A Comprehensive Guide to Precision Verification for Antimicrobial Susceptibility Testing
This article provides a systematic framework for the precision verification of Antimicrobial Susceptibility Testing (AST) methods, a critical quality process mandated by standards like ISO 15189 and CLSI M52.
A Comprehensive Guide to Precision Verification for Antimicrobial Susceptibility Testing
Abstract
This article provides a systematic framework for the precision verification of Antimicrobial Susceptibility Testing (AST) methods, a critical quality process mandated by standards like ISO 15189 and CLSI M52. Aimed at researchers and development professionals, it covers foundational principles of accuracy and precision, detailed methodological protocols for comprehensive and limited verification studies, strategies for troubleshooting common challenges, and advanced validation techniques for novel technologies and regulatory compliance. By synthesizing current guidelines and emerging trends, this guide supports the implementation of robust, reliable AST systems essential for combating antimicrobial resistance and ensuring effective patient treatment.
The Principles and Imperatives of AST Verification
In the field of clinical microbiology, particularly in antimicrobial susceptibility testing (AST), the terms "verification" and "validation" represent distinct quality assurance processes mandated by international standards. Adherence to these processes is critical for ensuring reliable patient results and meeting accreditation requirements. Within the framework of precision verification for AST methods research, a clear understanding of these concepts is fundamental. The Clinical and Laboratory Standards Institute (CLSI) and the International Organization for Standardization (ISO) 15189 standard provide specific, though complementary, guidance on these requirements [1] [2] [3].
Verification is the process of collecting objective evidence to confirm that a previously validated testing system performs according to the manufacturer's specifications within the user's laboratory environment [1]. It is a laboratory's responsibility when introducing a new, commercially approved method.
Validation, in contrast, is a more extensive process of establishing performance characteristics for a new method before it is put into routine use. According to CLSI, validation involves collecting a wide set of performance data, often generated by multiple operators and study sites, which can be used to seek regulatory clearance (e.g., from the FDA) [1]. This work is typically performed by the method's manufacturer.
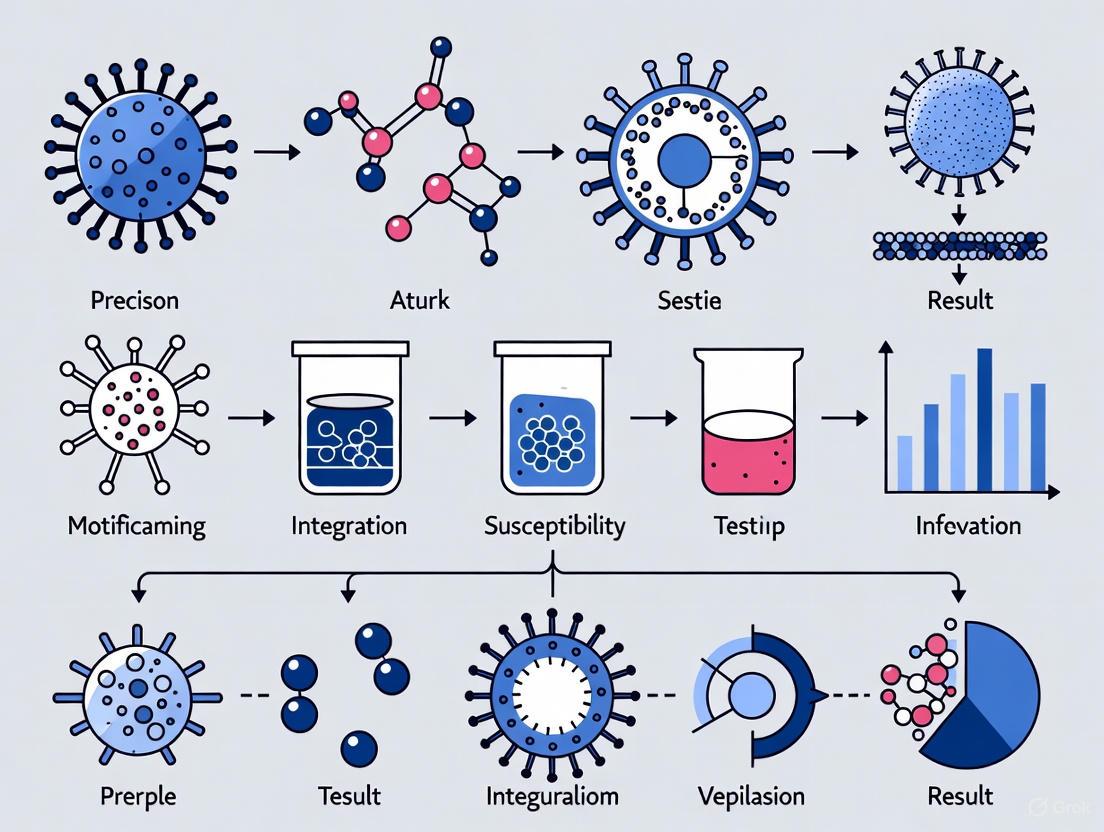
The following diagram illustrates the logical relationship and workflow distinction between these two processes.
Regulatory and Standard Requirements
ISO 15189 Requirements
The ISO 15189 standard, "Medical laboratories — Requirements for quality and competence," defines the general framework for quality management in medical laboratories. The 2022 version places significant emphasis on the verification and validation of examination procedures [2] [3]. Key requirements are anchored in Clause 7, "Process Requirements," which mandates that laboratories must verify or validate all examination procedures for their intended use [3]. This includes defined procedures for sample handling, result reporting, and data traceability, all underpinned by risk-based quality assurance. The standard requires that laboratories use only methods that have been validated for their intended use and must subsequently verify their ability to reproduce the manufacturer's performance claims before implementation [2] [3].
CLSI Guidelines
CLSI provides granular, practical guidelines for executing verification studies specifically in clinical microbiology. While ISO 15189 sets the overarching quality management system requirements, CLSI documents like M52, "Verification of Commercial Microbial Identification and Antimicrobial Susceptibility Testing Systems," offer detailed protocols [1]. These guidelines are considered the gold standard for designing and conducting AST verification studies, providing specific acceptance criteria for accuracy and precision, as well as recommendations for the number of isolates to test [4] [1].
Table: Summary of Standard Requirements
| Aspect | ISO 15189 | CLSI Guidelines |
|---|---|---|
| Primary Focus | Quality Management System (QMS) for the entire laboratory [3] | Technical protocols for specific procedures (e.g., AST) [4] [1] |
| Core Mandate | Labs must verify/validate all examination procedures for intended use [3] | Provides the "how-to" for verifying commercial AST systems [1] |
| Key Documents | ISO 15189:2022 Standard (Clauses 4-8) [3] | CLSI M52, M100, among others [4] [1] |
| Relationship | Defines the "what" - the requirement that must be met for accreditation [3] | Defines the "how" - one accepted method to fulfill the ISO requirement [1] |
Experimental Protocols for AST Verification
For researchers conducting precision verification of AST methods, the following protocols, synthesized from CLSI guidelines, provide a structured experimental roadmap.
Comprehensive Verification Protocol (for a new AST system)
This protocol applies when a laboratory introduces a new AST platform or makes a fundamental change in testing methodology [1].
1. Objective: To verify the accuracy and precision of a new commercial AST system against a reference method before its implementation for routine clinical testing.
2. Experimental Design:
- Sample Size: A minimum of 30 bacterial isolates for accuracy testing [1].
- Strain Selection: Select clinical strains, including those with relevant resistance mechanisms, that are representative of those encountered in the laboratory's patient population [1]. Proficiency testing isolates or strains from repositories like the CDC-FDA Antimicrobial Resistance Isolate Bank are highly recommended [1] [5].
- Reference Method: The test method (e.g., a novel rapid phenotypic system) must be compared against one of the following:
3. Data Collection and Analysis:
- Accuracy (Categorical Agreement, CA): Determine the percentage of isolates where the susceptibility category (S, I, R) is consistent between the new method and the reference method [1] [5].
- Accuracy (Essential Agreement, EA): For minimum inhibitory concentration (MIC) methods, determine the percentage of results where the new MIC is within ±1 doubling dilution of the reference MIC [1].
- Precision (Reproducibility): Test a subset of 5 isolates (can be quality control strains or clinical isolates) in triplicate to assess the reproducibility of categorical and MIC results [1].
4. Acceptance Criteria:
- Categorical Agreement: ≥ 90% of test results [1].
- Error Rates: < 3% for combined very major errors (false susceptible) and major errors (false resistant) [1].
- Precision: ≥ 95% agreement of test results upon repeat testing [1].
Limited Verification Protocol (for a new antimicrobial agent)
This streamlined protocol is used when adding a new antimicrobial agent to an existing, verified AST system [1].
1. Objective: To verify the performance of a single new antimicrobial agent on an already operational AST platform.
2. Experimental Design:
- Sample Size: A minimum of 10 bacterial isolates [1].
- Strain Selection: Isolates should represent the spectrum of susceptibility (susceptible, intermediate, resistant) to the new agent.
- Reference Method: As described in the comprehensive protocol.
3. Data Collection and Analysis:
- Identical to the comprehensive protocol (CA, EA).
4. Acceptance Criteria:
- Identical to the comprehensive protocol.
Table: Verification Study Design Summary
| Parameter | Comprehensive Verification (New System) | Limited Verification (New Agent) |
|---|---|---|
| Scenario | New AST system or change in testing method [1] | New antimicrobial agent on an existing system [1] |
| Accuracy Testing | ≥ 30 isolates [1] | ≥ 10 isolates [1] |
| Precision Testing | 5 isolates tested in triplicate [1] | Test QC strains 3x for 5 days or 1x/day for 20 days [1] |
| Key Acceptance Criteria | CA ≥ 90%; VME/ME < 3%; Precision ≥ 95% [1] | CA ≥ 90%; VME/ME < 3% [1] |
| Example from Literature | Evaluation of Selux DX system (n=332 clinical + 97 reference isolates) [5] | Not explicitly detailed in results, but follows M52 framework [1] |
The Scientist's Toolkit: Research Reagent Solutions
Successful execution of AST verification and validation studies requires carefully selected materials. The following table details key research reagents and their critical functions.
Table: Essential Research Reagents for AST Verification & Validation
| Reagent / Material | Function & Importance in Research |
|---|---|
| Clinical & Challenge Isolates | Clinical isolates ensure real-world relevance, while challenge isolates with well-defined resistance mechanisms (e.g., ESBL, carbapenemase-producers) are critical for testing the limits of a new method's detection capability [1] [5]. |
| Reference Strain Panels | Certified strains from collections like the CDC-FDA AR Bank or ATCC provide a gold standard with known phenotypes and genotypes, essential for establishing accuracy and ensuring result comparability across studies [1] [5]. |
| QC Strains | Quality Control strains are used repeatedly in precision experiments to monitor the day-to-day reproducibility and stability of the AST system under evaluation [1]. |
| Reference Method Materials | Supplies for CLSI reference methods (e.g., broth microdilution panels per M07, Mueller-Hinton agar) are necessary to generate the comparator data against which the new method is judged [4] [1]. |
The following workflow diagram maps the application of these key reagents into the overall experimental process for AST verification.
Analysis of Discrepancies and Data Interpretation
A critical phase in AST verification is the analysis of discrepancies between the new method and the reference. Errors are categorized to assess clinical risk [5]:
- Very Major Error (VME): The new method calls an isolate "Susceptible" when the reference method calls it "Resistant." This is the most critical error type as it could lead to failed therapy.
- Major Error (ME): The new method calls an isolate "Resistant" when the reference method calls it "Susceptible." This could lead to the unnecessary use of broader-spectrum antibiotics.
- Minor Error (mE): The new method reports an "Intermediate" result while the reference is either "Susceptible" or "Resistant," or vice-versa.
Recent evaluations of novel systems, such as the Selux DX platform, demonstrate the application of these criteria. In one study, across 5124 drug-bug combinations, investigators reported 55 VMEs (1.1%), 42 MEs (0.8%), and 203 mEs (4.0%), with most discrepancies occurring in specific drug-class combinations [5]. This level of detailed discrepancy analysis is essential for a thorough understanding of a method's performance.
Antimicrobial susceptibility testing (AST) is a critical component of modern clinical microbiology, providing essential data to guide effective antibiotic therapy and combat the global threat of antimicrobial resistance (AMR) [6]. The reliability of AST results hinges on rigorously verifying the core performance specifications of the testing method, primarily accuracy, precision, and essential agreement [1] [7]. Within a research framework focused on precision verification for AST methods, understanding and quantifying these parameters is fundamental to developing and implementing reliable assays. These specifications ensure that tests perform consistently with established standards, providing researchers and clinicians with confidence in the data used for critical decisions regarding patient treatment and antimicrobial stewardship [8]. This document outlines the definitions, experimental protocols, and acceptance criteria for verifying these core specifications in AST systems.
Defining the Core Performance Specifications
In the context of AST verification, the terms accuracy, precision, and essential agreement have specific and distinct meanings. A clear understanding of these concepts is the foundation for a robust verification study.
Accuracy refers to the closeness of agreement between a test result and an accepted reference value [9]. In AST, this is typically assessed through categorical agreement (CA), which compares the interpretive category (Susceptible (S), Intermediate (I), or Resistant (R)) of the new method against the reference method [1].
Precision describes the closeness of agreement between independent test results obtained under stipulated conditions [10] [9]. It is a measure of the method's repeatability and reproducibility, evaluating the consistency of results when the same sample is tested multiple times, whether by the same operator, across different days, or using different instruments [8].
Essential Agreement (EA) is a more granular measure of accuracy for quantitative AST methods, such as those reporting a Minimum Inhibitory Concentration (MIC). It is defined as the agreement between the MIC value obtained from the test method and the reference method within a specified doubling dilution range, usually ±1 dilution [1].
The diagram below illustrates the logical relationships between the core performance specifications, their components, and the final determination of method reliability.
Performance Criteria and Data Presentation
Regulatory bodies and standards organizations provide clear acceptance criteria for AST verification studies. Adherence to these benchmarks is mandatory for concluding that a test method is performing adequately.
Table 1: Acceptance Criteria for AST Verification Studies
| Performance Characteristic | Definition | Acceptance Limit |
|---|---|---|
| Categorical Agreement (CA) | Percentage of results where S, I, R interpretations are consistent between test and reference methods [1]. | ≥ 90% of test results [1]. |
| Essential Agreement (EA) | Percentage of MIC results within ±1 doubling dilution of the reference MIC [1]. | ≥ 90% of test results [1]. |
| Precision (Reproducibility) | Percentage of S, I, R interpretations or MIC values (within ±1 dilution) that are reproducible [1]. | ≥ 95% of test results [1]. |
| Error Rates | Very Major Error (false susceptible) or Major Error (false resistant) [1]. | < 3% total discrepancies [1]. |
The distinction between accuracy and precision is critical for troubleshooting. A method can be precise but inaccurate, or accurate but imprecise; the goal is to achieve both simultaneously.
Table 2: Interpreting Combinations of Accuracy and Precision
| Scenario | Accuracy | Precision | Interpretation |
|---|---|---|---|
| 1 | High | High | Ideal scenario. The method is reliable and producing correct, consistent results. |
| 2 | High | Low | Measurements center on the true value but are scattered. The average may be correct, but individual results are unreliable. |
| 3 | Low | High | Measurements are consistent but systematically deviate from the true value. Indicates a calibration or systematic bias issue. |
| 4 | Low | Low | The method is unreliable. Results are neither correct nor consistent. |
Experimental Protocols for Verification
A well-designed verification study is crucial for generating meaningful data. The following protocols are adapted from established guidelines, including CLSI M52 [1] [7] [8].
Protocol for Assessing Accuracy and Essential Agreement
This protocol is designed to verify that a new AST system correctly categorizes bacterial isolates and provides accurate MIC measurements compared to a reference method.
1. Experimental Design:
- A minimum of 30 bacterial isolates is required for a comprehensive verification of a new system or method [1]. For verification of a new antimicrobial agent added to an existing system, a minimum of 10 isolates may be sufficient [1].
- Isolate selection must be deliberate, covering a range of clinically relevant species and including strains with relevant and defined resistance mechanisms [1] [11]. The selection should be representative of the organisms for which the antimicrobial agents are clinically indicated [1].
2. Reference Method:
- The reference method can be a clinical laboratory standard such as broth microdilution or agar dilution [1]. Alternatively, testing can be performed against a previously verified and FDA-cleared commercial AST system, or by using well-characterized isolates from repositories like the CDC-FDA Antimicrobial Resistance Isolate Bank [1].
3. Procedure:
- Test each of the selected 30 isolates in the new AST system according to the manufacturer's instructions.
- In parallel, test each isolate using the chosen reference method.
- Ensure that all testing is performed on fresh, subcultured isolates to ensure viability and purity.
4. Data Analysis:
- For each organism-drug combination, compare the interpretive category (S, I, R) from the test method to the reference method. Calculate Categorical Agreement (CA) as: (Number of category agreements / Total number of comparisons) × 100.
- For quantitative methods, compare the MIC value from the test method to the reference MIC. Calculate Essential Agreement (EA) as: (Number of MICs within ±1 doubling dilution / Total number of comparisons) × 100.
- Compare the calculated CA and EA percentages against the acceptance criteria of ≥90% [1].
Protocol for Assessing Precision (Reproducibility)
This protocol evaluates the consistency of AST results when the testing conditions are varied.
1. Experimental Design:
- Select a minimum of 5 bacterial isolates. These can be clinical isolates or quality control (QC) strains [1].
- The study should incorporate multiple variables, such as different operators, different instruments of the same model, and testing performed over multiple days [8].
2. Procedure:
- Test each of the 5 isolates in triplicate (three separate test runs) [1].
- This testing should be performed by at least two different analysts, each using their own reagents and equipment where possible [10].
- The entire process should be repeated over 3-5 days to capture day-to-day variation [1].
3. Data Analysis:
- For qualitative results (S/I/R), calculate the percentage of interpretations that are consistent across all replicates and conditions.
- For quantitative results (MIC), calculate the percentage of MIC results that are reproducible within ±1 doubling dilution.
- The precision is considered acceptable if ≥95% of the results are reproducible [1].
The following workflow provides a visual overview of the complete verification process, from planning to implementation.
The Scientist's Toolkit: Research Reagent Solutions
Successful execution of an AST verification study requires access to well-characterized biological and control materials. The following table details essential resources for this research.
Table 3: Key Research Reagents and Resources for AST Verification
| Resource | Function and Application in AST Verification |
|---|---|
| Clinical & QC Isolates | Well-characterized bacterial strains used as test samples. Clinical isolates provide real-world relevance, while QC strains ensure day-to-day procedural control and are selected for endpoint clarity and reproducibility [1] [8]. |
| CDC-FDA AR Isolate Bank | A repository of curated, phenotypically and genotypically defined antimicrobial-resistant isolates. Provides a standardized, reliable source of challenging organisms with specific resistance mechanisms for verification studies [1]. |
| Reference AST Methods | Established, gold-standard methods like broth microdilution. Serves as the comparator against which the performance of the new commercial or investigational AST system is measured to determine accuracy [1]. |
| CLSI Guidelines (e.g., M52) | Documents providing standardized protocols and acceptance criteria for verification studies. Ensure that the study design, execution, and interpretation of results are consistent with international regulatory and scientific standards [1] [7]. |
The rigorous verification of accuracy, precision, and essential agreement is a non-negotiable step in the implementation of any antimicrobial susceptibility testing method. By adhering to structured experimental protocols and predefined acceptance criteria, researchers and laboratory scientists can ensure the generation of reliable, actionable data. In the broader context of AMR, robust AST is a cornerstone of effective antimicrobial stewardship, guiding appropriate therapy and helping to mitigate one of the most pressing global health threats of our time. The frameworks and protocols detailed in this document provide a pathway to achieving this essential reliability.
For clinical laboratories, particularly those engaged in antimicrobial susceptibility testing (AST), navigating the interlocking regulatory requirements of the Clinical Laboratory Improvement Amendments (CLIA), the U.S. Food and Drug Administration (FDA), and the International Organization for Standardization (ISO) 15189 standard is paramount for ensuring patient safety, test accuracy, and legal compliance. These frameworks collectively govern laboratory operations, from test development and verification to daily quality management. CLIA establishes the mandatory federal regulations for all U.S. clinical laboratories testing human specimens, enforcing quality standards across personnel qualifications, proficiency testing, and quality control procedures [12]. The FDA regulates medical devices, including in vitro diagnostic (IVD) tests, and, with its evolving stance on laboratory-developed tests (LDTs), now imposes additional requirements on labs that manufacture these tests [12]. In contrast, ISO 15189 is a voluntary international standard that specifies requirements for quality and competence, often serving as a mark of excellence and a framework for a robust quality management system that extends beyond CLIA's baseline [12] [13].
A critical and evolving challenge in this landscape is the regulatory treatment of LDTs. Historically, the FDA exercised enforcement discretion, but with a newly finalized rule, it is phasing out this discretion, meaning laboratories that offer IVDs as LDTs are increasingly being considered "manufacturers" and must comply with FDA regulations to prove the safety and effectiveness of their tests [12]. It is a common misconception that FDA regulation replaces CLIA requirements; in reality, FDA regulations are in addition to, not instead of, existing CLIA obligations [12]. This layered regulatory environment creates a "perfect storm" for laboratories, demanding rigorous protocols for test verification and validation, especially for precision-focused research like AST method development [12].
Comparative Analysis of Regulatory Bodies
Scope, Focus, and Legal Status
The following table summarizes the core characteristics, roles, and legal standing of the three primary regulatory bodies governing clinical laboratories in the United States.
Table 1: Key Characteristics of CLIA, FDA, and ISO 15189
| Feature | CLIA | FDA | ISO 15189 |
|---|---|---|---|
| Full Name | Clinical Laboratory Improvement Amendments [12] | U.S. Food and Drug Administration [12] | International Organization for Standardization 15189 [12] |
| Nature & Legal Status | Mandatory federal regulations; legally binding [12] | U.S. federal regulatory agency; legally binding [12] | Voluntary international standard; not legally binding unless adopted by a country [12] |
| Primary Focus & Scope | Quality standards for laboratory operations: personnel, quality control, proficiency testing, specimen handling [12] | Regulation of medical devices (IVDs), including safety and effectiveness; categorization of test complexity [12] | Requirements for quality management systems and technical competence in medical laboratories [12] |
| Governing/Administering Body | Centers for Medicare & Medicaid Services (CMS) [12] | U.S. Food and Drug Administration [12] | International Organization for Standardization [12] |
| Applicability to U.S. Labs | All clinical laboratories testing human specimens [12] | Manufacturers of IVDs and, increasingly, laboratories offering LDTs [12] | Optional; demonstrates commitment to quality and may be required for international work [13] |
Areas of Overlap, Distinction, and Potential Conflict
The regulatory frameworks of CLIA, FDA, and ISO 15189 are not isolated; they exhibit significant overlap, particularly in their shared emphasis on quality systems. However, their distinct focuses can lead to duplicative or, in some cases, potentially conflicting demands.
Overlap and Duplication: A key area of overlap exists between CLIA and ISO 15189, as both address laboratory process quality. However, ISO 15189 often incorporates a broader quality management system that includes aspects like continuous improvement and customer feedback, which are less explicitly detailed in CLIA [12] [13]. For laboratories developing LDTs, the FDA's quality system requirements (aligned with ISO 13485) and CLIA's quality standards may be duplicative, requiring labs to satisfy two sets of quality mandates using different terminologies [12].
Potential Conflicts and Challenges: A primary challenge arises from the FDA's new LDT rule. Experts note that laboratories may face redundant reporting requirements, such as reporting an adverse event both as the "manufacturer" (per FDA rules) and the "user" (per existing requirements) of the same LDT [12]. Furthermore, the FDA may mandate more specific validation protocols than CLIA, for instance, requiring adherence to specific Clinical & Laboratory Standards Institute (CLSI) guidelines it recognizes, whereas CLIA provides general recommendations [12]. For AST specifically, a significant challenge has been the lag between updated breakpoints from standards organizations like CLSI and their incorporation into the FDA-cleared labeling of commercial AST systems. Implementing non-FDA breakpoints is considered a test modification under CLIA, requiring a resource-intensive laboratory-led verification study [14].
