical confidence and reliability. A higher RPN should correlate with higher confidence/reliability targets (e.g., 95/95 for a medium-risk product, as shown in the search results) [10].
- Determine the Sample Size: Using a pre-established table based on the non-parametric binomial model (like Table 2 above), select the minimum sample size that corresponds to your chosen confidence and reliability levels with zero allowable failures [10].
- Document the Rationale: The sample size justification must be explicitly recorded in the study protocol or a supporting document. This documentation should be a standalone, clear narrative understandable by an auditor without additional explanation.
The Scientist's Toolkit: Research Reagent Solutions
The following reagents and materials are essential for executing a typical microbiological verification study.
Table 3: Essential Research Reagents and Materials for Method Verification
| Item | Function / Purpose |
|---|---|
| Reference Strains | Well-characterized microorganisms from a recognized culture collection (e.g., ATCC). Used to challenge the method and demonstrate specificity and accuracy. |
| Selective and Non-Selective Media | Nutrient media, both general and selective, used for the growth, isolation, and identification of target microorganisms. Performance must be verified. |
| Neutralizing Agents | Chemical agents (e.g., diluents, inactivators) used to eliminate the antimicrobial effect of a product, ensuring accurate microbial recovery [46]. |
| Positive and Negative Controls | Samples with known content (positive contains target microbe, negative is sterile) used to validate that the test system is functioning correctly in each run. |
Data Presentation and Documentation for Audits
Clear and synthetic presentation of data is crucial for audit readiness [68] [69]. Every table and graph should be self-explanatory [68].
Sample Size Justification Table
The core of the documentation is a clear summary of the decision-making process.
Table 4: Example Documentation of Sample Size Justification
| Justification Factor | Description / Value | Reference / Rationale |
|---|---|---|
| Method Type | Qualitative Sterility Test | USP <71> / Ph. Eur. 2.6.1 |
| Risk Priority Number (RPN) | 320 (Medium Risk) | Severity=10, Occurrence=4, Detection=8 |
| Target Confidence Level | 95% | Based on RPN and internal quality policy |
| Target Reliability Level | 95% | Based on RPN and patient risk |
| Statistical Model | Non-parametric Binomial, 0 failures | Industry standard for attribute data [10] |
| Minimum Sample Size | 59 | Derived from binomial table for 95/95 with 0 failures |
Documentation Workflow and Final Report Structure
The final audit package should tell a coherent story from planning to execution.
The final report must synthesize all elements:
- Conclusion: A definitive statement on whether the method verification was successful.
- Data Summary: Tables presenting the results for all required validation parameters (e.g., specificity, accuracy/LOD) [46] [70].
- Deviation Log: Documentation and impact assessment of any deviations from the approved protocol.
- Approvals: Signed approval by the study director and quality assurance unit.
Conclusion
A scientifically sound sample size is not merely a statistical formality but a critical component of a reliable and compliant microbiological method verification. By integrating foundational statistical principles with the specific framework of standards like ISO 16140, researchers can generate defensible data that instills confidence in their methods. As rapid microbiological methods and complex biologics continue to evolve, future directions will demand more adaptive and sophisticated models for sample size estimation, further underscoring its pivotal role in advancing the quality and safety of pharmaceutical and food products.
