ISO 16140 Method Verification: The Complete Guide for Pharmaceutical and Clinical Research Professionals
This guide provides researchers, scientists, and drug development professionals with a comprehensive understanding of the ISO 16140 series for microbiological method validation and verification.
ISO 16140 Method Verification: The Complete Guide for Pharmaceutical and Clinical Research Professionals
Abstract
This guide provides researchers, scientists, and drug development professionals with a comprehensive understanding of the ISO 16140 series for microbiological method validation and verification. Covering foundational principles, practical implementation protocols, troubleshooting strategies, and validation frameworks, it addresses the critical need for standardized methods in pharmaceutical and clinical research. The content explores the distinct roles of method validation and verification, detailing the multi-stage processes outlined in ISO 16140 standards to ensure method reliability, regulatory compliance, and robust quality control in biomedical applications.
Understanding ISO 16140: Core Principles and Scope for Pharmaceutical Applications
The ISO 16140 series of international standards provides a critical framework for the validation and verification of microbiological methods used throughout the food and feed chains. These standards are designed to assist food and feed testing laboratories, test kit manufacturers, competent authorities, and food and feed business operators in implementing reliable microbiological methods that ensure the safety and quality of products [1]. The series establishes standardized protocols that help laboratories demonstrate their technical competence and generate reliable, reproducible results, which is particularly important in regulatory compliance and international trade.
Within the context of method verification standards, the ISO 16140 series creates a harmonized approach for confirming that analytical methods are fit for their intended purpose. The standards outline a two-stage process that must be completed before a method can be used routinely in a laboratory: first, proving that the method itself is fit for purpose (validation), and second, demonstrating that the laboratory can properly perform the method (verification) [1]. This structured approach provides confidence in microbiological test results that impact public health decisions.
The Structure of the ISO 16140 Series
The ISO 16140 series consists of seven distinct parts, each addressing specific aspects of method validation and verification. The development of this series represents a significant advancement in standardizing microbiological method evaluation, with each part serving a unique role in the overall ecosystem of method qualification. The following table provides a comprehensive overview of all seven parts and their specific scopes and applications.
Table: Overview of the ISO 16140 Parts and Their Specific Roles
| Standard Part | Title | Primary Focus and Application |
|---|---|---|
| ISO 16140-1 | Vocabulary | Defines terms and principles used throughout the series to ensure consistent interpretation [1]. |
| ISO 16140-2 | Protocol for the validation of alternative (proprietary) methods against a reference method | Core standard for validating commercial alternative methods; includes method comparison and interlaboratory study protocols [1]. |
| ISO 16140-3 | Protocol for the verification of reference methods and validated alternative methods in a single laboratory | Guides laboratories in demonstrating competence with validated methods before implementation [1]. |
| ISO 16140-4 | Protocol for method validation in a single laboratory | Validates methods within one laboratory without interlaboratory study; results apply only to that laboratory [1]. |
| ISO 16140-5 | Protocol for factorial interlaboratory validation for non-proprietary methods | Validates non-proprietary methods requiring rapid validation or when fewer laboratories are available [1]. |
| ISO 16140-6 | Protocol for the validation of alternative (proprietary) methods for microbiological confirmation and typing procedures | Validates confirmation procedures (e.g., biochemical confirmation) and typing techniques (e.g., serotyping) [1]. |
| ISO 16140-7 | Protocol for the validation of identification methods of microorganisms | Validates identification methods (e.g., PCR, DNA sequencing, mass spectrometry) where no reference method exists [1]. |
The relationships between the different parts of the standard are strategically designed to guide users in selecting the appropriate protocol based on their specific needs. According to the Introduction of parts 3, 4, and 5, a flow chart is provided that illustrates the links between the different parts of the ISO 16140 series and helps users select the right part based on the purpose of their study [1].
Core Concepts: Validation vs. Verification
A fundamental understanding of the ISO 16140 series requires a clear distinction between method validation and method verification, two related but distinct processes that are often confused.
Method Validation
Method validation is the primary process for proving that a method is fit for its intended purpose [1]. It answers the question: "Does this method work consistently and reliably to detect or quantify the target microorganism?" Validation is typically conducted through:
- A method comparison study where the alternative method is compared against a reference method, usually performed by one laboratory [1].
