Molecular Mechanisms and Therapeutic Applications of Host-Microbiome Interactions in Health and Disease
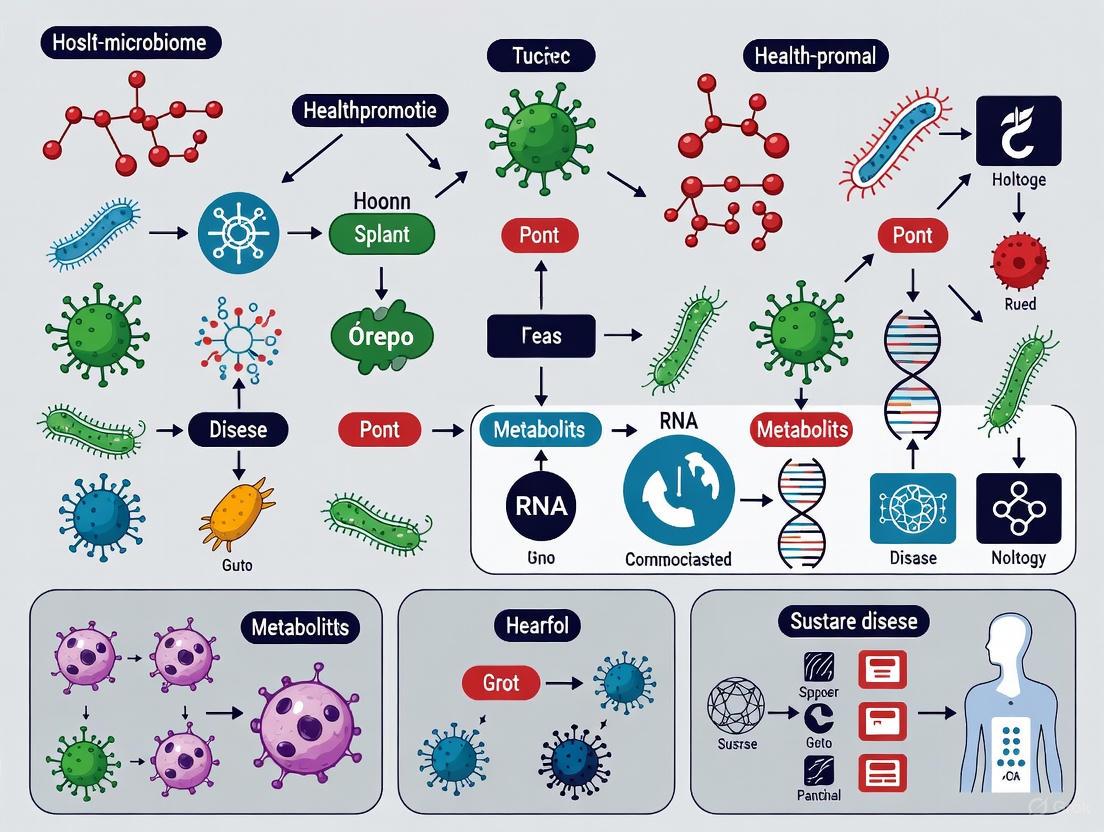
This article synthesizes current research on the intricate molecular dialogues between the host and its microbiome, exploring their profound impact on health and disease pathogenesis.
Molecular Mechanisms and Therapeutic Applications of Host-Microbiome Interactions in Health and Disease
Abstract
This article synthesizes current research on the intricate molecular dialogues between the host and its microbiome, exploring their profound impact on health and disease pathogenesis. We delve into foundational mechanisms, including immune modulation via microbial metabolites and signaling pathways, and examine the causal role of dysbiosis in conditions from inflammatory bowel disease to preterm birth. The review critically assesses advanced methodological tools—from multi-omics to physiologically relevant tissue models and gnotobiotic systems—for investigating these interactions. Furthermore, we evaluate the translational potential of microbiome-based therapeutics, such as fecal microbiota transplantation and probiotics, while addressing the challenges of establishing causality and the imperative for standardized models to bridge the gap between basic research and clinical application for precision medicine.
The Molecular Language of Host-Microbiome Symbiosis and Dysbiosis
The human microbiome, once regarded as a passive passenger, is now recognized as a dynamic and essential determinant of human physiology, shaping immunity, metabolism, and host defense across the lifespan [1]. A healthy microbiome is not defined by a universal taxonomic blueprint but rather by the core functional capabilities that promote host homeostasis. These core functions—metabolic regulation, immune education, and colonization resistance—are maintained through complex host-microbe and microbe-microbe interactions [1] [2]. Advances in multi-omic technologies and analytical frameworks have shifted the focus from "who is there" to "what are they doing," revealing mechanistic insights into how microbial communities modulate host systems [1] [3]. This technical guide synthesizes current evidence on the defining functional attributes of a healthy microbiome, providing researchers and drug development professionals with structured data, experimental protocols, and analytical frameworks for investigating host-microbiome interactions in health and disease.
Core Functional Pillars of a Healthy Microbiome
Metabolic Regulation and Nutrient Processing
A cornerstone of microbiome health is its metabolic capacity to transform dietary components into signaling molecules that regulate host physiology. The gut microbiota functions as a bioreactor, converting complex carbohydrates and other indigestible fibers into short-chain fatty acids (SCFAs) including acetate, propionate, and butyrate [1]. These metabolites serve as crucial energy sources for colonocytes and play fundamental roles in systemic metabolic regulation.
Table 1: Key Microbial Metabolites and Their Physiological Roles in Host Health
| Metabolite | Primary Producers | Physiological Functions | Association with Disease |
|---|---|---|---|
| Butyrate | Faecalibacterium prausnitzii, Roseburia spp. | Primary energy source for colonocytes, enhances gut barrier function, anti-inflammatory properties [1] | Reduced in IBD, metabolic syndrome [4] |
| Propionate | Bacteroides spp., Akkermansia muciniphila | Gluconeogenesis precursor, regulates appetite, cholesterol synthesis inhibitor | Depleted in obesity, type 2 diabetes [4] |
| Acetate | Bifidobacterium spp., Lactobacillus spp. | Cross-feeds other bacteria, systemic metabolic regulator, modulates immune function | Altered in inflammatory conditions [1] |
Beyond SCFA production, microbial metabolism influences bile acid transformation, vitamin synthesis (B vitamins, vitamin K), and the bioavailability of phytonutrients. The integration of microbial metabolic functions with host pathways creates a symbiotic relationship where the host provides substrate and the microbiota provides metabolic outcomes that the host cannot achieve alone [1]. Metabolic dysfunction, characterized by shifts in these microbial metabolic pathways, has been implicated in conditions ranging from inflammatory bowel disease (IBD) to metabolic syndrome and cancer [4].
Immunomodulation and Immune System Education
The microbiome serves as a foundational instructor for the developing and mature immune system, shaping both mucosal and systemic immunity through continuous dialogue with host immune cells [1]. From the neonatal period onward, microbial colonization is critical for proper immune maturation, with specific windows of opportunity where microbial exposure has lasting effects on immune function.
Microbial immunomodulation occurs through multiple mechanisms:
- Pattern Recognition Receptor Signaling: Microbial-associated molecular patterns (MAMPs) interact with host pattern recognition receptors (PRRs) such as Toll-like receptors (TLRs), regulating immune tone and inflammatory responses [1].
- T Cell Polarization: Specific microbial taxa influence the differentiation of naive T cells into regulatory (Treg), helper (Th1, Th2, Th17), or other effector subsets, balancing pro-inflammatory and tolerogenic responses [1].
- Cytokine and Chemokine Regulation: Microbial metabolites, including SCFAs, modulate the production of inflammatory mediators and homing molecules that recruit immune cells to mucosal sites [1].
The critical importance of early-life microbial exposure is demonstrated by studies showing that neonatal antibiotic exposure significantly impairs vaccine-induced antibody responses, an effect attributed to the depletion of beneficial Bifidobacterium species during critical windows of immune programming [1]. Similarly, breastfeeding facilitates the transfer of maternal microbes and human milk oligosaccharides (HMOs) that selectively support the growth of immunoregulatory taxa like Bifidobacterium infantis, which promotes immune homeostasis by suppressing pro-inflammatory Th2 and Th17 cytokines [1].
Colonization Resistance and Pathogen Exclusion
A healthy microbiome provides protection against pathogenic organisms through the principle of colonization resistance—the ability of resident microbial communities to limit the expansion and invasion of pathogens. This function is mediated through multiple complementary mechanisms:
- Resource Competition: Commensals compete with pathogens for nutrients and physical binding sites on the mucosal surface [1].
- Production of Antimicrobial Compounds: Beneficial bacteria produce bacteriocins, defensins, and other antimicrobial substances that directly inhibit pathogens [4].
- Environmental Modification: Microbial metabolism alters local pH, oxygen tension, and other environmental conditions to create an unfavorable niche for pathogens [1].
- Immune System Priming: By maintaining appropriate immune system tone, a healthy microbiome ensures rapid pathogen clearance upon exposure [1].
The therapeutic implications of colonization resistance are exemplified by the success of fecal microbiota transplantation (FMT) for recurrent Clostridium difficile infection, where restoration of a diverse microbial community displaces the pathogen [4]. However, research is now moving beyond traditional FMT toward precisely defined consortia of core probiotics that can reconstitute this protective function with reduced risk [4].
Methodological Framework for Microbiome Research
Diversity Metrics and Analytical Approaches
Robust assessment of microbiome health requires appropriate analytical tools that capture the ecological features of microbial communities. Alpha diversity metrics, which describe within-sample diversity, are commonly used but often misapplied without understanding their mathematical assumptions and biological interpretations [3]. These metrics can be categorized into four complementary classes, each capturing different aspects of microbial ecology:
Table 2: Categories and Applications of Alpha Diversity Metrics in Microbiome Research
| Metric Category | Key Metrics | Biological Interpretation | Technical Considerations |
|---|---|---|---|
| Richness | Chao1, ACE, Observed ASVs | Estimates total number of species/ASVs in a sample | Highly dependent on sequencing depth; Chao1 and ACE account for unobserved species [3] |
| Phylogenetic Diversity | Faith's PD | Incorporates evolutionary relationships between organisms | Depends on both number of features and singletons; requires phylogenetic tree [3] |
| Evenness/Dominance | Simpson, Berger-Parker, Gini | Measures distribution abundance across species | Berger-Parker has clear interpretation (proportion of most abundant taxon) [3] |
| Information Indices | Shannon, Pielou's | Combines richness and evenness into single value | Sensitive to both number of ASVs and their distribution [3] |
Recent guidelines recommend that microbiome analyses should include metrics from multiple categories to provide a comprehensive characterization of microbial communities [3]. For instance, while richness estimators quantify the number of taxa, dominance metrics like Berger-Parker reveal whether the community is dominated by a few taxa or exhibits balanced distribution—a feature particularly relevant in dysbiotic states where pathobionts may expand to dominate the community.
Experimental Workflows for Functional Characterization
Comprehensive functional analysis of the microbiome requires integrated multi-omic approaches that move beyond taxonomic profiling to capture the functional potential and activities of microbial communities.
Detailed Protocol for Integrated Multi-omic Analysis:
Sample Collection and Preservation:
- Collect fresh stool samples in DNA/RNA stabilizing buffer or flash-freeze in liquid nitrogen
- For metabolomics, preserve samples at -80°C with cryoprotectants
- Record comprehensive metadata including host diet, medications, and clinical parameters [3]
Nucleic Acid Extraction:
- Use mechanical lysis with bead beating to ensure disruption of tough bacterial cell walls
- Employ extraction kits validated for microbiome studies to minimize bias
- Include extraction controls to monitor for contamination [3]
Sequencing and Metabolomic Profiling:
- For 16S rRNA sequencing: Amplify V4 region using 515F/806R primers with dual-indexing approach
- For shotgun metagenomics: Sequence on Illumina platform to minimum depth of 10 million reads per sample
- For metabolomics: Use LC-MS/MS with reverse-phase chromatography for broad metabolite detection [4]
Bioinformatic Analysis:
- Process 16S data with DADA2 or DEBLUR for amplicon sequence variant (ASV) calling
- Analyze shotgun data with HUMAnN2 or MetaPhlAn for taxonomic and functional profiling
- Integrate datasets using multi-omics factor analysis (MOFA) or similar integration frameworks [3]
Research Reagent Solutions for Microbiome Science
Table 3: Essential Research Tools for Investigating Microbiome Function
| Reagent/Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| DNA Extraction Kits | MoBio PowerSoil Kit, QIAamp DNA Stool Mini Kit | Standardized microbial DNA isolation | Bead beating step critical for Gram-positive bacteria [3] |
| 16S rRNA Primers | 515F/806R (Earth Microbiome Project) | Amplification of hypervariable regions for taxonomic profiling | Covers most bacterial and archaeal diversity; minimizes host amplification [3] |
| Standards for Metabolomics | Stable isotope-labeled SCFAs, bile acids | Quantification of microbial metabolites using LC-MS/MS | Enables absolute quantification; corrects for matrix effects [4] |
| Gnotobiotic Mouse Models | Germ-free C57BL/6, Humanized microbiota mice | In vivo functional validation of microbial communities | Essential for establishing causal relationships; requires specialized facilities [1] |
| Bacterial Cultivation Media | YCFA, Gifu Anaerobic Medium, M2GSC | Cultivation of fastidious anaerobic gut bacteria | Pre-reduced media with oxygen-free atmosphere essential for strict anaerobes [4] |
| Live Biotherapeutic Products | Defined consortia (e.g., Faecalibacterium prausnitzii, Akkermansia muciniphila) | Targeted microbiome modulation for functional restoration | Addresses limitations of traditional FMT; requires optimized cryopreservation [4] |
Translational Applications and Future Directions
From Microbial Functions to Targeted Therapies
The functional understanding of a healthy microbiome is driving the development of novel therapeutic strategies that target specific microbial activities rather than overall composition. Precision microbiome interventions are evolving beyond traditional probiotics and FMT toward defined consortia of core probiotics with specific functional attributes [4]. These live biotherapeutic products (LBPs) represent a new class of medicines designed to restore specific microbial functions rather than simply altering community composition.
Promising candidates include:
- Faecalibacterium prausnitzii: Associated with IBD maintenance through its impact on gut mucosal immunity and butyrate production [4].
- Akkermansia muciniphila: Linked to metabolic health through improvement of gut barrier function and insulin sensitivity [4].
- Lactobacillus reuteri: Recommended by World Gastroenterology Organisation for pediatric acute gastroenteritis and infant colic [4].
The future of microbiome-based therapeutics lies in matching specific functional deficiencies with targeted microbial interventions. This requires deeper understanding of the mechanisms underlying microbial influence on host pathways and the development of robust diagnostic biomarkers to identify patients most likely to respond to specific microbiome-directed therapies [4].
Methodological Considerations for Robust Science
Microbiome research faces several methodological challenges that must be addressed to advance the field:
Standardization of Diversity Metrics: The field suffers from a proliferation of diversity metrics without clear biological interpretation. Guidelines now recommend reporting a comprehensive set of metrics including richness, phylogenetic diversity, entropy, dominance, and an estimate of unobserved microbes to capture different aspects of microbial communities [3].
Appropriate Use of Population Descriptors: Research identifying "race-based" differences in microbiome composition often mistakenly attributes these to biological rather than socio-environmental factors [2]. Race is a social construct, not a biological determinant, and differences between racial groups likely reflect variation in environmental exposures, diet, socioeconomic factors, and structural inequities [2]. Study designs should directly measure these specific variables rather than using race as a proxy.
Integration of Multi-omic Data: Combining metagenomic, metatranscriptomic, and metabolomic data remains challenging but is essential for connecting microbial community structure to function. Computational frameworks like the iProbiotics machine learning platform can facilitate rapid probiotic screening and identification of core functional members of the gut microbiota [4].
A healthy microbiome is defined by its functional capacity to maintain metabolic equilibrium, educate the immune system, and provide colonization resistance against pathogens. These core functions are conserved across different microbial community structures and represent the ultimate therapeutic targets for microbiome-based interventions. As research moves toward precision microbiome medicine, the focus will increasingly shift from taxonomic composition to functional capabilities, enabling development of targeted therapies that restore specific microbial functions in a personalized manner. The integration of advanced multi-omic technologies, standardized analytical frameworks, and appropriate consideration of socio-environmental factors will be essential for translating our understanding of microbiome function into effective interventions for human health.
The gut microbiome exerts a profound influence on host physiology and disease susceptibility through a complex network of molecular interactions. This whitepaper provides an in-depth technical analysis of three fundamental classes of microbial mediators: short-chain fatty acids (SCFAs), tryptophan derivatives, and microbial antigens. We examine their production pathways, receptor interactions, signaling mechanisms, and functional impacts on host immunity, metabolism, and barrier function. Within the framework of host-microbiome interactions in health and disease, this review synthesizes current mechanistic understandings and presents standardized methodological approaches for investigating these key molecular players, offering researchers a comprehensive resource for advancing therapeutic development in microbiome-mediated conditions.
The human gastrointestinal tract hosts trillions of microorganisms that continuously communicate with host systems through molecular signaling. This dialogue is essential for maintaining homeostasis but, when disrupted, can contribute to disease pathogenesis across multiple organ systems [5] [6]. The molecular mediators of this cross-talk can be categorized into three primary classes: short-chain fatty acids (SCFAs) produced from dietary fiber fermentation, tryptophan derivatives generated through host and microbial metabolism of essential amino acids, and microbial antigens that directly interface with host pattern recognition receptors. These mediators orchestrate a broad spectrum of host responses, from immune cell differentiation and epithelial barrier maintenance to neuroendocrine signaling and metabolic regulation [7] [8] [9]. Understanding their precise mechanisms of action provides crucial insights for developing novel therapeutic strategies for inflammatory, metabolic, autoimmune, and neoplastic diseases.
Short-Chain Fatty Acids (SCFAs)
Production and Basic Properties
Short-chain fatty acids (SCFAs), primarily acetate (C2), propionate (C3), and butyrate (C4), are produced by anaerobic bacterial fermentation of dietary fibers and resistant starch in the colon [7] [10]. Their production depends on gut microbiota composition, with key producers including Bacteroides spp., Blautia spp., Ruminococcus, and Bifidobacterium [7] [11]. The molar ratio of acetate, propionate, and butyrate in colonic contents is approximately 60–70:20–30:10–20, reflecting acetate as the most abundant SCFA [7] [10]. In peripheral blood, this ratio shifts dramatically to approximately 91:5:4 due to significant hepatic metabolism of propionate and butyrate, while acetate bypasses hepatic clearance [7].
More than 90% of SCFAs are absorbed from the intestinal lumen. Colonocytes utilize butyrate as their primary energy source, providing 60–70% of their energy requirements [7]. SCFAs not metabolized by colonocytes enter the portal circulation and are transported to the liver, where propionate and butyrate are almost entirely extracted [7]. The concentration of SCFAs in the colon is approximately 100 mM, while plasma concentrations range from 0.1 mM to 10 mM, with fecal concentrations providing a reliable indicator of colonic production [12].
Table 1: SCFA Concentrations Across Biological Compartments
| Compartment | Total SCFAs | Acetate | Propionate | Butyrate | Notes | Source |
|---|---|---|---|---|---|---|
| Colon Contents | ~100 mM | 60-70% | 20-30% | 10-20% | Molar ratio | [7] [12] |
| Peripheral Blood | Variable | ~91% | ~5% | ~4% | Molar ratio | [7] |
| Adult Feces | ~543.4 µmol/g | Predominant | Secondary | Tertiary | Concentration | [11] |
| Neonate Feces (1-month) | ~267.6 µmol/g | Predominant | Secondary | Tertiary | Increases with microbiome maturation | [11] |
| Preterm Neonate Feces | Significantly lower | ~75.6 µmol/g | ~17.0 µmol/g | ~0.5 µmol/g | At 1 month old | [11] |
Receptors and Signaling Pathways
SCFAs mediate their effects through multiple mechanisms: activation of specific G-protein-coupled receptors (GPCRs), inhibition of histone deacetylases (HDACs), and metabolic integration as energy substrates [7].
GPCR Activation: Three primary SCFA receptors have been characterized:
- GPR41 (FFAR3): Couples to Gαi/o subunits, shows preference for propionate > butyrate > acetate, and is expressed in intestine, lymph nodes, sympathetic ganglia, and peripheral blood mononuclear cells [7] [12].
- GPR43 (FFAR2): Couples to both Gαi/o and Gαq subunits, responds to acetate ≥ propionate ≥ butyrate, and is highly expressed on immune cells including neutrophils, monocytes, and lymphocytes [7] [12].
- GPR109A (HCAR2): Couples to Gαi/o, is activated exclusively by butyrate, and is expressed on intestinal epithelial cells, adipocytes, monocytes, macrophages, and dendritic cells [7].
HDAC Inhibition: Butyrate and, to a lesser extent, propionate function as potent histone deacetylase (HDAC) inhibitors, particularly affecting HDAC1, HDAC3, and HDAC4 [7]. This inhibition increases histone acetylation, altering gene expression patterns in immune and epithelial cells, which contributes to anti-inflammatory and anti-proliferative effects.
Cellular Uptake: SCFAs enter cells via passive diffusion and active transport through monocarboxylate transporters (MCT1, MCT2, MCT4) and sodium-coupled monocarboxylate transporters (SMCT1 and SMCT2) [7] [10].
Figure 1: SCFA Signaling Pathways and Mechanisms of Action
Quantitative Analysis of SCFA Receptors
Table 2: SCFA Receptor Characteristics and Signaling Properties
| Receptor | Aliases | SCFA Affinity | Gα Subunit Coupling | Primary Tissue/Cellular Expression | Key Functions |
|---|---|---|---|---|---|
| GPR41 | FFAR3 | Propionate > Butyrate > Acetate | Gαi/o | Intestine, lymph nodes, sympathetic ganglia, peripheral blood mononuclear cells | Regulation of energy homeostasis, sympathetic nervous system activity, PYY secretion |
| GPR43 | FFAR2 | Acetate ≥ Propionate ≥ Butyrate | Gαi/o, Gαq | Immune cells (neutrophils, monocytes, lymphocytes), intestine, spleen | Neutrophil chemotaxis, inflammatory cytokine regulation, Treg differentiation, metabolic regulation |
| GPR109A | HCAR2 | Butyrate exclusively | Gαi/o | Colon, adipocytes, monocytes, macrophages, dendritic cells, neutrophils | Anti-inflammatory effects, induction of Treg cells, maintenance of epithelial barrier |
Experimental Protocols for SCFA Research
SCFA Quantification in Fecal Samples:
- Sample Collection: Collect fresh fecal samples in pre-weighed sterile tubes, immediately freeze in liquid nitrogen, and store at -80°C.
- Extraction: Homogenize 50-100 mg of fecal material in ultrapure water (1:10 w/v). Centrifuge at 14,000 × g for 20 minutes at 4°C.
- Derivatization: Transfer supernatant to GC vials and derivative with N-tert-butyldimethylsilyl-N-methyltrifluoroacetamide (MTBSTFA) at 70°C for 60 minutes.
- GC-MS Analysis: Separate derivatives using gas chromatography with a DB-5MS column and detect with mass spectrometry in selected ion monitoring mode. Use isotope-labeled internal standards for quantification.
SCFA Receptor Signaling Assay:
- Cell Transfection: Transfect HEK293 cells with plasmids encoding GPR41, GPR43, or GPR109A along with a CRE-luciferase or NFAT-luciferase reporter.
- Stimulation: Treat cells with SCFAs at varying concentrations (0.1 μM to 10 mM) for 6-8 hours.
- Detection: Measure luciferase activity using a luminometer. For calcium flux assays, use calcium-sensitive dyes in FLIPR systems.
HDAC Inhibition Assay:
- Nuclear Extract Preparation: Isolate nuclei from treated cells and extract nuclear proteins.
- Enzyme Activity: Incubate extracts with fluorogenic HDAC substrate (e.g., Ac-Lys(Ac)-AMC) in HDAC assay buffer for 1-2 hours at 37°C.
- Detection: Stop reaction with developer containing trichostatin A and nicotinamide, then measure fluorescence (excitation 360 nm, emission 460 nm).
Tryptophan Derivatives
Metabolic Pathways and Key Metabolites
Tryptophan, an essential amino acid obtained from dietary protein, is metabolized through three major pathways: the host kynurenine pathway, host serotonin pathway, and various microbial metabolic pathways [8] [9]. The kynurenine pathway, initiated by indoleamine 2,3-dioxygenase (IDO1) or tryptophan 2,3-dioxygenase (TDO), accounts for over 90% of tryptophan catabolism and generates multiple immunologically active metabolites [8] [13]. The serotonin pathway produces the neurotransmitter serotonin in enterochromaffin cells and central nervous system neurons [8]. Gut microbiota metabolize tryptophan into various indole derivatives through different enzymatic pathways [8] [9].
Table 3: Major Tryptophan Metabolites and Their Microbial Producers
| Metabolite Class | Specific Metabolites | Producing Bacteria | Key Enzymes | Reported Concentrations |
|---|---|---|---|---|
| Indoles | Indole | Escherichia coli, Clostridium spp., Bacteroides spp. | Tryptophanase (TnaA) | Feces: ~2.6 mM [9] |
| Indole Derivatives | IAA, IAld, ILA | Lactobacillus spp., Bifidobacterium spp., Clostridium spp. | Aromatic amino acid aminotransferase, ILDH | Serum IAA: ~1.3 μM; Serum ILA: ~0.15 μM [9] |
| Aryl Hydrocarbon Receptor Ligands | IPA, IA | Clostridium sporogenes, Peptostreptococcus spp. | Phenyllactate dehydratase gene cluster (fldAIBC) | Serum IPA: ~1.0 μM (50 nM reported recently) [9] |
| Neuroactive Amines | Tryptamine | Ruminococcus gnavus, Clostridium spp. | Tryptophan decarboxylase (TrpD) | Urine (pregnant women): ~9 μM [9] |
Receptor Interactions and Signaling Mechanisms
Tryptophan metabolites signal through multiple receptors with diverse downstream effects:
Aryl Hydrocarbon Receptor (AHR) Activation: Multiple microbial tryptophan catabolites including IAld, IAA, ILA, and IPA function as AHR ligands [9]. AHR activation regulates immune cell differentiation, enhances epithelial barrier function, and modulates xenobiotic metabolism. In intestinal immunity, AHR signaling promotes IL-22 production by type 3 innate lymphoid cells, supporting epithelial repair and antimicrobial defense [9].
GPCR Signaling: Several tryptophan metabolites activate specific GPCRs:
- Kynurenic acid activates GPR35, influencing energy expenditure and gastrointestinal motility [13].
- Tryptamine activates trace amine-associated receptor 1 (TAAR1) and 5-HT4 receptors, modulating serotonin signaling and gut motility [8].
Neuroendocrine Modulation: Serotonin (5-hydroxytryptamine, 5-HT) synthesized in enterochromaffin cells regulates gut motility, secretion, and platelet function [8]. Although peripheral serotonin cannot cross the blood-brain barrier, it influences the gut-brain axis via vagal afferent signaling.
Immune Regulation: Kynurenine pathway metabolites, particularly kynurenine itself, regulate T cell differentiation and function. High kynurenine levels promote regulatory T cell differentiation while suppressing effector T cell responses, creating an immunotolerant environment [8] [13].
Figure 2: Tryptophan Metabolic Pathways and Signaling Mechanisms
Experimental Protocols for Tryptophan Metabolite Research
Quantification of Tryptophan Metabolites:
- Sample Preparation: Extract metabolites from serum, feces, or cell culture supernatant using methanol precipitation (2:1 methanol:sample). Centrifuge at 14,000 × g for 15 minutes.
- LC-MS/MS Analysis: Separate metabolites using reverse-phase chromatography (C18 column) with a water-acetonitrile gradient containing 0.1% formic acid. Detect using multiple reaction monitoring on a triple quadrupole mass spectrometer.
- Quantification: Use stable isotope-labeled internal standards for each metabolite (e.g., d5-tryptophan, d4-kynurenine) for precise quantification.
AHR Activation Assay:
- Reporter Cell Line: Use HepG2 or other cell lines stably transfected with an AHR-responsive luciferase construct (e.g., XRE-luciferase).
- Treatment: Incubate cells with tryptophan metabolites or test compounds for 16-24 hours.
- Detection: Measure luciferase activity using a luminometer. Include known AHR ligands (e.g., FICZ) as positive controls and AHR antagonists (e.g., CH223191) as specificity controls.
IDO1 Activity Assay:
- Cell Culture: Stimulate human dendritic cells or macrophages with IFN-γ (100 ng/mL) for 24 hours to induce IDO1 expression.
- Incubation: Add tryptophan (100 μM) and test compounds for additional 24 hours.
- Measurement: Quantify kynurenine in supernatant by HPLC or spectrophotometrically (kynurenine absorbs at 360 nm). Calculate IDO1 activity as kynurenine production normalized to total protein.
Microbial Antigens
Classification and Immune Recognition
Microbial antigens represent a diverse category of structural components, secreted factors, and metabolic products that directly interface with the host immune system. They can be broadly classified into inflammatory commensals that stimulate effector immune responses and immunoregulatory commensals that promote tolerance [6]. These antigens engage pattern recognition receptors (PRRs) including Toll-like receptors (TLRs), NOD-like receptors (NLRs), and C-type lectin receptors on host immune cells [5].
Key microbial antigens include:
- Polysaccharide A (PSA) from Bacteroides fragilis: Signals through TLR2/TLR1 and Dectin-1 to promote anti-inflammatory responses and regulatory T cell development [5].
- Segmented Filamentous Bacteria (SFB) antigens: Adhere to intestinal epithelium and induce potent Th17 cell responses through antigen-specific mechanisms [6].
- Bacteroidetes β-hexosaminidase: Recognized by CD4 T cells as a conserved antigen driving their differentiation into CD4+CD8αα+ intraepithelial lymphocytes [14].
Mechanisms of Immune Modulation
Microbial antigens shape host immunity through several mechanisms:
T Cell Polarization: Specific commensal antigens direct T cell differentiation into distinct functional subsets. SFB antigens promote Th17 differentiation, while PSA from B. fragilis and Clostridium clusters promote regulatory T cell development [5] [6].
Innate Immune Training: Microbial antigens prime innate immune cells for enhanced or tempered responses to subsequent challenges. This trained immunity involves epigenetic reprogramming and metabolic alterations in myeloid cells [5].
Mucosal Barrier Reinforcement: Certain microbial antigens strengthen epithelial barrier function by enhancing tight junction expression and promoting mucus production. For instance, indole metabolites from microbial tryptophan metabolism upregulate tight junction proteins [5].
Compartmentalization: The immune system maintains compartmentalization of microbial antigens to the mucosal surface through multiple mechanisms including IgA coating, antimicrobial peptide production, and mucus layer maintenance [5].
Experimental Protocols for Microbial Antigen Research
Bacterial Antigen Preparation:
- Polysaccharide Isolation: Culture bacteria in appropriate medium, harvest supernatant, and precipitate polysaccharides with ethanol (3:1 v/v). Purify using ion-exchange chromatography and confirm structure by NMR.
- Cell Wall Fraction Preparation: Lyse bacteria by sonication, treat with DNase/RNase, and extract cell wall components using detergent-based methods.
- Protein Antigen Purification: Clone genes of interest into expression vectors, express in E. coli, and purify using affinity chromatography.
T Cell Polarization Assay:
- Antigen Presentation: Isolate naive CD4+ T cells from mouse spleen or human PBMCs using magnetic bead separation.
- Differentiation Culture: Co-culture naive T cells with bone marrow-derived dendritic cells pulsed with microbial antigens (1-10 μg/mL) in the presence of polarizing cytokines:
- Th17: TGF-β (2 ng/mL), IL-6 (20 ng/mL), anti-IFN-γ, anti-IL-4
- Treg: TGF-β (5 ng/mL), IL-2 (100 U/mL)
- Flow Cytometry Analysis: After 5 days, restimulate cells with PMA/ionomycin, stain for intracellular cytokines (IL-17A for Th17, FoxP3 for Treg) and analyze by flow cytometry.
Epithelial Barrier Function Assay:
- Transepithelial Electrical Resistance (TEER): Culture epithelial cells (Caco-2 or T84) on transwell inserts until differentiated. Treat with microbial antigens and measure TEER daily using volt-ohm meter.
- Paracellular Permeability: Add FITC-dextran (4 kDa) to the apical compartment and measure flux to the basolateral compartment after 4 hours using a fluorometer.
- Immunofluorescence: Stain for tight junction proteins (ZO-1, occludin) and visualize by confocal microscopy.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Investigating Microbial Mediators
| Reagent Category | Specific Examples | Key Applications | Supplier Examples |
|---|---|---|---|
| SCFA Standards & Inhibitors | Sodium butyrate, Sodium propionate, Acetate, GPR41/43 antagonists (CATPB, GLPG0974) | Receptor signaling studies, HDAC inhibition assays, in vitro and in vivo functional studies | Sigma-Aldrich, Tocris, Cayman Chemical |
| Tryptophan Metabolites & Modulators | Kynurenine, Kynurenic acid, Indole-3-carbinol, FICZ, AHR antagonist CH223191, IDO1 inhibitor Epacadostat | AHR activation assays, T cell polarization studies, metabolic pathway analysis | Sigma-Aldrich, Enzo Life Sciences, MedChemExpress |
| Microbial Antigens | Bacteroides fragilis PSA, SFB antigens, LPS, Flagellin, Peptidoglycan | Immune cell activation studies, antigen-specific T cell responses, barrier function assays | InvivoGen, ATCC, laboratory isolation |
| Receptor Expression Constructs | GPR41/43/109A overexpression plasmids, AHR reporter constructs, TLR expression vectors | Receptor signaling studies, high-throughput compound screening, mechanism of action studies | cDNA ORF clones, Addgene |
| Detection Antibodies | Anti-GPR41/43, Anti-AHR, Anti-FoxP3, Anti-IL-17A, Phospho-specific antibodies for signaling | Flow cytometry, Western blot, immunohistochemistry, ELISA development | BioLegend, Cell Signaling Technology, R&D Systems |
| Analytical Standards | 13C-labeled SCFAs, d5-Tryptophan, d4-Kynurenine, Isotope-labeled indole derivatives | Mass spectrometry quantification, internal standards for metabolomics | Cambridge Isotope Laboratories, Sigma-Aldrich |
| Regaloside E | Regaloside E, MF:C20H26O12, MW:458.4 g/mol | Chemical Reagent | Bench Chemicals |
| fusarisetin A | fusarisetin A, MF:C22H31NO5, MW:389.5 g/mol | Chemical Reagent | Bench Chemicals |
The molecular mediators produced by the gut microbiota—SCFAs, tryptophan derivatives, and microbial antigens—form a complex signaling network that fundamentally shapes host physiology and disease susceptibility. These mediators operate through defined receptors and signaling pathways to regulate immune responses, maintain barrier integrity, and modulate metabolic processes. Their integrated study requires sophisticated methodological approaches spanning molecular biology, immunology, and metabolomics. As research in this field advances, targeting these microbial mediators offers promising therapeutic opportunities for a wide range of conditions, including inflammatory diseases, metabolic disorders, cancer, and neurological conditions. The experimental frameworks and technical resources provided in this whitepaper offer researchers a foundation for advancing our understanding of host-microbiome interactions and developing novel microbiome-based therapeutics.
Barrier tissues—the gut, skin, and lungs—form the critical interface between the external environment and the internal body. They are not passive shields but dynamic ecosystems where host epithelial and immune cells engage in constant, complex communication with commensal microorganisms to maintain immune homeostasis. This equilibrium is orchestrated through a sophisticated network of epithelial sensing, immune cell regulation, and microbial metabolite signaling. Disruption of this delicate balance, termed dysbiosis, is a hallmark of numerous inflammatory, allergic, and infectious diseases. This whitepaper synthesizes the core mechanisms governing immune homeostasis at barrier tissues, detailing the tissue-specific cellular players, molecular pathways, and the pivotal role of the microbiome. Framed within the context of host-microbiome interactions, it provides a technical guide for researchers and drug development professionals, integrating current experimental models, key reagents, and quantitative data to inform future therapeutic innovation.
Barrier tissues, including the gastrointestinal tract, skin, and respiratory system, provide the first line of defense against environmental insults, pathogens, and toxins. Their primary function is to establish a physical barrier while simultaneously enabling selective absorption and sensing. The integrated ecosystem of a barrier tissue comprises the epithelial layer, a diverse population of resident and recruited immune cells, the commensal microbiota (bacteria, fungi, viruses), and their collective metabolite milieu [15] [16]. The immune system at these sites must therefore perform a delicate balancing act: mounting robust protective responses against genuine threats while maintaining tolerance to harmless antigens, food particles, and beneficial commensals. This state of controlled alertness is immune homeostasis.
The host-microbiome interaction is a cornerstone of this homeostatic regulation. The human body harbors a vast community of commensal microbes, with the gut microbiota alone being referred to as a "second genome" due to its profound influence on host physiology [17]. The microbiome is now understood to be a key environmental factor shaping the development, function, and tuning of the host immune system at barrier sites and beyond [18] [19]. This review will dissect the mechanisms of immunomodulation that sustain homeostasis, explore the consequences of their breakdown, and outline the experimental tools driving discovery in this field.
Core Mechanisms of Homeostasis at Barrier Tissues
The Epithelial Layer: More Than a Physical Barrier
The epithelium is the foundational cellular component of all barrier tissues. Far from being a simple wall, it is an active sensory and signaling organ equipped with an arsenal of pattern-recognition receptors (PRRs) and mechanisms for direct microbial interaction.
- Innate Immune Sensing: Epithelial cells express a diverse array of Toll-like receptors (TLRs) and cytosolic sensors (e.g., NLRs, inflammasomes) that detect pathogen-associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs) [20]. The localization of these sensors is critical. In the intestinal epithelium, certain TLRs are strategically positioned apically or basolaterally to distinguish between luminal commensals (requiring tolerance) and invasive pathogens (eliciting a strong defense) [20].
- Secretory Functions: Epithelial cells secrete a multitude of factors that shape the barrier environment. These include:
- Mucus: Goblet cells in the gut and airway produce mucus layers that trap microbes and particulates, preventing direct contact with the epithelium [15].
- Antimicrobial Peptides (AMPs): Paneth cells in the intestinal crypts and keratinocytes in the skin produce defensins, cathelicidins, and other AMPs that directly inhibit or kill microorganisms, thereby controlling microbial colonization [15] [21].
- Cytokines and Alarmins: Epithelial-derived cytokines like TSLP, IL-25, and IL-33 alert the underlying immune system to barrier damage and help polarize subsequent immune responses [15] [22].