Application to Antimicrobial Susceptibility Testing (AST) Verification
Regulatory Demands for AST Verification
CLIA regulations unequivocally require laboratories to verify the performance of any diagnostic test before its implementation for patient care [14]. The extent of this verification depends on whether the test is FDA-cleared or is a modified or laboratory-developed test. For an unmodified, FDA-cleared AST system, the CLIA requirement is to demonstrate that the test achieves performance specifications comparable to those established by the manufacturer [14]. However, if a laboratory modifies an FDA-cleared test—such as by implementing revised interpretive breakpoints not yet approved in the device's labeling—it must perform a more extensive verification to establish the performance specifications of the modified test [14]. ISO 15189 also underscores the need to verify examination procedures before introduction, ensuring they are suitable for clinical use [1].
Quantitative Verification Requirements for AST Systems
The verification of a new AST system requires rigorous assessment of accuracy and precision (reproducibility). The following table outlines the typical verification study design as recommended by guidelines such as CLSI M52 [1].
Table 2: AST Verification Study Design & Acceptance Criteria
| Criteria | Definition & Measurement | Acceptance Limit |
|---|---|---|
| Accuracy (Categorical Agreement) | Agreement in susceptibility category (S, I, R) between the new method and a reference method. | ≥ 90% categorical agreement with < 3% very major errors (false susceptible) or major errors (false resistant) [1]. |
| Accuracy (Essential Agreement) | Minimum Inhibitory Concentration (MIC) result from the new method is within ±1 doubling dilution (or ±2 for yeast) of the reference MIC [1]. | ≥ 90% essential agreement [1]. |
| Precision (Reproducibility) | Ability to reproduce identical categorical (S, I, R) or MIC (±1 doubling dilution) results on repeated testing of the same isolates [1]. | ≥ 95% agreement of test results [1]. |
Table 3: Scope of Verification Based on Type of Change
| Type of Change in Laboratory | Accuracy (Number of Isolates) | Precision (Testing Scheme) |
|---|---|---|
| Comprehensive Verification (e.g., new AST system or testing method) | Minimum of 30 isolates [1] | Test 5 isolates, each on 3 separate runs [1] |
| Limited Verification (e.g., new antimicrobial agent on an existing system) | Minimum of 10 isolates [1] | Test quality control (QC) strains 3 times for 5 days or once daily for 20 days [1] |
Experimental Protocol for Comprehensive AST System Verification
This protocol provides a step-by-step methodology for verifying a new commercial AST system, as required by CLIA and aligned with ISO 15189 principles.
1. Pre-Verification Planning:
- Define Scope and Plan: Determine if the verification is comprehensive or limited. Document the plan, including the reference method, number and type of isolates, acceptance criteria, and antimicrobial agents to be verified. This plan must be approved by the Laboratory Director [14].
- Select Reference Method: The reference method can be an FDA-cleared and previously verified method, a CLSI reference broth microdilution or agar dilution method, or well-characterized isolates with known AST results from an external, verified source [1].
- Select Bacterial Isolates: For a comprehensive verification of 30 isolates, select fresh clinical strains that are representative of the patient population. The set should include strains with relevant resistance mechanisms to challenge the system's performance. Proficiency testing isolates or strains from resources like the CDC-FDA Antimicrobial Resistance Isolate Bank are excellent choices [1].
2. Inoculum Preparation and Standardization:
- Select 3-5 well-isolated colonies from an 18-24 hour culture plate [15].
- Prepare a bacterial suspension in saline or broth.
- Adjust the turbidity of the suspension to a 0.5 McFarland standard, which corresponds to approximately 1-2 x 10^8 CFU/mL [15]. For MIC methods, a subsequent 1:20 dilution is often required to achieve the final inoculum concentration of ~5 x 10^5 CFU/mL [15].
3. Inoculation and Incubation:
- For Disk Diffusion: Inoculate a Mueller-Hinton Agar (MHA) plate uniformly with the standardized suspension. Apply antimicrobial disks to the agar surface using sterile forceps, ensuring adequate spacing [15].
- For MIC Panels: Using the diluted inoculum, fill the wells of the commercial MIC panel according to the manufacturer's instructions, often using a pronged device [15].
- Incubate the inoculated plates or panels at 35±2°C for 16-20 hours (standard bacteria) in an ambient atmosphere. Adjust incubation time and atmosphere for fastidious organisms [15].
4. Reading and Interpreting Results:
- Disk Diffusion: Measure the diameter of each zone of inhibition (including the disk) to the nearest millimeter using a caliper [15].
- MIC Method: Read the MIC as the lowest concentration of antimicrobial that completely inhibits visible growth [15].
- Interpret the results (S, I, R) using the appropriate clinical breakpoints (e.g., from CLSI or EUCAST). The same breakpoints must be used for both the new and reference methods.
5. Data Analysis and Final Review:
- Compare the results from the new system to the reference method for each isolate and antimicrobial agent.
- Calculate the percentage categorical agreement and essential agreement. Classify and count any discrepancies (very major, major, minor).
- Compare the results against the pre-defined acceptance criteria. The Laboratory Director must review all data and formally approve the verification study before the test system is released for patient testing [14] [15].
AST Verification Workflow
The Scientist's Toolkit: Key Reagent Solutions for AST
Table 4: Essential Research Reagents for Antimicrobial Susceptibility Testing
| Reagent / Material | Function in AST Verification |
|---|---|
| Mueller-Hinton Agar (MHA) | The standardized, non-selective medium recommended by CLSI and EUCAST for disk diffusion and agar dilution AST. It provides reproducible diffusion of antimicrobial agents and supports the growth of non-fastidious organisms [15]. |
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | The standardized broth medium used for broth microdilution MIC testing. The cation adjustment (Ca²⁺, Mg²⁺) is critical for obtaining accurate and reproducible results with aminoglycosides and polymyxins [15]. |
| McFarland Standards | A set of reference suspensions (e.g., 0.5 McFarland) used to visually standardize the turbidity (and thus the approximate cell density) of bacterial inocula for AST, ensuring a consistent challenge to the antimicrobial agents [15]. |
| Quality Control (QC) Strains | Frozen or lyophilized reference bacterial strains with well-defined MIC and zone diameter ranges (e.g., S. aureus ATCC 29213, E. coli ATCC 25922). Used to monitor the day-to-day performance and precision of the AST system [1] [15]. |
| Characterized Clinical Isolates | Well-characterized bacterial isolates from clinical specimens or strain banks (e.g., CDC-FDA AR Bank). These are essential for verification studies to challenge the AST system with strains possessing known resistance mechanisms [1]. |
Successfully navigating the regulatory demands of CLIA, FDA, and ISO 15189 is not merely an exercise in compliance but a fundamental component of scientific rigor and patient safety in antimicrobial susceptibility testing. A proactive, integrated approach is essential. Laboratories must prioritize CLIA compliance as the mandatory foundation, then layer on FDA requirements for LDTs, and finally, consider ISO 15189 accreditation as a strategic tool for achieving operational excellence and international recognition [12] [13]. The recent updates to CLIA personnel qualifications and the FDA's LDT rule underscore that this landscape is dynamic, requiring continuous vigilance and education [16]. By embedding these interlocking requirements into a robust quality management system—centered on thorough test verification, rigorous quality control, and a culture of continuous improvement—research scientists and drug development professionals can ensure their AST methods are not only compliant but also yield the precise, reliable, and clinically actionable data necessary to combat the growing threat of antimicrobial resistance.
The Critical Role of Verification in Antimicrobial Stewardship and Patient Outcomes
In the global fight against antimicrobial resistance (AMR), Antimicrobial Stewardship Programs (ASPs) have emerged as critical interventions for optimizing antibiotic use and preserving the efficacy of existing agents [17]. The core objective of ASPs is to ensure that patients receive the most appropriate antimicrobial therapy, a decision that hinges on reliable diagnostic information. Antimicrobial Susceptibility Testing (AST) serves as the fundamental tool guiding these therapeutic decisions, making its accuracy and reliability paramount [18]. Verification of AST methods—the rigorous process of confirming that a test system performs as intended—is therefore not merely a quality control step but a vital contributor to patient safety and positive clinical outcomes. Without robust verification protocols, ASP interventions are built on uncertain foundations, potentially leading to inappropriate prescribing, worsened patient prognoses, and accelerated antimicrobial resistance [19]. This application note details the critical importance of verification within the context of precision AST and provides structured protocols for its implementation in a research setting.
The Imperative for Verified AST in Stewardship Outcomes
Verification ensures that AST results are accurate, reproducible, and clinically actionable. Inaccurate results can directly undermine ASP efforts. For instance, a false susceptible result may lead to the use of an ineffective antibiotic, while a false resistant result may preclude the use of a safe, narrow-spectrum agent [15]. The consequences are measurable: a 2025 study of a newly implemented ASP demonstrated that prospective audit and feedback of restricted antibiotics, guided by AST results, maintained a consistent rejection rate of 3.65% to 4.68% for inappropriate prescriptions, directly influencing prescribing behavior [20].
The global AMR crisis, associated with an estimated 4.95 million deaths annually, underscores the non-negotiable need for diagnostic precision [21]. ASPs have been shown to reduce antibiotic consumption by up to 91% and achieve cost savings of up to 82% in antibiotic expenditures, but their effectiveness is entirely dependent on the reliability of the underlying AST data [17]. Verification acts as the critical bridge between laboratory testing and effective stewardship, transforming raw data into trusted evidence for clinical decision-making.
Current AST Methods and Verification Benchmarks
Clinical laboratories and research institutions employ a range of AST methods, each with distinct verification requirements. The choice of method often depends on the balance between speed, resource availability, and the need for comprehensive phenotypic information.
Table 1: Overview of Common Antimicrobial Susceptibility Testing Methods
| Method Type | Principle | Typical Time-to-Result (after isolate) | Key Verification Parameters |
|---|---|---|---|
| Disk Diffusion [15] | Measurement of zone of inhibition around an antibiotic-impregnated disk. | 16-24 hours | Zone diameter reproducibility, correlation with quality control (QC) strain ranges. |
| Broth Microdilution [15] | Determination of Minimum Inhibitory Concentration (MIC) in liquid medium. | 16-24 hours | MIC reproducibility, essential and categorical agreement with reference methods. |
| Automated Systems [18] | Automated reading of microbial growth in the presence of antibiotics. | 6-24 hours | Agreement with CLSI/EUCAST reference methods, system reproducibility. |
| Rapid Phenotypic Tests [11] | Various novel methods to accelerate growth detection or viability assessment. | 0.5 - 8 hours | Categorical agreement, major error rates, and very major error rates against gold standard. |
| Genotypic Methods [22] | Detection of known resistance genes (e.g., mecA, blaKPC) via PCR or sequencing. | 1-6 hours | Analytical sensitivity and specificity for each genetic target. |
The gold standard for phenotypic AST remains broth microdilution, as defined by the Clinical and Laboratory Standards Institute (CLSI) and the European Committee on Antimicrobial Susceptibility Testing (EUCAST) [15] [18]. These bodies provide rigorously developed clinical breakpoints, which are specific MIC values or zone diameters that categorize organisms as "Susceptible," "Resistant," or "Intermediate" [15]. Verification of any new or alternative AST method must demonstrate high categorical agreement with these reference methods and established breakpoints.
Quantitative Impact of Verified Rapid AST on Stewardship
Rapid AST technologies can dramatically shorten the time to optimal therapy, a critical factor in severe infections like sepsis. However, their clinical utility must be validated through stringent verification. The following table synthesizes outcomes from recent studies implementing rapid or verified AST methods alongside ASPs.
Table 2: Impact of Verified and Rapid AST on Stewardship and Patient Outcomes
| Study / Technology Focus | Key Verification Metric | Impact on Stewardship and Clinical Outcomes |
|---|---|---|
| Modified RAST Protocol [23] | Categorical Agreement (CA) for key antibiotics: Gentamicin (98.2%), Meropenem (94.7%) vs. standard AST. | Reduced time-to-result by >24 hours, enabling earlier therapy adjustment. |
| New ASP Implementation [20] | N/A (Program outcome based on verified AST) | Restricted antibiotic rejection rate stable at ~4%; intervention acceptance for prolonged therapy rose to 82.5%. |
| Rapid Phenotypic AST Pipeline [11] | Technology Readiness Level (TRL) and Phase of Clinical Validation framework for >90 technologies. | Roadmap for validating next-gen tests for use in low-resource settings to curb empiric overuse. |
| Molecular PCR Panels [19] | >98% sensitivity for influenza vs. 36% for clinical diagnosis alone. | Guides precise treatment, reduces unnecessary antibiotic prescriptions for viral infections. |
A 2025 study on a modified Rapid AST (RAST) protocol highlights the profound impact of verified rapid testing. The protocol, which minimized resource requirements by delaying species identification, achieved high categorical agreement for several key antibiotics [23]. This allowed for reliable results directly from positive blood culture bottles, cutting the time-to-result by at least 24 hours and enabling stewardship teams to make informed interventions a full day earlier than with conventional methods [23].
Experimental Protocols for AST Method Verification
This section provides a detailed framework for verifying a commercial or novel AST method against a reference standard, such as broth microdilution, in a research setting.
Protocol: Verification of an Antimicrobial Susceptibility Test
1. Objective: To verify the performance (accuracy and precision) of a test AST method against a CLSI/EUCAST reference method for specific organism-antimicrobial combinations.
2. Materials and Reagents:
- Bacterial Strains: A challenge panel of 50-100 well-characterized clinical isolates, including target organisms (e.g., E. coli, K. pneumoniae, P. aeruginosa, S. aureus) and QC strains (e.g., E. coli ATCC 25922, S. aureus ATCC 29213) [15] [23].
- Antimicrobial Agents: A panel of antibiotics relevant to the target organisms, sourced as certified powder or commercial disks/panels.
- Culture Media: Mueller-Hinton Agar (MHA) and Mueller-Hinton Broth (MHB), quality-controlled for compliance with CLSI/EUCAST standards [15].
- Equipment: The test AST system (automated, manual, or rapid), incubator (35±2°C), and standard laboratory equipment for microbiology.
3. Experimental Workflow: The verification process follows a structured pathway from strain selection to final performance analysis, as outlined in the diagram below.
4. Procedure:
- Inoculum Preparation: For each test isolate, prepare a bacterial suspension equivalent to a 0.5 McFarland standard [15].
- Parallel Inoculation: Inoculate both the test system and the reference method (e.g., broth microdilution panel or MHA plate for disk diffusion) within 15 minutes of each other using the same standardized inoculum [15].
- Incubation: Incubate all test and reference panels/plates at 35±2°C for 16-24 hours, as required by the respective methods.
- Reading and Recording: Read the MIC for dilution-based methods or the zone diameter for disk diffusion. Record all results.
5. Data Analysis and Acceptance Criteria: Calculate the following performance metrics by comparing the test method results to the reference method results:
- Essential Agreement (EA): The percentage of isolates for which the test MIC is within one doubling dilution of the reference MIC. Target: ≥90% [11].
- Categorical Agreement (CA): The percentage of isolates assigned to the same susceptibility category (S/I/R) by both methods. Target: ≥90% [23].
- Error Rates:
- Major Error (ME): Test result is "Resistant" but reference result is "Susceptible." Target: ≤3%.
- Very Major Error (VME): Test result is "Susceptible" but reference result is "Resistant." Target: ≤3% [11].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for AST Verification Studies
| Reagent / Material | Function in Verification Protocol | Key Considerations |
|---|---|---|
| Quality Control Strains [15] | To ensure testing conditions, media, and reagents are performing within established limits. | Must include strains with defined MIC ranges for all antibiotics tested (e.g., E. coli ATCC 25922, P. aeruginosa ATCC 27853). |
| Standardized Culture Media [15] | Provides a consistent and defined growth environment for reproducible AST. | Mueller-Hinton Agar/Broth must be validated for pH, cation concentrations, and thickness (for agar). |
| CLSI/EUCAST Guidelines [15] [18] | The definitive source for reference methods, QC ranges, and clinical breakpoints. | Critical for designing a compliant verification study and interpreting results correctly. |
| Characterized Clinical Isolates | Serves as the challenge panel to evaluate test performance across a range of phenotypes. | Should include strains with common and rare resistance mechanisms to thoroughly challenge the test. |
| Reference Antimicrobials | The benchmark against which the test method is compared. | Use from certified sources to ensure accurate potency and performance. |
Advanced Considerations: Verification of Novel Technologies
The AST landscape is evolving with innovations in rapid phenotypic and genotypic technologies. Verifying these requires tailored approaches:
- Rapid Phenotypic AST: For technologies claiming results in hours, verification must account for shorter incubation times. The primary focus should be on categorical agreement and error rates compared to the standard method, with careful attention to the potential for increased minor and major errors due to altered growth dynamics [11].
- Genotypic AST (e.g., PCR/WGS): Verification here shifts from phenotype to genotype. The process must validate the analytical sensitivity and specificity of the assay for detecting specific resistance markers (e.g., mecA, blaKPC). A key challenge is the genotype-phenotype discrepancy; a detected resistance gene may not always be expressed, leading to a false-positive resistant prediction by the molecular test [22] [18]. Therefore, correlation with phenotypic AST remains crucial.
Verification is the linchpin that connects diagnostic science to effective antimicrobial stewardship and positive patient outcomes. As the 2025 study on RAST protocols concludes, even modified, resource-conscious verification methods can reduce the time-to-result significantly, enabling early and appropriate adjustment of antimicrobial therapy [23]. For researchers and scientists driving innovation in AST, a rigorous, standardized approach to verification is not just a procedural requirement—it is a fundamental contribution to preserving the efficacy of antibiotics and safeguarding global public health against the relentless threat of antimicrobial resistance.
Designing and Executing a Robust AST Verification Study
In the critical field of antimicrobial susceptibility testing (AST), the selection of an appropriate reference method forms the bedrock of reliable and reproducible data. For researchers and drug development professionals, this choice directly impacts the quality of resistance monitoring, the validity of new antimicrobial agent evaluations, and the understanding of resistance mechanisms. The global threat of antimicrobial resistance (AMR) necessitates precise AST methods to ensure the continued efficacy of existing treatments and to facilitate the development of new therapeutic agents [24]. Within this context, the scientific community primarily relies on three established approaches: the reference broth microdilution (BMD), the reference agar dilution (AD), and the use of verified commercial AST systems. Each method offers distinct advantages and limitations, making their comparative understanding essential for designing robust experimental protocols in both research and development settings. The recent joint guidance from CLSI and EUCAST emphasizes that while the reference BMD method is the recognized gold standard, understanding the appropriate application of each method—and the rigorous verification required for commercial systems—is crucial for scientific progress [24] [25].
Comparative Analysis of Reference and Commercial Methods
The table below summarizes the core characteristics, applications, and performance metrics of the three primary AST methods, synthesizing data from recent comparative studies and standards organization guidelines.
Table 1: Comparison of Antimicrobial Susceptibility Testing Methods
| Feature | Broth Microdilution (BMD) | Agar Dilution (AD) | Verified Commercial System |
|---|---|---|---|
| Reference Status | Gold standard per CLSI M07 & ISO 20776-1 [24] [25] | Reference method for anaerobes & population studies [26] [27] [28] | Alternative for routine use after verification [1] |
| Primary Application | Drug development, reference testing, defining breakpoints [25] | Testing multiple isolates against a single antibiotic concentration [26] [29] | High-throughput, routine clinical or research testing [30] |
| Throughput | Medium | High for multiple isolates [29] | High |
| Cost & Labor | Moderate (higher if commercial panels) | Lower for many isolates [28] | Higher initial cost, less labor-intensive |
| Quantitative Output | Yes (MIC) | Yes (MIC) | Yes (MIC) |
| Key Advantage | Standardized, well-defined quality control | Cost-effective for large-scale screening [29] | Standardized, easy to use, often automated |
| Key Limitation | Can be time-consuming and labor-intensive | Not practical for small numbers of isolates [28] | Requires extensive verification before use [1] |
Performance Agreement in Comparative Studies
Recent studies have quantitatively evaluated the agreement between these methods, providing a data-driven basis for selection.
Table 2: Observed Method Agreement in Recent Studies
| Study & Organism | Methods Compared | Essential Agreement (EA) | Categorical Agreement (CA) | Key Findings |
|---|---|---|---|---|
| Clostridiales spp. [27] | BMD (Sensititre) vs. AD | Variable by drug: 33.3% (Clindamycin) to 100% (Vancomycin) | Variable by drug: 33.3% (Clindamycin) to 100% (Metronidazole, Vancomycin) | Vancomycin showed high EA and CA; highest errors for clindamycin. |
| Bacteroides fragilis group [28] | In-house BMD vs. AD | >90% for most drugs | >90% for most drugs (Cefoxitin <90%) | In-house BMD is a cheaper, reliable alternative to AD for small sample numbers. |
| Campylobacter jejuni/coli [31] | BMD vs. Etest vs. AD | BMD vs. Etest: 90.0%BMD vs. AD: 78.7% | High correlation for ciprofloxacin and erythromycin | BMD is a reliable and easy method for Campylobacter AST. |
| Arcobacter butzleri [29] | AD vs. BMD (Reference) | High for Ciprofloxacin, Erythromycin, Gentamicin | High agreement | Aerobic AD at 24h showed the highest agreement with reference BMD. |
Experimental Protocols for Reference Methods
Protocol 1: Reference Broth Microdilution Method
This protocol is based on the CLSI M07 standard, recognized as the reference method for AST [24] [25].
Principle: The lowest concentration of an antimicrobial agent that prevents visible growth of a microorganism in a standardized broth after 16-20 hours of incubation is determined as the Minimum Inhibitory Concentration (MIC).
Materials:
- Cation-Adjusted Mueller-Hinton Broth (CAMHB)
- Sterile, U-bottom 96-well microdilution trays
- Antimicrobial stock solutions
- Bacterial suspension adjusted to 0.5 McFarland standard (~1.5 x 10^8 CFU/mL)
- Incubator set at 35±2°C
Procedure:
- Prepare Antimicrobial Dilutions: Perform two-fold serial dilutions of the antimicrobial agent in CAMHB directly in the microdilution trays. The final volume in each well is 100 µL.
- Inoculate Trays: Dilute the standardized bacterial suspension to a final concentration of approximately 5 x 10^5 CFU/mL in CAMHB. Add 100 µL of this suspension to each well of the tray, achieving a final inoculum of ~5 x 10^4 CFU/well.
- Incubate: Seal the trays to prevent evaporation and incubate aerobically at 35±2°C for 16-20 hours. For fastidious organisms, supplementation (e.g., with blood or serum) and extended incubation may be necessary [29].
- Read and Interpret MIC: The MIC is the lowest concentration of antimicrobial that completely inhibits visible growth. Compare results to appropriate quality control (QC) ranges for the organism and drug.
Protocol 2: Reference Agar Dilution Method
This protocol is widely used as a reference method for anaerobic bacteria and for screening large numbers of bacterial isolates against a single antibiotic concentration [26] [29] [28].
Principle: The MIC is determined as the lowest concentration of antimicrobial agent in an agar-based medium that prevents visible bacterial growth after a standard incubation period.
Materials:
- Mueller-Hinton Agar (MHA)
- Antimicrobial stock solutions
- Steers replicator or automated spotting device
- Bacterial suspension adjusted to 0.5 McFarland standard (~1.5 x 10^8 CFU/mL)
- Incubator (aerobic, microaerophilic, or anaerobic as required)
Procedure:
- Prepare Agar Plates: Incorporate two-fold serial dilutions of the antimicrobial agent into molten MHA. Pour into sterile Petri dishes. For fastidious organisms, supplement the agar (e.g., with 5% defibrinated sheep blood) [29].
- Spot Inoculate: Dilute the standardized bacterial suspension 1:10 to achieve a final inoculum of ~1.5 x 10^7 CFU/mL. Using a replicator, spot approximately 1-2 µL of this suspension onto the surface of the agar plates, delivering a final inoculum of 10^4 CFU/spot.
- Incubate: Allow the inoculum to dry and incubate the plates under the required atmospheric conditions (aerobic, microaerophilic, or anaerobic) and temperature for the prescribed time (typically 16-24 hours, or 48h for slow-growing organisms) [29].
- Read and Interpret MIC: The MIC is the lowest antimicrobial concentration that inhibits growth, or allows less than a predetermined number of colonies (e.g., <1 colony for a pure inoculum).
