Mastering CLSI EP12: A Comprehensive Guide to Evaluating Qualitative Binary Test Performance
This guide provides researchers, scientists, and drug development professionals with a complete framework for evaluating qualitative, binary output examinations based on the CLSI EP12 protocol.
Mastering CLSI EP12: A Comprehensive Guide to Evaluating Qualitative Binary Test Performance
Abstract
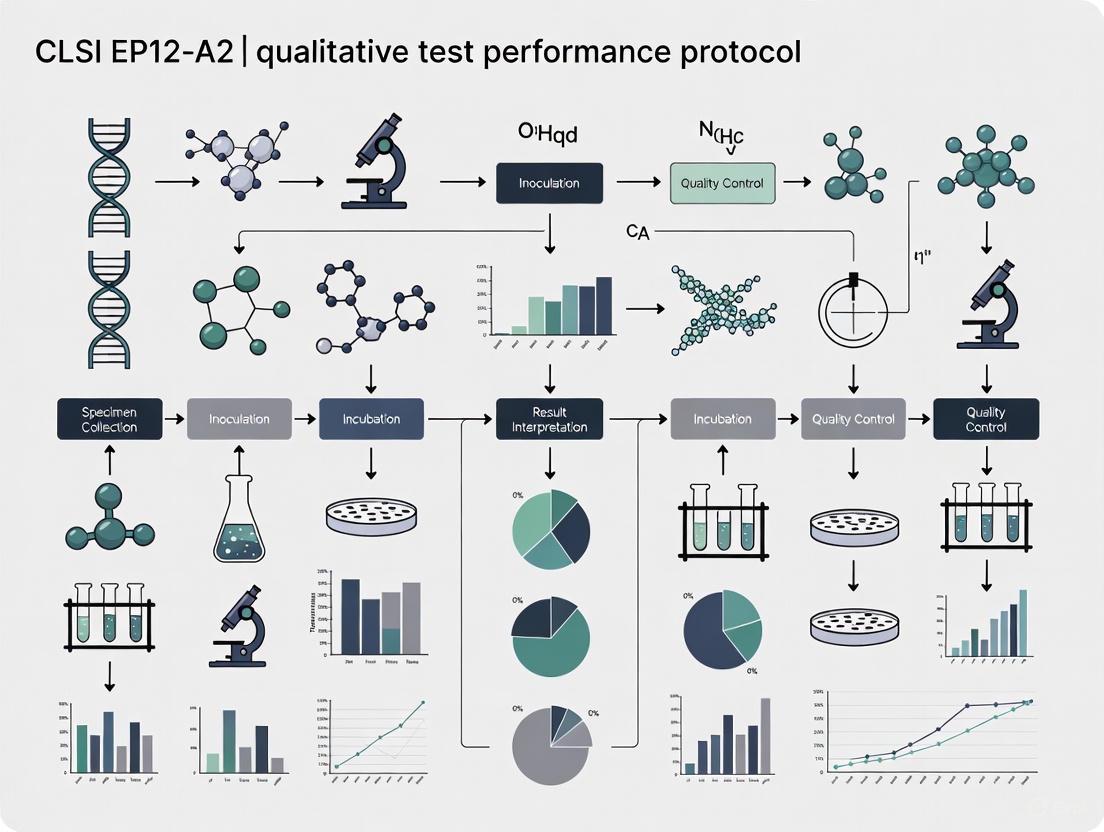
This guide provides researchers, scientists, and drug development professionals with a complete framework for evaluating qualitative, binary output examinations based on the CLSI EP12 protocol. Covering foundational principles, methodological protocols, troubleshooting strategies, and validation techniques, it addresses the transition from the established EP12-A2 guideline to the current 3rd edition. The content synthesizes CLSI standards with practical applications, including precision estimation, clinical agreement studies, interference testing, and the assessment of modern assay types, to ensure reliable performance verification in both development and laboratory settings.
Understanding CLSI EP12: The Foundation of Qualitative Test Evaluation
The Clinical and Laboratory Standards Institute (CLSI) guideline EP12 - Evaluation of Qualitative, Binary Output Examination Performance provides a standardized framework for evaluating the performance of qualitative diagnostic tests that produce binary outcomes [1]. This protocol establishes rigorous methodologies for assessing key performance parameters of tests that yield simple "yes/no" results, such as positive/negative, present/absent, or reactive/nonreactive [2]. The guideline serves as a critical resource for ensuring the reliability and accuracy of qualitative tests across the medical laboratory landscape, from simple rapid tests to complex molecular assays.
The third edition of EP12, published in March 2023, represents a significant evolution from the previous EP12-A2 version published in 2008 [1] [2]. This updated standard has been officially recognized by the U.S. Food and Drug Administration (FDA) for use in satisfying regulatory requirements for medical devices, underscoring its importance in the diagnostic regulatory landscape [3]. The guideline is designed for both manufacturers developing commercial in vitro diagnostics (IVDs) and medical laboratories creating laboratory-developed tests (LDTs), providing protocols applicable throughout the test life cycle [1].
Scope and Applications of EP12
CLSI EP12 provides comprehensive guidance for performance evaluation during the Establishment and Implementation Stages of the Test Life Phases Model of examinations [1]. The standard specifically characterizes a target condition with only two possible outputs, making it applicable to a wide range of qualitative tests used in clinical practice and research settings.
The scope of EP12 covers several critical areas essential for proper test evaluation. For test developers, including both commercial manufacturers and laboratory developers, EP12 offers product design guidance and performance evaluation protocols [1]. For end-users in medical laboratories, the guideline provides methodologies to verify examination performance in their specific testing environments, ensuring that performance claims are met in practice [1]. The standard also addresses multiple performance characteristics including imprecision, clinical performance (sensitivity and specificity), stability, and interference testing [1].
Notably, tests that fall outside EP12's scope include those providing outputs with more than two possible categories in an unordered set or those reporting ordinal categories [1]. The guideline's applications span diverse testing platforms, from simple home tests for detecting pathogens like the COVID-19 virus to complex next-generation sequencing assays for diagnosing specific cancers [2].
Table: Key Applications of CLSI EP12 Across Test Types
| Test Category | Examples | EP12 Application Focus |
|---|---|---|
| Simple Rapid Tests | Home tests (e.g., COVID-19 antigen tests) | Clinical performance verification, imprecision assessment |
| Molecular Assays | PCR-based detection methods | Lower limit of detection determination, precision evaluation |
| Complex Sequencing | Next-generation sequencing for cancer diagnosis | Precision evaluation, clinical performance validation |
| Laboratory-Developed Tests | Laboratory-developed binary examinations | Complete performance validation, stability assessment |
Core Components and Evaluation Framework
Precision and Imprecision Assessment
EP12 provides detailed methodologies for evaluating the precision of qualitative, binary output examinations, with a particular focus on estimating C5 and C95 values [1]. These statistical measures represent the analyte concentrations at which the examination produces positive results 5% and 95% of the time, respectively, effectively defining the concentration range where test results transition from consistently negative to consistently positive. Determining these transition points is crucial for understanding the reliability of a qualitative test across different analyte concentrations.
The guideline includes specific protocols for assessing observer precision, which is particularly relevant for tests involving subjective interpretation of results [2]. For advanced technologies like next-generation sequencing, EP12 provides specialized approaches for precision evaluation that account for the unique characteristics of these platforms [2]. The precision assessment framework helps developers and laboratories identify and quantify the random variation inherent in qualitative testing processes, enabling them to establish the reproducibility and repeatability of their examinations under defined conditions.
Clinical Performance Evaluation
The evaluation of clinical performance represents a cornerstone of the EP12 framework, focusing primarily on the assessment of sensitivity and specificity [1]. These fundamental metrics measure a test's ability to correctly identify true positives (sensitivity) and true negatives (specificity) when compared to an appropriate reference standard. The guideline provides standardized protocols for designing studies that generate reliable and statistically valid estimates of these parameters, ensuring that performance claims are substantiated by robust evidence.
EP12 emphasizes the importance of examination agreement in method comparison studies, providing methodologies for evaluating how well a new test aligns with established reference methods or clinical outcomes [1]. The clinical performance assessment protocols are designed to be flexible enough to accommodate different types of binary examinations while maintaining methodological rigor, whether the test is intended for diagnostic, screening, or monitoring purposes.
Stability and Interference Testing
The third edition of EP12 introduces expanded guidance on reagent stability testing, addressing the need to establish how long reagents maintain their performance characteristics under specified storage conditions [1] [2]. This component is critical for both manufacturers establishing shelf-life claims and laboratories verifying stability upon receipt of reagents. The standard provides systematic approaches for evaluating stability over time, helping to ensure that test performance remains consistent throughout a product's claimed shelf life.
The guideline also comprehensively addresses interference testing, providing methodologies to identify and quantify the effects of various interfering substances that may affect test performance [1]. These protocols help developers and laboratories understand how common interferents such as hemolysis, lipemia, icterus, or specific medications might impact test results, enabling them to establish limitations for the test or provide appropriate warnings to users.
Experimental Protocols and Methodologies
Precision Study Design
EP12 outlines structured approaches for designing precision studies that generate meaningful, statistically valid data for qualitative tests. The precision evaluation protocol involves testing multiple replicates of samples with analyte concentrations spanning the anticipated transition zone between negative and positive results. This approach allows for comprehensive characterization of a test's imprecision profile across the clinically relevant concentration range.
A typical precision study following EP12 recommendations would include several key elements. Sample selection should include concentrations near the expected C5 and C95 points to adequately characterize the transition zone. Replication strategies involve testing multiple replicates (typically 60 or more as recommended in previous editions) across multiple runs, days, and operators to capture different sources of variation. For observer precision studies, the protocol incorporates multiple readers interpreting the same set of samples to assess inter-observer variability, which is particularly important for tests with subjective interpretation components [2].
Table: Key Components of EP12 Precision Evaluation
| Study Element | Protocol Specification | Purpose |
|---|---|---|
| Sample Concentration Levels | Multiple levels spanning negative, transition, and positive ranges | Characterize performance across analytical measurement range |
| Replication Scheme | Multiple replicates across runs, days, operators | Capture different sources of variation |
| Statistical Analysis | C5 and C95 estimation with confidence intervals | Quantify transition zone with precision |
| Observer Variability | Multiple readers, blinded interpretation | Assess subjectivity in result interpretation |
Clinical Performance Study Methodology
The clinical performance evaluation protocol in EP12 provides a rigorous framework for establishing the diagnostic accuracy of qualitative tests through method comparison studies. The fundamental approach involves testing a set of clinical samples with both the test method and a reference method, then comparing the results to calculate performance metrics including sensitivity, specificity, and overall agreement.
The recommended methodology encompasses several critical design considerations. Sample selection should include an appropriate mix of positive and negative samples reflecting the intended use population, with sample size calculations providing sufficient statistical power for reliability estimates. Reference method requirements specify that the comparator should be a well-established method with known performance characteristics, preferably a gold standard for the condition being detected. Blinding procedures ensure that operators performing the test method and reference method are blinded to each other's results to prevent interpretation bias. For tests with an internal continuous response, EP12 provides additional guidance on establishing appropriate cutoff values that optimize the balance between sensitivity and specificity [2].
Verification Protocols for Implementation
CLSI EP12 includes specific guidance for verification studies conducted by end-user laboratories to confirm that a test performs according to manufacturer claims or established specifications in their specific testing environment [1]. The companion document EP12IG - Verification of Performance of a Qualitative, Binary Output Examination Implementation Guide provides practical guidance for laboratories on conducting these verification studies [4].
The verification protocol focuses on confirming several key performance characteristics using a manageable number of samples. Precision verification typically involves testing negative, low-positive, and positive samples in replicates across multiple runs to confirm reproducible results. Clinical performance verification usually requires testing a panel of well-characterized samples to confirm stated sensitivity and specificity claims. Stability verification may involve testing reagents near their expiration date or under stressed conditions to confirm performance throughout the claimed shelf life. Interference verification often includes testing samples with and without potential interferents to confirm that common substances do not affect results.
Essential Research Reagent Solutions
The implementation of EP12 protocols requires specific research reagents and materials carefully selected to ensure comprehensive test evaluation. These reagents form the foundation of robust performance studies that generate reliable, reproducible data.
Table: Essential Research Reagents for EP12 Compliance Studies
| Reagent Category | Specific Examples | Function in EP12 Studies |
|---|---|---|
| Characterized Clinical Samples | Positive samples with known concentrations, negative samples from healthy donors, borderline samples near cutoff | Serve as test materials for precision and clinical performance studies |
| Interference Substances | Hemolysed blood, lipid emulsions, bilirubin solutions, common medications | Evaluate test robustness against potential interferents |
| Stability Testing Materials | Reagents at different manufacturing dates, accelerated stability samples | Assess reagent stability over time and storage conditions |
| Reference Standard Materials | International standards, certified reference materials, well-characterized patient samples | Serve as comparator for method comparison studies |
| Quality Control Materials | Negative, low-positive, and high-positive control materials | Monitor assay performance throughout study duration |
Relationship with Other CLSI Standards
CLSI EP12 does not function in isolation but forms part of an interconnected ecosystem of standards that collectively support comprehensive test evaluation throughout the test life cycle. Understanding these relationships is essential for proper implementation of the guideline and for navigating the broader landscape of laboratory standards.
EP12 maintains a particularly important relationship with CLSI EP19 - A Framework for Using CLSI Documents to Evaluate Medical Laboratory Test Methods [1] [5]. EP19 provides the overarching Test Life Phases Model that defines the Establishment and Implementation stages for which EP12 provides specific guidance [2]. Laboratories are encouraged to use EP19 as a fundamental resource to identify relevant CLSI EP documents, including EP12, for verifying performance claims for both laboratory-developed tests and regulatory-cleared or approved test methods [5].
For laboratories implementing qualitative tests, CLSI offers EP12IG, a dedicated implementation guide that provides practical, step-by-step guidance for verifying the performance of qualitative, binary output examinations in routine laboratory practice [4]. This companion document helps laboratories apply the more comprehensive principles outlined in EP12 to their specific verification needs, outlining minimum procedures for assessing imprecision, clinical performance, stability, and interferences.
Regulatory Impact and Industry Significance
The recognition of CLSI EP12 by the U.S. Food and Drug Administration as a consensus standard for medical devices significantly enhances its importance in the diagnostic industry [3]. This formal recognition means that manufacturers can use EP12 protocols to generate data that supports premarket submissions for FDA clearance or approval of qualitative tests, potentially streamlining the regulatory pathway for new diagnostic devices.
The FDA has evaluated EP12 and determined that it possesses the scientific and technical merit necessary to support regulatory requirements [3]. The standard is recognized in its entirety, reflecting the agency's confidence in the comprehensive nature of the guidance it provides [3]. Relevant FDA guidance documents that align with EP12 include "Statistical Guidance on Reporting Results from Studies Evaluating Diagnostic Tests" and "Appropriate Use of Voluntary Consensus Standards in Premarket Submissions for Medical Devices" [3].
For the global diagnostic industry, EP12 provides a harmonized approach to evaluating qualitative test performance, potentially facilitating international market access for tests developed according to its principles. The standard's comprehensive coverage of key performance parameters—including precision, clinical performance, stability, and interference—ensures that tests evaluated using its protocols undergo rigorous assessment comparable to international standards.
CLSI EP12 represents a comprehensive, scientifically robust framework for evaluating the performance of qualitative, binary output examinations throughout their development and implementation lifecycle. The third edition, published in 2023, incorporates significant advances in laboratory medicine since the previous 2008 edition, expanding its applicability to contemporary testing platforms from simple rapid tests to complex molecular assays [1] [2].
The guideline's structured approach to assessing precision, clinical performance, stability, and interference provides developers and laboratories with a standardized methodology for generating reliable performance data. Its recognition by regulatory bodies like the FDA further underscores its importance in the medical device ecosystem [3]. As qualitative tests continue to evolve in complexity and application, CLSI EP12 will remain an essential resource for ensuring their reliability, accuracy, and clinical utility in modern laboratory medicine.
Defining Qualitative, Binary Output Examinations and Their Scope
In the clinical laboratory, qualitative, binary output examinations are diagnostic tests designed to characterize a target condition with only two possible results [1] [2]. These outcomes are typically reported as dichotomous pairs such as positive/negative, present/absent, or reactive/nonreactive [1]. Within the framework of CLSI EP12 research, these tests are distinguished from quantitative assays (which provide a continuous numerical result) and other qualitative tests with more than two unordered output categories (nominal) or ordered outputs (ordinal or semi-quantitative), which fall outside the scope of the EP12 guideline [1] [6]. The fundamental objective of a binary examination is to deliver a straightforward "yes" or "no" answer regarding the presence of a specific analyte or condition, supporting critical clinical decisions in areas ranging from simple home testing to complex molecular diagnostics for diseases like cancer [2].
The Clinical and Laboratory Standards Institute (CLSI) published the third edition of the EP12 guideline, "Evaluation of Qualitative, Binary Output Examination Performance," in March 2023 [2]. This document supersedes the earlier EP12-A2 version published in 2008 and provides an expanded framework for developers—including both commercial manufacturers and medical laboratories creating laboratory-developed tests (LDTs)—to design and evaluate binary examinations during the Establishment and Implementation stages of the Test Life Phases Model [1] [2]. The protocol is also intended to aid end-users in verifying examination performance within their specific testing environments, ensuring reliability and compliance with regulatory requirements recognized by bodies such as the U.S. Food and Drug Administration (FDA) [1].
The Evaluation Framework: Key Performance Parameters
Evaluating the performance of qualitative, binary tests requires a specific approach distinct from that used for quantitative assays. The CLSI EP12 guideline provides a structured framework for this evaluation, focusing on several critical parameters that collectively define a test's reliability and diagnostic utility [1].
Precision (Imprecision)
For qualitative tests, precision refers to the closeness of agreement between independent test results obtained under stipulated conditions, essentially measuring the test's random error and reproducibility [6]. In the context of binary outputs, precision evaluation often involves estimating the C5 and C95 thresholds—the analyte concentrations at which the test result is positive 5% and 95% of the time, respectively [1]. These thresholds help define the concentration range where the test response transitions from consistently negative to consistently positive, characterizing the assay's imprecision around its cutoff value. Precision studies may also include observer precision evaluations, particularly for tests that involve subjective interpretation of results [2].
Clinical Performance: Sensitivity and Specificity
The clinical performance of a binary test is primarily assessed through its sensitivity and specificity [1] [6]. These metrics evaluate the test's analytical accuracy or agreement with a reference method or clinical truth.
- Sensitivity (diagnostic sensitivity) measures the test's ability to correctly identify positive cases, calculated as the proportion of true positives detected among all actual positive samples.
- Specificity (diagnostic specificity) measures the test's ability to correctly identify negative cases, calculated as the proportion of true negatives detected among all actual negative samples.
Evaluation of clinical performance typically involves method comparison studies using contingency tables (2x2 tables) to compare the new test's results against a reference standard [6]. The experimental design must include appropriate clinical samples that adequately represent the intended use population and target condition.
Stability and Interference Testing
The updated EP12 guideline expands beyond precision and clinical performance to include evaluations of reagent stability and the effects of interfering substances [1] [2]. Stability testing determines the shelf-life of reagents and the test system's performance over time, while interference testing identifies substances that might adversely affect the test result, leading to false positives or false negatives. These additional parameters are crucial for ensuring the test's robustness under routine laboratory conditions and are particularly important for developers creating laboratory-developed tests or modifying existing commercial assays.
Table 1: Key Performance Parameters for Qualitative, Binary Output Examinations
| Parameter | Definition | Evaluation Method | Significance |
|---|---|---|---|
| Precision (Imprecision) | Closeness of agreement between independent test results [6] | Estimation of C5 and C95 thresholds; reproducibility studies [1] | Measures random error and reproducibility |
| Sensitivity | Proportion of true positives correctly identified [6] | Method comparison with reference standard using contingency tables [6] | Ability to detect positive cases |
| Specificity | Proportion of true negatives correctly identified [6] | Method comparison with reference standard using contingency tables [6] | Ability to detect negative cases |
| Stability | Performance maintenance over time and under specified storage conditions [1] | Repeated testing of stored reagents at intervals [1] | Determines shelf-life and reliability |
| Interference | Effect of substances that may alter test results [1] | Testing samples with and without potential interferents [1] | Identifies sources of false positives/negatives |
Experimental Protocols and Evaluation Methodologies
Integrated Protocol for Precision and Accuracy
A fundamental advancement in the evaluation of qualitative tests is the implementation of a single-experiment approach that simultaneously assesses both precision and accuracy [6]. This efficient protocol involves repeatedly testing a panel of samples that span the assay's critical range, particularly around the clinical cutoff point. The panel should include samples with known status (positive, negative, and near the cutoff) tested in multiple replicates across different runs, days, and operators if applicable. The resulting data allows for the construction of contingency tables that facilitate the calculation of both within-run and between-run precision (as percent agreement) and accuracy compared to the reference method [6]. This integrated approach provides a comprehensive view of the test's analytical performance while optimizing resource utilization.
Method Comparison Studies
When introducing a new binary test to replace an existing method, a method comparison study is essential [6]. This study involves testing an appropriate number of clinical samples (typically 50-100) by both the new and comparison methods, ensuring that the sample panel adequately represents the entire spectrum of the target condition, including positive, negative, and borderline cases. The results are then tabulated in a 2x2 contingency table, from which metrics such as overall percent agreement, positive percent agreement (analogous to sensitivity), and negative percent agreement (analogous to specificity) can be calculated. For complex tests such as those based on PCR methods or next-generation sequencing, the EP12 guideline provides supplemental information on determining the lower limit of detection and precision evaluation specific to these technologies [2].
Verification of Manufacturer Claims
For laboratories implementing commercially developed binary tests, the focus shifts from full validation to verification of the manufacturer's performance claims [6]. The CLSI EP12 protocol provides guidance for this verification process, which typically involves confirming the claimed sensitivity, specificity, and precision using a smaller set of samples tested in the laboratory's own environment with its personnel. This verification ensures that the test performs as expected in the specific setting where it will be used routinely and is required by accreditation standards such as CAP, ISO 15189, and ISO 17025 [6].
Essential Research Reagent Solutions
The evaluation of qualitative, binary output examinations requires specific materials and reagents to ensure accurate and reproducible results. The following table details key components essential for conducting performance assessments according to CLSI EP12 protocols.
Table 2: Essential Research Reagents and Materials for Evaluation Studies
| Reagent/Material | Function and Specification | Application in Evaluation |
|---|---|---|
| Characterized Clinical Samples | Well-defined positive and negative samples for target analyte; should include levels near clinical cutoff [6] | Precision studies, method comparison, determination of sensitivity and specificity [6] |
| Reference Method Materials | Complete test system for comparison method (gold standard) [6] | Method comparison studies to establish accuracy and agreement [6] |
| Interference Test Substances | Potential interferents specific to test platform (e.g., hemoglobin, bilirubin, lipids, common medications) [1] | Interference testing to identify substances that may cause false positives or negatives [1] |
| Stability Testing Materials | Reagents stored under various conditions (temperature, humidity, light) and timepoints [1] | Stability evaluation to determine shelf-life and optimal storage conditions [1] |
| Quality Control Materials | Positive and negative controls with defined expected results [6] | Daily quality assurance, precision monitoring, lot-to-lot reagent verification [6] |
The CLSI EP12 guideline provides a standardized framework for defining and evaluating qualitative, binary output examinations, emphasizing their distinct nature from quantitative and semi-quantitative assays. The third edition, published in 2023, expands upon the previous EP12-A2 standard by incorporating broader test types, integrated protocols for design and validation, and additional evaluation parameters including stability and interference testing. For researchers and drug development professionals, understanding this scope and the corresponding evaluation methodologies is fundamental to ensuring the reliability and accuracy of binary tests across their development and implementation lifecycle. Proper application of these protocols—encompassing precision studies, clinical performance assessment, and interference testing—ensures that these clinically vital diagnostic tools perform consistently and meet regulatory requirements for their intended use.
Key Changes from EP12-A2 to the Current 3rd Edition
The Clinical and Laboratory Standards Institute (CLSI) guideline EP12, titled "Evaluation of Qualitative, Binary Output Examination Performance," serves as a critical framework for assessing the performance of qualitative diagnostic tests that produce binary outcomes (e.g., positive/negative, present/absent, reactive/nonreactive). The evolution from the Second Edition (EP12-A2) to the Third Edition (EP12-Ed3) represents a significant advancement in laboratory medicine protocols, reflecting the changing landscape of diagnostic technologies and regulatory requirements. Published on March 7, 2023, this latest edition incorporates substantial revisions that expand its applicability, enhance methodological rigor, and address emerging challenges in qualitative test evaluation [1].
The transition from EP12-A2 to EP12-Ed3 marks a paradigm shift from a primarily user-focused protocol to a comprehensive guideline serving both developers and end-users. While EP12-A2, published in 2008, provided "the user with a consistent approach for protocol design and data analysis when evaluating qualitative diagnostics tests" [7], the third edition substantially broadens this scope to include "product design guidance and protocols for performance evaluation of the Establishment and Implementation Stages of the Test Life Phases Model of examinations" [1]. This expansion acknowledges the growing complexity of qualitative examinations and the need for robust evaluation frameworks throughout the test lifecycle, from initial development through clinical implementation.
Expanded Scope and Application
Broadened Procedural Coverage
The third edition of EP12 significantly expands the types of procedures covered to reflect ongoing advances in laboratory medicine [1]. While EP12-A2 focused primarily on traditional qualitative diagnostics tests, EP12-Ed3 addresses the evaluation needs of contemporary binary output examinations, including laboratory-developed tests (LDTs) and advanced commercial assays. This expansion ensures the guideline remains relevant amidst rapid technological innovations in diagnostic testing.