The Microbiome and Its Metabolites: Instructive Signals for Immunity
The commensal microbiota is essential for the proper development and regulation of the immune system. Germ-free (GF) mice exhibit significant immune deficiencies, including underdeveloped lymphoid structures and reduced immune cell populations, which can be partially rescued by microbial colonization [21] [18]. The microbiome exerts its immunomodulatory effects through two primary mechanisms: direct molecular interaction and metabolite production.
- Direct Molecular Interaction: Microbial-associated molecular patterns (MAMPs) from commensals engage host PRRs, providing tonic signals that maintain baseline immune readiness and promote homeostasis. For instance, commensal bacteria can promote the expansion of anti-inflammatory regulatory T cells (Tregs) via TLR2 signaling [18].
- Microbial Metabolites: The fermentation of dietary fiber by gut bacteria produces short-chain fatty acids (SCFAs), such as acetate, propionate, and butyrate. SCFAs are potent immunomodulators with systemic effects [21]. They function by:
- Inhibiting histone deacetylases (HDACs), thereby influencing gene expression in immune cells and promoting Treg differentiation [18].
- Signaling through G-protein-coupled receptors (GPCRs) like GPR41 and GPR43 on immune and epithelial cells, modulating inflammatory cytokine production and enhancing barrier integrity [21] [18].
Table 1: Key Immunomodulatory Metabolites from the Microbiome
| Metabolite | Primary Microbial Producers | Immunological Functions | Target Barrier Tissues |
|---|---|---|---|
| Short-chain fatty acids (SCFAs) | Bacteroidetes, Firmicutes | Promote Treg differentiation; inhibit HDAC; strengthen epithelial barrier; modulate macrophage function | Gut, Lung, Skin |
| Tryptophan derivatives | Various commensal bacteria | Activate Aryl Hydrocarbon Receptor (AhR); promote IL-22 production; maintain barrier function | Gut, Skin |
| Secondary bile acids | Certain Clostridium species | Anti-inflammatory; regulate innate immune responses | Gut |
Tissue-Resident and Recruited Immune Cells: The Executors of Homeostasis
A specialized repertoire of immune cells resides in or patrols barrier tissues, executing the commands issued by the epithelium and the microbiome.
- Innate Lymphoid Cells (ILCs): These tissue-resident cells respond rapidly to cytokine signals from epithelia. ILC2s, for instance, are activated by IL-25 and IL-33 to produce type 2 cytokines, which are important for anti-helminth defense and tissue repair but also drive allergic pathology when dysregulated [15]. The microbiota shapes the composition and function of ILC populations [18].
- T Lymphocytes: Barrier tissues harbor diverse T cell populations. Tissue-resident memory T cells (Trm) provide localized protection against re-infection. Regulatory T cells (Tregs) are critical for enforcing tolerance to commensals and food antigens, preventing inappropriate inflammation. Specific commensals, such as Clostridium species, are known to induce colonic Tregs [18].
- Macrophages and Dendritic Cells (DCs): These professional antigen-presenting cells sample the environment and dictate the nature of the T cell response. Intestinal macrophages and DCs are particularly adept at inducing Tregs in a steady state, a process influenced by retinoic acid and TGF-β [15]. They also transport gut-derived antigens to mesenteric lymph nodes, shaping systemic immune tolerance.
The following diagram illustrates the core cellular and molecular interactions that maintain homeostasis at a typical barrier tissue, such as the gut or lung.
Core Homeostatic Circuitry at Barrier Tissues
Tissue-Specific Immune Adaptations
While the core principles of barrier immunity are shared, the gut, skin, and lungs have evolved unique anatomical and immunological adaptations tailored to their distinct environmental challenges.
The Intestinal Barrier
The gut mucosa represents the body's largest barrier surface and hosts the densest microbial community. Its homeostasis relies on extreme specialization.
- Cellular Diversity: The intestinal epithelium is a single cell layer comprising absorptive enterocytes and several secretory lineages: Goblet cells (mucus production), Paneth cells (AMP secretion in the small intestine), Enteroendocrine cells (hormone secretion), and Tuft cells (sensing and initiating type 2 immunity) [15] [20].
- Compartmentalization: The mucus layer physically separates the bulk of the microbiota from the epithelium. In the colon, this layer is structured as an inner, sterile stratum and an outer, microbially colonized stratum [15].
- Immune Induction Sites: Structures like Peyer's patches and isolated lymphoid follicles serve as specialized sites for antigen sampling and the initiation of adaptive immune responses, including the generation of IgA-producing B cells, which is the most abundant antibody isotype in the gut and crucial for microbiota control [18].
The Skin Barrier
The skin epidermis is a multi-layered, keratinizing epithelium that must withstand physical, chemical, and biological trauma.
- Stratified Epithelium: Epidermal stem cells (EpdSCs) generate a stratified squamous epithelium, with terminally differentiated, enucleated corneocytes (squames) forming the outermost, waterproof barrier sealed by lipid bilayers [15].
- Resident Immune Sentinels: The epidermis is patrolled by Dendritic Epidermal T Cells (DETCs), a specialized population of resident γδ T cells, and Langerhans cells, tissue-resident macrophages. These cells work with EpdSCs to mount rapid responses upon barrier breach [15].
- Inflammatory Memory: Following an inflammatory experience, skin epithelial stem cells can retain an epigenetic memory, allowing for a more robust response to subsequent challenges. This "trained immunity" in parenchymal cells is a key adaptation [15].
The Pulmonary Barrier
The lungs present a unique challenge, requiring a thin epithelium for efficient gas exchange while being continuously exposed to inhaled antigens and microbes.
- Dynamic Microbiome: Unlike the gut, the healthy lung microbiome is low-biomass and transient, continually seeded by microaspiration from the upper respiratory tract and removed by mucociliary clearance and host immune mechanisms [21] [23]. The core healthy lung bacteriome includes genera like Pseudomonas, Streptococcus, and Veillonella [23].
- The Gut-Lung Axis: There is a well-established gut-lung axis, where gut-derived metabolites, particularly SCFAs, can modulate lung immunity. SCFAs can suppress allergic inflammation in the lung and enhance resistance to respiratory pathogens [21]. This explains how diet and gut dysbiosis can influence the susceptibility and severity of respiratory diseases like asthma [24] [21].
Table 2: Comparative Overview of Barrier Tissue Homeostasis
| Feature | Gut | Skin | Lung |
|---|---|---|---|
| Epithelial Structure | Single layer | Stratified squamous | Single layer, ciliated |
| Key Microbial Habitat | Dense, diverse community | Less dense, site-specific | Low biomass, dynamic |
| Dominant Commensals | Bacteroidetes, Firmicutes | Staphylococcus, Cutibacterium | Pseudomonas, Streptococcus |
| Specialized Immune Cells | Paneth cells, IELs | DETCs, Langerhans cells | Alveolar macrophages |
| Critical Secretions | Mucus, AMPs (defensins) | AMPs (defensins), sebum | Surfactant, mucus |
| Primary Communication Axis | Gut-Lung, Gut-Brain | Gut-Skin | Gut-Lung |
Experimental Models and Methodologies
Investigating barrier immunity requires sophisticated models that recapitulate the complexity of host-microbe interactions. The following section details key experimental approaches and their associated protocols.
In Vivo and In Vitro Models
- Germ-Free (GF) and Gnotobiotic Mice: GF mice, raised in sterile isolators with no resident microbiota, are the gold standard for establishing the microbiome's causal role in immune phenotypes. These mice can be colonized with a single or defined consortium of microbes (gnotobiotic) to dissect specific host-microbe relationships [21] [18].
- Protocol Outline: 1) Maintain breeding colony in flexible film isolators. 2) Verify sterility via regular culturing and 16S rRNA PCR of feces. 3) For colonization experiments, transfer GF mice to a separate isolator and introduce a bacterial suspension via oral gavage. 4) Monitor microbial engraftment and host immune responses over time.
- 3D Human Mucosal Models: Advanced in vitro systems that mimic human disease pathology. For example, a 3D model of inflammatory bowel disease (IBD) integrates epithelial cells, stromal fibroblasts, and immune elements within a scaffold, replicating barrier dysfunction, immune activation, and stromal remodeling [16].
- Protocol Outline: 1) Seed human intestinal epithelial cells onto a collagen scaffold with embedded fibroblasts. 2) Culture at an air-liquid interface to promote polarization and differentiation. 3) Introduce immune cells (e.g., peripheral blood mononuclear cells) into the system. 4) Stimulate with TNF-α or other cytokines to induce disease-like pathology. 5) Assess outcomes via transepithelial electrical resistance (TEER), cytokine ELISAs, and RNA sequencing.
- Antibiotic-Induced Dysbiosis: A common method to deplete the host microbiota and study its functional impact.
- Protocol Outline: 1) Administer a broad-spectrum antibiotic cocktail (e.g., ampicillin, vancomycin, neomycin, metronidazole) in the drinking water of specific pathogen-free (SPF) mice for 2-4 weeks. 2) Confirm depletion of gut microbiota via 16S rRNA sequencing of fecal samples. 3) Challenge mice with an allergen (e.g., house dust mite for lung inflammation) or pathogen and compare immune responses to untreated controls [21].
The Scientist's Toolkit: Key Research Reagents
The following table catalogues essential reagents and their applications in studying barrier tissue immunology.
Table 3: Essential Research Reagents for Barrier Immunity Studies
| Reagent / Tool | Function / Target | Key Application Examples |
|---|---|---|
| Anti-CD3ε / Anti-IL-10R mAb | T cell activation / IL-10 signaling blockade | Inducing T cell-driven colitis model in mice to study gut inflammation and tolerance. |
| Recombinant Cytokines (TSLP, IL-25, IL-33) | Activate ILC2s and type 2 immunity | Studying the role of epithelial alarmins in allergic asthma or atopic dermatitis models. |
| TLR Agonists (e.g., LPS, Poly(I:C)) | Activate specific PRR pathways (TLR4, TLR3) | Probing innate immune sensing mechanisms in primary epithelial cells or in vivo. |
| SCFAs (Butyrate, Propionate) | HDAC inhibitors; GPCR agonists | In vitro treatment of T cells to induce Treg differentiation; in vivo administration to suppress inflammation. |
| Clostridium spp. clusters | Induce colonic Tregs | Gnotobiotic colonization of GF mice to study mechanisms of peripheral tolerance induction. |
| FTY720 (Sphingosine-1-phosphate receptor modulator) | Sequesters lymphocytes in lymph nodes | Distinguishing between tissue-resident and recirculating immune cell populations in barrier tissues. |
| DSS (Dextran Sodium Sulfate) | Epithelial toxicant | Chemically inducing colitis in mice to model IBD and study wound repair mechanisms. |
| Fluorescently-labeled ZO-1/Occludin Antibodies | Tight junction proteins | Visualizing and quantifying epithelial barrier integrity via immunofluorescence and confocal microscopy. |
| Neohesperidose | Neohesperidose, CAS:19949-48-5, MF:C12H22O10, MW:326.30 g/mol | Chemical Reagent |
| Villocarine A | Villocarine A, MF:C22H26N2O3, MW:366.5 g/mol | Chemical Reagent |
The workflow for a typical experiment investigating the role of the gut-lung axis in allergic asthma is depicted below.
Gut-Lung Axis Experiment Workflow
The study of immunomodulation at barrier tissues has evolved from a focus on static defense to a dynamic understanding of a deeply integrated, multi-kingdom ecosystem. The mechanisms that maintain homeostasis—epithelial sensing, microbial metabolite signaling, and educated immune cell responses—are interconnected and finely tuned. Dysregulation at any point in this network can lead to a breakdown of tolerance and the emergence of disease, as seen in the atopic march (the progression from atopic dermatitis to food allergy and asthma) [24] and in chronic inflammatory conditions like IBD.
Future research and therapeutic development will be guided by several key frontiers:
- Spatio-Temporal Dynamics: Advanced imaging and single-cell multi-omics will reveal how immune responses are organized with micron-level precision within tissues and how they evolve over time.
- Personalized Microbiome Interventions: Moving beyond broad-spectrum probiotics, next-generation therapies will involve defined microbial consortia or microbiome-derived metabolites tailored to an individual's microbial and immune profile [18].
- Barrier-Strengthening Strategies: Therapies aimed not only at suppressing inflammation but actively restoring epithelial barrier function—through SCFAs, tight junction stabilizers, or stem cell therapies—hold great promise [16].
- Systemic Axis Targeting: Acknowledging the interconnectedness of barriers via axes like the gut-lung and gut-skin will enable novel treatments for remote inflammatory diseases by targeting the gut microbiome.
A deep understanding of the immunomodulatory mechanisms at barrier tissues is no longer a niche field but a central pillar of immunology, indispensable for developing the next generation of therapeutics for allergic, autoimmune, infectious, and neoplastic diseases.
The human body exists in a state of intricate symbiosis with trillions of microorganisms, collectively known as the microbiome, which contribute over 150 times more genetic information than the human genome itself [25]. This complex ecosystem, particularly within the gastrointestinal tract, functions as a metabolic organ essential for host homeostasis, contributing to nutrient extraction, immune system maturation, and protection against pathogens [25] [26]. In a state of health, the gut microbiota exhibits remarkable stability, resilience, and taxonomic diversity, dominated primarily by the phyla Firmicutes and Bacteroidetes, which account for approximately 90% of all gut microbial species [27] [28]. This symbiotic relationship represents a finely tuned equilibrium where microbial communities engage in beneficial cross-talk with host systems through the production of metabolites, immune modulation, and maintenance of epithelial barrier integrity.
The transition from this symbiotic state to dysbiosis—defined as an alteration in the ecosystem associated with pathology—represents a critical juncture in disease pathogenesis [29]. Dysbiosis manifests through multiple mechanisms: reduced microbial diversity, altered functional capacities, outgrowth of pathobionts, and diminished production of beneficial metabolites [27] [29]. While the precise definition of a "healthy" microbiome remains elusive due to considerable interindividual variation, the dysbiotic state has been consistently linked to a range of chronic inflammatory and metabolic conditions, including inflammatory bowel disease (IBD), type 2 diabetes, and obesity [27] [30] [31]. This shift from mutualism to dysfunction involves a complex interplay between host genetics, environmental exposures, and microbial community dynamics that disrupts homeostatic mechanisms and propagates disease processes throughout the host system.
Mechanisms of Dysbiosis-Driven Pathogenesis
Metabolic Network Disruption in Host-Microbiome Crosstalk
Advanced metabolic modeling of host-microbiome interactions in IBD has revealed concomitant changes in metabolic activity across multiple data layers, highlighting profound disruptions in NAD, amino acid, one-carbon, and phospholipid metabolism [32]. During inflammatory flares, microbiome metabolic modeling demonstrates reduced within-community metabolic exchange, particularly affecting key metabolites including amylotriose, glucose, propionate, oxoglutarate, succinate, alanine, and aspartate [32]. These disruptions directly impact the host through multiple interconnected pathways:
- NAD Biosynthesis Impairment: Elevated host tryptophan catabolism during inflammation depletes circulating tryptophan pools, thereby impairing NAD biosynthesis—a cofactor fundamental to cellular energy production and redox homeostasis [32].
- Nitrogen Homeostasis Disruption: Reduced host transamination reactions disrupt nitrogen balance, subsequently impairing polyamine and glutathione metabolism essential for cellular protection and proliferation [32].
- One-Carbon Cycle Suppression: The suppressed one-carbon metabolism in patient tissues alters phospholipid profiles due to limited choline availability, affecting cellular membrane integrity and signaling [32].
Simultaneously, the microbiome exhibits complementary metabolic shifts in NAD, amino acid, and polyamine metabolism that exacerbate these host metabolic imbalances, creating a self-reinforcing cycle of metabolic dysfunction that perpetuates the inflammatory state [32].
Immunological Consequences of Microbial Dysbiosis
The gut microbiome plays an indispensable role in the education and regulation of the host immune system, with dysbiosis directly contributing to inappropriate immune activation in chronic inflammatory conditions. The intestinal epithelium serves as the primary interface for interactions between immune cells and gut microbes, with dendritic cells sampling microbial antigens to induce gut-resident Foxp3+ regulatory T cells (Tregs) [28]. This process depends significantly on specific Clostridia species that produce short-chain fatty acids (SCFAs), particularly butyrate, which enhances the integrity of intestinal epithelial cells and promotes anti-inflammatory responses [28].
Dysbiosis disrupts this delicate immunoregulatory balance through several mechanisms:
- Barrier Function Compromise: Dysbiosis is associated with altered physical epithelial barrier function, a thinner mucus layer, and impaired responses to endoplasmic reticulum stress, facilitating microbial translocation and immune activation [27].
- Pathobiont Expansion: Inflammatory conditions favor the expansion of pathobionts such as adherent-invasive Escherichia coli (AIEC), which can survive within macrophages and exert potent proinflammatory effects [29].
- SCFA Reduction: Diminished production of SCFAs, particularly butyrate and propionate, reduces their anti-inflammatory effects and impairs maintenance of colonic homeostasis [27].
The resultant immune dysregulation features inappropriate activation of both innate and adaptive immunity against gut antigens, with characteristic increases in proinflammatory cytokines and recruitment of inflammatory cells that perpetuate tissue damage and disease progression [27].
Table 1: Key Microbial Metabolites in Health and Disease
| Metabolite | Role in Symbiosis | Change in Dysbiosis | Consequence |
|---|---|---|---|
| Short-chain fatty acids (Butyrate, Propionate) | Primary energy source for colonocytes; Anti-inflammatory; Strengthen epithelial barrier | Reduced [27] | Impaired barrier function; Increased inflammation |
| Tryptophan metabolites | NAD biosynthesis; Immune regulation | Depleted circulating tryptophan [32] | Impaired NAD production; Disrupted cellular energy |
| Polyamines | Cell proliferation; Tissue repair | Disrupted metabolism [32] | Impaired mucosal healing |
| Bile acids | Lipid digestion; Antimicrobial effects | Altered composition; Reduced deconjugation [32] | Digestive dysfunction; Altered microbial composition |
Visceral Hypersensitivity and Neurological Implications
Beyond local intestinal inflammation, dysbiosis significantly impacts neurological function and pain perception through the gut-brain axis. Up to 30-50% of IBD patients in remission experience chronic abdominal pain despite the absence of active inflammation, suggesting altered sensory neuronal processing [33]. The gut microbiome influences visceral hypersensitivity through the production of neuroactive molecules including neurotransmitters (GABA, serotonin) and microbial metabolites such as SCFAs [33]. These molecules can directly interact with nociceptors to modulate hypersensitivity or indirectly influence pain signaling through immune stimulation [33].
Metabolomic approaches have identified approximately 5,000 low molecular weight molecules that mediate host-microbiome dynamics in pain perception [33]. The "sensitization" of nociceptors—characterized by a decreased threshold for stimulation and increased response magnitude—represents a key mechanism through which dysbiosis contributes to chronic pain states even in the absence of ongoing inflammation [33].
Methodological Approaches for Investigating Host-Microbiome Interactions
Metabolic Modeling and Multi-Omic Integration
To unravel the complex metabolic interactions between host and microbiome in inflammatory diseases, researchers have developed sophisticated modeling approaches that integrate multi-omic datasets:
- Constraint-Based Metabolic Modeling: This approach uses genome-scale metabolic models of the gut microbiome and host intestine to study host-microbiome metabolic cross-talk in the context of inflammation [32]. The modeling framework incorporates both coupling-based (MicrobiomeGS2) and agent-based (BacArena) approaches to predict flux distributions within bacterial communities [32].
- Context-Specific Metabolic Model (CSMM) Reconstruction: Using bulk RNA from colon biopsies and blood samples, researchers reconstruct tissue-specific metabolic models to calculate metabolic potential [32]. Reaction activity is estimated through multiple approaches: reaction-level expression activities (rxnExpr), reaction presence/absence in CSMM (PA), and flux variability analysis to determine upper and lower flux bounds (FVA.center, FVA.range) [32].
- Longitudinal Multi-Omic Profiling: Dense profiling of microbiome, transcriptome, and metabolome signatures from longitudinal IBD cohorts before and after drug therapy initiation allows identification of dynamic changes across biological layers [32].
Table 2: Experimental Models for Host-Microbiome Research
| Model System | Applications | Advantages | Limitations |
|---|---|---|---|
| Germ-free mice | Establishing causality in microbiome-disease relationships | Microbiome can be controllably manipulated; Absence of confounding microbes | Immune system develops abnormally without microbial exposure |
| Humanized microbiota mice | Studying human-relevant microbial communities | Human-derived microbiota in controlled environment | Limited translation due to host-specific differences |
| Organoids | Host-microbe interactions at epithelial interface | Human-derived; High-throughput capability | Lack full complexity of intestinal microenvironment |
| Cohort studies (Human) | Identifying disease-associated signatures | Direct human relevance; Assessment of real-world diversity | Correlation does not equal causation; Confounding factors |
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for Host-Microbiome Studies
| Category | Specific Tools/Reagents | Application | Key Features |
|---|---|---|---|
| Sequencing Technologies | PacBio HiFi full-length 16S rRNA gene sequencing [34] | Microbiome composition analysis | High-resolution taxonomic classification |
| Metagenomic shotgun sequencing [27] | Functional potential assessment | Identifies microbial genes and pathways | |
| Metabolomics Platforms | LC-MS (Liquid Chromatography-Mass Spectrometry) [33] | Metabolite identification and quantification | Broad detection of polar and non-polar metabolites |
| GC-MS (Gas Chromatography-Mass Spectrometry) [33] | Volatile compound analysis | Ideal for SCFA measurement | |
| Animal Models | TNBS-induced colitis mouse model [34] | IBD pathophysiology studies | Chemically-induced intestinal inflammation |
| Germ-free mice [27] [26] | Causality establishment | Absence of native microbiome | |
| Computational Tools | MicrobiomeGS2 [32] | Metabolic modeling | Coupling-based approach emphasizing cooperation |
| BacArena [32] | Agent-based metabolic modeling | Individual-based simulation of microbial competition | |
| Bupleuroside XIII | Bupleuroside XIII, MF:C42H70O14, MW:799.0 g/mol | Chemical Reagent | Bench Chemicals |
| Kuwanon O | Kuwanon O | Kuwanon O is a natural resorcinol polyphenol from Morus australis. It is For Research Use Only (RUO) and not for human consumption. | Bench Chemicals |
Diagnostic and Therapeutic Implications
Microbiome-Based Biomarkers and Diagnostic Approaches
The identification of specific microbial signatures associated with disease states enables the development of microbiome-based biomarkers for diagnostic and prognostic applications. In IBD, consistent alterations include reduced abundance of anti-inflammatory commensals such as Faecalibacterium prausnitzii and increased representation of Proteobacteria members including Escherichia coli [27]. Specific pathobionts such as adherent-invasive E. coli (AIEC) have been isolated from 21.7% of Crohn's disease chronic lesions compared to 6.2% of controls, suggesting their potential utility as diagnostic markers [29].
Functional biomarkers beyond taxonomic composition show particular promise for clinical application:
- Reduced Metabolic Exchanges: Inflammation-associated decreases in microbial cross-feeding of key metabolites including glucose, succinate, and aspartate may serve as functional indicators of dysbiosis [32].
- SCFA Production Deficits: Diminished production of butyrate and propionate represents a quantifiable functional deficiency in IBD microbiota [27].
- Microbial Diversity Metrics: Lower Shannon diversity indices have been associated with accelerated IBD onset (HR = 0.58 [0.49; 0.71]), highlighting the prognostic value of diversity measures [30].
Diagnosis of gut microbial dysbiosis typically involves comprehensive digestive stool analysis to determine bacterial types and quantities, though these analyses remain complex to perform and interpret [31]. Emerging approaches incorporate multi-parameter assessment including microbial composition, functional potential, and metabolic output to provide a more complete picture of the dysbiotic state.
Microbiome-Targeted Therapeutic Interventions
Current therapeutic approaches targeting the microbiome focus on restoring symbiotic relationships through multiple mechanisms:
- Dietary Interventions: High-quality nutrition significantly delays disease onset in both IBD (HR = 0.81 [0.66; 0.98]) and type 2 diabetes (HR = 0.45 [0.28; 0.72]) [30]. Dietary patterns that increase fiber intake support SCFA production and microbial diversity.
- Prebiotics and Probiotics: These interventions aim to directly modulate microbial community composition by introducing beneficial microorganisms or substrates that promote their growth [28].
- Fecal Microbiota Transplantation (FMT): Transfer of entire microbial communities from healthy donors has shown efficacy particularly for ulcerative colitis, though evidence for Crohn's disease remains less convincing [29].
- Novel Therapeutic Compounds: Plant-derived compounds such as galloyl-lawsoniaside A and uromyrtoside have demonstrated ability to restore microbial balance in colitis models by modulating key bacterial pathways including peptidoglycan biosynthesis [34].
- Pharmaceutical Modulation: Advanced metabolic models of host and microbe metabolism can predict dietary interventions that remodel the microbiome to restore metabolic homeostasis, suggesting novel therapeutic strategies for IBD [32].
The investigation of host-microbiome interactions has evolved from descriptive associations to mechanistic understandings of how microbial communities influence host physiology in health and disease. The transition from symbiosis to dysbiosis represents a critical pathway in the pathogenesis of chronic inflammatory and metabolic disorders, characterized by complex disruptions in metabolic cross-talk, immune regulation, and barrier function. Advanced multi-omic approaches and metabolic modeling have revealed the profound interconnectedness of host and microbial metabolic networks, demonstrating how inflammation induces complementary disruptions in both systems that perpetuate disease states.
Future research directions must focus on:
- Causality Establishment: While numerous associations between dysbiosis and disease are established, determining primary causal relationships remains challenging [29].
- Spatiotemporal Dynamics: Understanding how microbial communities vary along the gastrointestinal tract and over time will provide critical insights into disease mechanisms [33] [28].
- Personalized Interventions: Developing microbiome-based therapeutics tailored to individual microbial and host metabolic profiles represents the next frontier in precision medicine [32] [34].
- Standardization of Methodologies: Establishing consistent protocols for microbiome analysis and dysbiosis quantification will enhance reproducibility and clinical translation [29] [31].
As our understanding of host-microbiome interactions continues to deepen, the potential for targeting these relationships to prevent and treat chronic diseases offers promising avenues for therapeutic development. The integration of multi-omic data, advanced computational modeling, and targeted interventions positions microbiome research at the forefront of personalized medicine, with the potential to fundamentally reshape our approach to inflammatory and metabolic disorders.
The human body exists as a supraorganism, comprising human cells and a vast consortium of commensal microorganisms. Complex communication networks, known as microbial axes, facilitate crucial host-microbiome interactions that maintain systemic homeostasis. This whitepaper examines the core mechanisms and systemic implications of the gut-brain, gut-lung, and oral-systemic axes. We synthesize current understanding of how these axes influence pathophysiology across organ systems through neural, immune, endocrine, and metabolic pathways. Emerging therapeutic strategies targeting these axes, including precision microbiota interventions and barrier-strengthening approaches, are discussed alongside detailed experimental methodologies and reagent solutions for research applications.
The human microbiome represents a functional interface between host physiology and environmental factors. The gastrointestinal tract harbors the most dense and diverse microbial community, with the gut microbiota playing a crucial role in regulating host metabolism, immunity, and neurological function [18]. The conceptual framework of microbial axes has emerged as a fundamental paradigm for understanding how bidirectional communication between distant organ systems contributes to both health and disease.
The gut-brain axis, gut-lung axis, and oral-systemic axis represent distinct yet interconnected pathways through which microbial communities influence systemic physiology. These axes form dynamic, integrated networks involving neural signaling, immune modulation, metabolite transport, and microbial translocation. Disruption of homeostasis along these axes—through dysbiosis, barrier dysfunction, or immune dysregulation—has been implicated in the pathogenesis of numerous conditions, including neurodegenerative diseases, respiratory infections, metabolic disorders, and cancer [18] [35] [36].
This review integrates findings from microbiology, immunology, and neurobiology to elucidate the mechanistic basis of these systemic axes and their translational relevance for drug development.
The Gut-Brain Axis (GBA)
Core Components and Communication Pathways
The gut-brain axis constitutes a multichannel communication system linking emotional and cognitive centers of the brain with peripheral intestinal functions. Key components include the gut microbiota, intestinal mucosal barrier, enteric nervous system (ENS), vagus nerve, neuroendocrine signaling systems, and the blood-brain barrier (BBB) [36].
Communication occurs through several integrated pathways:
- Neural Pathways: The vagus nerve serves as a direct neural highway between gut and brainstem, transmitting sensory information about gut state and microbial metabolites to the central nervous system (CNS) [36].
- Immune Signaling: Gut microbes shape host immunity from development through adulthood. Microbial-associated molecular patterns (MAMPs) can activate Toll-like receptors (TLRs) in peripheral tissues and the brain, influencing neuroinflammation [18] [36].
- Endocrine Pathways: Enteroendocrine cells detect luminal contents and release neuroactive hormones and peptides that influence brain function [36].
- Metabolic Signaling: Microbiota-derived metabolites, including short-chain fatty acids (SCFAs), tryptophan derivatives, and bile acids, circulate systemically and can cross the BBB to influence CNS physiology [18] [36].
Mechanisms of Interaction and Systemic Effects
Microbial metabolites function as key messengers along the GBA. SCFAs (acetate, propionate, butyrate) produced by bacterial fermentation of dietary fiber exert profound effects on both peripheral and central physiology. They function as histone deacetylase (HDAC) inhibitors and activate G-protein-coupled receptors (GPCRs) to modulate inflammation, epithelial barrier integrity, and neurotransmitter synthesis [18].
The gut microbiota also directly produces or precursors a range of neuroactive molecules, including gamma-aminobutyric acid (GABA), serotonin, dopamine, and acetylcholine, which can influence brain function and behavior [36]. Additionally, gut microbes regulate the metabolism of tryptophan, the primary precursor for serotonin synthesis, thereby influencing serotonin availability in the brain [18].
Immune activation represents another critical pathway. Gut microbiota composition regulates the differentiation of pro-inflammatory T helper 17 (Th17) cells versus anti-inflammatory regulatory T cells (Tregs). These immune cells can traffic to the CNS, influencing neuroinflammation in conditions like multiple sclerosis [36].
Experimental Models and Methodologies
Research on the GBA employs sophisticated models to elucidate causal mechanisms:
- Germ-Free (GF) Animals: Mice raised without any microorganisms provide a controlled system to study microbiota contributions to neurodevelopment and behavior. Colonization of GF mice with specific microbiota reveals microbial influences on stress responses, neurotransmitter levels, and brain-derived neurotrophic factor (BDNF) [18].
- Gnotobiotic Models: Animals colonized with defined microbial communities allow reductionist studies of specific host-microbe interactions. A landmark Drosophila melanogaster study with all 32 combinations of five core bacterial species revealed that microbial interactions shape host fitness through life history tradeoffs [37].
- Chemical and Genetic Manipulation: Antibiotic-induced microbiota depletion, fecal microbiota transplantation (FMT), and genetically engineered bacterial strains enable functional studies of microbial contributions to brain function and behavior.
Table 1: Key Microbial Metabolites in Gut-Brain Communication
| Metabolite | Primary Producers | Receptors/Targets | Neurological Effects |
|---|---|---|---|
| Short-chain fatty acids (SCFAs) | Bacteroides, Firmicutes | GPCRs (GPR41, GPR43, GPR109a), HDACs | Enhance blood-brain barrier integrity, regulate microglia homeostasis, influence neuroinflammation |
| Tryptophan metabolites | Lactobacillus, Bifidobacterium | Aryl hydrocarbon receptor (AhR) | Regulate astrocyte activity, influence neuroinflammation, precursor for serotonin synthesis |
| Secondary bile acids | Bacteroides, Clostridium | Farnesoid X receptor (FXR), TGR5 | Modulate neuroinflammation, influence blood-brain barrier function |
| GABA | Lactobacillus, Bifidobacterium | GABAâ‚ and GABAâ‚ receptors | Primary inhibitory neurotransmitter in CNS; microbial production may influence anxiety-related behaviors |
The Gut-Lung Axis
Mechanisms of Cross-Talk
The gut-lung axis represents a bidirectional communication network wherein gut microbiota influences respiratory immunity and function, while lung inflammation can reciprocally affect gut homeostasis. This axis operates primarily through immune cell trafficking and microbial metabolite distribution [38].
Key mechanisms include:
- Immune Cell Priming: Gut microbiota shapes the development and function of mucosal-associated immune tissues (MALT). Dendritic cells sample gut microbiota and migrate to mesenteric lymph nodes where they initiate immune responses; subsequently, primed immune cells travel to distant mucosal sites, including the lungs [38].
- Metabolite Signaling: SCFAs produced by gut microbiota enter circulation and influence lung immunity by regulating neutrophil and macrophage function, inhibiting HDACs, and promoting regulatory T-cell differentiation [38].
- Systemic Inflammation: Gut barrier dysfunction permits translocation of microbial products into circulation, potentially triggering low-grade systemic inflammation that compromises pulmonary function [38].
Implications for Respiratory Health
The gut microbiota plays a particularly crucial role in early-life immune programming that establishes lifelong respiratory health trajectories. Children with asthma demonstrate distinct gut microbiota compositions, with reduced abundance of Lachnospira, Veillonella, Faecalibacterium, and Rothia, alongside disordered SCFA profiles [38]. This dysbiosis before age three correlates with increased asthma risk, highlighting the developmental window of vulnerability.
In respiratory infections, gut microbiota influences host defense mechanisms. Antibiotic-induced dysbiosis exacerbates severity of influenza and respiratory syncytial virus (RSV) infections by impairing adaptive immune responses, including antibody production and T cell-mediated immunity [38].
Table 2: Gut-Lung Axis in Respiratory Diseases
| Respiratory Condition | Gut Microbiota Alterations | Key Mechanisms | Systemic Consequences |
|---|---|---|---|
| Asthma | Reduced Lachnospira, Veillonella, Faecalibacterium, Rothia; Decreased SCFA production | Imbalanced Th1/Th2 response; Impaired Treg differentiation; Altered B cell immunity | Increased airway hyperresponsiveness; Enhanced allergic inflammation |
| COPD | Reduced microbial diversity; Altered Firmicutes/Bacteroidetes ratio | Systemic inflammation; Increased circulating LPS; Impaired macrophage function | Accelerated lung function decline; Increased exacerbation frequency |
| RSV Infection | Increased Clostridiales; Specific pathogen abundance correlates with severity | Altered T cell priming; Modified antiviral immunity; Reduced IgA production | More severe lower respiratory symptoms; Prolonged viral shedding |
| COVID-19 | Depleted beneficial commensals; Enriched opportunistic pathogens | Systemic immune dysregulation; Impaired interferon response; Gut barrier disruption | Increased disease severity; Prolonged post-acute symptoms |
Experimental Approaches
Research methodologies for studying the gut-lung axis include:
- Antibiotic Manipulation: Specific pathogen-free (SPF) mice treated with antibiotics exhibit altered susceptibility to respiratory pathogens and allergens, demonstrating gut microbiota's role in pulmonary immunity [38].
- Microbiota Transplantation: FMT from diseased to germ-free animals tests causal relationships between gut microbiota and respiratory phenotypes.
- Metabolite Supplementation: Direct administration of SCFAs or other microbial metabolites evaluates their protective effects against respiratory inflammation and infection [38].
The Oral-Systemic Axis
Oral-Gut Connection
The oral cavity harbors the second most diverse microbial community after the gut, with an estimated 700+ bacterial species. The oral-gut axis represents a direct pathway through which oral microbes influence systemic health. Individuals with periodontitis may swallow up to 10â¹-10¹Ⱐbacterial cells daily, presenting a substantial microbial load to the gastrointestinal tract [35].
Oral pathobionts, including Porphyromonas gingivalis and Fusobacterium nucleatum, can survive gastric transit and colonize the gut, disrupting intestinal barrier function and promoting inflammation [35]. These bacteria employ specific virulence mechanisms:
- Fusobacterium nucleatum expresses FadA adhesin, which binds E-cadherin on colonic epithelial cells, activating β-catenin signaling to drive tumor proliferation [35].
- Porphyromonas gingivalis decreases expression of tight junction proteins (ZO-1, occludin), altering intestinal barrier integrity and promoting systemic endotoxemia [35].
Systemic Disease Connections
Oral microbiota dysbiosis has been linked to numerous systemic conditions through multiple pathways:
- Cardiovascular Disease: Oral bacteria can directly infect atherosclerotic plaques or generate pro-inflammatory mediators that accelerate atherosclerosis. Microbial metabolites like trimethylamine-N-oxide (TMAO) produced by dysbiotic gut microbiota also contribute to cardiovascular pathology [35].
- Colorectal Cancer: Fusobacterium nucleatum is frequently detected in colorectal carcinoma tissue, where it promotes tumor progression through Fap2 protein-mediated immune evasion by binding to TIGIT on natural killer cells and T cells [35].
- Inflammatory Bowel Disease: Ectopic gut colonization by oral bacteria such as Haemophilus parainfluenzae and Klebsiella species induces Th1 and Th17 immune responses that exacerbate intestinal inflammation [35] [39].
- Neurodegenerative Diseases: Oral administration of P. gingivalis in murine models exacerbates Parkinsonian pathology and cognitive impairment through gut permeability disruption and neuroinflammation [35].
Integrated Experimental Approaches
Methodologies for Studying Microbial Axes
Advanced methodological approaches enable comprehensive investigation of host-microbiome interactions across systemic axes:
- Multi-omics Integration: Combining metagenomics (microbial community DNA), metatranscriptomics (gene expression), metabolomics (metabolite profiling), and host transcriptomics provides systems-level understanding of functional interactions [40].
- Gnotobiotic Models: Animals colonized with defined human microbial communities allow controlled studies of specific host-microbe and microbe-microbe interactions [37].
- Barrier Integrity Assessment: Techniques including FITC-dextran permeability, transepithelial electrical resistance (TEER), and tight junction protein immunostaining quantify gut and blood-brain barrier function.
- Immune Profiling: Flow cytometry, cytokine arrays, and single-cell RNA sequencing characterize local and systemic immune responses to microbial perturbations.
Table 3: Essential Research Reagents for Microbial Axis Studies
| Reagent/Category | Specific Examples | Research Applications | Key Functions |
|---|---|---|---|
| Gnotobiotic Models | Germ-free mice; Defined flora mice; Drosophila with 5-core species | Causal studies of microbial influence; Reductionist community interactions | Controlled microbial exposure; Elimination of confounding variables |
| Bacterial Strains | Lactobacillus plantarum; Bacteroides fragilis; Segmented filamentous bacteria | Probiotic studies; Mechanism exploration; Immune modulation research | Specific microbial functions; Immune cell differentiation; Barrier enhancement |
| Molecular Tools | 16S rRNA sequencing; Shotgun metagenomics; RNA-seq; Metabolomics | Community profiling; Functional potential assessment; Metabolic pathway analysis | Microbial identification; Gene expression; Metabolite quantification |
| Barrier Assessment | FITC-dextran; TEER measurements; Antibodies to ZO-1, occludin | Permeability studies; Tight junction integrity evaluation | Quantification of barrier function; Localization of junction proteins |
| Immune Monitoring | Flow cytometry panels; Cytokine ELISA/MSD; TLR agonists/antagonists | Immune cell population analysis; Inflammatory response quantification | Immune profiling; Pathway activation studies |
Visualization and Data Analysis
Complex host-microbiome datasets require advanced analytical and visualization approaches:
- Network Analysis: Correlation networks integrate microbial abundances, metabolite levels, and host gene expression to identify interaction modules [40].