- An interlaboratory study that demonstrates the method's performance across multiple laboratories [1].
For alternative methods, ISO 16140-2 serves as the base standard, requiring both a method comparison study and an interlaboratory study [1]. The data generated during validation provides potential end-users with performance data for a given method, enabling informed decisions about implementation.
Method Verification
Method verification is the process where a laboratory demonstrates that it can satisfactorily perform a validated method [1]. It answers the question: "Can our laboratory successfully implement this validated method and obtain the expected results?" Verification applies only to methods that have been validated using an interlaboratory study and is described in ISO 16140-3 [1].
ISO 16140-3 outlines two distinct stages of verification:
- Implementation verification: The laboratory demonstrates it can perform the method correctly by testing one of the same items evaluated in the validation study [1].
- Item verification: The laboratory demonstrates capability in testing challenging food items within its scope of accreditation by testing several such items and confirming performance characteristics [1].
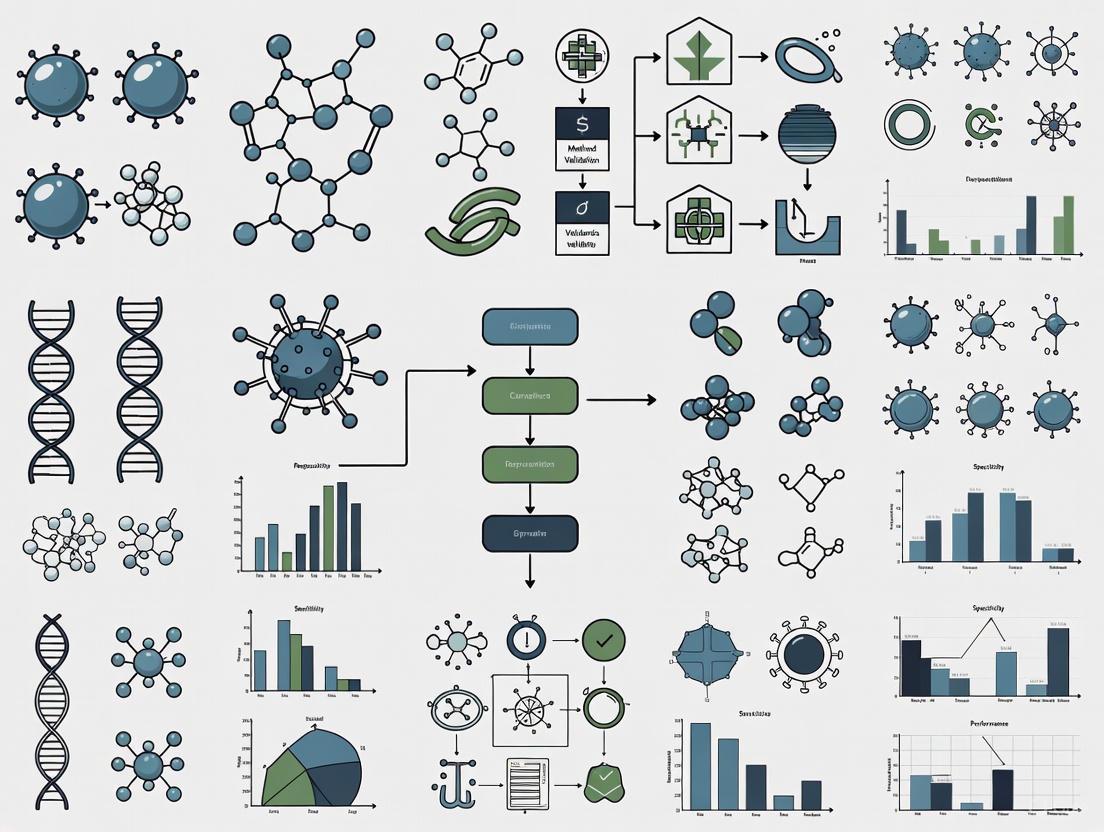
Diagram: Method Validation and Verification Workflow in ISO 16140
Detailed Examination of Each Part
ISO 16140-1: Vocabulary
As the foundational document of the series, ISO 16140-1 establishes the terminology and definitions used throughout the remaining parts. This standardization of language is critical for ensuring consistent interpretation and implementation across different stakeholders, including testing laboratories, kit manufacturers, and regulatory authorities. Without this common vocabulary, the technical requirements and performance criteria outlined in subsequent parts could be subject to varying interpretations, potentially compromising the reliability of method validation and verification studies.