Verification of Commercial Antimicrobial Susceptibility Testing Systems
Introducing a commercial AST system into a laboratory requires a rigorous verification process to ensure it performs as specified by the manufacturer in the local environment [1]. This is distinct from validation, which is performed by the manufacturer.
Verification Workflow
The following diagram illustrates the critical steps for verifying a commercial AST system.
Key Verification Criteria and Definitions
Accuracy measures how close the test results are to the reference method results [1].
- Categorical Agreement (CA): The percentage of isolates where the susceptibility category (Susceptible, Intermediate, Resistant) matches the reference method. Acceptance: ≥90%.
- Essential Agreement (EA): The percentage of isolates where the test MIC is within ±1 two-fold dilution of the reference MIC. Acceptance: ≥90%.
Precision (Reproducibility) measures the ability to reproduce the same result on repeated testing. Acceptance: ≥95% agreement. [1]
Error Rates:
- Very Major Error (VME): False susceptible. The reference method calls the isolate Resistant, but the test method calls it Susceptible.
- Major Error (ME): False resistant. The reference method calls the isolate Susceptible, but the test method calls it Resistant.
- Acceptance: <3% for VME and ME combined. [1]
Essential Research Reagent Solutions
The following table details key reagents and materials required for establishing reference AST methods in a research setting.
Table 3: Key Reagents and Materials for Antimicrobial Susceptibility Testing
| Reagent/Material | Function/Description | Application Notes |
|---|---|---|
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standardized growth medium for BMD; divalent cation content is controlled for reproducible antibiotic activity. | The gold-standard medium for reference BMD per CLSI M07 and ISO 20776-1 [24] [25]. |
| Mueller-Hinton Agar (MHA) | Standardized solid medium for agar dilution and other diffusion-based AST methods. | May require supplementation with blood (5% sheep blood) or other growth factors for fastidious organisms [29]. |
| Defibrinated Sheep Blood | Common supplement to provide essential growth factors for fastidious pathogens like Campylobacter and Arcobacter. | Improves colony visualization on agar plates, aiding in clear MIC determination [31] [29]. |
| Fetal Bovine Serum (FBS) | Serum supplement for broths to support the growth of challenging microorganisms. | Note: Not currently approved for AST under CLSI standards for some organisms, where blood is the preferred supplement [29]. |
| Quality Control Strains | Well-characterized strains (e.g., E. coli ATCC 25922, S. aureus ATCC 29213) used to monitor the performance of the AST system. | QC testing is recommended every day of testing. Essential for both method setup and ongoing verification [1] [29]. |
| Sensititre Dried MIC Panels | Example of a commercial broth microdilution system with pre-dried antibiotics. | Must be verified against a reference method before implementation for in-use testing [30]. |
The selection of a reference method for AST is a strategic decision that balances scientific rigor, practical feasibility, and research objectives. Broth microdilution remains the undisputed gold standard, particularly for drug development and defining clinical breakpoints, as underscored by recent CLSI and EUCAST guidance [24] [25]. Agar dilution offers a robust, cost-effective alternative for specific applications, such as anaerobic bacteriology and large-scale epidemiological studies. Verified commercial systems provide excellent reproducibility and efficiency for high-throughput routine testing but require a substantial initial investment in validation.
For the research scientist, the key is to align the method with the experimental question. Foundational studies on resistance mechanisms and drug development should prioritize the reference BMD method. In contrast, surveillance studies involving hundreds of isolates may find agar dilution more practical. Regardless of the choice, adherence to standardized protocols and a commitment to rigorous verification, as outlined in this document, are non-negotiable for generating reliable, comparable, and scientifically valid data in the global fight against antimicrobial resistance.
Within the framework of precision verification for antimicrobial susceptibility testing (AST) methods, the strategic selection of bacterial strains forms the cornerstone of reliable and clinically relevant research. The growing global threat of antimicrobial resistance (AMR), which caused nearly 5 million deaths in 2019 according to WHO estimates, underscores the critical importance of accurate susceptibility testing [32]. This document provides detailed application notes and protocols for the rational selection and utilization of clinical isolates and quality control (QC) strains in AST research, with a specific focus on elucidating resistance mechanisms. Proper strain selection ensures that novel AST methods, whether phenotypic or genotypic, are accurately validated against clinically significant resistance patterns, thereby enabling precise therapeutic decisions and combating the AMR crisis [33].
Strain Selection Strategies for AST Research
The selection of appropriate bacterial strains is fundamental for generating meaningful AST data. A strategic approach combines well-characterized QC strains for method standardization with clinically relevant isolates that represent current resistance trends.
Table 1: Categories of Bacterial Strains for AST Research
| Strain Category | Purpose | Key Examples | Applications in AST Development |
|---|---|---|---|
| Quality Control (QC) Strains | Method verification, precision monitoring, reproducibility assurance | American Type Culture Collection (ATCC) standards | Daily run monitoring, inter-laboratory comparison, troubleshooting |
| Clinical Isolates | Representing current resistance epidemiology, novel mechanism discovery | Multidrug-resistant (MDR) pathogens from patient specimens | Evaluating test clinical correlation, detecting emerging resistances |
| Genetically Characterized Strains | Linking genotype to phenotype, validating molecular tests | Isogenic mutants with defined resistance mutations | Benchmarking genetic against phenotypic AST, pathway analysis |
Clinical Isolates: Capturing the Resistance Landscape
Clinical isolates provide the real-world context necessary for validating AST methods against circulating resistant pathogens. When selecting clinical isolates for precision verification studies, researchers should prioritize organisms listed by global surveillance systems. According to WHO reports, key pathogens of concern include carbapenem-resistant Acinetobacter baumannii, extended-spectrum β-lactamase (ESBL)-producing Escherichia coli and Klebsiella pneumoniae, and methicillin-resistant Staphylococcus aureus (MRSA) [33]. Recent data indicates that over 40% of E. coli and 55% of K. pneumoniae isolates globally are resistant to third-generation cephalosporins, highlighting the critical need for accurate detection methods for these pathogens [33].
For comprehensive method evaluation, isolate collections should encompass:
- Species diversity: Include Gram-negative rods (e.g., E. coli, K. pneumoniae, P. aeruginosa), Gram-positive cocci (e.g., S. aureus, Enterococcus spp.), and fastidious organisms.
- Resistance mechanism variety: Ensure representation of major resistance phenotypes (e.g., ESBL, carbapenemase production, vancomycin resistance).
- Recent isolates: Prioritize isolates collected within the past 1-2 years to reflect current resistance epidemiology.
Quality Control Strains: Ensuring Precision and Reproducibility
QC strains serve as the reference standard for verifying the precision and reproducibility of AST methods. These well-characterized strains with defined MIC ranges are essential for:
- Daily precision monitoring: Tracking inter-day and inter-operator variability.
- Method comparison: Standardizing results across different laboratories and platforms.
- Troubleshooting: Identifying technical issues in test performance.
Protocol 1 in Section 5.1 details the systematic incorporation of QC strains into AST verification workflows. The recent establishment of China-specific clinical breakpoints for eravacycline by the ChinaCAST committee exemplifies the importance of standardized QC in AST method harmonization [34].
Resistance Mechanisms Informing Strain Selection
Understanding molecular resistance mechanisms is crucial for intelligent strain selection in AST research. The table below outlines common resistance mechanisms and their genetic determinants that should be represented in a comprehensive strain collection.
Table 2: Key Resistance Mechanisms and Genetic Determinants for Strain Selection
| Resistant Pathogen | Primary Resistance Mechanism | Genetic Determinants | Phenotypic Expression |
|---|---|---|---|
| MRSA | Alteration of penicillin-binding protein (PBP2a) | mecA, mecC [32] | Resistance to β-lactam antibiotics |
| ESBL-producing Enterobacteriaceae | Production of extended-spectrum β-lactamases | blaTEM, blaSHV, blaCTX-M [32] | Resistance to penicillins, cephalosporins, aztreonam |
| Carbapenem-resistant Enterobacteriaceae (CRE) | Production of carbapenemases | blaKPC, blaOXA-48-like, blaNDM, blaIMP, blaVIM [32] | Resistance to carbapenems |
| Vancomycin-resistant Enterococci (VRE) | Alteration of peptidoglycan precursor targets | vanA, vanB [32] | Resistance to vancomycin |
| MDR Mycobacterium tuberculosis | Mutations in drug activation/target sites | katG, inhA, rpoB [32] | Resistance to isoniazid, rifampin |
Experimental Protocols for Strain Characterization
Protocol 1: Precision Verification of AST Methods Using QC Strains
Principle: This protocol establishes a framework for verifying the precision of novel AST methods through systematic testing of QC strains with defined MIC expectations.
Materials:
- QC strains (e.g., ATCC 25922 E. coli, ATCC 29213 S. aureus, ATCC 27853 P. aeruginosa)
- Cation-adjusted Mueller-Hinton broth (CAMHB)
- Antimicrobial stock solutions
- Novel AST platform/method for verification
Procedure:
- Strain Preparation:
- Subculture QC strains onto appropriate agar media.
- Incubate at 35±2°C for 18-24 hours.
- Prepare 0.5 McFarland standard suspensions in saline (~1.5 × 108 CFU/mL).
Method Implementation:
- For broth-based methods: Dilute bacterial suspension to ~5 × 105 CFU/mL in CAMHB containing serial dilutions of antimicrobial agents.
- For rapid methods: Follow manufacturer's instructions for inoculation.
- Incubate under appropriate conditions (35±2°C) for method-defined duration.
Precision Assessment:
- Test each QC strain in triplicate on three separate days (n=9 replicates total).
- Record MIC values or categorical interpretations (S/I/R) for each replicate.
- Calculate essential agreement (EA) and categorical agreement (CA) with reference methods.
Acceptance Criteria:
- ≥95% of results within established QC ranges for reference methods.
- For novel methods: ≥90% EA with reference MICs and ≥95% CA for categorical interpretations.
Protocol 2: Characterization of Clinical Isolates for Novel AST Development
Principle: This protocol provides a comprehensive approach for characterizing clinical isolates to validate novel rapid AST methods against traditional culture-based techniques.
Materials:
- Clinical isolates from specimen bank (prioritize MDR pathogens)
- Blood culture bottles (for simulated positive blood cultures)
- Reference AST materials (broth microdilution panels, antibiotic discs)
- Rapid AST platform (e.g., impedance-based, microscopic, fluorescent)
Procedure:
- Isolate Verification:
- Confirm species identification using MALDI-TOF MS or molecular methods.
- Verify purity by subculturing and examining colonial morphology.
Reference AST Testing:
- Perform reference broth microdilution according to CLSI/EUCAST guidelines.
- Incubate at 35±2°C for 16-20 hours before reading results.
- Document MIC values for key antimicrobial agents.
Rapid AST Parallel Testing:
- For impedance-based methods: Inoculate 2-hour broth cultures into detection system and monitor every 15 minutes for 4-8 hours [35].
- For microscopic methods: Use microfluidic systems to track single-cell division; analyze images algorithmically (30 min - 4 hours) [35].
- For fluorescence-based methods: Stain with SYBR Green I/PI or use resazurin reduction; measure fluorescence at 30-120 minutes [35].
Data Analysis:
- Compare time-to-result between reference and novel methods.
- Calculate essential agreement (EA) and categorical agreement (CA).
- Perform error rate analysis (very major errors, major errors, minor errors).
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for AST Strain Selection Studies
| Item | Function/Application | Example Specifications |
|---|---|---|
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standardized medium for broth microdilution AST | Contains adjusted Ca2+, Mg2+ ions; pH 7.2-7.4 |
| ATCC/NCTC QC Strains | Precision verification, method calibration | E. coli ATCC 25922, S. aureus ATCC 29213, P. aeruginosa ATCC 27853 |
| Antimicrobial Standard Powders | Preparation of exact drug concentrations for MIC testing | ≥90% purity; stored at -70°C; usage within stability period |
| Microtiter Pllets | High-throughput AST screening | 96-well, U-bottom; tissue culture treated |
| Fluorescent Vital Dyes (SYBR Green I/PI) | Viability assessment in rapid AST methods | SYBR Green I (1:10,000 dilution), PI (20 µg/mL) [35] |
| Resazurin Sodium Salt | Metabolic activity indicator in colorimetric AST | 0.01% w/v in saline; filter-sterilized [35] |
| DNA Extraction Kits | Nucleic acid isolation for molecular resistance detection | Spin-column technology; elution volume 50-100 µL |
| qPCR Master Mixes | Amplification of resistance genes | Contains DNA polymerase, dNTPs, buffers; freeze-dried stable |
Workflow Visualization
AST Strain Selection Workflow
Resistance Mechanism Detection Pathways
Strategic strain selection employing both standardized QC strains and clinically relevant isolates is fundamental to precision verification in antimicrobial susceptibility testing research. The protocols and frameworks outlined in this document provide a systematic approach for researchers to validate novel AST methods against current resistance challenges. As molecular methods continue to evolve alongside phenotypic techniques, maintaining comprehensive strain collections that represent the dynamic landscape of antimicrobial resistance will be crucial for developing the rapid, accurate diagnostic tools needed to address the global AMR crisis. The integration of strain selection strategies with mechanistic understanding of resistance pathways will ultimately enhance the precision and clinical utility of AST methods, supporting optimized patient care and antimicrobial stewardship efforts worldwide.
Verification of antimicrobial susceptibility testing (AST) systems is a critical quality process in clinical microbiology laboratories, ensuring that systems perform according to manufacturer specifications within a local laboratory environment [1]. Unlike validation, which is conducted by manufacturers to obtain regulatory clearance, verification is performed by laboratories when introducing new testing methods, new antimicrobial agents, or new instruments [1]. This application note provides detailed protocols for comprehensive and limited verification studies, framed within the broader context of precision verification for AST methods research. We outline specific sample size requirements, study designs, and acceptance criteria aligned with Clinical and Laboratory Standards Institute (CLSI) guidelines to ensure reliable implementation of AST systems for researchers, scientists, and drug development professionals.
Comprehensive vs. Limited Verification: Key Concepts
The choice between comprehensive and limited verification depends on the nature of the change being implemented in the laboratory. Each approach has distinct applications and procedural requirements.
Table 1: Verification Types and Their Applications
| Type of Change | Verification Approach | Typical Scenarios |
|---|---|---|
| Fundamental Change | Comprehensive Verification | New AST system implementation; Change in testing methodology (e.g., disk diffusion to automated system) |
| Incremental Change | Limited Verification | Adding a new antimicrobial agent to an existing panel; Adding a second instrument of the same model |
| Minor Update | Limited Verification | New dilutions added for MIC testing (e.g., due to breakpoint changes) |
Comprehensive verification is required when implementing a fundamentally new testing system or methodology. This approach demands more rigorous testing to establish performance baseline [1]. Limited verification applies to incremental changes where the core system remains unchanged, requiring a more focused dataset to confirm performance for the specific modification [1].
Sample Size Requirements and Acceptance Criteria
Adherence to prescribed sample sizes and acceptance criteria is fundamental to generating statistically valid verification data. The following parameters ensure reliable verification outcomes.
Table 2: Sample Size Requirements and Acceptance Criteria for AST Verification
| Parameter | Comprehensive Verification | Limited Verification |
|---|---|---|
| Accuracy (Number of isolates) | Minimum of 30 isolates [1] | Minimum of 10 isolates (new agent) or 30 isolates (new dilutions) [1] |
| Accuracy (Categorical Agreement - CA) | ≥ 90% agreement [1] | ≥ 90% agreement [1] |
| Accuracy (Essential Agreement - EA) | ≥ 90% agreement [1] | ≥ 90% agreement [1] |
| Accuracy (Error Rates) | < 3% very major errors (false susceptible) or major errors (false resistant) [1] | < 3% very major errors or major errors [1] |
| Precision/Reproducibility | Test 5 isolates x 3 replicates [1] | Test QC strains 3x for 5 days or 1x daily for 20 days [1] |
| Precision Agreement | ≥ 95% of test results [1] | ≥ 95% of QC strain results within specifications [1] |
Key Definitions for Acceptance Criteria
- Categorical Agreement (CA): The percentage of isolates where the susceptibility category (Susceptible-S, Intermediate-I, or Resistant-R) matches between the new method and the reference method [1].
- Essential Agreement (EA): For minimum inhibitory concentration (MIC) methods, the percentage of results where the new method's MIC is within ±1 doubling dilution (or ±2 doubling dilutions for yeast) of the reference method result [1].
- Very Major Error (VME): Occurs when the new method incorrectly reports an isolate as "Susceptible" but the reference method categorizes it as "Resistant" [1].
- Major Error (ME): Occurs when the new method incorrectly reports an isolate as "Resistant" but the reference method categorizes it as "Susceptible" [1].
Experimental Protocol for Comprehensive Verification
Isolate Selection and Preparation
Select a minimum of 30 unique clinical bacterial isolates [1]. The selection should strategically include:
- Strains with relevant resistance mechanisms to challenge the system's detection capabilities [1].
- A representative mix of species clinically relevant to the antimicrobial agents being verified [1].
- Quality Control (QC) strains with well-defined AST profiles, such as E. coli ATCC 25922 and Pseudomonas aeruginosa ATCC 27853 [36].
- Proficiency testing isolates or strains obtained from external sources like the CDC-FDA Antimicrobial Resistance Isolate Bank to ensure unbiased assessment [1].
Prepare inoculum according to CLSI standards. Briefly, select 3-5 well-isolated colonies from an 18-24 hour culture, suspend in sterile saline, and adjust turbidity to a 0.5 McFarland standard [15]. Use the standardized inoculum within 15-20 minutes of preparation [15] [36].
Testing Procedure and Data Analysis
- Concurrent Testing: Test all selected isolates using both the new AST system and the reference method (e.g., broth microdilution) in parallel [1].
- Quality Control: Include appropriate QC strains in each run to verify testing conditions [15].
- Incubation: Follow manufacturer-recommended incubation conditions (typically 35°C for 16-20 hours for non-fastidious organisms) [15].
- Result Interpretation: Read and interpret results according to the manufacturer's instructions and CLSI/EUCAST breakpoints [15].
Calculate performance metrics:
- Categorical Agreement (CA): (Number of category agreements / Total number of comparisons) × 100
- Essential Agreement (EA): (Number of MICs within ±1 doubling dilution / Total number of MIC comparisons) × 100
- Error Rates: Calculate very major error and major error rates as defined in Section 3.1
Compare calculated metrics against acceptance criteria in Table 2. Document all discrepancies and investigate any outliers.
Experimental Protocol for Limited Verification
Scenarios and Testing Strategies
Scenario A: New Antimicrobial Agent
- Test a minimum of 10 clinical isolates [1].
- Select isolates with a range of susceptibilities (susceptible, intermediate, resistant) to the new agent, if available.
- Follow testing procedures outlined in Section 4.2, focusing analysis specifically on the new antimicrobial agent.
Scenario B: New Instrument of Same Model
- Perform reproducibility testing using QC strains tested 3 times for 5 days, or once daily for 20 days [1].
- Compare results between the new instrument and the existing verified instrument.
- Ensure all QC results fall within established quality control ranges [1].
Scenario C: New Dilutions or Breakpoint Changes
- Test a minimum of 30 clinical isolates [1].
- Focus on isolates with MICs near the new breakpoints to challenge the revised categorization.
- Verify that categorical interpretations align with expectations based on the new breakpoints.
Precision (Reproducibility) Testing
For both comprehensive and limited verification, precision testing confirms result consistency:
- Test 5 bacterial isolates (either QC strains or clinical isolates) in triplicate (on different days or by different operators) [1].
- For MIC methods, results are considered reproducible if they fall within ±1 doubling dilution [1].
- For categorical results, interpretations (S, I, R) should be 95% reproducible [1].
Workflow and Logical Relationships
The following diagram illustrates the decision-making process and workflow for planning and executing an AST verification study:
The Scientist's Toolkit: Research Reagent Solutions
Successful verification requires specific materials and reagents with standardized quality.
Table 3: Essential Research Reagents and Materials for AST Verification
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standardized growth medium for broth microdilution AST | Ensures consistent ion concentration; Required for reliable MIC results [36] |
| Mueller-Hinton Agar (MHA) | Standardized solid medium for disk diffusion and agar dilution | Batch consistency critical for zone size reproducibility [15] |
| 0.5 McFarland Standard | Turbidity standard for inoculum preparation | Essential for standardizing bacterial suspension to ~1.5 × 10⁸ CFU/mL [15] |
| Quality Control Strains | Verification of test system performance | Use well-characterized strains (e.g., E. coli ATCC 25922, P. aeruginosa ATCC 27853) [36] |
| Reference Antimicrobial Powders | Preparation of reference method dilutions | Source from certified suppliers; Verify potency and purity [36] |
| Antimicrobial Disks | For disk diffusion method | Store desiccated at -20°C; Use before expiration date [15] |
| EZMTT Reagent | Metabolic indicator for colorimetric AST | Enhances detection sensitivity; Identifies resistant subpopulations [36] |
Robust verification of antimicrobial susceptibility testing systems requires careful consideration of sample size and study design. Comprehensive verification (minimum 30 isolates) is necessary for new systems or methodologies, while limited verification (minimum 10 isolates) suffices for incremental changes. Adherence to established acceptance criteria—including ≥90% categorical and essential agreement with <3% major error rates—ensures reliable system performance. By following these structured protocols, laboratories can confidently implement new AST systems and modifications, ultimately contributing to accurate patient results and effective antimicrobial stewardship.
Precision verification is a cornerstone of method development in antimicrobial susceptibility testing (AST), ensuring that new or modified testing systems produce reliable, reproducible results that correlate with clinical outcomes. Establishing statistically sound acceptance criteria for categorical agreement (CA) and essential agreement (EA) is fundamental for validating AST methods against reference standards [1]. These metrics quantitatively assess the precision and accuracy of a test system, forming the critical bridge between experimental data and clinical applicability. For researchers and drug development professionals, rigorous verification protocols are not merely regulatory hurdles but essential practices for generating credible data that informs therapeutic decisions and combats the escalating antimicrobial resistance crisis [37].
Defining Agreement Metrics and Acceptance Thresholds
In AST verification, Categorical Agreement and Essential Agreement serve distinct but complementary purposes for comparing a new test method to a reference method.
- Categorical Agreement (CA) measures the percentage of isolates for which the interpretive category result (Susceptible (S), Intermediate (I), or Resistant (R)) from the new test method is identical to the result from the reference method [1].
- Essential Agreement (EA) measures the percentage of isolates for which the Minimum Inhibitory Concentration (MIC) obtained by the new test method is within a pre-defined dilution range (typically ±1 two-fold dilution) of the MIC determined by the reference broth microdilution method [1].
Acceptance criteria for these metrics are standardized by guidelines such as the Clinical and Laboratory Standards Institute (CLSI) M52 document [1]. The following table summarizes the key performance thresholds for a comprehensive verification study.
Table 1: Acceptance Criteria for Antimicrobial Susceptibility Testing System Verification
| Performance Criteria | Definition | Acceptance Threshold |
|---|---|---|
| Accuracy | ||
| Categorical Agreement (CA) | Agreement in S/I/R categorization between new and reference method | ≥ 90% of test results [1] |
| Essential Agreement (EA) | MIC result within ±1 doubling dilution of reference MIC | ≥ 90% of test results [1] |
| Discrepancy Errors | Very Major Error (VME): False susceptible by new methodMajor Error (ME): False resistant by new method | < 3% for VME/ME combined [1] |
| Precision (Reproducibility) | Agreement of MIC values or categorical interpretations in repeat testing | ≥ 95% of test results [1] |
Experimental Protocols for Verification Studies
Study Design and Isolate Selection
A robust verification study begins with careful planning and isolate selection to ensure results are clinically relevant and statistically powerful.
- Strain Panel Composition: Test a minimum of 30 unique bacterial isolates for a comprehensive verification (e.g., for a new system or a change in testing method) [1]. For limited verification (e.g., adding a new antimicrobial agent to an existing method), a minimum of 10 isolates may be sufficient [1].
- Strain Characteristics: The selected isolates should represent a diverse range of clinically relevant species and resistance mechanisms. The panel must include:
- Strains with known resistance mechanisms (e.g., ESBL, carbapenemase-producing, methicillin-resistant Staphylococcus aureus [37]).