- Longitudinal Modeling: Time-series analyses capture dynamic relationships between microbial shifts and physiological outcomes.
- Spatial Mapping: Techniques like fluorescence in situ hybridization (FISH) visualize microbial localization within tissues.
Therapeutic Implications and Future Directions
Microbiota-Targeted Interventions
Understanding microbial axes opens innovative therapeutic avenues for systemic diseases:
- Probiotics and Prebiotics: Selective microbial strains and growth substrates designed to restore beneficial communities and metabolite production [18] [36].
- Fecal Microbiota Transplantation: Transfer of entire microbial communities from healthy donors shows promise for conditions like IBD and is being investigated for neurological applications [36].
- Postbiotics: Administration of beneficial microbial metabolites (e.g., SCFA supplements) bypasses the need for live microorganisms [18] [38].
- Barrier-Strengthening Strategies: Compounds that enhance tight junction function may reduce systemic inflammatory burden from axis dysregulation [18].
Challenges and Opportunities
Several challenges remain in translating axis biology to clinical applications:
- Inter-individual Variability: Personalized approaches accounting for host genetics, baseline microbiota, and environmental exposures will be essential for therapeutic success [40].
- Causality Establishment: Most human evidence remains correlative; sophisticated experimental models are needed to establish mechanistic links.
- Biomarker Development: Identifying reliable biomarkers for axis dysfunction will enable early intervention and patient stratification [36].
Future research should prioritize multi-omics integration, longitudinal human cohorts, and mechanistic studies to clarify causal relationships along these systemic axes. The development of microbiota-directed therapeutics represents a paradigm shift in managing complex systemic diseases, offering potential for personalized interventions that address underlying pathophysiology rather than just symptoms.
The gut-brain, gut-lung, and oral-systemic axes represent fundamental communication networks that integrate distant organ systems through microbial, immune, neural, and metabolic signaling. Dysregulation of these axes contributes to the pathogenesis of diverse conditions spanning neurological, respiratory, gastrointestinal, and metabolic diseases. Understanding these complex interactions enables a more holistic perspective on human physiology and pathology, emphasizing that organs function not in isolation but as interconnected components of a supraorganism. As research methodologies advance and therapeutic applications emerge, targeting these microbial axes offers transformative potential for developing innovative, personalized approaches to prevent and treat systemic diseases.
Advanced Models and Multi-Omic Technologies for Deciphering Host-Microbe Dynamics
The Integrative Human Microbiome Project (iHMP or HMP2) represents a paradigm shift in human microbiome research, moving beyond foundational cataloging to dynamic, multi-omic analysis of host-microbiome interactions in health and disease. This whitepaper synthesizes core findings and methodologies from this landmark initiative. Through longitudinal multi-omic profiling, the iHMP has generated unprecedented insights into the complex interplay between the human host and its microbiota during three model conditions: pregnancy and preterm birth, inflammatory bowel disease, and the onset of prediabetes. We detail the experimental protocols, key data resources, and analytical frameworks that enable a mechanistic understanding of host-microbe dynamics. The project establishes a new standard for integrative biology, providing a foundational resource for researchers and drug development professionals aiming to decode microbiome-mediated mechanisms and identify novel therapeutic targets.
The National Institutes of Health (NIH) launched the Human Microbiome Project (HMP) in 2007 with the primary goal of establishing a comprehensive reference dataset of the microbial communities found in and on the human body [41]. This first phase (HMP1) revealed that the taxonomic composition of the microbiome alone was often a poor correlate of host phenotype, which was better predicted by prevalent microbial molecular function or personalized strain-specific makeup [41]. This critical finding necessitated a more holistic approach.
The second phase, the Integrative Human Microbiome Project (iHMP), was thus conceived to explore host-microbiome interplay by analyzing both microbiome and host activities in longitudinal studies of disease-specific cohorts [42]. The project was founded on the hypothesis that a multi-omic approach—simultaneously measuring multiple layers of molecular information over time—is essential to elucidate the mechanisms underlying host-microbe interactions in health and disease [41] [42]. The iHMP focused on three dynamic models of human conditions: pregnancy and preterm birth (PTB); inflammatory bowel diseases (IBD); and stressors that affect individuals with prediabetes [41]. These studies provide a framework for understanding how microbiome dynamics contribute to complex human diseases, offering a roadmap for future precision medicine initiatives.
Core Study Cohorts and Multi-Omic Data Landscape
The iHMP was structured around three longitudinal cohorts, each designed to investigate host-microbiome dynamics during critical periods of physiological change or disease activity. The scale and depth of data generation across these cohorts represent a significant leap forward in microbiome science.
Table 1: Overview of iHMP Core Longitudinal Cohorts
| Cohort (Model Condition) | Cohort Size & Design | Primary Biospecimens Collected | Key Clinical/ Phenotypic Outcomes |
|---|---|---|---|
| Pregnancy & Preterm Birth (PTB) | 1,527 women followed longitudinally through pregnancy; 12,039 samples from 597 pregnancies analyzed in-depth [41] | Maternal vaginal, buccal, rectal, skin, and blood samples; infant cord blood, meconium, and stool [41] [42] | Term birth vs. spontaneous preterm birth (<37 weeks gestation) [41] |
| Inflammatory Bowel Disease (IBD) | >100 individuals with Crohn's disease or ulcerative colitis, and non-IBD controls, followed for up to one year [41] [43] | Stool, blood, and intestinal biopsy samples [41] [42] | Disease flare vs. remission states [41] [44] |
| Prediabetes / Type 2 Diabetes Onset | Individuals with and without prediabetes followed for up to 4 years [43] [42] | Stool, anterior nares swabs, blood (PBMCs, plasma), and urine [42] | Insulin resistance status; progression to type 2 diabetes [45] [43] |
Table 2: Multi-Omic Data Types Generated by the iHMP
| Omics Layer | Measured Molecules | Example Analytical Method | Primary Repository |
|---|---|---|---|
| Microbiome Composition | 16S rRNA gene, Whole metagenome shotgun sequences | Metagenomic phylogenetic analysis | SRA [42] |
| Microbiome Function | Microbial RNA (Metatranscriptome), Proteins (Metaproteome), Metabolites | LC-MS/MS, Metatranscriptome sequencing | EBI PRIDE, SRA, Metabolomics Workbench [42] [46] |
| Host Genomics & Transcriptomics | Host exome/whole genome, Host RNA transcripts | Whole transcriptome sequencing, Genotyping arrays | dbGaP, GEO [42] [46] |
| Host Immune & Proteomic Response | Cytokines, Host proteins, Serum antibodies | LC-MS/MS, Immunoassays | EBI PRIDE, Study-specific DB [42] |
| Integrated Host-Microbe Profiling | Global metabolite and lipid profiles | Untargeted and targeted LC-MS | Metabolomics Workbench [42] |
Project Architecture and Data Integration
The following diagram illustrates the integrative design and flow of data generation in the iHMP:
Key Mechanistic Insights into Host-Microbiome Interactions
Vaginal Microbiome Dynamics in Pregnancy and Preterm Birth
The Multi-Omic Microbiome Study: Pregnancy Initiative (MOMS-PI) revealed that the vaginal microbiome undergoes predictable, structured changes during pregnancy. A key finding was that women with full-term pregnancies often showed a convergence towards a more homogeneous, Lactobacillus-dominated microbiome by the second trimester, even if they began pregnancy with a microbiome of greater ecological complexity [41]. This trend was most pronounced in women of African ancestry with lower socioeconomic profiles [41].
Crucially, the study identified specific microbial and host signatures associated with a higher risk for spontaneous preterm birth (PTB):
- Microbial Taxa: Women who experienced PTB were less likely to have a vaginal microbiome dominated by Lactobacillus crispatus and were more likely to have an increased abundance of Sneathia amnii, Prevotella-related clades, BVAB1 (Lachnospiraceae), and TM7-H1 (Saccharibacteria) [41].
- Host Response: These PTB-associated taxa were positively correlated with elevated vaginal pro-inflammatory cytokines, including IL-1β, IL-6, MIP-1β, and eotaxin-1 [41].
- Clinical Utility: The most distinct microbial signatures of PTB were observed early in pregnancy (before 24 weeks), enabling the development of preliminary predictive models for PTB risk [41].
Gut Microbiome Ecosystem in Inflammatory Bowel Disease
The IBD Multi'omics Database (IBDMDB) provided an unparalleled view of the gut ecosystem in Crohn's disease and ulcerative colitis. The project confirmed known dysbiosis patterns, such as reduced microbial diversity and depletion of commensal bacteria like Faecalibacterium prausnitzii and Roseburia intestinalis [43] [44]. More importantly, it extended these findings through functional multi-omics.
- Microbial Gene Expression: A landmark discovery was the identification of a "dormant" gut microbiota in IBD, where certain highly abundant bacteria showed low transcriptional activity [44]. Conversely, some taxa like Ruminococcus gnavus exhibited RNA levels three times higher than their DNA abundance, indicating that small compositional changes can have outsized functional impacts [44].
- Host-Microbe Metabolic Cross-Talk: Integrated analysis revealed microbial functional shifts, including disruptions in microbial butyrate production and bile acid metabolism, which were linked to host inflammatory responses [43] [44].
- Microbial Genetic Variation: Investigation of microbial genomic architecture revealed that single nucleotide variants (SNVs) in specific species like F. prausnitzii could more accurately distinguish IBD from other diseases than taxonomic abundance alone, highlighting the potential of strain-level genetics for diagnostics [44].
Systemic Host-Microbe Dynamics in Prediabetes
Longitudinal multi-omic profiling of individuals with prediabetes revealed that microbiome stability is intimately linked to host metabolic status. A key finding was that insulin-resistant individuals exhibited altered microbiome stability and disrupted correlations between microbiome features and host molecular markers [45]. This suggests a breakdown in the normal dialogue between host and microbiota in metabolic disease.
The study also provided insights into the personalization of host-microbe interactions:
- Individual-Specific Dynamics: The stability of the microbiome was found to be highly body-site specific and individualized. Stool and oral microbiomes were more stable than skin and nasal microbiomes [45].
- Coordinated Systemic Dynamics: Microbiome dynamics were correlated across body sites, suggesting the influence of systemic host factors on all resident microbial communities [45].
- Multi-omic Triggers: Integration of host transcriptomics, metabolomics, and proteomics with microbiome data identified specific host pathways and microbial metabolites associated with metabolic deterioration, offering potential targets for intervention [43].
Experimental Protocols and Methodologies
The iHMP established rigorous, standardized protocols for longitudinal multi-omic studies. The following workflow details the core experimental pipeline used across the consortium.
Integrated Multi-Omic Workflow
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagents and Computational Tools for Multi-Omic Microbiome Studies
| Category | Reagent / Tool | Specific Function in iHMP | Application Context |
|---|---|---|---|
| Sequencing Platforms | Illumina Sequencing Systems | High-throughput generation of 16S, metagenomic, metatranscriptomic, and host transcriptomic data [42] [46] | All omics layers involving nucleic acids |
| Mass Spectrometry | LC-MS/MS (Liquid Chromatography with Tandem Mass Spectrometry) | Untargeted and targeted profiling of metabolites, lipids, and proteins from host and microbiome [42] [46] | Metaproteomics, metabolomics, lipidomics |
| Reference Databases | HMP Reference Strain Collection (ATCC/BEI) | Repository of bacterial isolates for functional validation and genomic comparison [42] | Strain-specific analysis and culture-based experiments |
| Computational Tools | HUMAnN2 (The HMP Unified Metabolic Analysis Network 2) | Species-level functional profiling of metagenomic and metatranscriptomic data [43] [46] | Inference of microbial community metabolic pathways |
| Computational Tools | Qiita Web Platform | Rapid, web-enabled microbiome meta-analysis of standardized multi-omic data [43] | Data integration and cross-study comparison |
| Data Repositories | HMP Data Coordination Center (DCC) | Centralized portal for accessing iHMP data, protocols, and analytical resources [41] [43] | Data retrieval and study replication |
| Sikokianin E | Sikokianin E, MF:C42H42O22, MW:898.8 g/mol | Chemical Reagent | Bench Chemicals |
| Acetylsventenic acid | Acetylsventenic Acid|High-Purity Research Chemical | Acetylsventenic Acid is a high-purity chemical for research use only (RUO). Explore its applications and value for scientific investigation. Not for human consumption. | Bench Chemicals |
Discussion and Future Perspectives
The Integrative Human Microbiome Project has successfully created a new paradigm for studying host-associated microbial communities. By moving beyond static compositional analysis to dynamic, multi-omic profiling, the project has begun to elucidate the mechanisms that govern host-microbiome interactions in health and disease. The key legacy of the iHMP is not merely the vast data resources it has generated, but the demonstration that only through integrated, longitudinal studies can the functional interplay between host and microbiota be decoded.
The findings from the three cohort studies share common themes that will guide future research:
- Temporal Dynamics are Crucial: Microbial community composition is volatile, but functional and metabolic outputs follow more predictable temporal patterns that are deeply intertwined with host physiology [41] [45] [44].
- Personalization is Paramount: Host factors, including genetics, immune status, and life history, create a unique ecological niche that shapes an individual's microbiome, influencing its stability and response to perturbation [45] [44].
- Mechanism Requires Integration: Disruptions in health states, from preterm birth to IBD to insulin resistance, are reflected not in a single omic layer, but in the discordance between multiple layers of host and microbial molecular data [41] [45] [44].
For the research community and drug development professionals, the iHMP provides a template and a rich resource. The protocols, data standards, and analytical tools developed by the consortium lower the barrier for future large-scale integrative studies. The insights into specific microbial functions, host pathways, and their dynamic interplay offer a new landscape of potential therapeutic targets. Future research must build upon this foundation, prioritizing even larger and more diverse cohorts, refining single-cell and spatial multi-omic technologies, and developing more sophisticated computational models to truly predict and modulate the host-microbiome interface for improving human health.
The intricate relationship between host organisms and their microbiota is a cornerstone of modern biomedical research, influencing fields from immunology to neurobiology. Preclinical models that allow for controlled manipulation of the microbiome are indispensable for advancing our understanding of host-microbe interactions in health and disease. Germ-free (GF) animals and human microbiota-associated (HMA) models represent two powerful, complementary approaches for establishing causal relationships and elucidating underlying mechanisms. These models have evolved beyond simple tools for association studies to become sophisticated platforms for decoding complex host-microbiome signaling pathways, testing therapeutic interventions, and developing personalized medicine approaches. This technical guide examines the foundational principles, methodological considerations, and cutting-edge applications of these model systems, providing researchers with a comprehensive framework for their implementation in microbiome research.
Germ-Free Animal Models
Fundamental Principles and Derivation
Germ-free animals are raised in completely sterile isolators and lack all detectable microorganisms, including bacteria, viruses, fungi, and archaea [47]. This axenic state creates a "clean slate" that enables researchers to study host physiology in the absence of microbial influence or to introduce specific microbial communities under controlled conditions. GF animals belong to a broader category of gnotobiotic animals (from the Greek "gnotos" for known and "bios" for life), in which every microorganism present is defined and known to the researcher [47].
The derivation of GF mice is technically demanding and can be achieved through two primary methods: cesarean delivery or in vitro fertilization (IVF) followed by embryo transfer [47]. IVF is considered the preferred method as it significantly reduces the risk of microbial contamination from pathogens that can cross the placental barrier, such as Lymphocytic Choriomeningitis Virus (LCMV) or Pasteurella pneumotropica [47]. Following derivation, GF animals are maintained in tightly controlled and monitored isolators with strict husbandry protocols and rigorous testing regimens to confirm the germ-free status.
Table 1: Key Characteristics of Germ-Free Animals
| Characteristic | Description |
|---|---|
| Microbial Status | Completely devoid of all microorganisms (axenic) |
| Housing Requirements | Tightly controlled isolators with rigorous monitoring |
| Derivation Methods | Cesarean delivery or in vitro fertilization (IVF) with embryo transfer |
| Confirmation Methods | Microbial culturing and molecular detection techniques |
| Related Models | Gnotobiotic animals (associated with defined microbial communities) |
Research Applications and Therapeutic Areas
The complete absence of microorganisms makes GF animals invaluable for establishing causal relationships between microbes and host phenotypes. Research applications span multiple therapeutic areas:
- Immunology: GF animals exhibit underdeveloped immune systems, including reduced Peyer's patches, smaller mesenteric lymph nodes, and altered T-cell populations, making them ideal for studying immune development and function [47].
- Metabolism: The metabolic contributions of microbes can be quantified by comparing GF animals with conventionalized counterparts, particularly in studies of energy harvest, obesity, and metabolic syndrome [47].
- Gastroenterology: GF models enable precise studies of gut barrier function, epithelial turnover, and digestive processes without microbial interference [47].
- Neuroscience: The gut-brain axis can be investigated by colonizing GF animals with specific microbes and measuring neurological outcomes [47].
- Oncology: The impact of microbes on cancer development, progression, and therapy response can be determined using GF models [47] [48].
- Drug Discovery: GF animals help researchers understand how drug responses are modulated by the microbiome and develop strategies to target the microbiome therapeutically [47].
Human Microbiota-Associated (HMA) Models
Conceptual Framework and Establishment
Human microbiota-associated (HMA) models are created by transplanting human-derived microbial communities into recipient germ-free or antibiotic-treated animals. These models have become indispensable tools for investigating microbe-host interactions and disease pathogenesis by allowing researchers to study human-relevant microbiota in a controlled experimental system [49] [50]. The successful establishment of HMA models involves multiple critical stages: donor screening, fecal suspension preparation, recipient preparation, and fecal microbiota transplantation (FMT) with subsequent engraftment validation [49].
The conceptual foundation of HMA models rests on evidence demonstrating that they can effectively reconstruct donor microbial signatures and metabolomic profiles [49]. Current applications span four key research domains: (1) composition of gut microbial consortia, (2) regulation of gut microbiota in host development, (3) causal associations between microbes and diseases, and (4) evaluation of targeted microbiota therapeutic strategies [49].
Methodological Standardization
Donor Screening and Selection
Standardized protocols for selecting human fecal donors are crucial for experimental reproducibility. Current HMA models predominantly use two donor cohorts: healthy individuals and patients with specific diseases under investigation [49]. Established inclusion criteria for healthy donors typically include:
- Minimum of 2-12 months without antibiotic exposure [49]
- Elimination of laxative agents for ≥3 months [49]
- Omnivorous diet including both vegetarian and meat components [49]
- Absence of gastrointestinal disorders, recent pathogen infections, and acute or chronic illnesses that alter gut microbe composition [49]
Common exclusion criteria include recent exposure to antimicrobials, prebiotics, or probiotics; active neuropsychiatric disorders; excessive alcoholism or smoking habits; and pregnancy or lactation [49]. For disease donors, additional requirements include clinical manifestations, laboratory tests, and pathological findings that satisfy diagnostic criteria for the specific condition [49].
Recipient Preparation and FMT Protocols
The most commonly used recipients for HMA modeling include germ-free animals and pseudo-germ-free animals generated through antibiotic-mediated microbiota depletion [49] [50]. Although FMT with a single gavage of fecal suspension can establish the model, multiple frequencies and longer FMT durations significantly improve donor microbiota colonization efficiency [49].
Fecal samples should be processed as soon as possible after collection in anaerobic environments, with suitable protectants added if preservation at low temperatures is necessary [49]. Microbial community profiling via 16S rRNA gene sequencing represents the primary method for analyzing microbiome composition and verifying microbiota engraftment efficacy throughout FMT procedures [49] [50].
Advanced Model Systems and Recent Innovations
Wildling Models with Natural Microbiota
Conventional specific pathogen-free (SPF) laboratory mice harbor microbiota that lack the complexity and resilience of naturally co-evolved microbial communities, contributing to irreproducibility in biomedical research [51]. To address this limitation, researchers have developed "wildling" models by transplanting natural gut microbiota from wild mice into laboratory mice. These TXwildling models adopt structural and functional wildling-like microbiota and host physiology toward a more mature immune system with characteristics similar to adult humans [51].
Wildling microbiota demonstrate superior ecological fitness, outcompeting conventional lab microbiota despite numerical disadvantages [51]. These models also transfer non-bacterial microorganisms (fungi, viruses) and develop pathogen experiences crucial for immune system education [51]. The wildling approach represents a significant advancement for improving reproducibility and translational success in preclinical research.
Animal-Free Miniature Gut Models
The GuMI platform is an innovative animal-free miniature gut system that creates a microenvironment supporting both anaerobic bacteria and human epithelial cells [52]. This device features two compartments with an oxygen-poor environment for bacteria and an oxygenated environment for human cells, with controlled conditions for nutrients and pH [52].
Current applications include testing probiotics and investigating how probiotic products can boost immunity [52]. Future applications may incorporate immune cells to study immune development, particularly in inflammatory bowel diseases, and enable personalized treatments by using patient tissue to understand differential therapy responses [52].
Table 2: Comparison of Preclinical Model Systems for Microbiome Research
| Model System | Key Features | Advantages | Limitations |
|---|---|---|---|
| Germ-Free Animals | Axenic; no microorganisms | Clean slate for establishing causality; controlled microbial introduction | Altered physiology; technically demanding and expensive |
| HMA Models | Human microbiota in gnotobiotic animals | Human-relevant microbiota; study host-microbe interactions in vivo | Potential loss of some human microbes; host filter effects |
| Wildling Models | Natural mouse microbiota in lab mice | Complex, resilient microbiota; improved immune maturation | Requires specialized derivation; potential pathogen transfer |
| GuMI Platform | Microphysiological system with human cells | Animal-free; human cells; controlled oxygen gradient | Doesn't fully capture in vivo complexity; limited community diversity |
Experimental Design and Methodologies
HMA Model Generation Workflow
The following diagram illustrates the standardized workflow for generating HMA models:
Host Signaling Pathways Modulated by Microbiome
Microbial components and metabolites significantly influence host cellular functions by modulating diverse intracellular signaling pathways. The following diagram illustrates key host signaling pathways influenced by the microbiome:
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Microbiome Model Systems
| Reagent/Resource | Function/Application | Key Considerations |
|---|---|---|
| Germ-Free Mice | Provide microbiome-free baseline for studies; recipients for microbial transplantation | Source consistently (commercial providers preferred); verify germ-free status regularly [47] |
| Defined Microbial Communities | Create gnotobiotic models with specific microbial functions | Select communities based on research questions; consider synthetic vs. natural communities |
| Anaerobic Chambers | Maintain oxygen-sensitive bacteria during sample processing | Essential for preserving viability of anaerobic microbes during fecal processing [49] |
| Cryopreservation Solutions | Protect microbial viability during frozen storage | Include suitable protectants for optimal microbial survival [49] |
| 16S rRNA Sequencing Kits | Analyze microbiome composition and verify engraftment | Primary method for community analysis; consider shotgun metagenomics for functional insights [49] |
| Gnotobiotic Isolators | Maintain defined microbial status in animal models | Required for long-term maintenance of gnotobiotic animals [47] |
| Antibiotic Cocktails | Create pseudo-germ-free animals for HMA studies | Use specific regimens to deplete endogenous microbiota without excessive host toxicity [49] |
| Xanthevodine | Xanthevodine, CAS:477-78-1, MF:C16H13NO5, MW:299.28 g/mol | Chemical Reagent |
| Schisanlignone C | Schisanlignone C, MF:C23H26O7, MW:414.4 g/mol | Chemical Reagent |
Applications in Host-Microbiome Interaction Research
Mechanistic Insights into Disease Pathogenesis
HMA and GF models have provided fundamental insights into how microbes contribute to disease pathogenesis across multiple systems:
- Inflammatory Bowel Disease: HMA models have revealed how specific pathogens like Porphyromonas gingivalis aggravate colitis through gut microbiota-linoleic acid metabolism-Th17/Treg cell balance axis disruption [48].
- Cancer: Microbiome studies in GF models have uncovered mechanisms by which microbiota influence cancer progression and therapy response, including the role of specific microbial metabolites in modulating treatment efficacy [53] [48].
- Metabolic Disorders: HMA models have demonstrated causal relationships between gut microbiota and conditions like obesity and type 2 diabetes, revealing how microbial metabolites influence host metabolism [49] [54].
- Neurological Disorders: GF models have been instrumental in elucidating gut-brain axis communications, showing how microbiota influence neurodevelopment, behavior, and neurodegenerative processes [54].
Therapeutic Development and Screening
These model systems are increasingly used in drug discovery and therapeutic development:
- Live Biotherapeutic Products: GF and HMA models provide essential platforms for testing efficacy and safety of microbiome-based therapeutics [55].
- Microbiome-Mediated Drug Metabolism: GF models help identify how microbial metabolism influences drug efficacy and toxicity [47].
- Fecal Microbiota Transplantation: HMA models enable mechanistic studies of FMT action and optimization of protocols for various conditions [49] [50].
- Personalized Medicine Approaches: HMA models created with patient-derived microbiota can help predict individual treatment responses and guide therapeutic decisions [52].
Germ-free animals and human microbiota-associated models represent sophisticated experimental platforms that have dramatically advanced our understanding of host-microbiome interactions in health and disease. The continued refinement of these models, including the development of wildling models with natural microbiota and innovative animal-free systems like the GuMI platform, addresses critical challenges in reproducibility and translational relevance. As these technologies evolve, they will increasingly enable researchers to decode the molecular mechanisms underlying microbiome-host communication, develop targeted therapeutic interventions, and ultimately realize the promise of personalized microbiome medicine. The integration of these model systems with multi-omics technologies and advanced computational approaches will further accelerate discoveries in this rapidly advancing field.
The study of host-microbiome interactions represents a frontier in understanding human health and disease, yet has long been constrained by the limitations of traditional experimental systems. Two-dimensional cell cultures fail to replicate the three-dimensional architecture and cellular complexity of human tissues, while animal models exhibit fundamental differences in microbiome composition and host response that limit their translational relevance [56]. This technological gap has impeded progress across numerous fields, from inflammatory bowel disease and colorectal cancer to periodontal disease and systemic inflammatory conditions.
The emergence of sophisticated in vitro platforms has begun to bridge this critical gap. Organoids, organs-on-chips, and engineered tissue models now enable researchers to recapitulate key aspects of human physiology with unprecedented fidelity. These systems share a common principle: recreating the essential functional units of human organs in miniature form, complete with tissue-specific architecture, cellular diversity, and physiologically relevant microenvironments [57] [58]. Within the specific context of host-microbiome research, these platforms provide the necessary complexity to study the dynamic, multi-directional interactions between human cells and microbial communities that were previously impossible to model in vitro.
The significance of these advances extends beyond basic science to therapeutic development. By capturing patient-specific biology, these platforms enable personalized investigation of disease mechanisms and treatment responses [59]. Furthermore, they allow for the controlled manipulation of individual variables within the host-microbiome interface, facilitating mechanistic studies that can establish causality rather than merely correlation. This technical guide explores the fundamental principles, methodological considerations, and research applications of three transformative platforms that are reshaping host-microbiome research: organoids, gut-on-a-chip systems, and physiologically relevant gingival tissue models.
Organoid Technology: Bridging the Gap Between Cell Culture and Physiology
Fundamental Principles and Classification
Organoids are three-dimensional, self-organizing micro-organ structures generated in vitro from stem cells that recapitulate the functional and structural characteristics of native tissues [58]. The foundation of modern organoid technology rests on harnessing the innate self-renewal and differentiation capabilities of stem cells—either adult stem cells (ASCs) isolated from tissue biopsies or pluripotent stem cells (PSCs)—and guiding their development through precisely controlled microenvironmental cues [59]. These cues include biochemical signals from growth factors and cytokines, biomechanical signals from the extracellular matrix (ECM), and in more advanced systems, fluid flow and mechanical stress.
Intestinal organoids, among the most well-established systems, demonstrate the remarkable capabilities of this technology. They develop polarized epithelial layers with crypt-villus architecture containing multiple functionally differentiated cell subtypes, including enterocytes, goblet cells, Paneth cells, and enteroendocrine cells [59]. This cellular diversity emerges through self-organization processes that mirror intestinal development in vivo, resulting in structures that exhibit region-specific functions such as nutrient absorption, mucus secretion, and barrier integrity.
The classification of organoid systems reflects their diverse applications in host-microbiome research:
- Patient-derived organoids (PDOs): Generated from patient tissue biopsies, PDOs retain the genetic and phenotypic heterogeneity of the original tumor or diseased tissue, making them particularly valuable for personalized medicine applications and studying patient-specific disease mechanisms [59].
- Adult stem cell-derived organoids: These models excel at recapitulating normal intestinal development and host-microbe interactions, forming 3D structures with authentic crypt-villus architecture and containing multiple epithelial cell subtypes [59].
- Multi-cell/microbe co-culture organoids: By incorporating immune cells, microbiota, or microbial metabolites, these advanced systems better mimic the microbial-immune crosstalk characteristic of in vivo microenvironments [59].
Table 1: Classification and Applications of Intestinal Organoid Systems in Host-Microbiome Research
| Organoid Type | Key Features | Primary Applications in Host-Microbiome Research | Notable Limitations |
|---|---|---|---|
| Patient-derived Organoids (PDOs) | Retain genetic and phenotypic heterogeneity of original tumor; support co-culture with microbiota | Individualized drug sensitivity testing; studies of tumor heterogeneity and carcinogenic mechanisms; personalized host-microbe interaction studies | Limited tumor microenvironment components (e.g., lack of immune/stromal components); high cost |
| Adult Stem Cell-derived Organoids | Form 3D structures with crypt-villus architecture; include multiple epithelial cell subtypes | Research on intestinal barrier function; microbial colonization; inflammation and repair mechanisms; normal host-microbe interactions | Limited ability to simulate disease-specific mutations and complex tissue dynamics |
| Multi-cell/Microbe Co-culture Organoids | Incorporate immune cells, microbiota, or microbial metabolites (e.g., SCFAs, bile acids) | Immune regulation studies; immunotherapy response mechanisms; microbial metabolite function evaluation; trans-kingdom interactions | Technically complex; microbial community stability challenging to maintain long-term |
| Organ-on-a-Chip Integrated Models | Combine microfluidics with organoids to simulate fluid flow, mechanical forces, and microbial gradients | Simulating peristalsis and metabolic gradients; bacterial invasion and host response; drug toxicity/pharmacokinetics; microbiome dynamics | High technical threshold; not yet widely adopted; relatively expensive |
Methodological Framework: Culture Systems and Matrix Considerations
The establishment of physiologically relevant organoid cultures requires careful attention to both the biochemical and biophysical microenvironment. The extracellular matrix (ECM) serves as a critical instructive component, providing not merely structural support but also essential biochemical and mechanotransduction cues that guide organoid development and function [58].
Matrix Selection and Optimization: Multiple matrix platforms have been developed for gastrointestinal organoid culture, each with distinct advantages and limitations:
- Basement membrane extracts (BME): Materials like Matrigel, Cultrex, and Geltrex, derived from mouse sarcoma cells, represent the most widely used matrices for organoid culture [58]. These BMEs contain a complex mixture of ECM proteins, including laminin, collagen IV, and entactin, along with growth factors that support organoid formation and growth. While versatile and commercially accessible, BMEs suffer from batch-to-batch variability, undefined composition, and limited control over mechanical properties.
- Decellularized ECM hydrogels: Derived from native tissues, these matrices offer tissue-specific biochemical composition that may better recapitulate the native microenvironment [58]. However, they also present challenges in standardization and may contain residual cellular material.
- Defined natural protein hydrogels: Composed of purified ECM components such as collagen, fibrin, or alginate, these systems provide greater control over composition and mechanical properties while maintaining biological relevance [58].
- Synthetic polymer hydrogels: Fully defined systems such as polyethylene glycol (PEG)-based hydrogels offer precise control over mechanical properties and biochemical functionalization but may lack innate bioactivity [58].
The mechanical properties of the matrix, including stiffness, viscoelasticity, and degradability, profoundly influence organoid behavior through mechanotransduction pathways. Matrix stiffness, for instance, activates integrin signaling and focal adhesion assembly, driving YAP/TAZ nuclear translocation and subsequent transcriptional responses that influence cell proliferation, differentiation, and function [58].
Media Formulations and Differentiation: Organoid media must provide appropriate niche signals to maintain stemness or promote differentiation along specific lineages. Typical intestinal organoid media include a base medium supplemented with essential niche factors such as:
- Wnt agonists (e.g., R-spondin-1, Wnt-3a) to support stem cell maintenance
- EGF to promote proliferation
- Noggin to inhibit BMP signaling and enable crypt formation
- Other tissue-specific factors such as FGF, Nodal, or various small molecules depending on the target cell types
For host-microbiome interaction studies, differentiation protocols often aim to enhance barrier function and the presence of specific cell types involved in host-microbe interactions, such as goblet cells for mucus production or Paneth cells for antimicrobial peptide secretion.
Diagram 1: Organoid Generation Workflow
Applications in Host-Microbiome Interaction Research
Organoids have enabled significant advances in understanding host-microbiome interactions, particularly in the context of gastrointestinal health and disease. Their application spans multiple research domains:
Modeling Host-Microbe Dynamics: Intestinal organoids provide a unique platform for studying the complex relationships between host epithelial cells and commensal or pathogenic microorganisms. Through microinjection into the organoid lumen or co-culture in specialized systems, researchers can introduce defined microbial communities or individual bacterial strains to investigate diverse biological processes, including microbial colonization, barrier function, antimicrobial peptide production, and immune activation [59]. The ability to maintain organoids in a controlled, sterile environment prior to intentional microbial introduction enables precise manipulation of variables that is impossible in in vivo systems.
Cancer Microbiome Research: Organoids have emerged as transformative tools for investigating the role of tumor-associated microbes in cancer initiation, progression, and therapeutic response. Patient-derived tumor organoids retain the genetic and phenotypic characteristics of the original tumors while allowing for manipulation of associated microbial communities [59]. This capability has enabled researchers to dissect how specific microbes or microbial communities influence carcinogenic processes, modulate the tumor immune microenvironment, and affect responses to chemotherapeutic agents and immunotherapies.
Personalized Medicine Approaches: The capacity to generate organoid biobanks from multiple patients, including those with different disease subtypes or treatment histories, facilitates the investigation of inter-individual variation in host-microbiome interactions [59]. These biobanks enable high-throughput screening of microbial metabolites, therapeutic compounds, or personalized microbial consortia to identify patient-specific responses, laying the foundation for precision medicine approaches that account for an individual's unique microbiome and tissue characteristics.
Gut-on-a-Chip Systems: Introducing Physiological Dynamics
Core Principles and Design Considerations
Gut-on-a-chip technology represents a significant evolution beyond static organoid cultures by incorporating critical physiological dynamics typically absent in traditional systems. These microfluidic devices, typically about the size of a USB stick, contain hollow microchannels lined with living human cells through which fluids continuously flow, recreating conditions that mimic blood circulation, peristalsis-like motions, and other physical stresses present in the gastrointestinal tract [57].
The fundamental innovation of gut-on-a-chip systems lies in their ability to replicate the dynamic mechanical environment of the human gut. Unlike static cultures where cells exist in a largely unchanging environment, cells in gut-on-a-chip devices experience fluid shear stresses, cyclic strain, and mechanical compression that profoundly influence their differentiation, function, and response to external stimuli [57]. This dynamic environment more accurately mirrors the in vivo situation where intestinal epithelial cells are continuously exposed to flowing luminal contents, peristaltic movements, and interactions with vascular and immune components.
Advanced gut-on-a-chip platforms incorporate multiple parallel channels separated by porous membranes, enabling co-culture of different cell types in compartmentalized but interacting microenvironments. A typical configuration might include an upper "intestinal lumen" channel lined with epithelial cells and a lower "vascular" channel lined with endothelial cells, with the two compartments separated by a permeable membrane that allows for molecular exchange and cellular crosstalk [57]. This design facilitates the study of complex processes such as nutrient absorption, immune cell trafficking, and host-microbe interactions in a physiologically relevant context.
Protocol for Establishing a Gut-on-a-Chip System
The development of a functional gut-on-a-chip model involves a multi-step process that integrates cells, materials, and fluidic systems to recreate intestinal physiology:
Step 1: Device Fabrication and Preparation
- Microfluidic devices are typically fabricated from transparent, biocompatible polymers such as polydimethylsiloxane (PDMS) using soft lithography techniques
- The device architecture includes at least two parallel microchannels separated by a porous polyester or PDMS membrane (0.2-10 μm pore size)
- Prior to cell culture, devices may be sterilized (ethanol, UV irradiation, or autoclaving) and coated with extracellular matrix proteins (collagen IV, fibronectin) to promote cell adhesion
Step 2: Cell Seeding and Differentiation
- Intestinal epithelial cells (either cell lines, primary cells, or pre-differentiated organoids) are introduced into the upper channel
- Endothelial cells (e.g., HUVECs or human intestinal microvascular endothelial cells) are seeded in the lower channel to recreate the vascular interface
- Cells are allowed to adhere and form confluent monolayers under static conditions (24-48 hours)
- Epithelial cells are stimulated to differentiate through appropriate cytokine and growth factor exposure
Step 3: System Operation and Conditioning
- Once confluent, fluid flow is initiated using precision syringe or peristaltic pumps
- Lumenal flow rates are typically calibrated to produce physiological shear stresses (0.02-0.1 dyne/cm²)
- Peristalsis-like mechanical deformation may be introduced through cyclic suction applied to side chambers (10% strain, 0.15 Hz frequency)
- Culture medium is circulated through the vascular channel to simulate blood flow
Step 4: Introduction of Microbiome Components
- Commensal or pathogenic bacteria can be introduced into the luminal channel at physiologically relevant densities (10â·-10⸠CFU/mL)
- The continuous flow helps maintain microbial populations while preventing overgrowth
- Sampling ports allow for periodic collection of effluents for analysis of microbial composition, metabolite production, and host factor secretion
The Jalili lab's gut-on-a-chip platform demonstrates the capabilities of this technology, where intestinal epithelial cells form finger-like villi structures and secrete mucus, recreating key features of the intestinal barrier [57]. When bacterial communities are introduced, they colonize the mucus layer in a pattern reminiscent of in vivo colonization, and added immune cells actively migrate toward bacteria during infection, mimicking the surveillance and defense mechanisms of the human gut.