ISO 16140-2: Validation of Alternative Methods
ISO 16140-2 represents the core validation standard for alternative (typically proprietary) microbiological methods against reference methods. This part includes comprehensive protocols for both qualitative and quantitative method validation, consisting of two mandatory phases: the method comparison study and the interlaboratory study [1]. The standard has recently been updated with Amendment 1 (published in September 2024), which introduced new calculations for qualitative method evaluation and the Relative Limit of Detection (RLOD) of the interlaboratory study [1]. A significant addition in this amendment addresses the validation of methods for commercial sterility testing for specific products like sterilized or UHT dairy and plant-based liquid products [1].
The data generated through ISO 16140-2 validation provides potential end-users with comprehensive performance data for a given method, enabling informed choices about implementation. These data also serve as the basis for certification of alternative methods by independent organizations, a process that also includes evaluation of the quality control during the method's manufacturing [1].
ISO 16140-3: Method Verification in a Single Laboratory
ISO 16140-3 provides the protocol for laboratories to verify that they can competently implement methods that have already been validated through an interlaboratory study (such as those validated according to ISO 16140-2) [1]. This standard is particularly important for laboratories accredited to ISO/IEC 17025, as they are required to perform verification of validated methods before implementation [2]. Even in non-accredited laboratories, verification following ISO 16140-3 is considered a best practice [2].
The verification process in ISO 16140-3 consists of two sequential stages:
- Implementation verification confirms that the user laboratory can perform the method correctly by testing one of the same items evaluated in the validation study [1].
- Item verification demonstrates that the laboratory can accurately test challenging items within its specific scope of application by testing several such items and confirming performance characteristics [1].
A 2025 amendment to ISO 16140-3 (AMD 1:2025) specifically addresses the protocol for verifying validated identification methods of microorganisms [3] [4].
ISO 16140-4: Single Laboratory Validation
ISO 16140-4 addresses situations where method validation occurs within a single laboratory without an interlaboratory study [1]. In such cases, the validation results are only applicable to the laboratory that conducted the study, and method verification as described in ISO 16140-3 is not applicable [1]. This approach may be suitable for specialized methods, methods developed in-house, or when limited resources prevent a full multi-laboratory study.
Amendment 2 of ISO 16140-4, published in 2025, specifies the protocol for single-laboratory validation of identification methods of microorganisms [1]. Additionally, Amendment 1 (published in 2024) addresses the validation of larger test portion sizes for qualitative methods [5], responding to industry needs for detecting low-level contaminants.
ISO 16140-5: Factorial Interlaboratory Validation for Non-Proprietary Methods
ISO 16140-5 describes protocols for the interlaboratory validation of non-proprietary methods in specific cases where a more rapid validation is required or when the method to be validated is highly specialized and the number of participating laboratories required by ISO 16140-2 cannot be reached [1]. Unlike ISO 16140-2, which is designed primarily for proprietary methods, this part addresses the validation of methods that are typically publicly available.
This standard can be used for validation against a reference method for both qualitative and quantitative methods, but can also be used for validation without a reference method for quantitative methods only [1].
ISO 16140-6: Validation of Confirmation and Typing Methods
ISO 16140-6 covers the validation of alternative confirmation methods and typing techniques, which represents a more specialized application compared to other parts of the series [1]. The standard is restricted to validation of confirmation procedures that advance a suspected result to a confirmed positive result, such as biochemical confirmation of Enterobacteriaceae [1]. It also covers validation of alternative typing techniques like serotyping of Salmonella [1].