- Quality Control (QC) strains with well-defined MIC ranges [15].
- Isolates from reputable sources such as the CDC-FDA Antimicrobial Resistance Isolate Bank or EUCAST strain panels [1].
- Reference Method: The gold standard for comparison is the reference broth microdilution (rBMD) method performed according to ISO 20776-1 or CLSI M07 standards [38]. Alternative reference methods can include a previously verified in-vitro diagnostic (IVD) method or testing against isolates with known AST results from an external verified system [1].
Procedure for Parallel Testing
The core experimental workflow involves testing the entire panel of isolates in parallel using both the new method and the reference method.
Diagram: Experimental Workflow for AST Method Verification
Detailed Methodology:
Inoculum Preparation:
- Select 3-5 well-isolated colonies from an 18-24 hour fresh subculture [15].
- Create a bacterial suspension in saline or broth to a density equivalent to a 0.5 McFarland standard (approximately 1-2 x 10^8 CFU/mL) [15] [39].
- Verify turbidity with a densitometer. Within 15 minutes of preparation, further dilute the suspension in standardized Mueller-Hinton Broth (for rBMD) or as required by the new test system to achieve a final inoculum of ~5 x 10^5 CFU/mL [15] [39].
Testing and Incubation:
- Inoculate the rBMD panels and the new test system in parallel using the same standardized inoculum [39].
- Inculate panels or plates according to guidelines: typically at 35°C ± 2°C for 16-20 hours in an ambient atmosphere [15]. Fastidious organisms may require different conditions or media supplements [38].
Endpoint Reading and Recording:
- For rBMD and MIC-based methods, read the Minimum Inhibitory Concentration (MIC) – the lowest concentration of antimicrobial that completely inhibits visible growth [38].
- For disk diffusion, measure the diameter of the zone of inhibition (including the disk) to the nearest millimeter using a caliper [15].
- Record all raw data (MICs in µg/mL or zone diameters in mm) for subsequent analysis.
Data Analysis and Interpretation
Analyze the collected data to calculate key performance metrics against the pre-defined acceptance criteria.
Table 2: Formulas for Calculating Key Verification Metrics
| Metric | Calculation Formula |
|---|---|
| Essential Agreement (EA) | (Number of isolates with test MIC within ±1 doubling dilution of reference MIC / Total number of isolates tested) x 100 |
| Categorical Agreement (CA) | (Number of isolates with identical S/I/R categorization by both methods / Total number of isolates tested) x 100 |
| Very Major Error (VME) | (Number of isolates false susceptible by the test method but resistant by reference method / Total number of resistant isolates by reference method) x 100 |
| Major Error (ME) | (Number of isolates false resistant by the test method but susceptible by reference method / Total number of susceptible isolates by reference method) x 100 |
| Minor Error (mE) | (Number of isolates with intermediate result by one method and susceptible or resistant by the other / Total number of isolates tested) x 100 |
Interpretation Logic: Compare the calculated values for EA, CA, and errors against the acceptance thresholds in Table 1. The test system is considered to have met verification criteria if all thresholds are satisfied for the antimicrobial agents being evaluated [1].
Diagram: Decision Logic for Verification Outcome
The Scientist's Toolkit: Research Reagent Solutions
Successful AST verification relies on high-quality, standardized reagents and materials. The following table details essential components for setting up reference broth microdilution studies.
Table 3: Essential Research Reagents and Materials for AST Verification
| Item | Function/Description | Key Specifications |
|---|---|---|
| Reference Strains | Quality control organisms to ensure test conditions and reagents are performing within established limits [15]. | E. coli ATCC 25922, P. aeruginosa ATCC 27853, S. aureus ATCC 29213 [39]. |
| Cation-Adjusted Mueller Hinton Broth (CAMHB) | Standardized growth medium for broth microdilution AST [38]. | Must contain controlled levels of Ca²⁺, Mg²⁺, and sometimes Zn²⁺ ions, which can affect MICs of certain drugs like aminoglycosides and tetracyclines [38]. |
| Antimicrobial Powders | Pure substance for preparing stock solutions to create dilution panels [39]. | High-purity, certified reference standards. Solubilized in CLSI/ISO-recommended solvents (e.g., water, dimethyl sulfoxide) [39]. |
| Microtiter Plates | Platform for preparing and performing broth microdilution tests [39]. | 96-well, sterile, non-tissue-culture-treated polystyrene plates. |
| Sterile Saline (0.85-0.9%) | Suspension medium for preparing bacterial inoculum to the required McFarland standard [15]. | Clear, particle-free solution. |
| McFarland Standards | Reference for standardizing the density of bacterial inocula to ensure a consistent number of organisms in each test [15]. | 0.5 McFarland standard for AST, equivalent to ~1.5 x 10⁸ CFU/mL. |
The establishment and strict adherence to acceptance criteria for categorical and essential agreement are non-negotiable for the precision verification of AST methods. The thresholds of ≥90% for EA and CA, with a combined major error rate of less than 3%, provide a rigorous benchmark that, when met, gives researchers and regulators confidence in the test system's clinical reliability. By following the detailed experimental protocols outlined—from careful isolate selection and standardized parallel testing to systematic data analysis—professionals in drug development and microbiology can ensure their AST methods are accurately characterized, ultimately contributing to more effective patient treatment and strengthened antimicrobial stewardship.
Step-by-Step Protocol for Testing Accuracy and Reproducibility
Precision verification is a cornerstone of reliable antimicrobial susceptibility testing (AST) in clinical and research microbiology. Before a new AST system can be routinely deployed, laboratories must verify that it performs according to the manufacturer's specifications within their own operational environment [40]. This process ensures the accuracy and reproducibility of results, which are critical for both patient care and antimicrobial resistance research [2]. This protocol outlines a standardized, step-by-step procedure for verifying the accuracy and reproducibility of AST methods, framed within the broader context of precision verification for antimicrobial susceptibility testing research.
Adhering to this protocol helps laboratories meet international standards, such as those described in the Clinical and Laboratory Standards Institute (CLSI) M52 guideline [40] and ISO 15189 requirements [2]. The following sections provide detailed methodologies for planning, executing, and analyzing verification studies for AST systems.
Verification Framework and Definitions
Validation vs. Verification: It is crucial to distinguish between these two processes. Validation involves the extensive collection of performance data, often by the manufacturer across multiple sites, to seek regulatory clearance (e.g., FDA, IVD/CE marking) [40]. In contrast, verification is performed by the end-user laboratory to confirm that a commercially validated system operates correctly in its specific environment and according to the manufacturer's claims [40].
Two tiers of verification exist:
- Comprehensive Verification: Required when introducing a completely new AST system or a fundamental change in methodology.
- Limited Verification: Sufficient when adding a new antimicrobial agent to an existing, verified method [40].
Pre-Verification Planning
Selection of Reference Method and Strains
A critical first step is selecting an appropriate reference method against which the new AST system will be compared. According to guidelines, one of the following three reference options should be selected [40]:
- IVD Labelled Method: A previously verified and clinically established testing method.
- Reference AST Method: A standardized reference method such as broth microdilution or agar dilution for Minimum Inhibitory Concentration (MIC) testing [41].
- Isolates with Known AST Results: Bacterial isolates with well-characterized and verified AST results, which can be sourced from external repositories.
The selection of bacterial strains is paramount to a robust verification. The isolates tested must cover a clinically relevant range and include strains with known resistance mechanisms [40]. The selection should be representative of the organisms for which the antimicrobial agents are clinically indicated. Proficiency testing isolates and strains from resources like the CDC-FDA Antimicrobial Resistance Isolate Bank (AR Bank) or the EUCAST panels of phenotypically defined strains are excellent choices [40].
Table 1: Essential Resources for Strain Selection
| Resource | Description | Use Case |
|---|---|---|
| CDC-FDA AR Isolate Bank [40] | Provides various bacterial isolates with characterized resistance. | Sourcing strains with specific, defined resistance mechanisms. |
| EUCAST Strain Panels [40] | Panels of phenotypically defined strains. | Verifying performance against European standards. |
| Clinical Isolates [40] | Strains from local clinical cases representative of the patient population. | Ensuring the verification is relevant to the local epidemiology. |
Determination of Sample Size
The number of isolates tested depends on the type of verification being performed. While specific numbers should be confirmed against the latest CLSI M52 guideline, the principle is that a comprehensive verification requires a larger set of isolates to robustly assess performance across different organism groups and resistance phenotypes, whereas a limited verification for a single new antimicrobial may require fewer isolates [40].
Experimental Protocols
Protocol 1: Testing for Accuracy
Objective: To determine the degree of agreement between the results obtained from the new AST system and the results from the selected reference method.
Materials:
- Selected bacterial isolates (as per Section 3.1)
- New AST system and all required reagents
- Materials for the reference method
- Quality control strains
Methodology:
- Sub-culturing: Revive all selected isolates onto appropriate non-selective solid media to ensure purity and good viability.
- Inoculum Preparation: Prepare standardized inoculum suspensions of each test isolate according to both the new AST system's instructions and the reference method's guidelines. Use McFarland standards or automated turbidimetry to ensure accurate cell density.
- Parallel Testing: Test each isolate simultaneously (or in the same batch) using the new AST system and the reference method. This minimizes variability due to time or sub-culture passage.
- Incubation: Incubate tests under the specified conditions (temperature, atmosphere, duration) for both methods.
- Result Reading: Interpret and record the results for both methods. For MIC-based systems, record the exact MIC value in µg/mL [41]. For disk diffusion, record the zone diameter in millimeters. For categorical agreements (Susceptible, Intermediate, Resistant), use established clinical breakpoints (e.g., from CLSI or EUCAST) for interpretation [41].
Data Analysis:
- For MIC tests, calculate the Essential Agreement (EA), which is the percentage of isolates for which the MIC result from the new system is within ±1 two-fold dilution of the MIC from the reference method.
- For categorical results, calculate the Categorical Agreement (CA), which is the percentage of isolates placed in the same interpretive category (S, I, or R) by both the new system and the reference method.
- Discrepancies should be investigated. Major errors (ME) occur when the reference method result is "Susceptible" and the new system result is "Resistant." Very major errors (VME) occur when the reference method result is "Resistant" and the new system result is "Susceptible" [11].
Protocol 2: Testing for Reproducibility
Objective: To assess the precision of the new AST system by determining its ability to yield consistent results when the same sample is tested multiple times under defined conditions.
Materials:
- A panel of 3-5 bacterial isolates, selected to include susceptible and resistant strains.
- New AST system and all required reagents.
Methodology: A reproducibility study should evaluate different sources of variability:
- Within-run (Repeatability): Test the same panel of isolates multiple times (e.g., 3-5 repetitions) in a single run by a single operator using the same equipment and reagents.
- Between-run: Test the same panel of isolates in different runs performed on different days.
- Between-operator: Have multiple trained technologists (e.g., 2-3) test the same panel of isolates independently.
Data Analysis:
- Calculate the percentage of results that are in agreement for each strain across all repetitions.
- The reproducibility is considered acceptable if a high percentage of results (e.g., ≥95%) are in essential and categorical agreement across all tested conditions for a given strain.
Table 2: Key Performance Metrics and Acceptance Criteria
| Metric | Definition | Interpretation |
|---|---|---|
| Essential Agreement (EA) | Percentage of MICs within ±1 doubling dilution of the reference MIC. | Measures quantitative precision of the MIC value. |
| Categorical Agreement (CA) | Percentage of results in the same susceptibility category (S/I/R). | Measures clinical interpretative agreement. |
| Major Error (ME) | False-resistant result (Reference: S, New: R). | Indicates a potential for limiting effective treatment options. |
| Very Major Error (VME) | False-susceptible result (Reference: R, New: S). | A critical error that could lead to treatment failure. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for AST Verification
| Item | Function / Explanation |
|---|---|
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | The standardized medium for broth microdilution AST, ensuring consistent ion concentration for reliable antibiotic activity [41]. |
| Mueller-Hinton Agar Plates | The standardized medium for agar-based AST and disk diffusion testing [42]. |
| McFarland Standards | Suspensions of barium sulfate used to standardize the turbidity (and thus the approximate cell density) of bacterial inoculums. |
| Quality Control (QC) Strains | Strains with well-defined MIC ranges (e.g., E. coli ATCC 25922, S. aureus ATCC 29213). Used to monitor the daily performance of the AST system [40]. |
| Antimicrobial Powders/Disks | Pure, potency-defined antibiotics for preparation of in-house panels or for disk diffusion tests. |
| 96-Well Microtiter Plates | Used for custom or commercial broth microdilution panels [41]. |
| Sterile Saline or Broth | For diluting and standardizing bacterial suspensions. |
Workflow and Logical Relationships
The following diagram illustrates the complete verification workflow, from initial planning to final implementation of the AST system.
Analysis and Troubleshooting
After completing the experiments, data analysis focuses on calculating the performance metrics outlined in Table 2. The verification is typically considered successful if the calculated EA and CA meet or exceed the thresholds defined by the manufacturer's claims and relevant guidelines (e.g., CLSI M52). The rates of Major and Very Major Errors must fall below established safety limits.
Failed verification requires a systematic investigation. Potential causes include:
- Incorrect inoculum preparation: Re-check the turbidity standardization process.
- Compromised reagents: Check the storage conditions and expiration dates of all antimicrobials and media. Repeat testing with fresh Quality Control strains.
- Deviation from protocol: Ensure all steps were performed exactly as specified by both the new system's instructions and the reference method.
- Technical error: Review the techniques of the personnel involved and provide re-training if necessary.
Once the issue is identified and corrected, the verification study, or the failed portion of it, must be repeated.
This protocol provides a detailed framework for laboratories to verify the accuracy and reproducibility of new antimicrobial susceptibility testing systems. By rigorously following these step-by-step procedures for planning, execution, and analysis, researchers and clinical scientists can ensure that the AST data generated is reliable, precise, and fit for its intended purpose in both patient management and antimicrobial resistance research. A successful verification is the final, critical step before a new AST method can be trusted for routine diagnostics and data generation, thereby strengthening the overall framework of precision medicine in microbiology.
Overcoming Common Verification Challenges and Streamlining Workflows
In antimicrobial susceptibility testing (AST), discrepant results between a new method and a reference standard are systematically categorized into specific error types. These discrepancies carry significant implications for patient treatment and antimicrobial stewardship. Very major errors (VMEs) represent the most critical category, occurring when a resistant organism is incorrectly reported as susceptible, potentially leading to treatment failure with ineffective antibiotics [1]. Major errors (MEs) happen when a susceptible organism is misclassified as resistant, which may result in the unnecessary avoidance of a potentially effective drug [1]. A third category, minor errors, involve discrepancies in intermediate categorization but do not directly impact susceptible/resistant interpretation [43].
Establishing standardized protocols for resolving these errors is fundamental to precision verification in AST method development. The consistent application of these definitions ensures data comparability across studies and maintains the integrity of the verification process, which is critical for researchers and drug development professionals validating new AST systems or reagents [1].
Performance Standards and Acceptance Criteria
Regulatory bodies and standards organizations provide clear quantitative benchmarks for AST method verification. Adherence to these criteria is essential for demonstrating methodological robustness.
Table 1: Acceptance Criteria for AST Verification Studies
| Performance Metric | Definition | Acceptance Limit |
|---|---|---|
| Categorical Agreement (CA) | Percentage of results where susceptibility category (S, I, R) matches the reference method [1]. | ≥ 90% of test results [1]. |
| Essential Agreement (EA) | Percentage of MIC results within ±1 doubling dilution (or ±2 for yeast) of the reference MIC [1]. | ≥ 90% of test results [1]. |
| Very Major Error (VME) Rate | Percentage of false susceptible results among reference-resistant isolates [1]. | < 3% of resistant isolates [1]. |
| Major Error (ME) Rate | Percentage of false resistant results among reference-susceptible isolates [1]. | < 3% of susceptible isolates [1]. |
| Precision (Reproducibility) | Agreement of repeated results for the same isolate and antimicrobial [1]. | ≥ 95% of test results [1]. |
Experimental Protocol for Error Resolution
This detailed protocol provides a step-by-step workflow for investigating and resolving VMEs and MEs during AST method verification.
Initial Identification and Documentation
- Discrepancy Log: Create a log of all discrepant results, noting the isolate identifier, antimicrobial agent, result from the test method, result from the reference method, and the calculated error type (VME, ME) [1].
- Raw Data Review: Examine the raw data from both tests. For disk diffusion, re-measure zone diameters. For broth microdilution, review growth patterns in each well. For automated systems, check the growth curve and interpretation data [43].
Investigative and Confirmatory Testing
- Repeat Testing: Repeat the AST using the test method and the reference method from a fresh subculture of the original isolate. This controls for technical errors in the initial test setup [1].
- Reference Method Confirmation: The gold standard for resolution is a validated reference method, most commonly broth microdilution (BMD) or agar dilution [1] [44]. Use the same inoculum for both the repeat test method and the reference BMD to minimize variability.
- Utilize Reference Strains: Include quality control (QC) strains with known AST profiles in the confirmation process. Strains from the CDC-FDA Antimicrobial Resistance Isolate Bank or EUCAST-defined strain sets are recommended for this purpose [1].
Root Cause Analysis and Final Categorization
- Analyze Resistance Mechanisms: If VMEs or MEs persist after confirmation, investigate underlying resistance mechanisms. Techniques like whole-genome sequencing (WGS) can identify resistance genes (e.g., blaKPC, blaNDM, blaOXA) that may not be reliably detected by the test method [44] [43].
- Phenotypic Characterization: Employ supplementary phenotypic tests, such as the modified carbapenem inactivation method (mCIM) for carbapenemase production, to confirm resistance phenotypes that may explain discrepancies [44] [43].
- Final Interpretation: Reclassify the result based on the confirmatory reference method and mechanistic data. The confirmed result overrides the initial test method result for the final analysis.
The following workflow diagrams the logical pathway for resolving these critical errors.
The Scientist's Toolkit: Key Reagents and Materials
Successful verification and error resolution require specific, high-quality reagents and reference materials.
Table 2: Research Reagent Solutions for AST Verification
| Reagent/Material | Function in Protocol | Application Example |
|---|---|---|
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standardized medium for broth microdilution, ensures consistent ion concentration for reliable MIC results [44]. | Serves as the base for reference BMD during confirmatory testing [1]. |
| Fastidious Anaerobe Agar (FAA) | Specialized medium for agar dilution AST of fastidious organisms like Clostridioides difficile; improves inter-laboratory reproducibility [45]. | Used as a standardized medium for AST of anaerobic bacteria [45]. |
| Defibrinated Horse/Sheep Blood | Supplement for culture media to support growth of fastidious organisms in quality control processes [23]. | Added to blood culture bottles for QC strains in rapid AST protocols [23]. |
| Quality Control (QC) Strains | Reference strains with well-defined AST profiles (e.g., E. coli ATCC 25922, P. aeruginosa ATCC 27853) for monitoring test precision and accuracy [1]. | Used daily to ensure AST system performance is within specified control limits [1]. |
| CDC-FDA AR Isolate Bank Strains | Panels of clinically relevant isolates with characterized resistance mechanisms for comprehensive system verification [1]. | Used to challenge a new AST system with strains harboring specific resistance genes (e.g., carbapenemases) [1]. |
Case Study: Proficiency Testing with Carbapenemase-Producing Isolates
A 2025 nationwide proficiency study in Spain highlights the practical challenges in error resolution. The study distributed single (SCP) and double carbapenemase-producing (DCP) Gram-negative isolates to 73 laboratories to evaluate their performance in reporting reliable carbapenem susceptibility and detecting carbapenemase production [43].
- Key Findings on Errors: The study found that DCP isolates generally showed lower essential agreement (EA) and a higher number of clinical errors compared to SCP isolates when tested with gradient strips [43]. This underscores that complex resistance mechanisms can increase discrepancy rates.
- Method-Dependent Sensitivity: The sensitivity of phenotypic methods varied significantly. For instance, the carbapenem inactivation method (CIM) showed 100% sensitivity for DCP isolates but only 93% for SCP isolates. Conversely, disk diffusion with inhibitors showed lower sensitivity for DCP (83.3%) than for SCP isolates (90.4%) [43].
- Resolution with Molecular Methods: Molecular methods (e.g., lateral flow immunoassays, PCR) demonstrated higher sensitivity for carbapenemase gene detection in DCP isolates than most phenotypic methods, highlighting their value in root cause analysis for VMEs involving these pathogens [43].
This case demonstrates that the choice of confirmatory method is critical and must be appropriate for the resistance mechanisms suspected in the isolate.
The escalating threat of antimicrobial resistance (AMR) necessitates rigorous and precise antimicrobial susceptibility testing (AST) in research and development. The CDC/FDA Antimicrobial Resistance (AR) Isolate Bank and international proficiency testing (PT) programs, such as the Proficiency Test for Antimicrobial Susceptibility Testing (PTAST), provide essential, well-characterized biological resources to meet this need [46] [47]. These repositories offer isolates critical for validating new diagnostic tests, challenging novel antimicrobial drugs, and ensuring the accuracy and comparability of AST data across laboratories [46] [48]. This application note details protocols for the effective utilization of these resources within the specific context of precision verification for AST methods, providing researchers with a framework to overcome common sourcing challenges.
Table: Overview of Key Isolate Banks for AST Research
| Resource Name | Managing Agency/Organization | Primary Application | Key Features |
|---|---|---|---|
| CDC/FDA AR Isolate Bank | CDC and FDA [46] | Diagnostic test validation, drug R&D, resistance mechanism studies [46] [48] | No cost for approved institutions; provides isolate panels with susceptibility profiles and WGS data [46] [48] |
| PTAST | UN FAO & Chulalongkorn University Veterinary [47] | External quality assurance for AMR surveillance in Asia [47] | No participation fee; assesses lab performance in ID and AST for specific pathogens [47] |
| ARLG Virtual Biorepository | Antibacterial Resistance Leadership Group [46] | Research | Access to clinically well-characterized Gram-positive and Gram-negative bacteria [46] |
| BEI Resources | NIAID [46] | Research | Reagents for studying priority pathogens and emerging infectious diseases [46] |
Resource Characterization and Acquisition
The CDC/FDA AR Isolate Bank
The AR Isolate Bank is a curated biorepository containing bacterial and fungal isolates gathered from national surveillance, outbreak activities, and collaborators [46] [48]. It is uniquely positioned to provide "isolates for action," which are characterized by:
- Comprehensive Data: Each order includes the isolate's antimicrobial susceptibility profile, known resistance biomarkers, source, collection year, and links to publicly available Whole Genome Sequence data [46].
- Panel-Based Distribution: Isolates are grouped into panels tailored to specific resistance threats or research needs, facilitating systematic testing rather than piecemeal evaluation [46] [48].
- Accessibility: The isolates are provided at no cost to approved institutions, which only bear the cost of shipping, thereby reducing barriers to engagement in AMR research [48].
The PTAST Proficiency Testing Program
The PTAST program is an external quality assurance system designed to help laboratories, particularly those involved in national AMR surveillance in Asia, consistently produce reliable AST results [47]. Key offerings include:
- Targeted Test Strains: PTAST provides sets for key pathogens like Salmonella, E. coli, Campylobacter, Enterococcus, and mixed cultures for detecting ESBL-, AmpC-, or carbapenemase-producing E. coli [47].
- Structured Timeline: The program operates on an annual cycle with defined deadlines for sign-up, isolate shipment, result submission, and receipt of evaluation reports, ensuring synchronized participation and feedback [47].
Table: Example of PTAST Test Strain Components and Testing Scope
| PTAST Set Name | Test Strain Composition | Identification & AST Protocol |
|---|---|---|
| Salmonella set | 5 Salmonella & 2 non-Salmonella isolates [47] | Identify 5 Salmonella strains, determine serovars, perform AST on Salmonella only [47] |
| E. coli set | 5 E. coli & 2 non-E. coli isolates [47] | Identify 5 E. coli strains, perform AST on E. coli only [47] |
| MBac set | 5 lyophilized mixed bacterial cultures from meat [47] | Selectively isolate ESBL-, AmpC-, or carbapenemase-producing E. coli and perform AST [47] |
Experimental Design and Protocols
Workflow for Precision Verification of AST Methods
The following diagram illustrates the integrated workflow for using reference and proficiency testing isolates in a precision verification study.