References
- 1. Method Validation vs Method Verification: Which is Better ... [https://www.labmanager.com/method-validation-vs-method-verification-which-is-better-for-use-in-laboratories-33982]
- 2. Validating Rapid Microbiological Methods [http://rapidmicromethods.com/files/validation.php]
- 3. Planning a Method Verification Study in Clinical ... [https://asm.org/articles/2022/january/planning-a-method-verification-study-in-clinical-m]
- 4. Validation vs. Verification: What's the Difference? [https://www.idexxcurrents.com/en/latest/validation-vs-verification-what-s-the-difference/]
- 5. Food Safety Testing: Understanding Microbiological ... [https://www.eurofinsus.com/food-testing/resources/food-safety-testing-understanding-microbiological-method-validation-verification-and-fitness-for-purpose/]
- 6. Method Validation Vs. Verification - A Simple Breakdown [https://cptclabs.com/method-validation-vs-verification/]
- 7. Sample size, power and effect size revisited: simplified and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7745163/]
- 8. Sample size, power and effect size revisited: simplified ... [https://www.biochemia-medica.com/en/journal/31/1/10.11613/BM.2021.010502/fullArticle]
- 9. Method validation and method verification - Introduction - ISO [https://committee.iso.org/sites/tc34sc9/home/essential-information/content-left-area/validation-of-methods/method-validation-and-method-ver.html]
- 10. How to determine a valid sample size for testing medical ... [https://www.packagingdigest.com/medical-packaging/how-to-determine-a-valid-sample-size-for-testing-your-medical-device-package]
- 11. FAQ: <72> Respiration-Based Microbiological Methods for ... [https://www.uspnf.com/notices/gc-72-73-faq]
- 12. Challenges of Microbiological Sampling Plans [https://www.foodsafety-experts.com/challenges-of-microbiological-sampling-plans/]
- 13. Microbial testing in food safety: effect of specificity and ... [https://www.sciencedirect.com/science/article/abs/pii/S2214799316300790]
- 14. Criteria for Validation of Methods in Microbial Forensics [https://pmc.ncbi.nlm.nih.gov/articles/PMC2547046/]
- 15. What Is Analytical Method Development And Validation? [https://promptpraxislabs.com/what-is-analytical-method-development-and-validation/]
- 16. ISO 16140-3:2021 Method Verification Roundtable [https://www.neogen.com/en/neocenter/resources/iso-16140-32021-method-verification-roundtable-perspectives-from-the-industry/]
- 17. Validation of Microbiological Tests [https://www.biopharminternational.com/view/validation-microbiological-tests]
- 18. AOAC & MicroVal Method Validation Training [https://microval.org/2025/09/02/aoac-microval-method-validation-training-microbial-method-validation-detailed-insights/]
- 19. What Does Effect Size Tell You? [https://www.simplypsychology.org/effect-size.html]
- 20. A Guide to Choosing the Effect Size for Sample ... [https://www.statsols.com/guides/choosing-the-effect-size-for-sample-size-calculations]
- 21. Determination of Effect Sizes for Power Analysis ... [https://www.mdpi.com/2073-4425/14/6/1239]
- 22. Determination of Effect Sizes for Power Analysis for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10297957/]
- 23. Sample size determination: A practical guide for health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10000262/]
- 24. The Power of Microbiome Studies: Some Considerations ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2021.796025/full]
- 25. How To Establish Sample Sizes For Process Validation ... [https://www.bioprocessonline.com/doc/how-to-establish-sample-sizes-for-process-validation-using-statistical-tolerance-intervals-0001]
- 26. A bioassay method validation framework for laboratory and ... [https://malariajournal.biomedcentral.com/articles/10.1186/s12936-023-04717-w]
- 27. Quantitative and Qualitative Microbiological Testing [https://www.eurofinsus.com/food-testing/resources/small-world-it-is-quality-and-quantity-that-matter/]
- 28. AOAC validation of qualitative and quantitative methods for ... [https://www.sciencedirect.com/science/article/abs/pii/S0168160598001433]
- 29. 10 Critical Validation Parameters For Microbiological ... [https://www.outsourcedpharma.com/doc/critical-validation-parameters-for-microbiological-experiments-0001]
- 30. How to Calculate Sample Size for Different Study Designs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3775042/]
- 31. How to verify and validate a clinical microbiology test ... [https://www.sciencedirect.com/science/article/pii/S1198743X24003094]
- 32. QuickCalcs [https://www.graphpad.com/quickcalcs/]
- 33. Quick Statistics Calculators [https://www.socscistatistics.com/tests/]
- 34. The Bayesian microbial subtyping attribution model [https://inria.hal.science/pasteur-01112825/]
- 35. BIRDMAn: A Bayesian differential abundance framework ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9915500/]