Research Applications in Host-Microbiome Interactions
Gut-on-a-chip systems enable investigation of host-microbiome interactions with unprecedented physiological relevance. Specific applications include:
Real-Time Observation of Host-Microbe-Immune Interactions: The transparency of microfluidic devices allows for direct, real-time visualization of cellular behaviors and interactions. Researchers can observe immune cell migration, bacterial colonization patterns, and epithelial responses as they unfold, providing dynamic information that static systems cannot capture [57]. Fluorescent labeling of specific cell types or bacteria further enhances the ability to track these interactions.
Investigation of Barrier Function and Pathogen Invasion: The presence of fluid flow and mechanical strain promotes the development of robust epithelial barriers with well-formed tight junctions and physiological permeability. This enables more relevant studies of how commensal microbes reinforce barrier function and how pathogens compromise it. The system allows for continuous monitoring of barrier integrity through transepithelial electrical resistance (TEER) measurements and tracer flux assays.
Microbiome-Metabolite Interactions: The continuous flow in gut-on-a-chip systems facilitates the study of microbial metabolite production, absorption, and systemic effects. Metabolites produced by microbes in the luminal channel can be transported across the epithelial barrier and detected in the vascular channel, mimicking their entry into systemic circulation [57]. This capability is particularly valuable for investigating how microbiome-derived metabolites influence host physiology and disease processes.
Table 2: Quantitative Parameters for Gut-on-a-Chip Systems in Host-Microbiome Research
| Parameter Category | Specific Parameters | Typical Values/Ranges | Physiological Relevance |
|---|---|---|---|
| Fluid Dynamics | Luminal flow rate | 30-500 μL/hour | Mimics fluid movement in intestinal lumen |
| Shear stress | 0.02-0.1 dyne/cm² | Represents physiological shear on epithelial surface | |
| Vascular flow rate | 100-1000 μL/hour | Simulates blood flow in capillaries | |
| Mechanical Properties | Peristalsis-like deformation | 0.15 Hz, 10% strain | Recapitulates intestinal motility |
| Membrane pore size | 0.4-3.0 μm | Allows molecular transport and immune cell migration | |
| Cell Culture Conditions | Epithelial cell density | 1-5×10ⶠcells/mL | Ensures formation of confluent monolayer |
| Microbial inoculation density | 10â·-10⸠CFU/mL | Represents physiological microbial loads | |
| TEER values | 150-300 Ω×cm² | Indicates formation of functional barrier | |
| Analysis Timeframes | Short-term responses | Minutes to hours | Acute immune signaling, barrier disruption |
| Medium-term interactions | 1-3 days | Microbial colonization, stable co-culture | |
| Long-term studies | 5+ days | Chronic inflammation, microbiome evolution |
Physiologically Relevant Gingival Tissue Models: Recapitulating the Oral Microenvironment
Architectural and Functional Requirements
The development of physiologically relevant gingival models addresses a critical gap in oral microbiome research, where traditional systems have failed to capture the complexity of the periodontal niche. The gingiva presents unique challenges for in vitro modeling, including its stratified epithelial structure, continuous exposure to salivary flow, and the presence of both shedding and non-shedding surfaces that support distinct microbial communities [56]. Successfully recapitulating this environment requires attention to multiple architectural and functional parameters.
A key advancement in gingival tissue engineering has been the recognition that three-dimensional architecture is not merely a structural consideration but a functional imperative. The development of physiological oxygen gradients within the model is particularly critical, as oxygen tension varies significantly from the superficial to deep regions of the periodontal pocket and plays a determinative role in shaping microbial community composition and host cell behavior [56]. Models that incorporate these gradients successfully support the coexistence of aerobic, facultative anaerobic, and obligate anaerobic bacteria that characterize the native oral microbiome.
The incorporation of dynamic salivary flow represents another essential element often missing from traditional models. Saliva provides not only moisture and nutrients but also contains antimicrobial factors, buffers pH fluctuations, and generates mechanical shear forces that influence both host tissue and microbial communities [56]. The non-Newtonian rheological properties of saliva, including its shear-thinning behavior and viscoelasticity, further contribute to its functional role and must be considered in model development.
Experimental Protocol for Gingival Tissue Model
The establishment of a physiologically relevant gingival tissue model involves a multi-step process that integrates appropriate biomaterials, primary human cells, and dynamic culture conditions:
Step 1: Scaffold Fabrication
- Scaffolds are fabricated from natural proteins such as silk fibroin, which provides appropriate mechanical properties and biocompatibility
- The scaffold architecture is designed to replicate the cyto-architecture and oxygen profile of human gingiva, typically featuring a porous structure that supports cell infiltration and nutrient diffusion
- Scaffolds may be functionalized with cell adhesion motifs (e.g., RGD sequences) to enhance cell attachment
Step 2: Cell Seeding and Tissue Maturation
- Primary human gingival epithelial cells and fibroblasts are isolated from tissue biopsies or obtained from commercial sources
- Cells are seeded in a stratified manner: fibroblasts first into the deeper scaffold regions, followed by epithelial cells on the surface
- Constructs are cultured under static conditions for 3-7 days to allow initial cell attachment and proliferation
- Tissue maturation is promoted through air-liquid interface culture, which enhances epithelial stratification and differentiation
Step 3: Integration into Bioreactor System
- Matured tissue constructs are transferred to custom-designed bioreactors capable of simulating salivary flow
- The bioreactor design includes precise control over inlet position, flow velocity, and vorticity to replicate physiological shear stress (typically 0.5-5 dyne/cm²)
- Saliva-mimicking medium is circulated through the system, with composition reflecting the ionic profile, viscosity, and non-Newtonian behavior of human saliva
Step 4: Microbiome Inoculation and Monitoring
- Subgingival plaque samples collected from healthy donors or patients are inoculated into the model's periodontal pocket region
- Microbial viability and composition are monitored over time using flow cytometry, viability staining, and 16S rRNA sequencing
- Host responses are assessed through measurement of antimicrobial peptide secretion (e.g., hBD2), cytokine profiling, and histological analysis of barrier integrity
This protocol has supported the investigation of host-microbiome interactions in healthy conditions within a human oral tissue model for up to seven days—a significant advancement over previous systems that typically supported co-culture for only 24 hours [56]. The long-term viability of both host tissue and microbial communities enables investigation of progressive changes in host-microbe relationships that more closely mirror in vivo dynamics.
Research Applications in Oral-Systemic Health
Advanced gingival models provide unprecedented opportunities to investigate the relationship between oral microbiome dynamics and both local and systemic health outcomes:
Periodontal Disease Pathogenesis: These models enable detailed investigation of the transition from healthy symbiotic relationships to dysbiotic states characteristic of periodontal disease. Researchers can track how specific changes in microbial composition, host immune responses, or environmental factors disrupt homeostasis and drive disease progression [56]. The ability to sequentially sample both host and microbial factors over time provides dynamic information about disease trajectories that is difficult to obtain from clinical studies.
Oral-Systemic Disease Connections: The gingival model offers a platform for investigating mechanistic links between oral health and systemic conditions such as inflammatory bowel disease, rheumatoid arthritis, and Alzheimer's disease [56]. By monitoring the production of inflammatory mediators, bacterial translocation, and tissue barrier function, researchers can identify potential pathways through which oral dysbiosis might influence distant disease processes.
Therapeutic Testing and Intervention Strategies: The system supports evaluation of antimicrobial agents, probiotics, anti-inflammatory compounds, and other therapeutic interventions under physiologically relevant conditions. For example, the model has been used to simulate oral hygiene regimens, including rinsing with commercial mouthwash, to assess their effects on both microbial communities and host tissue [56]. This application is particularly valuable for screening potential therapies before advancing to costly clinical trials.
Diagram 2: Gingival Tissue Model Workflow
Comparative Analysis and Integration of Platforms
Technical Capabilities and Limitations
Each platform offers distinct advantages and suffers from particular limitations that make them suitable for different research applications. Understanding these trade-offs is essential for selecting the appropriate system for specific research questions in host-microbiome science.
Organoids excel in capturing tissue-specific cellular heterogeneity and patient-specific biology, making them ideal for studying developmental processes, disease mechanisms, and personalized therapeutic responses [59] [58]. Their ability to be expanded and biobanked enables high-throughput applications such as drug screening. However, organoids typically lack key elements of the native tissue microenvironment, including vascularization, immune components, and physiological mechanical forces. Additionally, their closed, spherical architecture can present challenges for microbial access and experimental manipulation.
Gut-on-a-chip systems address many of these limitations by incorporating fluid flow, mechanical stress, and multi-cellular interactions [57]. The dynamic environment promotes enhanced epithelial barrier function, cellular differentiation, and more physiologically relevant host responses to microbial challenges. The ability to directly observe and manipulate interactions in real time provides a significant advantage for mechanistic studies. However, these systems are technically complex, require specialized equipment and expertise, and can be lower-throughput than traditional organoid cultures.
Gingival tissue models demonstrate the importance of tissue-specific architectural and environmental factors in maintaining host-microbiome homeostasis [56] [60]. The incorporation of salivary flow, oxygen gradients, and appropriate scaffold materials enables long-term co-culture of complex microbial communities with host tissue—a challenge that has proven difficult in many other systems. The main limitations include the specialized nature of the platform, which may limit broad adoption, and the focus on a specific tissue type.
Integrated Approaches and Future Directions
The most physiologically relevant models often combine elements from multiple platforms to overcome individual limitations. Integrated approaches that leverage the strengths of different systems represent the future of in vitro modeling for host-microbiome research.
Organoid-on-Chip Systems: Combining organoids with microfluidic technology creates systems that benefit from both the cellular complexity of organoids and the physiological dynamics of chip-based platforms [59]. In these integrated systems, organoids are incorporated into microfluidic devices where they experience fluid flow, mechanical forces, and interactions with other cell types such as endothelial cells or immune cells. This approach enhances organoid maturation and function while enabling more controlled study of host-microbe interactions.
Multi-Organ Systems: Linking different organ models through microfluidic networks creates multi-organ systems that can investigate systemic effects of host-microbiome interactions. For example, connecting gut models with liver, brain, or other tissue models allows researchers to study how microbiome-derived metabolites or inflammatory factors produced in one tissue may influence distant organs [57]. These systems are particularly valuable for understanding the systemic consequences of oral or intestinal dysbiosis.
Advanced Analytical Integration: All platforms benefit from integration with sophisticated analytical approaches, including multi-omics technologies (genomics, transcriptomics, metabolomics), high-resolution imaging, and computational modeling. The combination of physiologically relevant models with these powerful analytical tools enables comprehensive characterization of host-microbiome interactions across multiple biological scales, from molecular mechanisms to tissue-level phenotypes [59].
Table 3: Essential Research Reagents for Advanced In Vitro Platforms
| Reagent Category | Specific Examples | Function in Host-Microbiome Research | Considerations for Selection |
|---|---|---|---|
| Matrices/Scaffolds | Matrigel, Cultrex BME, Silk fibroin, Collagen, Fibrin, Synthetic PEG hydrogels | Provide 3D structural support; present biochemical and mechanical cues to cells | Batch-to-batch variability (BME); tissue-specific composition; mechanical properties; degradability |
| Cell Sources | Intestinal organoids from adult stem cells, Primary gingival epithelial cells/fibroblasts, Endothelial cells (HUVECs), Immune cells (PBMCs, macrophages) | Recreate tissue-specific cellular composition and patient-specific biology | Donor variability; expansion capability; functional characterization; ethical considerations |
| Microbiome Components | Patient-derived stool or plaque samples, Defined microbial communities, Individual bacterial strains, Microbial metabolites (SCFAs, bile acids) | Introduce relevant microbial partners for interaction studies | Viability maintenance; community stability; physiological relevance; safety considerations |
| Culture Media Components | Wnt agonists (R-spondin), Noggin, EGF, Tissue-specific cytokines, Saliva-mimicking solutions, Blood-mimicking solutions | Support cell viability and function; recreate physiological fluid composition | Optimization required for specific applications; defined vs. undefined formulations; cost |
| Analysis Tools | TEER electrodes, Metabolic assays (LDH, MTT), Cytokine arrays, 16S rRNA sequencing, Metabolomics platforms, Live-cell imaging dyes | Assess host and microbial responses; characterize interaction outcomes | Sensitivity; throughput; multiplexing capability; compatibility with platform materials |
The development of innovative in vitro platforms—including organoids, gut-on-a-chip systems, and physiologically relevant gingival models—represents a paradigm shift in our ability to study host-microbiome interactions under controlled yet physiologically relevant conditions. Each platform offers unique capabilities that address different limitations of traditional systems, enabling researchers to investigate complex biological questions that were previously intractable.
These advanced models share a common emphasis on recapitulating key aspects of native tissue environments, including three-dimensional architecture, cellular heterogeneity, dynamic fluid flow, and mechanical forces. This physiological fidelity enhances the translational relevance of findings and provides greater confidence in extrapolating results to human biology and disease. Furthermore, the ability to incorporate patient-derived cells and microbiomes enables personalized approaches to investigating disease mechanisms and therapeutic responses.
As these technologies continue to evolve and become more widely adopted, they promise to accelerate our understanding of the critical relationships between human hosts and their microbial partners. This knowledge will undoubtedly yield new insights into disease pathogenesis and novel therapeutic strategies for conditions ranging from inflammatory bowel disease and colorectal cancer to periodontal disease and systemic inflammatory disorders. The integration of these platforms with advanced analytical technologies and computational approaches will further enhance their power, ultimately contributing to the development of more effective, personalized approaches to maintaining health and treating disease.
The study of host-microbiome interactions has been revolutionized by the integration of multi-omics approaches, which provide a comprehensive framework for understanding the molecular mechanisms governing health and disease states. Metagenomics, metabolomics, and proteomics each contribute unique layers of biological information that, when integrated, offer unprecedented insights into the complex dialogue between host and microbiome. Metagenomics enables the characterization of microbial community structure and functional potential, metabolomics provides a snapshot of the biochemical outputs and small molecule metabolites, while proteomics reveals the functional proteins executing cellular processes [61] [62]. This multi-dimensional perspective is essential for advancing beyond correlation to establishing causal relationships in microbiome-associated diseases, thereby enabling the discovery of robust diagnostic biomarkers and therapeutic targets [63] [48].
The challenge in biomarker discovery lies not only in identification but in validation and clinical translation. Despite the publication of thousands of potential biomarkers, very few have been approved for clinical use [63]. This highlights the critical need for systematic, evidence-based approaches that prioritize biological consistency and clinical utility. The National Cancer Institute's Early Detection Research Network (EDRN) has established a five-phase roadmap for biomarker development that emphasizes prospective specimen collection and retrospective blinded evaluation (PROBE design) to ensure rigorous validation [63]. Within this framework, multi-omics data provides the foundational evidence for selecting the most promising biomarker candidates based on both statistical significance and biological relevance.
Metagenomic Biomarker Discovery
Analytical Approaches and Tools
Metagenomic biomarker discovery focuses on identifying microbial taxa, genes, or pathways whose relative abundances consistently differentiate between biological states, such as health and disease. The analytical landscape for metagenomic biomarker discovery encompasses both statistical and machine learning approaches, each with distinct strengths for handling the high-dimensionality and compositional nature of microbiome data [61] [64].
LEfSe (Linear Discriminant Analysis Effect Size) is a widely used algorithm that couples statistical significance tests with biological consistency and effect size estimation [61]. It first uses the non-parametric factorial Kruskal-Wallis sum-rank test to identify features with significant differential abundance, followed by pairwise Wilcoxon tests to assess biological consistency across subcategories. Finally, LDA is employed to estimate the effect size of each differentially abundant feature, ranking them by biological relevance [61]. This approach is particularly valuable for its ability to detect biomarkers that are statistically significant, biologically consistent, and have meaningful effect sizes.
For enhanced reproducibility, Regularized Low Rank-Sparse Decomposition (RegLRSD) formulates biomarker discovery as a matrix decomposition problem [64]. This algorithm models bacterial abundance data as the superposition of a sparse matrix (representing differentially abundant microbes) and a low-rank matrix (representing non-differentially abundant microbes). By incorporating prior knowledge that non-informative microbes do not exhibit significant variation, RegLRSD improves consistency across studies—a critical consideration for clinical translation [64].
Table 1: Key Computational Tools for Metagenomic Biomarker Discovery
| Tool | Methodology | Key Features | Applications |
|---|---|---|---|
| LEfSe | Statistical testing + LDA effect size | Identifies features with both statistical significance and biological consistency; Provides effect size estimation | Human microbiome body site differentiation; Disease vs. healthy comparisons [61] |
| RegLRSD | Regularized low-rank sparse matrix decomposition | Models microbial abundance as sparse + low-rank matrices; Improves reproducibility; Accounts for inter-microbe dependencies | Robust biomarker identification in inflammatory bowel disease, obesity [64] |
| METASTATS | Permutation t-test + Fisher's exact test | Handles sparse and non-sparse features; Addresses multiple comparisons with FDR correction | Comparative analysis of microbial communities across phenotypes [64] |
Experimental Workflow and Protocols
A standardized metagenomic biomarker discovery workflow begins with sample collection from relevant sources (stool, saliva, skin swabs), followed by DNA extraction and sequencing using either 16S rRNA gene amplicon or whole-genome shotgun approaches. Bioinformatic processing includes quality filtering, denoising, and clustering into operational taxonomic units (OTUs) or amplicon sequence variants (ASVs) [65]. The resulting feature tables then undergo statistical analysis to identify differentially abundant taxa.
For LEfSe analysis, the protocol involves: (1) Formatting input data with class labels and subclasses; (2) Running the non-parametric factorial Kruskal-Wallis test to identify features with significant differential abundance (p < 0.05); (3) Performing pairwise Wilcoxon tests among subclasses to ensure biological consistency; (4) Applying LDA to estimate effect size and rank biomarkers; (5) Visualizing results on taxonomic trees or cladograms [61]. The biological consistency step is particularly crucial as it ensures that identified biomarkers show consistent patterns across biologically relevant subcategories within the main classes being compared.
For the RegLRSD algorithm, the implementation involves: (1) Constructing a bacterial abundance matrix D ∈ ℜ^(p×n) where p represents OTUs and n represents samples; (2) Decomposing D into low-rank (L) and sparse (S) matrices through optimization: minimize rank(L) + λ∥S∥₀ subject to D = L + S; (3) Applying regularization to enforce smoothness in the low-rank component; (4) Extracting biomarkers from the sparse matrix S [64]. This convex optimization formulation ensures global optimality and efficient computation while maintaining interpretability of results in the original feature domain.
Figure 1: Metagenomic Biomarker Discovery Workflow. The process begins with sample collection and proceeds through DNA extraction, sequencing, bioinformatic processing, statistical analysis, and validation.
Metabolomic Biomarker Discovery
Technological Platforms and Analytical Strategies
Metabolomic biomarker discovery focuses on identifying small molecule metabolites (typically <1500 Da) that serve as downstream readouts of host and microbial metabolic activity. These metabolites include amino acids, lipids, organic acids, carbohydrates, and various exogenous compounds that reflect the functional state of biological systems [62]. Metabolomics offers a unique advantage over other omics approaches by providing the closest link to phenotypic expression and capturing the dynamic metabolic responses to pathophysiological stimuli [62].
The two primary analytical platforms for metabolomics are mass spectrometry (MS) and nuclear magnetic resonance (NMR) spectroscopy. MS-based approaches, particularly when coupled with liquid or gas chromatography (LC-MS/GC-MS), offer high sensitivity and the ability to detect thousands of metabolites simultaneously [62]. Recent advances in mass spectrometry imaging (MSI) enable spatial visualization of metabolite distributions within tissues, providing insights into localized metabolic processes [62]. NMR spectroscopy, while less sensitive than MS, provides robust quantitative analysis and structural elucidation capabilities, making it valuable for biomarker verification [62].
Metabolomic studies employ either untargeted or targeted approaches. Untargeted metabolomics aims to comprehensively measure all detectable metabolites in a sample, enabling hypothesis-free discovery of novel biomarkers [62]. Targeted metabolomics focuses on precise quantification of predefined metabolite panels, offering higher sensitivity and reproducibility for biomarker validation [62]. The integration of both approaches creates a powerful pipeline for biomarker discovery and verification.
Table 2: Metabolomic Biomarker Discovery Platforms and Applications
| Platform | Key Features | Advantages | Clinical Applications |
|---|---|---|---|
| LC-MS/GC-MS | High sensitivity and resolution; Wide metabolite coverage; Structural information via fragmentation | Capable of detecting thousands of metabolites; Compatible with diverse sample types | Discovery of diagnostic biomarkers for cancer, metabolic disorders, neurodegenerative diseases [62] |
| Mass Spectrometry Imaging (MSI) | Spatial resolution of metabolite distribution; Tissue localization information | Visualizes metabolic heterogeneity in tissues; Correlates metabolite patterns with histopathology | Tumor metabolism mapping; Drug distribution studies; Spatial metabolomics in host-microbiome interactions [62] |
| NMR Spectroscopy | Non-destructive; Quantitative; Structural elucidation | High reproducibility; Minimal sample preparation; Identifies novel metabolite structures | Biomarker classification for kidney diseases, cardiovascular diseases, Alzheimer's disease [62] |
Metabolite Biomarker Workflow
The standard workflow for metabolomic biomarker discovery begins with careful sample collection and preparation from biofluids (serum, plasma, urine) or tissues, followed by metabolite extraction using appropriate solvents. Samples are then analyzed using LC-MS, GC-MS, or NMR platforms, generating raw data that undergoes preprocessing including peak detection, alignment, and normalization [62]. Statistical analysis identifies differentially abundant metabolites, followed by structural identification and biological interpretation.
A critical consideration in metabolomic studies is the selection of biological matrix, as different biofluids provide complementary information. Serum and plasma offer systemic metabolic profiles, urine provides information on excretion and kidney function, while feces directly captures gut microbial metabolic activity [62]. For host-microbiome interaction studies, multi-matrix approaches are often necessary to distinguish host-derived from microbiome-derived metabolites.
For untargeted metabolomics, the protocol includes: (1) Sample preparation using protein precipitation with cold organic solvents; (2) LC-MS analysis in both positive and negative ionization modes; (3) Data preprocessing with peak picking, retention time alignment, and intensity normalization; (4) Multivariate statistical analysis (PCA, PLS-DA) to identify group separations; (5) Significance testing (t-tests, ANOVA) with multiple testing correction; (6) Metabolite identification using accurate mass, retention time, and fragmentation spectra; (7) Pathway analysis to determine biological context [62].
For targeted metabolomics, the approach involves: (1) Selection of candidate metabolites based on untargeted discovery or prior knowledge; (2) Development of optimized LC-MS/MS methods with multiple reaction monitoring (MRM); (3) Preparation of calibration curves with stable isotope-labeled internal standards; (4) Sample extraction and analysis with quality controls; (5) Absolute quantification using standard curves; (6) Statistical validation of biomarker performance [62].
Figure 2: Metabolomic Biomarker Discovery Workflow. The process encompasses sample preparation, analytical measurement, data processing, statistical analysis, metabolite identification, and biological interpretation.
Proteomic Biomarker Discovery
Mass Spectrometry-Based Proteomic Approaches
Proteomic biomarker discovery aims to identify proteins with differential expression between disease and healthy states, providing functional insights into disease mechanisms. Mass spectrometry-based proteomics has become the primary technology for protein biomarker discovery due to its ability to simultaneously quantify thousands of proteins across complex samples [66]. The proteomic biomarker pipeline follows a structured process involving discovery, verification, and validation phases, with different MS techniques employed at each stage [66].
In the discovery phase, shotgun proteomics using data-dependent acquisition (DDA) is typically employed for non-targeted relative quantification of proteins across a small number of samples (typically 10-20 per group) [66]. This approach uses liquid chromatography-tandem mass spectrometry (LC-MS/MS) to identify and quantify peptides, which serve as surrogates for protein inference. Various quantification strategies can be employed, including label-free methods (spectral counting, peak intensity) or isotopic labeling approaches (iTRAQ, TMT) [66]. The output is a list of candidate biomarker proteins with relative fold-changes between experimental conditions.
The verification phase assesses candidate biomarkers on larger sample sets (typically 50-100 samples) using targeted mass spectrometry approaches, most commonly multiple reaction monitoring (MRM) or parallel reaction monitoring (PRM) [66]. These methods provide high specificity and sensitivity by focusing MS resources on detecting specific peptides from candidate proteins. MRM assays monitor predefined precursor-to-fragment ion transitions, enabling precise quantification of target proteins with high reproducibility and dynamic range [66].
Table 3: Mass Spectrometry Approaches in the Proteomic Biomarker Pipeline
| Pipeline Stage | MS Approach | Sample Throughput | Key Characteristics | Applications |
|---|---|---|---|---|
| Discovery | Shotgun Proteomics (DDA) | Low (10-20 samples/group) | Relative quantification; Identifies thousands of proteins; Output as fold-changes | Initial biomarker screening; Pathway analysis; Hypothesis generation [66] |
| Verification | Multiple Reaction Monitoring (MRM) | Medium (50-100 samples) | Targeted quantification; High specificity and sensitivity; Absolute quantification possible | Candidate biomarker verification; Assay development; Clinical assay translation [66] |
| Validation | Immunoassays or Clinical MS | High (100-1000s samples) | High-throughput; Clinical grade precision; Regulatory compliance | Large-scale clinical validation; FDA approval studies; Companion diagnostic development [66] |
Proteomic Workflow and Experimental Design
A robust proteomic biomarker discovery workflow begins with sample preparation, including protein extraction, denaturation, reduction, alkylation, and digestion (typically with trypsin) to generate peptides. Following LC-MS/MS analysis, data processing involves database searching for protein identification and quantitative analysis to determine differential expression. Candidate biomarkers are then selected based on statistical significance and fold-change criteria for downstream verification.
For shotgun proteomics discovery, the protocol includes: (1) Protein extraction and quantification; (2) In-solution or in-gel digestion with trypsin; (3) Peptide cleanup and concentration measurement; (4) LC-MS/MS analysis with data-dependent acquisition; (5) Database searching using tools like MaxQuant, Proteome Discoverer, or SEQUEST; (6) Statistical analysis to identify differentially expressed proteins; (7) Bioinformatics analysis including pathway enrichment and protein interaction networks [66]. Quality control measures such as pool samples and technical replicates are essential throughout the process.
For targeted proteomics verification, the MRM assay development involves: (1) Selection of proteotypic peptides for candidate biomarkers; (2) Optimization of collision energies for each peptide; (3) Synthesis of stable isotope-labeled standard (SIS) peptides; (4) Method development with retention time scheduling; (5) Analysis of verification cohort samples; (6) Quantification using internal standard calibration curves; (7) Statistical assessment of biomarker performance [66]. The use of SIS peptides enables absolute quantification and improves measurement precision and accuracy.
A critical consideration in proteomic biomarker studies is the selection of biological matrix. While tissue samples provide direct information about disease processes, plasma and serum are more accessible for clinical translation. However, plasma proteomics presents challenges due to the extreme dynamic range of protein abundances, requiring depletion of high-abundance proteins or enrichment of low-abundance candidates [66].
Figure 3: Proteomic Biomarker Discovery Pipeline. The workflow progresses from sample preparation through discovery proteomics, candidate selection, verification, and clinical validation.
Integrating Multi-Omics for Causal Insights
Strategies for Multi-Omics Integration
The integration of metagenomics, metabolomics, and proteomics data provides a powerful approach for establishing causal relationships in host-microbiome interactions and moving beyond correlative associations. Integrative analysis can reveal how microbial genetic potential (metagenomics) translates into functional metabolic activities (metabolomics) and host responses (proteomics), creating a comprehensive mechanistic understanding of disease processes [48].
Several computational approaches enable multi-omics integration. Correlation-based networks identify statistical associations between features across different omics layers, revealing potential functional relationships between microbial taxa and host metabolites or proteins [65]. Multivariate methods such as multiple kernel learning or multi-block PLS can identify latent factors that capture co-variation patterns across omics datasets [65]. Pathway-based integration maps differentially abundant features from each omics layer onto biological pathways, revealing coordinated alterations in specific metabolic or signaling pathways [62] [48].
A compelling example of multi-omics integration comes from studies of Porphyromonas gingivalis and inflammatory bowel disease (IBD). Metagenomic analysis reveals colonization by this oral pathogen, metabolomics identifies alterations in linoleic acid metabolism, and proteomics/proteomics reveals shifts in Th17/Treg cell balance, collectively demonstrating a mechanistic pathway linking periodontal disease to intestinal inflammation [48]. Similarly, studies of Akkermansia muciniphila have used multi-omics approaches to reveal its effects on host immune function through metabolic modulation [48].
Establishing Causal Relationships
While correlative patterns from multi-omics data generate hypotheses, establishing causality requires additional experimental approaches. Mendelian randomization uses genetic variants as instrumental variables to infer causal relationships between exposures and outcomes, helping to determine whether specific microbial features or metabolites directly influence disease risk [62]. Microbial colonization experiments in gnotobiotic mice can directly test whether specific bacteria or bacterial communities recapitulate disease phenotypes and associated molecular changes [48]. Intervention studies with probiotics, prebiotics, or antibiotics can demonstrate reversibility and further support causal relationships [48].
The integration of multi-omics data also facilitates the distinction between driver and passenger effects in disease processes. Driver microorganisms or metabolites are those that actively contribute to disease pathogenesis, while passenger effects are secondary consequences of disease. Multi-omics longitudinal studies can help differentiate these by tracking the temporal sequence of molecular events during disease development and progression [63]. Experimental validation in model systems is then essential to confirm putative driver mechanisms.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents for Multi-Omics Biomarker Discovery
| Reagent/Material | Function | Application Notes |
|---|---|---|
| DNA Extraction Kits (Mobio, DNeasy) | Isolation of high-quality microbial DNA from complex samples | Critical for metagenomic studies; Must efficiently lyse diverse bacterial species; Should minimize host DNA contamination [61] [64] |
| Stable Isotope-Labeled Standards (SIS) | Internal standards for precise quantification | Essential for targeted proteomics and metabolomics; Enables absolute quantification; Corrects for matrix effects and recovery variations [62] [66] |
| Protein Depletion Columns | Removal of high-abundance proteins | Improves detection of low-abundance protein biomarkers in plasma/serum; Common targets: albumin, IgG; Can use immunoaffinity or chemical depletion [66] |
| Trypsin (Sequencing Grade) | Proteolytic digestion of proteins to peptides | Standard enzyme for bottom-up proteomics; Requires high purity and specificity; Modified trypsin prevents autolysis [66] |
| iTRAQ/TMT Labeling Reagents | Multiplexed isotopic labeling for relative quantification | Enables simultaneous analysis of multiple samples in single MS run; Reduces technical variability; 4-plex to 11-plex formats available [66] |
| C18 Solid-Phase Extraction Cartridges | Peptide and metabolite cleanup and concentration | Removes salts, detergents, and other interfering compounds; Desalting step before LC-MS analysis; Improves sensitivity and reproducibility [62] [66] |
| Quality Control Reference Materials | Monitoring analytical performance and reproducibility | Pooled quality control samples; Standard reference materials (NIST); Used to monitor instrument stability and data quality [62] [66] |
| Heteroclitin C | Heteroclitin C|Lignan Reference Standard | Heteroclitin C, a high-purity Kadsura lignan for research. Explore its bioactivities in anti-inflammatory and blood tonic studies. For Research Use Only. Not for human or diagnostic use. |
| 5-O-Methyllatifolin | 5-O-Methyllatifolin|RUO |
The integration of metagenomics, metabolomics, and proteomics provides a powerful framework for advancing biomarker discovery from correlation to causation in host-microbiome research. While each omics layer offers valuable insights independently, their integration reveals interconnected biological networks that more accurately reflect the complexity of host-microbe interactions. The future of biomarker discovery lies in developing more sophisticated computational methods for multi-omics integration, standardized protocols for cross-study validation, and advanced experimental systems for causal validation.
As the field progresses, several key challenges must be addressed: the need for standardized protocols and reporting standards across omics technologies, improved computational methods for integrating heterogeneous data types, and development of more sophisticated experimental models for establishing causality. Furthermore, the successful translation of multi-omics biomarkers to clinical practice will require close collaboration between basic researchers, clinical investigators, and regulatory scientists throughout the discovery and validation pipeline. By addressing these challenges, multi-omics approaches will continue to advance our understanding of host-microbiome interactions and deliver clinically valuable biomarkers for diagnosis, prognosis, and therapeutic monitoring.
The human microbiome, a complex ecosystem of trillions of microorganisms, constitutes a functional organ integral to host physiology, influencing everything from nutrient metabolism to immune system calibration. Disruption of this delicate ecological balance, known as dysbiosis, is increasingly recognized as a critical factor in the pathogenesis of a broad spectrum of diseases [67] [68]. This understanding has propelled the development of therapeutic strategies designed to modulate the microbiome to restore health. These interventions range from administering specific beneficial microbes to transplanting entire microbial communities. Within the framework of host-microbiome interactions, these therapies act by re-establishing homeostatic relationships between the host and its microbial inhabitants, influencing disease trajectories through immune, metabolic, and barrier function pathways [69]. The growing field of microbiome-based therapeutics, including probiotics, prebiotics, postbiotics, and Fecal Microbiota Transplantation (FMT), represents a paradigm shift in managing neoplastic, metabolic, autoimmune, and infectious diseases [67] [70] [71]. This review provides an in-depth technical analysis of these modalities, framed within the context of contemporary research on host-microbiome crosstalk.
Probiotics: Engineered Live Biotherapeutics
Definitions and Mechanisms of Action
Probiotics are defined by the FAO/WHO as "live microorganisms that confer a health benefit when administered in adequate amounts" [72] [69]. Originally dominated by strains of Lactobacillus, Bifidobacterium, and Saccharomyces, the category has expanded to include Next-Generation Probiotics (NGPs), which are investigated as live biotherapeutic drugs [72]. Their mechanisms of action are multifaceted and include:
- Immune Modulation: Probiotics regulate the host immune response by influencing T-cell differentiation and cytokine production, leading to enhanced anti-tumor immunity or suppressed inflammation [69].
- Pathogen Suppression: Through competitive exclusion, they inhibit the colonization and biofilm formation of pathogens [70].
- Intestinal Barrier Reinforcement: They contribute to the strengthening of the epithelial barrier, reducing intracellular pathogen invasion and systemic inflammation [69].
- Metabolic Regulation: Probiotics and their metabolites, such as short-chain fatty acids (SCFAs), directly impact tumor cell dynamics and host metabolism [69].
Advanced Engineering and Clinical Applications
Advances in synthetic biology have enabled the engineering of probiotics with novel, therapeutic-enhanced functions [67]. These engineered probiotics are being developed for diagnostic purposes and as targeted disease treatments. Bibliometric analysis of clinical applications reveals a significant and continuous growth in research, with hotspots focusing on diseases such as "inflammation", "obesity", "insulin resistance", "depression", "hyperlipidemia", and "cancer" [72]. In oncology, specific strains of Lactobacillus and Bifidobacterium demonstrate strain-specific antitumor potential, capable of inducing apoptosis in cancer cells and enhancing responses to checkpoint inhibitor immunotherapy [69].
Table 1: Clinical Research Focus Areas for Probiotics (2000-2025)
| Research Focus / Disease Area | Key Investigated Strains | Primary Mechanisms |
|---|---|---|
| Inflammation / IBD | Lactobacillus spp., Bifidobacterium spp. | Immune modulation, barrier reinforcement, pathogen inhibition [72] |
| Metabolic Health (Obesity, Insulin Resistance) | L. acidophilus, L. rhamnosus, B. longum | Metabolic regulation, SCFA production, anti-inflammatory effects [72] |
| Cancer | Engineered Lactobacillus, Bifidobacterium | Immune activation, carcinogen neutralization, apoptosis induction [67] [69] |
| Mental Health (Depression) | L. plantarum, B. breve | Gut-brain axis modulation, neurotransmitter production [72] |
| Infectious Diseases | Saccharomyces boulardii | Pathogen suppression, toxin neutralization [72] |
Experimental Protocol: Assessing Probiotic Engraftment and Function
Objective: To evaluate the engraftment and functional impact of a probiotic strain in a murine model of antibiotic-induced dysbiosis.
- Animal Model: C57BL/6 mice treated with a broad-spect antibiotic cocktail (e.g., ampicillin, vancomycin, neomycin) in drinking water for 1-2 weeks.
- Probiotic Administration: Orally gavage with a defined dose (e.g., 1x10^9 CFU) of the engineered probiotic strain daily for 7 days. Control groups receive a vehicle.
- Sample Collection: Collect fecal pellets at baseline, post-antibiotic treatment, and post-probiotic administration for microbial analysis. Sacrifice animals and collect colon, cecum, and blood samples.
- Metagenomic Analysis: Extract DNA from fecal and tissue samples. Perform shotgun metagenomic sequencing to track the relative abundance and strain-level engraftment of the administered probiotic. Bioinformatic tools like MAGEnTa can be used for efficient tracking of donor strains without relying on external databases [68].
- Functional Assessment: Quantify microbial metabolites (e.g., SCFAs) via mass spectrometry. Assess host immune response by measuring cytokine levels (e.g., IL-10, TNF-α) in serum and colon tissue using ELISA. Evaluate epithelial barrier integrity by measuring transepithelial electrical resistance (TEER) on colonoid cultures or by immunohistochemistry for tight junction proteins.
Figure 1: Workflow for evaluating probiotic engraftment and functional impact in a dysbiosis model.
Prebiotics and Synbiotics: Fueling a Healthy Microbiome
Classification and Mechanisms
Prebiotics are "non-digestible food components that selectively stimulate the growth and/or activity of beneficial gut microbes" [73]. They are categorized into:
- Traditional Prebiotics: Include inulin, fructooligosaccharides (FOS), galactooligosaccharides (GOS), and human milk oligosaccharides (HMOs).
- Emerging Prebiotics: Such as polyphenols [73].
Their primary mechanism involves selective fermentation by commensal bacteria like Bifidobacterium and Lactobacillus, leading to the production of health-promoting metabolites, most notably short-chain fatty acids (SCFAs) like acetate, propionate, and butyrate [73] [69]. These SCFAs serve as an energy source for colonocytes, strengthen the gut barrier, and exert systemic anti-inflammatory and immunomodulatory effects. The combination of probiotics and prebiotics is termed synbiotics, which are designed to improve the survival and engraftment of the beneficial microbes [73] [69].
Technological Innovations and Health Applications
Recent advancements in prebiotic research include innovations in formulation technologies such as microencapsulation, which enhances the stability and targeted delivery of prebiotics and synbiotics [73]. Clinical evidence supports the role of prebiotics in promoting digestive, metabolic, immune, and mental health. In the context of cancer, prebiotics help shape a microbiota that supports antitumor immunity and can reduce therapy-related toxicities [69]. The field is increasingly moving towards personalized nutrition, recognizing that interindividual microbiome differences dictate the efficacy of specific prebiotics [73].