Protocol 1: Precision Verification Using CDC/FDA AR Bank Isolates
This protocol leverages the well-characterized isolates from the AR Bank to assess the reproducibility and precision of a novel AST method.
1. Resource Acquisition and Reconstitution:
- Order the relevant isolate panel (e.g., carbapenem-resistant Enterobacterales panel) via the AR Isolate Bank portal [46].
- Upon receipt, reconstitute lyophilized isolates according to the provided instructions, typically using appropriate broth medium.
- Subculture onto non-selective agar plates to ensure purity and viability.
2. Preparation of Inoculum:
- Select well-isolated colonies to prepare a bacterial suspension adjusted to a 0.5 McFarland standard [25].
- Further dilute the suspension to the target inoculum concentration as required by the reference method (e.g., ~5 x 10^5 CFU/mL for broth microdilution) [25].
3. Precision Testing Execution:
- Intra-day Precision: For a selected subset of isolates (e.g., 3-5 isolates with varying resistance mechanisms), perform replicate testing (n=3) in a single run. Test against a panel of antimicrobials relevant to the isolates' profiles.
- Inter-day Precision: Repeat the testing for the same subset of isolates over three consecutive days using fresh inoculum preparations each day.
- Include Controls: Each run must include quality control reference strains (e.g., E. coli ATCC 25922, P. aeruginosa ATCC 27853) with known MIC ranges [49].
4. Data Analysis and Interpretation:
- Calculate Essential Agreement (EA): The percentage of MIC results by the test method that are within ±1 two-fold dilution of the reference MIC provided by the AR Bank [11].
- Calculate Categorical Agreement (CA): The percentage of results interpreted with the same susceptibility category (Susceptible, Intermediate, Resistant) as the reference.
- Precision Metrics: Determine the reproducibility of MIC results across replicates. The goal is 95% or greater essential and categorical agreement for a validated method.
Protocol 2: External Assessment via Proficiency Testing (PTAST)
This protocol uses a proficiency testing program as a blinded external assessment to validate the entire AST workflow, from identification to susceptibility reporting.
1. Enrollment and Receipt:
- Sign up for the PTAST program during the registration period (e.g., by October 10 for the 2025 cycle) [47].
- Upon receipt of the test strain sets, record the condition of the shipment and the lyophilized pellets.
2. Blinded Testing Procedure:
- Reconstitute and culture the test strains as per PTAST instructions, maintaining blinding.
- Identification: Perform the required identification of the target organisms (e.g., identify 5 E. coli from a set of 7 isolates) using standard laboratory methods [47].
- Antimicrobial Susceptibility Testing: Perform AST on the correctly identified target organisms using the method under verification. Adhere strictly to the PTAST timeline for result submission.
3. Data Submission and Evaluation:
- Submit all identification and AST results through the password-protected PTAST website by the deadline (e.g., November 30) [47].
- The PTAST organizer will generate an evaluation report comparing your laboratory's results to the expected results.
- Analyze this report to identify any discrepancies in organism identification or AST interpretation, which can reveal specific weaknesses in the testing protocol.
The Scientist's Toolkit: Key Research Reagent Solutions
Table: Essential Materials for AST Precision Verification Studies
| Item/Category | Function in AST Research | Examples & Sourcing Considerations |
|---|---|---|
| Reference Isolates | Gold standard for validating new tests; provide benchmark MICs and resistance mechanisms [46] [48]. | CDC/FDA AR Isolate Bank panels; ATCC & NCTC strains. Select based on relevant resistance mechanisms. |
| Proficiency Test Isolates | External, blinded assessment of entire lab testing process, from ID to AST [47]. | PTAST sets; CAP AST surveys (e.g., QP211) [50]. Use to fulfill regulatory quality requirements. |
| Quality Control Strains | Monitor the precision and accuracy of AST procedures daily [49]. | CLSI-recommended strains (e.g., E. coli ATCC 25922). Must be used in every test run. |
| Culture Media | Supports growth of organisms for AST; consistency is critical for reproducible MIC results. | Cation-adjusted Mueller-Hinton Broth (CAMHB) is the standard for broth microdilution [25]. |
| Reference AST Methods | The benchmark method against which new or rapid tests are compared [11] [25]. | Broth microdilution (BMD) per CLSI M07 or ISO 20776-1 [25]. |
Critical Considerations for AST Research
Navigating Breakpoint Updates and Regulatory Hurdles
A significant challenge in AST research and implementation is the timely adoption of updated clinical breakpoints. Using obsolete breakpoints can lead to misinterpretation of MIC data and inappropriate treatment, posing a direct risk to patient care [49]. Researchers and laboratories must:
- Proactively Monitor Updates: Regularly check for breakpoint updates from standards organizations like CLSI and EUCAST [49].
- Engage with Manufacturers: Determine if commercial AST systems have received FDA clearance for updated breakpoints. Implementing non-cleared breakpoints requires a more extensive in-house validation [49].
- Follow a Structured Update Plan: Prioritize updates for critical drug-bug combinations (e.g., carbapenems for Enterobacterales) and perform rigorous verification/validation studies as outlined in resources like the breakpoint implementation toolkit developed by CLSI, CDC, APHL, ASM, and CAP [49].
Sourcing and Logistics Management
Effective planning is required to overcome practical sourcing challenges:
- Lead Times: Account for order processing and shipping times when planning experiments. The AR Isolate Bank and PTAST operate on specific schedules [46] [47].
- Customs and Import Regulations: For international shipments, participating laboratories are responsible for any applicable taxes or custom fees, which should be factored into the project budget [47].
- Storage and Stability: Ensure appropriate storage conditions (e.g., -80°C or lyophilized) upon receipt to maintain isolate integrity for future use.
Antimicrobial resistance (AMR) represents a formidable threat to global health, demanding the urgent evolution of diagnostic methods and therapeutic strategies [51]. Within clinical microbiology laboratories, the introduction of new antimicrobial drugs and automated susceptibility testing instruments is a critical component of this response. However, the verification process required before implementing these new tools can be a significant bottleneck, potentially delaying patient access to life-saving treatments [7]. Verification ensures that a system functions correctly within a specific laboratory environment, confirming that personnel can produce accurate and reproducible results according to the manufacturer's specifications [1]. This document outlines streamlined, standardized strategies for verifying new antimicrobial agents on existing instruments and for implementing new AST systems, providing a practical framework that maintains rigorous standards while enhancing feasibility for busy clinical laboratories.
Verification Framework and Regulatory Context
Distinguishing Verification from Validation
A fundamental step in simplifying processes is understanding key terminology. In the context of laboratory testing and medical devices:
- Verification confirms through examination and objective evidence that specified requirements have been fulfilled. For AST, it asks, "Does the new test or instrument perform accurately and reproducibly in our laboratory environment as the manufacturer claims?" [1] [52]. This is a laboratory's responsibility.
- Validation confirms through examination and objective evidence that the particular requirements for a specific intended use can be consistently fulfilled. It asks, "Did the manufacturer design the right device?" and is performed by the manufacturer to seek regulatory clearance [1] [52].
For laboratories, verification is required by various guidelines, including the ISO 15189 standard, EUCAST recommendations, and CLIA regulations, whenever a new AST system is introduced or a significant change like a new drug is added to an existing system [1] [7].
Streamlined Verification Approaches
The CLSI guideline M52 offers a practical framework for verification, categorizing the process based on the type of change being implemented [1] [7]. This allows laboratories to tailor the effort to the complexity of the change, preventing unnecessary workload.
Table 1: Verification Requirements Based on Type of Change
| Type of Change | Accuracy Testing (Minimum Isolates) | Reproducibility Testing | Typical Scenario |
|---|---|---|---|
| Comprehensive Verification | 30 isolates | 5 isolates tested in triplicate | New AST system or change in testing method [1]. |
| Limited Verification | 10 isolates | QC strains tested over 3-5 days | New antimicrobial agent added to an existing, verified system [1]. |
| Limited Verification | 30 isolates | QC strains tested once daily for 5 days | New dilutions added for an MIC test (e.g., breakpoint change) [1]. |
Experimental Protocols for Simplified Verification
Protocol 1: Verification of a New Antimicrobial Agent on an Existing AST System
This protocol applies when a laboratory adds a new drug to a panel on an instrument already in use and verified.
Objective: To verify the performance of a new antimicrobial agent on an existing FDA-cleared/CE-marked AST system with limited verification.
Materials and Reagents:
- AST System: The existing, verified instrument and its consumables.
- New Antimicrobial: The specific drug panel or cartridge containing the new agent.
- Bacterial Isolates: A minimum of 10 well-characterized clinical isolates. These should include strains with known resistance mechanisms relevant to the new drug and a range of MICs (from susceptible to resistant) [1] [7].
- QC Strains: Appropriate quality control strains as specified by the manufacturer or CLSI guidelines for the new drug.
- Reference Method: Materials for a reference method such as broth microdilution or an existing, verified AST system to serve as a comparator [1].
Methodology:
- Strain Selection: Select a minimum of 10 clinical isolates. Ideally, obtain strains from recognized banks like the CDC-FDA Antimicrobial Resistance Isolate Bank to ensure characterization and availability [1].
- Parallel Testing: Test each of the 10 isolates simultaneously with the new AST system (test method) and the reference method.
- QC Testing: Perform quality control testing for the new antimicrobial agent using designated QC strains. CLSI M52 suggests testing these strains in replicates over 3 to 5 days to establish precision [1].
- Data Analysis: Compare the results from the test method against the reference method.
- Calculate Categorical Agreement (CA): The percentage of isolates where the interpretation (S, I, R) is identical between methods.
- Calculate Essential Agreement (EA): The percentage of isolates where the MIC result from the test method is within ±1 doubling dilution of the reference MIC.
- Error Discrepancies: Identify and quantify errors.
- Very Major Error (VME): The test method calls an isolate "Susceptible" when the reference method calls it "Resistant."
- Major Error (ME): The test method calls an isolate "Resistant" when the reference method calls it "Susceptible."
Acceptance Criteria: Verification is successful if [1]:
- CA ≥ 90% for the tested isolates.
- < 3% combined rate of VME and ME.
- QC results are within control limits for all testing days.
Protocol 2: Comprehensive Verification of a New AST Instrument
This protocol is for laboratories introducing a completely new AST system.
Objective: To comprehensively verify the accuracy and precision of a new AST instrument before implementation for patient testing.
Materials and Reagents:
- New AST Instrument: The complete system, including hardware and software.
- Test Kits/Panels: All associated consumables.
- Bacterial Isolates: A minimum of 30 clinical isolates, representing species and resistance profiles relevant to the laboratory's patient population [1].
- QC Strains: A set of QC strains for all antimicrobials on the panel.
- Reference Method: Materials for a validated reference method (e.g., broth microdilution) or a previously verified AST system [1].
Methodology:
- Strain Selection: Curate a collection of at least 30 clinical isolates that challenge the system with relevant resistance mechanisms (e.g., ESBLs, carbapenemases) [1].
- Accuracy Testing: Test all 30 isolates in parallel on the new system and the reference method.
- Precision (Reproducibility) Testing:
- Select 5 bacterial isolates (can be clinical or QC strains).
- Test each isolate in triplicate on the same run or over three different days to assess reproducibility of MICs and categorical interpretations [1].
- Data Analysis: For the 30-isolate set, calculate CA, EA, VME, and ME as described in Protocol 1. For precision, calculate the percentage of results that are reproducible.
Acceptance Criteria: Verification is successful if [1]:
- CA ≥ 90% and EA ≥ 90%.
- < 3% combined rate of VME and ME.
- Precision ≥ 95% for the reproducibility testing.
Workflow Visualization
The following diagram illustrates the decision-making pathway and key steps for verifying new drugs and instruments, as outlined in the protocols.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful verification relies on access to well-characterized biological materials and standardized reagents. The following table details key resources for executing the verification protocols.
Table 2: Essential Reagents and Resources for AST Verification
| Reagent/Resource | Function in Verification | Examples/Sources |
|---|---|---|
| Characterized Clinical Isolates | Serves as test samples for accuracy testing; must include strains with relevant resistance mechanisms to challenge the system. | CDC-FDA Antimicrobial Resistance (AR) Isolate Bank; EUCAST strain panels; internal lab biobanks [1]. |
| Quality Control (QC) Strains | Used to monitor the precision and day-to-day reproducibility of the AST system. | ATCC strains (e.g., E. coli ATCC 25922, P. aeruginosa ATCC 27853) as specified by CLSI and the manufacturer [1]. |
| Reference Method Materials | Provides the comparator "gold standard" against which the new test method is evaluated. | Broth microdilution panels, agar dilution materials, or a previously verified and validated AST system [1]. |
| Commercial AST Panels/Disks | The test method subject to verification; contains the antimicrobial agents being evaluated. | FDA-cleared/CE-marked panels for automated systems, gradient diffusion strips, or antibiotic disks for diffusion testing [1] [7]. |
Verification of new drugs and instruments need not be an insurmountable barrier to implementing advanced AST capabilities. By adopting a risk-based, targeted approach that distinguishes between comprehensive and limited verification, laboratories can streamline the process significantly. The strategies and protocols detailed herein provide a clear, actionable path for researchers and laboratory professionals to ensure the accuracy and reliability of their AST systems efficiently. This, in turn, accelerates the delivery of critical susceptibility data to clinicians, directly supporting antimicrobial stewardship and improving patient outcomes in the ongoing fight against antimicrobial resistance [51] [7].
Precision verification in antimicrobial susceptibility testing (AST) represents a systematic framework for ensuring the ongoing reliability, accuracy, and reproducibility of test results critical for patient care and antimicrobial resistance surveillance. This process integrates two complementary components: daily quality control (QC) procedures that monitor routine performance, and long-term verification studies that comprehensively validate system accuracy at implementation and after significant changes. Within research and drug development, rigorous precision verification provides the essential foundation for generating reliable susceptibility data, evaluating novel antimicrobial agents, and monitoring resistance patterns accurately [37] [53].
The Clinical Laboratory Improvement Amendment (CLIA) regulations mandate that laboratories verify the performance of diagnostic tests before clinical implementation, with specific considerations for FDA-cleared systems versus modified or laboratory-developed tests [53]. For AST systems, verification confirms that the method achieves performance specifications comparable to manufacturer claims and reference standards, ensuring categorical agreement and minimal errors in susceptibility categorization [1]. This integrated approach to quality management is particularly crucial in an era of escalating antimicrobial resistance, where inaccurate susceptibility data can directly impact treatment efficacy and contribute to the selective pressure driving resistance development [37].
Fundamental Principles of AST Quality Management
Key Definitions and Distinctions
- Verification: A one-time process conducted when implementing a new method, test, or breakpoint to confirm it performs according to specified requirements in the local laboratory environment [1] [53]. This establishes baseline performance before patient testing.
- Validation: An ongoing process evaluating test performance over time through quality control, proficiency testing, and competency assessments [53]. This ensures sustained reliability during routine operation.
- Quality Control (QC): Daily monitoring procedures using standardized reference strains to verify that test components and processes function within established parameters [54].
- Precision: The reproducibility of results, measured through repeated testing of the same isolates, with acceptance criteria of ≥95% agreement for AST systems [1].
- Accuracy: The correctness of results compared to a reference method, measured through categorical agreement (CA) and essential agreement (EA), with acceptance criteria of ≥90% agreement and <3% major errors [1].
Regulatory and Standards Framework
Multiple regulatory frameworks and standards govern AST verification and quality control, including CLIA regulations, ISO 15189 standards for medical laboratories, and guidelines from recognized standards organizations such as the Clinical and Laboratory Standards Institute (CLSI) and the European Committee on Antimicrobial Susceptibility Testing (EUCAST) [1] [2]. The FDA recognizes CLSI standards for susceptibility test interpretive criteria, creating a regulatory foundation for AST performance standards [55]. These frameworks collectively emphasize that ultimate responsibility for test performance rests with the laboratory director, who must establish appropriate verification protocols and acceptance criteria [53].
Daily Quality Control Testing Protocols
QC Strains and Materials
Daily quality control requires specific reference strains with defined susceptibility profiles to monitor AST system performance. EUCAST and CLSI provide detailed recommendations for QC strains covering aerobic, anaerobic, and fastidious bacteria [54]. These strains are available from culture collections such as the American Type Culture Collection (ATCC) and through proficiency testing programs. Essential materials include:
- QC reference strains with established MIC ranges and zone diameters [54]
- Standardized culture media meeting quality specifications (e.g., Mueller-Hinton agar and broth) [54]
- Quality-controlled antibiotic disks and dilution panels [54]
- Standardized inoculum preparation systems (e.g., 0.5 McFarland standard) [54]
Daily QC Testing Procedures
Daily QC procedures vary by testing methodology but share common principles of standardization and documentation:
- Disk Diffusion QC: Test appropriate QC strains following standardized inoculation, disk application, and incubation procedures. Measure zone diameters after 16-20 hours of incubation and compare to established QC ranges [54].
- Broth Microdilution QC: Prepare standardized inoculum from QC strains, inoculate wells of microdilution panels containing antibiotics at serial dilutions, incubate, and determine MIC values. Compare results to established QC ranges [37].
- Automated System QC: Follow manufacturer instructions for system-specific QC procedures, typically involving testing of designated QC strains with each batch of patient isolates or according to a defined schedule [1].
All QC results must be documented, with out-of-range triggers prompting investigation and corrective action before patient testing proceeds.
Rapid AST (RAST) Directly from Positive Blood Cultures
EUCAST has developed and validated a rapid AST method directly from positive blood culture bottles, providing susceptibility results within 4-8 hours for critical bloodstream infections. This method requires specific quality control criteria and designated breakpoints different from conventional AST [56]. The RAST method involves direct inoculation of Mueller-Hinton agar plates from positive blood cultures, immediate application of antibiotic disks, and reading of inhibition zones after abbreviated incubation periods of 4, 6, 8, or 16-20 hours [56]. Implementation requires strict adherence to the EUCAST RAST methodology and quality control criteria to ensure reliable results.
Long-Term Verification Methodologies
Verification Study Design
Comprehensive verification studies are required when implementing new AST systems, testing methods, or significant changes such as revised breakpoints [1] [53]. The verification study design must address several key components:
- Reference Method Selection: Choose an appropriate reference method such as CLSI or EUCAST disk diffusion, broth microdilution, or a previously verified AST system [1].
- Isolate Selection: Test a minimum of 30 bacterial isolates for comprehensive verification, including clinical strains with relevant resistance mechanisms and appropriate QC strains [1].
- Antimicrobial Agents: Include all antibiotics routinely tested in the laboratory, ensuring adequate representation of different drug classes [1].
- Data Analysis: Compare results between the new and reference methods, calculating categorical agreement, essential agreement, and error rates [1].
Acceptance Criteria for Verification
AST system verification requires meeting predefined performance targets for accuracy and precision:
Table 1: Acceptance Criteria for AST System Verification
| Parameter | Definition | Acceptance Criteria |
|---|---|---|
| Categorical Agreement (CA) | Percentage of isolates with consistent susceptibility categorization (S, I, R) between methods | ≥90% agreement |
| Essential Agreement (EA) | Percentage of MIC results within ±1 doubling dilution of reference method | ≥90% agreement |
| Very Major Error (VME) | Resistant by reference method but susceptible by new method | <3% |
| Major Error (ME) | Susceptible by reference method but resistant by new method | <3% |
| Precision | Reproducibility of results when testing the same isolate repeatedly | ≥95% agreement |
Isolate Selection for Comprehensive Verification
Verification studies should include clinically relevant isolates representing the laboratory's patient population and containing relevant resistance mechanisms. Recommended sources include:
- Clinical isolates with defined resistance mechanisms (e.g., ESBL producers, carbapenem-resistant Enterobacterales, MRSA, VRE) [1]
- Proficiency testing isolates with well-characterized susceptibility profiles [1]
- CDC-FDA Antimicrobial Resistance Isolate Bank strains for specific resistance mechanisms [1]
- EUCAST panels of phenotypically defined strains [1]
The isolate selection should challenge the system's ability to detect important resistance mechanisms while representing the spectrum of organisms routinely encountered in the laboratory.
Integrated QC Workflow and Verification Strategy
The relationship between daily QC testing and long-term verification represents a comprehensive quality management system for AST. The following diagram illustrates this integrated workflow:
Diagram 1: Integrated QC and Verification Workflow
This integrated approach ensures continuous monitoring through daily QC while providing structured verification at critical implementation points, creating a robust system for maintaining AST precision and accuracy.
Research Reagent Solutions for Precision Verification
Table 2: Essential Research Reagents for AST Verification
| Reagent Category | Specific Examples | Function in Verification |
|---|---|---|
| QC Reference Strains | E. coli ATCC 25922, P. aeruginosa ATCC 27853, S. aureus ATCC 29213 | Daily monitoring of AST system performance, establishing baseline accuracy [54] |
| Characterized Clinical Isolates | CDC-FDA AR Bank isolates, EUCAST defined strains, proficiency testing isolates | Comprehensive verification including relevant resistance mechanisms [1] |
| Standardized Culture Media | Mueller-Hinton agar and broth from qualified manufacturers | Ensuring consistent growth characteristics and antibiotic diffusion [54] |
| Antimicrobial Agents | Quality-controlled antibiotic disks, gradient strips, microdilution panels | Providing consistent antibiotic potency for reliable susceptibility testing [54] |
| Standardized Inoculum Systems | 0.5 McFarland standards, turbidity meters, colony suspension systems | Ensuring appropriate inoculum density for reproducible results [54] |
Advanced Considerations for Research Applications
Next-Generation Rapid Phenotypic AST Technologies
The field of AST is evolving with over 90 rapid phenotypic technologies in development, promising significantly faster time-to-results compared to conventional methods [11]. These technologies employ various innovative approaches including:
- Microfluidics and single-cell analysis reducing incubation time by detecting early growth response
- Morphological changes detection through microscopic imaging and analysis
- Hypothesis-free nucleic acid-based methods quantifying bacterial load without predefined targets
- Biosensor technologies detecting metabolic changes or physical properties [11]
Implementation of these novel technologies requires extensive verification against reference methods, with particular attention to their ability to detect resistant subpopulations and various resistance mechanisms.
Breakpoint Updates and Verification Requirements
Antimicrobial breakpoints are periodically revised based on evolving resistance patterns, pharmacokinetic/pharmacodynamic data, and clinical outcome correlations. Recent examples include revised aminoglycoside breakpoints for Enterobacterales and Pseudomonas aeruginosa in CLSI M100 33rd Edition [57]. Implementing revised breakpoints requires verification studies to ensure accurate categorization, particularly when applying updated breakpoints to FDA-cleared systems that may still contain previous breakpoints in their software [53]. This process involves testing a panel of characterized isolates to confirm categorical agreement with the new breakpoints before clinical implementation.
Troubleshooting and Error Resolution
When verification studies or daily QC results fail to meet acceptance criteria, systematic troubleshooting is required. Potential causes include:
- Technical errors in inoculum preparation, incubation conditions, or result reading
- Reagent problems with expired, improperly stored, or poor-quality materials
- System limitations in detecting specific resistance mechanisms
- Methodological discordance between different testing approaches [53]
Resolution may involve retesting, verifying technical procedures, consulting manufacturer recommendations, or modifying testing algorithms for problematic organism-drug combinations.
Integrating daily quality control testing with systematic long-term verification creates a robust framework for ensuring precision in antimicrobial susceptibility testing. This comprehensive approach provides the foundation for reliable AST results essential for clinical decision-making, antimicrobial stewardship, and resistance surveillance. As AST technologies evolve toward more rapid methodologies and breakpoints are updated to reflect contemporary resistance patterns, this integrated quality management system becomes increasingly critical for maintaining test accuracy and reproducibility. For research and drug development applications, rigorous precision verification supports the generation of valid susceptibility data for evaluating novel antimicrobial agents and monitoring resistance trends, ultimately contributing to the global effort against antimicrobial resistance.
Workflow Optimization for Laboratories Without 24/7 Operation
The precision verification of antimicrobial susceptibility testing (AST) systems is a critical quality process in clinical microbiology, required when introducing new methods or analytes into the laboratory [1]. For laboratories operating without 24/7 staffing, workflow optimization presents unique challenges in maintaining compliance with standards such as CLSI M52 and ISO 15189 while delivering timely results that impact patient care [1] [58]. This application note details optimized protocols and strategies that enable non-continuous laboratories to implement rigorous AST verification and testing while significantly reducing turnaround time (TAT) through strategic workflow redesign, automation, and informed prioritization.