A critical aspect of validation under ISO 16140-6 is that it clearly specifies the selective agar(s) from which strains can be confirmed using the alternative confirmation method. If successfully validated, the alternative confirmation method can only be used if strains are recovered on an agar that was used and shown to be acceptable within the validation study [1].
ISO 16140-7: Validation of Identification Methods
ISO 16140-7 addresses the validation of microbial identification procedures, such as molecular identification using multiplex PCR, DNA sequencing, or mass spectrometry [1]. This part differs significantly from other parts of the series because it is intended for microbial identification where no reference method exists, making traditional method comparison studies impossible [1].
Instead of comparing against a reference method, validation under ISO 16140-7 relies on testing a panel of well-characterized strains. The validation study must specify the identification method principle, the identification database and algorithm (when appropriate), and the agar(s) from which strains can be identified [1].
Experimental Protocols and Methodologies
Validation Protocol for Alternative Methods (ISO 16140-2)
The validation process for alternative methods following ISO 16140-2 involves a rigorous two-phase approach designed to generate comprehensive performance data:
- Method Comparison Study: In this initial phase, the alternative method is compared against the reference method in a single laboratory. For qualitative methods, this involves testing inclusivity and exclusivity panels of target and non-target strains, as well as contaminated and uncontaminated food samples. For quantitative methods, this phase includes determination of quantitative performance characteristics such as accuracy profile, linearity, and measurement uncertainty.
- Interlaboratory Study: This phase involves a minimum of eight to ten laboratories testing a standardized set of contaminated and uncontaminated samples. The study includes five different food categories selected from fifteen defined categories, which enables the method to be regarded as validated for a "broad range of foods" [1]. The interlaboratory study evaluates interlaboratory consistency, relative accuracy, relative detection level, and relative specificity and sensitivity.
Verification Protocol in a Single Laboratory (ISO 16140-3)
The verification process for laboratories implementing previously validated methods involves a structured two-stage approach:
Implementation Verification Protocol:
- Select at least one food item that was used in the original validation study
- Test a minimum number of replicates (typically 5 uncontaminated and 5 contaminated test portions for qualitative methods)
- Compare results with expected outcomes from the validation study
- Demonstrate statistical equivalence for quantitative methods
Item Verification Protocol:
- Select challenging food items relevant to the laboratory's scope
- Include a minimum of five food items covering different categories
- Test contaminated and uncontaminated samples for each item
- Evaluate performance characteristics against defined criteria
- Document all procedures and results for assessment
Table: Essential Research Reagent Solutions for ISO 16140 Method Validation
| Reagent Category | Specific Examples | Function in Validation/Verification |
|---|---|---|
| Reference Strains | ATCC, NCTC, or other internationally recognized strains | Serve as target and non-target microorganisms for inclusivity/exclusivity testing [1]. |
| Selective Agar Media | Specific agars mentioned in validation studies (e.g., for Enterobacteriaceae confirmation) | Used for recovery of strains; validation is agar-specific [1]. |
| Artificially Contaminated Food Samples | Representative food categories (e.g., heat-processed milk, ready-to-eat foods) | Evaluate method performance in relevant matrices [1]. |
| Identification Reagents | PCR primers, sequencing kits, mass spectrometry matrices | Enable microbial identification in validation of identification methods [1]. |
Recent Developments and Amendments
The ISO 16140 series continues to evolve to address emerging needs in microbiological method validation. Several significant amendments have been published recently or are forthcoming:
- ISO 16140-2 Amendment 1 (2024): Introduced new calculations for qualitative method evaluation and RLOD of the interlaboratory study, with special attention to validation of methods for commercial sterility testing [1].
- ISO 16140-3 Amendment 1 (2025): Specified the protocol for verification of validated identification methods of microorganisms [3] [4].
- ISO 16140-4 Amendment 1 (2024): Addressed validation of larger test portion sizes for qualitative methods, with a transition period allowing existing laboratory-owned validation data until 2028 [1] [5].
- ISO 16140-4 Amendment 2 (2025): Provided protocol for single-laboratory validation of identification methods of microorganisms [1].
These amendments reflect the dynamic nature of microbiological testing and the need for standards to adapt to technological advancements and emerging challenges in food safety.