The scope explicitly characterizes "a target condition (TC) with only two possible outputs (eg, positive or negative, present or absent, reactive or nonreactive)" [1]. The guideline maintains clear boundaries, excluding "examinations that provide outputs with more than two possible categories in an unordered (nominal) set or that report ordinal categories" [1]. This precise scope definition provides clarity for developers and laboratories in determining the appropriate evaluation framework for their specific tests.
Enhanced Target Audience
EP12-Ed3 is deliberately "written for both manufacturers of qualitative, binary, results-reporting or output examinations (referred to as qualitative, binary examinations throughout) and medical laboratories that create laboratory-developed, binary examinations (both termed developers)" [1]. This represents a substantial shift from EP12-A2, which primarily addressed laboratory personnel conducting verification studies. The expanded audience reflects the growing responsibility of both manufacturers and laboratories in ensuring test performance and reliability throughout the test lifecycle.
Table: Comparison of EP12-A2 and EP12-Ed3 Scope and Application
| Feature | EP12-A2 (2008) | EP12-Ed3 (2023) |
|---|---|---|
| Primary Focus | User evaluation of qualitative test performance [7] | Product design and performance evaluation for establishment and implementation stages [1] |
| Target Audience | Laboratory users conducting method evaluation [7] | Manufacturers and laboratories developing binary examinations (termed "developers") [1] |
| Procedures Covered | Qualitative diagnostic tests [7] | Expanded types reflecting advances in laboratory medicine [1] |
| Regulatory Recognition | FDA recognized [8] | FDA evaluated and recognized for regulatory requirements [1] [3] |
Key Technical Enhancements and Novel Content
Comprehensive Protocol Additions
EP12-Ed3 introduces substantial technical enhancements by adding "protocols to be used by developers, including commercial manufacturers or medical laboratories, during examination procedure design as well as for validation and verification" [1]. These protocols provide a structured framework for test development and evaluation that was not comprehensively addressed in the previous edition. The added protocols facilitate a more systematic approach to test design, potentially reducing development iterations and enhancing final product quality.
The third edition also incorporates "topics such as stability and interferences to the existing coverage of the assessment of precision and clinical performance (or examination agreement)" [1]. These additions address critical analytical performance characteristics that directly impact test reliability in real-world settings. Stability testing protocols help establish appropriate storage conditions and shelf-life determinations, while interference testing provides methodologies for identifying and quantifying substances that may affect test results.
Statistical Reorganization
A notable structural change in EP12-Ed3 involves "moving most of the statistical details, including equations, to the appendixes" [1]. This reorganization improves the document's usability by presenting essential methodological guidance in the main body while providing comprehensive statistical details in referenced appendices. This approach caters to both general users who require procedural overviews and statistical experts who need detailed computational methods.
The statistical foundation remains robust, with maintained focus on "imprecision, including estimating C5 and C95, clinical performance (sensitivity and specificity)" [1]. These statistical measures are essential for characterizing the analytical and clinical performance of qualitative tests, providing developers with standardized approaches for quantifying key performance parameters.
Enhanced Evaluation Framework
EP12-Ed3 Enhanced Evaluation Framework Diagram
Experimental Protocols and Methodologies
Precision Evaluation for Qualitative Tests
The precision evaluation protocols in EP12-Ed3 provide methodologies for assessing imprecision in qualitative, binary output examinations, including estimating C5 and C95 values [1]. These statistical measures help define the concentration levels at which a qualitative test has a 5% and 95% probability of producing a positive result, respectively. This approach allows for more nuanced understanding of test performance near the discrimination point.
The experimental design for precision studies typically involves:
- Sample Preparation: Selection or creation of samples with analyte concentrations spanning the expected decision point
- Repeated Testing: Multiple replicate measurements (typically 20-40) at each concentration level
- Data Analysis: Calculation of positive rates at each concentration level and determination of C5, C50, and C95 through probit or logit regression
- Contextual Interpretation: Consideration of precision estimates in relation to the clinical decision point
This methodology represents an advancement over EP12-A2 by providing more granular approaches for characterizing and quantifying imprecision in qualitative tests.
Clinical Performance Assessment
Clinical performance assessment, often described as examination agreement in qualitative tests, focuses on establishing sensitivity and specificity through method comparison studies [1]. EP12-Ed3 enhances these protocols to ensure robust determination of clinical utility.
The experimental workflow includes:
- Reference Method Selection: Identification of an appropriate reference method (gold standard) for comparison
- Sample Selection: Careful selection of clinical samples representing the entire spectrum of the target condition
- Blinded Testing: Parallel testing using both the new method and reference method without knowledge of results
- Statistical Analysis: Calculation of sensitivity, specificity, predictive values, and likelihood ratios with confidence intervals
- Agreement Assessment: Evaluation of overall agreement and chance-corrected agreement using statistics like kappa
Table: Key Performance Characteristics in EP12 Evaluations
| Performance Characteristic | EP12-A2 Coverage | EP12-Ed3 Enhancements |
|---|---|---|
| Precision/Imprecision | Included with C5/C95 estimation [1] | Enhanced protocols with expanded statistical guidance [1] |
| Clinical Performance (Sensitivity/Specificity) | Method-comparison studies [7] | Comprehensive clinical performance assessment with stability and interference considerations [1] |
| Stability | Not explicitly covered | Added as a new topic with dedicated protocols [1] |
| Interference | Not explicitly covered | Added as a new topic with dedicated protocols [1] |
| Statistical Framework | Integrated in main text | Reorganized with equations in appendices [1] |
Stability and Interference Testing
The addition of stability and interference testing protocols represents one of the most significant enhancements in EP12-Ed3 [1]. These methodologies address critical real-world factors that impact test performance but were not comprehensively covered in the previous edition.
Stability Testing Protocol:
- Study Design: Implementation of real-time stability studies under intended storage conditions
- Time Points: Testing at multiple time points (e.g., 0, 3, 6, 9, 12 months) to establish performance degradation profiles
- Environmental Conditions: Evaluation of stability under various temperature, humidity, and light exposure conditions
- Reagent Performance: Assessment of critical reagent performance characteristics over time
- Data Analysis: Determination of expiration dates and storage requirements based on stability data
Interference Testing Protocol:
- Interferent Selection: Identification of potential interferents based on sample matrix and test methodology
- Sample Preparation: Creation of test samples with and without potential interferents at clinically relevant concentrations
- Experimental Comparison: Parallel testing of interferent-containing and control samples
- Result Analysis: Quantitative assessment of interference effects on test results
- Clinical Significance: Determination of whether observed interference has clinical significance
The Researcher's Toolkit: Essential Research Reagent Solutions
Table: Key Research Reagent Solutions for EP12 Protocol Implementation
| Reagent/Material | Function in EP12 Evaluations |
|---|---|
| Characterized Clinical Samples | Serve as test materials for precision, clinical performance, and stability studies; must represent intended patient population [1] |
| Stability Testing Materials | Includes reagents, calibrators, and controls stored under various conditions for stability assessment [1] |
| Interference Testing Panels | Characterized samples containing potential interferents (hemolyzed, icteric, lipemic samples) at known concentrations [1] |
| Reference Standard Materials | Well-characterized materials for method comparison studies; serves as gold standard for clinical performance assessment [1] |
| Statistical Analysis Software | Specialized software supporting CLSI protocols for data analysis according to EP12 guidelines [9] |
| 2-Heptyl-4-quinolone-15N | 2-Heptyl-4-quinolone-15N, MF:C16H21NO, MW:244.34 g/mol |
| Cholesteryl isovalerate | Cholesteryl isovalerate, MF:C32H54O2, MW:470.8 g/mol |
Implications for Diagnostic Research and Development
The evolution from EP12-A2 to EP12-Ed3 has profound implications for diagnostic researchers, scientists, and drug development professionals. The enhanced framework supports more robust test development, potentially reducing late-stage development failures and facilitating regulatory submissions. The FDA's formal recognition of EP12-Ed3 "for use in satisfying a regulatory requirement" [1] [3] underscores its importance in the regulatory landscape.
For researchers implementing the updated guideline, the expanded scope necessitates earlier consideration of evaluation criteria during test design phases. The addition of stability and interference testing protocols requires allocation of additional resources during development but ultimately produces more comprehensive performance data. The reorganization of statistical content makes the guideline more accessible while maintaining technical rigor, potentially broadening its implementation across organizations with varying statistical expertise.
The continued focus on fundamental performance characteristics like sensitivity, specificity, and imprecision, while adding contemporary considerations, ensures that tests evaluated under EP12-Ed3 meet both traditional quality standards and modern performance expectations. This balanced approach facilitates the development of reliable qualitative diagnostics that can withstand the challenges of real-world clinical implementation.
The Clinical and Laboratory Standards Institute (CLSI) EP12 guideline, titled "Evaluation of Qualitative, Binary Output Examination Performance," provides a critical framework for the performance assessment of qualitative diagnostic tests that produce binary results (e.g., positive/negative, present/absent, reactive/nonreactive). This protocol is essential for researchers, scientists, and drug development professionals involved in bringing in vitro diagnostic (IVD) tests to market or implementing them in clinical laboratories. The third edition of this guideline, published in March 2023, supersedes the EP12-A2 version and expands upon its predecessors by covering a broader range of modern procedures and providing more comprehensive guidance for the entire test life cycle [1] [2].
The core purpose of EP12 is to outline standardized methodologies for evaluating key analytical performance characteristics, ensuring that qualitative tests are reliable and clinically meaningful. Evaluations conducted according to EP12 are recognized by regulatory bodies, including the U.S. Food and Drug Administration (FDA), for satisfying regulatory requirements [1]. This guide focuses on the three pillars of performance characterization as defined within the EP12 framework: impression, clinical performance, and stability. A thorough understanding of these characteristics is fundamental to developing robust diagnostic tests and making evidence-based decisions about their adoption and use.
Evaluation of Imprecision
In the context of qualitative tests, imprecision refers to the random variation in test results upon repeated testing of the same sample. Unlike quantitative assays where imprecision is expressed as standard deviation or coefficient of variation, the evaluation of imprecision for binary output tests focuses on the consistency of the categorical result (positive or negative) [6].
Key Concepts and Protocols
A core concept in evaluating imprecision for qualitative assays is the estimation of the C5 and C95 concentrations. The C5 is the analyte concentration at which the test yields a positive result 5% of the time (the concentration where 5% of replicates are positive), while the C95 is the concentration at which 95% of replicates are positive. The range between C5 and C95 provides a measure of the assay's random error around its cutoff level [1]. Determining this range is crucial for understanding how an analyte's concentration near the decision threshold can lead to inconsistent categorical results.
CLSI EP12 recommends that precision studies be conducted over a period of 10 to 20 days to capture realistic sources of variation that might occur in the routine laboratory environment, such as different reagent lots, calibrators, operators, and environmental conditions [10]. This approach ensures that the estimated imprecision reflects the test's reproducibility in practice.
Experimental Design and Data Analysis
The experiment should include repeated testing of panels of samples with analyte concentrations known to be near the clinical decision point or the assay's cutoff. These samples should be tested in replicate over the designated time frame. The results are then analyzed to determine the proportion of positive and negative results at each concentration level.
The following workflow outlines the key steps for designing and executing an imprecision study according to EP12 principles:
Table 1: Key Reagents and Materials for Imprecision Studies
| Research Reagent/Material | Function in Experimental Protocol |
|---|---|
| Panel of Clinical Samples | Comprises the test specimens with analyte concentrations near the assay's cutoff, essential for defining the C5-C95 interval [10]. |
| Multiple Reagent Lots | Different manufacturing batches of the test kit reagents are used to incorporate inter-lot variation into the imprecision estimate [1]. |
| Quality Control Materials | Characterized samples with known expected results (positive and negative) used to monitor the assay's performance throughout the study duration. |
Evaluation of Clinical Performance
Clinical performance evaluation assesses a test's ability to correctly classify subjects who have the target condition (e.g., a disease) and those who do not. The primary metrics for this evaluation are diagnostic sensitivity and diagnostic specificity [1] [11] [10].
Sensitivity and Specificity
- Diagnostic Sensitivity is defined as the percentage of subjects with the target condition who test positive. It measures the test's ability to correctly identify true positives. A test with low sensitivity produces false negatives, which is critical to avoid in scenarios like blood donor screening or infectious disease diagnosis [11] [10].
- Diagnostic Specificity is the percentage of subjects without the target condition who test negative. It measures the test's ability to correctly identify true negatives. Low specificity leads to false positives, which can cause unnecessary anxiety and follow-up testing [11] [10].
To calculate these metrics, test results are compared against Diagnostic Accuracy Criteria (DAC), which represent the best available method for determining the true disease status (e.g., a gold standard reference method or a clinical consensus standard) [12] [10]. The comparison is typically presented in a 2x2 contingency table.
Table 2: 2x2 Contingency Table for Diagnostic Accuracy
| Diagnostic Accuracy Criteria (Truth) | ||
|---|---|---|
| Candidate Test Result | Positive | Negative |
| Positive | True Positive (TP) | False Positive (FP) |
| Negative | False Negative (FN) | True Negative (TN) |
| Sensitivity = TP / (TP + FN) x 100 | Specificity = TN / (TN + FP) x 100 |
Positive and Negative Percent Agreement (PPA/NPA)
In situations where a true gold standard is not available, and the candidate method is being compared to a non-reference comparative method, the terms Positive Percent Agreement (PPA) and Negative Percent Agreement (NPA) are used. The calculations are identical to those for sensitivity and specificity, but the context is different, as they measure agreement with a comparator rather than true diagnostic accuracy [12].
Experimental Design and Key Considerations
A robust clinical performance study requires careful planning. CLSI EP12 recommends testing a minimum of 50 positive and 50 negative specimens as determined by the DAC to reliably estimate sensitivity and specificity, respectively [11]. The samples must be representative of the intended use population and should account for various factors that can affect performance.
Several factors can significantly influence the observed sensitivity and specificity, and must be documented [11]:
- Reference Technique Used: The choice of DAC directly impacts the results.
- Type of Sample: The same test may perform differently with different sample matrices (e.g., nasal vs. nasopharyngeal swabs).
- Sample Group and Clinical Status: The stage of disease or patient demographics in the study group can affect performance.
Table 3: Essential Research Reagents for Clinical Performance Studies
| Research Reagent/Material | Function in Experimental Protocol |
|---|---|
| Well-Characterized Clinical Samples | Banked specimens with disease status confirmed by Diagnostic Accuracy Criteria; the foundation for calculating sensitivity and specificity [11] [10]. |
| Reference Standard Method | The gold standard test or established clinical criteria used as the DAC to define the true positive and true negative status of every sample [12]. |
| Blinded Sample Panels | The set of samples, with identities concealed from the analyst, to prevent bias during testing with the candidate method [12]. |
Evaluation of Stability
Stability testing is critical for determining the shelf-life of reagents and the suitable storage conditions for samples, ensuring that test performance does not deteriorate over time. The third edition of EP12 has expanded its coverage of this topic, providing protocols for developers to establish and verify stability claims [1].
Types of Stability Evaluations
- Reagent Stability: This involves testing the performance of reagents throughout their proposed shelf-life, including the evaluation of real-time stability (storage under recommended conditions) and in-use stability (after first opening or reconstitution) [1].
- Sample Stability: This evaluation determines how long a sample can be stored before analysis without affecting the test result. Stability is assessed under different conditions (e.g., room temperature, refrigerated, frozen) and time points [1].
Experimental Protocol
The fundamental approach to stability testing is to compare the results obtained using aged reagents or stored samples against the results from fresh materials. The test samples used should include both positive and negative samples, with concentrations close to the clinical cutoff, as these are most sensitive to degradation.
A stability claim is generally supported when the agreement between the results from aged and fresh materials remains within a pre-defined acceptance criterion (e.g., ≥95% agreement) [1]. The point at which performance falls below this threshold defines the end of the stability period.
Table 4: Key Materials for Stability Evaluation
| Research Reagent/Material | Function in Experimental Protocol |
|---|---|
| Challenging Sample Panel | Includes weak positive samples and negative samples, which are most likely to show performance degradation due to reagent or sample instability [1]. |
| Aged Reagent Lots | Reagents stored for predetermined times under recommended and stress conditions (e.g., elevated temperature) to establish expiration dates [1]. |
| Stored Clinical Samples | Aliquots of patient samples stored for various durations and under different temperature conditions to establish sample stability claims [1]. |
The rigorous evaluation of impression, clinical performance, and stability is a non-negotiable requirement for the development and implementation of any reliable qualitative diagnostic test. The CLSI EP12 protocol provides a standardized, statistically sound framework for this characterization, ensuring that tests meet the necessary quality standards for clinical use. For researchers and drug development professionals, adherence to these guidelines is not merely a regulatory hurdle but a fundamental scientific process. It mitigates the risk of deploying unreliable tests, which can lead to misdiagnosis, patient harm, and inefficient use of resources. By systematically applying the principles and experimental designs outlined in CLSI EP12, the diagnostic industry can continue to advance, providing healthcare providers with the accurate and dependable tools essential for modern medicine.
The U.S. Food and Drug Administration's recognition of consensus standards represents a critical mechanism for streamlining the regulatory evaluation of medical devices, including in vitro diagnostic tests. This process allows manufacturers to demonstrate conformity with established standards, thereby providing a efficient pathway to market while ensuring device safety and effectiveness. The FDA Standards Recognition Program evaluates consensus standards for their appropriateness in reviewing medical device safety and performance, with technical and clinical staff throughout the Center for Devices and Radiological Health (CDRH) participating in standards development and evaluation [13]. For researchers and developers working with qualitative test performance protocols, understanding this recognition process is essential for navigating regulatory requirements and optimizing product development strategies.
The recognition system operates under the authority of the Federal Food, Drug, and Cosmetic Act (FD&C Act), which enables the FDA to identify standards to which manufacturers may submit a declaration of conformity to demonstrate they have met relevant regulatory requirements [13]. This framework creates a predictable pathway for device evaluation, potentially reducing the regulatory burden on manufacturers while maintaining the FDA's rigorous standards for safety and effectiveness. The agency may recognize standards wholly, partially, or not at all based on their scientific and technical merit and relevance to regulatory policies [3].
FDA Recognition of CLSI EP12 Standards
Evolution from EP12-A2 to EP12 3rd Edition
The CLSI EP12 standard has undergone significant evolution, with the FDA formally recognizing the most recent version. The trajectory of this standard demonstrates the dynamic nature of regulatory science and the importance of maintaining current knowledge of recognized standards:
Table: Evolution of CLSI EP12 Standard
| Standard Version | Status | Publication Date | Key Characteristics |
|---|---|---|---|
| EP12-A2 | Superseded | 2008 | Provided protocol design and data analysis guidance for precision and method-comparison studies [14] |
| EP12 3rd Edition | Active & FDA-Recognized | March 7, 2023 | Expanded procedures, added developer protocols, included stability and interference topics [1] |
The FDA formally recognized CLSI EP12 3rd Edition on May 29, 2023, granting it recognition number 7-315 and declaring it relevant to medical devices "on its scientific and technical merit and/or because it supports existing regulatory policies" [3]. This recognition signifies that developers of qualitative, binary output tests can submit a declaration of conformity to this standard in premarket submissions, potentially streamlining the regulatory review process.
Key Technical Scope of CLSI EP12 3rd Edition
The recognized EP12 3rd Edition provides comprehensive guidance for evaluating qualitative tests with binary outcomes (e.g., positive/negative, present/absent, reactive/nonreactive). Its technical scope encompasses:
- Performance evaluation protocols for both establishment and implementation stages of the Test Life Phases Model [1]
- Assessment of imprecision through C5 and C95 estimation [1]
- Clinical performance evaluation including sensitivity and specificity determinations [1]
- Stability and interference testing to ensure reagent integrity and result accuracy [1]
- Framework verification for laboratory-developed tests (LDTs) and manufacturer-developed examinations [1]
The standard specifically excludes evaluation of tests with more than two possible output categories (nominal sets) or ordinal categories, focusing exclusively on binary outputs [3]. This focused scope ensures specialized guidance for the unique statistical and validation challenges presented by qualitative binary tests.
FDA Recognition Process Framework
Standards Recognition Pathway
The FDA has established a structured process for evaluating and recognizing consensus standards, which is critical for developers to understand when planning regulatory strategies. The recognition pathway follows a systematic approach with defined timelines and requirements:
FDA Standards Recognition Pathway
The recognition process begins when any interested party submits a request containing specific information, including the standard's title, reference number, proposed list of applicable devices, and the scientific, technical, or regulatory basis for recognition [13]. The FDA commits to responding to all recognition requests within 60 calendar days from receipt, demonstrating the agency's commitment to timely standardization [13].
Upon positive determination, the standard is added to the FDA Recognized Consensus Standards Database, where it receives a recognition number and a Supplemental Information Sheet (SIS) [13]. Importantly, manufacturers may immediately begin using the standard for declarations of conformity once it appears in the database, without waiting for formal publication in the Federal Register, though such publication does occur periodically [15] [13].
Implementation in Regulatory Submissions
For researchers and developers, the practical implementation of recognized standards in regulatory submissions represents a critical phase of the product development lifecycle. The FDA provides clear guidelines for leveraging recognized standards:
- Voluntary Conformity: Manufacturers may voluntarily choose to conform to FDA-recognized consensus standards, but conformance is not mandatory unless a standard is "incorporated by reference" into regulation [13]
- Declaration of Conformity: When manufacturers elect to conform to recognized standards, they may submit a "declaration of conformity" to satisfy relevant regulatory requirements [13]
- Premarket Submission Identification: Applicants should clearly identify any referenced standards in their CDRH Premarket Review Submission Cover Sheet (Form FDA 3514) [13]
This framework creates efficiencies in the device review process by reducing redundant testing and providing a common language for evaluating device performance. As noted by the FDA, "Standards are particularly useful when an FDA-recognized consensus standard exists that serves as a complete performance standard for a specific medical device" [13].
Implications for Qualitative Test Development
Practical Application of CLSI EP12 3rd Edition
The recognition of CLSI EP12 3rd Edition carries significant implications for developers of qualitative binary tests. The standard provides specific methodological guidance that aligns with regulatory expectations:
Table: CLSI EP12 Experimental Framework Components
| Component | Protocol Guidance | Regulatory Application |
|---|---|---|
| Analytical Sensitivity | Protocols for limit of detection (LOD) determination, particularly for PCR-based methods [2] | Supports claims for test detection capabilities |
| Precision Evaluation | Procedures for estimating C5 and C95, including next-generation sequencing and observer precision studies [2] | Demonstrates test reproducibility under specified conditions |
| Clinical Performance | Framework for assessing sensitivity, specificity, and examination agreement [1] | Validates clinical utility and diagnostic accuracy |
| Interference Testing | Methodologies for identifying substances that may affect test performance [1] | Establishes test limitations and appropriate use conditions |
| Stability Assessment | Protocols for establishing reagent stability claims [1] | Supports labeled shelf life and storage conditions |
According to Jeffrey R. Budd, PhD, Chairholder of CLSI EP12, "The third edition of CLSI EP12 describes the different types of these tests, how to accurately provide yes/no results for each, and how to assess their analytical and clinical performance. It covers binary, qualitative examinations whether they have an internal continuous response or not" [2]. This comprehensive coverage makes the standard applicable across a wide range of technologies, from simple rapid tests to complex molecular assays.
Strategic Advantages for Test Developers
The use of FDA-recognized standards like CLSI EP12 3rd Edition provides strategic advantages throughout the product lifecycle:
- Streamlined Regulatory Review: Conformity with recognized standards facilitates the premarket review process for 510(k), De Novo, PMA, and other submission types [13]
- Reduced Submission Burden: Appropriate use of declarations of conformity may reduce the amount of supporting testing documentation typically needed [13]
- Early Regulatory Alignment: Engaging with recognized standards during development phases helps align products with regulatory expectations before submission
- Benchmarking Against Established Criteria: Provides objective performance criteria for evaluating test performance against market expectations
The FDA emphasizes that "Conformity to relevant standards promotes efficiencies and quality in regulatory review" [13], highlighting the mutual benefits for both developers and regulators.
Experimental Framework for Qualitative Test Evaluation
Core Methodological Approaches
CLSI EP12 3rd Edition establishes rigorous experimental frameworks for evaluating qualitative binary tests. The key methodological approaches include:
Experimental Framework for Qualitative Tests
The standard provides specific protocols for each evaluation dimension, with statistical details and equations moved to appendices in the current edition to improve usability [1]. This structure makes the standard more accessible while maintaining technical rigor.
Essential Research Reagent Solutions
The implementation of CLSI EP12 evaluation protocols requires specific reagent solutions with defined characteristics:
Table: Essential Research Reagents for Qualitative Test Evaluation
| Reagent Category | Function in Evaluation | Performance Requirements |
|---|---|---|
| Reference Standard Panels | Establish ground truth for clinical sensitivity/specificity studies | Well-characterized specimens with known target status [16] |
| Interference Substances | Identify potential interferents affecting test performance | Common endogenous and exogenous substances relevant to specimen type [1] |
| Stability Materials | Support claimed reagent stability under various storage conditions | Representative production lots stored under controlled conditions [1] |
| Precision Panels | Evaluate within-run and between-run imprecision | Samples with analyte concentrations near clinical decision points [1] |
| Calibration Materials | Standardize instrument responses across testing platforms | Traceable to reference materials when available [16] |
These reagent solutions form the foundation for robust test evaluation according to recognized standards, enabling developers to generate reliable evidence of performance characteristics.