Research demonstrates that delays in laboratory results can extend emergency department stays by 61% and delay treatment by 43% [58]. Each hourly delay in appropriate antibiotic therapy for sepsis significantly increases mortality odds [59]. These findings underscore the critical importance of optimized workflows in laboratories with limited operating hours.
Workflow Analysis and Optimization Strategies
Turnaround Time Components
Laboratory TAT is calculated from sample receipt to final report issuance and can be divided into three distinct phases [58]:
- Pre-analytical phase: Sample collection, labeling, transportation, and preparation
- Analytical phase: Core testing procedures including incubation and reading
- Post-analytical phase: Result validation, report generation, and communication to clinicians
For AST verification and testing, the analytical phase typically represents the most time-intensive component, particularly for conventional methods requiring 16-24 hours of incubation [60].
Strategic Workflow Optimization
Quantitative Impact of Workflow Optimization
Table 1: Turnaround Time Comparison Between Conventional and Optimized AST Workflows
| Workflow Component | Conventional AST | Optimized Workflow | Time Reduction | Implementation Requirements |
|---|---|---|---|---|
| Blood culture to AST result | 22-45 hours [60] | 10-11.5 hours [60] | 50-75% | Rapid AST system (e.g., QuickMIC) |
| Analytical phase (time-to-result) | 9-19 hours [60] | 3-4 hours [60] | 60-80% | Microfluidics-based AST |
| Total diagnostic process | 95.99 hours [61] | 60.81 hours [61] | 37% | Full automation integration |
| Gram-negative bacteremia TAT | Not specified | 44.87 hours [61] | >50% | Automated workflow systems |
| Gram-positive bacteremia TAT | Not specified | 27.24 hours [61] | >50% | Automated workflow systems |
Precision Verification of AST Systems: Protocols and Methodologies
Verification Requirements for AST Systems
According to CLSI guidelines, verification of commercial AST systems must establish performance comparable to manufacturer specifications [1]. The two primary performance criteria are:
- Accuracy: Measured as categorical agreement (CA) and essential agreement (EA) with reference methods
- Precision: Reproducibility of categorical interpretations and MIC values within acceptable variation ranges [1]
Table 2: AST System Verification Requirements Based on Implementation Scenario
| Type of Change | Accuracy Testing | Precision/Reproducibility Testing | Applicable Scenarios |
|---|---|---|---|
| Comprehensive Verification | Minimum 30 isolates | 5 isolates × 3 replicates (QC strains or clinical isolates) | New system implementation; Change in testing method |
| Limited Verification | Minimum 10 isolates | QC strains 3× for 5 days or 1× daily for 20 days | New antimicrobial agent; Second identical instrument |
| Limited Verification (Breakpoint changes) | Minimum 30 isolates | QC strains 1× for 5 days | New dilutions added for MIC testing |
Reference Method Selection for AST Verification
Laboratories have three options for reference methods during AST verification [1]:
- IVD-labeled and previously verified testing method
- AST reference method: Broth microdilution or agar dilution MIC testing
- External isolates with known AST results from a verified AST system
For laboratories without 24/7 operation, strategic selection of reference methodology is essential. Option 1 provides the most streamlined approach when available, while Option 3 offers flexibility in sourcing validated materials from reference laboratories or banks such as the CDC-FDA Antimicrobial Resistance Isolate Bank [1].
Experimental Protocol: Comprehensive AST Verification
Protocol Title: Comprehensive Verification of Antimicrobial Susceptibility Testing Systems for Laboratories with Limited Operating Hours
Objective: Verify that a new AST system performs according to manufacturer specifications for accuracy and precision, optimizing workflow for non-24/7 operations.
Materials and Equipment:
- AST system to be verified
- Reference method materials (as selected from Section 3.2)
- Minimum 30 clinical isolates representing locally relevant pathogens
- Quality control strains (e.g., ATCC strains)
- Appropriate culture media and supplies
- Incubation equipment
- Laboratory information management system (LIMS) or tracking system
Procedure:
Isolate Selection and Preparation:
- Select 30 clinical isolates representing species routinely tested in the laboratory
- Include strains with relevant resistance mechanisms based on local epidemiology
- Ensure isolates cover the susceptibility range (susceptible, intermediate, resistant) for antibiotics being verified
- Maintain isolates in appropriate storage conditions until testing
Batch Processing Schedule:
- Day 1 (Morning): Inoculate 10 isolates onto both verification and reference systems
- Day 1 (Afternoon): Read and record results from Day 1 morning batch
- Day 2 (Morning): Inoculate next 10 isolates, read any remaining results from previous day
- Day 2 (Afternoon): Continue reading results, prepare third batch
- Day 3: Complete remaining isolates and consolidate data
Accuracy Testing:
- Test all isolates against the AST panel using both verification and reference methods
- Maintain strict synchronization of inoculation times between systems
- Record MIC values and categorical interpretations (S, I, R) for all organism-antibiotic combinations
- Calculate categorical agreement (CA) and essential agreement (EA)
- Acceptable performance: ≥90% agreement with <3% very major errors/major discrepancies [1]
Precision Testing:
- Select 5 isolates (clinical or QC strains) for reproducibility assessment
- Test each isolate in triplicate on different days or shifts
- Ensure different operators perform testing when possible
- Record MIC values and categorical interpretations for each replicate
- Calculate percentage agreement between replicates
- Acceptable performance: ≥95% reproducibility [1]
Data Analysis and Acceptance Criteria:
- Compile all results in standardized format
- Calculate CA, EA, very major error rates, major error rates
- Compare results to acceptance criteria (≥90% CA, <3% very major errors)
- Document any discrepancies and investigate root causes for outliers
Workflow Optimization Notes:
- Batch isolates to maximize efficient use of instrument capacity during operational hours
- Schedule reading times to coincide with peak staffing availability
- Utilize middleware systems to automate result compilation and calculation [62]
- Implement electronic tracking to monitor progress through verification protocol
Implementation Tools and Solutions
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for AST Verification and Testing
| Item | Function | Application Notes |
|---|---|---|
| QC Strains (ATCC) | Quality control verification | Use for daily QC testing and precision assessment; select strains based on antibiotics tested |
| Clinical isolates with defined resistance | Accuracy assessment | Source from CDC-FDA AR Bank [1] or other validated collections; ensures relevant resistance patterns |
| Rapid AST systems (e.g., QuickMIC) | Decreased time-to-result | Microfluidics-based systems reduce TTR to 2-4 hours [60]; ideal for batch processing |
| Automated specimen processors | Streamlined subculturing | Systems like VPlus 50 automate positive culture processing, extending processing capability [61] |
| Middleware with analytics | Data consolidation and review | Software such as MAESTRIA merges results from multiple methods for final antibiogram [62] |
| Direct-from-blood-culture protocols | Bypass subculture step | Modified automated AST or disk diffusion methods enable same-shift results without 24/7 staffing [59] |
| Standardized antibiotic panels | Consistent testing conditions | Pre-configured panels ensure reproducibility; select based on local formulary and resistance patterns |
| Barcoded specimen tracking | Pre-analytical efficiency | Reduces misidentification and streamlines workflow [58]; integrates with LIMS |
Strategic Staff Optimization
Laboratories without 24/7 operation must maximize staff efficiency through several key strategies:
- Cross-training: Increase the number of personnel capable of performing critical AST procedures to enhance scheduling flexibility [63]
- Task delegation: Utilize support staff for routine pre-analytical and post-analytical tasks, freeing specialized technologists for analytical phases [64]
- Preventative maintenance: Implement scheduled maintenance procedures to reduce instrument downtime by nearly 53% [58]
- Dynamic scheduling: Staff for mid-level workload curves rather than peaks or valleys to balance cost and delivery requirements [63]
Research indicates that scientists lose approximately 12.5 weeks annually to non-core tasks including instrument setup, inventory management, and sample preparation [64]. Strategic reallocation of these tasks through automation and delegation can recover significant capacity for core verification activities.
Implementation of the optimized workflows and verification protocols detailed in this application note enables laboratories without 24/7 operation to achieve TAT reductions of 37-75% while maintaining rigorous precision verification standards [61] [60]. The integration of rapid AST technologies with strategic workflow redesign represents a paradigm shift for non-continuous laboratories, potentially transforming same-day AST reporting from theoretical possibility to operational reality.
Critical success factors include:
- Strategic technology selection prioritizing systems with rapid time-to-result compatible with operational hours
- Batch processing protocols that maximize resource utilization during staffed periods
- Implementation of middleware and automation to extend processing capability without expanding staffing
- Rigorous but efficient verification methodologies that comply with CLSI standards while respecting resource constraints
The compelling evidence from recent studies demonstrates that workflow-optimized laboratories can achieve TAT of 10-11.5 hours from positive blood culture to actionable AST result [60], making same-shift diagnostics feasible even without 24/7 staffing. These advancements directly support antimicrobial stewardship through earlier targeted therapy, with demonstrated benefits including reduced hospital stays, faster optimal therapy achievement, and lower healthcare costs [61].
Future developments in rapid phenotypic AST technologies promise further TAT reductions while maintaining the phenotypic accuracy essential for clinical decision-making [11]. For laboratories engaged in AST method research and precision verification, the workflow optimization strategies presented herein provide a framework for maintaining methodological rigor while achieving operational efficiency compatible with limited operating hours.
Advanced Validation for Novel Technologies and Comparative Analysis
Verification of Next-Generation Rapid Phenotypic AST Platforms
The escalating global antimicrobial resistance (AMR) crisis necessitates a paradigm shift in diagnostic capabilities. Next-generation rapid phenotypic Antimicrobial Susceptibility Testing (AST) platforms are emerging to address the critical need for faster results, enabling early targeted therapy and bolstering antimicrobial stewardship (AMS) initiatives [11]. Conventional AST methods, often requiring 3-5 days from specimen collection to final result, compel reliance on empirical broad-spectrum antibiotics, fueling the cycle of resistance [5] [65].
The defining characteristic of these new technologies is their focus on significantly reducing the turnaround time (TAT) from clinical specimen collection to actionable AST results, a key parameter linked to improved patient outcomes in sepsis and other serious infections [11] [66]. This document outlines a standardized framework for the verification of these innovative platforms, providing researchers and clinical scientists with detailed protocols to rigorously assess their performance within the context of precision diagnostics.
Technology Landscape and Verification Framework
The pipeline of rapid phenotypic AST technologies is diverse, encompassing over 90 platforms identified in a recent scoping review [11]. These systems leverage a variety of technical innovations to accelerate testing, including microfluidics, single-cell imaging, volatile organic compound (VOC) detection, and fluorescent signal measurement [11] [66] [65]. To standardize evaluation, a Technology Readiness Level (TRL) framework specific to AST has been proposed, categorizing systems from early proof-of-concept (TRL 1-3) to commercially available platforms with regulatory approval (TRL 9) [11].
A critical aspect of verification involves understanding the test's starting point. As illustrated in the workflow below, technologies can work directly from positive blood cultures, from standardized bacterial suspensions, or even directly from patient blood, each with implications for TAT and verification protocol design [11] [65].
Phases of Analytical Verification
A structured, phase-based framework is essential for comprehensive verification. This framework, adapted from regulatory guidelines and recent literature, ensures systematic evaluation from initial analytical performance to clinical impact assessment [11].
Performance Comparison of Selected Platforms
Recent studies have generated quantitative performance data for several leading rapid phenotypic AST platforms. The data below summarizes key metrics from published evaluations, providing a benchmark for verification studies.
Table 1: Comparative Performance of Selected Rapid Phenotypic AST Platforms
| Platform (Reference) | Technology Principle | Average Time-to-Result | Essential Agreement (EA) | Categorical Agreement (CA) | Major Error (ME) Rate |
|---|---|---|---|---|---|
| QuickMIC [66] | Microfluidic gradient | 3 h 2 min | 83.4% (vs. BMD) | 96.7% (vs. BMD) | <1% |
| Selux DX [5] | Fluorescent signal | 5.5 h | N/R | ≥90% (most combinations) | 0.8% |
| VITEK REVEAL [67] | VOC detection | 6 h 32 min | 97.1% | 98.3% | 0.9% |
| VITEK 2-RAST [67] | Colorimetric | 13 h 51 min | 96.2% | 98.4% | 1.0% |
| EUCAST DD-RAST [67] | Disk diffusion | 8 h | N/R | 98.2% | 1.8% |
N/R = Not Reported in the cited study
Table 2: Detailed Error Profile from a Selux DX System Evaluation [5]
| Error Category | Definition | Rate in Gram-Positive Isolates | Rate in Gram-Negative Isolates | Overall Rate (n=5124 combinations) |
|---|---|---|---|---|
| Very Major Error (VME) | False susceptible | 0.6% (6/937) | 0.9% (30/3249) | 1.1% (55) |
| Major Error (ME) | False resistant | 1.1% (10/937) | 0.9% (28/3249) | 0.8% (42) |
| Minor Error (mE) | Susceptible vs. Intermediate, etc. | 1.2% (11/937) | 4.0% (130/3249) | 4.0% (203) |
Experimental Protocols for Verification
Protocol 1: Basic Performance Verification against Reference Broth Microdilution
This protocol assesses the fundamental agreement between the rapid AST system and the reference broth microdilution (BMD) method as defined by ISO 20776-1 [66] [68].
Key Research Reagent Solutions:
- Cation-adjusted Mueller-Hinton Broth (CAMHB): Standardized growth medium for BMD and preparation of inoculum [66] [68].
- Mueller-Hinton Agar (MHA) Plates: Used for subculturing and purity checks of bacterial isolates [66] [68].
- 0.5 McFarland Standard: For standardizing bacterial inoculum density to approximately 1.5 x 10^8 CFU/mL [68] [5].
- Quality Control (QC) Strains: Reference strains with known MICs (e.g., E. coli ATCC 25922, P. aeruginosa ATCC 27853, S. aureus ATCC 29213) for daily system performance monitoring [66].
- Antibiotic Stock Solutions: Prepared from USP-grade reference powders for precise BMD panel preparation [66].
Procedure:
- Isolate Preparation: Revive clinical isolates or reference strains from frozen stock by subculturing twice on MHA plates and incubating at 35±2°C for 18-24 hours [66] [68].
- Inoculum Standardization: Prepare a bacterial suspension in sterile saline or CAMHB, adjusting the turbidity to a 0.5 McFarland standard [68] [5].
- Reference BMD: Perform BMD according to ISO 20776-1. Briefly, dilute the standardized inoculum in CAMHB to a final concentration of ~5x10^5 CFU/mL in each well of a pre-prepared antibiotic panel. Incubate at 35±2°C for 16-20 hours before reading the MIC visually [66].
- Rapid AST Testing: Process the standardized inoculum according to the manufacturer's instructions for the platform under verification (e.g., QuickMIC, Selux DX). Record the MIC result and the time-to-result [66] [5].
- Data Analysis: For each organism-antibiotic combination, calculate Essential Agreement (EA, % of MICs within ±1 doubling dilution of the BMD MIC) and Categorical Agreement (CA, % of interpretations matching BMD-based interpretations using CLSI or EUCAST breakpoints) [66] [5].
Protocol 2: Direct-from-Blood-Culture Performance Verification
This protocol evaluates the performance of systems designed to inoculate directly from positive blood culture bottles, a key feature for reducing overall TAT [67] [65].
Procedure:
- Sample Collection: Collect positive blood culture bottles (e.g., BacT/Alert FA Plus) signaling growth from the automated incubation system. Record the time of positivity [66] [67].
- Gram Staining: Perform Gram staining to confirm monomicrobial growth and organism morphology [65].
- Sample Preparation: Depending on the platform, sample processing may involve:
- Direct Inoculation: For systems like VITEK REVEAL, a small volume of the positive broth is directly used [67].
- Specimen Separation: For systems like Selux DX, using a component like the Positive Blood Culture Separator to isolate bacteria from blood cells and matrix inhibitors may be required [5] [65].
- Rapid AST Testing: Load the prepared sample onto the rapid AST platform with the appropriate antibiotic panel. Initiate the test and record the start time [5] [67].
- Comparative Analysis: Compare the MICs and categorical interpretations obtained from the rapid system with the results from the laboratory's routine AST method (e.g., disk diffusion, BMD, or a validated automated system) performed from purified subcultures. Calculate CA, EA, and error rates (VME, ME, mE) [5] [67].
- Turnaround Time Calculation: Calculate the total TAT from the recorded time of blood culture positivity to the availability of the final AST result for both the rapid and routine methods [66].
Protocol 3: Reproducibility and Precision Assessment
This protocol evaluates the precision of the rapid AST system by testing the same isolate multiple times under defined conditions.
Procedure:
- Strain Selection: Select a panel of 3-5 well-characterized isolates, including QC strains and clinical isolates with resistant, susceptible, and intermediate phenotypes for key antibiotics [66] [68].
- Replicate Testing: Test each selected isolate in replicates (e.g., n=3 or n=5) in a single run (within-day precision) and over at least three different days (between-day precision) [66].
- Data Analysis: Calculate the mode MIC and the standard deviation (SD) for each set of replicates. The interexperiment variability can be expressed as the SD as a percentage of the target MIC. Compare this against the acceptable standard of ±1 log2 unit (i.e., -50% to +100% deviation from target MIC) common for BMD [66].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful verification and implementation of rapid AST platforms require specific reagents and materials. The following table details key solutions used in the featured experiments.
Table 3: Key Research Reagent Solutions for Rapid AST Verification
| Reagent/Material | Function/Description | Application Example in Protocols |
|---|---|---|
| CAMHB | Standardized liquid growth medium, cation-adjusted for optimal antibiotic activity. | Serves as diluent for BMD and preparation of inoculum for AST [66] [68]. |
| MHA Plates | Solid growth medium for isolation and purity confirmation of bacterial colonies. | Used for subculturing clinical isolates prior to creating standardized inocula [66] [68]. |
| McFarland Standards | Suspensions of latex particles used to standardize the turbidity of bacterial inocula. | Critical for achieving the correct starting inoculum concentration (~1.5 x 10^8 CFU/mL) for both reference and rapid methods [68] [5]. |
| QC Reference Strains | Bacterial strains with well-defined and stable MICs for a range of antibiotics. | Used for daily quality control to monitor the precision and accuracy of the AST system [66]. |
| Antibiotic Disks/Powders | High-purity antibiotics in disk form for diffusion methods or powders for preparing BMD panels. | Creating concentration gradients for phenotypic susceptibility determination [68]. |
| Positive Blood Culture Bottles | Signal-positive blood culture bottles (e.g., BacT/Alert, BACTEC). | Used in direct-from-blood-culture protocols to assess real-world sample performance [66] [67]. |
| Sterile Saline Solution | Isotonic solution (0.85-0.9% NaCl). | Used for making bacterial suspensions and dilutions [68]. |
Antimicrobial susceptibility testing (AST) is a cornerstone of clinical microbiology, providing essential data for selecting effective antimicrobial therapy and combating the global threat of antimicrobial resistance (AMR) [15]. The evolution of AST methodologies has progressed from conventional phenotypic techniques to sophisticated automated and molecular systems, each offering distinct advantages and limitations. This analysis provides a detailed comparison of these approaches within the context of precision verification for AST method development, addressing the critical needs of researchers and drug development professionals engaged in validating and implementing these technologies.
The pressing need for accurate and rapid AST has never been greater. AMR is projected to become the leading cause of mortality globally by 2050, resulting in over 10 million deaths annually without effective intervention [6]. This crisis is exacerbated by delays in obtaining AST results, which often lead to empirical antibiotic use that fuels further resistance [23]. Technological innovations aim to shorten the time-to-results from specimen collection while maintaining the high accuracy required for precision medicine and antimicrobial stewardship programs.
Comparative Analysis of AST Methodologies
Conventional Phenotypic Methods
Disk Diffusion (Kirby-Bauer Method) The disk diffusion method is a foundational phenotypic technique that determines susceptibility by measuring the zone of inhibition around antibiotic-impregnated disks on a Mueller-Hinton agar plate inoculated with a standardized bacterial suspension [15] [69]. The diameter of the zone correlates with the susceptibility of the microorganism and is interpreted using clinical breakpoints established by organizations such as the Clinical and Laboratory Standards Institute (CLSI) and the European Committee on Antimicrobial Susceptibility Testing (EUCAST) [15].
- Key Protocol Steps:
- Preparation of 0.5 McFarland standard bacterial inoculum from well-isolated colonies (3-5 colonies)
- Even lawn inoculation onto Mueller-Hinton agar plates
- Application of antimicrobial disks with sterile forceps
- Incubation at 35°C for 16-18 hours (standard organisms)
- Measurement of inhibition zone diameters using calibrated calipers
- Interpretation based on CLSI/EUCAST breakpoints [15]
Broth Dilution Methods Broth dilution methods, including both macro- and micro-dilution techniques, determine the Minimum Inhibitory Concentration (MIC) - the lowest antimicrobial concentration that prevents visible bacterial growth [69]. This quantitative approach provides more precise data for therapeutic decision-making.
- Key Protocol Steps:
- Preparation of twofold serial dilutions of antimicrobial agents in broth
- Standardization of inoculum to approximately 5 × 10^5 CFU/mL
- Inoculation of diluted bacterial suspension into wells containing antimicrobial dilutions
- Incubation at 35°C for 16-20 hours
- Visual or automated reading of MIC (lowest concentration showing no growth)
- Interpretation using established breakpoints [15]
Gradient Diffusion (E-test) The E-test employs a predefined stable antimicrobial gradient on a plastic strip to determine MIC directly on agar plates, combining the simplicity of disk diffusion with the quantitative output of broth dilution [69] [6].
Automated AST Systems
Automated systems represent a significant advancement in AST technology, offering streamlined workflows and reduced hands-on time. These systems typically utilize optical or fluorescence signals to monitor bacterial growth in the presence of antimicrobials, automatically calculating and interpreting MIC values [6].
Technology Principles Most automated systems employ broth microdilution principles with sophisticated detection mechanisms. Platforms such as BD Phoenix (Becton Dickinson), VITEK 2 (bioMérieux), and Sensititre (Thermo Fisher Scientific) utilize colorimetric, turbidimetric, or fluorometric methods to detect bacterial growth, with integrated software analyzing growth patterns to determine MIC values [70] [6].
Key Protocol Steps:
- Preparation of standardized inoculum from isolated colonies
- Automated or manual loading of panels/cards with bacterial suspension
- System incubation with continuous or periodic monitoring
- Automated reading and interpretation of MIC values by system software
- Review and verification of results by laboratory personnel [1]
Molecular AST Systems
Molecular AST methods detect specific genetic markers associated with antimicrobial resistance through nucleic acid amplification techniques, whole genome sequencing, or other molecular approaches [69] [6]. Unlike phenotypic methods that measure observable growth inhibition, molecular techniques identify the genetic potential for resistance.
Technology Principles These systems target specific resistance mechanisms, such as the detection of mecA gene for methicillin resistance in Staphylococcus aureus or blaKPC for carbapenem resistance in Enterobacterales [6]. Emerging hypothesis-free nucleic acid-based methods represent an advanced approach that can detect or quantify bacteria in the presence of different antimicrobial conditions without pre-defined targets [11].