The ISO 16140 series provides a comprehensive, structured framework for the validation and verification of microbiological methods throughout the food chain. With its seven distinct parts, the series addresses the diverse needs of method developers, testing laboratories, and regulatory authorities by offering standardized protocols for different validation and verification scenarios. The clear distinction between method validation (proving a method is fit for purpose) and method verification (demonstrating laboratory competency with a validated method) represents a fundamental principle that ensures the reliability of microbiological testing.
The ongoing development of the series, evidenced by recent amendments addressing identification methods and larger test portion sizes, demonstrates the commitment to maintaining relevant and current standards. For researchers, scientists, and drug development professionals, understanding the specific roles and applications of each part of the ISO 16140 series is essential for designing appropriate validation studies, properly implementing methods in laboratory settings, and ensuring the generation of reliable, defensible microbiological data that ultimately protects public health.
In regulated industries such as pharmaceuticals, food safety, and environmental monitoring, the reliability of analytical testing methods is paramount. Method validation and method verification represent two distinct but interconnected processes that ensure analytical methods are fit for their intended purpose and correctly implemented within a specific laboratory environment. Within the framework of the ISO 16140 series, which provides comprehensive guidance for microbiological methods in the food chain, these processes are formally defined and standardized [1]. For researchers, scientists, and drug development professionals, understanding the critical distinction between validation and verification is not merely academic—it is a fundamental requirement for regulatory compliance, data integrity, and ultimately, product safety and efficacy. This guide provides an in-depth technical examination of both processes, their regulatory foundations, and detailed experimental protocols.
Defining the Concepts: Validation and Verification
Core Definitions and Regulatory Context
The distinction between method validation and verification is clearly established in international standards and regulatory guidelines.
Method Validation is a comprehensive, documented process that proves an analytical method is acceptable for its intended purpose [6] [7]. It is performed to demonstrate that the performance characteristics of a method meet the requirements for its specific analytical applications through rigorous laboratory studies [8]. Validation provides evidence that a method is scientifically sound and capable of producing reliable and reproducible results.
Method Verification is the process of confirming that a previously validated method performs as expected in a specific laboratory setting, with its particular personnel, equipment, and reagents [6] [9]. It is not a re-validation, but rather an assessment of how the analytical test procedure is suitable for its intended use under actual experimental conditions [8] [10].
The relationship between these processes is sequential: a method must first be validated to establish its performance characteristics, and then verified by each laboratory that implements it to confirm it functions correctly in that specific environment [1] [9].
When is Each Process Required?
The application of validation versus verification depends on the origin and status of the analytical method:
Method Validation is required when:
- Developing a new analytical method in-house [8].
- An established method is used for a new product or matrix outside its original validated scope [6].
- Submitting data for regulatory approvals, such as New Drug Applications (NDAs) or Biologic License Applications (BLAs) [6] [7].
- Transferring methods between labs or instruments where no prior validation data exists for the receiving lab [6].
Method Verification is required when:
- Implementing a compendial method (e.g., from USP, EP) for the first time in a laboratory [8] [10].
- Adopting a previously validated method from a client or another laboratory [8].
- Demonstrating competence for ISO/IEC 17025 accreditation [6] [2].
- Using standardized methods from organizations like EPA, AOAC, or ISO [6] [9].
The following diagram illustrates the decision-making workflow for determining whether validation or verification is needed:
Method Validation: Establishing Fitness for Purpose
Performance Characteristics and Assessment Protocols
Method validation requires a comprehensive assessment of multiple performance characteristics. The table below summarizes the key parameters, their definitions, and typical experimental protocols for assessment, based on ICH Q2(R1) and USP <1225> guidelines [8] [7].