Regulatory Integration and Future Directions
Integration with Broader Regulatory Framework
CLSI EP12 3rd Edition does not exist in isolation but functions within a broader ecosystem of regulatory standards and guidances. The FDA recognition of this standard intersects with several important regulatory policies:
- Special Controls Guidance: For certain device types, such as reagents for detection of specific novel influenza A viruses, the standard functions alongside special controls that may include distribution restrictions to qualified laboratories [16]
- Multiple Submission Pathways: The standard supports various regulatory pathways, including traditional and abbreviated 510(k) submissions, where declarations of conformity can reduce submission burden [13]
- Postmarket Performance Validation: The standard's frameworks support both premarket evaluation and postmarket validation activities, creating continuity across the device lifecycle [16]
The FDA emphasizes that "While manufacturers are encouraged to use FDA-recognized consensus standards in their premarket submissions, conformance is voluntary, unless a standard is 'incorporated by reference' into regulation" [13]. This balanced approach encourages standards use while maintaining regulatory flexibility.
Emerging Trends in Standards Recognition
The field of standards recognition continues to evolve, with several emerging trends impacting how researchers and developers should approach qualitative test evaluation:
- Accelerated Recognition Process: The FDA has implemented a more responsive recognition system with mandated 60-day response timelines and immediate effectiveness upon database entry [13]
- ASCA Program Expansion: The Accreditation Scheme for Conformity Assessment (ASCA) program enhances confidence in declarations of conformity through qualified accreditation bodies and testing laboratories [13]
- Dynamic Standard Updates: The recognition of the EP12 3rd Edition just months after its publication demonstrates the FDA's commitment to maintaining current standards [3] [2]
- Global Harmonization: International alignment of standards reduces barriers to global market access and facilitates efficient test development
These trends highlight the increasing importance of standards conformity as a strategic tool in the medical device development process, particularly for complex qualitative tests requiring robust performance validation.
The FDA recognition of consensus standards like CLSI EP12 3rd Edition represents a cornerstone of the modern medical device regulatory framework. For developers of qualitative binary tests, understanding and implementing this recognized standard provides a pathway to demonstrating both analytical and clinical performance in alignment with regulatory expectations. The rigorous methodological framework offered by EP12, combined with the efficiency of the FDA recognition process, creates a predictable environment for test development and validation. As the field of diagnostic testing continues to evolve with emerging technologies and novel applications, the role of recognized standards in ensuring test reliability while facilitating efficient market access will remain increasingly important for researchers, scientists, and drug development professionals.
Implementing EP12 Protocols: A Step-by-Step Methodological Guide
Designing Precision Studies and Estimating the Imprecision Interval (C5 to C95)
Within the framework of CLSI EP12, the evaluation of qualitative, binary-output tests (e.g., positive/negative, present/absent) is foundational to clinical laboratory medicine [1]. Unlike quantitative tests, which report numerical values over a continuous range, qualitative tests classify samples into one of two distinct categories. The precision of these tests—the agreement between repeated measurements of the same sample—cannot be expressed by conventional statistics like the mean and standard deviation. Instead, precision is characterized by an imprecision interval, defined by the concentrations C5 and C95 [17]. This interval is a critical performance parameter, describing the inherent random error of a binary measurement process and the uncertainty in classifying a sample near its medical decision point.
This guide provides an in-depth technical exploration of designing precision studies and estimating the C5 to C95 imprecision interval, framed within the context of advanced research on the CLSI EP12-A2 protocol [18]. Although the EP12-A2 guideline has been superseded by a newer third edition, its foundational principles for precision evaluation remain highly relevant for scientists and drug development professionals designing robust validation studies for in vitro diagnostics [1] [18]. A thorough understanding of this protocol is essential for developing reliable tests, from rapid lateral flow assays to sophisticated PCR-based examinations.
Core Theoretical Concepts
The Imprecision Interval (C5 to C95)
For qualitative tests with an internal continuous response, a cutoff (CO) value is established to dichotomize the raw signal into a binary output. The C50 is the analyte concentration at which a test produces 50% positive and 50% negative results; it represents the medical decision level and often aligns with the test's stated cutoff [17]. However, due to analytical imprecision, there is not a single concentration that cleanly separates "positive" from "negative" results. Instead, there exists a range of concentrations around the C50 where the test result becomes probabilistic.
The imprecision interval quantifies this uncertainty:
- C5: The analyte concentration at which only 5% of test results are positive (and 95% are negative). This is the lower bound of the imprecision interval.
- C95: The analyte concentration at which 95% of test results are positive (and 5% are negative). This is the upper bound of the imprecision interval.
The range from C5 to C95 effectively captures the concentration band where the test result is uncertain. A narrower interval indicates a more precise and reliable test, while a wider interval signifies greater random error and more misclassification near the cutoff [17].
Relationship to Binary Data and Probability
The relationship between analyte concentration and the probability of a positive result is described by a cumulative distribution function, which produces an S-shaped curve [17]. This curve can be derived from the proportion of positive results observed at different analyte concentrations. The key idea is that random variation, or imprecision, in a binary measurement process can be fully characterized by this cumulative probability curve. The C5, C50, and C95 points are read directly from this curve, providing a complete description of the test's classification performance around its cutoff.
Table 1: Key Definitions for Imprecision Interval Estimation
| Term | Definition | Interpretation in Precision Evaluation |
|---|---|---|
| C5 | Analyte concentration yielding 5% positive results. | Concentration where a sample is almost always negative; lower limit of misclassification. |
| C50 | Analyte concentration yielding 50% positive results. | The medical decision level or cutoff; point of maximal uncertainty. |
| C95 | Analyte concentration yielding 95% positive results. | Concentration where a sample is almost always positive; upper limit of misclassification. |
| Imprecision Interval | The concentration range from C5 to C95. | Quantifies the "gray area" where result misclassification occurs; a narrower interval indicates better precision. |
| Binary Output | A test result with only two possible outcomes (e.g., Positive/Negative). | Prevents use of traditional mean/SD; requires estimation of proportions for precision studies. |
Experimental Design and Protocol
Designing a robust precision study according to CLSI EP12 principles requires careful planning of sample selection, replication, and data collection.
Sample Panel Preparation
The core of the precision experiment is a panel of samples with analyte concentrations spanning the expected imprecision interval, with a particular focus on concentrations near the C50.
- Target Concentrations: The study must include samples at the stated cutoff (C50) and at least two additional concentration levels: one between C5 and C50, and one between C50 and C95 [1] [17]. If the C5 and C95 values are unknown initially, a preliminary experiment using samples at 70%, 90%, 100%, 110%, and 130% of the cutoff can help bracket the interval.
- Sample Matrix: The sample matrix should mimic real patient specimens as closely as possible to ensure the results are clinically relevant.
- Replication: Each concentration level must be tested repeatedly to reliably estimate the proportion of positive results. CLSI EP12 recommends a minimum of 20 replicates per concentration level, though larger replication (e.g., 40 or 60) will provide a more precise estimate of the proportion [17].
Data Collection Workflow
The following diagram illustrates the logical workflow for conducting the precision experiment, from preparation to initial analysis.
Data Analysis and Estimation of C5 and C95
Fitting the Dose-Response Curve
The recorded data—consisting of concentrations and their corresponding observed proportions of positive results—must be fitted to a model to generate a smooth dose-response curve. The most common model used for this purpose is the logistic regression model (or probit model), which produces the characteristic S-shaped curve [17].
The logistic model is defined as: ( P(Positive) = \frac{1}{1 + e^{-(B0 + B1 \times \text{Concentration})}} ) where ( B0 ) and ( B1 ) are the intercept and slope parameters estimated from the data using statistical software.
Estimating C5, C50, and C95 from the Model
Once the logistic model is fitted, the C5, C50, and C95 concentrations are calculated by solving the model equation for the concentration (X) that yields probabilities (P) of 0.05, 0.50, and 0.95, respectively.
- C50 Calculation: Set ( P = 0.50 ). Since ( e^0 = 1 ), the equation simplifies to ( C50 = -B0 / B1 ).
- C5 and C95 Calculation: Set ( P = 0.05 ) and ( P = 0.95 ) respectively and solve for X. The general formula is: ( C = [ln(\frac{P}{1-P}) - B0] / B1 )
This analysis is typically performed with statistical software (e.g., R, SAS, Python) which can provide both the parameter estimates and confidence intervals for the estimated C5 and C95 points.
Table 2: Example Data and Results from a Simulated Precision Study
| Analyte Concentration | Number of Replicates | Number of Positive Results | Observed Proportion Positive |
|---|---|---|---|
| 0.8 × Cutoff | 40 | 3 | 0.075 |
| 0.9 × Cutoff | 40 | 12 | 0.300 |
| 1.0 × Cutoff (C50) | 40 | 21 | 0.525 |
| 1.1 × Cutoff | 40 | 32 | 0.800 |
| 1.2 × Cutoff | 40 | 37 | 0.925 |
| Calculated Parameter | Estimated Value | 95% Confidence Interval | |
| C5 | 0.82 × Cutoff | (0.78 - 0.86) × Cutoff | |
| C50 | 1.01 × Cutoff | (0.98 - 1.04) × Cutoff | |
| C95 | 1.20 × Cutoff | (1.16 - 1.24) × Cutoff | |
| Imprecision Interval | 0.38 × Cutoff |
The Scientist's Toolkit: Essential Research Reagents and Materials
The following reagents and materials are critical for executing a precision study according to CLSI EP12.
Table 3: Key Research Reagent Solutions for Precision Studies
| Reagent / Material | Function in the Precision Study |
|---|---|
| Characterized Panel of Samples | A set of samples with analyte concentrations spanning the C50. Used to challenge the test across its imprecision interval. |
| Negative Control (Blank) Matrix | The sample matrix without the target analyte. Essential for establishing the baseline response and for use in preparation of diluted samples. |
| Positive Control Material | A material with a known, high concentration of the analyte. Used to create the dilution series for the precision panel. |
| Stable Reference Material | A well-characterized control material used for long-term monitoring of the C50 and imprecision interval, ensuring consistency across multiple experiment runs. |
| Interference Substances | While primarily for specificity studies, these are used in related experiments to assess the robustness of the C50 against common interferents like lipids or hemoglobin [1] [17]. |
| GPhos Pd G6 | GPhos Pd G6, MF:C47H70BrO4PPdSi, MW:944.4 g/mol |
| Cholesteryl 11(Z)-Vaccenate | Cholesteryl 11(Z)-Vaccenate, MF:C45H78O2, MW:651.1 g/mol |
Integration with Broader Test Performance Validation
Estimating the imprecision interval is not an isolated activity; it is a core component of a comprehensive test validation strategy as outlined in CLSI EP12. The findings from the precision study directly inform other critical validation phases.
- Clinical Agreement Studies: The estimated C5 and C95 values help explain the test's performance at the "clinical gray zone," providing context for observed false positives and false negatives in method comparison studies [19] [17]. A sample with an analyte concentration near the C95, for instance, might be a true positive that is occasionally misclassified, impacting clinical sensitivity.
- Analytical Specificity (Interference) Studies: The precision interval should be re-evaluated in the presence of potential interferents. A stable C50 in the presence of interferents indicates a robust method, whereas a significant shift suggests vulnerability to interference [1] [17].
- Setting Quality Control Rules: Understanding the width of the imprecision interval is vital for designing a statistically sound QC plan. Laboratories can use this information to select appropriate QC concentrations and establish Westgard rules that effectively monitor for significant shifts in the test's calibration (C50) or precision (C5-C95 width) [17].
Designing rigorous precision studies and accurately estimating the C5 to C95 imprecision interval are fundamental to establishing the reliability of any qualitative, binary-output examination. The CLSI EP12-A2 protocol provides a structured, statistically sound framework for this process, guiding researchers through sample preparation, replicate testing, and sophisticated data analysis to quantify the "gray zone" of a test. In an era of rapidly evolving diagnostic technologies, from point-of-care tests to high-throughput automated systems, mastering these principles is indispensable for scientists and developers committed to delivering accurate and trustworthy diagnostic tools that support optimal patient care.
Clinical agreement studies are fundamental to the validation and verification of qualitative laboratory tests, which yield binary outcomes such as positive/negative or present/absent. These studies assess the degree to which a new candidate test method agrees with an established comparative method. Within the framework of the CLSI EP12-A2 protocol—the "User Protocol for Evaluation of Qualitative Test Performance"—this process provides a consistent approach for protocol design and data analysis for both precision and method-comparison studies [20]. The fundamental goal is to determine if the candidate test's performance is acceptable for its intended clinical use.
It is critical to distinguish between diagnostic accuracy and test agreement. Diagnostic accuracy, characterized by sensitivity and specificity, can only be calculated when the true disease status of the subject is known, typically verified by a reference standard which is the best available method for establishing the presence or absence of the target condition [21] [22]. In contrast, many real-world method comparisons lack a perfect reference standard. Instead, a comparative method, which may be another laboratory test, is used. In these cases, the statistics calculated are Positive Percent Agreement (PPA) and Negative Percent Agreement (PNA), which estimate the agreement between the two methods rather than absolute accuracy [21]. Using the terms "sensitivity" and "specificity" when a non-reference standard is used is a misnomer and can lead to misinterpretation [21] [22].
Core Statistical Definitions and Calculations
The data from a clinical agreement study is organized in a 2x2 contingency table (also known as a "truth table"), which cross-tabulates the results from the candidate and comparative methods [23].
The 2x2 Contingency Table
The structure of this table is as follows:
Table 1: Structure of a 2x2 Contingency Table for Clinical Agreement Studies
| Candidate Method | Comparative Method: Positive | Comparative Method: Negative | Total |
|---|---|---|---|
| Positive | a (True Positives) | b (False Positives) | a + b |
| Negative | c (False Negatives) | d (True Negatives) | c + d |
| Total | a + c | b + d | n (Total Samples) |
Legend: This table summarizes the agreement between a candidate method and a comparative method. Cells 'a' and 'd' represent agreements, while cells 'b' and 'c' represent disagreements [23].
Key Performance Statistics
From this table, the three primary statistics for assessing agreement are calculated.
Table 2: Key Agreement Statistics and Their Formulae
| Statistic | Synonym (if Ref. Std.) | Formula | Interpretation |
|---|---|---|---|
| Positive Percent Agreement (PPA) | Sensitivity (if Ref. Std.) | [a/(a+c)] * 100 |
The proportion of comparative method-positive results that the candidate method correctly identifies as positive [23]. |
| Negative Percent Agreement (PNA) | Specificity (if Ref. Std.) | [d/(b+d)] * 100 |
The proportion of comparative method-negative results that the candidate method correctly identifies as negative [23]. |
| Percent Overall Agreement (POA) | Efficiency (if Ref. Std.) | [(a+d)/n] * 100 |
The overall proportion of samples where the two methods agree [23]. |
It is essential to recognize that PPA and PNA are asymmetric measures. Their values depend on which test is designated as the candidate and which as the comparative method. Interchanging the two methods will change the calculated statistics [21]. Furthermore, while the formulas for PPA and PNA are identical to those for sensitivity and specificity, their interpretation is different and hinges on the nature of the comparative method [21].
The following workflow diagram illustrates the logical sequence for designing the study, organizing the data, and calculating the key agreement metrics.
Diagram 1: Workflow for a Clinical Agreement Study
Confidence Intervals
Point estimates for PPA, PNA, and POA are more meaningful when accompanied by their 95% confidence intervals (CI), which convey the reliability and precision of the estimate [23]. Wider confidence intervals indicate less precise estimates, which is common with smaller sample sizes. The formulas for calculating these intervals, as recommended in CLSI EP12-A2, are provided below [23].
Calculations for confidence limits for PPA:
- Q1 = 2a + 3.84
- Q2 = 1.96 * √[3.84 + (4ac/(a+c))]
- Q3 = 2(a+c) + 7.68
- PPA Lower Limit = 100 * (Q1 - Q2) / Q3
- PPA Upper Limit = 100 * (Q1 + Q2) / Q3
Calculations for confidence limits for PNA:
- Q4 = 2d + 3.84
- Q5 = 1.96 * √[3.84 + (4bd/(b+d))]
- Q6 = 2(b+d) + 7.68
- PNA Lower Limit = 100 * (Q4 - Q5) / Q6
- PNA Upper Limit = 100 * (Q4 + Q5) / Q6
Calculations for confidence limits for POA:
- Q7 = 2(a+d) + 3.84
- Q8 = 1.96 * √[3.84 + (4(a+d)(b+c)/n)]
- Q9 = 2n + 7.68
- POA Lower Limit = 100 * (Q7 - Q8) / Q9
- POA Upper Limit = 100 * (Q7 + Q8) / Q9
Experimental Protocols and Study Design
Adhering to a structured protocol is essential for generating reliable and defensible data. The following section outlines key methodological considerations based on regulatory guidance and CLSI recommendations.
Sample Selection and Size
For a robust agreement study, samples should be selected to challenge the test across its intended range. The U.S. Food and Drug Administration (FDA) often recommends a minimum of 30 reactive and 30 non-reactive specimens [23]. The reactive specimens should include a mix of concentrations: for instance, 20 low-reactive samples (with analyte concentrations 1 to 2 times the test's Limit of Detection) and 10 higher-reactive samples that span the testing range [23]. This approach ensures the test is evaluated at its clinical decision point and across potentially challenging scenarios. Using contrived clinical specimens (e.g., samples spiked with inactive control material) is an acceptable practice to achieve these targets [23].
The Comparative Method
The choice of a comparative method is a critical decision. In an ideal scenario, this would be a reference standard with proven diagnostic accuracy. However, in practice, it is often another established test method, which could be a previously authorized test or one used by a reference laboratory [21] [23]. It is vital to understand that when a non-reference standard is used, the resulting PPA and PNA are measures of agreement, not true sensitivity and specificity. Disagreements between the two methods do not, by themselves, indicate which test is correct; further investigation is required to resolve such discrepancies [21].
Interpreting Results and Limitations
The Percent Overall Agreement (POA) can be misleadingly high if the prevalence of the condition in the sample population is skewed. A test can achieve a high POA simply by correctly identifying the dominant class (e.g., negatives in a low-prevalence population), even if its performance for the other class (positives) is poor [23]. Therefore, the primary metrics for judging acceptability should be PPA and PNA, not POA. The 95% confidence intervals for PPA and PNA must also be considered. For a study with 30 positive and 30 negative samples, even a perfect 100% agreement will have a lower confidence limit of approximately 89%. A single false positive or false negative in such a study will lower this limit further, underscoring the need for adequate sample sizes [23].
The Scientist's Toolkit: Essential Research Reagents and Materials
Executing a valid clinical agreement study requires careful selection and preparation of materials. The following table details key reagents and their functions.
Table 3: Essential Materials for a Clinical Agreement Study
| Item | Function & Specification |
|---|---|
| Clinical Specimens | Well-characterized patient samples used for the method comparison. These should be representative of the test's intended use and stored under appropriate conditions to preserve analyte stability [23]. |
| Contrived Samples | Artificially created samples, for example by spiking a known negative matrix with a high-level control material. These are vital when a sufficient number of native positive clinical samples is unavailable [23]. |
| Reference/Comparative Method | The established test against which the candidate method is compared. This could be an FDA-authorized test, a method used by a reference lab, or a recognized gold standard [23]. |
| Positive & Negative Controls | Quality control samples with known status (reactive and non-reactive) that are analyzed with each run of patient samples to monitor the test's performance and ensure it is working correctly [23]. |
| Candidate Method Reagents | All proprietary reagents, calibrators, and consumables required to perform the new test according to the manufacturer's instructions. |
| 2,3,5-Trimethylpyrazine-D10 | 2,3,5-Trimethylpyrazine-D10, MF:C7H10N2, MW:132.23 g/mol |
| Saroglitazar sulfoxide-d4 | Saroglitazar sulfoxide-d4, MF:C25H29NO5S, MW:459.6 g/mol |
Data Analysis and Interpretation: A Worked Example
Consider the following example data from the CLSI EP12-A2 document [23]:
Table 4: Example Data from a Clinical Agreement Study
| Candidate Method | Comparative Method: Positive | Comparative Method: Negative | Total |
|---|---|---|---|
| Positive | a = 285 | b = 15 | 300 |
| Negative | c = 14 | d = 222 | 236 |
| Total | 299 | 237 | n = 536 |
Using the formulas provided earlier:
- PPA = [285 / (285 + 14)] * 100 = 95.3%
- PNA = [222 / (15 + 222)] * 100 = 93.7%
- POA = [(285 + 222) / 536] * 100 = 94.6%
The 95% confidence intervals for these estimates are:
- PPA: 92.3% - 97.2%
- PNA: 89.8% - 96.1%
- POA: 92.3% - 96.2%
This data can be interpreted as follows: The candidate test shows strong positive (95.3%) and negative (93.7%) agreement with the comparative method. The confidence intervals are reasonably narrow, providing confidence in the reliability of these estimates. The lower confidence limit for PPA is 92.3% and for PNA is 89.8%. A laboratory would compare these values, particularly the lower confidence limits, to its pre-defined acceptability criteria to decide whether to implement the new test. The relationship between the point estimate and its confidence interval is visualized in the following diagram.
Diagram 2: Interpreting Point Estimates and Confidence Intervals
Conducting a rigorous clinical agreement study is a multi-stage process that requires meticulous planning, execution, and analysis. Framing this process within the CLSI EP12-A2 protocol ensures a consistent and statistically sound approach. The core of the analysis lies in the correct use of the 2x2 contingency table to calculate Positive Percent Agreement and Negative Percent Agreement, with careful attention to their associated confidence intervals. Researchers must remember that these statistics measure agreement with a comparative method and should only be interpreted as sensitivity and specificity when a true reference standard is used. By following the detailed methodologies for sample selection, data analysis, and interpretation outlined in this guide, scientists and drug development professionals can robustly validate qualitative tests, ensuring their reliability and fitness for purpose in clinical decision-making.
Protocols for Stability Testing and Interference Assessment
The Clinical and Laboratory Standards Institute (CLSI) guideline EP12 provides a critical framework for evaluating the performance of qualitative, binary output examinations in clinical laboratories and in vitro diagnostic (IVD) development [1] [2]. These tests produce simple yes/no, positive/negative, or present/absent results that inform critical medical decisions. Unlike quantitative assays, qualitative tests require specialized validation protocols to ensure reliable performance in real-world conditions.
The third edition of CLSI EP12, published in March 2023, represents a significant evolution from the previous EP12-A2 version [2]. This updated guideline expands the types of procedures covered to reflect advances in laboratory medicine and adds comprehensive protocols for stability testing and interference assessment alongside established precision and clinical performance evaluation [1]. These protocols are intended for both manufacturers developing commercial tests and laboratories creating laboratory-developed tests (LDTs), providing a standardized approach for verification in local testing environments [1] [2].
This technical guide focuses specifically on the methodologies for stability testing and interference assessment within the CLSI EP12 framework, providing researchers and drug development professionals with detailed experimental protocols and analytical approaches essential for comprehensive test validation.
Stability Testing Protocols
Objectives and Scope
Stability testing evaluates how environmental factors and time affect the performance of qualitative examinations. Proper stability assessment ensures that tests maintain their claimed performance characteristics throughout their shelf life and under various storage conditions. According to CLSI EP12, stability evaluation covers multiple aspects including reagent stability, sample stability, and calibrator stability [1].
The fundamental objective is to determine the boundaries within which the test continues to perform as intended, identifying critical control points that may affect clinical decision-making. For binary output tests, this specifically means maintaining consistent cut-off values and discrimination power between positive and negative results over time and across defined storage conditions.
Experimental Design and Methodologies
A well-designed stability study incorporates controlled challenge conditions with statistical rigor to establish expiration dating and storage requirements. The following table summarizes the core stability study types:
Table 1: Stability Testing Protocols for Qualitative Examinations
| Study Type | Experimental Approach | Key Parameters Measured | Acceptance Criteria |
|---|---|---|---|
| Real-time Stability | Testing under actual recommended storage conditions at predetermined timepoints | Agreement with reference method, C5/C95 limits | Sensitivity/specificity maintained within predefined limits |
| Accelerated Stability | Exposure to elevated stress conditions (temperature, humidity) | Rate of performance degradation | Extrapolated shelf life meets minimum requirements |
| In-use Stability | Testing after opening/ reconstitution over defined period | Performance at scheduled intervals | Maintained performance throughout claimed in-use period |
| Freeze-thaw Stability | Multiple cycles of freezing and thawing | Signal strength, cut-off drift | Tolerance to expected handling variations |
The experimental workflow begins with establishing a baseline performance using fresh reagents and samples, then monitoring deviations under challenge conditions:
For tests with continuous response variables (such as immunoassays), CLSI EP12 recommends estimating the C5 and C95 limits - the analyte concentrations yielding positive results in 5% and 95% of replicates, respectively [1]. Monitoring the drift of these critical decision points over time provides a quantitative assessment of stability. The experimental design should include sufficient replicates at each timepoint to achieve statistical power, typically 20-40 replicates per level for binary output tests.
Data Analysis and Interpretation
Statistical analysis of stability data focuses on detecting significant changes in clinical performance (sensitivity and specificity) and analytical performance (C5/C95 limits for tests with continuous response). The "stability endpoint" is defined as the point where performance falls below predetermined acceptance criteria, which should be based on clinical requirements rather than statistical significance alone.
For accelerated stability studies, the Arrhenius model is commonly employed to predict shelf life at recommended storage temperatures based on degradation rates at elevated temperatures. This approach allows for preliminary shelf-life estimation without conducting full real-time studies, though final expiration dating should be verified with real-time data.
Interference Assessment Protocols
Fundamentals of Interference Testing
Interference assessment systematically evaluates how substances commonly encountered in clinical samples affect qualitative test performance. Interferents can include endogenous substances (hemoglobin, bilirubin, lipids, proteins), medications (prescription and over-the-counter drugs), and sample matrix components that might cause false positive or false negative results [1].
CLSI EP12 categorizes interference studies into two primary approaches: (1) testing specific suspected interferents at pathological concentrations, and (2) testing a broad panel of potentially interfering substances representative of the patient population. The selection of interferents should be based on the test's intended use, the sample matrix, and likely concomitant medications or conditions.