Key Protocol Steps:
- Nucleic acid extraction from bacterial isolates or directly from specimens
- Amplification of target resistance genes using PCR, isothermal amplification, or other techniques
- Detection of amplification products through various detection systems
- Interpretation based on presence/absence of targeted resistance markers
- Correlation with known resistance phenotypes [11]
Comparative Performance Data
Table 1: Method Comparison - Performance Characteristics and Applications
| Parameter | Conventional Phenotypic | Automated Systems | Molecular Systems |
|---|---|---|---|
| Time to Result (after isolate) | 16-24 hours [69] | 4-8 hours [6] | 2-4 hours [6] |
| Throughput Capacity | Low to moderate | High | Moderate to high |
| Quantitative Output | MIC (broth dilution), Zone size (disk diffusion) | MIC | Qualitative or semi-quantitative |
| Key Advantages | Low cost, well-standardized, flexible | High-throughput, rapid, standardized | Fastest method, detects resistance in non-culturable organisms |
| Key Limitations | Labor-intensive, subjective interpretation | High initial cost, limited customization | Limited to known mechanisms, may not correlate with phenotype |
| Best Applications | Reference testing, low-resource settings, special organisms | Routine high-volume testing, urgent cases | Screening, outbreak investigation, when rapid results critical |
Table 2: Precision Verification Requirements for AST Systems
| Verification Parameter | Conventional Methods | Automated Systems | Molecular Systems |
|---|---|---|---|
| Accuracy (Categorical Agreement) | ≥90% vs reference method [1] | ≥90% vs reference method [1] | ≥90% vs reference method [1] |
| Essential Agreement (MIC) | ≥90% within ±1 doubling dilution [1] | ≥90% within ±1 doubling dilution [1] | Not applicable |
| Precision/Reproducibility | ≥95% agreement [1] | ≥95% agreement [1] | ≥95% agreement [1] |
| Minimum Isolates for Verification | 30 isolates per organism group [1] | 30 isolates per organism group [1] | 30 isolates per organism group [1] |
| QC Strain Requirements | ATCC strains with defined MIC ranges [15] | ATCC strains with defined MIC ranges [15] | Controls for extraction, amplification, detection |
Experimental Protocols for Precision Verification
Comprehensive Method Verification Protocol
Verification of new AST systems is mandatory under various guidelines including ISO 15189 and CLSI M52 when implementing a new testing method or instrument [1]. The following protocol outlines the comprehensive verification process for a new AST system.
Sample Preparation
- Select a minimum of 30 well-characterized bacterial isolates representing clinically relevant species and resistance mechanisms
- Include QC strains with defined MIC ranges (e.g., E. coli ATCC 25922, P. aeruginosa ATCC 27853, S. aureus ATCC 29213)
- Ensure isolates cover susceptible, intermediate, and resistant phenotypes for targeted antimicrobials
- Utilize resources such as the CDC-FDA Antimicrobial Resistance Isolate Bank for strains with characterized resistance mechanisms [1]
Accuracy Assessment
- Test all selected isolates in parallel using the new method and a validated reference method (broth microdilution or approved commercial system)
- Calculate categorical agreement (CA) - percentage of isolates with identical susceptibility category (S/I/R) between methods
- Calculate essential agreement (EA) for MIC-based methods - percentage of MICs within ±1 doubling dilution of reference method
- Acceptability criteria: ≥90% agreement for both CA and EA, with <3% very major errors (false susceptible) or major errors (false resistant) [1]
Precision/Reproducibility Assessment
- Test 5 bacterial isolates (QC strains or clinical isolates) in triplicate over 3 separate runs
- For MIC-based methods, acceptable variation is ±1 doubling dilution for bacteria
- For categorical methods, interpretation (S/I/R) should be reproducible
- Acceptability criteria: ≥95% of results reproducible [1]
Quality Control Implementation
- Perform QC testing with appropriate strains each day of patient testing or according to manufacturer recommendations
- Ensure ≥95% of QC results fall within established acceptable ranges
- Investigate and resolve any QC failures before reporting patient results [15]
Rapid AST (RAST) Protocol Modification for Resource-Limited Settings
Recent research has focused on modifying existing RAST protocols to enhance accessibility while maintaining accuracy. The following protocol modification reduces resource requirements while providing results within 4-20 hours of positive blood culture [23].
Protocol Modifications
- Delayed Species Identification: Perform identification at the final RAST time point (16-20h) rather than immediately from positive blood culture
- Pan-Species Breakpoints: Use breakpoints applicable to bacterial groups rather than specific species where possible
- Simplified Quality Control: Evaluate the necessity of sheep blood addition to blood culture bottles for QC procedures [23]
Procedure
- Inoculate 100-150 μL of positive blood culture broth onto Mueller-Hinton agar
- Spread evenly and apply appropriate antibiotic disks
- Incubate and read inhibition zones at 4, 6, 8, and 16-20 hour time points
- Perform species identification at 20h time point using MALDI-TOF or rapid phenotypic tests
- Interpret results using appropriate breakpoints based on identified organism [23]
Validation Results
- Modified protocol reduced time-to-result by ≥24 hours compared to standard AST
- High categorical agreement (>90%) maintained for key antimicrobials including gentamicin, ampicillin, meropenem, and trimethoprim-sulfamethoxazole for Gram-negative bacilli
- Suitable for implementation in settings with limited resources [23]
Workflow Visualization
Diagram 1: Comparative AST Method Workflow. This diagram illustrates the procedural timeline from specimen collection to targeted therapy, highlighting the time savings offered by automated and molecular systems compared to conventional methods.
Diagram 2: Precision Verification Framework for AST Methods. This diagram outlines the systematic approach to verifying the performance of new antimicrobial susceptibility testing systems, following CLSI M52 guidelines.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for AST Development
| Reagent/Material | Function/Application | Examples/Specifications |
|---|---|---|
| Mueller-Hinton Agar | Standardized medium for disk diffusion and agar-based AST | Must meet CLSI/EUCAST specifications for cation concentrations and pH [15] |
| Cation-Adjusted Mueller-Hinton Broth | Liquid medium for broth microdilution | Required for accurate MIC determination of certain antimicrobials [15] |
| McFarland Standards | Inoculum density standardization | 0.5 McFarland standard (∼1.5 × 10^8 CFU/mL) for AST inoculum preparation [15] |
| AST Panels/Plates | Customizable antimicrobial agent combinations | Preconfigured plates with serial dilutions (e.g., Sensititre, TREK) [1] |
| Quality Control Strains | Verification of test system performance | ATCC strains (e.g., E. coli ATCC 25922, S. aureus ATCC 29213) with established MIC ranges [15] |
| Antimicrobial Disks | Disk diffusion testing | Stable, predefined antibiotic concentrations; require proper storage (-20°C or 2-8°C) [15] |
| Reference Isolates | Method verification and validation | CDC-FDA AR Bank isolates with characterized resistance mechanisms [1] |
Emerging Technologies and Future Directions
The field of AST is rapidly evolving with several promising technologies in development. Next-generation rapid phenotypic AST technologies represent the cutting edge, with over 90 technologies currently identified in various stages of development [11]. These platforms aim to dramatically reduce the time from specimen collection to results through innovations including:
- Microfluidics and Microdroplet Technologies: These systems enable AST at the single-cell level or with minimal sample volumes, significantly reducing incubation time while maintaining phenotypic relevance [69].
- Hypothesis-Free Nucleic Acid-Based Tests: These emerging methods use genomic recognition elements to detect or quantify bacteria in the presence of different antimicrobial conditions without pre-defined targets, representing a hybrid approach between genotypic and phenotypic methods [11].
- AI-Enhanced AST: Machine learning and deep learning technologies are being applied to predict pathogen antibiotic resistance by analyzing imaging and laboratory data, providing novel auxiliary diagnostic tools for AST [6].
The technology readiness level (TRL) of these emerging systems varies considerably, with only a fraction having achieved regulatory approval (FDA clearance or CE marking) [11]. Implementation of these technologies into routine clinical practice will require extensive validation to establish performance characteristics comparable to conventional methods.
The comparative analysis of conventional, automated, and molecular AST systems reveals a complex landscape where method selection must balance speed, accuracy, cost, and technical requirements. Conventional methods remain the gold standard for reference testing, while automated systems offer efficiency advantages for high-volume laboratories. Molecular methods provide unprecedented speed but are limited by their dependence on known resistance mechanisms.
Precision verification represents a critical component in the implementation of any AST methodology, requiring rigorous assessment of accuracy, precision, and reproducibility. The protocols and frameworks presented herein provide researchers and drug development professionals with standardized approaches for validating AST systems across methodological categories. As technology continues to evolve, with emerging platforms promising further reductions in time-to-results, the principles of rigorous verification and validation will remain essential for ensuring the accuracy and reliability of antimicrobial susceptibility testing.
The landscape of antimicrobial susceptibility testing (AST) in the United States underwent a significant transformation in 2025. The U.S. Food and Drug Administration (FDA) made a pivotal decision to recognize most breakpoints published in the Clinical and Laboratory Standards Institute (CLSI) M100 35th Edition and other key standards [71]. This change, driven by the 21st Century Cures Act, represents a pragmatic solution to the challenge of updating interpretive criteria in response to evolving antimicrobial resistance [72]. For researchers and drug development professionals, this alignment between CLSI and FDA breakpoints facilitates more streamlined development of AST methods and devices, ensuring that clinical laboratories can more readily adopt updated standards that reflect current resistance patterns [71].
The 2025 Regulatory Landscape: Key Updates and Transitions
Recognition of CLSI Standards
In early 2025, the FDA formally recognized multiple CLSI standards, marking a substantial shift from the previous approach of evaluating individual breakpoints. The agency now fully recognizes the standards listed in Table 1, with any exceptions specifically noted on its website [55] [73].
Table 1: CLSI Standards Recognized by the FDA in 2025
| Standard Document | Edition | Focus Area | FDA Recognition Date |
|---|---|---|---|
| CLSI M100 [4] | 35th Edition | Performance Standards for Antimicrobial Susceptibility Testing | February 12, 2025 [73] |
| CLSI M45 [55] | 3rd Edition | Infrequently Isolated or Fastidious Bacteria | January 16, 2025 [73] |
| CLSI M24S [55] | 2nd Edition | Mycobacteria, Nocardia spp., and Other Aerobic Actinomycetes | January 16, 2025 [73] |
| CLSI M43-A [55] | 1st Edition | Human Mycoplasmas | January 16, 2025 [73] |
This "recognize-by-default" approach means that unless the FDA lists a specific exception, all breakpoints within these recognized standards are available for use in clinical laboratories and for supporting premarket submissions for AST devices [71] [74]. The FDA provides a transition period until July 4, 2027, during which declarations of conformity to the prior M100 34th Edition will still be accepted for device submissions [74].
Noteworthy Changes and Exceptions
While the FDA's broad recognition is comprehensive, some important exceptions and additions exist. These are detailed on the FDA's Antibacterial Susceptibility Test Interpretive Criteria (STIC) webpage, which is updated every six months [72] [55]. Key changes for specific drugs in 2025 included the recognition of M100 standards for amikacin and gentamicin for Enterobacterales and Pseudomonas aeruginosa, while for chloramphenicol, the M45 standard for certain bacteria was not recognized [73]. This structured approach ensures that researchers can clearly identify the few areas where CLSI and FDA criteria may still differ.
Experimental Protocols for Verification and Implementation
Adhering to recognized standards is fundamental for generating reliable AST data. The following protocols outline the key methodologies referenced in the CLSI M100 standard and the verification process for implementing updated breakpoints.
Core AST Methodologies per CLSI Standards
The validity of the breakpoints in CLSI M100 is contingent upon using the specific methodologies detailed in companion standards CLSI M02, M07, and M11 [4] [74].
Table 2: Core AST Methodologies from CLSI Standards
| Methodology | CLSI Standard | Brief Description | Primary Application |
|---|---|---|---|
| Disk Diffusion | M02 [4] | Measures zone of inhibition around antimicrobial-impregnated disks on agar surface. | Aerobic bacteria [4] |
| Broth Dilution | M07 [4] | Determines Minimal Inhibitory Concentration (MIC) via serial drug dilutions in liquid medium. | Aerobic bacteria [4] |
| Agar Dilution | M07 [4] | Determines MIC via incorporation of serial drug dilutions into agar plates. | Aerobic bacteria [4] |
| Broth/Agar Dilution | M11 [4] | Specialized dilution methods for anaerobic bacteria. | Anaerobic bacteria [4] |
Protocol: Verification of Updated Breakpoints on Commercial AST Systems
When updating an FDA-cleared AST system to use the newly recognized CLSI breakpoints, a verification study is essential. This protocol is based on guidelines from CLSI M52 [75].
Experimental Workflow
The verification process follows a structured pathway from planning to implementation, as shown in the workflow below.
Materials and Reagents
Table 3: Research Reagent Solutions for AST Verification
| Item | Function/Description | Example/Specification |
|---|---|---|
| Quality Control Strains | Verifies accuracy and precision of the AST system. | CLSI-recommended strains (e.g., E. coli ATCC 25922, S. aureus ATCC 29213) [4]. |
| Clinical Isolate Panel | Challenges the new breakpoints across a range of phenotypes. | 20-30 well-characterized isolates including susceptible, resistant, and intermediate strains [75]. |
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standard medium for broth microdilution AST. | Prepares according to CLSI M07 standard for reproducible results [4]. |
| Antimicrobial Powder | Reference material for preparing in-house dilution panels. | Obtain from reputable manufacturer with certified potency [75]. |
| AST System & Panels | Commercial FDA-cleared platform being verified. | Use current lots of antimicrobial panels; ensure proper storage [75]. |
Step-by-Step Procedure
- Study Design: Define the scope of verification, including the specific drug-bug combinations for which breakpoints are being updated.
- Isolate Selection: Assemble a panel of 20-30 bacterial isolates that encompasses the range of MICs or zone diameters for the antimicrobials in question. Include QC strains to ensure day-to-day precision [75].
- Parallel Testing: Test the entire isolate panel simultaneously using two methods:
- Reference Method: Perform broth microdilution according to CLSI M07 [4] as the gold standard.
- Test System: Perform testing using the commercial AST system according to the manufacturer's instructions.
- Incubation and Reading: Incubate all tests at 35±2°C for 16-20 hours, as per CLSI M100 guidelines. Read MICs for the reference method and record both MICs and interpretations from the test system [4].
- Data Analysis: Calculate the categorical agreement (CA), which compares the interpretive category (Susceptible, Intermediate, Resistant) between the reference and test methods. The verification is considered successful if CA is ≥90% for each drug-bug combination [75].
- Resolution of Discrepants: Any major (false Susceptible or false Resistant) or very major (false Susceptible) errors must be investigated. Repeat testing is performed to confirm results.
- Documentation: Compile a final report detailing the materials, methods, raw data, analysis, and final approval for implementation.
The Scientist's Toolkit: Essential Materials for AST Research
Successfully navigating the updated breakpoints requires specific reagents, reference materials, and controls.
Table 4: Essential Research Toolkit for AST Breakpoint Studies
| Tool Category | Specific Items | Research Application |
|---|---|---|
| Reference Standards | CLSI M100-Ed35 [4], M07 [4], M02 [4] | Provide the definitive breakpoint tables and reference method protocols for R&D. |
| Quality Control Strains | ATCC strains specified in M100 [4] | Essential for daily quality control, method verification, and troubleshooting. |
| Culture Media | Mueller-Hinton Agar and Broth (cation-adjusted) [4] | Standardized media required for reproducible disk diffusion and broth microdilution testing. |
| Reference Materials | Pure antimicrobial powders [75] | Critical for preparing in-house reference MIC panels for verification studies. |
| Data Resources | FDA STIC Website [72] [55] | The primary source for checking the most current FDA-recognized breakpoints and exceptions. |
The FDA's broad recognition of CLSI standards in 2025 represents a monumental step forward in the fight against antimicrobial resistance. For the research and development community, this alignment streamlines the pathway for validating new AST methods and devices. By adhering to the detailed protocols for verification and utilizing the essential tools outlined, scientists can confidently generate robust, reliable susceptibility data. This ensures that clinical laboratories can effectively implement current breakpoints, ultimately contributing to more precise patient treatment and improved antimicrobial stewardship.
Validation Frameworks for Laboratory-Developed Tests (LDTs) and Modifications
The escalating global antimicrobial resistance (AMR) crisis necessitates rapid and accurate diagnostic solutions. Where standardized, FDA-cleared tests are unavailable for novel or resistant pathogens, clinical laboratories must develop and validate their own Laboratory-Developed Tests (LDTs) and modifications to existing test systems [71] [76]. The U.S. Food and Drug Administration (FDA) has historically exercised enforcement discretion for most LDTs. However, a final rule issued in 2024 now phases out this policy, bringing LDTs under formal FDA regulatory oversight as medical devices [71] [77] [78]. This shift, coupled with the critical need for timely antimicrobial susceptibility testing (AST), creates an urgent need for precise and compliant validation frameworks. This document provides detailed application notes and experimental protocols for the validation of LDTs and modified AST methods, specifically framed within a research context emphasizing precision verification.
Regulatory and Standards Landscape
Navigating the evolving regulatory and standards landscape is fundamental to developing compliant LDTs.
Key Regulatory Bodies and Standards Organizations
Table 1: Key Organizations Governing LDT and AST Validation
| Organization/Agency | Primary Role in LDT/AST Validation | Key Documents/Guidance |
|---|---|---|
| U.S. Food and Drug Administration (FDA) | Regulates in vitro diagnostic devices (IVDs) and, as of 2024, LDTs. Recognizes breakpoints and standards [71] [77]. | FDA Recognized Interpretive Criteria (STIC); Final Rule on LDTs (2024) |
| Centers for Medicare & Medicaid Services (CMS) | Enforces the Clinical Laboratory Improvement Amendments (CLIA), the foundational regulation for all U.S. clinical laboratories [77]. | CLIA '88 Regulations |
| Clinical and Laboratory Standards Institute (CLSI) | Develops consensus standards and guidelines for test performance and validation, widely adopted globally [71] [7]. | CLSI M52, M07, M100, M39-A4 |
| International Organization for Standardization (ISO) | Provides international standards for quality and competence in medical laboratories [2] [77]. | ISO 15189:2022 |
Recent Major Regulatory Shifts
Two pivotal changes in 2024-2025 directly impact AST and LDT validation:
- FDA Regulation of LDTs: The FDA's final rule ends its longstanding enforcement discretion, subjecting LDTs to a phased-in risk-based regulatory framework similar to other IVDs [71] [77] [78]. This means modifications to FDA-cleared AST devices—such as updating to current CLSI breakpoints or adding a new organism-drug combination—now constitute an LDT requiring FDA compliance [71]. This change has been met with legal challenges from industry groups, highlighting its significant impact [78].
- FDA Recognition of CLSI Breakpoints: In a major advancement for January 2025, the FDA recognized numerous CLSI breakpoints that were previously unmet needs, including those for infrequently isolated or fastidious bacteria (CLSI M45), mycobacteria (M24S), and fungi (M27M44S, M38M51S) [71]. This pragmatic move provides a clearer pathway for manufacturers and laboratories to develop tests for these challenging pathogens. The FDA's STIC website now defaults to recognizing all breakpoints within specific CLSI standards unless an exception is explicitly listed [71].
Validation Framework and Experimental Protocols
A rigorous validation framework is essential to establish the accuracy, precision, and reliability of any LDT or modified AST method. The following protocols are aligned with CLSI and regulatory requirements.
Core Validation Parameters and Acceptance Criteria
All validation studies must demonstrate that the test meets predefined performance standards. The following table outlines key parameters and typical acceptance criteria for AST LDTs.
Table 2: Core Validation Parameters and Acceptance Criteria for AST LDTs
| Validation Parameter | Definition | Experimental Approach | Typical Acceptance Criteria |
|---|---|---|---|
| Accuracy | Agreement between the test result and a reference method result. | Comparison to a reference standard (e.g., CLSI broth microdilution M07) [7] [37]. | Categorical Agreement (CA) ≥ 90% [79]. |
| Precision | Closeness of agreement between repeated measurements under stipulated conditions (repeatability and reproducibility). | Testing a panel of quality control and challenge isolates in replicates across multiple days and operators [2]. | ≥ 95% essential agreement for replicate results [2]. |
| Categorical Agreement (CA) | Concordance of interpretive category (S, I, R) between the test and reference method [79]. | Direct comparison of interpreted results from a set of clinical isolates. | ≥ 90% [79]. |
| Essential Agreement (EA) | Agreement where the test MIC is within one doubling dilution of the reference MIC [79]. | Comparison of MIC values from the test and reference methods. | ≥ 90% [79]. |
| Error Rates | Very Major Error (VME): Test=S, Reference=R. Major Error (ME): Test=R, Reference=S. Minor Error (mE): Test=I, Reference=S/R (or vice versa) [79]. | Calculated from the discrepancy analysis between test and reference results. | VME < 3%; ME < 3%; mE rates determined by lab director [79]. |
Protocol 1: Verification of a New Antimicrobial Agent on an Existing AST System
This protocol fulfills CLIA requirements when adding a new drug to an already-verified commercial AST system, a common laboratory modification [7].
1. Principle To verify that a laboratory can accurately perform and interpret AST for a new antimicrobial agent on its existing, verified platform (e.g., automated broth microdilution, disk diffusion) before implementing it for patient care.
2. Scope Applicable to clinical microbiology laboratories implementing a new antimicrobial agent on an FDA-cleared AST system that has already undergone a full initial verification.
3. Responsibilities The Laboratory Director is responsible for overseeing the verification study and approving the final report. The Technical Supervisor or designee performs the testing.
4. Materials and Reagents Table 3: Research Reagent Solutions for AST Verification
| Item | Function/Explanation | Example(s) |
|---|---|---|
| Cation-adjusted Mueller-Hinton Broth (CAMHB) | Standardized growth medium for broth microdilution AST to ensure consistent cation concentrations that impact aminoglycoside and polymyxin activity [37]. | Commercially prepared powder or liquid. |
| Mueller-Hinton Agar (MHA) Plates | Standardized solid medium for disk diffusion and agar dilution AST [37] [79]. | Commercially prepared plates, 4-5 mm depth. |
| Antimicrobial Powder/Disks | The active pharmaceutical ingredient for testing. Must be obtained from a reliable source and stored appropriately [37]. | USP-grade powder for BMD; commercially prepared disks for disk diffusion. |
| Quality Control (QC) Strains | Well-characterized strains with defined MIC ranges used to monitor the precision and accuracy of daily test procedures [7] [37]. | E. coli ATCC 25922, S. aureus ATCC 29213, P. aeruginosa ATCC 27853. |
| Challenge Panel of Clinical Isolates | A collection of well-characterized clinical isolates, including susceptible and resistant strains, to challenge the test across the range of expected MICs and resistance mechanisms [7]. | Includes isolates with known resistance mechanisms (e.g., ESBL, carbapenemase-producing). |
5. Procedure
- Study Design: The verification must include a minimum of 30 unique clinical isolates for the target organism group, plus appropriate QC strains [7]. The isolate panel should encompass a range of MICs (from susceptible to resistant) and include strains with relevant resistance mechanisms.
- Testing: Test all isolates in parallel using the new method (test system with the new drug) and the reference method (CLSI broth microdilution M07) [7] [37]. All testing must adhere to standardized inoculum preparation (e.g., 0.5 McFarland standard) and incubation conditions [79].
- Data Collection: Record MICs for both methods or zone diameters for disk diffusion.
- Data Analysis:
- Calculate the Essential Agreement (EA) and Categorical Agreement (CA).
- Classify and calculate the rates of Very Major Errors (VME), Major Errors (ME), and Minor Errors (mE).
- Acceptance: The test is verified if performance meets the predefined acceptance criteria (e.g., CA ≥ 90%, VME < 3%, ME < 3%) [79].
The following workflow diagrams the verification process for this protocol:
Protocol 2: Validation of a Novel AST Methodology (LDT)
This protocol outlines the more extensive studies required for a completely novel AST method not based on an FDA-cleared system, such as a broth disk elution method for colistin or a novel rapid phenotypic platform [71] [79].
1. Principle To establish the performance characteristics of a novel AST method (LDT) before clinical use, ensuring it is accurate, precise, and reliable for predicting patient treatment response.
2. Scope Applicable to clinical or research laboratories developing novel AST methods, including rapid phenotypic platforms (e.g., microfluidics, morphokinetic analysis) or non-reference methods like broth disk elution [71] [79].
3. Responsibilities A multidisciplinary team including the Laboratory Director, Principal Investigator, and research/technical staff.
4. Materials and Reagents
- Novel AST Platform: The instrument or test kit being validated.
- Reference Method Materials: As described in Protocol 1.
- Extended Challenge Panel: A larger panel of >100 clinical isolates is recommended to ensure robust statistical power and coverage of diverse species and resistance mechanisms [2].
- Software for Data Analysis: If the platform includes automated interpretation.
5. Procedure
- Analytical Sensitivity/LOD: Determine the lowest concentration of bacteria the test can reliably detect. Perform serial dilutions of a standardized inoculum and test with the novel method.