Table 2: Classification and Health Applications of Prebiotics
| Prebiotic Category | Examples | Key Health Applications | Proposed Mechanisms |
|---|---|---|---|
| Oligosaccharides | FOS, GOS, XOS, HMOs | Metabolic health, immune support | Selective stimulation of bifidobacteria; SCFA production; pathogen exclusion [73] [69] |
| Polysaccharides | Inulin, Resistant Starch | Digestive health, glycemic control | Increased microbial diversity; enhanced gut barrier function; GLP-1 secretion [73] |
| Emerging Prebiotics | Polyphenols | Cardiometabolic health, anti-inflammatory | Modulation of microbial ecology; production of bioactive postbiotics (e.g., urolithins) [73] |
Experimental Protocol: Evaluating Prebiotic Selectivity and Metabolic Output
Objective: To determine the selectivity of a prebiotic compound for beneficial microbes and its subsequent metabolic profile in vitro.
- Culture Setup: Inoculate an anaerobic bioreactor with a defined human gut microbial community or a complex fecal slurry from a healthy donor.
- Prebiotic Supplementation: Supplement the culture medium with the test prebiotic (e.g., XOS) at a physiological concentration. Controls include a no-carbon-source baseline and a glucose-positive control.
- Microbial Composition Analysis: Monitor the microbial community dynamics over 24-48 hours using 16S rRNA gene amplicon sequencing or flow cytometry. Calculate the Prebiotic Index (increase in beneficial bacteria relative to total bacteria).
- Metabolomic Profiling: Collect supernatant samples at multiple time points. Analyze SCFA production (butyrate, acetate, propionate) using Gas Chromatography-Mass Spectrometry (GC-MS). Quantify other relevant microbial metabolites like branched-chain fatty acids or polyphenol-derived compounds.
- Data Integration: Integrate microbial abundance data with metabolite concentrations to construct correlation networks and identify key producer-consumer relationships within the community.
Postbiotics: Non-viable Microbial Therapeutics
Definition and Therapeutic Advantages
Postbiotics are a "preparation of inanimate microorganisms and/or their components that confer a health benefit on the host" [70]. This category includes cell-free supernatants, microbial cell fragments, and purified metabolites like SCFAs, exopolysaccharides, and enzymes. Their key advantages over live probiotics include:
- Enhanced Safety: Eliminating the risk of bacterial translocation or gene transfer, particularly crucial for immunocompromised patients.
- Improved Stability and Shelf-life: Easier storage and transportation.
- Dose Precision: Allows for precise standardization and dosing of the active component [70].
Mechanisms and Application in Wound Healing
Postbiotics mimic the beneficial effects of live probiotics by restoring a healthy microbiome through pathogen inhibition and immune regulation [70]. Their therapeutic potential is particularly evident in cutaneous wound healing. Postbiotics stimulate multiple cellular components of the wound healing process: they promote keratinocyte migration and proliferation to re-establish the epithelial barrier, modulate the function of fibroblasts and immune cells, and suppress pathogenic biofilm formation [70]. This makes them a promising, safe, and effective therapeutic strategy for managing chronic wounds, especially in the era of rising antimicrobial resistance.
Experimental Protocol: Testing Postbiotics in a Wound Healing Model
Objective: To investigate the efficacy of a postbiotic preparation in an in vitro model of cutaneous wound healing.
- Postbiotic Preparation: Culture a beneficial strain (e.g., Lactobacillus reuteri). Harvest the supernatant by centrifugation and filtration (0.22 µm) to create a cell-free postbiotic. Alternatively, use heat-killed bacteria.
- Cell Culture Model: Use a monolayer of human keratinocytes (HaCaT cell line). Create a uniform "wound" scratch using a pipette tip.
- Treatment: Treat the wounded monolayer with the postbiotic preparation at various concentrations. Positive controls can include growth factor-enriched media.
- Monitoring and Analysis: Acquire images of the scratch at 0, 12, 24, and 48 hours under a microscope. Use image analysis software (e.g., ImageJ) to quantify the wound closure area over time.
- Mechanistic Investigation: Perform downstream analyses such as qPCR or Western Blot to examine the expression of genes and proteins involved in cell migration (e.g., integrins) and inflammation (e.g., IL-6, IL-10) to elucidate the molecular mechanisms.
Figure 2: Proposed mechanism of action for postbiotics in cutaneous wound healing, involving multiple cell types.
Fecal Microbiota Transplantation (FMT): Community-Level Restoration
Pharmacology and Clinical Indications
FMT is the process of transferring fecal material from a healthy, screened donor into a recipient's gastrointestinal tract to directly regulate their gut microbiota [71]. It represents the most complex level of microbiome intervention, effectively transplanting an entire microbial community. While highly effective for recurrent Clostridioides difficile infection (rCDI), with remission rates as high as 92%, its application is expanding to other gastrointestinal, metabolic, and neurological disorders [68] [71]. The pharmacology of FMT is fundamentally different from traditional drugs. Its key parameters can be described as Engraftment, Metagenome, Distribution, and Adaptation (EMDA), which mirror the classic Absorption, Distribution, Metabolism, Excretion (ADME) parameters [68]. Success depends on a complex donor-recipient interplay, including factors like immune system function, diet, drug use, and the ecological dynamics between the resident and donor microbes [68] [71].
Regulatory and Technical Challenges
The regulatory landscape for FMT is evolving. In the US, the FDA classified FMT as a drug, leading to commercial development and associated high costs and access limitations. In contrast, the European Union's Substances of Human Origin (SoHO) Regulation aims to balance patient access with product development, emphasizing donor safeguards [68]. Key technical challenges include donor screening and the move towards non-profit, ethically-managed stool donor programs to ensure safety and integrity [68]. The complexity of FMT is considered a feature, not a bug, as the complete donor-derived community may offer greater resilience and functional redundancy compared to defined consortia, potentially providing better long-term protection against colonization with antibiotic-resistant pathobionts [68].
Experimental Protocol: Standardized FMT and Engraftment Analysis
Objective: To perform FMT in a murine model and analyze donor microbiota engraftment and functional consequences.
- Donor Material Preparation: Collect fresh fecal pellets from healthy, genetically defined donor mice. Homogenize in sterile, anaerobic PBS. Centrifuge briefly to remove large particulates. The supernatant, containing the microbiota, is used for transplantation. Aliquots are saved for metagenomic reference.
- Recipient Model: Use a germ-free mouse or a mouse with antibiotic-induced dysbiosis as the recipient.
- Transplantation: Administer the donor material to the recipient via oral gavage. Multiple administrations may be performed.
- Longitudinal Sampling: Collect fecal samples from recipients pre- and post-FMT over several weeks for metagenomic analysis.
- Engraftment Analysis: Perform shotgun metagenomic sequencing on all donor, recipient pre-FMT, and recipient post-FMT samples. Use bioinformatic pipelines (e.g., MAGEnTa, StrainPhlan) to track the persistence and abundance of donor-derived microbial strains and genes in the recipient over time [68]. This analysis focuses on Community Coalescence and long-term Resilience of the new community.
- Phenotypic Assessment: Monitor relevant host phenotypes (e.g., weight gain, resolution of disease symptoms, changes in metabolic markers) and correlate with engraftment success.
The Scientist's Toolkit: Key Reagents and Methodologies
Table 3: Essential Research Reagents and Tools for Microbiome Therapeutics
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| Gnotobiotic Mice | Provides a sterile host for colonization with defined microbial communities. | Essential for establishing causal relationships between a specific probiotic or FMT and a host phenotype [68]. |
| Shotgun Metagenomic Sequencing | Comprehensive profiling of all genes in a microbial community. | Tracking strain-level engraftment of donor microbes in FMT recipients; functional profiling [68]. |
| MAGEnTa Pipeline | Bioinformatic tool for tracking engraftment using metagenome-assembled genomes. | Cost-efficient analysis of donor vs. recipient microbiota dynamics without external databases [68]. |
| Gas Chromatography-Mass Spectrometry (GC-MS) | Quantification of microbial metabolites. | Measuring SCFA (butyrate, acetate, propionate) production in response to prebiotic or probiotic intervention [69]. |
| Anaerobic Chamber/Workstation | Creates an oxygen-free environment for culturing obligate anaerobic gut bacteria. | Critical for preparing and manipulating FMT material and cultivating next-generation probiotics [68]. |
| Caco-2 Cell Line | Human epithelial cell line model of the intestinal barrier. | In vitro assessment of probiotic or postbiotic effects on epithelial barrier integrity and immune response [70]. |
| Cryoprotectants (e.g., Glycerol) | Protect microbial cells during freeze-thaw cycles. | Preparation of stable, cryopreserved FMT or probiotic formulations for long-term storage [68]. |
| Chartarlactam A | Chartarlactam A, MF:C23H29NO5, MW:399.5 g/mol | Chemical Reagent |
| Leucanthogenin | Leucanthogenin, MF:C17H14O8, MW:346.3 g/mol | Chemical Reagent |
The therapeutic landscape of host-microbiome interactions is rapidly advancing from broad-spectrum interventions like FMT towards precision, mechanism-based applications. The future lies in personalized microbiota therapies, where an individual's microbiome profile will inform the choice of probiotic strain, prebiotic fiber, or postbiotic preparation [73] [68]. Engineered microbial consortia and single strains, designed using synthetic biology to produce therapeutic molecules in situ, represent a frontier for treating metabolic disorders, cancers, and infectious diseases [67]. Key challenges that must be addressed include the standardization of manufacturing processes, the conduct of large-scale randomized controlled trials, and the development of a robust pharmacologic framework for these complex live biotherapeutic products [68] [69]. As research unravels the intricate molecular dialogue between the host and its microbiome, the integration of these targeted, safe, and effective microbiome-based therapeutics into mainstream clinical practice will be essential for advancing the field of precision medicine.
Addressing Research Gaps: Establishing Causality and Improving Model Translationality
The translation of microbiome research into clinical applications has been significantly hampered by challenges in establishing causality and the limitations of existing preclinical models. In response, the Human Microbiome Action Consortium, an international network of over 30 research institutions funded by the EU's Horizon 2020 program, has developed a comprehensive consensus to address these methodological gaps. This whitepaper synthesizes their expert recommendations, providing a structured framework for selecting, validating, and implementing preclinical models in host-microbiome interaction studies. The consensus emphasizes standardized methodologies, rigorous causal inference, and multi-model approaches to enhance the predictive value and clinical translatability of microbiome research, ultimately accelerating the development of microbiome-based therapeutics for conditions ranging from inflammatory bowel disease to neurological disorders.
The gut microbiome, a complex ecosystem of trillions of microorganisms, exerts profound influence on human health by modulating host metabolism, immune responses, and neuronal functions. Disruption in gut microbiome composition, known as dysbiosis, has been implicated in numerous inflammatory, metabolic, and neurodegenerative conditions [74] [75]. However, a fundamental challenge persists: the difficulty in distinguishing correlation from causation in the relationship between microbial communities and host pathophysiology.
The Human Microbiome Action Consortium (HMAC) initiated a rigorous Delphi survey process to address this challenge, gathering insights from a diverse range of stakeholders through structured workshops and iterative questionnaires [76] [75]. This process identified critical gaps in current approaches to studying host-microbiome interactions, particularly the limited external validity of many preclinical models and the absence of standardized frameworks for establishing causal relationships. The resulting consensus provides guidance for researchers seeking to overcome these limitations and generate clinically relevant findings.
Methodological Framework: The Delphi Consensus Approach
The HMAC employed a structured, iterative Delphi methodology to develop evidence-based recommendations for microbiome research. This approach encompassed multiple stages designed to synthesize expert opinion and build consensus across the international research community.
Table: Delphi Survey Methodology for Microbiome Research Consensus
| Phase | Objective | Activities | Outcomes |
|---|---|---|---|
| Preparation | Identify key challenges | Comprehensive literature review; Expert stakeholder mapping | List of critical gaps and priority areas |
| Workshop | Gather preliminary insights | Facilitated discussions with clinicians, researchers, industry representatives | Initial perspectives on model strengths/limitations |
| Questionnaire | Assess utility of preclinical models | Structured surveys evaluating animal and cell-based models | Quantitative data on model suitability for specific research questions |
| Consensus Building | Refine recommendations | Iterative feedback rounds; Draft statement circulation | Finalized consensus statements and guidelines |
The Delphi process specifically focused on evaluating preclinical models capable of addressing complex host-microbiome interactions and causality, including germ-free animals, organoids, and organ-on-a-chip systems, while excluding simpler in vitro fermentation models that cannot fully recapitulate host physiology [75]. This methodological rigor ensures that the resulting recommendations are both evidence-based and practical for implementation across diverse research settings.
Critical Analysis of Preclinical Models in Microbiome Research
Strengths and Limitations of Current Model Systems
The consensus statement provides a critical evaluation of the primary models used in microbiome research, acknowledging both their utility and inherent limitations for studying host-microbiome interactions.
Table: Comparative Analysis of Preclinical Models for Microbiome Research
| Model System | Key Strengths | Major Limitations | Recommended Applications |
|---|---|---|---|
| Germ-free Animals | Enable precise microbial manipulation; Establish causal relationships | Do not fully replicate human gut microbiome; Limited translational potential | Human microbiota-associated (HMA) studies; Core mechanism discovery |
| Organoids | Recapitulate native tissue architecture; Enable cellular-level host interaction studies | Lack full microenvironment (immune, stromal, vascular components); Difficult long-term culture | Epithelial barrier function; Personalized therapy development |
| Organ-on-a-Chip | Dynamic physiological relevance; Real-time monitoring of cellular responses | Technical complexity; High cost; Specialized equipment requirements | Drug metabolism studies; Barrier integrity assessment |
| Human Microbiota-Associated (HMA) Mice | Bridge human microbiota with animal physiology; Disease-relevant modeling | Limited persistence of human microbiota; Species-specific host responses | Therapeutic screening; Microbiota-disease causality studies |
Addressing External Validity Challenges
A fundamental limitation across all preclinical models concerns external validity - the extent to which research findings from one species or setting can be reliably applied to another. The consensus acknowledges that species differences between animal models and humans will always present challenges for translation [77]. Common issues include:
- Unrepresentative samples: Laboratory animals are typically young, healthy, and genetically homogeneous, unlike heterogeneous human patient populations who often present with comorbidities and polypharmacy [77].
- Simplified disease modeling: Most animal models fail to mimic the slow, progressive nature of human chronic diseases or the complexity of comorbidity [77].
- Divergent timelines: Recovery from experimental conditions in animals (e.g., stroke) often occurs in days or weeks, whereas equivalent human conditions may require years of recovery [77].
To mitigate these limitations, the consensus emphasizes the importance of Human Microbiota-Associated (HMA) models, where germ-free animals are colonized with human-derived fecal microbiota, thereby creating a more physiologically relevant system for studying host-microbiome interactions [75].
Experimental Protocols and Methodological Recommendations
Integrated Workflow for Causality Assessment
The consensus recommends a multi-model approach to establish causality in host-microbiome interactions, leveraging complementary strengths of different experimental systems.
Standardized Methodologies for Key Model Systems
Human Microbiota-Associated (HMA) Mouse Model Protocol
- Donor selection: Recruit human donors with well-characterized clinical phenotypes; process fecal samples within 30 minutes of collection under anaerobic conditions [75].
- Recipient preparation: Maintain germ-free mice in flexible film isolators; verify germ-free status through regular culturing and 16S rRNA testing [75].
- Colonization procedure: Administer 200μL of 50mg/mL fecal slurry via oral gavage to 6-8 week old recipients; house colonized mice in individually ventilated cages [75].
- Validation measures: Confirm engraftment through 16S rRNA sequencing at weekly intervals; assess functional integration via metabolomic profiling of serum and fecal samples [75].
Host-Microbiome Interaction Studies in Organoids
- Organoid establishment: Generate intestinal organoids from primary human intestinal crypts or induced pluripotent stem cells; culture in Matrigel with essential growth factors (EGF, Noggin, R-spondin) [75].
- Microbial exposure: Introduce specific bacterial strains or defined communities at controlled multiplicities of infection (MOI 10-100:1); monitor viability through ATP-based assays [75].
- Response assessment: Quantify epithelial barrier integrity via transepithelial electrical resistance (TEER); profile immune responses through cytokine multiplex assays; analyze transcriptomic changes via RNA sequencing [75].
- Limitation mitigation: Co-culture with immune cells or stromal components to enhance physiological relevance; utilize microfluidic systems to introduce flow and shear stress [75].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table: Key Research Reagents for Advanced Microbiome Studies
| Reagent / Material | Function | Application Notes |
|---|---|---|
| Gnotobiotic Isolators | Maintain germ-free animals for HMA studies | Require specialized training; Regular sterility verification essential |
| Defined Microbial Communities | Standardized consortia for reductionist studies | Commercially available (e.g., Novobiome); Enable reproducible experiments |
| Organoid Culture Systems | 3D models of human intestinal epithelium | Matrigel-based; Require specific growth factor cocktails |
| Anaerobic Chamber | Maintain oxygen-free conditions for bacterial culture | Critical for working with obligate anaerobes; Typically set at <1 ppm Oâ‚‚ |
| Multi-omics Kits | Simultaneous analysis of multiple data layers | Integrated DNA/RNA extraction kits preserve sample integrity |
| Fecal Sampling Kits | Standardized collection and stabilization | Preserve microbial composition at time of collection; Enable DNA/RNA analysis |
Signaling Pathways in Host-Microbiome Interactions
The consensus highlights several key mechanistic pathways through which the microbiome influences host physiology, providing validated targets for therapeutic intervention.
Implementation Framework and Future Directions
Standardization and Reproducibility Measures
The consensus emphasizes that enhancing reproducibility requires implementing standardized protocols across several key areas:
- Methodological harmonization: Adopt FAIR (Findable, Accessible, Interoperable, Reusable) principles for data management; establish standardized operating procedures for sample collection, processing, and analysis [78].
- Model validation: Implement rigorous quality control measures for preclinical models, including verification of microbial engraftment in HMA models and functional characterization of organoid systems [75].
- Multi-omics integration: Combine genomic, transcriptomic, proteomic, and metabolomic datasets to capture the full complexity of host-microbiome interactions, moving beyond taxonomic composition to functional assessment [75] [78].
Translational Applications and Therapeutic Development
The consensus identifies several promising avenues for translating basic research on host-microbiome interactions into clinical applications:
- Microbiome-based biomarkers: Develop predictive signatures for treatment response, particularly in oncology where microbiome features can predict immunotherapy efficacy with good sensitivity and accuracy [78].
- Microbial therapeutics: Advance targeted interventions including probiotics, prebiotics, and fecal microbiota transplantation, with rigorous evaluation through optimized preclinical models [75].
- Personalized medicine approaches: Leverage individual microbiome variations to tailor therapeutic strategies, particularly for conditions with unmet medical needs such as graft-versus-host disease and amyotrophic lateral sclerosis [78].
The consensus concludes that while significant challenges remain, the systematic implementation of these recommendations will accelerate the translation of microbiome research into effective therapies that target the intricate relationships between microbial communities and human health [76] [75] [78].
A fundamental challenge in biomedical research is creating experimental models that faithfully recapitulate the complexity of human physiology. Traditional models, including animal studies and two-dimensional cell cultures, consistently fall short in replicating the intricate host-microbiome interactions crucial to human health and disease. These systems fail to capture three critical dimensions: the specialized microenvironment that supports cellular function, the dynamic microbial stability maintained by host immune mechanisms, and the systemic organ-organ interactions that coordinate whole-body physiology. This whitepaper examines these challenges through the lens of modern research initiatives and technological advances, providing a technical guide for researchers and drug development professionals seeking to create more human-relevant models for studying health and disease.
The imperative to overcome these challenges is not merely academic but increasingly driven by regulatory and scientific necessity. Recent coordinated pushes from agencies like the NIH and FDA are shifting the preclinical landscape toward human-relevant testing, creating a "human-centric mandate" that prioritizes models capable of capturing interconnected physiological systems [79]. This transition acknowledges that diseases often emerge from disrupted equilibrium across multiple systems rather than isolated pathology in single organs.
The Microenvironment Challenge: Beyond Simple Cell Culture
The Extracellular Matrix and Cellular Composition
The cellular microenvironment comprises both the physical scaffold of the extracellular matrix (ECM) and the precise balance of different cell types. In native human tissues, cells exist within a three-dimensional ECM that provides structural support and biochemical cues. Simplified models that neglect this complexity fail to replicate key cellular behaviors. Advanced models now address this through engineered "neuromatrix" scaffolds that mimic the brain's ECM with custom blends of polysaccharides, proteoglycans, and basement membrane components [80].
Equally critical is achieving the proper cellular composition and ratios. In neural tissue, for instance, the proportions of different cell types have been debated for decades, with estimates ranging from 45-75% for oligodendroglia and 19-40% for astrocytes [80]. The multicellular integrated brain (miBrain) platform exemplifies how researchers are addressing this challenge by experimentally iterating cell type ratios to achieve functional, properly structured neurovascular units.
Table 1: Key Components of Physiological Microenvironments in Advanced Models
| Component | Function | Implementation in Advanced Models |
|---|---|---|
| Extracellular Matrix (ECM) | Provides 3D structural support, biochemical signaling, and mechanical cues | Custom hydrogel blends of polysaccharides, proteoglycans, and basement membrane components [80] |
| Multiple Cell Types | Enables cell-cell signaling and emergent tissue functions | Balanced ratios of all major tissue-specific cell types (e.g., 6 major brain cell types in miBrains) [80] |
| Vasculature | Enables nutrient delivery, waste removal, and provides barrier functions | Self-assembling endothelial cells forming blood-brain-barrier capable structures [80] |
| Neuro-immune Interface | Integrates neural and immune system crosstalk | Inclusion of microglia and other tissue-resident immune cells [80] |
Experimental Protocols for Microenvironment Recapitulation
Protocol 1: Establishing a Multicellular Human Brain Model
- Generate patient-specific cell types: Derive the six major brain cell types (neurons, astrocytes, oligodendrocytes, microglia, oligodendrocyte precursor cells, and vascular cells) from individual donors' induced pluripotent stem cells (iPSCs) [80].
- Culture cells separately: Maintain distinct cell populations in specialized media to ensure proper differentiation and viability [80].
- Prepare neuromatrix scaffold: Create a hydrogel-based scaffold mimicking the brain's extracellular matrix with a custom blend of polysaccharides, proteoglycans, and basement membrane components [80].
- Combine cell types in optimized ratios: Experimentally determine functional ratios of different cell types that result in self-assembling neurovascular units. This laborious iterative process is essential for proper tissue function [80].
- Validate model functionality: Confirm the presence of key features including blood-brain barrier function, nerve signal conduction, and immune defense capabilities [80].
Protocol 2: Genetic Modification for Disease Modeling
- Leverage modular design: Utilize the separately cultured cell types to introduce genetic modifications specific to one cell type while maintaining others in a wild-type state [80].
- Employ gene editing technologies: Use CRISPR/Cas9 or other precise gene editing tools to introduce disease-associated variants (e.g., APOE4 for Alzheimer's disease research) [80].
- Assemble edited cells: Combine genetically modified cells with other cell types in the neuromatrix to study cell-type-specific contributions to disease pathology [80].
Figure 1: Workflow for establishing multicellular human brain models with physiological microenvironments, from iPSCs to functional validation.
Microbial Stability: The Immune Tolerance Dimension
Regulatory T Cells and the FOXP3 Factor
Microbial stability at host-microbiome interfaces depends critically on immune tolerance mechanisms, particularly those mediated by regulatory T cells (Tregs). The 2025 Nobel Prize in Physiology or Medicine recognized groundbreaking discoveries of how the immune system maintains peripheral immune tolerance through Tregs [79]. These cells actively suppress immune responses against commensal microorganisms and self-antigens, preventing inappropriate inflammation while maintaining protective immunity.
The molecular key to Treg function is the transcription factor FOXP3, identified as the master regulator of immune tolerance. Discoveries by Brunkow and Ramsdell revealed that mutations in the Foxp3 gene cause fatal autoimmune disorders in both mice (scurfy mouse) and humans (IPEX syndrome) [79]. This established that self-tolerance is not a passive process but requires active, cell-mediated suppression coordinated through specific genetic pathways.
Table 2: Key Elements in Microbial Stability and Immune Tolerance
| Component | Role in Microbial Stability | Experimental/Disease Evidence |
|---|---|---|
| Regulatory T Cells (Tregs) | Actively suppress immune responses to commensal microbiota and prevent autoimmunity | Removal causes multi-organ autoimmune disease; identified by Sakaguchi et al. [79] |
| FOXP3 Transcription Factor | Master regulator controlling Treg development and function | Mutations cause fatal lymphoproliferative disorder (scurfy mouse) and IPEX syndrome in humans [79] |
| IL-2 Receptor (CD25) | Cell surface marker identifying Treg population | CD25+ T cell subset shown to be essential for maintaining self-tolerance [79] |
| Suppressive Mechanisms (CTLA-4, IL-10, TGF-β) | Molecular mediators of Treg suppression | Enable Tregs to inhibit effector T cells through multiple pathways [79] |
Experimental Protocols for Studying Host-Microbiome Immune Interactions
Protocol 3: Modeling Immune-Epithelial Crosstalk in 3D Systems
- Establish 3D co-culture systems: Incorporate immune cells (such as macrophages) with epithelial and stromal cells in engineered microenvironments that mimic host-microbiome interfaces [79].
- Embed immune context: Create cytokine feedback loops and engineered immune interactions to capture regulatory dynamics present in vivo [79].
- Challenge with microbial components: Introduce pathogen-associated molecular patterns (PAMPs) or commensal-derived signals to study immune activation and resolution.
- Monitor immune parameters: Measure cytokine production, immune cell activation markers, and tissue integrity metrics to assess the balance between tolerance and defense.
- Perturb the system: Use genetic, pharmacological, or environmental interventions to disrupt immune homeostasis and study recovery mechanisms.
Protocol 4: Investigating Treg-Dependent Mechanisms in Microbial Stability
- Isolate Treg populations: Extract CD4+ CD25+ T cells from biological samples using fluorescence-activated cell sorting or magnetic bead separation [79].
- Deplete Tregs experimentally: Use anti-CD25 antibodies or genetic approaches to remove Tregs from experimental systems and observe resulting autoimmune or inflammatory phenotypes [79].
- Assess Treg function: Conduct in vitro suppression assays to measure the ability of Tregs to inhibit effector T cell responses.
- Analyze FOXP3 expression: Use transcriptional profiling, immunohistochemistry, or reporter systems to monitor FOXP3 expression and Treg differentiation [79].
Figure 2: Signaling pathway for regulatory T cell maintenance of microbial stability through active immune tolerance mechanisms.
Organ-Organ Interactions: Toward Whole-Person Physiology
The Whole Person Reference Physiome Initiative
Recognizing the limitations of studying isolated systems, the National Institutes of Health (NIH) has launched a landmark whole-person health research initiative to model how the body's systems function together to sustain health and well-being. This five-year project aims to build the Whole Person Reference Physiome, a unified framework connecting anatomy, physiology, and function through advanced data integration and physiological modeling [81].
Unlike traditional biomedical research organized around specific organs or diseases, this initiative emphasizes the interconnectedness of multiple systems. For example, lifestyle interventions including balanced diet, regular physical activity, and stress management simultaneously improve cardiovascular, metabolic, and musculoskeletal function—demonstrating the value of integrative research for understanding health holistically [81]. The approach connects common clinical measures such as blood pressure, glucose levels, and cholesterol to larger physiological processes, creating an interactive model capable of identifying patterns in health maintenance and decline.
Experimental Frameworks for Studying System-Level Interactions
Protocol 5: Developing Multi-System Models for Organ-Organ Interactions
- Leverage extensive datasets: Draw on resources such as the NIH Human Reference Atlas and the Human BioMolecular Atlas Program (HuBMAP) to create a digital map of healthy human function [81].
- Establish data standards: Implement standardized data formats, metadata alignment, and cross-platform collaboration protocols to enable interoperability between different research platforms [81].
- Form multidisciplinary teams: Assemble researchers spanning genomics, bioinformatics, clinical research, and computational modeling to work on shared frameworks for human physiology network design [81].
- Build computational networks: Develop integrated human physiology networks that connect clinical measurements to physiological processes at multiple scales [81].
- Validate predictive capabilities: Test model predictions against longitudinal health data and interventional outcomes to refine understanding of system-level interactions.
Protocol 6: Incorporating Personalization into Whole-Person Models
- Utilize individualized starting materials: Generate models from individual donors' induced pluripotent stem cells to create personalized systems reflecting genetic variation [80].
- Incorporate clinical metadata: Annotate models with donor health information, lifestyle factors, and environmental exposures to identify determinants of health trajectories.
- Enable comparative analysis: Study how the same intervention affects different genetic backgrounds by comparing responses across multiple donor-specific models.
Table 3: Components of the NIH Whole Person Reference Physiome Initiative
| Initiative Component | Description | Research Applications |
|---|---|---|
| Whole Person Reference Physiome | Unified framework connecting anatomy, physiology, and function through data integration and modeling | Foundation for understanding factors that drive health declines and pathways to restoration [81] |
| Human Reference Atlas | Comprehensive map of human anatomy at multiple scales | Spatial reference for integrating molecular, cellular, and physiological data [81] |
| Human BioMolecular Atlas Program (HuBMAP) | Tissue mapping initiative creating open global atlas of the human body at single-cell resolution | Cellular-level understanding of tissue organization and function [81] |
| Integrative Data Analysis | Synthesis of diverse data types across physiological systems | Identifying patterns in health maintenance and decline across multiple systems [81] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Research Reagent Solutions for Advanced Physiological Modeling
| Reagent/Material | Function | Application Examples |
|---|---|---|
| Induced Pluripotent Stem Cells (iPSCs) | Patient-specific starting material for generating differentiated cell types | Creating personalized models reflecting individual genetic backgrounds [80] |
| Custom Hydrogel Blends | Mimics native extracellular matrix; provides 3D scaffold for cell growth | Neuromatrix in miBrain models containing polysaccharides, proteoglycans, and basement membrane components [80] |
| Defined Cell Culture Media | Supports differentiation and maintenance of specific cell types | Specialized media for neurons, glial cells, and vascular cells in brain models [80] |
| CRISPR/Cas9 Gene Editing Systems | Enables precise genetic modifications to introduce disease-associated variants | Creating APOE4-versus APOE3-specific cells for Alzheimer's disease research [80] |
| Cell Type-Specific Markers | Identifies and validates different cell populations in complex cultures | Antibodies against neuronal, astrocyte, microglial, and vascular markers [80] |
| Cytokine/Chemokine Arrays | Measures soluble factors mediating cell-cell communication | Assessing immune activation states in co-culture systems [79] |
| Multi-electrode Arrays | Records electrical activity in neuronal cultures | Functional validation of neural network activity in brain models [80] |
| Single-Cell RNA Sequencing Reagents | Enables transcriptional profiling of individual cells in complex cultures | Characterizing cellular heterogeneity and identifying novel cell states [80] |
The challenges of recapitulating human physiology—including the cellular microenvironment, mechanisms maintaining microbial stability, and complex organ-organ interactions—represent significant but surmountable hurdles in biomedical research. The frameworks, protocols, and tools outlined in this technical guide provide a roadmap for researchers to create more physiologically relevant models that bridge the gap between traditional simplified systems and human complexity. As emphasized by the NIH's whole-person health initiative, future breakthroughs will come from embracing interconnected systems rather than studying components in isolation [81].
The growing capability to build integrated models that capture human physiology more accurately promises to transform both basic research and drug development. These advances align with regulatory shifts toward human-relevant testing and personalized medicine approaches. By focusing on the critical dimensions of microenvironment, microbial stability, and system-level interactions, researchers can develop predictive models that not only mimic organs but capture the regulatory balance that defines human health and enables more effective therapeutic interventions for complex diseases.
Strategies for Standardizing Methodologies and Improving Biomarker Validation Pipelines
The study of host-microbiome interactions has revolutionized our understanding of human health and disease, revealing the microbiome's critical role in pathologies ranging from inflammatory bowel disease (IBD) to diabetic retinopathy and sepsis [82] [83]. Despite exponential growth in microbiome research, the field faces a reproducibility crisis characterized by inconsistent results, conflicting biomarker claims, and methodological heterogeneity that hampers clinical translation [84] [85]. This technical guide addresses these challenges by presenting standardized methodologies and robust validation pipelines explicitly framed within host-microbiome research. Contradictory findings frequently emerge from microbiome studies due to uncontrolled confounders, compositional data artifacts, and insufficient validation frameworks [84] [86]. For instance, well-established microbiome targets like Fusobacterium nucleatum failed to maintain significant associations with colorectal cancer stages when rigorous confounder control was applied [84]. Such discrepancies underscore the urgent need for standardized approaches that can distinguish true biological signals from methodological artifacts and confounding effects. By implementing the strategies outlined in this guide, researchers can enhance the reliability, reproducibility, and clinical utility of microbiome biomarkers in host-microbiome interaction studies.
Key Challenges in Microbiome Biomarker Development
Technical and Biological Confounders
Multiple technical and biological variables introduce variability in microbiome studies, often masking genuine host-microbe interactions. Transit time, intestinal inflammation (measured by fecal calprotectin), and body mass index have been identified as primary microbial covariates that can supersede variance explained by disease diagnostic groups [84]. In colorectal cancer studies, these factors explained more microbial variation than the cancer diagnosis itself, fundamentally challenging previous biomarker associations. Batch effects represent another critical challenge, where technical variations between studies often exceed biological signals of interest [86]. Analysis of 2,742 gut microbiota samples from seven independent colorectal cancer studies revealed that differences among studies were significantly greater than those between case-control groups, with very few differentially abundant bacteria shared across multiple studies when proper normalization was applied [86].
Analytical and Methodological Limitations
The dominance of relative microbiome profiling (where taxon abundances are expressed as percentages) introduces compositionality artifacts, distorting biological interpretations and increasing false discovery rates [84]. Quantitative microbiome profiling (QMP) approaches that incorporate absolute microbial abundance measurements have shown superior performance in identifying robust biomarkers yet remain underutilized [84]. Additional limitations include high-dimensional data with small sample sizes, inconsistent bioinformatic processing pipelines, and incomplete documentation that collectively impede reproducibility [85]. The use of different hypervariable regions in 16S rRNA sequencing generates inconsistent taxonomic resolution, while the continued reliance on Operational Taxonomic Units (OTUs) rather than Amplicon Sequence Variants (ASVs) limits cross-study comparability [87] [85].
Table 1: Major Confounders in Microbiome Biomarker Studies
| Confounder Category | Specific Variables | Impact on Microbiome | Validation Study Findings |
|---|---|---|---|
| Physiological | Transit time, BMI, age | Alters community structure & diversity | Superseded variance explained by CRC diagnosis [84] |
| Inflammatory | Fecal calprotectin | Increases pro-inflammatory taxa | Higher in CRC (219.42 µg/g) vs. adenoma (70.24 µg/g) [84] |
| Methodological | Sequencing platform, primer region | Introduces technical batch effects | Study batch effect > case-control differences in 7 CRC cohorts [86] |
| Sample Processing | Storage conditions, DNA extraction | Varies DNA yield & community representation | Different kits recover different bacterial groups [87] |
Standardized Experimental Design Frameworks
Sample Collection and Preservation Protocols
Standardized sample collection is foundational for reproducible microbiome biomarker research. Sample type selection should align with research questions: fecal samples for gut microbiome, saliva/oral swabs for oral microbiome, and tissue biopsies for mucosal communities [87]. For gut microbiome studies in population-based research, stool collection should be standardized for timing (first specimen of the day), collection devices, and immediate freezing at -80°C or use of preservation buffers to prevent microbial community shifts [87]. The European General Data Protection Regulation (GDPR) requires careful donor anonymization and sample tracking in biobanks, with removal of human genetic data from publicly shared microbiome datasets to prevent re-identification [87]. For host-microbiome interaction studies involving multiple body sites, consistent collection methods across sites are essential. Skin microbiome sampling should account for ecological niches (sebaceous, moist, dry sites) using standardized swabbing techniques with pre-moistened swabs and consistent pressure [82]. Oral microbiome collections should specify sampling location (saliva, tongue swab, subgingival plaque) as each harbors distinct communities [82] [87].
Quantitative Profiling Technologies
Moving from relative to absolute abundance measurements is critical for accurate biomarker discovery. Quantitative microbiome profiling (QMP) incorporating flow cytometry with 16S rRNA amplicon sequencing or spike-in standards provides absolute microbial counts, overcoming compositionality limitations and reducing both false-positive and false-negative rates [84]. For functional insights, multi-omics approaches are essential. Metatranscriptomics reveals actively expressed microbial genes, providing dynamic functional information beyond the genetic potential captured by metagenomics [44] [88]. Metaproteomics identifies microbial proteins actually produced, while metabolomics profiles the functional readout of host-microbiome interactions through measurement of microbial metabolites like short-chain fatty acids, bile acids, and tryptophan derivatives [89] [88]. Mass spectrometry and NMR spectroscopy enable quantification of these metabolites, offering insights into microbial functional activities relevant to host physiology [89]. Shotgun metagenomics provides strain-level resolution and functional gene information but requires careful standardization to avoid batch effects [87].
Table 2: Analytical Approaches for Microbiome Biomarker Discovery
| Technology | Resolution | Key Applications | Standardization Requirements |
|---|---|---|---|
| 16S rRNA Sequencing | Genus to species | Taxonomic profiling, diversity | Consistent hypervariable regions (V3-V4), ASVs not OTUs [85] |
| Shotgun Metagenomics | Strain level | Functional potential, strain tracking | Constant DNA input, removal of host reads [87] |
| Metatranscriptomics | Active functions | Gene expression, microbial activity | RNA stabilizers, ribosomal RNA depletion [44] [83] |
| Metabolomics | Metabolic output | Microbial metabolites, host response | Standard curves, internal standards [89] |
| Quantitative Profiling | Absolute abundance | Biomarker quantification, load | Flow cytometry, spike-in standards [84] |
Computational and Statistical Validation Frameworks
Robust Biomarker Identification Algorithms
Advanced computational methods are essential for distinguishing true biomarkers from spurious associations. The NetMoss (Network Module Structure Shift) algorithm identifies robust biomarkers by assessing shifts in microbial network modules rather than relying solely on abundance changes [86]. This approach effectively removes batch effects by integrating multiple datasets through a univariate weighting method that assigns greater weight to larger datasets, thereby capturing genuine biological signals across studies [86]. For machine learning-based biomarker discovery, the Recursive Ensemble Feature Selection (REFS) methodology combined with DADA2 for Amplicon Sequence Variant (ASV) generation has demonstrated superior performance in identifying reproducible biomarker signatures [85]. In validation across inflammatory bowel disease, autism spectrum disorder, and type 2 diabetes datasets, REFS achieved higher area under the curve (AUC) and Matthews correlation coefficient values compared to traditional feature selection methods, maintaining diagnostic accuracy when applied to independent validation cohorts [85]. These computational approaches specifically address the high-dimensionality and sparse nature of microbiome data while controlling for false discoveries.