Experimental Methodologies
Interference testing follows a structured protocol comparing test performance with and without potential interferents:
Table 2: Interference Testing Protocol for Qualitative Examinations
| Protocol Component | Methodological Details | Quality Control Measures |
|---|---|---|
| Sample Preparation | Spiking candidate interferents into patient samples | Use of appropriate solvents with vehicle controls |
| Concentration Levels | Testing at clinically relevant concentrations | Inclusion of supratherapeutic levels for drugs |
| Sample Panels | Positive samples near cut-off, negative samples near cut-off | Minimum 3-5 replicates per condition |
| Interferent Selection | Common medications, endogenous substances, metabolites | Based on literature review and intended use |
| Statistical Analysis | Proportion agreement, Cohen's kappa, confidence intervals | Predefined acceptance criteria for clinical agreement |
The core experimental workflow for interference assessment involves careful sample preparation and comparative analysis:
A critical consideration in interference study design is selecting appropriate sample concentrations. CLSI EP12 recommends testing samples with analyte concentrations near the clinical decision point (cut-off), as these are most vulnerable to interference effects. This includes both positive samples near the cut-off and negative samples near the cut-off to detect both false-negative and false-positive interference, respectively.
Data Analysis and Clinical Interpretation
For binary output tests, interference data is typically analyzed using proportion agreement statistics between interferent-containing samples and controls. The Cohen's kappa statistic provides a measure of chance-corrected agreement, with values below acceptable thresholds indicating significant interference.
When analyzing results, researchers should calculate confidence intervals for sensitivity and specificity estimates to understand the precision of interference assessments. The 95% confidence interval for proportion of agreement should remain within predefined clinical acceptability limits. For tests with continuous response variables, statistical comparison of C5 and C95 values between test and control groups can provide more sensitive detection of interference effects.
The Researcher's Toolkit: Essential Materials and Reagents
Successful execution of stability and interference studies requires carefully selected materials and controls. The following table outlines key research reagent solutions and their applications in EP12-compliant studies:
Table 3: Essential Research Reagents for Stability and Interference Assessment
| Reagent Category | Specific Examples | Application in Protocols |
|---|---|---|
| Reference Materials | WHO International Standards, CRM | Establishing baseline performance and method comparison |
| Quality Controls | Positive, negative, and cut-off level controls | Monitoring assay performance throughout studies |
| Interference Stocks | Hemolysate, bilirubin, lipid emulsions, common medications | Simulating specific interference conditions |
| Matrix Components | Human serum, plasma, urine, swab extracts | Maintaining clinical relevance in sample preparation |
| Stability Materials | Lyophilized reagents, ready-to-use formulations | Testing across different presentation formats |
| Calibrators | Manufacturer's calibrators with assigned values | Monitoring drift in quantitative readouts |
| Cyanine3 hydrazide dichloride | Cyanine3 hydrazide dichloride, MF:C30H40Cl2N4O, MW:543.6 g/mol | Chemical Reagent |
| 4',7-Dimethoxyisoflavone-d6 | 4',7-Dimethoxyisoflavone-d6, MF:C17H14O4, MW:288.33 g/mol | Chemical Reagent |
Stability and interference protocols do not exist in isolation but must be integrated into a comprehensive test validation strategy. CLSI EP12 emphasizes the connection between these assessments and other performance characteristics including precision (imprecision near cut-off), clinical sensitivity, and clinical specificity [1].
The experimental data generated from stability and interference studies directly informs critical aspects of test implementation:
- Product labeling requirements including storage conditions, stability claims, and known interference limitations
- Laboratory standard operating procedures for sample acceptance and handling
- Quality control strategies for ongoing monitoring of test performance
- Troubleshooting guides for investigating aberrant results
For manufacturers, these studies provide essential data for regulatory submissions to bodies like the U.S. Food and Drug Administration, which has recognized CLSI EP12 as satisfying regulatory requirements [1]. For laboratories, properly executed verification of stability and interference claims ensures compliance with accreditation standards such as CAP, ISO 15189, and ISO 17025 [6].
Advancements in EP12 3rd Edition
The recently published third edition of CLSI EP12 introduces several important enhancements relevant to stability and interference assessment [2]. These include:
- Expanded scope covering emerging technologies such as next-generation sequencing and complex molecular assays
- Supplemental information on determining lower limit of detection for qualitative PCR-based examinations
- Enhanced protocols for observer precision studies relevant to tests with visual readouts
- Detailed guidance on reagent stability evaluation across different presentation formats
These updates reflect the evolving landscape of qualitative testing in modern laboratory medicine, particularly the increasing complexity of binary output examinations ranging from simple lateral flow tests to advanced nucleic acid detection systems [2].
By implementing the structured protocols outlined in this guide, researchers and drug development professionals can ensure their qualitative tests deliver reliable, clinically actionable results across the intended shelf life and in diverse patient populations with varying potential interferents.
The CLSI EP12-A2 guideline provides a critical framework for evaluating the performance of qualitative examinations that produce binary results, such as positive/negative or present/absent [1] [24]. This technical guide explores the application of EP12-A2 principles across three distinct test types: tests with an internal continuous response (ICR), tests with binary-only outputs, and PCR-based methods (including quantitative, digital, and real-time PCR). For researchers, scientists, and drug development professionals, understanding these nuanced applications is essential for designing robust validation protocols, ensuring regulatory compliance, and generating reliable data for clinical or research decisions.
The performance assessment of qualitative tests in medical laboratories has traditionally focused on metrics like clinical sensitivity and specificity [24]. EP12-A2 expands this view by incorporating protocols for characterizing the "imprecision curve" or "imprecision interval" that describes the uncertainty of classification for binary results [25]. This guide bridges the theoretical framework of EP12-A2 with practical experimental methodologies for different technological platforms, providing detailed protocols, data analysis techniques, and implementation considerations specific to each test type.
Test Type Fundamentals and EP12-A2 Framework
Core Principles of CLSI EP12-A2
EP12-A2, titled "Evaluation of Qualitative, Binary Output Examination Performance," establishes standardized protocols for evaluating tests with only two possible outputs [1]. The guideline addresses performance evaluations for imprecision (including C5 and C95 estimation), clinical performance (sensitivity and specificity), stability, and interference testing [1]. The recent third edition of this guideline (EP12Ed3) expands the types of procedures covered to reflect advances in laboratory medicine and adds protocols for use during examination procedure design, validation, and verification [1].
A fundamental concept in EP12-A2 is the recognition that binary classification often depends on a cutoff (CO) value, which might be set at the limit of detection (LoD) to maximize clinical sensitivity or higher to maximize clinical specificity [25]. The validation of this cutoff is therefore critical for characterizing overall test performance. The guideline acknowledges that different test technologies require tailored approaches for this validation, particularly distinguishing between tests that provide an internal continuous response versus those that generate only binary outputs.
Alignment with Broader Quality Standards
The EP12-A2 framework demonstrates consistency with international standards, particularly ISO 15189 requirements for medical laboratory quality management [24]. This alignment ensures that laboratories implementing EP12-A2 protocols simultaneously satisfy broader accreditation requirements. Additionally, the Eurachem/CITAC guide "Assessment of Performance and Uncertainty in Qualitative Chemical Analysis" complements EP12-A2 by introducing "uncertainty of proportion" concepts, reflecting the growing need to assess uncertainties for qualitative results [24].
Table: Key Standards and Guidelines for Qualitative Test Performance
| Standard/Guideline | Focus Area | Relevance to Binary Tests |
|---|---|---|
| CLSI EP12-A2 | Evaluation of qualitative, binary output examinations | Primary framework for imprecision, clinical sensitivity/specificity assessment |
| ISO 15189 | Medical laboratory quality management | General competence requirements for laboratories |
| Eurachem/CITAC AQA 2021 | Performance and uncertainty in qualitative chemical analysis | Uncertainty assessment for qualitative results, including proportion uncertainty |
Internal Continuous Response (ICR) Tests
Tests with an internal continuous response (ICR) generate an initial quantitative signal that is subsequently interpreted against a cutoff value to produce a final binary result [25]. A common example includes ELISA immunoassays, where the continuous optical density measurement is compared to a predetermined cutoff to determine positivity [25]. This continuous underlying signal provides rich data for performance characterization beyond mere binary classification.
The key advantage of ICR tests lies in the ability to directly visualize and quantify the analytical variation around the cutoff value. This enables more sophisticated performance characterization and optimization compared to binary-only tests. The continuous response can be analyzed using statistical methods typically applied to quantitative assays, while the final output aligns with qualitative performance requirements outlined in EP12-A2.
Performance Characterization and Experimental Protocol
For ICR tests, EP12-A2 describes a replication experiment for characterizing the "imprecision curve" or "imprecision interval" that describes the uncertainty of classification for binary results [25]. The experimental approach involves:
- Sample Preparation: Prepare a panel of samples with concentrations spanning the expected cutoff value. Include at least 5-7 different concentration levels with appropriate replication at each level (typically 20-100 replicates per concentration).
- Data Collection: Analyze all samples using the ICR test protocol, recording both the continuous response values and the final binary classification.
- Data Analysis: Calculate the proportion of positive results at each concentration level and plot these proportions against concentration to generate an imprecision curve.
Table: Key Parameters for ICR Test Characterization
| Parameter | Definition | Interpretation | Experimental Requirement |
|---|---|---|---|
| C50 | Concentration where 50% of measurements are positive | Cutoff concentration | Determined from imprecision curve |
| C5 | Concentration where 5% of measurements are positive | Lower imprecision limit | Requires testing below C50 |
| C95 | Concentration where 95% of measurements are positive | Upper imprecision limit | Requires testing above C50 |
| Imprecision Interval | Range between C5 and C95 | Region of classification uncertainty | Width indicates performance robustness |
The resulting data can be fitted to a cumulative probability distribution function, typically sigmoidal in shape. The limit of detection (LoD) for ICR tests can be determined using quantitative approaches, analyzing a blank sample with 20 replicates to calculate the Limit of Blank (LoB = Meanblk + 1.65 SDblk), followed by 20 replicates of a low positive sample to calculate LoD (LoD = LoB + 1.65 SD_pos) [25].
Binary-Only Output Tests
Binary-only output tests provide only categorical results without an underlying continuous signal [25]. Examples include simple lateral flow devices and other tests where visual interpretation leads directly to classification without intermediate quantitative values [25]. The absence of a continuous response presents unique challenges for performance characterization under EP12-A2, requiring alternative experimental approaches.
For these tests, the traditional quantitative approach to determining LoD cannot be applied because there is no variation for a blank solution—only a zero result is obtained [25]. Instead of estimating mean and standard deviation parameters, performance characterization relies entirely on replication experiments at different concentrations to determine positive proportions, positivity rates, detection rates, or "hit rates" [25].
Probit Analysis for Performance Characterization
Probit analysis serves as the primary statistical method for characterizing binary-only tests [25]. This technique, with roots in agricultural bioassays from the 1940s, converts observed proportions ("hit rates") to "probability units" (probits) related to standard deviations in a normal distribution [25]. The experimental protocol involves:
- Sample Preparation: Prepare samples at 3-5 concentrations near the expected cutoff. Include sufficient replicates at each concentration (minimum 20, preferably more).
- Testing and Data Collection: Test all replicates and record the binary results (positive/negative) for each.
- Probit Conversion: Convert the proportion of positive results at each concentration to probits using the formula: Probit = 5 + NORMSINV(P), where P is the proportion of positive results.
- Regression Analysis: Perform linear regression of probits against log-transformed concentration values.
- Parameter Estimation: Calculate C95 (LoD) from the regression equation using a probit value of 6.64.
EP17-A2 recommends a minimum of 3 data points between C10 and C90, one close to C95, and another outside the C5 to C95 range [25]. The limited number of data points is a practical constraint in many studies, making appropriate experimental design critical for obtaining reliable results.
Real-World Application Example
A multicenter study of the Cepheid Xpert Xpress SARS-CoV-2 test demonstrates probit analysis application for a binary-output NAAT test [25]. Researchers diluted SARS-CoV-2 virus in negative clinical matrix to 7 different levels near the estimated LoD, testing a minimum of 22 replicates at each level [25]. Probit regression analysis estimated the LoD at 0.005 PFU/mL, which was verified by a 100% hit rate (22/22 replicates) at the next highest concentration (0.01 PFU/mL) [25].
PCR-Based Methods
PCR-based methods, including real-time PCR (qPCR) and digital PCR (dPCR), represent a special category in binary test performance characterization. While these technologies often generate quantitative data, their applications in clinical diagnostics frequently involve binary classification (e.g., detected/not detected, mutant/wild-type). The global qPCR and dPCR market, estimated at $5 billion in 2025 with a projected CAGR of 7-8% through 2033, reflects the growing importance of these technologies [26].
The distinction between qPCR and dPCR is important in performance characterization. qPCR relies on amplification curves and threshold cycles (Ct) for quantification, while dPCR uses partitioning and Poisson statistics to enable absolute quantification without standard curves [27]. For binary classification, dPCR directly assesses the presence/absence of target molecules in partitions, making its binary nature fundamental rather than derived [27].
Statistical Methods for Comparison
A critical application of EP12-A2 principles to PCR methods involves comparing results across multiple experiments. Two novel statistical methods have been developed specifically for this purpose:
- Generalized Linear Models (GLM): Binomial regression models that explain binomially distributed response (positive partitions) using linear combinations of parameters (experiment names). The model employs a quasibinomial distribution to account for excessive zeros and uses the logarithm function to estimate mean copies per partition (λ) [27].
- Multiple Ratio Tests (MRT): Based on uniformly most powerful (UMP) ratio tests with null hypothesis H0: λ1/λ2 = 1, where λ1 and λ2 are mean template molecules per partition in two experiments [27]. This approach uses Wilson's confidence intervals with Dunn-Šidák correction for multiple comparisons [27].
Table: Comparison of Statistical Methods for Multiple dPCR Experiments
| Method | Statistical Basis | Key Features | Performance Characteristics |
|---|---|---|---|
| Generalized Linear Models (GLM) | Binomial regression with quasibinomial distribution | Can be refined by adding effects like technical replication; single-step procedure controlling familywise error | More sensitive to changes in template concentration; performance depends on number of runs |
| Multiple Ratio Tests (MRT) | Uniformly most powerful ratio test with multiple testing correction | Uses Wilson confidence intervals with Dunn-Šidák correction; faster and more robust for large-scale experiments | Less sensitive than GLM to concentration changes; more robust for large experiment series |
Evaluation of these methods through Monte Carlo simulation (over 2 million in silico dPCR runs) revealed that both have 'blind spots' where they cannot distinguish runs containing different template molecule numbers [27]. These limitations widen with increasing λ values, highlighting the importance of understanding methodological constraints when designing PCR experiments and interpreting results.
Experimental Considerations for PCR Methods
Implementing EP12-A2 principles for PCR methods requires specific experimental adaptations:
- Partitioning Considerations: For dPCR, the number and volume of partitions significantly impact performance parameters [27]. The essential information is the estimated mean copy per partition (λ), calculated as λ = -ln(1 - k/n), where k is positive partitions and n is total partitions [27].
- Multiplex Applications: The trend toward multiplexing in PCR enables simultaneous detection of multiple targets, enhancing efficiency and reducing costs [28]. This requires careful consideration of cutoff determination for each target.
- Limit of Detection Studies: For NAAT tests like PCR, the traditional blank measurement approach cannot be applied because there is no variation for a zero concentration [25]. Instead, probit analysis of hit rates at different concentrations characterizes the imprecision interval.
Research Reagent Solutions
Table: Essential Research Reagents for Qualitative Test Validation
| Reagent/Category | Function in Validation | Test Type Application |
|---|---|---|
| Panel of Positive Samples | Characterize detection rates across concentrations | All types (ICR, Binary, PCR) |
| Clinical Negative Matrix | Establish specificity, test interference | All types (ICR, Binary, PCR) |
| Reference Standards | Assign target concentrations to samples | All types (ICR, Binary, PCR) |
| Master Mixes & Amplification Reagents | Support nucleic acid amplification | PCR methods (qPCR, dPCR) |
| Enzymes & Substrates | Generate detectable signals in ICR tests | ICR tests (e.g., ELISA) |
| Stable Diluents | Prepare concentration gradients for probit studies | All types, especially binary-only |
| Quality Control Materials | Monitor assay performance over time | All types (ICR, Binary, PCR) |
The application of CLSI EP12-A2 principles across ICR, binary-only, and PCR test types demonstrates both unifying concepts and technology-specific adaptations. For all test types, rigorous determination of the imprecision interval around the cutoff and comprehensive characterization of clinical sensitivity and specificity remain fundamental requirements. However, the experimental approaches and statistical tools must be tailored to each technology's characteristics—leveraging continuous response data for ICR tests, implementing probit analysis for binary-only tests, and applying specialized statistical methods like GLM and MRT for PCR comparison studies.
The continuing evolution of test technologies, including trends toward multiplexing, automation, and point-of-care applications, will likely drive further refinement of EP12-A2 application protocols [28] [26]. Furthermore, the integration of artificial intelligence and machine learning tools in data analysis may enhance the interpretation capabilities of these platforms [26]. For researchers and drug development professionals, maintaining awareness of both the foundational EP12-A2 principles and their specific application to different test technologies is essential for generating robust, reliable performance data that supports accurate clinical or research decisions.
The Clinical and Laboratory Standards Institute (CLSI) EP12-A2 protocol provides a standardized framework for evaluating the performance of qualitative medical tests that yield binary outcomes (e.g., positive/negative, reactive/nonreactive). This guideline establishes rigorous methodologies for assessing critical performance metrics including diagnostic sensitivity, specificity, positive and negative predictive values, and the precision of qualitative examinations [1] [29]. For cervical cancer screening programs, which rely heavily on the Papanicolaou (Pap) test, applying a structured evaluation protocol is essential for ensuring reliable patient results. The EP12-A2 guideline offers a consistent approach for protocol design and data analysis, enabling laboratories to verify that their qualitative tests perform to the required standards [29]. This case study demonstrates the practical application of the EP12-A2 protocol to evaluate the performance of the Pap test within a Peruvian tertiary care hospital setting, providing a model for systematic quality assessment in cervical cytology.
Pap Test Performance Analysis Using EP12-A2
A 2023 prospective study conducted at the Hospital Nacional Docente Madre Niño San Bartolomé in Lima, Peru, utilized the CLSI EP12-A2 guideline to evaluate the quality and diagnostic performance of Pap test cytology against histopathological confirmation [19] [30]. The study analyzed 156 paired cytological and histological results, with samples processed using automated staining systems and interpreted according to the 2014 Bethesda system for cytology and the FIGO 2015 nomenclature for histopathology [19]. This methodological approach allowed researchers to calculate key performance indicators and assess the overall effectiveness of the cervical cancer screening test in a real-world clinical setting.
Performance Metrics and Statistical Analysis
The evaluation followed the EP12-A2 framework for calculating diagnostic performance metrics through contingency tables, determining sensitivity, specificity, predictive values, and likelihood ratios with 95% confidence intervals [19]. Researchers employed Cohen's weighted Kappa test to measure cyto-histological agreement and used Bayesian analysis to estimate post-test probabilities, providing a comprehensive statistical assessment of test performance [19] [30]. The study specifically addressed the challenge of indeterminate cytological results (such as ASCUS, ASC-H, and AGUS) by correlating them with histological findings to determine rates of overdiagnosis and underdiagnosis, a critical aspect of quality assurance in cervical cytology [19].
Table 1: Overall Diagnostic Performance of Pap Test Based on EP12-A2 Evaluation
| Performance Metric | Value (%) | 95% Confidence Interval |
|---|---|---|
| Sensitivity | 94.0 | 83.8 - 97.9 |
| Specificity | 74.6 | 66.6 - 81.2 |
| Positive Predictive Value (PPV) | 58.0 | 47.2 - 68.2 |
| Negative Predictive Value (NPV) | 97.1 | 91.8 - 99.0 |
| Cyto-histological Agreement (κ) | 0.57 (Moderate) | - |
Table 2: Distribution of Cyto-Histological Findings in the Study Cohort (n=156)
| Cytological Findings | Frequency n (%) | Corresponding Histological Findings | Frequency n (%) |
|---|---|---|---|
| Undetermined Abnormalities | 57 (36.5) | CIN 1 | 56 (35.9) |
| • ASCUS | 35 (22.4) | • With HPV pathognomony | 45 (28.8) |
| • ASC-H | 19 (12.2) | CIN 2 | 23 (14.7) |
| • AGUS | 3 (1.9) | CIN 3 | 23 (14.7) |
| LSIL | 34 (21.8) | Carcinoma in situ | 6 (3.8) |
| • With HPV changes | 10 (6.4) | Squamous Carcinoma | 7 (4.5) |
| HSIL | 42 (26.9) | Adenocarcinoma | 1 (0.6) |
| • With HPV changes | 7 (4.5) | HPV Changes Only | 15 (9.6) |
| Carcinoma | 7 (4.5) |
Key Findings and Clinical Implications
The EP12-A2 evaluation revealed that the Pap test demonstrated high sensitivity (94%) but only moderate specificity (74.6%) in detecting cervical abnormalities, with a strong negative predictive value (97.1%) that supports its role as an effective screening tool for ruling out disease [19]. The moderate cyto-histological agreement (κ=0.57) highlights limitations in exact categorization of abnormalities, particularly for indeterminate findings. The study identified significant overdiagnosis in atypical squamous cells of undetermined significance (ASCUS) and cannot exclude high-grade squamous intraepithelial lesions (ASC-H) categories, which showed overdiagnosis rates of 40% and 42.1% respectively [19]. These findings underscore the importance of using standardized protocols like EP12-A2 to identify specific areas for quality improvement in cervical cancer screening programs, particularly in resource-limited settings where Pap test accuracy is crucial for patient management.
Experimental Protocol for EP12-A2 Evaluation
Implementing the CLSI EP12-A2 guideline requires a systematic approach to study design, data collection, and statistical analysis. The following section outlines the detailed methodology employed in the case study, providing a replicable framework for researchers evaluating qualitative test performance.
Sample Processing and Diagnostic Criteria
The analytical process begins with proper sample collection and preparation. In the referenced study, cervical samples were collected using appropriate sampling devices and immediately fixed at the collection site to preserve cellular morphology [19]. The fixed samples were then transported to the central laboratory for processing using the Leica ST5010 autostainer XL stainer, an automated system capable of processing up to 200 slides per hour to ensure standardization and efficiency [19]. Cytological interpretation followed the 2014 Bethesda system, with screening performed by qualified medical technologists and all abnormal findings (including ASCUS, ASC-H, AGUS, LSIL, HSIL, and carcinomas) confirmed by pathologists to ensure diagnostic accuracy [19]. This systematic approach to sample handling and interpretation minimizes pre-analytical and analytical variables that could affect test performance.
Histopathological confirmation, serving as the reference standard, was conducted using tissue biopsies evaluated according to the FIGO 2015 nomenclature, which categorizes findings as cervical intraepithelial neoplasia grades 1, 2, or 3 (CIN 1, CIN 2, CIN 3), carcinomas, or other tissue diagnoses [19]. The paired coding of cytological and histological results was supervised by both computer technicians and pathologists to ensure accurate data linkage, with indeterminate cytological results specifically evaluated against their histopathological correlations to determine rates of accurate diagnosis, overdiagnosis, and underdiagnosis [19].
Statistical Evaluation Following EP12-A2 Guidelines
The EP12-A2 protocol requires specific statistical approaches to evaluate test performance comprehensively. The first step involves constructing 2x2 contingency tables comparing the qualitative test results (Pap test findings) against the reference standard (histopathological diagnosis), from which fundamental performance metrics are calculated [19] [29]. Sensitivity represents the test's ability to correctly identify patients with disease, while specificity measures its ability to correctly identify patients without disease. Positive and negative predictive values indicate the probability that positive or negative test results truly reflect the patient's actual condition, with these values being particularly influenced by disease prevalence in the population [19].
Beyond these basic metrics, the EP12-A2 framework incorporates more advanced statistical analyses. Cohen's weighted Kappa statistic (κ) is used to measure the level of agreement between cytological and histological categorizations beyond what would be expected by chance alone, with the study reporting moderate agreement (κ=0.57) [19]. Bayesian analysis is employed to calculate positive and negative likelihood ratios, which indicate how much a given test result will raise or lower the probability of disease, and to estimate post-test probabilities using Bayes' theorem [19]. This comprehensive statistical approach provides laboratories with a complete picture of test performance, enabling data-driven decisions about method implementation and quality improvement initiatives.
Essential Research Reagents and Materials
Successful implementation of the EP12-A2 protocol for Pap test evaluation requires specific laboratory equipment, reagents, and analytical tools. The following table details the essential components used in the referenced study and recommended for similar evaluations.
Table 3: Essential Research Reagents and Materials for EP12-A2 Pap Test Evaluation
| Item | Specification/Model | Application in EP12-A2 Evaluation |
|---|---|---|
| Automated Stainer | Leica ST5010 Autostainer XL | Standardized Papanicolaou staining of cervical cytology slides to ensure consistent staining quality and reduce technical variability [19]. |
| Cytological Classification System | 2014 Bethesda System | Standardized reporting system for cervical cytology results, providing consistent diagnostic categories (NILM, ASCUS, LSIL, HSIL, etc.) for performance evaluation [19]. |
| Histopathological Classification System | FIGO 2015 Nomenclature | Reference standard for histopathological diagnosis of cervical biopsies, categorizing findings as CIN 1, 2, 3, or carcinoma for correlation with cytology [19]. |
| Statistical Analysis Software | IBM SPSS v22.0 | Data analysis platform for performing EP12-A2 statistical calculations including sensitivity/specificity, predictive values, Kappa agreement, and Bayesian analysis [19]. |
| Specialized Validation Software | Analyse-it Method Validation Edition | Software specifically designed for CLSI protocol implementation, including EP12-A2 statistical analysis for qualitative test performance evaluation [9]. |
| Microscopy Equipment | Professional-grade light microscopes | High-quality cellular visualization for accurate cytological and histopathological interpretation by technologists and pathologists. |
Implications for Cervical Cancer Screening Programs
The application of the CLSI EP12-A2 protocol to Pap test evaluation provides valuable insights for improving cervical cancer screening programs, particularly in resource-limited settings. The high sensitivity (94%) and negative predictive value (97.1%) demonstrated in the study support the continued value of Pap testing as an effective screening tool for ruling out cervical abnormalities [19]. However, the moderate specificity (74.6%) and positive predictive value (58%) indicate limitations in accurately confirming disease presence based solely on cytological findings [19]. These performance characteristics underscore the importance of complementary testing approaches, such as HPV DNA testing, particularly for managing indeterminate cytological results like ASCUS and ASC-H that demonstrated high rates of overdiagnosis (40% and 42.1% respectively) [19].