- Analytical Specificity: Evaluate for cross-reactivity with genetically or morphologically similar non-target organisms.
- Precision Study: Perform repeatability (within-run) and reproducibility (between-run, between-operator, between-day) testing using a panel of at least 3 isolates (susceptible, intermediate, resistant) tested in triplicate over 5 days [2].
- Correlation/Accuracy Study: Test the extended challenge panel of isolates using both the novel LDT and the reference method. Calculate EA, CA, and error rates as in Protocol 1.
- Reportable Range: Verify the range of MICs the test can accurately report, ensuring it covers clinically relevant concentrations.
- Reference Range: Verify the defined breakpoints (S, I, R) are correctly applied by the test system's software or interpretation scheme.
The comprehensive validation of a novel LDT involves multiple parallel studies, as shown in the workflow below:
The regulatory environment for LDTs is dynamic, marked by the FDA's new rule and a concurrent, pragmatic recognition of essential CLSI standards [71] [77]. For researchers and developers, this underscores the non-negotiable requirement for robust, data-driven validation. The protocols provided here offer a foundational framework for precision verification. However, several critical considerations emerge:
First, the tension between innovation and regulation is palpable. While the new LDT rule aims to ensure test safety and efficacy, concerns persist that the associated costs and administrative burdens could stifle innovation, particularly for tests addressing rare pathogens or unmet needs in underserved populations [76]. Second, the validation process itself can be a barrier. The CLSI M52 guideline acknowledges that verification studies are burdensome, and simplified pathways—such as using curated isolate panels and streamlined statistical plans—are needed to facilitate the implementation of life-saving new antimicrobials without compromising quality [7].
The January 2025 FDA recognition of CLSI breakpoints for fastidious organisms is a monumental step forward. It provides a clear regulatory pathway for developing tests for pathogens that lack clinical trial data, enabling laboratories and manufacturers to better combat AMR [71]. Ultimately, successful navigation of this new era requires a collaborative effort between laboratories, regulatory bodies, and standards organizations. By adhering to rigorous validation frameworks and engaging with the evolving regulatory dialogue, the scientific community can ensure continued access to innovative, reliable, and precise diagnostic tools essential for winning the fight against antimicrobial resistance.
Assessing Technology Readiness Level and Clinical Validation Phases
The development and implementation of new Antimicrobial Susceptibility Testing (AST) systems require a structured pathway to transition from conceptual research to clinically validated diagnostic tools. Two complementary frameworks guide this process: Technology Readiness Level (TRL), which assesses technical maturity, and Clinical Validation Phases, which evaluate clinical performance and utility [11]. These frameworks provide developers, clinical microbiologists, and regulators with standardized approaches for assessing diagnostic technologies.
Antimicrobial resistance (AMR) represents one of the most urgent global public health threats, with AMR-associated bacteria causing approximately 929,000 deaths annually [37]. Accurate and rapid AST is fundamental to addressing this crisis by enabling appropriate antimicrobial therapy and supporting antimicrobial stewardship programs. The slow translation of novel AST technologies from research concepts to routine clinical practice underscores the critical importance of robust assessment frameworks [11] [80].
This application note provides detailed methodologies for assessing TRL and clinical validation phases specifically for AST technologies, including experimental protocols, reagent solutions, and visualization tools to support researchers, scientists, and drug development professionals in the field of precision verification for AST methods research.
Technology Readiness Level (TRL) Assessment for AST
AST-Specific TRL Framework
The TRL framework, adapted from aerospace and defense sectors, provides a systematic approach to benchmark the maturity of AST technologies throughout the development pipeline. For AST applications, this framework has been specifically tailored to address the unique requirements of microbiological diagnostics [11].
Table 1: Technology Readiness Levels for Antimicrobial Susceptibility Testing
| TRL | Stage Description | Key Milestones and Activities |
|---|---|---|
| TRL 1-2 | Basic principles observed and formulated | Initial concept describing application of basic principles for AST |
| TRL 3 | Experimental proof-of-concept | Active research and development with laboratory studies |
| TRL 4-5 | Technology validation in laboratory environment | Component/subsystem validation in simulated or representative environment |
| TRL 6 | Technology demonstrated in relevant environment | System/subsystem model or prototype demonstration in simulated clinical setting |
| TRL 7 | System prototype demonstration in clinical environment | System prototype demonstration in clinical environment with defined study protocols |
| TRL 8 | System complete and qualified through clinical validation | Actual system completed and qualified through clinical validation and implementation |
| TRL 9 | Actual system proven in clinical routine | Actual system proven in clinical routine through successful continuous operation |
The TRL framework enables objective assessment of where a technology stands in the development pathway, from basic research (TRL 1-3) to clinical implementation (TRL 7-9) [11]. For regulatory purposes, technologies must typically reach at least TRL 3 to be considered for further development funding, while CE marking requires progression to TRL 8 [81] [82].
TRL Assessment Protocol
Protocol 1: TRL Assessment for AST Technologies
Objective: To determine the Technology Readiness Level of a novel AST system using standardized evaluation criteria.
Materials:
- Technology description and specifications
- Laboratory facilities appropriate for technology development stage
- Bacterial reference strains with characterized antimicrobial susceptibility profiles
- Documentation system for development milestones
Procedure:
- Technology Characterization: Document the fundamental principles underlying the AST technology, including mechanism of action, detection methodology, and theoretical basis for determining antimicrobial susceptibility.
- Component Validation: For each major system component (detection, fluidics, temperature control, data analysis), demonstrate functionality in controlled laboratory conditions using reference materials.
- Analytical Performance Assessment: Determine analytical sensitivity, specificity, and limit of detection using characterized bacterial strains with defined antimicrobial resistance profiles.
- Integrated System Testing: Operate the complete technology prototype with clinical sample matrices (e.g., spiked blood, urine) to assess system integration and reliability.
- Environmental Testing: Evaluate technology performance under expected operational conditions (temperature variations, humidity, vibration) to assess robustness.
- Documentation Review: Compile evidence including engineering designs, performance specifications, validation data, and failure mode analyses.
Acceptance Criteria: Technology advances to next TRL when all key milestones for current level are successfully demonstrated and documented.
Clinical Validation Phases for AST Systems
Clinical Validation Framework
While TRL assesses technical maturity, clinical validation phases evaluate performance in increasingly clinically relevant settings. We have developed a comprehensive framework specifically for AST diagnostic studies that builds upon previous work for general diagnostics [11].
Table 2: Clinical Validation Phases for Antimicrobial Susceptibility Testing Systems
| Phase | Study Type | Primary Objectives | Typical Sample Size |
|---|---|---|---|
| Phase 0 | Analytical validity | Establish test reproducibility, repeatability, limit of detection | 20-50 isolates |
| Phase I | Retrospective repository specimens | Initial assessment of clinical performance against reference standard | 50-100 isolates |
| Phase II | Prospective single-site study | Define clinical sensitivity and specificity in controlled setting | 100-300 isolates |
| Phase III | Prospective multi-site study | Confirm performance across multiple sites and populations | 300-1000 isolates |
| Phase IV | Clinical impact and implementation | Assess effect on patient outcomes and antimicrobial stewardship | Variable, based on endpoints |
This framework enables standardized comparison across diverse AST technologies and provides a structured pathway for clinical translation [11]. The European Health and Digital Executive Agency (HaDEA) has emphasized the importance of progressive clinical validation in recent calls for developing rapid point-of-care AST devices [82].
Clinical Validation Protocols
Protocol 2: Phase I-II Clinical Validation for AST Systems
Objective: To assess the clinical performance of a novel AST system against reference methods in retrospective and prospective clinical specimens.
Materials:
- AST system prototype
- Reference AST method (broth microdilution, disk diffusion, or validated commercial system)
- Clinical bacterial isolates with relevant resistance mechanisms
- Quality control strains (e.g., ATCC strains)
- Culture media and reagents
- Data collection forms
Procedure:
- Study Design: Define inclusion/exclusion criteria for bacterial isolates, ensuring representation of clinically relevant species and resistance mechanisms.
- Sample Size Calculation: Determine appropriate sample size based on expected performance characteristics and statistical requirements.
- Isolate Collection: Procure well-characterized clinical isolates from repository or clinical laboratory, ensuring appropriate distribution of susceptible and resistant phenotypes.
- Testing Protocol: Perform parallel testing with novel AST system and reference method following standardized procedures.
- Data Analysis: Calculate categorical agreement (CA), essential agreement (EA), major errors (ME), and very major errors (VME) according to established guidelines [1].
- Statistical Analysis: Determine sensitivity, specificity, positive predictive value, and negative predictive value with 95% confidence intervals.
Acceptance Criteria: For AST systems, performance standards typically require ≥90% categorical agreement with reference methods, with very major error rates <3% and major error rates <3% [1].
Protocol 3: Phase III-IV Clinical Validation for AST Systems
Objective: To evaluate AST system performance in multi-center settings and assess impact on clinical outcomes and antimicrobial stewardship.
Materials:
- Validated AST systems
- Multiple clinical laboratory sites
- Patient outcome tracking system
- Antimicrobial stewardship team
- Data management and statistical analysis resources
Procedure:
- Site Selection: Identify multiple clinical laboratories representing different settings (academic, community, regional).
- Training and Standardization: Train personnel at all sites on standardized operating procedures for the AST system.
- Prospective Testing: Implement the AST system in routine workflow at participating sites with consecutive clinical isolates meeting inclusion criteria.
- Reference Testing: Perform parallel testing with reference method according to CLSI or EUCAST guidelines.
- Turnaround Time Assessment: Document time from specimen receipt to result availability for both systems.
- Clinical Impact Assessment: Evaluate effect on time to appropriate antibiotic therapy, antibiotic utilization patterns, and patient outcomes where feasible.
- Economic Analysis: Assess cost-effectiveness compared to standard approaches.
Acceptance Criteria: Consistent performance across sites with <5% variation in categorical agreement; demonstration of improved turnaround time; positive impact on antimicrobial stewardship metrics.
Workflow Visualization
AST TRL and Clinical Validation Pathway
Research Reagent Solutions
Table 3: Essential Research Reagents for AST Development and Validation
| Reagent/Category | Function in AST Development | Examples and Specifications |
|---|---|---|
| Reference Bacterial Strains | Quality control, method validation | ATCC strains with characterized susceptibility profiles; CDC-FDA AR Isolate Bank strains |
| Culture Media | Support bacterial growth under test conditions | Cation-adjusted Mueller-Hinton broth, Mueller-Hinton agar, blood culture media |
| Antimicrobial Agents | Prepare concentration gradients for susceptibility testing | USP reference standards, clinical formulations with known potency |
| Quality Control Organisms | Monitor assay precision and reproducibility | E. coli ATCC 25922, P. aeruginosa ATCC 27853, S. aureus ATCC 29213 |
| Clinical Isolate Panels | Assess clinical performance across resistance mechanisms | Collections with ESBL, carbapenemase, methicillin resistance; EUCAST recommended strain sets |
Advanced Applications and Future Directions
Emerging Technologies in AST
Next-generation AST technologies are incorporating innovative approaches including phenotypic methods with significantly reduced time-to-results, genotypic methods using next-generation sequencing, and personalized AST approaches informed by clinical prediction modeling [11] [83] [84]. These advancements are driving the need for updated TRL and clinical validation frameworks that can accommodate increasingly complex diagnostic systems.
Recent developments in personalized AST utilize clinical prediction modeling to adapt laboratory testing approaches based on individual patient characteristics, potentially increasing testing efficiency and promoting use of WHO Access category antibiotics [84]. Validation of these advanced systems requires novel assessment protocols that evaluate both analytical performance and clinical utility in guiding therapeutic decisions.
Regulatory Considerations
The regulatory landscape for AST systems continues to evolve, with increasing emphasis on demonstrating clinical utility alongside analytical performance. The European In Vitro Diagnostics Regulation (IVDR) and FDA requirements necessitate rigorous validation studies with appropriate clinical endpoints [83] [1]. Understanding these regulatory frameworks is essential for appropriate planning of TRL assessment and clinical validation studies.
Recent funding initiatives, such as the EU4Health call for tenders with an estimated budget of €12.86 million, highlight the strategic priority placed on developing rapid point-of-care AST devices that can provide results within one hour or less from sample collection [82]. These initiatives specifically require technologies to be at minimum TRL 3 with a clear pathway to achieving TRL 8 and regulatory certification.
Conclusion
Precision verification is not a one-time event but a cornerstone of quality in the clinical microbiology laboratory, directly impacting patient care and the global fight against antimicrobial resistance. A successful verification strategy seamlessly integrates foundational principles, a rigorous methodological approach, proactive troubleshooting, and forward-looking validation to ensure AST systems perform reliably. Future efforts must focus on standardizing verification for novel rapid technologies, harmonizing global breakpoints, and developing more accessible tools and strain banks to ease the implementation burden. By adhering to a comprehensive verification framework, researchers and laboratory professionals can ensure the delivery of accurate, timely, and actionable susceptibility data, ultimately guiding effective antimicrobial therapy and improving patient outcomes.
References
- 1. Verification of new AST testing systems [https://www.thermofisher.com/us/en/home/industrial/microbiology/microbiology-learning-center/susceptibility-testing-empowered/AST-verification.html]
- 2. How to verify and validate a clinical microbiology test ... [https://www.sciencedirect.com/science/article/pii/S1198743X24003094]
- 3. ISO 15189: Definition, Requirements, Implementation, and ... [https://simplerqms.com/iso-15189/]
- 4. M100 | Performance Standards for Antimicrobial ... [https://clsi.org/shop/standards/m100/]
- 5. Evaluation of a Novel Rapid Phenotypic Antimicrobial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562109/]
- 6. Advancements in AI-driven drug sensitivity testing research [https://pmc.ncbi.nlm.nih.gov/articles/PMC12081381/]
- 7. Expert Opinion on Verification of Antimicrobial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7587095/]
- 8. Planning a Method Verification Study in Clinical ... [https://asm.org/articles/2022/january/planning-a-method-verification-study-in-clinical-m]
- 9. Measurement System Accuracy vs. Precision: Key Differences ... [https://lean6sigmahub.com/measurement-system-accuracy-vs-precision-key-differences-explained-for-quality-improvement/]
- 10. Analytical Method Validation: Back to Basics, Part II [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-ii]
- 11. Next-generation rapid phenotypic antimicrobial ... [https://www.nature.com/articles/s41467-024-53930-x]
- 12. FDA, CLIA, and ISO—Which Regulations Apply to Your ... [https://www.clinicallab.com/fda-clia-and-iso-which-regulations-apply-to-your-clinical-lab-28044]
- 13. What is ISO 15189? A complete overview [https://www.qualio.com/blog/iso-15189]
- 14. Verification of Antimicrobial Susceptibility Testing Methods [https://www.sciencedirect.com/science/article/pii/S0196439913000251]
- 15. Antimicrobial Susceptibility Testing - StatPearls - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK539714/]
- 16. CMS Enacts New CLIA Regulations Effective January 2025 [https://www.bakerdonelson.com/cms-enacts-new-clia-regulations-effective-january-2025]
- 17. Global impact of antimicrobial stewardship programs in ... [https://www.sciencedirect.com/science/article/abs/pii/S1341321X25001503]
- 18. Antimicrobial Susceptibility Testing: A Comprehensive ... [https://www.mdpi.com/2079-6382/11/4/427]
- 19. Combat Antimicrobial Resistance Through Diagnostic ... [https://www.clinicallab.com/combat-antimicrobial-resistance-through-diagnostic-precision-28089]
- 20. Implementation and Early Outcomes of an Antimicrobial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12382939/]
- 21. Keeping Patients Safe from Escalating Antibiotic Resistance [https://www.cepheid.com/content/www-cepheid-com/en-US/insights/insight-hub/antimicrobial-stewardship/2025/10/keeping-patients-safe-from-escalating-antibiotic-resistance.html]
- 22. Paving the way for precise diagnostics of antimicrobial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9413203/]
- 23. Modification of the rapid antimicrobial susceptibility testing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12076145/]
- 24. CLSI and EUCAST Release New Guidance on ... [https://clsi.org/about/news/clsi-and-eucast-release-new-guidance-on-modifications-to-antimicrobial-susceptibility-testing-methods/]
- 25. Modification of antimicrobial susceptibility testing methods [https://pubmed.ncbi.nlm.nih.gov/40971802/]
- 26. In vitro antimicrobial susceptibility testing methods: agar ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5780537/]
- 27. Broth Microdilution and Gradient Diffusion Strips vs. ... [https://www.mdpi.com/2079-6382/10/8/975]
- 28. Comparative evaluation of agar dilution and broth ... [https://www.sciencedirect.com/science/article/abs/pii/S1075996421001268]
- 29. Evaluation of agar dilution as an alternative method for ... [https://www.nature.com/articles/s41598-025-16223-x]
- 30. Validation of Sensititre Dry-Form Broth Microdilution ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4505265/]
- 31. Comparison of Broth Microdilution, E Test, and Agar Dilution ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC150256/]
- 32. 【推荐】分子诊断技术在抗生素耐药性检测中的应用与未来 [https://www.biomart.cn/news/16/3219833.htm]
- 33. 世卫组织警告称全球普遍存在常用抗生素耐药性 [https://www.who.int/zh/news/item/13-10-2025-who-warns-of-widespread-resistance-to-common-antibiotics-worldwide]
- 34. 《依拉环素体外药物敏感性试验规范(2025)》正式发布 [https://bydrug.pharmcube.com/news/detail/16a53679ac0abb8ff7139f4ed88de2f0]
- 35. 【协和医学杂志】快速药敏检测新方法:现状与进展 [https://www.medsci.cn/article/show_article.do?id=cfbb901e06f5]
- 36. High-throughput clinical antimicrobial susceptibility testing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12211026/]
- 37. Antimicrobial Susceptibility Testing: A Comprehensive Review ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9024665/]
- 38. Contemporary Considerations for Establishing Reference ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10281161/]
- 39. Evaluation of digital dispense-assisted broth microdilution ... [https://www.nature.com/articles/s41598-021-88423-0]
- 40. Verification of new AST testing systems [https://www.selectscience.net/article/verification-of-new-ast-testing-systems]
- 41. Overview of Quantitative Methodologies to Understand ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7459578/]
- 42. Simple large-scale quantitative phenotyping and ... [https://www.nature.com/articles/s41596-025-01179-z]
- 43. Reporting antimicrobial susceptibility and detection of ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1605590/full]
- 44. Defining antimicrobial susceptibility testing methods and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12153331/]
- 45. Antimicrobial susceptibility testing of Clostridioides difficile [https://www.sciencedirect.com/science/article/pii/S1198743X25000369]
- 46. Overview | Antimicrobial Resistance Isolate Bank [https://wwwn.cdc.gov/arisolatebank/overview]
- 47. About PTAST - Proficiency Test for Antimicrobial ... [http://www.cuvetamr.vet.chula.ac.th/ptast/pt/content/pt_aboutus]
- 48. CDC and FDA Antimicrobial Resistance Isolate Bank [https://www.cdc.gov/antimicrobial-resistance/php/public-health-strategy/index.html]
- 49. Updating Breakpoints in Antimicrobial Susceptibility Testing [https://asm.org/articles/2022/february/updating-breakpoints-in-antimicrobial-susceptibili]
- 50. ANTIMICROBIAL SUSCEPTIBILITY TESTING-QP211 - CAP [https://estore.cap.org/OA_HTML/xxCAPibeCCtpItmDspRte.jsp?item=746859&sitex=10020:22372:US]
- 51. Antimicrobial Testing: Advancing Methodologies and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566307/]
- 52. Design Verification & Validation for Medical Devices [Guide] [https://www.greenlight.guru/blog/design-verification-and-design-validation]
- 53. Verification of Antimicrobial Susceptibility Testing Methods [https://www.sciencedirect.com/science/article/abs/pii/S0196439913000251]
- 54. Disk Diffusion and Quality Control [https://www.eucast.org/bacteria/methodology-and-instructions/disk-diffusion-and-quality-control/]
- 55. Antibacterial Susceptibility Test Interpretive Criteria [https://www.fda.gov/drugs/development-resources/antibacterial-susceptibility-test-interpretive-criteria]
- 56. Methods and Quality Control [https://www.eucast.org/bacteria/rapid-ast-in-blood-culture/methods-and-quality-control/]
- 57. M100 32nd and 33rd editions [https://pmc.ncbi.nlm.nih.gov/articles/PMC12421849/]
- 58. Strategies to improve Lab Turnaround Time (TAT) [https://diagnostics.roche.com/global/en/article-listing/lab-leaders/article/laboratory-turnaround-time.html]
- 59. leveraging existing antimicrobial susceptibility test methods ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11370233/]
- 60. impact on turnaround time compared to routine AST systems [https://link.springer.com/article/10.1007/s10096-025-05298-z]
- 61. reducing turnaround time and improving clinical outcomes [https://pubmed.ncbi.nlm.nih.gov/41217182/]
- 62. MAESTRIA™, a new generation microbiology middleware ... [https://www.biomerieux.com/ca/fr/press-releases/maestria---a-new-generation-microbiology-middleware-developed-by.html]
- 63. Improving Lab Scheduling to Drive Productivity and Flexibility [https://www.labmanager.com/improving-lab-scheduling-to-drive-productivity-and-flexibility-33383]
- 64. Strategies for Reducing Non-Core Tasks in the Lab [https://biopharmaboardroom.com/product-spotlight/73/2142/maximize-time-for-innovation-strategies-for-reducing-non-core-tasks-in-the-lab.html]
- 65. Making AST fast [https://myadlm.org/cln/articles/2025/mayjune/making-act-fast]
- 66. Evaluation of the Speed, Accuracy and Precision of the QuickMIC... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8984463/]
- 67. Comparison of Three Rapid AST System [https://www.rapidmicrobiology.com/journal-club/comparison-of-three-rapid-antimicrobial-susceptibility-testing-systems]
- 68. Validation of Antibiotic Susceptibility Testing Guidelines in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4068562/]
- 69. Conventional methods and future trends in antimicrobial ... [https://www.sciencedirect.com/science/article/pii/S1319562X2300027X]
- 70. Top Antimicrobial Susceptibility Testing Device Companies ... [https://www.linkedin.com/pulse/top-antimicrobial-susceptibility-testing-device-3naze/]
- 71. Major updates to FDA-recognized Clinical and Laboratory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12077184/]
- 72. Antibacterial Susceptibility Test Interpretive Criteria [https://www.fda.gov/drugs/development-resources/fda-recognized-antimicrobial-susceptibility-test-interpretive-criteria]
- 73. Notices of Updates [https://www.fda.gov/drugs/development-resources/notices-updates]
- 74. Recognized Consensus Standards: Medical Devices - FDA [https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfstandards/detail.cfm?standard__identification_no=46254]
- 75. M52 | Verification of Commercial Microbial Identification ... [https://clsi.org/shop/standards/m52/]
- 76. ASM Responds to FDA Proposed Rule on Laboratory- ... [https://asm.org/articles/policy/2023/december/asm-responds-to-fda-proposed-rule-on-laboratory-de]
- 77. Regulatory requirements for laboratory developed tests in ... [https://www.sciencedirect.com/science/article/abs/pii/S0022175925000134]
- 78. ACLA Sues the FDA Over Final Rule to Regulate ... [https://www.clinicallab.com/acla-sues-the-fda-over-final-rule-to-regulate-laboratory-developed-tests-as-medical-devices-27902]
- 79. Rapid Phenotypic and Genotypic Antimicrobial ... [https://www.mdpi.com/2079-6382/13/8/786]
- 80. Toward a Unified Technology Readiness Ladder for ... [https://www.isjtrend.com/article_226565.html]
- 81. HERA: 13m EUR call for rapid point-of-care susceptibility ... [https://amr.solutions/2025/02/19/era-13m-eur-call-for-rapid-point-of-care-susceptibility-devices/]
- 82. EU4Health call for tenders to develop point-of-care diagnostic ... [https://hadea.ec.europa.eu/news/eu4health-call-tenders-develop-point-care-diagnostic-medical-devices-antimicrobial-susceptibility-2025-03-24_en]
- 83. Next generation sequencing as a panacea for antibiotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399536/]
- 84. Personalised antimicrobial susceptibility testing with ... [https://www.nature.com/articles/s41467-024-54192-3]