Multi-Omics Data Integration Strategies
Integrating multiple data layers is crucial for understanding mechanistic links between microbiome communities and host health. Data-driven and knowledge-guided integration strategies help overcome the "curse of dimensionality" in multi-omics datasets [83]. Methods like Multi-Omics Factor Analysis (MOFA) enable simultaneous analysis of metagenomic, transcriptomic, proteomic, and metabolomic data to identify latent factors driving host-microbiome interactions [88] [90]. In sepsis research, integrated analysis of host transcriptional profiling with metagenomic pathogen detection has improved diagnostic accuracy and patient stratification [83]. For diabetic retinopathy, integrating gut metagenomics with retinal transcriptomics has revealed how microbial metabolites influence retinal inflammation through the gut-retina axis [88]. These integration approaches facilitate the transition from correlative associations to mechanistic understanding of host-microbiome interactions in health and disease.
Diagram 1: Multi-omics biomarker validation workflow with quality control checkpoints.
Experimental Protocols for Biomarker Validation
Protocol 1: Quantitative Biomarker Verification with Confounder Control
This protocol enables robust verification of candidate microbiome biomarkers while controlling for major confounders:
Sample Processing: Apply quantitative microbiome profiling using flow cytometry counting or internal standards before DNA extraction [84]. Use standardized DNA extraction kits with bead-beating for mechanical lysis across all samples.
Library Preparation: Employ shotgun metagenomic sequencing with constant DNA input (e.g., 100ng). Include negative controls and positive mock communities in each sequencing batch.
Metadata Collection: Systematically record transit time (Bristol Stool Scale), measure fecal calprotectin (ELISA), document BMI, medication use (especially antibiotics/proton pump inhibitors), and dietary patterns [84].
Statistical Analysis:
- Apply quantitative microbiome profiling (QMP) to convert relative to absolute abundances
- Include confounders as covariates in multivariate models
- Use the NetMoss algorithm to identify network module shifts [86]
- Validate findings in at least one independent cohort with comparable confounder assessment
Protocol 2: Multi-omics Functional Validation
This protocol validates the functional mechanisms linking microbiome biomarkers to host biology:
Sample Collection: Collect paired samples (e.g., stool and blood or tissue biopsies) from cases and controls with informed consent for multi-omics analysis.
Multi-omics Profiling:
- Metagenomics: Shotgun sequencing for taxonomic and functional profiling
- Metatranscriptomics: RNA sequencing with microbial rRNA depletion
- Metabolomics: LC-MS/MS for targeted quantification of microbial metabolites (SCFAs, bile acids, tryptophan derivatives) [89]
- Host Profiling: Transcriptomics or proteomics of host samples
Data Integration:
Experimental Validation:
- Culture candidate bacterial strains in vitro
- Measure production of putative bioactive metabolites
- Test host cell responses to bacterial isolates or their metabolites
Diagram 2: Biomarker validation pipeline with progressive evidence requirements.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Essential Research Reagents for Host-Microbiome Biomarker Studies
| Reagent/Solution | Function | Application Notes |
|---|---|---|
| DNA Stabilization Buffers | Preserves microbial community structure during storage | Enables room temperature transport; critical for field studies [87] |
| Mock Community Standards | Quality control for sequencing depth and accuracy | Should include rare and common species; used in each sequencing run [84] |
| Internal Standards (QMP) | Enables absolute quantification | Added before DNA extraction for quantitative microbiome profiling [84] |
| Bead Beating Matrix | Mechanical cell lysis for DNA extraction | Essential for Gram-positive bacteria; standardize bead size and shaking time [87] |
| rRNA Depletion Kits | Enriches mRNA for metatranscriptomics | Critical for assessing active microbial functions [44] [83] |
| Calprotectin ELISA Kit | Measures intestinal inflammation | Primary confounder in IBD and CRC studies [84] |
| SCFA Standards | Quantifies microbial metabolites | Used as calibration standards in mass spectrometry [89] |
| Cell Culture Media | Grows bacterial isolates | Enables functional validation of candidate biomarkers [82] |
Standardizing methodologies and strengthening validation pipelines for host-microbiome biomarker research requires a multifaceted approach addressing technical, analytical, and biological challenges. The strategies outlined in this guide—implementing quantitative profiling, controlling for key confounders, applying robust computational frameworks, and integrating multi-omics data—provide a roadmap for generating reproducible, clinically relevant biomarkers. As the field progresses, collaboration across institutions to establish standardized protocols, share well-characterized samples, and validate findings in diverse populations will be essential. Only through such rigorous and standardized approaches can we fully realize the potential of microbiome science to transform personalized medicine and improve human health.
Navigating Interindividual Variability and Long-Term Efficacy of Microbiome-Based Therapies
The human microbiome, once regarded as a passive passenger, is now recognized as a dynamic and essential determinant of human physiology, shaping immunity, metabolism, and neurodevelopment across the lifespan [91]. The clinical translation of this knowledge has begun to redefine early-life programming, cardiometabolic regulation, immune homeostasis, and neuropsychiatric resilience [91]. However, significant challenges persist, including high interindividual variability in microbiome composition, driven by diet, geography, host genetics, antibiotic exposure, and age [91]. This variability remains a key barrier to reproducibility and complicates the development of universally applicable diagnostic and therapeutic tools. Furthermore, the long-term efficacy of microbiome-targeting interventions remains questionable for many conditions, as the human microbiome exhibits great resilience and often returns to its baseline state after transient modifications [92]. This whitepaper examines the roots of these challenges and outlines strategic approaches for navigating them in therapeutic development, framed within the critical context of host-microbiome interactions in health and disease.
Foundations of Host-Microbiome Interactions
Mucosal Immunology and Microbial Homeostasis
The intestinal mucosal immune system must maintain intestinal integrity while tolerating an enormous quantity of external antigens, including food proteins and the microbiome [93]. This tolerance is not passive but involves active processes where specialized epithelial cells, M cells, actively transport antigen to underlying lymphoid follicles for immunological processing, and dendritic cells extend dendrites between epithelial cells to sample adherent bacterial species [93]. The balance between immune tolerance and inflammation is regulated through intricate crosstalk between epithelial and immune cells with the intestinal microbiota, involving multiple signaling pathways and molecules.
Direct contact with bacterial-associated structures, such as lipopolysaccharide (LPS), can activate host Toll-like receptors (TLRs), inducing signaling cascades that result in both innate and adaptive polarized immune responses [93]. For instance, MHC II-dependent presentation of segmented filamentous bacteria antigens by intestinal dendritic cells promotes the local induction of TH17 lymphocytes, whereas dendritic cells exposed to Bifidobacterium infantis 35624 promote polarization of regulatory T cells (TREGs) [93]. This immunological crosstalk creates a dynamic interface that varies significantly across individuals and forms the basis for personalized responses to microbiome-targeted therapies.
Microbial Metabolites as Signaling Molecules
Beyond direct contact, the intestinal microbiome is metabolically active, and microbial metabolites exert significant effects on host immune signaling networks. Short-chain fatty acids (SCFAs)—particularly butyrate, acetate, and propionate—produced through microbial fermentation of dietary fibers, demonstrate potent immunomodulatory effects, often mediated through G protein-coupled receptors (GPCRs) [93]. Butyrate promotes dendritic cell regulatory activity, resulting in the induction of TREG cells and IL-10-secreting T cells [93]. Other microbial metabolites, including histamine secreted by specific gut microbes, can modify chemokine and cytokine secretion by dendritic cells, with mucosal histamine levels being increased in patients with irritable bowel syndrome and inflammatory bowel disease [93]. These findings establish microbial metabolites as crucial mediators of host-microbiome interactions and attractive targets for therapeutic intervention.
The efficacy of microbiome-based therapies is profoundly influenced by multiple sources of interindividual variability that determine an individual's baseline microbial community and its responsiveness to intervention. The table below summarizes the key factors contributing to this variability and their therapeutic implications.
Table 1: Key Factors Contributing to Interindividual Variability in Microbiome Therapies
| Factor | Impact on Microbiome | Therapeutic Implications |
|---|---|---|
| Early Life Exposures | Determines foundational microbial succession patterns [91] | Window of opportunity for early intervention; may dictate long-term therapeutic responsiveness |
| Delivery Mode | Vaginal delivery facilitates transfer of Lactobacillus, Prevotella; C-section associated with skin-derived taxa (Staphylococcus, Corynebacterium) [91] | May require customized microbial consortia based on birth history |
| Dietary Patterns | Shapes functional capacity and metabolite production [94] | Background diet must be considered as a confounder in pre/probiotic trials [94] |
| Host Genetics | Genetic variation in carbohydrate-active enzymes (e.g., sucrase-isomaltase) affects nutrient processing [94] | Genotype-based dietary interventions may be necessary for specific patient subgroups |
| Geography/Environment | Influences microbial exposure and community assembly | Therapies may require localization or adaptation to regional microbiomes |
| Medication History | Antibiotics profoundly disrupt community structure and function [91] | May create preconditions for successful engraftment of therapeutic microbes |
The Challenge of Microbial Resilience and Ecological Dynamics
The human gut microbiome exhibits significant resilience, tending to return to its baseline state after perturbation, which poses a substantial challenge for achieving long-term efficacy with microbiome-based therapies [92]. This resilience is governed by ecological factors such as colonization resistance, nutrient availability, and niche specialization. The mucosa-associated microbiota, which differs significantly from the luminal microbiota in composition and function, may represent a particularly stable community that is harder to modify therapeutically [92]. Studies have identified a "crypt-specific core microbiota" (CSCM) in the cecum and proximal colon, composed predominantly of Firmicutes and Proteobacteria, which appears to play a central role in intestinal homeostasis by decreasing proliferation of epithelial cells [92]. This specialized community may be particularly resistant to modification through conventional interventions like probiotics, requiring more targeted approaches.
Methodologies for Assessing Variability and Efficacy
Advanced Multi-Omic Approaches
A multi-omics approach, integrating genomic, transcriptomic, proteomic, and metabolomic data, is essential for moving beyond taxonomic characterization to understand functional responses to microbiome-targeted therapies [94]. Valles-Colomer and colleagues have employed bioinformatics tools to strengthen the link between microbial disturbances and clinical outcomes like depression and quality of life by identifying microbial-derived metabolites with neuroactive potential and clustering biochemical pathways into 56 different gut-brain modules, each corresponding to a single neuroactive compound production or degradation process [94]. This functional approach provides a more nuanced understanding of how interventions affect microbial community function rather than just composition.
Table 2: Core Methodologies for Evaluating Microbiome Therapies
| Methodology | Application | Considerations |
|---|---|---|
| 16S rRNA Sequencing | Taxonomic profiling of microbial communities | Cost-effective but limited functional information |
| Shotgun Metagenomics | Functional potential assessment through gene cataloging | More expensive but provides pathway-level information |
| Metatranscriptomics | Assessment of actively expressed genes | Reveals real-time functional activity |
| Metabolomics | Measurement of microbial metabolite production | Direct readout of functional output |
| Microbial Culturomics | Isolation of novel organisms for therapeutic development | Essential for developing live biotherapeutics |
Experimental Models for Mechanistic Insight
Preclinical models remain essential for establishing causality and elucidating mechanisms of host-microbiome interactions. Gnotobiotic mouse models, colonized with defined human microbial communities, have been particularly valuable for studying the functional impact of specific microbial taxa or communities [92]. For example, neonatal mice inoculated with vaginal microbiota from women with different microbial profiles (Lactobacillus crispatus versus Gardnerella vaginalis and Atopobium vaginae) show differential outcomes in metabolism, immune function, and neurodevelopment [91]. Organoid systems have also emerged as powerful tools for studying host-microbiome interactions at the mucosal interface, with studies demonstrating that LPS from crypt-specific core microbiota species can lead to organoid hypotrophy and stimulation of goblet cell differentiation [92].
Multi-Omic Integration for Microbiome Therapeutic Development
Strategic Approaches for Personalization
Biomarker-Driven Patient Stratification
The development of validated biomarkers is essential for matching patients with appropriate microbiome-targeted therapies. Bacterial DNA in the blood emerges as a potential microbiome biomarker that may identify vulnerable people who could benefit most from a protective dietary intervention [94]. Similarly, assessing microbial capacity to produce or metabolize specific compounds can guide therapy selection; for instance, women with a gut microbial makeup that enables the conversion of soy isoflavones to equol experience a 75% greater reduction in some menopause symptoms when supplemented with isoflavones, compared to someone who lacks those specific microbial species [94]. Beyond microbial biomarkers, host characteristics also inform stratification. Genetic variation in sucrase-isomaltase (SI) and other human carbohydrate-active enzyme genes may predispose to carbohydrate maldigestion across a continuum of mild to severe bowel symptoms, supporting the development of genotype-based dietary interventions [94].
Next-Generation Therapeutic Modalities
Defined Microbial Consortia
Synthetic bacterial communities, defined as manually assembled consortia of two or more bacteria originally derived from the human gastrointestinal tract, represent a promising alternative to traditional probiotics [95]. These communities can model functional, ecological, and structural aspects of native communities within the gastrointestinal tract, occupying varying nutritional niches and providing the host with a stable, robust, and diverse gut microbiota that can prevent pathobiont colonization through colonization resistance [95]. This approach allows for more precise engineering of therapeutic communities with predictable ecological behaviors.
Phage-Based Precision Approaches
Phage therapy, the use of lytic phage to treat bacterial infections, offers exceptional specificity for targeting particular bacterial strains without disrupting the broader microbial community [95]. The rise of antimicrobial resistance has led to renewed interest in phage therapy, and the high specificity of phages for their hosts has spurred interest in using phage-based approaches to precisely modulate the microbiome [95]. This approach may be particularly valuable for conditions driven by specific pathobionts, such as the observation that 64% of women with endometriosis had Fusobacterium nucleatum infiltration in the uterus, with experimental models demonstrating that Fusobacterium infection can cause endometriotic lesion development [94].
Comparison of Microbiome-Targeting Therapeutic Approaches
Assessment Frameworks and Outcome Measures
Evaluating Long-Term Efficacy
Establishing long-term efficacy requires moving beyond short-term compositional changes to assess functional integration and clinical benefits. The following table outlines key parameters for evaluating the long-term success of microbiome-based therapies.
Table 3: Framework for Assessing Long-Term Efficacy of Microbiome Therapies
| Assessment Domain | Key Metrics | Timeline |
|---|---|---|
| Microbial Engraftment | Persistence of therapeutic strains, ecological integration | 1, 3, 6, 12 months post-treatment |
| Functional Impact | Metabolite production, pathway activity, host response | Baseline, 1, 6 months |
| Clinical Outcomes | Disease-specific endpoints, symptom scores, quality of life | 3, 6, 12 months and annually |
| Host-Microbe Interface | Mucosal integrity, immune parameters, inflammation markers | Baseline, 3, 12 months |
| Ecological Stability | Community resilience to perturbation, resistance to rebound | 6, 12 months and after challenges |
Standardization and Reproducibility Considerations
The field suffers from a lack of standardized methodologies, which complicates comparison across studies and contributes to inconsistent results [91]. Controlling for confounders such as transit time, regional changes, and horizontal transmission of the microbiome is essential for improving precision [94]. Several tools have been developed to assess microbial community states, including gut microbiota health indices and disease scores like the GA-map dysbiosis test, though these remain primarily research tools rather than clinically validated measures [94]. Beyond microbial assessment, dietary intake must be rigorously measured in trials of probiotics and prebiotics, as background diet can affect their efficacy through changes in the gut microbiome and in the metabolism and expression of genes of the probiotic [94].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for Microbiome Therapeutic Development
| Reagent/Category | Function/Application | Examples/Specifications |
|---|---|---|
| Gnotobiotic Systems | Establish causality in host-microbe interactions | Germ-free mouse models, humanized microbiota mice |
| Organoid Cultures | Study host-microbe interactions at mucosal interface | Intestinal organoids, gut-on-a-chip systems |
| Bacterial Library | Source of therapeutic candidates | Human Gut Microbiome Project isolates, commercial collections |
| 'Biotic Reagents | Modulate microbial community structure | Probiotics, prebiotics, synbiotics, postbiotics |
| Multi-Omic Kits | Comprehensive community assessment | 16S sequencing, shotgun metagenomics, metabolomics |
Navigating interindividual variability and ensuring long-term efficacy represent the central challenges in the development of effective microbiome-based therapies. Success in this endeavor requires a multifaceted approach that incorporates deep understanding of host-microbiome interactions, sophisticated biomarker-driven patient stratification, and next-generation therapeutic modalities designed for precise microbial manipulation. The continued integration of multi-omic technologies, advanced experimental models, and computational approaches will be essential for translating the promise of microbiome science into reproducible clinical benefits across diverse patient populations. As the field matures, addressing standardization, regulatory frameworks, and functional validation will enable microbiome-based therapies to fulfill their potential as powerful tools in the era of personalized medicine.
All eukaryotic host organisms exist in a state of symbiotic coexistence with complex microbial communities, forming a holistic biological unit known as the holobiont [96]. The intricate interactions between host and microbiome play an integral role in host metabolism, immune regulation, and overall survival, with dysbiosis—a disruption of the microbial community structure—frequently associated with disease states [96]. Understanding these complex relationships requires a shift from reductionistic approaches to integrative frameworks that consider both host and microbial genotypic potential. While multi-omic technologies (metagenomics, metatranscriptomics, proteomics, metabolomics) provide broad insights, they often lack the spatial and temporal resolution necessary to unravel critical metabolic cross-feeding relationships [96]. This technical limitation underscores the critical need for sophisticated computational frameworks that can guide experimental model selection to effectively study host-microbiome interactions in disease contexts. The emerging paradigm recognizes that host-microbe interactions are not merely associative but represent reciprocal adaptations with profound implications for understanding disease mechanisms and developing therapeutic interventions.
Computational and Experimental Modeling Approaches
Genome-Scale Metabolic Modeling (GEM)
Genome-scale metabolic models (GEMs) represent a powerful computational framework for investigating host-microbe interactions at a systems level [96]. A GEM is a mathematical representation of an organism's metabolic network based on its genome annotation, comprising a comprehensive set of biochemical reactions, metabolites, and enzymes that describe metabolic capabilities [96]. Within the framework of constrained-based reconstruction and analysis (COBRA), these models enable the simulation of metabolic fluxes and cross-feeding relationships, allowing researchers to explore metabolic interdependencies and emergent community functions [96].
The primary computational tool within COBRA is flux balance analysis (FBA), which estimates flux through reactions in the metabolic network by assuming steady-state metabolism and optimizing for a defined biological objective, typically maximum biomass production [96]. This approach transforms enzyme kinetics into linear programming problems solvable with specialized solvers (GLPK, Gurobi, CPLEX) [96]. The development of host-microbe GEMs typically involves: (i) collection of genomic and physiological data for host and microbial species; (ii) reconstruction of individual metabolic models using curated databases or automated pipelines; and (iii) integration into a unified computational framework [96].
Table 1: Key Resources for Metabolic Model Reconstruction
| Resource Type | Name | Application | Key Features |
|---|---|---|---|
| Microbial GEM Repositories | AGORA [96], BiGG [96] | Ready-to-use models | Well-curated models for various microbial species |
| Automated Reconstruction Tools | ModelSEED [96], CarveMe [96], gapseq [96] | Draft model generation | Rapid generation from genomic data |
| Eukaryotic Host Reconstruction Tools | RAVEN [96], merlin [96], PlantSEED [96] | Eukaryotic model development | Specialized for complex eukaryotic systems |
| Model Integration Platform | MetaNetX [96] | Namespace standardization | Unified namespace for model components |
Dynamic Covariance Mapping for Interaction Analysis
Dynamic Covariance Mapping (DCM) represents a complementary "top-down" approach to infer microbiome interaction matrices from abundance time-series data [97]. This method addresses the limitation that in natural environments, microbes experience multispecies interactions under complex conditions, often with unculturable members [97]. DCM expands the traditional community interaction matrix to include both intra-species and between-species interactions, crucially accounting for the effects of intra-species clonal variation on community dynamics [97].
The mathematical foundation of DCM describes the microbiome as a system of nonlinear ordinary differential equations where the time derivative of each member's abundance (({\dot{z}}{i})) is expressed as the product of its abundance ((z{i})) and its per-capita growth rate ((\phi_{i})), which is itself a function of all community members' abundances [97]. The core innovation of DCM is that the pairwise covariance between the abundance time series of one member and the time derivative of another's abundance provides an accurate estimate of their interaction strength [97]. When combined with high-resolution chromosomal barcoding techniques that track millions of distinct clonal lineages, DCM can quantify how specific E. coli clones interact with resident gut microbiota during colonization, revealing distinct temporal phases of community destabilization, partial recolonization, and quasi-steady states [97].
Diagram 1: Dynamic Covariance Mapping Workflow
Integrated Framework for Model Selection
Decision Matrix for Model Selection
Selecting the appropriate modeling approach depends on multiple factors including research question, data availability, and resolution requirements. The framework presented below enables systematic selection based on project-specific parameters.
Table 2: Model Selection Decision Matrix
| Research Objective | Recommended Primary Approach | Complementary Approach | Temporal Resolution | Data Requirements |
|---|---|---|---|---|
| Metabolic Mechanism Elucidation | GEM (COBRA/FBA) | ¹³C Metabolic Flux Analysis [96] | Steady-State | Genome annotations, physiological data [96] |
| Community Dynamics & Stability | Dynamic Covariance Mapping | Longitudinal 16S rRNA/shotgun sequencing [97] | High-Resolution Time Series | Abundance time-series, barcoding data [97] |
| Prediction of Metabolic Cross-Feeding | Integrated Host-Microbe GEM | Labeling experiments (¹³C, ¹âµN) [96] | Steady-State with Perturbations | Individual GEMs, exchange metabolite data [96] |
| Intra-Species Variation Effects | DCM with Chromosomal Barcoding | Whole-genome sequencing [97] | High-Resolution (Clonal Level) | Barcoded populations, high-resolution tracking [97] |
| Therapeutic Target Identification | GEM with Constraint Integration | In vivo validation (gnotobiotic models) [96] | Context-Dependent Steady States | Multi-omic data (transcriptomics, metabolomics) [96] |
Technical Implementation Considerations
Implementing these modeling approaches requires careful consideration of technical challenges. For GEM development, microbial metabolic models are relatively easier to derive due to high-quality repositories (AGORA, BiGG), while reconstructing host metabolic models, particularly for eukaryotic cells, is more complex due to incomplete genome annotations, biomass composition definition, and compartmentalization of metabolic processes [96]. Integration of host and microbial models presents additional challenges as models from different sources often use distinct nomenclatures for metabolites, reactions, and genes [96].
For DCM implementation, the critical requirement is high-resolution lineage tracking, achieved through chromosomal barcoding techniques that integrate hundreds of thousands of distinct DNA barcodes into populations, enabling tracking of clonal lineage dynamics at unprecedented resolution [97]. This approach has proven particularly useful in quantifying how bacterial populations adapt during evolution and in response to environmental perturbations [97].
Diagram 2: Host-Microbe GEM Integration Framework
Experimental Protocols and Methodologies
Protocol for Integrated Host-Microbe GEM Reconstruction
Objective: To construct an integrated host-microbe metabolic model capable of simulating metabolic interactions in a disease context.
Materials and Reagents:
- High-quality genome annotations for host and microbial species
- Curated metabolic databases (e.g., KEGG, MetaCyc)
- Computational resources with linear programming solvers (GLPK, Gurobi, or CPLEX)
Procedure:
- Data Collection and Curation
- Collect genome sequences, metagenome-assembled genomes (MAGs), and physiological data for both host and microbial species [96]
- Annotate metabolic functions and identify transport reactions
Draft Model Reconstruction
- For microbial models: Use automated reconstruction tools (CarveMe, ModelSEED, gapseq) or retrieve from curated repositories (AGORA, BiGG) [96]
- For host models: Use eukaryotic-specific tools (RAVEN, merlin, PlantSEED) followed by extensive manual curation [96]
- Define biomass composition appropriate for the specific host and microbial cells
Model Integration and Gap-Filling
- Standardize nomenclature across models using MetaNetX to resolve inconsistencies [96]
- Establish metabolite exchange reactions between host and microbial compartments
- Perform gap-filling to ensure metabolic functionality
- Detect and remove thermodynamically infeasible reaction cycles
Context-Specific Constraining
- Incorporate experimental data (transcriptomics, proteomics, metabolomics) to constrain reaction fluxes
- Define nutritional environment (diet, medium composition) relevant to the disease context
- Set physiological constraints based on experimental measurements
Model Simulation and Validation
- Perform flux balance analysis to predict metabolic fluxes
- Validate predictions against experimental data (e.g., ¹³C flux measurements, metabolite consumption/excretion rates)
- Iteratively refine model based on discrepancies
Protocol for Dynamic Covariance Mapping with Chromosomal Barcoding
Objective: To quantify inter- and intra-species interactions during microbial colonization or perturbation using high-resolution lineage tracking.
Materials and Reagents:
- Barcoded microbial populations (e.g., E. coli with Tn7 transposon-integrated barcodes) [97]
- Germ-free or gnotobiotic mouse models
- DNA extraction kits and high-throughput sequencing reagents
- Computational resources for time-series analysis
Procedure:
- Barcoded Population Preparation
- Generate barcoded microbial populations using Tn7 transposon machinery to integrate ~500,000 distinct chromosomal DNA barcodes [97]
- Verify barcode diversity and population size (typically 10⸠cells for adequate representation)
In Vivo Colonization Experiment
- Introduce barcoded populations to germ-free, antibiotic-perturbed, or innate microbiota mouse models [97]
- Collect samples at high temporal resolution (e.g., daily for first week, then weekly)
- Record abundance measurements for all community members
DNA Extraction and Barcode Sequencing
- Extract genomic DNA from collected samples
- Amplify and sequence barcode regions using high-throughput sequencing
- Process sequencing data to quantify barcode abundances over time
Dynamic Covariance Calculation
- Compute time derivatives of abundance for each community member (including clonal lineages)
- Calculate pairwise covariance between each member's abundance and the growth rates of others [97]
- Construct time-dependent community interaction matrix
Stability and Phase Analysis
- Perform eigenvalue decomposition of the community matrix to assess stability [97]
- Identify distinct temporal phases based on stability transitions
- Correlate phase transitions with specific ecological events or perturbations
Genetic Validation
- Perform whole-genome sequencing of dominant clonal clusters
- Identify genetic mutations underlying fitness advantages
- Validate specific gene-function relationships through targeted experiments
Table 3: Essential Research Reagents and Computational Tools
| Category | Item/Resource | Function/Application | Key Features |
|---|---|---|---|
| Experimental Models | Germ-free/Gnotobiotic Mice [96] | In vivo host-microbe interaction studies | Controlled microbial exposure |
| Organ-on-a-Chip/Organoids [96] | Reduced complexity systems | Isolate specific host-microbe interactions | |
| Molecular Biology Tools | Chromosomal Barcoding System [97] | High-resolution lineage tracking | Tn7 transposon with ~500,000 unique barcodes |
| ¹³C/¹âµN Labeled Substrates [96] | Metabolic flux analysis | Track metabolite fate in complex communities | |
| Computational Resources | COBRA Toolbox [96] | Metabolic modeling and FBA | MATLAB-based ecosystem for constraint-based modeling |
| DCM Analysis Pipeline [97] | Community interaction inference | R/Python implementation for covariance mapping | |
| Data Resources | AGORA/BiGG Models [96] | Curated metabolic models | Ready-to-use GEMs for diverse microbes |
| MetaNetX [96] | Metabolic namespace standardization | Cross-references between major metabolic databases |
Applications in Disease Research and Therapeutic Development
The integrated framework presented here enables researchers to select optimal modeling strategies for specific disease contexts. GEM approaches are particularly valuable for understanding how microbial metabolism influences host metabolic diseases (e.g., obesity, diabetes) or for predicting the metabolic consequences of dietary interventions [96]. The ability to simulate system-level metabolism makes GEMs powerful tools for identifying potential therapeutic targets that modulate host-microbe metabolic interactions.
DCM approaches excel in infectious disease contexts or situations where community stability is disrupted, such as following antibiotic treatment or during pathogenic invasion [97]. The method's ability to identify distinct temporal phases of community destabilization and recovery provides insights into critical intervention windows. Furthermore, DCM's capacity to resolve intra-species interactions enables understanding of how specific bacterial clones achieve dominance during disease states, with implications for targeting particularly fit subpopulations.
The combination of these approaches—using DCM to identify critical interaction networks and timepoints, followed by GEM to elucidate the underlying metabolic mechanisms—represents a powerful strategy for advancing our understanding of host-microbiome interactions in disease. This framework provides a systematic approach for researchers to select the most appropriate models based on their specific experimental goals, available data, and resolution requirements, ultimately accelerating the translation of microbiome research into clinical applications.
Comparative Analysis and Validation of Microbiome-Based Biomarkers and Therapies
The study of host-microbiome interactions represents one of the most rapidly advancing frontiers in biomedical research, with profound implications for understanding health and disease. As researchers seek to translate correlational findings into causative mechanisms and therapeutic applications, the need for robust experimental models has never been greater. Cross-model validation—the systematic comparison of insights across different experimental systems—has emerged as a critical methodology for strengthening scientific conclusions and accelerating translational progress. This approach is particularly vital in microbiome research, where the complexity of microbial communities and their interactions with host physiology presents unique challenges for experimental modeling [98].
Traditional biomedical research has heavily relied on animal models, particularly rodents, for preclinical investigations. While these models have contributed valuable insights into host-microbiome interactions, they come with well-documented limitations, including species-specific differences in gut anatomy, microbial composition, and immune system function [99]. These differences can significantly impact the translatability of findings from animal models to human applications. The high failure rate of drugs that advance from animal studies to human trials—approximately 95% according to recent analyses—underscores the critical need for more predictive model systems and rigorous validation frameworks [100] [101].
The emergence of sophisticated human-relevant models, including organoids, organs-on-chips, and complex in silico simulations, offers promising alternatives to traditional animal models. However, each of these systems has its own strengths and limitations, and no single model perfectly recapitulates the complexity of human biology. Cross-model validation provides a framework for leveraging the complementary advantages of different experimental systems, enabling researchers to distinguish robust biological signals from model-specific artifacts and to build greater confidence in their findings before proceeding to costly clinical trials [102] [98].
This whitepaper provides a comprehensive technical guide to cross-model validation strategies in host-microbiome research. We examine the comparative strengths and limitations of animal models, organoids, organs-on-chips, and human trials; present detailed methodological frameworks for validation; and explore how advanced computational approaches are transforming validation paradigms. Through standardized validation protocols and iterative model refinement, researchers can enhance the predictive power of their experimental systems and accelerate the translation of microbiome research into clinical applications.
Comparative Analysis of Experimental Models
A critical understanding of the distinct capabilities and limitations of available experimental models is fundamental to effective cross-model validation in host-microbiome research. The table below provides a systematic comparison of key models across multiple dimensions relevant to studying host-microbiome interactions.
Table 1: Comparative Analysis of Experimental Models in Host-Microbiome Research
| Model Type | Key Strengths | Major Limitations | Microbiome Application Examples | Translational Concordance |
|---|---|---|---|---|
| Animal Models | Whole-system physiology; Complex immune responses; Behavioral readouts | Species-specific differences in gut anatomy & microbiome; Artificial disease induction; Controlled environments lacking human diversity | Parkinson's disease models showing GI symptoms preceding motor manifestations; Inflammatory Bowel Disease models [99] | Limited; ~95% failure rate from animal to human trials [100] |
| Organoids | Human-derived cells; Preserve patient-specific genetics; 3D architecture resembling native tissue | Often lack immune components & microbial cues; Limited lifespan; Variable reproducibility between labs | Colonic organoids for studying epithelial-microbe interactions; Gut-brain axis modeling [103] | Promising but requires further validation; Improving with standardization efforts [104] |
| Organs-on-Chips | Dynamic fluid flow & mechanical forces; Human cells; Multi-tissue integration capability | Technically complex; Limited throughput; High cost; Still reductionist compared to whole organisms | Vascularized liver cancer-on-a-chip for evaluating embolic agents; Lung-on-a-chip with immune components [101] | Shows 80% predictive accuracy for human physiology vs. 30% for animal models in some systems [101] |
| Human Trials | Direct human relevance; Complete physiological context; Clinical endpoints | Ethical constraints; High cost & time requirements; Limited mechanistic insight; High variability | Machine learning meta-analysis of gut microbiome in Parkinson's disease (4,489 samples) [105] | Gold standard but impractical for early discovery |
The integration of computational approaches has introduced additional dimensions to this landscape. Machine learning models trained on large-scale human microbiome datasets can achieve impressive classification accuracy for disease states (average AUC of 71.9% within studies), though their performance often decreases when applied across different study populations (average AUC of 61% in cross-study validation) [105]. This pattern highlights both the promise and limitations of in silico models, which are increasingly being incorporated into cross-model validation frameworks.
Recent advances in model systems are rapidly addressing some of these limitations. For instance, the development of immune-component-integrated organoids and organs-on-chips represents a significant step forward. A notable example is a lung-on-a-chip platform that incorporates a functional immune system, enabling researchers to observe how human lungs respond to threats, how inflammation spreads, and how healing begins—addressing a critical gap in traditional in vitro models [101]. Similarly, initiatives like the NIH's $87 million Standardized Organoid Modeling Center aim to overcome reproducibility challenges through technologies including artificial intelligence, robotics, and standardized protocols [104] [101].
Methodological Framework for Cross-Model Validation
Implementing robust cross-model validation requires systematic approaches that account for the unique characteristics of each experimental system while enabling meaningful comparisons across platforms. The following section outlines standardized protocols and computational frameworks for validating findings across animal, organoid, organ-on-chip, and human trial data.
Standardized Validation Protocols
Multi-scale Microbiome Analysis Protocol: This protocol enables consistent comparison of microbiome findings across different model systems. The process begins with standardized sample collection and preservation methods, followed by DNA extraction using kits validated for different sample types (fecal, luminal content, organoid supernatant). For 16S rRNA sequencing, amplify the V4 region using 515F/806R primers with dual-index barcoding. For shotgun metagenomics, use library preparation kits that minimize host DNA amplification. Process sequencing data through a standardized bioinformatics pipeline: quality filter with Trimmomatic, denoise with DADA2 (for 16S) or remove host reads with KneadData (for metagenomics), then assign taxonomy using SILVA (16S) or MetaPhlAn (metagenomics). Analyze alpha diversity (Shannon, Chao1) and beta diversity (Bray-Curtis, UniFrac) metrics, comparing across models using PERMANOVA with appropriate multiple testing corrections [105].
Host Response Profiling Protocol: To enable cross-model comparison of host responses to microbiome perturbations, implement a multi-omics profiling approach. For transcriptomics, extract RNA using column-based methods with DNase treatment, followed by library preparation with ribosomal RNA depletion. For metabolomics, use dual extraction (methanol/chloroform/water) to cover both hydrophilic and hydrophobic metabolites, analyzing via LC-MS with appropriate internal standards. Process data through standardized pipelines: for RNA-seq, align with STAR, quantify with featureCounts, and perform differential expression with DESeq2; for metabolomics, perform peak picking with XCMS, annotate with CAMERA, and integrate with GNPS for molecular networking. Compare pathway enrichment across models using GSEA with Hallmark and KEGG gene sets, focusing on conserved responses across systems [98].
Barrier Function Assessment Protocol: Given the importance of barrier integrity in host-microbiome interactions, implement standardized barrier assessment across models. For animal models, measure intestinal permeability in vivo using FITC-dextran (4 kDa) gavage followed by serum measurement. For organoids, quantify barrier function using transepithelial electrical resistance (TEER) measurements or fluorescent dextran flux assays. For gut-on-chip models, use integrated electrodes for continuous TEER monitoring alongside periodic tracer flux measurements. Normalize all measurements to baseline values and include positive controls (e.g., EDTA-induced barrier disruption) to enable cross-model comparison [102].
Machine Learning Frameworks for Cross-Study Validation
The high dimensionality of microbiome data and the heterogeneity across studies present significant challenges for cross-model validation. Machine learning frameworks offer powerful approaches for addressing these challenges, as demonstrated by a recent large-scale meta-analysis of gut microbiome in Parkinson's disease encompassing 4,489 samples from 22 studies [105].
Cross-Study Validation Pipeline: Implement a standardized machine learning workflow to assess the generalizability of findings across models. First, preprocess data to account for technical variability: for 16S data, rarefy to even sequencing depth; for metagenomics, convert to counts per million. For each individual study/dataset, train multiple classifier types (Random Forest, Ridge Regression, LASSO) using within-study cross-validation (5-fold, repeated 10 times). Evaluate performance using area under the receiver operating characteristic curve (AUC). Then, perform cross-study validation by training on one study and testing on all others, calculating cross-study AUC for each pair. Finally, implement leave-one-study-out (LOSO) validation where models are trained on all but one study and tested on the held-out study, providing a more robust estimate of generalizability [105].
Table 2: Performance of Machine Learning Models in Cross-Study Microbiome Analysis
| Model Approach | Average Within-Study AUC | Average Cross-Study AUC | Key Findings | Recommended Applications |
|---|---|---|---|---|
| 16S Data (Random Forest) | 72.3% ± 11.7 | 61% | High variability between studies; Models from large studies generalize better | Preliminary screening; Study-specific hypothesis generation |
| Shotgun Metagenomics (Ridge Regression) | 78.3% ± 6.5 | 68% (LOSO) | Superior generalizability vs. 16S; More consistent feature importance | Biomarker validation; Cross-study meta-analyses |
| Multi-Study Ensemble Models | 75.2% ± 8.1 | 71.5% (LOSO) | Improved generalizability; More robust feature selection | Clinical translation; Diagnostic development |
| Pathway-Based Models | 70.1% ± 5.3 | 66.8% (LOSO) | Better biological interpretability; Conserved functional changes | Mechanistic studies; Therapeutic target identification |
Feature Concordance Analysis: To identify robust microbial signatures that translate across models, implement a feature importance concordance analysis. For each cross-study validation, extract feature importance scores (e.g., regression coefficients, Gini importance). Calculate concordance scores using rank-based methods (Spearman correlation) across study pairs. Identify features consistently ranked as important across multiple validations (e.g., in >70% of cross-study pairs). Validate these conserved features using independent methodological approaches (e.g., qPCR, culture-based assays) when possible [105].