The findings highlight the critical need for ongoing quality monitoring using standardized protocols like EP12-A2 in cervical cytology laboratories. The moderate cyto-histological agreement (κ=0.57) suggests significant room for improvement in diagnostic categorization, potentially achievable through enhanced training, standardized diagnostic criteria application, and implementation of quality control measures [19]. For researchers and clinicians, these results emphasize the importance of understanding the limitations of screening tests and the value of histopathological confirmation for abnormal cytological findings before proceeding with definitive treatment. As cervical cancer screening strategies evolve, particularly in middle-income countries like Peru, the EP12-A2 protocol provides a valuable framework for objectively evaluating new technologies and methodologies against established standards, ensuring that changes in practice yield genuine improvements in diagnostic accuracy and patient outcomes.
Troubleshooting EP12 Evaluations: Overcoming Common Challenges
Addressing Discrepant Results and Resolving Method Conflicts
Within the framework of CLSI EP12 protocol research, the evaluation of qualitative, binary output examinations is a cornerstone of diagnostic accuracy [1]. These tests, which yield results such as positive/negative or present/absent, are critical for clinical decision-making. A fundamental part of their validation, as per the CLSI EP12-A2 User Protocol and its subsequent third edition, involves method comparison studies [1] [31]. These studies are designed to measure the agreement between a new candidate method and a comparative method. In an ideal scenario, the results from both methods would be perfectly concordant. However, in practice, discrepant results are a common and expected occurrence, representing a core methodological conflict that must be systematically addressed.
The presence of a discrepancy indicates that the two methods have produced conflicting classifications for the same sample. Resolving these conflicts is not merely a statistical exercise; it is a rigorous process essential for determining the true clinical performance of a new assay [12]. Failure to adequately investigate discrepant results can lead to a biased overestimation of a test's performance, potentially resulting in the adoption of an assay that produces false positives or false negatives, with significant implications for patient care and drug development outcomes. This guide provides a detailed technical framework for identifying, analyzing, and resolving discrepant results, aligning with the best practices outlined in CLSI EP12 and related literature.
Fundamental Concepts and Definitions
The 2x2 Contingency Table: The Foundation of Analysis
The initial analysis of a method comparison study is universally summarized using a 2x2 contingency table (also known as a "truth table" or "confusion matrix") [10] [23]. This table provides a clear, quantitative snapshot of the agreement and disagreement between the candidate and comparative methods.
- True Positive (a): The number of samples classified as positive by both the candidate and comparative methods.
- False Positive (b): The number of samples classified as positive by the candidate method but negative by the comparative method.
- False Negative (c): The number of samples classified as negative by the candidate method but positive by the comparative method.
- True Negative (d): The number of samples classified as negative by both methods.
The cells b and c represent the discrepant results that form the central challenge of this analysis.
Key Performance Metrics Derived from the Contingency Table
From the contingency table, key metrics are calculated to quantify the method's agreement. It is critical to understand that when the comparative method is not a reference method, these are measures of agreement, not intrinsic diagnostic performance [12] [23].
- Positive Percent Agreement (PPA):
[a/(a+c)]*100| The ability of the candidate method to agree with the comparative method on positive samples. - Negative Percent Agreement (NPA):
[d/(b+d)]*100| The ability of the candidate method to agree with the comparative method on negative samples. - Overall Percent Agreement (POA):
[(a+d)/n]*100| The total proportion of samples where the two methods agree.
The following table summarizes these metrics and their calculations:
Table 1: Key Agreement Metrics Calculated from a 2x2 Contingency Table
| Metric | Calculation | Interpretation |
|---|---|---|
| Positive Percent Agreement (PPA) | [a/(a+c)] * 100 |
Agreement on positive samples between methods. |
| Negative Percent Agreement (NPA) | [d/(b+d)] * 100 |
Agreement on negative samples between methods. |
| Overall Percent Agreement (POA) | [(a+d)/n] * 100 |
Total proportion of concordant results. |
Diagnostic Accuracy vs. Method Comparison
A crucial distinction must be made between a method comparison study and a diagnostic accuracy study [10] [12].
- Diagnostic Accuracy: In this design, the candidate method's results are compared against a Diagnostic Accuracy Criteria, which is the best available method for determining the true condition of the sample (e.g., a clinical gold standard like viral culture or a composite reference standard). The resulting metrics are termed sensitivity (true positive rate) and specificity (true negative rate) [10].
- Method Comparison: Here, the candidate method is compared against another method which may not be a gold standard. The resulting metrics are PPA and NPA. Reporting them as "sensitivity" and "specificity" is misleading, as any error in the comparative method will inherently bias the estimates for the candidate method [12]. Resolving discrepancies is the process of moving from a simple method comparison closer to an understanding of true diagnostic accuracy.
A Systematic Protocol for Resolving Discrepant Results
Resolving discrepant results requires a predefined, unbiased protocol. Ad-hoc decisions introduce significant bias and invalidate the statistical analysis. The following workflow provides a robust framework for this process.
Pre-Planning: Establishing the Resolution Protocol
Before initiating the comparison study, a detailed protocol for resolving discrepancies must be documented to prevent bias [12]. This protocol should specify:
The Resolution Method: The definitive analytical technique used to adjudicate discrepancies. This should be a method with superior analytical specificity, sensitivity, or both, often referred to as an "orthogonal" method or gold standard [12] [11]. Examples include:
- Nucleic acid amplification tests (NAATs) with different gene targets.
- Sequencing (e.g., Sanger, NGS).
- Microbiological culture.
- A clinically defined composite reference standard.
Blinding Procedures: The personnel performing the resolution testing must be blinded to the results from both the candidate and comparative methods to prevent interpretive bias [12].
Decision Rules: Clear, objective criteria for how the resolution result will be used to reclassify the sample in the final contingency table. For example: "A sample where the resolution method confirms the candidate result will be reclassified as a True Positive/Negative."
The Resolution Process and Reclassification
Once a discrepancy is identified, the pre-defined resolution method is applied. The outcome leads to a reclassification of the sample, which directly impacts the final performance estimates.
- Resolving a False Positive (b): If the resolution method returns a negative result, the candidate method's positive finding is incorrect. The sample remains a False Positive. If the resolution method returns a positive result, the candidate method was correct, and the comparative method was wrong. The sample is reclassified from a False Positive to a True Positive.
- Resolving a False Negative (c): If the resolution method returns a negative result, the candidate method's negative finding is incorrect. The sample remains a False Negative. If the resolution method returns a positive result, the candidate method was wrong, and the comparative method was correct. The sample is reclassified from a False Negative to a True Negative.
This adjudication process refines the initial contingency table, providing a more accurate estimate of the candidate method's performance relative to the truth.
Table 2: Discrepant Result Reclassification Matrix
| Discrepant Category | Resolution Method Result | Reclassified As | Implication |
|---|---|---|---|
| False Positive (FP) | Negative | Remains FP | Confirms error in candidate method. |
| False Positive (FP) | Positive | True Positive (TP) | Error in comparative method; candidate was correct. |
| False Negative (FN) | Positive | Remains FN | Confirms error in candidate method. |
| False Negative (FN) | Negative | True Negative (TN) | Error in comparative method; candidate was correct. |
Experimental Design and Statistical Considerations
Sample Selection and Sizing
The reliability of a method comparison study is heavily dependent on appropriate sample selection and size [10] [11].
- Sample Matrix: Samples must be in the appropriate clinical matrix (e.g., serum, plasma, swab eluent) and should ideally reflect the patient population the test will serve [10] [32].
- Number of Samples: CLSI EP12-A2 recommends testing at least 50 positive and 50 negative specimens by the comparative method to achieve reasonably precise estimates of PPA and NPA [11]. Smaller sample sizes lead to unacceptably wide confidence intervals, reducing the statistical power of the study [10] [23]. For instance, with only 5 positive and 5 negative samples and perfect agreement, the lower 95% confidence limit for PPA and NPA can be as low as 57% [23].
Table 3: Recommended Sample Planning for a Qualitative Method Comparison Study
| Factor | Recommendation | Rationale |
|---|---|---|
| Total Sample Number | Minimum 100 samples | Provides a stable base for agreement estimates [11]. |
| Positive/Negative Ratio | Reflect expected disease prevalence or a 50/50 split | A 50/50 split provides the best statistical efficiency for estimating both PPA and NPA. |
| Sample Types | Include all specimen types (e.g., serum, plasma, swabs) for which the test is claimed. | Performance may vary significantly by matrix [11]. |
| Study Duration | 10 to 20 days [10]. | Captures inter-day analytical variation (e.g., reagent lot changes, operator differences). |
Calculating Confidence Intervals
Point estimates of PPA and NPA are insufficient without a measure of their precision. Reporting 95% confidence intervals (95% CI) is essential [10] [23]. The formulas for calculating these intervals, as provided in CLSI EP12-A2, are based on a Wilson Score interval and are more reliable than simple asymptotic formulas, especially for proportions near 0 or 1 and for small sample sizes [23].
The calculations, while manageable in a spreadsheet, involve multiple steps. For example, the lower (LL) and upper (HL) confidence limits for PPA are calculated as follows [23]:
- Q1 = 2a + 3.84
- Q2 = 1.96 * √[3.84 + (4a*c)/(a+c)]
- Q3 = 2(a+c) + 7.68
- PPA LL = 100 * (Q1 - Q2) / Q3
- PPA HL = 100 * (Q1 + Q2) / Q3
Similar calculations are performed for NPA and POA. The width of the confidence interval provides a direct visual representation of the reliability of the agreement estimate; narrow intervals indicate greater precision.
The Scientist's Toolkit: Essential Research Reagent Solutions
The successful execution of a discrepancy resolution study relies on a set of well-characterized materials and reagents.
Table 4: Essential Research Reagents and Materials for Discrepancy Resolution
| Item | Function & Importance | Technical Specifications |
|---|---|---|
| Characterized Clinical Panels | Comprised of well-defined positive and negative samples; used for the initial comparison study. | Must include samples near the clinical decision point (cut-off) to challenge assay robustness [10]. |
| Orthogonal Assay Kits | The third, superior method used for discrepancy resolution. | Must have demonstrated high analytical sensitivity and specificity, preferably targeting a different analyte or sequence [12] [11]. |
| Reference Standard Materials | Provides an objective, traceable basis for quantifying analyte and verifying assay performance. | Available from organizations like NIST or WHO. Crucial for harmonizing results across different labs. |
| Interference & Cross-Reactivity Panels | Evaluates analytical specificity by testing potential interferents (e.g., bilirubin, lipids) and structurally similar analytes. | Required for laboratory-developed tests (LDTs) per CLIA regulations [32]. |
| Stability Samples | Used to assess reagent and sample stability over time, a potential source of discrepancy. | Prepared at low and high analyte concentrations and tested over the claimed storage period [1]. |
| Ru(bpy)2(mcbpy-O-Su-ester)(PF6)2 | Ru(bpy)2(mcbpy-O-Su-ester)(PF6)2, MF:C36H29F12N7O4P2Ru, MW:1014.7 g/mol | Chemical Reagent |
| Sulfo-cyanine5.5 amine potassium | Sulfo-cyanine5.5 amine potassium, MF:C46H54K2N4O13S4, MW:1077.4 g/mol | Chemical Reagent |
Interpretation and Final Analysis
The final step is to interpret the refined data from the resolved contingency table. The recalculated PPA and NPA with their 95% CIs are compared against pre-defined performance goals. These goals should be based on the intended clinical use of the test and, where possible, regulatory guidance [11].
It is critical to perform a risk assessment on any remaining unresolved or confirmed discrepant results. Even a method with 98% agreement may be unacceptable if the 2% error rate leads to severe clinical consequences, such as missing an active infection or causing a unnecessary treatment regimen. The resolution of method conflicts through this rigorous process ensures that the final implemented test delivers the accuracy and reliability required for robust clinical research and patient diagnostics.
Evaluating the performance of qualitative, binary output tests presents unique challenges when dealing with rare diseases and limited sample materials. Within the framework of CLSI EP12 research, optimizing sample selection becomes critical for establishing reliable performance specifications while working with constrained resources. The CLSI EP12 guideline provides a structured framework for evaluating qualitative examinations that produce binary results (e.g., positive/negative, present/absent, reactive/nonreactive) [1]. This guidance is particularly valuable for developers of laboratory-developed tests who must establish performance specifications even when rare conditions limit available positive samples [32].
The fundamental challenge lies in the statistical reality that rare conditions yield fewer positive samples, creating tension between regulatory requirements for robust validation and practical limitations of sample availability. CLIA regulations mandate that laboratories establishing laboratory-developed tests must establish comprehensive performance specifications including accuracy, precision, reportable range, reference interval, analytical sensitivity, and analytical specificity [32]. This technical guide addresses protocols and methodologies for meeting these rigorous requirements while working within the constraints imposed by rare diseases and limited sample materials.
Core Principles of CLSI EP12 for Qualitative Test Evaluation
Understanding the EP12 Framework
The CLSI EP12 guideline provides product design guidance and protocols for performance evaluation during the Establishment and Implementation Stages of the Test Life Phases Model [1] [2]. The third edition, published in March 2023, represents a significant update from the previous EP12-A2 version, expanding the types of procedures covered to reflect advances in laboratory medicine and adding protocols for use during examination procedure design, validation, and verification [1].
A key concept in EP12 is the characterization of the imprecision interval, defined by C5 and C95 estimates [1] [17]. C50 represents the concentration that yields 50% positive results, while C5 and C95 represent concentrations yielding 5% and 95% positive results respectively [17]. This interval is critical for understanding the uncertainty around the cutoff point in qualitative tests, especially those with an internal continuous response that is converted to a binary output via a cutoff value [17].
Regulatory Context and Requirements
For laboratory-developed tests, CLIA regulations require establishments to define several key performance characteristics, as outlined in Table 1 [32].
Table 1: CLIA Requirements for Test Verification and Validation
| Performance Characteristic | Requirement for FDA-Approved/Cleared Test | Requirement for Laboratory-Developed Test |
|---|---|---|
| Reportable Range | 5-7 concentrations across stated linear range, 2 replicates at each concentration | 7-9 concentrations across anticipated measuring range; 2-3 replicates at each concentration |
| Analytical Sensitivity (Limit of Detection) | Not required by CLIA (but CAP requires for quantitative assays) | 60 data points (e.g., 12 replicates from 5 samples) over 5 days; probit regression analysis |
| Precision | For qualitative test: test 1 control/day for 20 days or duplicate controls for 10 days | For qualitative test: minimum of 3 concentrations (LOD, 20% above LOD, 20% below LOD) with 40 data points |
| Analytical Specificity | Not required by CLIA | Testing of interfering substances and genetically similar organisms |
| Accuracy | 20 patient specimens within the measuring interval | Typically 40 or more specimens tested in duplicate over at least 5 operating days |
| Reference Interval | May transfer manufacturer's stated interval if applicable to population | For qualitative tests, typically "negative" or "not detected" if target is always absent in healthy individuals |
Strategic Approaches for Rare Disease Sample Selection
When native patient samples from rare disease populations are limited, consider these alternative sample strategies:
- Artificial samples: Spiking known negative matrices with synthetic targets or recombinant proteins
- Retrospective samples: Utilizing banked specimens from rare disease registries or biobanks
- Cross-institutional collaborations: Pooling resources with other laboratories facing similar challenges
- Clinical trial specimens: Partnering with research institutions conducting clinical trials for rare conditions
- Surrogate samples: Using closely related analytes that demonstrate similar analytical behavior
For molecular tests targeting rare pathogens, CLSI EP12 recommends supplemental information on determining the lower limit of detection for qualitative examinations based on PCR methods, which is particularly valuable when positive samples are scarce [2].
Statistical Approaches for Small Sample Sizes
When working with limited numbers of positive samples, employ these statistical strategies:
- Bayesian statistics: Incorporating prior knowledge to supplement limited experimental data
- Bootstrap resampling: Using computational methods to estimate confidence intervals with small n
- Sequential analysis: Evaluating data as it is collected rather than waiting for a fixed sample size
- Pooled testing: Combining multiple samples to increase efficiency when disease prevalence is low
The FDA recognition of CLSI EP12 as a consensus standard for satisfying regulatory requirements provides assurance that protocols following this guideline will meet regulatory expectations even when sample sizes are challenging [1].
Experimental Protocols for Limited Sample Scenarios
Precision Evaluation with Scarce Materials
For precision studies with limited positive samples, EP12 recommends approaches that maximize information from each specimen:
Diagram: Precision Evaluation Workflow with Limited Samples
The precision experiment should focus on characterizing the imprecision interval around the cutoff, requiring fewer samples than full precision studies. Test samples at three key concentrations: the expected limit of detection (LOD), 20% above LOD, and 20% below LOD, obtaining at least 40 data points across these concentrations [32]. This approach efficiently characterizes the uncertainty in binary classification without requiring large numbers of rare positive samples.
Clinical Agreement Studies with Limited Positives
When true positive samples from rare conditions are scarce, employ this modified clinical agreement protocol:
Table 2: Modified Clinical Agreement Study for Rare Conditions
| Study Component | Standard Approach | Modified Approach for Rare Diseases |
|---|---|---|
| Positive Sample Size | 40+ specimens recommended | Leverage all available positives with statistical adjustments |
| Comparison Method | Established reference method | Composite reference standard (multiple methods) |
| Statistical Analysis | Percent agreement with confidence intervals | Bayesian approaches incorporating external data |
| Handling of Inconclusives | Typically excluded | Explicit protocol for tiered interpretation |
For qualitative tests, accuracy is characterized by clinical agreement with a comparative test or diagnostic classification [17]. When rare conditions limit positive samples, document the limitations transparently and employ statistical methods that appropriately quantify uncertainty with smaller sample sizes.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagent Solutions for Qualitative Test Development
| Reagent/Material | Function in Test Development | Considerations for Rare Diseases |
|---|---|---|
| Synthetic Targets | Artificial positive controls for optimization | Enables development when natural positives are scarce |
| Clinical Sample Pools | Negative matrix for specificity studies | Create large-volume pools to conserve rare positives |
| Stability Reference Panels | Evaluating reagent and sample stability | Small-panel designs with enhanced monitoring |
| Interference Test Kits | Assessing analytical specificity | Focus on most clinically relevant interferents |
| Cross-reactivity Panels | Evaluating analytical specificity | Prioritize genetically or structurally related organisms |
| Commutable Controls | Monitoring test performance over time | Ensure consistency across limited test runs |
| Dabigatran Etexilate-d11 | Dabigatran Etexilate-d11, MF:C34H41N7O5, MW:638.8 g/mol | Chemical Reagent |
| Cholylglycylamidofluorescein | Cholylglycylamidofluorescein, MF:C46H56N2O6, MW:732.9 g/mol | Chemical Reagent |
Methodologies for Key Experiments with Scarce Samples
Limit of Detection (LoD) Determination
For qualitative tests with limited positive samples, employ a modified LoD protocol:
Diagram: LoD Determination with Limited Samples
The CLSI-recommended approach for laboratory-developed tests requires approximately 60 data points collected over multiple days (e.g., 12 replicates from 5 samples) with probit regression analysis [32]. When samples from rare diseases are limited, increase replication at fewer concentration levels rather than testing many concentrations with minimal replication.
Analytical Specificity Testing
For rare diseases, focus specificity testing on the most clinically relevant interferents and cross-reactants:
- Sample-related interferences: Test effects of hemolysis, lipemia, and icterus using spiked samples at low positive concentrations [32]
- Cross-reactivity: Test genetically similar organisms or organisms found in the same sample sites with similar clinical presentations [32]
- High prevalence targets: Prioritize organisms that are more common and likely to be encountered in the same patient population
Optimizing sample selection for rare diseases within the CLSI EP12 framework requires strategic approaches to maximize information from limited materials. By implementing the protocols and methodologies outlined in this guide, researchers can generate scientifically valid performance data while acknowledging the limitations inherent in working with rare conditions. The recently published third edition of EP12 provides expanded guidance that supports these approaches, including enhanced protocols for stability evaluation, interference testing, and precision assessment [1] [2].
As molecular technologies continue to advance, particularly in areas like next-generation sequencing addressed in the updated EP12 guideline [2], the challenges of evaluating tests for rare conditions will continue to evolve. By adhering to the principles of CLSI EP12 while implementing creative solutions for sample management, researchers can advance diagnostic capabilities for rare diseases while maintaining scientific rigor and regulatory compliance.
In the context of CLSI EP12-A2 qualitative test performance protocol research, ensuring adequate statistical power through appropriate sample size determination is a fundamental requirement for producing scientifically valid and regulatory-accepted results. Statistical power, defined as the probability that a study will correctly reject a false null hypothesis, is critically dependent on sample size and directly impacts the reliability of diagnostic test evaluations [33]. Researchers developing qualitative tests with binary outputs (e.g., positive/negative, present/absent) must balance statistical rigor with practical constraints when designing validation studies [1]. Inadequate sample sizes lead to Type II errors (false negatives), where truly inaccurate tests appear acceptable, potentially compromising patient care and regulatory decisions [33]. Conversely, excessively large samples waste resources and may raise ethical concerns [33]. The CLSI EP12 guideline provides a structured framework for designing these evaluations, emphasizing that proper sample size planning is essential for generating reliable sensitivity and specificity estimates with acceptable confidence intervals [1] [10].
Foundational Concepts: Power, Error, and Effect Size
Type I and Type II Errors
Statistical hypothesis testing in diagnostic research involves balancing two potential errors. A Type I error (α), or false positive, occurs when researchers incorrectly reject a true null hypothesis (e.g., concluding a test is accurate when it is not) [33] [34]. The α-level is typically set at 0.05 (5%), meaning researchers accept a 5% chance of a false positive conclusion [33]. Conversely, a Type II error (β), or false negative, happens when researchers fail to reject a false null hypothesis (e.g., concluding a test is inaccurate when it actually performs well) [33] [34]. The relationship between these errors is inverse; reducing one increases the other, requiring careful balance in study design [33].
Statistical Power and Its Determinants
Statistical power, calculated as 1-β, represents the probability of correctly detecting a true effect or difference [33] [34]. For qualitative test validation, the "effect" typically represents the true sensitivity and specificity of the test. The ideal power for a study is generally considered to be 0.8 (80%) or higher, meaning the study has an 80% chance of detecting a true difference if one exists [33]. Power depends on several factors: (1) sample size - larger samples increase power; (2) effect size - larger true differences are easier to detect; (3) significance level (α) - stricter α-levels (e.g., 0.01 vs. 0.05) reduce power; and (4) population variability - more homogeneous populations increase power [33] [35].
Effect Size in Diagnostic Test Evaluation
Effect size (ES) quantifies the magnitude of a phenomenon in a standardized way that is independent of sample size [33]. In qualitative test validation, effect size may refer to the minimum acceptable performance for sensitivity and specificity compared to a gold standard or comparator method. For example, a researcher might determine that a new test must demonstrate at least a 15% improvement in sensitivity over an existing method to be clinically meaningful. accurately estimating the expected effect size is crucial for appropriate sample size calculation, as smaller effect sizes require larger samples to detect with adequate power [33].
Table 1: Key Statistical Concepts in Sample Size Determination
| Concept | Definition | Typical Threshold | Impact on Sample Size |
|---|---|---|---|
| Type I Error (α) | Probability of false positive (rejecting true H₀) | 0.05 | Stricter α (0.01) requires larger sample |
| Type II Error (β) | Probability of false negative (failing to reject false H₀) | 0.20 | Lower β requires larger sample |
| Statistical Power (1-β) | Probability of correctly detecting true effect | 0.80 | Higher power requires larger sample |
| Effect Size (ES) | Magnitude of the phenomenon or difference | Varies by context | Smaller ES requires larger sample |
Sample Size Calculation Methods for Qualitative Tests
CLSI EP12 Framework for Qualitative Test Validation
The CLSI EP12 guideline provides specific guidance for evaluating qualitative, binary output examinations, covering key aspects such as imprecision (C5 and C95 estimation), clinical performance (sensitivity and specificity), stability, and interference testing [1]. This framework emphasizes that sample selection should represent the target population, including appropriate representation of both infected and non-infected individuals for infectious disease tests [10]. The guideline recommends studies be conducted over 10 to 20 days to account for daily variability, though shorter periods may be acceptable if reproducibility conditions are assured [10]. For statistical inference, EP12 emphasizes reporting 95% confidence intervals around sensitivity and specificity estimates, with the understanding that these intervals are strongly influenced by sample size [10].