Table 1: Key Performance Characteristics for Method Validation
| Performance Characteristic | Definition | Experimental Protocol & Assessment |
|---|---|---|
| Accuracy | The closeness of agreement between the accepted reference value and the value found [8] [7]. | Protocol: Analyze a minimum of 3 concentration levels with 3 replicates each using spiked samples with known analyte concentrations. Assessment: Calculate percent recovery or difference from the true value. |
| Precision | The closeness of agreement between a series of measurements from multiple sampling of the same homogeneous sample [8] [7]. | Protocol: Includes repeatability (same conditions) and intermediate precision (different days, analysts, equipment). Assessment: Calculate relative standard deviation (RSD) or coefficient of variation (CV). |
| Specificity | The ability to assess unequivocally the analyte in the presence of components that may be expected to be present [8] [7]. | Protocol: Analyze samples with and without potential interferents (impurities, matrix components). Assessment: Demonstrate that the response is due to the analyte alone. |
| Linearity | The ability of the method to obtain test results proportional to the concentration of the analyte [8]. | Protocol: Prepare and analyze a minimum of 5 concentration levels across the specified range. Assessment: Calculate correlation coefficient, y-intercept, and slope of the regression line. |
| Range | The interval between the upper and lower concentrations of analyte for which the method has suitable accuracy, precision, and linearity [8]. | Protocol: Established from linearity studies, typically confirmed at the range limits. Assessment: Verify that accuracy, precision, and linearity meet criteria across the range. |
| Detection Limit (LOD) | The lowest concentration of an analyte that can be detected, but not necessarily quantified [8] [7]. | Protocol: Based on visual evaluation, signal-to-noise ratio, or standard deviation of the response. Assessment: Lowest concentration that provides a detectable signal above background. |
| Quantitation Limit (LOQ) | The lowest concentration of an analyte that can be quantified with acceptable accuracy and precision [8] [7]. | Protocol: Analyze multiple samples at low concentrations and determine where precision and accuracy become unacceptable. Assessment: Concentration that provides a signal with specified accuracy and precision (e.g., ≤20% RSD). |
| Robustness | The capacity of a method to remain unaffected by small, deliberate variations in method parameters [8] [7]. | Protocol: Vary parameters such as pH, temperature, mobile phase composition, flow rate. Assessment: Evaluate the impact on method performance (precision, specificity). |
Regulatory Frameworks for Validation
Method validation is governed by several key regulatory guidelines:
- ICH Q2(R1): Provides the primary international guideline for validating analytical procedures, defining the key characteristics listed above [8] [7].
- USP General Chapter <1225>: Covers the validation of compendial procedures and categorizes methods based on the level of validation required [8] [10].
- FDA Guidance for Industry: Details validation requirements for Chemistry, Manufacturing, and Controls (CMC) documentation in regulatory submissions [7].
For biological methods or those used in bioanalytical studies, the "FDA Bioanalytical Method Validation" guidance provides additional specific requirements [7].
Method Verification: Confirming Laboratory Competence
Scope and Requirements
Method verification confirms that a laboratory can satisfactorily perform a validated method [1]. According to USP <1226>, verification involves assessing "selected analytical performance characteristics to generate appropriate and relevant data, rather than repeating the entire validation process" [10]. The extent of verification depends on factors including the analyst's experience, the complexity of the method, and the specific article being tested [10].
The ISO 16140-3 standard specifically outlines two stages of verification for microbiological methods:
- Implementation Verification: Demonstrates that the user laboratory can perform the method correctly by testing one of the same items evaluated in the validation study [1].
- Item Verification: Demonstrates that the laboratory is capable of testing challenging items within its scope of accreditation by testing several such items and confirming performance characteristics [1].
Verification Protocols and Experimental Design
Unlike validation, verification does not require assessment of all performance characteristics. The parameters selected for verification should be those most critical to confirming the method works as intended in the new setting.