Advanced Technical Approaches and Reagent Solutions
Successful cross-model validation in host-microbiome research depends on specialized reagents, technologies, and methodologies tailored to the unique challenges of working across experimental systems. The following section details essential research tools and advanced technical approaches that enable robust comparative analyses.
Research Reagent Solutions for Cross-Model Validation
Table 3: Essential Research Reagents for Cross-Model Microbiome Studies
| Reagent/Category | Function | Application Notes | Model Compatibility |
|---|---|---|---|
| DNA/RNA Shield | Preserves microbiome composition and nucleic acid integrity during sample collection and storage | Critical for standardized comparisons across models with different processing timelines; Enables room temperature storage during transport | Animal studies, Human trials, Organoid experiments |
| Robotic Liquid Handlers | Enables high-throughput, reproducible sample processing and assay setup | Reduces technical variability in organoid and organ-on-chip studies; Essential for scaling validation experiments | Organoid screening, High-content imaging, Organ-on-chip systems |
| 16S rRNA PCR Primers (515F/806R) | Amplifies V4 region for bacterial community profiling | Standardized primers enable cross-study comparisons; Validated for diverse sample types | All biological models, In silico database integration |
| Cell Culture Media Supplements | Supports growth of specific microbial taxa or host cells | Critical for organoid/on-chip models; Requires optimization for different microbial communities | Organoid cultures, Organ-on-chip maintenance |
| Metabolomics Standards | Enables quantification and identification of microbial metabolites | Includes SCFA mixtures, bile acid panels, neurotransmitter analogs; Essential for functional validation | Animal models, Organ-on-chip systems, Human samples |
| TEER Measurement Electrodes | Quantifies epithelial barrier integrity in real-time | Different sizes/configurations needed for transwell vs. organ-on-chip applications | Gut organoids, Intestinal-on-chip models, Ex vivo tissues |
| CRISPR-Cas9 Systems | Enables genetic manipulation of host or microbial components | Essential for causal validation; Used with organoids for disease modeling | Organoid engineering, Bacterial genome editing |
Advanced Multi-Model Integration Techniques
CRISPR-Enhanced Organoid Models: The combination of organoid technology with CRISPR-Cas9 systems enables precise genetic manipulation for causal validation of host-microbiome interactions. A standard protocol involves generating patient-derived intestinal organoids from biopsy samples, expanding them in Matrigel domes with IntestiCult organoid growth medium. For genetic manipulation, electroporate organoids with ribonucleoprotein complexes (Cas9 protein + sgRNA) targeting genes of interest, then culture for 7-10 days to allow phenotype development. Validate edits via Sanger sequencing and functional assays. These engineered organoids can then be exposed to defined microbial communities or specific bacterial strains to investigate gene-microbe interactions in a human-relevant system [101].
Multi-Omics Data Integration: Integrating data across different molecular levels and model systems requires sophisticated computational approaches. Implement an iterative multi-omics integration pipeline that includes: (1) batch effect correction using ComBat or similar methods to account for technical variability across platforms; (2) multivariate statistical analysis (PLS-DA, O2PLS) to identify correlated signals across omics layers; (3) pathway enrichment analysis using MetaboAnalyst and GSEA to identify conserved biological processes; and (4) network inference using SPIEC-EASI or similar algorithms to reconstruct host-microbe interaction networks. This approach enables identification of robust, cross-model signatures while accounting for platform-specific technical artifacts [98].
Organ-on-Chip Microphysiological Systems: Advanced organ-on-chip platforms now incorporate functional immune systems and microbial components to better model host-microbiome interactions. A state-of-the-art gut-on-chip protocol involves: (1) seeding human intestinal epithelial cells (Caco-2 or primary cells) on a porous membrane within a microfluidic device; (2) establishing flow of medium through the apical and basal channels to create physiological shear stress; (3) adding immune cells (peripheral blood mononuclear cells or dendritic cells) to the basal channel; and (4) introducing defined microbial communities to the apical channel. These systems enable real-time monitoring of barrier function (via integrated TEER electrodes), host responses (via cytokine sampling), and microbial dynamics (via effluent sampling) under conditions that more closely mimic the human intestinal microenvironment [101] [106].
Visualization of Cross-Model Validation Workflows
Effective cross-model validation requires clearly defined workflows that systematically integrate data from multiple experimental systems. The following diagrams illustrate key processes and biological relationships in host-microbiome research.
Cross-Model Validation Workflow
Host-Microbiome Signaling in Gut-Brain Axis
Cross-model validation represents a paradigm shift in host-microbiome research, moving beyond the limitations of single-model systems to build more robust, translatable scientific knowledge. By systematically comparing findings across animal models, organoids, organs-on-chips, and human trials, researchers can distinguish fundamental biological mechanisms from model-specific artifacts, ultimately accelerating the translation of microbiome research into clinical applications. The integration of advanced computational approaches, particularly machine learning frameworks for cross-study validation, further enhances our ability to identify conserved signals across diverse experimental systems.
The field is rapidly evolving toward more integrated validation frameworks, as evidenced by recent initiatives such as the NIH's $87 million investment in a Standardized Organoid Modeling Center and the FDA's acceptance of organ-on-a-chip data for drug development applications [104] [101]. These developments, coupled with advances in single-cell technologies, multi-omics integration, and complex in vitro models, promise to further enhance the predictive power of preclinical research. However, significant challenges remain, including the need for better standardization, improved model complexity, and more sophisticated computational frameworks for data integration.
Looking forward, the most impactful advances in cross-model validation will likely come from deeper integration of human-relevant data throughout the research pipeline. Approaches such as "Phase 0 Human Trials" using perfused human organs [106], digital twin technologies [102], and advanced machine learning models trained on large-scale human datasets [105] offer promising paths toward more predictive validation frameworks. By continuing to refine these approaches and establish standards for cross-model validation, the research community can enhance the efficiency and success rate of translating microbiome discoveries into clinical applications that improve human health.
As the field progresses, researchers should prioritize the development of validation standards that are both rigorous and practical, enabling consistent comparison across laboratories and model systems. Through collaborative efforts across academia, industry, and regulatory agencies, cross-model validation can evolve from a best practice to a standardized framework that enhances the predictive power of host-microbiome research and accelerates the development of microbiome-based therapeutics.
Multi-omics technologies are revolutionizing our understanding of complex diseases by enabling comprehensive profiling of host and microbial molecules. This case study examines how integrated analyses of genomics, transcriptomics, proteomics, metabolomics, and microbiomics are revealing the functional signatures of host-microbiome interactions in Inflammatory Bowel Disease (IBD) and Prediabetes. These approaches are uncovering novel pathogenic mechanisms, identifying potential biomarkers for early detection, and informing the development of personalized therapeutic strategies for these complex conditions. The insights gained underscore the necessity of moving beyond single-omic analyses to capture the intricate biological networks underlying chronic disease progression.
The investigation of "omes" and "omics" represents a paradigm shift in biomedical research, focusing on the totality of any particular biological field and its study. While single-omics analyses can provide valuable information, the integration of several omics—multi-omics—enables a more comprehensive view of disease mechanisms by capturing the complex interactions between host physiology, genetics, and microbial communities [107]. This approach is particularly valuable for conditions like IBD and Prediabetes, which involve dysfunctional interactions between host systems and commensal microorganisms.
The Integrative Human Microbiome Project (iHMP) has pioneered longitudinal multi-omic studies to explore host-microbiome dynamics in both health and disease. This research begins to elucidate mechanisms of host–microbiome interactions and provides unique data resources representing a paradigm for future multi-omic studies of the human microbiome [41]. Such initiatives have demonstrated that taxonomic composition alone often fails to adequately correlate with host phenotype, which is better predicted by integrating data on microbial molecular function and personalized strain-specific makeup [41].
Multi-Omic Signatures in Prediabetes
Pathophysiological Context and Diagnostic Challenges
Prediabetes represents an intermediate metabolic state characterized by elevated blood glucose levels that fall below the threshold for diabetes diagnosis. It encompasses impaired fasting glucose (IFG), impaired glucose tolerance (IGT), or both, with approximately 70% of individuals progressing to diabetes over time [108]. The pathophysiology involves insulin resistance and β-cell dysfunction, with emerging evidence suggesting chronic low-grade inflammation and adipose tissue dysfunction also play pivotal roles [108].
Current diagnostic methods relying on hemoglobin A1c (HbA1c), fasting glucose, or oral glucose tolerance tests have significant limitations. HbA1c measurements can be influenced by biological variability and certain medical conditions, while by the time hyperglycemia is detected using standard methods, most pancreatic β cells have often undergone irreversible damage [108]. These limitations have driven the search for novel multi-omics biomarkers that can enable earlier detection and intervention.
Key Microbial and Molecular Alterations
Multi-omics studies have revealed distinctive host and microbial signatures in prediabetes. A longitudinal study profiling 106 healthy and prediabetic individuals over approximately four years revealed that insulin-resistant participants respond differently than insulin-sensitive participants during respiratory viral infections, and identified early personal molecular signatures that preceded T2D onset, including the inflammation markers interleukin-1 receptor antagonist (IL-1RA) and high-sensitivity C-reactive protein (CRP) paired with xenobiotic-induced immune signaling [109].
A 2025 integrated analysis of gut microbiota and metabolomics in prediabetes identified specific microbial alterations, including higher abundance of Megamonas funiformis and Parabacteroides merdae in the prediabetes group. Importantly, this study revealed Flavonifractor plautii's role in modulating blood glucose through influencing carbohydrate metabolism, highlighting how specific gut microbes may directly impact host metabolic pathways [110].
Table 1: Multi-Omic Alterations in Prediabetes
| Omic Layer | Specific Alterations | Functional Implications |
|---|---|---|
| Microbiome | ↑ Megamonas funiformis, ↑ Parabacteroides merdae; ↓ Akkermansia over time [110] [109] | Altered gut barrier function; modified carbohydrate metabolism |
| Metabolome | 795 metabolites altered, primarily in carbohydrate and lipid metabolism [110] | Disrupted energy metabolism; potential lipotoxicity |
| Proteome | ↑ IL-1RA, ↑ high-sensitivity CRP [109] | Systemic inflammation; early warning of dysregulation |
| Transcriptome | Xenobiotic-induced immune signaling [109] | Environmental factor response; detox pathway activation |
Longitudinal Dynamics and Disease Progression
A prospective 4-year study of 486 European patients with prediabetes revealed significant temporal changes in gut microbiota, including declines in bacterial and viral species richness and microbial pathway diversity. Despite these reductions, researchers identified 80 dominant core bacterial species and 78 core microbial pathways that persisted in 99% of individuals, representing a resilient component of the gut microbiota. Importantly, estimates of gut bacterial microbiota dynamics significantly correlated with temporal impairments in host metabolic health, suggesting a potential link between microbial community changes and disease progression [111].
The dynamics of these multi-omic signatures also show potential for predicting responses to interventions. A study on dietary inulin supplementation in prediabetic individuals found that the large inter-individual variability in metabolic effects was explained by differences in baseline glycemic status and microbiome-metabolome (MIME) signatures. Specifically, improved glycemic outcomes depended on the abundance of certain bacterial taxa (Blautia, Eubacterium halii group, Lachnoclostridium), serum concentrations of branched-chain amino acid derivatives and asparagine, and fecal concentrations of indole and other volatile organic compounds [112].
Multi-Omic Signatures in Inflammatory Bowel Disease
Pathobiological Framework and Microbial Ecologies
Inflammatory Bowel Disease, encompassing Crohn's disease and ulcerative colitis, represents a chronic immune-mediated inflammatory condition of the gastrointestinal tract with a complex, unpredictable, and heterogeneous nature. The investigation of host-microbiota cross-talk through integrating different interacting components—termed the interactome—has emerged as a systematic strategy to reveal key disease drivers [44].
Multi-omics approaches have revealed that IBD involves alterations across multiple biological layers. At the microbial composition level, patients with IBD typically show reduced diversity and richness of commensal bacteria (e.g., Firmicutes and Bacteroides), with an expansion of potentially pathogenic microorganisms (e.g., Proteobacteria) [44]. Core species including Roseburia intestinalis, Faecalibacterium prausnitzii, and Akkermansia muciniphila consistently show decreased abundances during both disease activity and remission stages, representing long-term gut microbial dysregulations in IBD [44].
Multi-Omic Dysregulation Patterns
Beyond simple taxonomic changes, multi-omics analyses have revealed functional disturbances in IBD that may not be evident from composition data alone. Microbial genomic studies have identified specific genetic variations that influence microbial fitness and pathogenicity. For instance, an increased copy number of a gene encoding for a major drug efflux protein in Roseburia inulinivorans and HlyD in Bacteroides uniformis (a component of RTX hemolytic toxin secretion) has been observed in IBD, potentially contributing to antibiotic resistance and pathogenicity [44].
Integration of microbial DNA and RNA measurements has successfully mirrored IBD pathology in real-time. Researchers have identified that in active colitis, bacteria display consistent patterns between genomic and transcriptomic levels for genes involved in nutrient deprivation responses, antimicrobial peptide production, and oxidative stress responses, providing reliable microbial markers to monitor disease activity [44].
Table 2: Multi-Omic Dysregulation in Inflammatory Bowel Disease
| Omic Layer | Specific Alterations | Functional Consequences |
|---|---|---|
| Metagenome | ↓ Microbial diversity; ↓ Firmicutes/Bacteroides; ↑ Proteobacteria [44] | Ecosystem instability; potential pathogen overgrowth |
| Metatranscriptome | Activated stress response genes; altered expression in nutrient deprivation pathways [44] | Microbial community adaptation to inflammatory environment |
| Metaproteome | Enriched orthologs of hemolysin, drug efflux systems [44] | Enhanced pathogenicity and survival under antibiotic pressure |
| Metabolome | Distinct SCFA profiles; bile acid transformations [44] | Modified signaling to host immune and epithelial cells |
Challenges in IBD Multi-Omics Integration
Despite substantial progress, current IBD multi-omics studies face significant challenges. Most reports remain based on simple associations of descriptive retrospective data from cross-sectional patient cohorts rather than longitudinally collected prospective datasets [107]. This limitation has hindered the translation of multi-omics findings into clinically useful tools, as no clinically applicable IBD genetic markers have been identified despite extensive genomics research [107].
True integration—moving beyond mere association to establish causal relationships—remains elusive in IBD multi-omics. As noted by Fiocchi (2023), "Regardless of the types of omes being analyzed, the majority of current reports are still based on simple associations of descriptive retrospective data from cross-sectional patient cohorts rather than more powerful longitudinally collected prospective datasets" [107]. This highlights the need for more sophisticated study designs and analytical approaches.
Comparative Analysis of Multi-Omic Signatures
Common Themes Across Disease States
Despite their different clinical manifestations, IBD and Prediabetes share several common features in their multi-omic signatures. Both conditions demonstrate reduced microbial diversity and consistent alterations in specific bacterial taxa, including decreases in anti-inflammatory butyrate-producers like Faecalibacterium prausnitzii and Akkermansia muciniphila [44] [109]. Both diseases also exhibit strong inflammatory components reflected across multiple omic layers, with distinct proteomic and metabolomic signatures of immune activation.
Another common theme is the individual variability in multi-omic signatures, which complicates the identification of universal biomarkers but offers opportunities for personalized medicine approaches. In both conditions, the integration of multiple omic layers provides better predictive power for disease progression and treatment response than any single omic measurement alone.
Distinctive Features
While sharing common themes, these conditions also display distinctive multi-omic signatures reflective of their different pathophysiologies. Prediabetes shows stronger signatures related to carbohydrate and lipid metabolism in the metabolome, while IBD exhibits more pronounced alterations in microbial virulence factors and host defense pathways. The longitudinal dynamics also differ, with prediabetes showing gradual progression of omic changes alongside metabolic decline, while IBD often demonstrates more fluctuating patterns corresponding to disease flares and remissions.
Experimental Methodologies and Workflows
Standardized Multi-Omic Profiling Protocols
Comprehensive multi-omic studies require standardized protocols for sample collection, processing, and data generation. The Integrative Human Microbiome Project established rigorous methodologies that can be adapted for studying host-microbiome interactions in various disease contexts.
Table 3: Core Methodologies for Multi-Omic Profiling
| Omic Layer | Core Technology | Key Outputs | Sample Types |
|---|---|---|---|
| Metagenomics | Shotgun sequencing (Illumina HiSeq) [111] | Taxonomic profiles; functional potential | Stool; mucosal biopsies |
| Metatranscriptomics | RNA sequencing [44] | Gene expression activity; pathway activation | Stool; mucosal biopsies |
| Proteomics | Sequential window acquisition of all theoretical mass spectra (SWATH-MS) [109] | Protein abundance; post-translational modifications | Plasma; serum; tissue |
| Metabolomics | Untargeted LC-MS/MS [109] [110] | Metabolite identification; pathway analysis | Plasma; serum; stool |
| Host Transcriptomics | Ribo-minus RNA-seq [109] | Gene expression; signaling pathways | PBMCs; tissue biopsies |
Integrated Data Analysis Workflows
The analysis of multi-omic data requires specialized computational workflows that can integrate diverse data types while accounting for technical variability and biological complexity. Key steps include:
- Quality Control: Filtering low-quality sequences or signals using tools like KneadData [111]
- Normalization: Accounting for technical variation using methods like centered log-ratio transformation for compositional data [112]
- Feature Selection: Identifying informative variables while reducing dimensionality
- Data Integration: Combining multiple omic datasets using statistical or network-based approaches
- Functional Annotation: Linking findings to biological pathways and mechanisms
Diagram 1: Multi-Omic Data Generation and Analysis Workflow. This workflow illustrates the parallel processing of different molecular layers from sample collection through data integration and biological interpretation.
Visualization Approaches for Multi-Omic Data
Metabolic Pathway Mapping
Effective visualization is crucial for interpreting complex multi-omic data. Tools like the Cellular Overview in Pathway Tools enable simultaneous visualization of up to four types of omics data on organism-scale metabolic network diagrams. These tools depict metabolic reactions, pathways, and metabolites as described in metabolic pathway databases, with different omics datasets painted onto distinct "visual channels" of the diagram [113].
For example, transcriptomics data can be displayed by coloring reaction arrows, proteomics data as reaction arrow thickness, and metabolomics data as metabolite node colors. This approach allows researchers to directly observe changes in activation levels of different metabolic pathways in the context of the full metabolic network, facilitating hypothesis generation about pathway dysregulation in disease states [113].
Spatial Data Visualization
For spatially resolved data, such as spatial transcriptomics, specialized visualization tools like Spaco (Spatially Aware Colorization) incorporate spatial relationships into color assignment decisions. This approach uses a Degree of Interlacement metric to construct a weighted graph that evaluates spatial relationships among different cell types, refining color assignments to enhance perceptual discrimination of biologically distinct neighboring cells [114].
Diagram 2: Multi-Omic Data Visualization Framework. This framework shows the processing steps from raw data to integrated visualization, highlighting the mapping of different data types to distinct visual channels.
Core Reagents and Technologies
Successful multi-omics research requires carefully selected reagents and technologies that maintain sample integrity while enabling comprehensive molecular profiling. The following table outlines essential resources for conducting multi-omics studies of host-microbiome interactions in IBD and Prediabetes.
Table 4: Essential Research Resources for Multi-Omic Studies
| Category | Specific Resource | Application | Key Considerations |
|---|---|---|---|
| DNA Extraction | NucleoSpin Soil DNA extraction kit [111] | Microbial DNA isolation from stool | Maintains integrity of diverse bacterial species |
| Sequencing | Illumina HiSeq 4000 system (2×150 bp) [111] | Shotgun metagenomic sequencing | Sufficient depth for low-abundance taxa |
| Proteomics | SWATH-MS (Sequential Window Acquisition) [109] | High-throughput protein quantification | Captures broad dynamic range of plasma proteins |
| Metabolomics | Untargeted LC-MS/MS [109] | Comprehensive metabolite profiling | Complementary NMR for validation |
| RNA Preservation | RNAlater or immediate freezing at -80°C [109] | Preserves transcriptomic signatures | Critical for accurate host and microbial RNA |
| Cell Counting | Flow cytometry with staining [111] | Absolute microbial quantification | Enables quantitative profiling |
Computational Tools and Databases
Beyond laboratory reagents, multi-omics research requires specialized computational tools for data analysis and integration:
- KneadData: For quality control and removal of host reads from metagenomic data [111]
- DADA2: For amplicon sequence variant analysis in 16S rRNA data [112]
- Pathway Tools: For metabolic network visualization and multi-omics data painting [113]
- Spaco: For spatially aware colorization of cellular data [114]
- HMP Data Coordination Center: For accessing standardized multi-omics datasets [109] [41]
Future Directions and Clinical Translation
The application of multi-omics technologies to IBD and Prediabetes research holds tremendous promise for advancing personalized medicine approaches. Future research directions should focus on:
- Prospective Longitudinal Designs: Moving beyond cross-sectional studies to capture dynamic changes during disease progression and intervention [107]
- Advanced Integration Methods: Developing computational approaches that can establish causal relationships rather than mere associations
- Standardization of Protocols: Establishing consensus protocols for multi-omic data generation and analysis to enable cross-study comparisons
- Intervention Studies: Applying multi-omic profiling to clinical trials to identify biomarkers of treatment response and mechanisms of resistance
As these technologies mature and analytical methods improve, multi-omics signatures are poised to transform clinical practice by enabling earlier detection, personalized treatment selection, and more precise monitoring of therapeutic responses in both IBD and Prediabetes. The continued integration of multi-omic approaches within a framework of host-microbiome interactions will undoubtedly yield new insights into the complex pathophysiology of these conditions and open new avenues for therapeutic intervention.
The human microbiome represents a critical frontier in therapeutic development, with microbiome-targeted interventions offering promising pathways for managing a range of metabolic, gastrointestinal, and neuropsychiatric conditions. This technical review provides a comprehensive efficacy comparison of fecal microbiota transplantation (FMT), probiotics, and dietary interventions within the framework of host-microbiome interactions. Current evidence indicates that therapeutic outcomes are highly context-dependent, influenced by intervention design, duration, and specific pharmacomicrobiomic interactions. While FMT enables rapid microbial community restructuring, probiotics and dietary approaches offer more gradual modulation of gut ecosystem function and microbial metabolite production. The emerging paradigm emphasizes precision microbiome medicine, where intervention selection is optimized based on individual host physiology, baseline microbiota status, and disease-specific pathways.
The human microbiome functions as an essential biological interface, maintaining systemic homeostasis through complex molecular dialogues with host systems. These host-microbiome interactions occur through multiple mechanistic pathways: direct microbial contact with host pattern-recognition receptors, production of microbial metabolites including short-chain fatty acids (SCFAs) and bile acids, and modulation of immune signaling networks [93]. The intestinal mucosal immune system maintains a delicate balance between tolerance to commensal organisms and defense against pathogens, a equilibrium that becomes disrupted in various disease states [93].
Therapeutic targeting of the microbiome represents a paradigm shift from traditional pharmacological approaches, aiming to restore ecological balance rather than single pathway inhibition. Microbiome-based therapeutics function through distinct yet complementary mechanisms: FMT introduces complete microbial communities for rapid ecosystem restructuring; probiotics administer defined beneficial strains to augment specific functions; and dietary interventions provide substrates that selectively modulate indigenous microbial communities [115] [116]. Understanding the relative efficacy, appropriate applications, and limitations of each approach is essential for researchers developing targeted microbiome interventions.
Quantitative Efficacy Comparisons Across Conditions
Table 1: Comparative Efficacy of Microbiome-Targeted Interventions for Metabolic Conditions
| Condition | Intervention | Key Efficacy Metrics | Effect Size | Notes |
|---|---|---|---|---|
| Type 2 Diabetes | Multi-strain Probiotics | HbA1c reduction | -0.2% to -0.4% [117] | Synergistic with metformin; attenuated with sulfonylureas |
| HOMA-IR improvement | Significant reduction [117] | Optimal duration ≥12 weeks | ||
| FMT | Insulin sensitivity (clamp) | Consistent improvement [117] | Particularly effective in insulin-resistant phenotypes | |
| HbA1c reduction | Less consistent [117] | Donor-dependent effects | ||
| Obesity/Metabolic Syndrome | Bifidobacterium longum APC1472 | Metabolic parameters | Significant improvement [94] | Demonstrated in overweight/obese individuals |
| FMT + Low-fermentable fiber | Insulin sensitivity | Significant improvement [118] | Superior to FMT alone | |
| FMT | BMI, triglyceride reduction | Significant improvement [118] | Linked to specific microbial shifts |
Table 2: Comparative Efficacy of Microbiome-Targeted Interventions for Gastrointestinal and Neuropsychiatric Conditions
| Condition | Intervention | Key Efficacy Metrics | Effect Size | Notes |
|---|---|---|---|---|
| Recurrent C. difficile Infection | FMT | Sustained remission | ≈90% [116] [118] | Superior to vancomycin therapy |
| Ulcerative Colitis | FMT | Clinical remission | Significant improvement [116] [118] | Donor selection critical |
| FMT + Anti-inflammatory diet | Clinical remission over 1 year | Significant improvement [118] | Combinatorial approach | |
| Irritable Bowel Syndrome | FMT | Symptom improvement | 89.1% response rate [116] | Dose-dependent effects |
| Multi-strain Probiotics | Symptom improvement | Significant improvement [115] | Strain-specific effects | |
| Depressive Symptoms | FMT | Symptom reduction (SMD) | -1.21 [119] | Especially effective in IBS-comorbid depression |
| (95% CI: -1.87 to -0.55) | ||||
| Necrotizing Enterocolitis | Multi-strain Probiotics | Incidence reduction | RR: 0.51 [120] | Particularly effective in preterm infants |
| Mortality reduction | RR: 0.72 [120] |
Mechanistic Insights and Pathway Analysis
Immunomodulatory Pathways in Microbiome-Targeted Therapies
Microbiome-targeted therapies converge on shared immunomodulatory pathways but engage them through distinct mechanistic entry points. FMT produces the most rapid transformation of microbial community structure, introducing diverse SCFA-producing taxa that directly engage host G-protein coupled receptors (GPCRs) to promote regulatory T-cell (Treg) differentiation [93] [118]. Probiotics function through more targeted mechanisms, with specific strains like Bifidobacterium infantis 35624 demonstrating capacity to induce Treg polarization and reduce pro-inflammatory biomarkers including C-reactive protein [93]. Dietary interventions, particularly fiber-rich approaches, provide fundamental substrates that enable endogenous microbial metabolism and SCFA production, indirectly supporting epithelial barrier integrity and immune homeostasis [116].
Gut-Brain Axis Engagement Mechanisms
The gut-brain axis represents a critical pathway through which microbiome-targeted interventions influence neuropsychiatric conditions. FMT demonstrates particularly robust effects on depressive symptoms, with a standardized mean difference of -1.21 (95% CI: -1.87 to -0.55) in meta-analyses [119]. These effects appear mediated through microbial metabolites that function as neuroactive compounds, with structured gut-brain modules corresponding to specific neurochemical production or degradation processes [94]. The efficacy of FMT for depressive symptoms is most pronounced in individuals with comorbid irritable bowel syndrome, highlighting the intersection of gastrointestinal and psychological health [119]. Both probiotics and dietary interventions engage similar pathways but typically produce more modest effects, suggesting their potential lies in prevention and maintenance rather than acute intervention.
Experimental Protocols and Methodological Considerations
FMT Clinical Protocol for Metabolic Syndrome
Objective: To evaluate the efficacy of FMT for improving insulin sensitivity in patients with metabolic syndrome.
Donor Selection & Screening:
- Comprehensive medical history excluding infectious diseases, risky behaviors, and chronic illnesses [116]
- Laboratory testing including blood (viral hepatitis, liver enzymes, CRP, complete blood count) and stool analysis (C. difficile toxin B, Campylobacter, Salmonella, Shigella, norovirus, rotavirus, Helicobacter pylori antigen) [116]
- Regular re-screening every 3 months for active donors [116]
Stool Preparation & Administration:
- Stool processing within 2 hours of defecation (refrigerated if exceeding 30 minutes) [116]
- Delivery routes: oral capsules, colonoscopic administration, or nasojejunal intubation [119] [116]
- Endoscopic or enema routes demonstrate superior efficacy for depressive symptoms compared to oral capsules (SMD: -1.29 vs. -1.06) [119]
Recipient Preparation & Monitoring:
- Pre-procedure dietary optimization with high-fiber, anti-inflammatory diet for ≥2 weeks [116]
- Efficacy assessment via hyperinsulinemic-euglycemic clamp (insulin sensitivity), HbA1c, inflammatory markers at baseline, 2, 6, and 12 weeks post-FMT [117]
- Engraftment monitoring through 16S rRNA sequencing of serial stool samples [118]
Probiotic Trial Design for Glycemic Control
Study Population: Adults with type 2 diabetes or prediabetes, with stratification by concomitant medications (particularly metformin vs. sulfonylureas) [117].
Intervention Protocol:
- Multi-strain probiotic formulations containing Lactobacillus and Bifidobacterium species [117] [115]
- Minimum intervention duration of 12 weeks to detect significant metabolic effects [117]
- Dose frequency: typically once or twice daily with meals
Outcome Measures:
- Primary: HbA1c change from baseline [117]
- Secondary: Fasting glucose, HOMA-IR, circulating SCFAs (butyrate), inflammatory markers (CRP) [117]
- Mechanistic: Microbiota composition shifts (enrichment of SCFA-producing taxa), bile acid profiling [117]
Dietary Intervention Protocol to Support Microbiome Therapies
Pre-/Post-FMT Dietary Protocol:
- High-fiber diet: Emphasizing psyllium, inulin-type fructans, and diverse plant sources [116]
- Anti-inflammatory components: Polyphenol-rich foods, omega-3 fatty acids [116] [118]
- Duration: Initiate 2-4 weeks pre-FMT and maintain for ≥8 weeks post-procedure [116]
Assessment Methods:
- Dietary adherence: Food frequency questionnaires, 3-day food records
- Microbiota metrics: 16S rRNA sequencing, SCFA quantification (fecal and serum)
- Clinical outcomes: Disease-specific symptom scores, metabolic parameters
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Microbiome Therapeutic Studies
| Reagent Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Microbiota Assessment | 16S rRNA sequencing primers (V3-V4) | Taxonomic profiling | Limited functional information |
| Shotgun metagenomics | Functional potential assessment | Higher cost, computational demands | |
| GA-map Dysbiosis Test | Standardized dysbiosis index | Commercial assay with defined reference | |
| Metabolite Profiling | GC-MS for SCFAs | Quantification of acetate, propionate, butyrate | Requires derivatization for detection |
| LC-MS for bile acids | Comprehensive bile acid profiling | Complex method development | |
| TMAO assays | Cardiovascular risk marker | ELISA kits available | |
| Host Response | Cytokine panels (IL-6, IL-10, TNF-α) | Inflammatory response monitoring | Multiplex platforms preferred |
| Intestinal fatty acid binding protein (I-FABP) | Gut barrier integrity assessment | Commercial ELISA available | |
| GLP-1, PYY | Enteroendocrine function | Specialized handling required | |
| Culture Media | YCFA medium | In vitro cultivation of anaerobes | Supports diverse gut species |
| Gifu Anaerobic Medium | Fastidious anaerobic growth | Standardized composition | |
| Animal Models | Germ-free mice | Microbial causality studies | Require specialized facilities |
| Gnotobiotic models | Defined consortium studies | Customizable complexity |
The comparative evaluation of FMT, probiotics, and dietary interventions reveals distinct yet complementary therapeutic profiles. FMT demonstrates superior efficacy for conditions requiring rapid microbial community restructuring, such as recurrent C. difficile infection and comorbid depression in IBS. Probiotics offer reproducible, defined interventions with particular value in glycemic control and NEC prevention, especially when utilizing multi-strain formulations. Dietary interventions provide the foundation for microbial health, significantly influencing the efficacy of other microbiome-targeted therapies.
Future research directions should prioritize precision microbiome medicine through improved patient stratification biomarkers, optimized donor-recipient matching algorithms, and standardized dietary support protocols. The emerging paradigm of combinatorial approaches - such as FMT followed by targeted probiotics and dietary support - represents a promising frontier for enhancing therapeutic durability. Furthermore, mechanistic studies dissecting microbial engraftment principles and pharmacomicrobiomic interactions will be essential for advancing from correlation to causation in microbiome therapeutics. As the field matures, integration of multi-omics datasets with machine learning approaches will enable predictive models of treatment response, ultimately fulfilling the promise of personalized microbiome medicine.
Validation of Predictive Biomarkers for Preterm Birth, Insulin Resistance, and Disease Flares
Within the framework of host-microbiome research, the validation of predictive biomarkers is paramount for transitioning from association to causation and clinical application. This technical guide provides a comprehensive overview of the current landscape for biomarker validation in three key areas: preterm birth, insulin resistance, and inflammatory disease flares. The complex interplay between host physiology and microbial communities creates dynamic biomarker profiles that, when accurately decoded, can offer unprecedented opportunities for early intervention and personalized medicine. This document details the quantitative evidence, experimental methodologies, and analytical frameworks required for robust biomarker validation, with a specific focus on the functional interfaces between host and microbiome. We present integrated multi-omics approaches that capture the complexity of these interactions, from microbial metabolite production to host immune and metabolic responses, providing researchers with validated benchmarks and standardized protocols for advancing diagnostic and therapeutic development.
Validated Biomarkers and Quantitative Evidence
The following tables synthesize key validated biomarkers across the three domains, presenting quantitative performance metrics essential for research and development.
Table 1: Validated Biomarkers for Preterm Birth Prediction
| Biomarker Category | Specific Biomarker | Prediction Performance (AUC) | Sample Timing (Gestational Weeks) | Study Details |
|---|---|---|---|---|
| Vaginal Microbiome | Gardnerella vaginalis dominance over L. crispatus and L. iners | 0.77 [121] | 20+0–22+6 | Asymptomatic women with prior PTB history or short cervix [121] |
| Vaginal Metabolite & Immune Panel | 5 metabolites + TNFR1 | 0.88 [121] | 26+0–28+6 | Combined model showing high predictive value [121] |
| Vaginal Immune | CXCL10 increase | 0.68 [121] | 20+0–28+6 | Increase in preterm vs. ~3-fold decline in term deliveries [121] |
| Vaginal Immune + fFN | CXCL10 + Fetal Fibronectin (FFN >50ng/mL) | 0.74 [121] | ≥22 | Combined protein marker model [121] |
| Systemic Inflammatory | Neutrophil-to-Lymphocyte Ratio (NLR) | 0.64-0.66 (for preterm birth) [122] | 8-14 | Pregnancies with pregestational diabetes; modest discriminative ability [122] |
| Clinical & Metabolic | HbA1c + Parity | OR: 1.71 (HbA1c), 1.62 (Parity) [122] | First Trimester | Independent predictors in pregestational diabetes [122] |
| Machine Learning (GDM+HDP) | ALT, AST, Albumin, LDH, SBP (32-36w) | 0.777 (External Validation) [123] | 32-36 | Naive Bayes model for high-risk comorbid population [123] |
Table 2: Validated Biomarkers for Insulin Resistance and Gut Microbiome Interactions
| Biomarker Category | Specific Biomarker | Association / Effect | Study Model | Proposed Mechanism |
|---|---|---|---|---|
| Gut Microbial Taxa | Lachnospiraceae (Dorea, Blautia) | Positive correlation with IR [124] | Human Multi-omics | Increased fecal monosaccharides (fructose, galactose, mannose, xylose) [124] |
| Gut Microbial Taxa | Bacteroidales (Bacteroides, Alistipes) | Negative correlation with IR [124] | Human Multi-omics & Mouse Model | Alistipes indistinctus reduced blood glucose and fecal monosaccharides in HFD mice [124] |
| Microbial Metabolites | Faecal Monosaccharides | Increased in IR and MetS [124] | Human Metabolomics | Promotes lipid accumulation and pro-inflammatory cytokine response [124] |
| Microbial Metabolites | Short-Chain Fatty Acids (Acetate, Propionate, Butyrate) | Improved insulin sensitivity [125] | In vitro & In vivo | Increased lipid oxidation, suppressed gluconeogenesis, promoted adipogenesis/thermogenesis [125] |
| Microbial Metabolites | Trimethylamine N-oxide (TMAO) | Increased gluconeogenesis, promoted inflammation [125] | Ex vivo & In vivo | Choline-derived metabolite affecting liver and adipose tissue [125] |
Table 3: Host-Microbiome Metabolic Biomarkers in Inflammatory Bowel Disease Flares
| Biomarker Domain | Specific Biomarker / Pathway | Association with Inflammation | Data Source | Functional Consequence |
|---|---|---|---|---|
| Microbiome Metabolic Exchanges | Lactate cross-feeding | Increased [126] | Metabolic Modeling (16S) | -- |
| Microbiome Metabolic Exchanges | Amylotriose, Glucose, Propionate, Succinate cross-feeding | Decreased [126] | Metabolic Modeling (16S) | Reduced SCFA production and precursor availability [126] |
| Microbiome-Host Exchanges | Butyrate production | Decreased [126] | Metabolic Modeling (16S) | Loss of anti-inflammatory SCFA [126] |
| Microbiome-Host Exchanges | Cholate, Glycocholate production | Decreased [126] | Metabolic Modeling (16S) | Altered bile acid metabolism [126] |
| Host Tissue Metabolism (Biopsy/Blood) | Tryptophan catabolism, NAD biosynthesis | Increased catabolism, depleted tryptophan, impaired NAD synthesis [126] | Host Metabolic Models (RNA) | Disrupted nitrogen homeostasis, polyamine/glutathione metabolism [126] |
| Host Tissue Metabolism (Biopsy/Blood) | One-carbon cycle, Phospholipid metabolism | Suppressed one-carbon cycle, altered phospholipid profiles [126] | Host Metabolic Models (RNA) | Limited choline availability [126] |
Experimental Protocols for Biomarker Validation
Protocol 1: Vaginal Host-Microbiome-Metabolite Profiling for Preterm Birth
This protocol outlines the longitudinal collection and multi-omics analysis of cervicovaginal (CV) fluid to identify interactions associated with spontaneous preterm birth (sPTB) [121].
Sample Collection and Storage
- Participants: Recruit asymptomatic pregnant women at high risk for PTB (e.g., prior PTB history or short cervical length ≤25mm). Exclude women with symptoms of preterm labour, PPROM, evidence of genital tract infection (e.g., BV), or recent antibiotic use [121].
- Time Points: Collect CV fluid at two gestational time points (GTP): GTP1 (20+0–22+6 weeks) and GTP2 (26+0–28+6 weeks). Collect samples before any vaginal examination or clinical intervention [121].
- Procedure: Use a sterile swab to collect CV fluid. Immediately after collection, store swabs at -20°C, transferring to -80°C within 1-3 days for long-term storage [121].