Sample Size Calculation Approaches
Different methodological approaches require specific sample size calculations. The following table summarizes key formulas for common study designs relevant to qualitative test validation:
Table 2: Sample Size Calculation Formulas for Different Study Types
| Study Type | Formula | Parameters |
|---|---|---|
| Proportion (Sensitivity/Specificity) | ( n = \frac{Z_{α/2}^2 \times P(1-P)}{E^2} ) | P = expected proportion, E = margin of error, Z_{α/2} = 1.96 for α=0.05 [34] |
| Two Proportions | ( n = \frac{(Z{α/2} + Z{1-β})^2 \times (p1(1-p1) + p2(1-p2))}{(p1 - p2)^2} ) | pâ‚, pâ‚‚ = proportions in two groups, Z_{1-β} = 0.84 for 80% power [34] |
| Diagnostic (ROC) Studies | ( n = \frac{(G_{1-α/2})^2 \times TPF \times FPF}{L^2} ) | TPF = true positive fraction, FPF = false positive fraction, L = desired CI width [34] |
Practical Considerations for Qualitative Tests
When applying these formulas to qualitative test validation per CLSI EP12, several practical considerations emerge. First, the prevalence of the condition in the study population affects the precision of sensitivity and specificity estimates [10]. For rare conditions, obtaining sufficient positive samples may require commercial panels or multi-center collaborations. Second, the intended use of the test determines which performance parameter is most critical; for example, blood screening tests prioritize sensitivity to minimize false negatives, while confirmatory tests may prioritize specificity to minimize false positives [10]. Third, researchers must consider practical constraints including cost, time, and sample availability when determining feasible sample sizes [33].
Implementing CLSI EP12 Protocols with Adequate Power
Diagnostic Accuracy Study Design
When the comparator method represents diagnostic accuracy criteria (gold standard), CLSI EP12 recommends using a 2×2 contingency table approach to calculate sensitivity, specificity, and their confidence intervals [10]. The required sample size depends on the minimum acceptable performance specifications for these parameters. For example, if a test must demonstrate at least 95% sensitivity and 90% specificity, sample size calculations should ensure adequate precision around these estimates. The table below illustrates how sample size affects the precision of sensitivity estimates:
Table 3: Sample Size Impact on Sensitivity Estimate Precision
| Number of Positive Samples | Observed Sensitivity | 95% Confidence Interval |
|---|---|---|
| 10 | 90% | 60% to 98% |
| 25 | 90% | 74% to 97% |
| 50 | 90% | 79% to 95% |
| 100 | 90% | 83% to 94% |
Alternative Comparator Study Design
When a gold standard is unavailable and the comparator is another method (not diagnostic accuracy criteria), the study design shifts to evaluating concordance between methods [10]. In this approach, sample size determination must account for the expected agreement rate and the clinical significance of disagreements. All discrepant results should undergo confirmatory testing using additional methods whenever possible. This design requires larger sample sizes than the diagnostic accuracy approach to achieve equivalent power, as the inherent imperfection of the comparator method introduces additional variability.
Case Study Application
Consider a validation study for a new qualitative virology test where the manufacturer specifies sensitivity must be ≥95% and specificity ≥98% [10]. Using 24 positive samples and 96 negative samples (based on gold standard determination), researchers observe 24 true positives and 94 true negatives. This yields:
- Sensitivity = 100% (95% CI: 86% to 100%)
- Specificity = 98.1% (95% CI: 93% to 99%)
The confidence intervals for both parameters contain the manufacturer's specifications, suggesting the test meets requirements. However, the relatively wide confidence interval for sensitivity (86% to 100%) indicates limited precision due to the small number of positive samples. To achieve a narrower interval (e.g., 90% to 100%), additional positive samples would be needed.
The Researcher's Toolkit for Sample Size Determination
Statistical Software and Tools
Various specialized software tools can facilitate sample size calculations for researchers implementing CLSI EP12 protocols. These tools provide user-friendly interfaces for the complex statistical calculations required for different study designs. The table below summarizes key resources mentioned in the literature:
Table 4: Essential Research Reagent Solutions for Qualitative Test Validation
| Tool/Resource | Type | Primary Application | Access |
|---|---|---|---|
| G-Power | Software | Comprehensive power analysis | Free |
| R Statistics | Software | Flexible power/sample size calculations | Free |
| CLSI EP12 | Guideline | Protocol for qualitative test evaluation | Purchase |
| Commercial Panels | Biological | Source of characterized positive samples | Purchase |
| (S)-1-Nitrosopiperidin-3-ol-d4 | (S)-1-Nitrosopiperidin-3-ol-d4, MF:C5H10N2O2, MW:134.17 g/mol | Chemical Reagent | Bench Chemicals |
Implementing Validation Experiments
When conducting validation studies per CLSI EP12, researchers should consider several practical aspects. First, sample characterization should include relevant sources of variation such as different subtypes of infectious agents, various stages of disease, and potentially interfering substances [10]. Second, study duration should be sufficient to account for expected reagent and operator variability, typically 10-20 days as recommended by CLSI [10]. Third, statistical analysis plans should be specified before data collection, including primary endpoints, statistical methods, and success criteria. This prevents methodological flexibility that could compromise study validity.
Determining appropriate sample sizes with adequate statistical power is a critical component of qualitative test validation following CLSI EP12 protocols. This process requires careful consideration of statistical principles (Type I/II error balance, effect size, power), regulatory requirements (FDA-recognized standards), and practical constraints (sample availability, cost). By implementing the methodologies outlined in this guide—including proper study design, appropriate sample size calculations, and comprehensive performance evaluation—researchers can ensure their qualitative test validations produce reliable, reproducible results suitable for regulatory submission and clinical implementation. The framework provided by CLSI EP12, when combined with rigorous statistical planning, creates a robust foundation for establishing the diagnostic accuracy of binary output examinations across various medical applications.
Avoiding Common Pitfalls in Diagnostic Accuracy Criteria Creation
Within the framework of CLSI EP12-A2 qualitative test performance protocol research, the creation of robust diagnostic accuracy criteria represents the cornerstone of reliable test evaluation. Diagnostic Accuracy Criteria provide the best currently available information about the presence or absence of the measured condition, forming the essential reference standard against which new methods are judged [12]. The Clinical and Laboratory Standards Institute (CLSI) guidelines emphasize that without properly constructed criteria, measurements of sensitivity, specificity, and predictive values lack validity and may lead to erroneous conclusions about test performance [12] [1].
The methodological rigor in establishing these criteria directly impacts every subsequent performance metric, influencing how laboratories, regulators, and clinicians interpret and apply test results. This technical guide examines the critical pitfalls encountered during criteria development and provides evidence-based strategies to overcome them, ensuring that study outcomes truly represent the analytical and clinical performance of qualitative, binary-output examinations [1] [2].
Core Concepts: Diagnostic Accuracy vs. Method Comparison
A fundamental distinction must be drawn between diagnostic accuracy studies and method comparison studies, as conflating these approaches represents one of the most common and critical pitfalls in qualitative test evaluation.
Defining Key Study Types
- Diagnostic Accuracy Studies: These aim to measure the intrinsic performance of a new method by comparing it against Diagnostic Accuracy Criteria (the reference standard), allowing calculation of true sensitivity and specificity [12].
- Method Comparison Studies: These assess the agreement between a new candidate method and an existing comparative method, reporting Positive Percent Agreement (PPA) and Negative Percent Agreement (NPA) rather than true sensitivity and specificity [12].
Consequences of Conflation
When laboratories report sensitivity and specificity based solely on comparison to an existing method rather than a true reference standard, two primary problems emerge [12]:
- There is no reliable way to determine whether discrepant results stem from errors in the candidate method or the comparative method
- There is no visibility into situations where both methods might concurrently produce false results
Table 1: Key Differences Between Study Approaches
| Aspect | Diagnostic Accuracy Study | Method Comparison Study |
|---|---|---|
| Reference | Diagnostic Accuracy Criteria (reference standard) | Existing method (comparative method) |
| Primary Metrics | Sensitivity, Specificity | Positive Percent Agreement (PPA), Negative Percent Agreement (NPA) |
| Interpretation | Measures true test performance | Measures agreement between methods |
| Sample Requirements | Requires known true positive and true negative status | Requires samples tested by both methods |
Critical Pitfalls and Methodological Solutions
Pitfall 1: Incorporation Bias in Criteria Formation
The Problem: Allowing results from the candidate method to influence the construction or interpretation of the Diagnostic Accuracy Criteria introduces incorporation bias, fundamentally compromising the validity of the reference standard [12].
The Solution: Establish complete independence between the candidate method and the reference standard through blinded interpretation and sequential testing [12].
Pitfall 2: Inadequate Sample Characterization and Sizing
The Problem: Using poorly characterized samples or insufficient sample sizes undermines the statistical reliability of performance estimates, particularly for rare conditions or subpopulation analyses [12].
The Solution: Implement rigorous sample planning that addresses both composition and statistical power requirements.
Sample Composition Considerations:
- Use authentic clinical samples from the target population whenever possible
- Clearly document the origin, processing, and storage conditions of all samples
- Exercise caution with artificial samples, as they may not reflect real-world performance [12]
Statistical Considerations:
- Calculate sample size requirements based on desired confidence intervals for sensitivity and specificity
- For rare conditions, consider enriched designs while accounting for prevalence in predictive value calculations [12]
- The CLSI EP12 framework provides specific guidance on sample planning for binary output examinations [1]
Pitfall 3: Failure to Account for Prevalence in Predictive Values
The Problem: Positive Predictive Value (PPV) and Negative Predictive Value (NPV) calculations that do not account for condition prevalence in the target population can significantly misrepresent clinical utility [12].
The Solution: Apply prevalence-adjusted calculations when study population prevalence differs from the clinical setting of intended use.
Prevalence-Adjusted Formulas [12]:
- PPV = (Sensitivity × Prevalence) / [(Sensitivity × Prevalence) + (1 - Specificity) × (1 - Prevalence)]
- NPV = (Specificity × (1 - Prevalence)) / [(Specificity × (1 - Prevalence)) + (1 - Sensitivity) × Prevalence)]
Table 2: Impact of Prevalence on Predictive Values (Sensitivity 95%, Specificity 90%)
| Prevalence | PPV | NPV | Clinical Interpretation |
|---|---|---|---|
| 1% | 8.7% | 99.9% | Positive results mostly false positives |
| 10% | 51.3% | 99.4% | Moderate PPV, high NPV |
| 25% | 76.0% | 98.1% | Good PPV, excellent NPV |
| 50% | 90.5% | 94.7% | High both PPV and NPV |
Implementing CLSI EP12-A2 Frameworks with Modern Extensions
The CLSI EP12-A2 protocol provides the foundational framework for evaluating qualitative test performance, with the recently published third edition expanding to address technological advancements [1] [2].
Core EP12-A2 Principles
The EP12-A2 guideline establishes standardized approaches for [1] [24]:
- Precision assessment for qualitative methods, including estimation of C5 and C95
- Clinical performance evaluation through sensitivity and specificity
- Interference and stability testing protocols
- Method comparison studies with appropriate statistical analysis
Enhancements in the Third Edition
The updated EP12 standard addresses evolving technologies and methodologies [2]:
- Expanded procedure coverage reflecting advances in laboratory medicine
- Protocols for commercial manufacturers and medical laboratories during examination procedure design
- Enhanced precision evaluation for next-generation sequencing
- Observer precision studies for tests involving subjective interpretation
- Guidance on lower limit of detection determination for PCR-based qualitative examinations
Integrated Experimental Workflow for Robust Criteria Development
A systematic, phased approach ensures comprehensive evaluation while avoiding common methodological traps.
The Researcher's Toolkit: Essential Reagent Solutions
The implementation of robust diagnostic accuracy criteria requires specific research reagents and materials selected for their traceability, stability, and characterization.
Table 3: Essential Research Reagents for Diagnostic Accuracy Studies
| Reagent Category | Specific Examples | Critical Function | Validation Parameters |
|---|---|---|---|
| Reference Standard Materials | CDC influenza reference panels, NIBSC controls | Provides benchmark for true positive/negative status | Traceability, stability, commutability |
| Characterized Clinical Samples | Banked respiratory samples, serum panels | Represents real-world matrix effects | Origin documentation, pre-testing results, storage conditions |
| Interference Substances | Lipids, hemoglobin, common medications | Challenges assay robustness | Concentration verification, purity documentation |
| Calibrators and Controls | Manufacturer-provided controls, third-party controls | Monitors assay performance | Value assignment method, stability documentation |
| Molecular Reagents | Extraction controls, amplification inhibitors | Tests assay vulnerability to interference | Purity, concentration, compatibility |
Regulatory and Quality Considerations
Alignment with International Standards
Successful diagnostic accuracy criteria creation requires harmonization with multiple regulatory and quality frameworks [24]:
- ISO 15189 requirements for medical laboratory quality management
- FDA guidance for in vitro diagnostic devices, particularly for infectious disease detection [16]
- CLSI EP12-A2 and EP12 Ed.3 frameworks for qualitative test evaluation [1] [2]
- Eurachem/CITAC guidance on uncertainty in qualitative analysis [24]
Documentation and Traceability
Comprehensive documentation provides the foundation for defensible diagnostic accuracy criteria [12] [16]:
- Sample provenance including collection, processing, and storage conditions
- Reference method justification with established performance characteristics
- Blinding procedures demonstrating independence between candidate and reference testing
- All data including outliers and protocol deviations
- Statistical analysis plans specified prior to study initiation
The creation of robust diagnostic accuracy criteria demands meticulous attention to methodological细节, particularly in maintaining the independence of reference standards, appropriate sample characterization, and proper statistical analysis. By recognizing and avoiding the common pitfalls outlined in this guide—incorporation bias, inadequate sample planning, and unadjusted predictive values—researchers can generate reliable, defensible performance data that accurately represents test capability.
The framework established by CLSI EP12-A2 and its subsequent editions provides a validated foundation for these evaluations, while ongoing attention to regulatory guidance ensures that developed tests meet the rigorous standards required for clinical implementation. As qualitative testing technologies continue to evolve, adherence to these fundamental principles of diagnostic accuracy criteria creation will remain essential for delivering meaningful results to researchers, clinicians, and ultimately, patients.
Within cervical cancer screening programs, the precise classification of epithelial cell abnormalities is fundamental to effective patient management. The Bethesda System establishes standardized categories for reporting cervical cytology, among which the indeterminate interpretations—Atypical Squamous Cells of Undetermined Significance (ASC-US), Atypical Squamous Cells, cannot exclude High-Grade Squamous Intraepithelial Lesion (ASC-H), and Atypical Glandular Cells (AGUS)—present a significant clinical challenge. These categories represent cellular changes that are suggestive of a potential squamous intraepithelial lesion or glandular abnormality but are qualitatively or quantitatively insufficient for a definitive diagnosis [36] [37]. This whitepaper examines the evaluation and management of these categories through the rigorous framework of the CLSI EP12-A2 protocol, "User Protocol for Evaluation of Qualitative Test Performance" [38]. This guideline provides a consistent approach for the design and data analysis of precision and method-comparison studies for qualitative diagnostic tests, making it an essential tool for researchers and developers aiming to improve the reliability of diagnostic examinations that yield binary (positive/negative) outputs [1] [38].
Cytological Categories and Clinical Significance
Atypical Squamous Cells of Undetermined Significance (ASC-US)
- Definition and Etiology: ASC-US describes cytologic changes that suggest a Squamous Intraepithelial Lesion (SIL) but are qualitatively and quantitatively less definitive than a clear SIL diagnosis [36]. These changes may be related to a transient HPV infection, inflammation, atrophy, or other artifacts, but approximately 10-20% of patients with ASC-US are found to have an underlying Cervical Intraepepithelial Neoplasia (CIN) [36].
- Epidemiology: The reported incidence of ASC-US varies widely, from 2.5% to as high as 19.1% in different studies [36]. This variation underscores the subjective component in its interpretation and the need for robust, standardized testing protocols to guide subsequent management.
- hrHPV Correlation: The high-risk Human Papillomavirus (hrHPV) positivity rate in ASC-US cases is a critical risk stratification marker. Studies report rates ranging from 50% in U.S. screening populations to 81% in specific cohorts, with HPV 16 and 18 being the most prevalent oncogenic types identified [36].
Atypical Squamous Cells, cannot exclude HSIL (ASC-H)
- Definition and Clinical Impact: ASC-H refers to cytologic changes that are suggestive of a High-Grade Squamous Intraepithelial Lesion (HSIL) but are insufficient for a definitive interpretation [37]. This category is characterized by sparse cellularity featuring immature (basal or parabasal) squamous cells with high nuclear-to-cytoplasmic (N:C) ratios and nuclei approximately 1.5 to 2.5 times larger than normal intermediate cell nuclei [37].
- Prevalence and Risk: ASC-H accounts for a median of 0.3% of all Pap test results and represents less than 10% of all ASC interpretations [37]. Despite its low incidence, it carries a significant risk. The five-year risk for histologic HSIL and cancer is 12% for ASC-H with a negative hrHPV test and rises to 45% for ASC-H with a positive hrHPV test [37].
Atypical Glandular Cells (AGUS)
- Note on Terminology: The term "AGUS" (Atypical Glandular Cells of Undetermined Significance) was used in earlier versions of the Bethesda System but has since been replaced by more specific categories under the broader heading "Atypical Glandular Cells (AGC)" [36]. These categories include "not otherwise specified" (NOS) or "favor neoplastic" for endocervical and endometrial cells, with the distinct entity of "endocervical adenocarcinoma in situ (AIS)" [36]. Given the user's specified title, this guide will address the general principles of evaluating glandular cell abnormalities.
- Clinical Significance: Glandular cell abnormalities are less common than their squamous counterparts but are clinically significant due to their association with both pre-cancerous and cancerous lesions of the endocervix and endometrium.
Table 1: Summary of Atypical Cervical Cytology Categories
| Category | Definition | Reported Incidence | Key Risk Indicator | Associated 5-Year CIN 3+ Risk |
|---|---|---|---|---|
| ASC-US | Cellular changes suggestive of SIL but not definitive [36]. | 2.5% - 19.1% [36] | ~50-81% hrHPV positive [36] | Varies with hrHPV status |
| ASC-H | Cellular changes suggestive of, but insufficient for, HSIL diagnosis [37]. | Median 0.3% of all tests [37] | 45% risk if hrHPV+ [37] | 12% (hrHPV -), 45% (hrHPV +) [37] |
| AGC | Atypical endocervical or endometrial cells (replaces AGUS) [36]. | Less common than ASC | Not primarily HPV-driven | Requires thorough glandular lesion workup |
Evaluation Within the CLSI EP12-A2 Framework
The CLSI EP12-A2 protocol provides a standardized methodology for evaluating the performance of qualitative tests that produce binary outcomes, such as "positive" or "negative" [38]. This framework is directly applicable to developing and validating testing algorithms for managing indeterminate cervical cytology. The core components of evaluation include:
Assessment of Precision (Imprecision)
- Objective: To determine the reproducibility of the test result when the same sample is tested multiple times. In the context of indeterminate cytology, this relates to the consistency of interpretation for a given slide or the reproducibility of a reflex hrHPV test.
- Protocol: The guideline provides methods for designing studies to estimate the C5 and C95 thresholds—the analyte concentrations at which the test produces a positive result 5% and 95% of the time, respectively. This is crucial for understanding the gray zone where results may be inconsistent [1].
Assessment of Clinical Performance (Sensitivity and Specificity)
- Objective: To evaluate the ability of a test (e.g., hrHPV testing for triaging ASC-US) to correctly identify patients with and without the target disease (e.g., CIN 2+).
- Method-Comparison Studies: CLSI EP12-A2 guides the comparison of a new test against a reference method. For example, the clinical performance of a new hrHPV assay can be established by testing a cohort of women with ASC-US cytology and using histologically confirmed CIN 2+ as the reference standard [1] [38].
- Data Analysis: The protocol provides a consistent approach for calculating sensitivity, specificity, and predictive values, along with their confidence intervals, from the resulting 2x2 contingency tables.
Stability and Interference Testing
- Scope: While the previous edition (EP12-A2) focused on precision and method-comparison, the latest iteration (EP12Ed3) has expanded to include protocols for evaluating sample stability and the effect of potential interferents (e.g., blood, mucus, inflammatory cells) on test performance [1]. This is critical for ensuring reliable hrHPV test results from liquid-based cytology specimens.
The following workflow diagram illustrates the application of the CLSI EP12 framework to the evaluation of a qualitative test used in managing atypical cytology:
Experimental Protocols and Methodologies
Protocol for hrHPV Triage of ASC-US
- Objective: To verify the clinical sensitivity and specificity of a qualitative hrHPV test for detecting CIN 2+ in a cohort of patients with ASC-US cytology, per CLSI EP12-A2 guidelines.
- Sample Collection: Obtain residual liquid-based cytology specimens from women diagnosed with ASC-US. Ensure informed consent and IRB approval.
- Reference Method: Colposcopy with directed biopsy is the reference standard. Patients are classified as having CIN 2+ or
- Index Test Performance: The hrHPV test (e.g., using one of the FDA-approved platforms: Qiagen Hybrid Capture, Hologic Cervista, Hologic Aptima, Roche Cobas, or BD Onclarity) is performed on the ASC-US specimen [37].
- Data Analysis: Construct a 2x2 table comparing hrHPV test results (Positive/Negative) against the histological outcome (CIN 2+ /
Table 2: Key Reagent Solutions for hrHPV Triage Studies
| Research Reagent / Platform | Function in Evaluation |
|---|---|
| Liquid-Based Cytology Media | Preserves cellular material for both cytological review and subsequent nucleic acid extraction for hrHPV testing [36]. |
| Roche Cobas HPV Test | Qualitative PCR-based test to detect 14 hrHPV types, with specific genotyping for HPV 16 and 18; FDA-approved for primary screening [37]. |
| Hologic Aptima HPV Assay | Qualitative test targeting E6/E7 mRNA of 14 hrHPV types; used for triage and co-testing [37]. |
| BD Onclarity HPV Assay | Qualitative test that extends genotyping beyond HPV 16/18; FDA-approved for primary screening [37]. |
| Hybrid Capture 2 (Qiagen) | A DNA-based test for 13 hrHPV types; historically used for ASC-US triage [37]. |
Protocol for Evaluating ASC-H Management Pathways
- Objective: To assess the performance of a risk-based management algorithm for patients with ASC-H cytology.
- Study Design: A longitudinal cohort study following patients with ASC-H results through management (e.g., immediate colposcopy vs. hrHPV triage to colposcopy).
- Data Collection: Record cytology (ASC-H), hrHPV result (positive/negative, and genotype if available), colposcopic findings, and histological outcomes.
- Performance Metrics: The "performance" of the management pathway is evaluated by its ability to correctly identify and direct patients with CIN 2+ to appropriate treatment. The primary metric is the cumulative incidence of CIN 2+ detected under the pathway.
The logical relationship and risk stratification for managing ASC-H results are demonstrated in the following pathway:
Data Presentation and Analysis
The application of the CLSI EP12-A2 framework generates quantitative data essential for validating the test methods used in managing indeterminate cytology. The following table summarizes the type of data and key metrics that should be captured and analyzed.
Table 3: CLSI EP12-Based Evaluation Metrics for Indeterminate Cytology Tests
| Evaluation Type | Study Output | Statistical Analysis | Clinical/Regulatory Utility |
|---|---|---|---|
| Precision (Repeatability) | C5/C95 concentration estimates; Percent agreement across replicates [1]. | Cohen's Kappa (for categorical agreement); Estimation of probability of positive result vs. analyte concentration [1]. | Determines test robustness and gray zone; critical for manufacturer claims. |
| Clinical Sensitivity | Proportion of CIN 2+ cases correctly identified as positive by the index test (e.g., hrHPV). | Point estimate and 95% confidence interval [38]. | Informs clinical efficacy; key for regulatory submissions (FDA). |
| Clinical Specificity | Proportion of | Point estimate and 95% confidence interval [38]. | Informs clinical utility by limiting false positives and unnecessary procedures. |
| Interference Testing | Signal strength or result interpretation in the presence and absence of potential interferents. | Descriptive comparison; significance testing if quantitative. | Ensures reagent and assay reliability under varied clinical sample conditions [1]. |
The indeterminate cytological categories of ASC-US, ASC-H, and AGUS represent a critical challenge in cervical cancer prevention, requiring a nuanced and evidence-based approach to patient management. The CLSI EP12-A2 protocol provides an indispensable methodological framework for researchers and diagnostic developers. By enforcing rigorous standards for the evaluation of precision, clinical performance (sensitivity and specificity), and stability, this guideline ensures that the qualitative tests and algorithms used to triage these ambiguous results are reliable, accurate, and clinically meaningful. The integration of robust hrHPV testing, guided by these standardized evaluation principles, has fundamentally modernized the management of ASC-US and ASC-H, enabling risk-stratified approaches that maximize the detection of precancerous lesions while minimizing unnecessary invasive procedures. Continued adherence to such standardized evaluation protocols is paramount for the development and implementation of future diagnostic technologies in cervical cancer screening.
Validation and Comparative Analysis: Ensuring Method Reliability
Diagnostic accuracy criteria form the foundation for evaluating qualitative, binary output examinations in clinical laboratories and diagnostic test development. These criteria serve as the reference standard against which new tests are measured to determine their clinical utility and reliability. Within the framework of CLSI EP12 guidelines, proper establishment of diagnostic accuracy criteria is essential for validating tests that yield binary results (e.g., positive/negative, present/absent, reactive/nonreactive) [1] [2]. The Clinical and Laboratory Standards Institute (CLSI) recently published the third edition of EP12 in March 2023, replacing the previous EP12-A2 version from 2008, with expanded protocols for examination procedure design, validation, and verification [1] [2].
The fundamental importance of diagnostic accuracy criteria lies in their role for determining clinical sensitivity (the percentage of subjects with the target condition who test positive) and clinical specificity (the percentage of subjects without the target condition who test negative) [10]. These metrics allow researchers and clinicians to understand the true performance characteristics of qualitative tests, which is particularly critical for applications ranging from simple home tests to complex next-generation sequencing for disease diagnosis [2]. The U.S. Food and Drug Administration (FDA) has officially recognized CLSI EP12 as a consensus standard for satisfying regulatory requirements for medical devices, further underscoring its importance in the diagnostic development pipeline [3].