Table 2: Typical Verification Parameters and Experimental Approaches
| Verification Parameter | Typical Experimental Protocol | Acceptance Criteria |
|---|---|---|
| Accuracy/Precision | Protocol: Analyze a minimum of 3 replicates at a single concentration level (for quantitative methods) or test reference materials with known status (for qualitative methods). ISO 16140-3 Approach: Follow the standard's specific protocol for implementation and item verification [1] [2]. | Criteria: Results fall within the validated method's specified range or established quality control limits. |
| Specificity/Selectivity | Protocol: Test the method against potentially interfering substances specific to the laboratory's sample matrices. | Criteria: No significant interference observed; method correctly identifies/quantifies analyte. |
| Limit of Detection (LOD) | Protocol: For qualitative methods, confirm the validated LOD by testing low-level inoculated samples. | Criteria: Consistent detection at or below the validated LOD. |
| Linearity/Range | Protocol: For quantitative methods, a limited linearity check with 3-4 data points may be sufficient. | Criteria: Correlation coefficient meets the method's specified requirement. |
| Robustness | Protocol: Minor, intentional variations in critical parameters (if applicable to the laboratory's specific implementation). | Criteria: Method performance remains acceptable despite variations. |
For laboratories implementing a compendial HPLC method, verification might focus primarily on precision and specificity, whereas for a microbiological method like an enzyme substrate test for water quality, verification would focus on specificity, selectivity, and repeatability through side-by-side comparison of 10-20 split samples [9] [10].
Comparative Analysis: Validation vs. Verification
The table below provides a direct comparison of the key attributes of method validation and verification, highlighting their distinct roles and requirements.
Table 3: Comprehensive Comparison of Method Validation and Verification
| Aspect | Method Validation | Method Verification |
|---|---|---|
| Objective | Prove the method is fit for its intended purpose [8] [6]. | Confirm the laboratory can properly perform the validated method [1] [6]. |
| When Performed | During method development; for new methods; for regulatory submissions [8] [6]. | When implementing a previously validated method in a new laboratory for the first time [8] [9]. |
| Scope | Comprehensive assessment of all relevant performance characteristics [8] [7]. | Limited assessment of selected performance characteristics deemed appropriate for the specific context [6] [10]. |
| Regulatory Basis | ICH Q2(R1), USP <1225>, FDA guidance [8] [7]. | USP <1226>, ISO 16140-3, ISO/IEC 17025 [1] [10]. |
| Resource Intensity | High (time-consuming, resource-intensive, costly) [6]. | Moderate (faster, more economical) [6]. |
| Data Requirements | Extensive data set to fully characterize the method [8] [7]. | Sufficient data to demonstrate laboratory competence with the method [6] [10]. |
| Primary Responsibility | Method developer or originating laboratory [8]. | User laboratory implementing the method [9]. |
The ISO 16140 Framework for Microbiological Methods
The ISO 16140 series, "Microbiology of the food chain - Method validation," provides a standardized international approach for the validation and verification of microbiological methods, particularly for food and feed testing [1]. The series consists of multiple parts, each addressing specific aspects of the validation and verification process:
- ISO 16140-1: Vocabulary [1]
- ISO 16140-2: Protocol for the validation of alternative (proprietary) methods against a reference method [1]
- ISO 16140-3: Protocol for the verification of reference methods and validated alternative methods in a single laboratory [1] [2]
- ISO 16140-4: Protocol for method validation in a single laboratory [1]
- ISO 16140-5: Protocol for factorial interlaboratory validation for non-proprietary methods [1]
- ISO 16140-6: Protocol for the validation of alternative methods for microbiological confirmation and typing procedures [1]
- ISO 16140-7: Protocol for the validation of identification methods of microorganisms [1]
Implementation of ISO 16140-3 for Verification
The publication of ISO 16140-3 in 2021 provided the first internationally recognized standard for the verification of microbiological methods [2]. This standard is particularly relevant for laboratories accredited to ISO/IEC 17025, which requires verification of validated methods before implementation [2]. The standard guides laboratories through the process of selecting appropriate food categories and items for verification, ensuring that the method performs as expected for the specific sample types tested within the laboratory's scope [1].
Essential Research Reagents and Materials
The following table details key reagents and materials commonly required for method validation and verification studies, particularly in microbiological and chemical analyses.