- 36. A Model To Estimate the Optimal Sample Size ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC201250/]
- 37. A Comprehensive Methodology for Microbial Strain Typing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11207048/]
- 38. Sample size calculation in biomedical, clinical and ... [https://link.springer.com/article/10.1007/s43994-024-00153-x]
- 39. A Guide to Improving Sample Size Using Bayesian Thinking [https://www.statsols.com/guides/improving-sample-size-using-bayesian-thinking]
- 40. Method Detection Limit - Frequent Questions [https://www.epa.gov/cwa-methods/method-detection-limit-frequent-questions]
- 41. Validation of analytical methods in compliance with good ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3765465/]
- 42. Guidelines for Designing and Evaluating Feasibility Pilot ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8849521/]
- 43. Statistics for Method Verification of Qualitative Assays in ... [https://www.sciencedirect.com/science/article/abs/pii/S0196439917300259]
- 44. power and sample size calculation for microbiome studies [https://www.sciencedirect.com/science/article/pii/S1933021922017366]
- 45. 11 Summarising quantitative data | Scientific Research and ... [https://bookdown.org/pkaldunn/SRM-Textbook/SummariseQuantData.html]
- 46. Validation of microbiological methods [https://mpl.loesungsfabrik.de/en/english-blog/method-validation/validation-of-microbiological-methods]
- 47. Getting Rigor Right: A Framework for Methodological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10727457/]
- 48. Basic concepts for sample size calculation: Critical step ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4916819/]
- 49. Sample size calculation in clinical trial using R [https://www.e-jmis.org/journal/view.html?pn=&uid=679&vmd=Full]
- 50. The Multiphase Optimization Strategy (MOST) and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2062525/]
- 51. Using the Multiphase Optimization Strategy (MOST ... - Trials [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-019-3853-y]
- 52. Optimal allocation to treatments in a sequential multiple ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8649474/]
- 53. POWER ANALYSIS FOR COMPLEX MEDIATIONAL DESIGNS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3737006/]
- 54. Full Factorial Design: Comprehensive Guide for Optimal ... [https://www.6sigma.us/six-sigma-in-focus/full-factorial-design/]
- 55. Implementing optimal allocation in clinical trials with ... [https://www.sciencedirect.com/science/article/abs/pii/S0378375816301069]
- 56. USP–NF PF 51(5) Draft: Updates In Microbiology ... [https://gmpinsiders.com/uspnf-pf-515-draft/]
- 57. Rapid Microbiological Methods for Pharmaceutical ... [https://www.rapidmicrobiology.com/test-method/rapid-microbiological-methods-for-pharmaceutical-laboratories]
- 58. Challenges of growth-based microbiological methods in ... [https://link.springer.com/article/10.1007/s44395-025-00020-6]
- 59. Points to Consider Regarding Second Analyst Verification [https://www.americanpharmaceuticalreview.com/Featured-Articles/562304-Microbiological-Data-Integrity-Points-to-Consider-Regarding-Second-Analyst-Verification/]
- 60. Evaluating Microbiological Method Equivalence [https://www.foodprotection.org/publications/food-protection-trends/archive/2023-05-evaluating-microbiological-method-equivalence-a-decision-guide/]
- 61. Microbiological methods - assuring the alternatives [https://www.newfoodmagazine.com/article/97500/microbiological-methods-assuring-the-alternatives/]
- 62. for Bioequivalence Tests... - Biostatistics.ca Sample Size Calculation [https://www.biostatistics.ca/sample-size-calculation-for-bioequivalence-tests-a-powertost-tutorial-with-downloadable-r-code/]
- 63. for the development of biosimilar products Sample size calculations [https://pubmed.ncbi.nlm.nih.gov/25032735/]
- 64. Sterility Testing Guide: Direct Inoculation vs. Membrane ... [https://contractlaboratory.com/sterility-testing/]
- 65. Safeguarding Quality: The Role of Commercial Sterility in ... [https://www.beerandbrewing.com/safeguarding-quality-the-role-of-commercial-sterility-in-modern-beverage-manufact]
- 66. Validation protocol for commercial sterility testing methods [https://www.sciencedirect.com/science/article/pii/S0956713519301288]
- 67. All you need to know about equipment validation for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12421869/]
- 68. Presenting data in tables and charts - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4008059/]
- 69. Scientific Data Presentation: a Picture Is Worth a Thousand ... [https://www.aje.com/arc/scientific-data-presentation-picture-worth-thousand-words]
- 70. Presenting the Results of Quantitative Analysis [https://pressbooks.ric.edu/socialdataanalysis/chapter/writing-about-quantitative-data/]