Types of Diagnostic Accuracy Criteria
Reference Methods as Diagnostic Accuracy Criteria
Reference methods represent the gold standard approach for establishing diagnostic accuracy, providing the highest level of confidence in classification. According to CLSI guidelines, when the comparator represents true diagnostic accuracy criteria, the study design follows a primary design diagnostic accuracy model intended to measure "the extent of agreement between the information from the test under evaluation and the diagnostic accuracy criteria" [10]. This approach directly measures how well a new test identifies subjects with and without the target condition as determined by the most definitive diagnostic method available.
The key characteristic of reference methods is their established superiority in correctly classifying subjects. Examples include histopathological examination for cancer diagnosis, viral culture for infectious disease confirmation, or advanced imaging with definitive diagnostic criteria. When using reference methods, all subjects in the validation study must have definitive classification based on the reference standard, which serves as the benchmark for calculating sensitivity and specificity [10]. This approach provides the most straightforward and interpretable assessment of a new test's performance characteristics, as it directly compares against the best available truth standard.
Composite Standards as Diagnostic Accuracy Criteria
In many diagnostic scenarios, a single reference method may not exist or may be impractical for validation studies. Composite standards (also known as composite reference standards) combine multiple diagnostic methods, clinical findings, or follow-up data to establish the most accurate possible classification of subjects. This approach is particularly valuable when no single perfect reference standard exists, or when the reference standard is invasive, expensive, or otherwise unsuitable for large-scale validation studies.
Composite standards integrate various sources of diagnostic information, which may include multiple laboratory tests, clinical symptoms, imaging results, treatment response, and long-term follow-up data. The specific combination depends on the target condition and available diagnostic tools. For example, a composite standard for a respiratory pathogen might include PCR testing, clinical symptom profiles, and serological confirmation. The development of composite standards requires careful consideration of the diagnostic context and should incorporate expert clinical judgment to establish appropriate classification rules before evaluating the new test [10].
Table 1: Comparison of Reference Methods and Composite Standards
| Characteristic | Reference Methods | Composite Standards |
|---|---|---|
| Definition | Single superior diagnostic method | Combination of multiple diagnostic approaches |
| When Used | Gold standard exists and is feasible | No perfect reference standard available |
| Advantages | Simple interpretation, established validity | Practical, comprehensive assessment |
| Limitations | May be unavailable or impractical | More complex to implement and interpret |
| Statistical Analysis | Direct calculation of sensitivity/specificity | May require latent class analysis or similar methods |
Experimental Design and Methodologies
Sample Selection and Characterization
Proper sample selection is critical for meaningful validation of qualitative tests using diagnostic accuracy criteria. The samples must represent the target population in which the test will ultimately be used, including appropriate demographics and clinical presentations. For infectious disease tests, this includes consideration of viral subtypes, mutations, and potential seronegative window periods that might affect performance [10]. Samples from infected individuals should ideally come from definitively diagnosed cases, while non-infected individuals should be carefully confirmed as healthy/non-infected through appropriate methods.
The number of samples directly impacts the statistical power of the validation study. While practical considerations often limit sample size, researchers should recognize that small samples yield wide confidence intervals. For instance, with only 5 positive samples, the 95% confidence interval for sensitivity cannot be narrower than 56.6% to 100% [10]. CLSI EP12 recommends studies be conducted over 10 to 20 days to ensure reproducibility conditions are properly assessed, though shorter periods may be acceptable if reproducibility is adequately demonstrated [10].
Diagnostic Accuracy Study Protocol
The fundamental protocol for establishing diagnostic accuracy involves comparison against the reference standard using a 2x2 contingency table approach. This methodology forms the basis for calculating essential performance metrics and should be implemented with careful attention to experimental design and execution.
Figure 1: Diagnostic Accuracy Validation Workflow
The experimental sequence begins with clear definition of the target condition and appropriate reference or composite standard. Researchers then select a representative sample cohort including both subjects with and without the target condition. The index test (new qualitative test) and reference standard test are performed independently, ideally with blinding to prevent bias. Results are then organized in a 2x2 contingency table for calculation of performance metrics.
Statistical Analysis and Performance Metrics
Fundamental Performance Calculations
The core statistical analysis for diagnostic accuracy studies centers on the 2x2 contingency table, which cross-tabulates results from the new test against the reference standard. This approach enables calculation of critical performance metrics that characterize the test's clinical utility.
Table 2: 2x2 Contingency Table and Core Performance Metrics
| Reference Standard Positive | Reference Standard Negative | Performance Metric | Calculation | |
|---|---|---|---|---|
| Test Positive | True Positive (TP) | False Positive (FP) | Sensitivity | TP/(TP+FN)×100 |
| Test Negative | False Negative (FN) | True Negative (TN) | Specificity | TN/(TN+FP)×100 |
| Positive Predictive Value | TP/(TP+FP)×100 | |||
| Negative Predictive Value | TN/(TN+FN)×100 |
These metrics provide complementary information about test performance. Sensitivity and specificity are intrinsic test characteristics that measure accuracy in diseased and healthy populations, respectively. Positive predictive value (PPV) and negative predictive value (NPV) indicate the probability that positive or negative test results correctly classify subjects, and are influenced by disease prevalence in the tested population [10].
Confidence Interval Estimation
Precision of performance estimates is determined through confidence interval calculation. For sensitivity and specificity, 95% confidence intervals can be calculated using specific formulas that account for sample size and observed proportions [10]:
Sensitivity 95% Confidence Interval:
- A1 = 2×TP+1.96²
- A2 = 1.96×(1.96²+4×TP×FN/(TP+FN))¹/²
- A3 = 2×(TP+FN+1.96²)
- Sensitivity Lower Limit = (A1-A2)/A3×100
- Sensitivity Upper Limit = (A1+A2)/A3×100
Specificity 95% Confidence Interval:
- B1 = 2×TN+1.96²
- B2 = 1.96×(1.96²+4×TN×FP/(TN+FP))¹/²
- B3 = 2×(TN+FP+1.96²)
- Specificity Lower Limit = (B1-B2)/B3×100
- Specificity Upper Limit = (B1+B2)/B3×100
These confidence intervals are essential for interpreting validation results, as they quantify the uncertainty in performance estimates due to sample size limitations. Wider intervals indicate less precise estimates and may necessitate larger validation studies for definitive conclusions.
Implementation Considerations
Regulatory and Accreditation Framework
Implementation of diagnostic accuracy criteria occurs within a well-defined regulatory framework. The FDA recognizes CLSI EP12 as a consensus standard for satisfying regulatory requirements for medical devices [3]. This recognition provides manufacturers with a clearly established pathway for preclinical evaluation of qualitative, binary output examinations before regulatory submission.
Laboratories must distinguish between verification and validation processes. Verification applies to unmodified FDA-approved or cleared tests and confirms that performance characteristics match manufacturer claims in the user's environment. Validation establishes performance for laboratory-developed tests or modified FDA-approved tests [39]. For qualitative tests, CLIA regulations require verification of accuracy, precision, reportable range, and reference range before implementing patient testing [39].
Practical Implementation Challenges
Several practical challenges emerge when implementing diagnostic accuracy criteria. Sample availability often limits validation studies, particularly for conditions with low prevalence or difficult diagnosis. Commercial panels may be necessary to obtain sufficient positive samples, but these can be expensive [10]. Imperfect reference standards present another challenge, as many conditions lack perfect diagnostic methods, necessitating careful development of composite standards.
Spectrum bias represents a particular concern, wherein test performance varies across different clinical presentations or disease stages. Validation studies should include the full spectrum of subjects who will encounter the test in clinical practice, including those with mild, moderate, and severe disease, as well as conditions that might cross-react or cause interference [10]. Blinding procedures are essential to prevent bias in interpretation of both index and reference tests, while independent interpretation ensures that results from one method do not influence the other.
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Diagnostic Accuracy Studies
| Reagent/Resource | Function in Diagnostic Accuracy Studies |
|---|---|
| Commercial Reference Panels | Provide characterized positive and negative samples with known status against reference methods |
| Quality Control Materials | Monitor assay performance throughout validation study |
| Clinical Isolates | Represent circulating strains or variants in target population |
| Archived Clinical Samples | Enable access to rare conditions or presentations |
| Interference Substances | Test assay specificity against potential cross-reactants |
| Stability Testing Materials | Assess reagent stability under various storage conditions |
Proper establishment of diagnostic accuracy criteria using reference methods and composite standards is fundamental to the validation of qualitative, binary output examinations according to CLSI EP12 guidelines. These criteria enable calculation of essential performance metrics including sensitivity, specificity, and predictive values that inform clinical utility. The recent publication of CLSI EP12's third edition provides updated frameworks for test developers and clinical laboratories to ensure reliable assessment of qualitative tests throughout the test life cycle. As qualitative diagnostics continue to evolve with advancing technologies, rigorous application of these principles will remain essential for delivering accurate, clinically useful diagnostic information to healthcare providers and patients.
Evaluating qualitative tests is a fundamental requirement in clinical laboratories and in vitro diagnostic development. The CLSI EP12 guideline provides the foundational framework for this process, specifically for examinations with binary outputs (e.g., positive/negative, present/absent) [1] [2]. A critical conceptual understanding within this framework is the distinction between assessing a test's diagnostic accuracy versus its agreement with another method. Diagnostic accuracy, expressed through sensitivity and specificity, requires comparison to an objective gold standard that definitively identifies the true disease state of a subject [40] [41]. In contrast, agreement metrics, namely Positive Percentage Agreement (PPA) and Negative Percentage Agreement (NPA), are used when a perfect gold standard is not available or not used, and the new test is compared to an existing non-reference method [21].
Confusing these concepts can lead to significant misinterpretation of a test's performance. This guide, contextualized within the CLSI EP12 protocol for qualitative test performance, will delineate the theoretical and practical differences between these metrics, provide methodologies for their calculation, and outline their proper application for researchers and drug development professionals.
Theoretical Foundations: Diagnostic Accuracy vs. Method Agreement
Diagnostic Accuracy: Sensitivity and Specificity
Sensitivity and specificity are intrinsic properties of a test that describe its validity against a gold standard. They are prevalence-independent, meaning their values do not change with the prevalence of the condition in the population being tested [41].
Sensitivity (True Positive Rate): This is the probability that a test will correctly classify an individual who has the condition as positive. It measures how well a test identifies true positives [40] [41].
Specificity (True Negative Rate): This is the probability that a test will correctly classify an individual who does not have the condition as negative. It measures how well a test identifies true negatives [40] [41].
Method Agreement: PPA and NPA
Positive Percentage Agreement (PPA) and Negative Percentage Agreement (NPA) are measures of concordance between a new test method and a comparative method (which may not be a perfect gold standard) [21].
Positive Percentage Agreement (PPA): The proportion of samples that are positive by the comparative method which also yield a positive result with the new test method [21].
- Calculation: PPA = Number of Positive Results with New Test / Number of Positive Results with Comparative Method.
Negative Percentage Agreement (NPA): The proportion of samples that are negative by the comparative method which also yield a negative result with the new test method [21].
It is crucial to understand that while the formulas for PPA and sensitivity (and for NPA and specificity) may be mathematically identical, their interpretation is fundamentally different [21]. This difference stems entirely from the nature of the comparator. PPA and NPA do not measure truth but rather consensus with a specific method. If the comparative method itself is imperfect, the agreement statistics will reflect its biases and inaccuracies. Consequently, it is not possible to infer that one test is better than another based solely on agreement statistics, as there is no way to know the true state of the subject in cases of disagreement [21]. To avoid confusion, it is recommended to consistently use the terms PPA and NPA when the comparator is not a gold standard [21].
The table below provides a clear, structured comparison of these two pairs of performance metrics.
Table 1: Core Differences Between Diagnostic Accuracy and Method Agreement Metrics
| Feature | Sensitivity & Specificity | PPA & NPA |
|---|---|---|
| Definition | Measures of diagnostic accuracy against a gold standard [40] [41]. | Measures of method agreement with a non-reference comparator [21]. |
| Comparator | Gold Standard (Best available method to determine true disease state) [40]. | Comparative Method (An existing test, which may be imperfect) [21]. |
| Interpretation | Answers: "How well does the test identify the actual truth?" | Answers: "How well does the new test agree with the existing method?" |
| Dependency | Prevalence-independent [41]. | Dependent on the performance and results of the comparative method. |
| Key Limitation | Requires a definitive, objective gold standard, which can be difficult or expensive to obtain. | Cannot determine which test is correct in cases of disagreement; does not measure truth [21]. |
Experimental Protocols and Methodologies
Adhering to standardized protocols is essential for robust test evaluation. The following methodologies are aligned with the principles of CLSI EP12 [1] [2] [10].
Protocol for Determining Sensitivity and Specificity
This protocol is based on a primary diagnostic accuracy model where the true disease status is known [10].
Sample Selection and Gold Standard:
- Select a panel of well-characterized samples. The "target condition" (disease state) for each sample must be definitively determined by the gold standard test [40].
- Samples from subjects with the disease (positive status) and without the disease (negative status) should be representative of the intended use population [10]. CLSI EP12 suggests the study be performed over 10-20 days to account for reproducibility [10].
Testing Procedure:
- Perform the new qualitative test on all samples in the panel, following the standard operating procedure.
- The personnel performing the test should be blinded to the gold standard results to prevent bias.
Data Analysis and 2x2 Contingency Table:
- Tabulate the results in a 2x2 contingency table against the gold standard.
- Calculate Sensitivity, Specificity, and their 95% confidence intervals (95% CI). The confidence interval is critical as it conveys the precision of the estimate, which is heavily influenced by the number of samples tested [10].
Table 2: 2x2 Table for Diagnostic Accuracy Calculation vs. Gold Standard
| Gold Standard: Positive | Gold Standard: Negative | |
|---|---|---|
| New Test: Positive | True Positive (TP) | False Positive (FP) |
| New Test: Negative | False Negative (FN) | True Negative (TN) |
| Calculation | Sensitivity = TP / (TP + FN) | Specificity = TN / (TN + FP) |
Protocol for Determining PPA and NPA
This protocol is used when a gold standard is not available, and the goal is to verify performance against a designated comparative method [21] [10].
Sample Selection and Comparative Method:
- Select a panel of samples that have been tested using the established comparative method. The comparative method should itself have a known and acceptable level of performance.
- The panel should include a range of samples that are positive and negative by the comparative method.
Testing Procedure:
- Perform the new qualitative test on all samples in the panel.
- Blinding of personnel to the results of the comparative method is still recommended.
Data Analysis and 2x2 Contingency Table:
- Tabulate the results in a 2x2 contingency table against the comparative method.
- Calculate PPA, NPA, and their 95% confidence intervals. It is important to note that all discrepant results (samples where the new test and comparative method do not agree) should be investigated with a confirmatory test, if possible [10].
Table 3: 2x2 Table for Method Agreement Calculation vs. Comparative Method
| Comparative Method: Positive | Comparative Method: Negative | |
|---|---|---|
| New Test: Positive | Agreement on Positive (A) | Disagreement (B) |
| New Test: Negative | Disagreement (C) | Agreement on Negative (D) |
| Calculation | PPA = A / (A + C) | NPA = D / (B + D) |
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key materials required for conducting a robust test evaluation according to CLSI EP12 principles.
Table 4: Key Research Reagent Solutions for Qualitative Test Validation
| Item | Function & Importance |
|---|---|
| Characterized Panel Samples | Well-defined samples with known status (via gold standard or comparative method). The cornerstone of the study, as the quality of the panel directly determines the validity of the results [10]. |
| Gold Standard Test Materials | Reagents and equipment for the definitive diagnostic method. Used to establish the "truth" for sensitivity/specificity studies [40]. |
| Comparative Method Test Kits | Established test kits or laboratory-developed procedures used as the benchmark for PPA/NPA studies [21]. |
| Confirmatory Test Reagents | Materials for a third, definitive test (e.g., PCR, sequencing) used to resolve discrepancies between the new test and the comparative method [10]. |
| Statistical Analysis Software | Tools for calculating performance metrics (sensitivity, specificity, PPA, NPA) and their 95% confidence intervals, which are essential for interpreting the statistical power of the study [10]. |
Decision Workflow for Metric Selection
The following diagram illustrates the logical decision process for choosing the appropriate performance metrics and experimental protocol, based on the availability of a gold standard.
Within the framework of CLSI EP12, the rigorous evaluation of qualitative, binary-output tests demands a clear understanding of the distinction between diagnostic accuracy and method agreement. Sensitivity and specificity are the metrics of choice when the objective is to measure a test's ability to discern the underlying truth, as defined by a gold standard. When such a standard is unavailable and the goal is to benchmark a new test against an existing method, PPA and NPA are the appropriate metrics for reporting concordance. Selecting the correct protocol and metrics is not merely a statistical formality; it is fundamental to generating reliable, interpretable, and regulatory-compliant data that accurately communicates the performance of a diagnostic test to the scientific community.
Protocols for Verification in the User's Laboratory Environment
Within the comprehensive framework of CLSI EP12 research, the process of verification in the user's laboratory represents a critical phase for ensuring that qualitative, binary-output tests perform as intended in their specific operational environment. The CLSI EP12 guideline, specifically the third edition published in March 2023, provides a standardized framework for this process, characterizing a target condition with only two possible outputs, such as positive/negative, present/absent, or reactive/nonreactive [1] [2]. This protocol is intended for medical laboratories implementing either manufacturer-developed tests or laboratory-developed tests (LPDs), providing a structured approach to verify examination performance claims within the user's own testing environment [1]. The verification process confirms, through the provision of objective evidence, that the specific requirements for the test's intended use have been fulfilled, with a particular focus on minimizing the risk of false results that could directly impact clinical decision-making [10].
The scope of this verification protocol encompasses binary result examinations, while explicitly excluding tests with more than two possible categories in an unordered set or those reporting ordinal categories [1]. For laboratories operating under regulatory frameworks, it is significant to note that the U.S. Food and Drug Administration (FDA) has evaluated and recognized the CLSI EP12 approved-level consensus standard for use in satisfying regulatory requirements [1].
Core Performance Characteristics for Verification
Verification of qualitative, binary-output tests requires assessment of three fundamental performance characteristics: precision, clinical agreement, and analytical specificity. The approach varies depending on the nature of the test method being verified [17].
Table 1: Performance Characteristics for Different Qualitative Test Types
| Performance Characteristic | Qualitative Test with Internal Continuous Response (ICR) | Qualitative Test with Binary Output Only | Qualitative PCR Tests |
|---|---|---|---|
| Analytical Sensitivity | Limit of Detection (LoD) or Cutoff Interval (C5 to C95) | Cutoff Interval (C5 to C95) | C95 as LoD |
| Precision | Replication Experiment | Replication Experiment | |
| Accuracy/Clinical Performance | Clinical Agreement Study | Clinical Agreement Study | Clinical Agreement Study |
| Analytical Specificity | Cross Reactivity, Interference | Cross Reactivity, Interference | Cross Reactivity, Interference |
Precision and the Imprecision Interval
For qualitative tests with an internal continuous response, precision is characterized by the uncertainty of the cutoff interval, known as the imprecision interval [17]. This interval describes the random error inherent in the binary measurement process and is defined by several key concentrations:
- C50: The concentration that yields 50% positive results, representing the medical decision level for binary classification.
- C5: The concentration at which only 5% of results are positive.
- C95: The concentration at which 95% of results are positive [17].
The range between C5 and C95 defines the imprecision interval, providing a quantitative measure of the uncertainty around the cutoff concentration. This concept is particularly relevant for tests like immunoassays and other methods where an internal continuous response is converted to a binary result using a cutoff value [17].
Clinical Agreement and Diagnostic Accuracy
Clinical agreement validates the test's ability to correctly classify samples relative to a reference method or diagnostic accuracy criteria. The key metrics for this assessment are derived from a 2x2 contingency table comparing the test under evaluation against a comparator [10].
Table 2: Clinical Agreement Metrics and Calculations
| Metric | Calculation | Explanation |
|---|---|---|
| Diagnostic Sensitivity (Se%) | TP/(TP+FN)×100 | Percentage of true positive results among subjects with the target condition |
| Diagnostic Specificity (Sp%) | TN/(TN+FP)×100 | Percentage of true negative results among subjects without the target condition |
| Positive Predictive Value (PPV%) | TP/(TP+FP)×100 | Probability that a positive result truly indicates the target condition |
| Negative Predictive Value (NPV%) | TN/(TN+FN)×100 | Probability that a negative result truly indicates absence of the target condition |
| Efficiency (E%) | (TP+TN)/n×100 | Overall percentage of correct results |
These metrics should be presented with their 95% confidence intervals to account for statistical uncertainty in the estimates, particularly when working with limited sample sizes [10] [17].
Experimental Verification Protocols
Sample Selection and Study Design
Proper sample selection is fundamental to a robust verification study. The following considerations should guide this process:
- Target Population: Patient samples should be representative of the intended use population and include both positive and negative samples [10].
- Sample Characteristics: For infectious disease testing (e.g., virology), consider variations such as agent types and subtypes, mutations, and the seronegative window period [10].
- Sample Size: The number of samples directly impacts the statistical power of the study and the width of confidence intervals. For example, with only 5 positive samples, the 95% confidence interval for sensitivity cannot be smaller than 56.6% to 100% [10].
- Study Duration: CLSI EP12 recommends performing the study over 10 to 20 days to ensure reproducibility conditions are adequately assessed, though shorter periods may be acceptable if reproducibility is demonstrated [10].
Protocol 1: Precision Verification Using Imprecision Interval
For tests with an internal continuous response, precision is verified through replication experiments that define the imprecision interval:
- Sample Preparation: Select samples with concentrations near the expected cutoff value. Include at least one low-positive sample.
- Replication Scheme: Perform repeated testing (at least 20 replicates per sample) over multiple days (5-10 days) to capture both within-run and between-day variability.
- Data Analysis: For each concentration level, calculate the proportion of positive results.
- Interval Determination: Plot the proportion of positive results against concentration and determine C5, C50, and C95 concentrations through logistic regression or probit analysis.
- Acceptance Criteria: Verify that the imprecision interval (C5 to C95) falls within manufacturer claims or predetermined specifications [17].
Protocol 2: Clinical Agreement Study
The clinical agreement study validates the test's ability to correctly classify samples relative to a reference method:
Comparator Selection:
- Primary Design: Use diagnostic accuracy criteria as the comparator when possible.
- Secondary Design: Use an existing test with established performance characteristics when diagnostic accuracy criteria are unavailable [10].
Testing Procedure:
- Test all selected samples with both the method under evaluation and the comparator method.
- Ensure testing is performed under reproducibility conditions, with operators blinded to the comparator results.
Data Analysis:
- Construct a 2x2 contingency table comparing results.
- Calculate sensitivity, specificity, predictive values, and efficiency.
- Compute 95% confidence intervals for sensitivity and specificity using appropriate statistical methods [10].
- Discrepant Analysis: Resolve any discrepant results between methods using a third, definitive method if available.
Protocol 3: Interference and Cross-Reactivity Testing
Analytical specificity is verified through interference and cross-reactivity studies:
Interference Testing:
- Select potentially interfering substances based on the test system and patient population (e.g., hemolyzed, icteric, or lipemic samples).
- Test samples with and without the interfering substance.
- Compare results to detect any false positives or negatives caused by the interferent.
Cross-Reactivity Testing:
- Identify structurally similar compounds or analytes that might cause false-positive results.
- Test samples containing these potentially cross-reacting substances.
- Verify that cross-reactivity does not exceed acceptable limits [17].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential Materials for Verification Studies
| Reagent/Material | Function in Verification Protocol |
|---|---|
| Commercial Reference Panels | Provides characterized samples with known status when natural clinical samples are scarce or difficult to characterize [10] |
| Commutable Processed Samples | Maintains characteristics similar to native patient samples when used in comparison studies [9] |
| Interference Kits | Standardized materials for evaluating effects of common interferents (hemoglobin, bilirubin, lipids) [17] |
| Stability Materials | Reagents and materials for evaluating reagent stability over time [1] |
| Statistical Software | Tools for calculating performance metrics, confidence intervals, and generating receiver operating characteristic (ROC) curves [9] |
Data Analysis and Interpretation
Statistical Analysis of Binary Data
The binary nature of qualitative test results requires specialized statistical approaches:
- Confidence Interval Calculation: For sensitivity and specificity, use the Clopper-Pearson exact or Wilson score methods for calculating confidence intervals [9]. These methods provide robust interval estimates for proportion data.
- Sample Size Considerations: The number of samples directly affects the precision of estimates. Smaller sample sizes yield wider confidence intervals, reducing the statistical power to detect meaningful differences in performance [10].
- Example Calculation: As illustrated in a case study, with 24 true positives and 0 false negatives, sensitivity is 100% with a 95% confidence interval of 86% to 100%. Similarly, with 94 true negatives and 2 false positives, specificity of 98.1% has a confidence interval of 93% to 99% [10].
Acceptance Criteria and Decision Making
Establish predefined acceptance criteria based on:
- Manufacturer's Claims: For commercially developed tests.
- Intended Use: Considering the clinical context and consequences of false results.
- Regulatory Requirements: Meeting guidelines from relevant authorities.
When interpreting results, consider both the point estimates (e.g., sensitivity, specificity) and their confidence intervals. The verification is successful only if both the point estimates and the confidence intervals meet the predefined acceptance criteria [10].
The verification of qualitative, binary-output tests in the user's laboratory environment represents a critical quality assurance process within the comprehensive CLSI EP12 framework. By implementing structured protocols for assessing precision, clinical agreement, and analytical specificity, laboratories can ensure that these tests perform reliably in their specific operational context. The experimental approaches outlined—including imprecision interval characterization, clinical agreement studies with proper statistical analysis, and interference testing—provide a robust methodology for verifying test performance. As the field of laboratory medicine continues to evolve, with new technologies and applications emerging, these verification protocols remain fundamental to maintaining test quality and, ultimately, ensuring optimal patient care.