- Concurrent Test: Following CV fluid collection, measure fetal fibronectin (FFN) levels from the CV space. A level >50 ng/mL at or after 22 weeks is considered high risk for sPTB [121].
DNA Extraction and 16S rRNA Sequencing
- Elution: Thaw swabs and elute CV fluid by adding 500 µL PBS and vortexing for 5 minutes. Centrifuge the swab to draw out any remaining fluid [121].
- Lysis: Incubate the 500 µL CV fluid with 75 µL of 20 mg/mL lysozyme at 37°C for 1 hour to degrade bacterial cell walls [121].
- Extraction: Purify DNA using a commercial kit (e.g., QIAmp DNA mini kit, Qiagen) according to the manufacturer's instructions. Elute DNA in 50 μL of buffer AE [121].
- PCR and Sequencing: Perform 16S rRNA PCR amplification using barcoded primers (e.g., 319F and MCRevA). Use a sequencing platform such as Nanopore MinION for analysis [121].
Metabolomic and Cytokine Profiling
- Metabolomics: Analyze CV fluid using analytical techniques like liquid chromatography-mass spectrometry (LC-MS) to identify and quantify metabolites (e.g., pantothenate, urate) [121].
- Cytokine Analysis: Quantify concentrations of cytokines and chemokines (e.g., CXCL9, CXCL10, CXCL11, TNF-α, eotaxin, TNFR1) in CV fluid using multiplex immunoassays (e.g., Luminex) or ELISA [121].
Data Integration and Model Validation
- Statistical Analysis: Compare microbiota composition (α- and β-diversity), metabolite levels, and cytokine concentrations between term and preterm groups at each GTP. Use multivariate analyses (e.g., PLS-DA) and calculate AUC values for key biomarkers [121].
- Validation: Validate the predictive performance of identified biomarker panels (e.g., microbiota, metabolites, cytokines) using ROC analysis in the study cohort and, if possible, an independent validation cohort [121].
Protocol 2: Multi-omics Validation of Gut Microbiome Biomarkers for Insulin Resistance
This protocol describes an integrative multi-omics approach to link gut microbial metabolism to host insulin resistance (IR), combining human cohort analysis with mechanistic validation in mice [124].
Human Cohort Profiling
- Cohort Design: Recruit a well-phenotyped human cohort (e.g., n=306 without diabetes). Collect fresh fecal samples for metagenomics and metabolomics, and blood samples for host metabolomics and transcriptomics [124].
- Metagenomic Sequencing: Perform shotgun metagenomic sequencing of fecal DNA to profile the taxonomic and functional potential of the gut microbiome [124].
- Metabolomic Profiling:
- Host Transcriptomics: Isolve RNA from peripheral blood mononuclear cells (PBMCs) or other accessible tissues for transcriptomic analysis to assess host inflammatory and metabolic pathways [124].
- Correlation Analysis: Integrate datasets using correlation networks and multivariate statistics to identify associations between specific microbial taxa (e.g., Lachnospiraceae, Bacteroidales), faecal metabolites (e.g., monosaccharides), and host IR status/transcriptome signatures [124].
Mechanistic Validation in Mouse Models
- Animal Model: Use a mouse model of diet-induced IR (e.g., high-fat diet fed). Monitor body weight, blood glucose, and insulin tolerance [124].
- Bacterial Intervention: Isolate or procure the identified IR-alleviating bacterial strain (e.g., Alistipes indistinctus). Administer the live bacteria orally to HFD-fed mice. Include a control group receiving a placebo vehicle [124].
- Outcome Measures:
- Metabolic Phenotyping: Measure changes in blood glucose, insulin sensitivity (e.g., by GTT, ITT), and faecal monosaccharide levels post-intervention [124].
- Tissue Analysis: Analyze liver, skeletal muscle, and adipose tissue for lipid accumulation (e.g., by histology) and assess key insulin signaling pathways (e.g., IRS/PI3K/AKT) by immunoblotting or RT-qPCR [124].
- Inflammation Assessment: Measure levels of pro-inflammatory cytokines in serum and tissues [124].
Protocol 3: Host-Microbiome Metabolic Modeling in Inflammatory Bowel Disease
This protocol employs metabolic modeling of longitudinal IBD cohorts to decipher deregulated host-microbiome metabolic networks during disease flares [126].
Cohort Design and Sample Collection
- Cohort: Establish a longitudinal cohort of IBD patients (Crohn's disease and Ulcerative Colitis). Collect matched samples before and after initiation of advanced drug therapy [126].
- Sample Types: Collect multiple sample types: colonic biopsies (for host transcriptomics), blood (for host transcriptomics and serum metabolomics), and stool (for 16S rRNA sequencing or metagenomics) [126].
Data Generation and Preprocessing
- Microbiome Profiling: Perform 16S rRNA gene sequencing or shotgun metagenomics on stool samples. Map sequencing data to curated genomic databases (e.g., the HRGM collection) [126].
- Host Transcriptomics: Conduct RNA sequencing on RNA isolated from colonic biopsies and blood samples [126].
- Serum Metabolomics: Perform untargeted or targeted metabolomic profiling on serum samples [126].
Metabolic Model Reconstruction and Analysis
- Microbiome Metabolic Modeling (MMM):
- Reconstruction: Reconstruct genome-scale metabolic models for the bacterial species identified in the microbiome profiles [126].
- Analysis: Use both coupling-based (e.g., MicrobiomeGS2) and agent-based (e.g., BacArena) modeling approaches to predict community-level metabolic fluxes. This allows assessment of both cooperative and competitive microbial interactions [126].
- Outputs: Quantify fluxes of individual bacterial reactions, cross-feeding of metabolites between bacteria, and exchange of metabolites between the microbiome and the host [126].
- Host Metabolic Modeling:
- Reconstruction: Reconstruct a generic genome-scale metabolic model of human cells (e.g., Recon3D) [126].
- Contextualization: Create context-specific metabolic models (CSMMs) for host colon tissue and blood cells by integrating RNA-seq data from biopsies and blood using algorithms like FASTCORE or INIT [126].
- Analysis: Use methods like Flux Variability Analysis (FVA) to estimate the metabolic potential (reaction activity scores) of the host tissues in different states [126].
Data Integration and In Silico Intervention
- Association with Disease Activity: Build linear mixed models to associate predicted microbial reaction fluxes, metabolite exchanges, and host tissue reaction activities with clinical disease activity scores (e.g., HBI/Mayo score), using patient ID as a random effect to account for longitudinal sampling [126].
- Pathway Analysis: Identify significantly altered metabolic pathways on both the microbiome and host sides (e.g., NAD, amino acid, one-carbon, phospholipid metabolism) [126].
- Model Validation: Validate model predictions (e.g., reduced microbial butyrate production, altered host tryptophan catabolism) against measured serum metabolomics data [126].
- Therapeutic Prediction: Leverage the microbiome metabolic models to predict nutritional interventions (e.g., specific dietary compounds) that could remodel the microbial community to restore metabolic homeostasis [126].
Signaling Pathways and Host-Microbiome Interactions
The following diagrams, generated using Graphviz DOT language, illustrate the key signaling pathways and metabolic networks involved in host-microbiome interactions related to preterm birth, insulin resistance, and inflammatory bowel disease.
Vaginal Microbiome-Induced Inflammatory Pathway in Preterm Birth
This diagram illustrates the mechanism by which vaginal dysbiosis triggers a host inflammatory response that can lead to spontaneous preterm birth.
Gut Microbiome Modulation of Host Insulin Sensitivity
This diagram depicts the mechanism by which gut microbiota and their metabolites influence host insulin sensitivity in peripheral tissues.
Host-Microbiome Metabolic Crosstalk in Inflammatory Bowel Disease
This diagram illustrates the disrupted metabolic networks between the host and microbiome during an IBD flare, highlighting key intersecting pathways.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents and Platforms for Host-Microbiome Biomarker Studies
| Reagent / Platform | Function / Application | Example Use Case | Key Considerations |
|---|---|---|---|
| QIAamp DNA Mini Kit (Qiagen) | Microbial DNA extraction from complex samples (stool, vaginal swabs) | DNA preparation for 16S rRNA sequencing of vaginal fluid [121] | Includes lysozyme incubation step for effective Gram-positive bacterial lysis [121] |
| Nanopore MinION Sequencer | Long-read, real-time DNA/RNA sequencing | 16S rRNA PCR product sequencing for vaginal microbiota profiling [121] | Enables rapid, in-field sequencing; suitable for 16S rRNA amplicon and metagenomic sequencing |
| Luminex Multiplex Immunoassays | Simultaneous quantification of multiple cytokines/chemokines in biofluids | Measuring CV fluid levels of CXCL9, CXCL10, CXCL11, TNF-α [121] | Allows for comprehensive immune profiling from small volume samples |
| GC-MS / LC-MS Systems | Untargeted and targeted metabolomic analysis | Quantifying faecal monosaccharides or CV fluid metabolites [124] [121] | GC-MS for volatile compounds; LC-MS for broader polar/non-polar metabolites |
| Genome-Scale Metabolic Models (GEMs) | Computational modeling of metabolic networks | Predicting microbiome metabolic fluxes and host-microbiome exchanges in IBD [126] | Require curated databases (e.g., HRGM, AGORA, Recon3D) and constraint-based modeling tools |
| BacArena / MicrobiomeGS2 | Agent-based and coupling-based microbial community modeling | Simulating competitive and cooperative microbial interactions in gut communities [126] | BacArena for spatial dynamics; MicrobiomeGS2 for metabolic coupling analysis |
| FASTCORE / INIT Algorithms | Reconstruction of context-specific metabolic models from omics data | Building host colon tissue metabolic models from biopsy RNA-seq data [126] | Integrates transcriptomic data to create tissue- or condition-specific metabolic networks |
The human microbiome, once regarded as a passive passenger, is now recognized as a dynamic and essential determinant of human physiology, shaping immunity, metabolism, neurodevelopment, and therapeutic responsiveness across the lifespan [91]. The clinical translation of microbiome research represents a paradigm shift in medicine, moving from descriptive associations to intervention-ready, mechanistically grounded models [1]. This transition, however, introduces complex challenges at the ethical, regulatory, and economic interfaces that must be systematically benchmarked for successful translation.
Host-microbiome interactions form the fundamental biological context for this translation. These intricate relationships involve continuous crosstalk between microbial communities and human physiological systems via microbial metabolites, immune signaling, and neural pathways [91] [1]. The gastrointestinal tract harbors one of the most complex and functionally diverse microbial ecosystems, with gut microbiota functioning as both a guardian of host homeostasis and a driver of diverse pathologies [91]. Understanding these interactions is crucial for developing effective microbiome-based therapies (MbTs) and benchmarking their success across the translational pathway.
Quantitative Landscape of Microbiome Translation
Market Dynamics and Therapeutic Pipeline
The microbiome therapeutic market demonstrates explosive growth potential, reflecting increasing investment and clinical validation. The table below summarizes key market metrics and their translational implications.
Table 1: Market Landscape for Human Microbiome-Based Products
| Market Segment | 2024 Market Value (USD) | Projected 2030 Market Value (USD) | Compound Annual Growth Rate (CAGR) | Key Translational Implications |
|---|---|---|---|---|
| Total Microbiome Market | 990 million | 5.1 billion | 31% | Rapid market expansion driving investment diversity |
| Live Biotherapeutic Products (LBPs) | 425 million | 2.39 billion | ~31% | Shift from FMT to defined consortia |
| Fecal Microbiota Transplantation (FMT) | 175 million | 815 million | ~29% | Gold standard for rCDI, being overtaken by LBPs |
| Diagnostics & Biomarkers | 140 million | 764 million | ~33% | Critical for patient stratification and therapy monitoring |
| Nutrition-Based Interventions | 99 million | 510 million | ~31% | Bridges wellness and medical applications |
The clinical pipeline for microbiome therapeutics has diversified dramatically beyond gastrointestinal applications. As of September 2025, approximately 243 candidates are in development across more than 100 companies, spanning every phase of clinical testing [127]. The distribution across development stages reveals a sector still in early translation: preclinical programs (60%), Phase I trials (20%), Phase II trials (15%), and Phase III trials (<5%) [127]. This distribution indicates significant opportunity for attrition as programs progress through later-stage clinical development.
Table 2: Selected Microbiome Therapeutics in Clinical Development (2025)
| Company / Product | Indication(s) | Modality & Mechanism | Development Stage |
|---|---|---|---|
| Seres Therapeutics – Vowst (SER-109) | rCDI; exploring ulcerative colitis | Oral live biotherapeutic; purified Firmicutes spores | Approved |
| Ferring Pharma/Rebiotix – Rebyota (RBX2660) | rCDI | Rectally administered fecal microbiota transplant | Approved |
| Vedanta Biosciences – VE303 | rCDI | Defined eight-strain bacterial consortium | Phase III |
| 4D Pharma – MRx0518 | Oncology (solid tumors) | Single-strain Bifidobacterium longum engineered to activate immunity | Phase I/II |
| MaaT Pharma – MaaT013 | Graft-versus-host disease | Pooled FMT product to restore immune homeostasis | Phase III |
| Synlogic – SYNB1934 | Phenylketonuria (PKU) | Engineered E. coli Nissle expressing phenylalanine ammonia lyase | Phase II |
| Eligo Bioscience – Eligobiotics | Carbapenem-resistant infections | CRISPR-guided bacteriophages delivering DNA payloads | Phase I |
Regulatory Frameworks and Standardization Challenges
Evolving Regulatory Landscape for Microbiome-Based Therapies
The regulatory landscape for MbTs is rapidly evolving in response to scientific advances and the first marketing approvals. The European Union has implemented significant changes through the Regulation on Substances of Human Origin (SoHO), providing a structured framework for microbiome-based therapy development [128]. In the United States, the FDA has established complementary pathways, with both regions recognizing the need for specialized regulatory science to evaluate these complex products.
The spectrum of MbTs represents a continuum from minimally manipulated microbiota transplantation (MT) to highly characterized live biotherapeutic products (LBPs) [128]. This spectrum can be visualized through the following regulatory classification pathway:
A critical regulatory challenge remains the definition and standardization of key concepts. There is currently no consensus on a scientific or legal definition of microbiota transplantation (MT) at the European Union level [128]. Similarly, terminology for more complex products varies, with ongoing efforts to harmonize definitions for "faecal microbiota-based medicinal products" or more precisely "human intestinal microbiome whole-ecosystem-based medicinal products" [128].
Regulatory Science and Standardization Gaps
The emergence of 'regulatory science' addresses fundamental challenges in evaluating MbTs. According to the EMA definition, regulatory science refers to "the range of scientific disciplines that are applied to the quality, safety and efficacy assessment of medicinal products and that inform regulatory decision-making throughout the lifecycle of a medicine" [128]. This field is developing new tools, standards, and methodologies specifically for evaluating innovative regulated products like MbTs.
Key standardization challenges include:
- Characterization Complexity: For whole-ecosystem products, current analytical methods cannot fully characterize these complex microbiome samples, creating evaluation challenges [128].
- Batch-to-Batch Consistency: For rationally designed ecosystem products, consistency remains challenging due to the complexity of co-fermenting multiple strains and differential impacts of downstream processing [128].
- Potency Assays: Appropriate potency tests and critical quality attributes related to safety and efficacy are crucial for marketing authorization but difficult to define for complex consortia [128].
Methodological Framework for Host-Microbiome Research
Experimental Models for Host-Microbiome Interaction Studies
Understanding host-microbiome interactions requires sophisticated experimental models that recapitulate human physiology while enabling mechanistic insights. The following experimental workflow illustrates the integration of various models in microbiome research:
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagent Solutions for Host-Microbiome Studies
| Research Tool Category | Specific Examples | Function and Application | Key Considerations |
|---|---|---|---|
| Animal Models | Germ-free mice; Defined microbiota mice; Zebrafish (Danio rerio); Drosophila melanogaster | Controlled study of host-microbiota interactions in whole organisms | Genetic tractability; Microbial community control; Physiological relevance |
| In Vitro Systems | Organ-on-chip (OOC); Gut-on-chip (GOC); Organoids | Human-relevant modeling with microbial co-culture capability | Oxygen gradient control; Flow dynamics; Microbial diversity maintenance |
| Multi-Omics Technologies | Metagenomics; Metaproteomics; Metabolomics; 16S rRNA sequencing | Comprehensive characterization of microbiome composition and function | Resolution (strain-level); Functional annotation; Integration capabilities |
| Computational & AI Tools | Machine learning classifiers; Bioinformatic pipelines; AI-driven analytics | Patient stratification; Pattern recognition; Predictive modeling | Data standardization; Algorithm transparency; Clinical validation |
| Microbial Culturing Tools | Culturomics; Anaerobic chambers; Specialized media | Isolation and expansion of fastidious microbes; Bank creation | Viability maintenance; Contamination prevention; Scale-up challenges |
Advanced Protocol: Gut-on-Chip Technology for Host-Microbe Studies
Gut-on-chip (GOC) technologies have emerged as promising alternatives to animal models, overcoming limitations of traditional systems while maintaining tissue-level complexity [129]. The following detailed protocol outlines the application of GOC for studying host-microbiota-probiotic interactions:
System Setup and Configuration:
- Utilize a polydimethylsiloxane (PDMS) chip with two culture chambers separated by a porous flexible membrane [129]
- Culture intestinal epithelial cells in the upper chamber under continuous nutrient flow (10-100 μL/hour)
- Mimic underlying endothelium or stromal compartment in the lower chamber
- Apply physiological vacuum (0.15 Hz frequency, 10% strain) to lateral chambers to recapitulate peristaltic motions [129]
- Maintain physiological oxygen gradients (anaerobic lumen to aerobic tissue) using specialized membrane systems
Microbial Introduction and Monitoring:
- Introduce bacterial species (mono-associations or defined consortia) directly into the intestinal lumen
- For complex microbiota co-cultures: Integrate hypoxia and mucus layer to sustain obligate anaerobes [129]
- Monitor microbial dynamics via 16S rRNA sequencing (200+ Operational Taxonomic Units achievable) [129]
- Employ high-resolution imaging for spatio-temporal visualization of microbial-epithelial interactions
- Validate system integrity through transepithelial electrical resistance (TEER) measurements
Functional Readouts:
- Quantify barrier function via fluorescent dextran permeability assays
- Measure immune activation through cytokine profiling (IL-8, IL-6, TNF-α)
- Analyze microbial metabolites via LC-MS (short-chain fatty acids, bile acids)
- Assess host transcriptomic responses via RNA sequencing
This protocol enables sustained co-culture of human fecal microbiota for up to 3 days without major alterations in intestinal barrier integrity, providing a powerful platform for mechanistic studies of host-microbe interactions [129].
Ethical and Safety Considerations in Microbiome Translation
Donor Screening and Biobanking Ethics
The development of MbTs raises unique ethical challenges, particularly for donor-derived products. Donor screening represents a critical safety gate, as preparations used during MT procedures may be associated with higher risk of pathogen transmission and potential long-term negative health outcomes for recipients [128]. Recent studies have revealed that prior antibiotic exposure in healthy donors can durably alter microbial composition, phage dynamics, and resistance gene profiles, raising critical safety considerations that extend beyond standard pathogen screening [130].
The ethical framework for microbiome biobanking must address:
- Informed Consent: Specificity regarding future uses of microbiome samples and data
- Donor Privacy: Protection against re-identification from microbiome sequences
- Benefit Sharing: Equitable distribution of commercial benefits derived from donor samples
- Long-Term Safety Monitoring: Post-treatment surveillance for unexpected consequences
Microbiome Engraftment and Ecological Safety
A fundamental safety challenge in MbTs lies in predicting and controlling engraftment outcomes. The "gray zones" in FMT investigation include [130]:
- Community Coalescence: Studying microbiome shifts following FMT engraftment
- Indicator Features: Assessing specific microbiome features as signals of engraftment
- Resilience: Evaluating post-FMT recipients' microbiomes' resistance to shifts
These factors complicate safety assessment, as engraftment success varies significantly between individuals based on their baseline microbiota, immune status, and ecological factors. The field urgently needs validated biomarkers of engraftment success and safety to guide clinical application [130].
Economic Challenges and Commercialization Pathways
Manufacturing and Scale-Up Hurdles
The transition from research to commercially viable MbTs presents distinctive manufacturing challenges that impact economic sustainability:
Donor-Dependent Products:
- Variability Management: Donor stool samples exhibit substantial inter-individual variation, challenging batch consistency
- Screening Costs: Comprehensive donor screening for pathogens, antibiotic resistance genes, and metabolic profiles adds significant expense
- Supply Limitations: Dependence on qualified donors constrains production scalability
Defined Consortia Products:
- Co-Fermentation Complexity: Growing multiple strains together introduces ecological interactions difficult to control at scale
- Process Validation: Demonstrating consistent product characteristics despite microbial community complexity
- Stability Assurance: Maintaining viability and function through freezing, storage, and transportation
Innovative delivery methods are being developed to address some challenges, including encapsulation protocols for stable, capsule-based administration [130]. However, these advances must balance sophistication with cost-effectiveness for commercial viability.
Reimbursement and Market Access Strategies
The unique characteristics of MbTs create distinctive market access challenges:
Evidence Generation:
- Health Economic Data: Demonstrating cost-effectiveness compared to standard care, particularly for premium-priced therapies
- Long-Term Value: Capturing potential benefits beyond immediate clinical outcomes, such as reduced antibiotic usage or hospitalization rates
- Real-World Evidence: Complementing clinical trial data with post-market surveillance given the novel mechanisms of action
Market Positioning:
- Therapeutic vs. Preventive Positioning: Distinct reimbursement pathways for disease treatment versus prevention applications
- Diagnostic Companion Strategies: Developing microbiome-based diagnostics to identify patient populations most likely to respond
- Staged Market Entry: Initial focus on high-unmet-need indications (like rCDI) before expansion to broader applications
Benchmarking success in the clinical translation of microbiome research requires an integrated approach addressing the interconnected ethical, regulatory, and economic challenges detailed throughout this analysis. The field stands at a pivotal moment, with scientific advances increasingly enabling rational design of MbTs while regulatory frameworks mature to evaluate these complex products.
Successful translation will depend on several critical factors: First, continued development of regulatory science specifically tailored to microbiome-based products, with standardized endpoints and evaluation criteria. Second, advancement of experimental models that better recapitulate human host-microbiome interactions, particularly for predicting engraftment and ecological outcomes. Third, innovative business models that ensure commercial viability while maintaining appropriate safety and efficacy standards.
The growing convergence of biotechnology, computation, and clinical medicine is turning microbiome research into actionable healthcare tools [131]. As the field advances, benchmarking success must evolve beyond traditional pharmaceutical metrics to include ecological parameters, long-term microbiome stability, and host-microbiome integration measures. Through systematic attention to these multifaceted challenges, microbiome-based therapies can realize their potential to transform concepts of disease etiology, therapeutic design, and the future of individualized medicine [91].
Conclusion
The study of host-microbiome interactions has evolved from descriptive correlations to a mechanistic understanding of molecular causality, driven by multi-omics and advanced physiological models. Key takeaways confirm that microbial metabolites and community structures are pivotal in directing immune responses and maintaining systemic health, while their disruption is a actionable therapeutic target. Future research must prioritize standardizing translational models, validating causal mechanisms in human populations, and developing personalized microbiome-based interventions. The integration of artificial intelligence with multi-omic data holds promise for predicting disease risk and tailoring therapies, ultimately cementing the microbiome's role in the future of precision medicine and drug development.
References
- 1. Frontiers | The human microbiome in clinical translation: from bench to bedside [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1632435/full]
- 2. Prioritizing precision: guidelines for the better use of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12542624/]
- 3. Key features and guidelines for the application of microbial ... [https://www.nature.com/articles/s41598-024-77864-y]
- 4. Precision Microbiome: A New Era of Targeted Therapy with Core Probiotics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11938712/]
- 5. Interaction between microbiota and immunity in health and ... [https://www.nature.com/articles/s41422-020-0332-7]
- 6. Immune-microbiota interactions in health and disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4943041/]
- 7. Short-chain fatty acids: key antiviral mediators of gut microbiota [https://pmc.ncbi.nlm.nih.gov/articles/PMC12331605/]
- 8. Tryptophan Metabolism: A Link Between the Gut Microbiota ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7231603/]
- 9. Microbial tryptophan catabolites in health and disease [https://www.nature.com/articles/s41467-018-05470-4]
- 10. The Role of Short-Chain Fatty Acids From Gut Microbiota in ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2020.00025/full]
- 11. Short-chain fatty acids—a key link between the gut ... [https://www.nature.com/articles/s41390-025-04075-0]
- 12. the role of microbial short chain fatty acid metabolites in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5243208/]
- 13. Tryptophan Dietary Impacts Gut Barrier and Metabolic ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2019.02113/full]
- 14. Decoding immune interactions of gut microbiota for ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2023.1238822/full]
- 15. Inflammatory Adaptation in Barrier Tissues - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8336675/]
- 16. Editorial: Immune responses at barrier tissues [https://pmc.ncbi.nlm.nih.gov/articles/PMC12171184/]
- 17. The role of the microbiome on immune homeostasis ... [https://pubmed.ncbi.nlm.nih.gov/40821767/]
- 18. decoding the gut–immune–brain axis in health and disease [https://www.nature.com/articles/s41423-025-01333-3]
- 19. Role of the microbiome in regulation of the immune system [https://www.sciencedirect.com/science/article/pii/S1323893024001631]
- 20. Innate immune sensing by epithelial barriers [https://www.sciencedirect.com/science/article/abs/pii/S0952791521001072]
- 21. Possible role of gut microbes and host's immune response ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9581402/]
- 22. Host-microbiome interactions in atopic and allergic diseases [https://www.sciencedirect.com/science/article/pii/S2468202023000359]
- 23. Lung microbiome: new insights into the pathogenesis of ... [https://www.nature.com/articles/s41392-023-01722-y]
- 24. The Role of Skin-Gut-Lung Microbiome in Allergic Diseases [https://www.sciencedirect.com/science/article/pii/S2213219825004106]
- 25. Microbiota in health and diseases [https://www.nature.com/articles/s41392-022-00974-4]
- 26. The Central Role of the Gut Microbiota in Chronic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4189530/]
- 27. Dysbiosis in Inflammatory Bowel Disease: Pathogenic Role ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8998182/]
- 28. The relationship between gut microbiome and human ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1516010/full]
- 29. Dysbiosis in inflammatory bowel diseases: egg, not chicken [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2024.1395861/full]
- 30. and lifestyle factors accelerate Metabolic onset and alter gut... disease [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-024-03709-0]
- 31. Gut Microbial Dysbiosis - One Health Institute [https://onehealth.colostate.edu/2022/02/03/gut-microbial-dysbiosis/]
- 32. modeling reveals a multi-level... | Nature Communications Metabolic [https://www.nature.com/articles/s41467-025-60233-2?error=cookies_not_supported&code=7d6071d3-7cac-444f-93ea-d2a63330ffee]
- 33. Frontiers | Metabolomics: The Key to Unraveling the Role of the... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2022.917197/full]
- 34. Novel plant-derived compounds modulate gut microbiome ... [https://www.sciencedirect.com/science/article/pii/S0944501325003027]
- 35. The Oral–Gut–Systemic Axis: Emerging Insights into ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609195/]
- 36. Microbiota–gut–brain axis in neurodegenerative diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436269/]
- 37. Microbiome interactions shape host fitness - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6304949/]
- 38. Gut–Lung Axis: Microbial Crosstalk in Pediatric Respiratory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8637285/]
- 39. Interrelationship between oral and systemic diseases [https://www.sciencedirect.com/science/article/pii/S1933021923000892]
- 40. Mucosal host-microbe interactions associate with clinical ... [https://www.nature.com/articles/s41467-024-45855-2]
- 41. The Integrative Human Microbiome Project [https://www.nature.com/articles/s41586-019-1238-8]
- 42. The Integrative Human Microbiome Project: Dynamic Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5109542/]
- 43. Human Microbiome Project, part 2 [https://www.nature.com/collections/fiabfcjbfj]
- 44. Integrating multi-omics data to reveal the host-microbiota ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11901428/]
- 45. Longitudinal profiling of the microbiome at four body sites ... [https://www.sciencedirect.com/science/article/pii/S1931312824000568]
- 46. Multi-omic approaches for host-microbiome data integration [https://pmc.ncbi.nlm.nih.gov/articles/PMC10766395/]
- 47. Germ-Free Mice: Powerful Tools for Microbiome Research [https://www.taconic.com/resources/what-are-germ-free-mice]
- 48. Mechanistic insights into human host and microbiome ... [https://www.nature.com/collections/ihcfhcieic]
- 49. Human microbiota-associated animal models: a review [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1644187/full]
- 50. Human microbiota-associated animal models: a review [https://pubmed.ncbi.nlm.nih.gov/40937436/]
- 51. Laboratory mice engrafted with natural gut microbiota ... [https://www.nature.com/articles/s41467-025-60554-2]
- 52. Animal-free miniature gut model for microbiome research [https://www.uva.nl/en/shared-content/faculteiten/en/faculteit-der-natuurwetenschappen-wiskunde-en-informatica/news/2025/09/animal-free-miniature-gut-model-for-microbiome-research.html?origin=tm%2BGL7J1QJuL0jTefKFYWQ]
- 53. Molecular mechanisms of host-microbiome interactions [https://www.sciencedirect.com/journal/cell-host-and-microbe/special-issue/1003XGLDPK0]
- 54. Bridging two worlds: Host Microbiota crosstalk in health and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12576186/]
- 55. Human Microbiome Market Industry Research 2025-2035 [https://finance.yahoo.com/news/human-microbiome-market-industry-research-081200143.html]
- 56. Underscoring long-term host-microbiome interactions in a ... [https://www.nature.com/articles/s41522-024-00641-2]
- 57. Science in 3D: How organoids and organs-on-chips can ... [https://www.jax.org/news-and-insights/2025/september/science-in-3d-how-organoids-and-organs-on-chips-can-help-scientists-study-host-immune-microbiome-interactions]
- 58. Developments in gastrointestinal organoid cultures to ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1521044/full]
- 59. the role of organoids in studying the gut microbiota-tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12555020/]
- 60. A physiologically relevant culture platform for long-term ... [https://pubmed.ncbi.nlm.nih.gov/37331612/]
- 61. Metagenomic biomarker discovery and explanation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3218848/]
- 62. Small molecule metabolites: discovery of biomarkers and ... [https://www.nature.com/articles/s41392-023-01399-3]
- 63. Systematic, Evidence-Based Discovery of Biomarkers at the NCI [https://pmc.ncbi.nlm.nih.gov/articles/PMC3679913/]
- 64. Reliable Biomarker discovery from Metagenomic data via ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-017-1738-1]
- 65. Exploring the Microbiome Analysis and Visualization Landscape [https://pmc.ncbi.nlm.nih.gov/articles/PMC9580862/]
- 66. Mass spectrometry based biomarker discovery, verification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5528535/]
- 67. Recent advances of engineered probiotics for therapeutic ... [https://www.sciencedirect.com/science/article/pii/S2693125725000408]
- 68. The challenges and opportunities in the expanding horizons ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12584655/]
- 69. Microbial Therapeutics in Cancer: Translating Probiotics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12551701/]
- 70. Postbiotics as microbial-derived therapeutics for wound ... [https://pubmed.ncbi.nlm.nih.gov/41286901/]
- 71. Fecal Microbiota Transplantation: Application Scenarios ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1556827/full]
- 72. Research status and development trends of probiotics in ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1650883/full]
- 73. Recent advances in prebiotics: Classification, mechanisms, ... [https://www.sciencedirect.com/science/article/pii/S266683352500142X]
- 74. A Consensus Statement on establishing causality, ... [https://pubmed.ncbi.nlm.nih.gov/40033063/]
- 75. A Consensus Statement on establishing causality ... [https://www.nature.com/articles/s41575-025-01041-3]
- 76. A Consensus Statement on establishing causality ... [https://humanmicrobiomeaction.eu/a-consensus-statement-on-establishing-causality-therapeutic-applications-and-the-use-of-preclinical-models-in-microbiome-research/]
- 77. Is it possible to overcome issues of external validity in ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-018-1678-1]
- 78. New consensus on the healthy human microbiome concept [https://www.gutmicrobiotaforhealth.com/new-consensus-on-the-healthy-human-microbiome-concept/]
- 79. Nobel 2025: Immune Tolerance and 3D In Vitro Models [https://insphero.com/nobel2025-celebrating-discoveries-in-immune-tolerance/]
- 80. MIT researchers invent new human brain model to enable ... [https://news.mit.edu/2025/researchers-invent-human-brain-model-to-enable-disease-research-drug-discovery-1105]
- 81. NIH Launches New Framework to Model Whole-Person ... [https://www.labmanager.com/nih-launches-new-framework-to-model-whole-person-health-34468]
- 82. Innovative engineering approaches to model host-microbiome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12646538/]
- 83. Multi-omics decodes host-specific and environmental ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1618177/full]
- 84. Microbiome confounders and quantitative profiling ... [https://www.nature.com/articles/s41591-024-02963-2]
- 85. Methodology for biomarker discovery with reproducibility in ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-024-05639-3]
- 86. Large-scale microbiome data integration enables robust ... [https://www.nature.com/articles/s43588-022-00247-8]
- 87. The potential of including the microbiome as biomarker in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11538166/]
- 88. Systems biology and microbiome innovations for ... [https://www.nature.com/articles/s41540-025-00607-w]
- 89. Microbiome metabolite quantification methods enabling ... [https://www.sciencedirect.com/science/article/pii/S1046202323002189]
- 90. Microbiome-guided precision medicine: Mechanistic ... [https://www.sciencedirect.com/science/article/pii/S3050632825000186]
- 91. The human microbiome in clinical translation: from bench to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12479421/]
- 92. Host/microbiota interactions in health and diseases—Time ... [https://www.nature.com/articles/s41385-021-00383-w]
- 93. Hostâ€microbiome interactions in health and disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6490538/]
- 94. Nutrition & microbiome research highlights NeuroGASTRO ... [https://www.gutmicrobiotaforhealth.com/nutrition-and-microbiome-research-highlights-from-neurogastro-2025/]
- 95. Present and future of microbiome-targeting therapeutics [https://pmc.ncbi.nlm.nih.gov/articles/PMC12126222/]
- 96. Metabolic modeling of host-microbe interactions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12538087/]
- 97. Quantifying the intra- and inter-species ... [https://www.nature.com/articles/s41467-025-61368-y]
- 98. From big data and experimental models to clinical trials [https://www.sciencedirect.com/science/article/pii/S0092867425001072]
- 99. Replacing Animal Testing with Stem Cell-Organoids [https://pmc.ncbi.nlm.nih.gov/articles/PMC11319430/]
- 100. Why a human-first approach is the future of drug discovery [https://www.drugdiscoverynews.com/why-a-human-first-approach-is-the-future-of-drug-discovery-16647]
- 101. Non-Animal & Human-Relevant Research News [https://riseforanimals.org/news/sci-news-sept-2025/]
- 102. Artificial intelligence-, organoid-, and organ-on-chip-powered ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12615408/]
- 103. Mapping the Trajectory of Organoid Research: Insights into ... [https://www.sciencedirect.com/science/article/pii/S2666138125000179]
- 104. First-of-its-kind organoid centre to reduce reliance on ... [https://www.ddw-online.com/first-of-its-kind-organoid-centre-to-reduce-reliance-on-animal-models-37405-202510/]
- 105. Machine learning-based meta-analysis reveals gut ... [https://www.nature.com/articles/s41467-025-56829-3]
- 106. Beyond Animals: Revolutionizing Drug Discovery with Human ... [https://wyss.harvard.edu/news/beyond-animals-revolutionizing-drug-discovery-with-human-relevant-models/]
- 107. Omics and Multi-Omics in IBD: No Integration, ... [https://www.mdpi.com/1422-0067/24/19/14912]
- 108. Frontiers | Multi-omics approaches for biomarker discovery and precision diagnosis of prediabetes [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1520436/full]
- 109. Longitudinal multi-omics of host–microbe dynamics in prediabetes | Nature [https://www.nature.com/articles/s41586-019-1236-x]
- 110. Integrated multi-omics analysis reveals the functional ... [https://pubmed.ncbi.nlm.nih.gov/40488467/]
- 111. The dynamics of the gut microbiota in prediabetes during a ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-025-01508-7]
- 112. Multi-omics signatures in new-onset diabetes predict metabolic response to dietary inulin: findings from an observational study followed by an interventional trial | Nutrition & Diabetes [https://www.nature.com/articles/s41387-023-00235-5]
- 113. Visual analysis of multi-omics data [https://www.frontiersin.org/journals/bioinformatics/articles/10.3389/fbinf.2024.1395981/full]
- 114. Spaco: A comprehensive tool for coloring spatial data at ... [https://www.sciencedirect.com/science/article/pii/S2666389923003240]
- 115. Unveiling The Therapeutic Potential of Probiotics: A Review [https://www.sciencedirect.com/science/article/pii/S2772566925002630]
- 116. The Impact of Diet on the Fecal Microbiota Transplantation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567472/]
- 117. Probiotics, Prebiotics, Synbiotics, and FMT for Glycemic ... [https://www.sciencedirect.com/science/article/pii/S2589936825000751]
- 118. Fecal microbiota transplantation-current perspective on ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1523870/full]
- 119. Clinical efficacy of fecal microbiota transplantation in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12536323/]
- 120. The effectiveness of treatment with probiotics in preventing ... [https://pubmed.ncbi.nlm.nih.gov/40217146/]
- 121. Vaginal host immune-microbiome-metabolite interactions ... [https://www.nature.com/articles/s41522-025-00671-4]
- 122. Association of Early Pregnancy Inflammatory Indices with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12524358/]
- 123. An Explainable Machine Learning Model for Predicting ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1665935/full]
- 124. Gut microbiome regulates inflammation and insulin ... [https://www.nature.com/articles/s41392-024-01746-y]
- 125. Mechanisms linking gut microbial metabolites to insulin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8192250/]
- 126. Metabolic modeling reveals a multi-level deregulation of ... [https://www.nature.com/articles/s41467-025-60233-2]
- 127. Human Microbiome Market & Therapeutic Pipeline 2025 [https://www.strategicmarketresearch.com/blogs/human-microbiome-market-clinical-trials-pipeline]
- 128. The regulatory framework for microbiome-based therapies [https://www.nature.com/articles/s41522-025-00683-0]
- 129. Gut bioengineered models to study host-microbiota- ... [https://www.oaepublish.com/articles/mrr.2025.45]
- 130. challenges in translating microbiome research to clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12550608/]
- 131. Targeting Microbiota 2025: Decoding the microbiome to ... [https://www.eurekalert.org/news-releases/1104444]