In the clinical laboratory, the evaluation of qualitative, binary-output tests—which yield results such as positive/negative or present/absent—requires a distinct approach compared to quantitative assays. The Clinical and Laboratory Standards Institute (CLSI) EP12 guideline, titled "Evaluation of Qualitative, Binary Output Examination Performance," provides the foundational framework for designing and analyzing studies to verify the performance of these tests [1]. This document establishes protocols for both manufacturers developing new tests and laboratories verifying performance at the point of use, ensuring reliability and accuracy in clinical decision-making [1].
The current third edition of EP12, published in March 2023, represents a significant evolution from the previous EP12-A2 version. It expands the types of procedures covered to reflect advances in laboratory medicine and incorporates additional protocols for examination procedure design, validation, and verification [1]. Furthermore, it adds topics such as stability and interferences to the existing coverage of precision and clinical performance assessment [1]. For researchers and drug development professionals, understanding this guideline is essential for conducting compliant and scientifically rigorous comparative method studies.
Categorizing Qualitative Examination Types
Not all qualitative tests operate on the same principle. Understanding their fundamental design is crucial for selecting appropriate validation protocols. The CLSI EP12 guideline categorizes binary-output examinations based on their underlying measurement process, with each category requiring specific validation approaches [17].
The table below outlines the primary categories of qualitative tests and their key characteristics:
Table 1: Categories of Qualitative, Binary-Output Examinations
| Test Category | Internal Response | Result Conversion | Common Examples | Key Performance Focus |
|---|---|---|---|---|
| Qualitative with Internal Continuous Response (ICR) | Continuous numerical signal | Compared to a cutoff value to yield binary result | Immunoassays (ELISA), some chemistry tests | Cutoff interval (C5-C95), precision near cutoff |
| Pure Qualitative Binary Output | Direct binary readout | No conversion; result is intrinsically binary | Lateral flow assays, agglutination tests | Clinical agreement, direct proportion of positive results |
| Qualitative with Discontinuous Internal Response | Discrete numerical values (e.g., Ct values) | Interpreted relative to a decision threshold | PCR and other molecular amplification methods | Limit of Detection (LoD), clinical agreement |
Tests with an Internal Continuous Response (ICR) generate a numerical signal (e.g., optical density, luminescence) that is compared against a predetermined cutoff value to classify the result as positive or negative [17]. In contrast, pure qualitative tests produce a binary result directly without an intermediate numerical value [10]. Qualitative PCR tests represent a hybrid category, generating discontinuous internal numerical data (Cycle threshold, Ct) that is interpreted against a threshold to yield a binary outcome [17].
The following diagram illustrates the operational workflow for these different test categories:
Core Performance Characteristics and Evaluation Protocols
The evaluation of qualitative tests focuses on three core performance characteristics: precision (analytical sensitivity), accuracy (clinical agreement), and analytical specificity. The experimental protocols for assessing these characteristics differ significantly from those used for quantitative methods.
Precision and the Imprecision Interval (C5-C95)
For qualitative tests, precision is not expressed as a standard deviation but is characterized by the imprecision interval around the medical decision point, particularly for tests with an internal continuous response [17]. This interval describes the range of analyte concentrations where the test result becomes uncertain due to random analytical variation.
The key parameters of the imprecision interval are:
- C50: The analyte concentration at which 50% of test results are positive. This represents the effective cutoff or medical decision level [17].
- C5 and C95: The concentrations at which 5% and 95% of results are positive, respectively. The range between C5 and C95 (the imprecision interval) defines the concentration range where the test transitions from consistently negative to consistently positive results [17].
A narrower imprecision interval indicates better test precision, as the transition from negative to positive results occurs over a smaller concentration range. The experimental protocol for determining this interval involves testing samples with concentrations spanning the expected cutoff value in multiple replicates (CLSI EP12 recommends 40-60 replicates per sample) and plotting the proportion of positive results versus concentration [17].
Clinical Agreement Studies (Accuracy)
Accuracy for qualitative tests is established through clinical agreement studies that compare the new test's results to those from a reference method or diagnostic accuracy criteria [17] [10]. The data from these studies are typically presented in a 2x2 contingency table and analyzed using measures of diagnostic accuracy.
Table 2: Metrics for Assessing Clinical Agreement in Qualitative Tests
| Metric | Calculation | Interpretation | Application Context |
|---|---|---|---|
| Diagnostic Sensitivity (Se%) | (TP/(TP+FN))×100 | Probability the test is positive when the target condition is present | Critical for ruling out disease; high value minimizes false negatives |
| Diagnostic Specificity (Sp%) | (TN/(TN+FP))×100 | Probability the test is negative when the target condition is absent | Critical for ruling in disease; high value minimizes false positives |
| Positive Predictive Value (PPV%) | (TP/(TP+FP))×100 | Probability the target condition is present when the test is positive | Highly dependent on disease prevalence |
| Negative Predictive Value (NPV%) | (TN/(TN+FN))×100 | Probability the target condition is absent when the test is negative | Highly dependent on disease prevalence |
| Overall Efficiency (E%) | ((TP+TN)/n)×100 | Proportion of all tests that yield correct results | Overall measure of correctness |
The experimental protocol requires testing a sufficient number of well-characterized clinical samples that represent the intended patient population [10]. The study should be conducted over 10-20 days to account for daily analytical variations [10]. When the comparator is other than the diagnostic accuracy criteria (e.g., a marketed test), all discrepant results should be resolved using a confirmatory method [10].
Analytical Specificity: Interference and Cross-Reactivity
Analytical specificity refers to a test's ability to measure only the target analyte without interference from other substances that might be present in the sample [17]. Evaluation involves two primary approaches:
- Interference Studies: Testing samples containing potentially interfering substances (e.g., hemoglobin, bilirubin, lipids, common medications) to determine if they affect the test result.
- Cross-Reactivity Studies: For tests detecting specific analytes like infectious agents, evaluating reactivity with structurally similar organisms or analytes that could cause false-positive results.
The experimental design should include testing samples with and without potential interferents at clinically relevant concentrations [17]. The FDA's Emergency Use Authorization (EUA) requirements for COVID-19 tests highlighted the importance of demonstrating class specificity for tests distinguishing between different antibody classes (e.g., IgM and IgG) [17].
Experimental Design and Statistical Analysis
Sample Selection and Sizing
Appropriate sample selection is critical for meaningful validation results. Samples should represent the target population and include relevant pathological conditions that might be encountered in clinical practice [10]. For infectious disease tests, this includes consideration of agent types, subtypes, potential mutations, and the seronegative window period [10].
The number of samples directly impacts the statistical power and precision of estimates. Smaller sample sizes yield wider confidence intervals, reducing confidence in the performance estimates. For example, with only 5 positive samples, the 95% confidence interval for sensitivity could range from 56.6% to 100%, regardless of the point estimate [10]. CLSI EP12 provides guidance on appropriate sample sizes for validation studies, though practical considerations often influence the final number.
Statistical Analysis of Binary Data
The binary nature of qualitative test results requires specialized statistical approaches. Proportions (e.g., sensitivity, specificity) should be reported with their 95% confidence intervals to communicate the precision of the estimate [17] [10]. The confidence interval for a proportion can be calculated using appropriate statistical methods, such as the Wilson score interval or the Clopper-Pearson exact method [10].
For tests with an internal continuous response, traditional quantitative statistics (mean, standard deviation) can be applied to the internal signal, while the binary classification is analyzed using proportion-based methods [17]. This dual approach provides a more comprehensive understanding of test performance.
The following workflow outlines the key decision points in designing a comparative method study for qualitative tests:
The Scientist's Toolkit: Essential Research Reagent Solutions
The successful execution of comparative method studies requires careful selection of reagents and materials. The following table details key research reagent solutions and their functions in qualitative test evaluation:
Table 3: Essential Research Reagent Solutions for Qualitative Test Evaluation
| Reagent/Material | Function in Evaluation | Key Considerations |
|---|---|---|
| Characterized Clinical Panels | Serve as test samples for clinical agreement studies; may include positive, negative, and borderline samples | Well-characterized using reference method; appropriate matrix; covers clinical range of targets |
| Commercial Performance Panels | Provide difficult-to-source specimens (e.g., infected samples, rare markers) | Traceability to reference methods; stability data; commutability with native patient samples |
| Interference Test Kits | Standardized materials for assessing analytical specificity | Clinically relevant concentrations of interferents; prepared in appropriate matrix |
| Cross-Reactivity Panels | Evaluate assay specificity against structurally similar organisms or analytes | Includes common cross-reactants; appropriate viability/purity |
| Stability Study Materials | Assess reagent and sample stability under various storage conditions | Multiple lots; proper documentation of storage conditions and timepoints |
| Calibrators and Controls | Ensure proper test system operation throughout validation | Traceable to reference standards; cover clinically relevant concentrations including cutoff |
Regulatory and Accreditation Considerations
Compliance with regulatory requirements and accreditation standards is essential when implementing qualitative tests. The U.S. Food and Drug Administration (FDA) has formally recognized CLSI EP12 as a consensus standard for satisfying regulatory requirements [1]. This recognition underscores the importance of adhering to this guideline for test developers and manufacturers.
Laboratories must also comply with requirements from accreditation bodies such as the College of American Pathologists (CAP) and standards such as ISO 15189 and ISO 17025 [6]. These require verification of precision, accuracy, and method comparison when replacing an existing method with a new one [6]. For FDA-cleared tests, verification typically includes accuracy, precision, and method comparison, while for laboratory-developed tests (LDTs) or modified tests, more extensive validation establishing diagnostic sensitivity and specificity is required [6].
The evolution of regulatory expectations was particularly evident during the COVID-19 pandemic, where Emergency Use Authorizations initially emphasized clinical agreement studies, with increasing demands for more comprehensive validation data as the emergency phase progressed [17].
Comparative method studies for qualitative tests require a specialized approach distinct from quantitative method validation. The CLSI EP12 guideline provides a comprehensive framework for designing and executing these studies, with a focus on precision expressed as an imprecision interval (C5-C95), accuracy determined through clinical agreement studies (sensitivity, specificity), and analytical specificity assessed through interference and cross-reactivity testing. As qualitative technologies continue to evolve, adhering to these evidence-based protocols ensures that laboratory professionals, researchers, and drug developers can reliably verify test performance, ultimately supporting accurate clinical decision-making and patient care.
Assessing Cross-Reactivity and Interference for Analytical Specificity
Within the comprehensive framework of the CLSI EP12 protocol for evaluating qualitative test performance, establishing analytical specificity is a critical pillar. Analytical specificity refers to a method's ability to accurately detect the target analyte without interference from cross-reacting substances or other confounding factors present in the sample matrix. For developers and users of qualitative, binary-output examinations—which yield results such as positive/negative or present/absent—a rigorous assessment of cross-reactivity and interference is non-negotiable for ensuring result reliability. This guide details the experimental protocols and methodological considerations for this essential validation activity, contextualized within the broader requirements of the CLSI EP12-A2 standard and its subsequent third edition [1] [2].
Analytical Specificity within the CLSI EP12 Framework
The CLSI EP12 guideline provides a structured framework for the evaluation of qualitative test performance, covering precision, clinical agreement, and analytical specificity [1] [17]. The third edition of EP12, published in 2023, expands upon its predecessors by adding protocols for the design and development stages of tests, and by incorporating topics like stability and interferences more explicitly into the performance evaluation [1] [2].
The Role of Specificity in Test Performance
For a qualitative test, analytical specificity is demonstrated through two primary types of studies:
- Cross-reactivity Studies: Assessing whether structurally similar or taxonomically related substances cause a false-positive signal.
- Interference Studies: Assessing whether common endogenous or exogenous substances affect the detection of the target analyte, leading to either false-positive or false-negative results.
These studies are a regulatory requirement for laboratory-developed tests (LDTs) under the Clinical Laboratory Improvement Amendments (CLIA) [32]. While the CLSI EP12 guideline itself is recognized by the U.S. Food and Drug Administration (FDA), the specific protocols for establishing these performance characteristics are foundational for both manufacturers and clinical laboratories creating LDTs [1].
Experimental Protocols
A robust experimental design is crucial for generating defensible data on analytical specificity. The following protocols outline the key steps for conducting cross-reactivity and interference studies.
Protocol for Cross-Reactivity Assessment
The goal of this protocol is to challenge the test system with substances that are potentially cross-reactive to ensure they do not produce a false-positive result.
1. Identify Potential Cross-Reactants:
- Compile a list of substances that are structurally similar to the target analyte, genetically related organisms (for infectious disease tests), or substances known to be present in the intended patient population that could cause cross-reactivity. For an antibiotic test, this could include metabolites or drugs from the same class [32].
2. Source and Prepare Test Samples:
- Obtain purified forms of the cross-reactants. Prepare test samples by spiking a negative sample matrix (e.g., pooled human plasma, serum) with a high concentration of each potential cross-reactant. The concentration should exceed the level expected physiologically or pathologically in clinical samples [17] [32].
- A negative control (matrix only) and a positive control (matrix with the target analyte at a low concentration, e.g., near the cutoff) should be included in every run.
3. Testing and Data Analysis:
- Test each cross-reactant sample, the negative control, and the positive control in a sufficient number of replicates (CLSI recommends a minimum of 2-3 replicates, though larger studies may be needed for statistical confidence) [32].
- A sample is considered non-cross-reactive if all replicates yield a negative result. Any positive result warrants further investigation to determine the threshold for cross-reactivity.
Protocol for Interference Assessment
This protocol evaluates the effect of interfering substances on the accurate detection of the target analyte, both at low positive and negative concentrations.
1. Select Interfering Substances:
- Choose substances commonly encountered in patient samples. Key endogenous interferents include hemoglobin (from hemolysis), bilirubin (icterus), and lipids (lipemia) [32]. Exogenous interferents can include common drugs (e.g., anticoagulants, analgesics), vitamins, or nutritional supplements.
2. Prepare Test Samples:
- Prepare a panel of samples in the appropriate clinical matrix:
- Low Positive Sample: Contains the target analyte at a concentration slightly above the assay's limit of detection (LoD) or clinical cutoff.
- Negative Sample: Contains no target analyte.
- For each of these base pools, create aliquots that are:
- Spiked with a high concentration of the interferent.
- Spiked with an equivalent volume of the interferent's solvent (as a control).
- The concentration of the interferent should be at the high end of what is clinically relevant [32].
3. Testing and Data Analysis:
- Test the interferent-spiked samples and their corresponding controls in multiple replicates (e.g., in duplicate over multiple runs) [32].
- Use paired statistical analyses (e.g., a paired-difference t-test) to compare the results of the interferent-containing samples with their controls [32].
- For binary output tests, the outcome is the proportion of positive results. A significant difference in the positivity rate between the interferent sample and its control indicates interference.
The following diagram illustrates the core experimental workflow for assessing interference.
Data Presentation and Analysis
The data generated from specificity studies should be summarized clearly to facilitate interpretation and reporting.
Table 1: Example Cross-Reactivity Testing Results for a Hypothetical SARS-CoV-2 Antigen Test
| Potential Cross-Reactant | Concentration Tested | Test Result (Positive/Negative) | Conclusion |
|---|---|---|---|
| Human Coronavirus 229E | 1.0 x 10âµ TCIDâ‚…â‚€/mL | Negative | No cross-reactivity |
| Human Coronavirus OC43 | 1.0 x 10âµ TCIDâ‚…â‚€/mL | Negative | No cross-reactivity |
| Influenza A (H1N1) | 1.0 x 10âµ TCIDâ‚…â‚€/mL | Negative | No cross-reactivity |
| MERS-CoV | 1.0 x 10â´ TCIDâ‚…â‚€/mL | Negative | No cross-reactivity |
| Negative Control | N/A | Negative | Valid Run |
| Positive Control | ~C95 of the assay | Positive | Valid Run |
TCIDâ‚…â‚€: 50% Tissue Culture Infective Dose
Table 2: Example Interference Testing Results for a Hypothetical Cardiac Troponin I Qualitative Assay
| Sample Type | Interferent | Concentration | n/N (%) Positive | Control n/N (%) Positive | Conclusion |
|---|---|---|---|---|---|
| Low Positive | Hemoglobin (Hemolysis) | 500 mg/dL | 19/20 (95%) | 20/20 (100%) | No significant interference |
| Low Positive | Bilirubin (Icterus) | 20 mg/dL | 18/20 (90%) | 20/20 (100%) | No significant interference |
| Low Positive | Intralipids (Lipemia) | 3000 mg/dL | 5/20 (25%) | 20/20 (100%) | Significant interference |
| Negative | Hemoglobin (Hemolysis) | 500 mg/dL | 0/20 (0%) | 0/20 (0%) | No interference |
| Negative | Bilirubin (Icterus) | 20 mg/dL | 0/20 (0%) | 0/20 (0%) | No interference |
| Negative | Intralipids (Lipemia) | 3000 mg/dL | 0/20 (0%) | 0/20 (0%) | No interference |
n/N: Number of positive replicates / Total number of replicates
The Scientist's Toolkit: Key Research Reagent Solutions
The following table catalogues essential materials and reagents required for executing the described experimental protocols.
Table 3: Essential Research Reagents for Specificity Testing
| Item | Function and Description |
|---|---|
| Characterized Clinical Matrix | A well-defined, analyte-negative pooled sample (e.g., serum, plasma, urine) used as the base for preparing all spiked samples. It ensures the experimental conditions mimic the clinical setting. |
| Purified Target Analyte | The highly purified substance of interest used to prepare positive control samples and low-positive pools for interference testing. |
| Purified Cross-Reactants | Structurally similar or related substances in purified form, used to challenge the assay and evaluate potential for false-positive results. |
| Interference Stocks | Prepared solutions of common interferents: Hemolysate (hemoglobin), Bilirubin, Lipid Emulsions (e.g., Intralipid), and common medications. |
| Reference Material | Certified standard with a known concentration of the analyte, used for calibrating spiking procedures and verifying sample concentrations. |
Regulatory and Strategic Considerations
In the context of CLIA regulations, establishing analytical specificity is a mandatory step for laboratory-developed tests [32]. While CLSI EP12 provides the methodological framework, the ultimate responsibility lies with the laboratory director to ensure the clinical utility and analytical validity of the tests performed [32].
The strategic design of specificity studies should be risk-based. The selection of cross-reactants and interferents should be guided by the test's intended use, the patient population, and known limitations of the technology. Furthermore, it is critical to note that while this guide is framed within the context of CLSI EP12-A2, this version has been superseded by the third edition, EP12-Ed3 [1] [2]. The current edition offers expanded coverage, including protocols for modern techniques like next-generation sequencing and PCR-based assays, and incorporates stability assessment more fully into the evaluation process [2].
Conclusion
The CLSI EP12 framework provides an indispensable, standardized approach for evaluating qualitative binary tests, ensuring reliability from initial development through laboratory implementation. Mastering its protocols for precision, clinical agreement, and interference testing is crucial for generating trustworthy yes/no results in clinical diagnostics and drug development. As laboratory medicine advances with new technologies like next-generation sequencing, the principles outlined in EP12 will continue to form the bedrock of robust test validation. Future directions will likely involve adapting these core principles to increasingly complex assay formats while maintaining the rigorous statistical foundation that defines the standard, ultimately driving improvements in diagnostic accuracy and patient safety across biomedical research.
References
- 1. EP12 | Evaluation of Qualitative, Binary Output ... [https://clsi.org/shop/standards/ep12/]
- 2. CLSI EP12 3rd Ed. on Qualitative Testing | News [https://clsi.org/about/news/clsi-publishes-the-third-edition-of-ep12-evaluation-of-qualitative-binary-output-examination-performance/]
- 3. Recognized Consensus Standards: Medical Devices - FDA [https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfStandards/detail.cfm?standard__identification_no=44491]
- 4. EP12IG | Verification of Performance of a Qualitative, ... [https://clsi.org/shop/standards/ep12ig/]
- 5. Verifying Performance Claims for Medical Laboratory Tests [https://clsi.org/resources/insights/verifying-performance-claims-for-medical-laboratory-tests/]
- 6. Evaluation of analytical performance of qualitative and ... [https://www.sciencedirect.com/science/article/abs/pii/S0009898119319552]
- 7. EP12-A - User Protocol for Evaluation of Qualitative Test Performance; Approved Guideline [https://webstore.ansi.org/standards/clsi/ep12]
- 8. CLSI EP12-A2 | AIA Store [https://store.accuristech.com/aia/standards/clsi-ep12-a2?product_id=1533987]
- 9. Analyse-it® Method Validation Edition [https://analyse-it.com/products/method-validation]
- 10. Basic validation of qualitative tests [https://www.westgard.com/lessons/basic-method-validation/validating-qualitative-tests.html]
- 11. How to compare sensitivity and specificity in in vitro diagnostic ... [https://operondx.com/how-to-compare-sensitivity-and-specificity-in-in-vitro-diagnostic-tests/]
- 12. How to compare qualitative tests - essential tips for running ... [https://finbiosoft.com/method-comparison-diagnostic-accuracy-sensitivity-specificity/]
- 13. Division of Standards and Conformity Assessment [https://www.fda.gov/medical-devices/premarket-submissions-selecting-and-preparing-correct-submission/division-standards-and-conformity-assessment]
- 14. CLSI EP12-A2 - User Protocol for Evaluation of Qualitative ... [https://webstore.ansi.org/standards/clsi/clsiep12a2?srsltid=AfmBOooZwp3X4VRKPClOxsySTKDGBgYs2jU0RTnZs7WkGGkIYWOP1P0d]
- 15. Recognized Consensus Standards: Medical Devices [https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfstandards/search.cfm]
- 16. Establishing the Performance Characteristics of In Vitro ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/establishing-performance-characteristics-in-vitro-diagnostic-devices-detection-or-detection-and]
- 17. True or False? You can validate a qualitative method [https://www.westgard.com/lessons/basic-method-validation/performance-validation-qualitative-methods.html]
- 18. : 2ED 2008 user Clsi for evaluation of qualitative t EP 12 A 2 protocol [https://www.intertekinform.com/en-us/standards/clsi-ep12-a2-2ed-2008-357288_saig_clsi_clsi_813905/]
- 19. Quality and Performance of Papanicolaou Test using the Clinical and... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10305902/]
- 20. CLSI EP12-A2 - User Protocol for Evaluation of Qualitative ... [https://webstore.ansi.org/standards/clsi/clsiep12a2?srsltid=AfmBOor3jqi4qD6rT7-RijSTUdur_s70FTmzBRdLR3thzT-zD71bo9A3]
- 21. Diagnostic accuracy (sensitivity/specificity) versus ... [https://analyse-it.com/blog/2020/4/diagnostic-accuracy-sensitivity-specificity-versus-agreement-ppa-npa-statistics]
- 22. Sensitivity and Specificity or Positive and Negative Percent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5654895/]
- 23. Estimating Clinical Agreement for a Qualitative Test [https://www.westgard.com/lessons/basic-method-validation/qualitative-test-clinical-agreement.html]
- 24. Eurachem/CITAC Guide “Assessment of Performance and ... [https://www.mdpi.com/2305-6703/2/2/14]
- 25. Probit Analysis, Part One - Basic Method Validation [https://www.westgard.com/lessons/basic-method-validation/probit-part-one.html]
- 26. Quantitative PCR 2025-2033 Trends and Competitor ... [https://www.datainsightsmarket.com/reports/quantitative-pcr-1170480]
- 27. Methods for comparing multiple digital PCR experiments [https://pmc.ncbi.nlm.nih.gov/articles/PMC4983647/]
- 28. Digital PCR and Real-time PCR(qPCR) 2025-2033 Analysis [https://www.marketreportanalytics.com/reports/digital-pcr-and-real-time-pcrqpcr-314646]
- 29. CLSI EP12-A2 - User Protocol for Evaluation of Qualitative ... [https://webstore.ansi.org/standards/clsi/clsiep12a2?srsltid=AfmBOopd8Fl1UQGFgWzUpnFWK4U25nou0_kXqmTB3pAcriK2QeKZ2nlf]
- 30. Quality and Performance of Papanicolaou Test using the ... [https://pubmed.ncbi.nlm.nih.gov/37388397/]
- 31. CLSI EP12-A2 - User Protocol for Evaluation of Qualitative ... [https://webstore.ansi.org/standards/clsi/clsiep12a2?srsltid=AfmBOoqxoH1mc_orFlVttvW2pV2qqjLZxjofWvZ8E-qqpifi79n-zYCN]
- 32. Validation of Laboratory-Developed Molecular Assays for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2901657/]
- 33. Sample size, power and effect size revisited: simplified and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7745163/]
- 34. Sample size, power and effect size revisited: simplified ... [https://www.biochemia-medica.com/en/journal/31/1/10.11613/BM.2021.010502/fullArticle]
- 35. 12 Sample size & power [https://www.bristol.ac.uk/medical-school/media/rms/red/12_sample_size__power.html]
- 36. Atypical Squamous Cells of Undetermined Significance - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK557739/]
- 37. ASC-H (cytology) - Cervix [https://www.pathologyoutlines.com/topic/cervixASCH.html]
- 38. CLSI EP12-A2 - User Protocol for Evaluation of Qualitative ... [https://webstore.ansi.org/standards/clsi/clsiep12a2?srsltid=AfmBOoo1ZGRx-Gcekin3ADVs6A5cNT1hVH4EV2m54hBb44w4A8xLACag]
- 39. Planning a Method Verification Study in Clinical ... [https://asm.org/articles/2022/january/planning-a-method-verification-study-in-clinical-m?sr_id=23df675c-421d-4816-a54e-4d751ba62574&sr_pos=3]
- 40. Understanding and using sensitivity, specificity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2636062/]
- 41. Sensitivity and specificity [https://en.wikipedia.org/wiki/Sensitivity_and_specificity]