Table 4: Essential Research Reagent Solutions for Method Validation/Verification
| Reagent/Material | Function & Application in Validation/Verification |
|---|---|
| Certified Reference Materials (CRMs) | Provide a known, traceable quantity of analyte for establishing accuracy, precision, and linearity during validation [7]. |
| Quality Control Strains | For microbiological methods, used to verify specificity, LOD, and accuracy during verification studies [9]. |
| Inoculated/Spiked Samples | Samples with a known concentration of analyte (microorganism or chemical) used to assess recovery, accuracy, and LOD [9]. |
| Selective Culture Media | Used in microbiological methods to assess specificity by differentiating target microorganisms from non-target organisms [1]. |
| Internal Standards | For chromatographic methods, used to normalize results and improve the precision and accuracy of quantification [8]. |
| Matrix-Blank Samples | Samples free of the target analyte used to demonstrate the absence of interference, confirming method specificity [7]. |
Method validation and method verification are distinct but complementary processes that form the foundation of reliable analytical testing in regulated environments. Validation is a comprehensive process to establish that a method is scientifically sound and fit for its intended purpose, while verification is a targeted process to confirm that a laboratory can successfully implement a previously validated method. The ISO 16140 series provides a critical framework for these processes in microbiological testing, with ISO 16140-3 offering specific guidance for method verification. For researchers and drug development professionals, a clear understanding of these processes, their respective requirements, and the associated experimental protocols is essential for generating reliable data, maintaining regulatory compliance, and ensuring product quality and safety.
In regulated scientific fields, demonstrating the reliability of analytical methods and the competence of the personnel performing them is a foundational requirement. The two-stage framework of method validation (proving a method is fit-for-purpose) and method verification (proving a laboratory can competently perform the method) provides a systematic approach to ensuring data integrity. This framework is codified in international standards, most notably the ISO 16140 series for microbiology, and is supported by broader laboratory competence standards like ISO/IEC 17025. This guide provides an in-depth technical exploration of this framework, detailing the experimental protocols, competency requirements, and documentation needed for compliance and scientific rigor. Adherence to this structured process is critical for generating reliable, defensible data in research and drug development.
Before any laboratory implements a new test method for routine use, it must answer two critical questions: First, is the method itself technically sound and fit for its intended purpose? Second, can our laboratory personnel and systems execute this method correctly and consistently? The two-stage framework directly addresses these questions through distinct, sequential processes.
- Stage 1: Method Validation is the process of proving through an objective experiment that a method is fit-for-purpose. It answers the question, "Does this method work?" According to the ISO 16140 series, validation is conducted to provide evidence that a method meets the performance criteria for its intended application [1]. This stage is typically performed by the method developer or manufacturer and involves rigorous testing against a reference method in a multi-laboratory study to establish its performance characteristics, such as accuracy, precision, and specificity [1].
- Stage 2: Method Verification is the process by which a laboratory provides objective evidence that it has the competence and capability to successfully perform a validated method. It answers the question, "Can we perform this method correctly in our lab?" As outlined in ISO 16140-3, verification is where "a laboratory demonstrates that it can satisfactorily perform a validated method" [1]. For laboratories accredited to ISO/IEC 17025, this is not merely a best practice but a mandatory requirement [2].
The logical relationship between these stages is sequential and interdependent, as illustrated below.
The Sequential Workflow of Method Validation and Verification
Stage 1: Proving Method Fitness (Validation)
Method validation is the foundational first stage, providing the performance data that proves a method's reliability.
Key Validation Standards and Protocols
The ISO 16140 series provides a comprehensive structure for the validation of microbiological methods. The selection of the appropriate validation protocol depends on the method type and the goal of the study [1].
Table: Parts of the ISO 16140 Series for Method Validation
| ISO Standard Part | Title | Scope and Application |
|---|---|---|
| ISO 16140-2 | Protocol for the validation of alternative (proprietary) methods against a reference method | The base standard for alternative method validation; includes a method comparison study and an interlaboratory study [1]. |
| ISO 16140-4 | Protocol for method validation in a single laboratory | Used when validation is conducted within one laboratory only; results are specific to that lab [1]. |
| ISO 16140-5 | Protocol for factorial interlaboratory validation for non-proprietary methods | For validation of non-proprietary methods in specific cases requiring rapid validation or when a full number of labs cannot be recruited [1]. |
Detailed Experimental Protocol for Validation
For a validation study against a reference method according to ISO 16140-2, the protocol is highly structured. The following methodology outlines the core steps for a quantitative method.
Study Design and Planning:
- Objective: To demonstrate the alternative method's performance is equivalent or non-inferior to the reference method.
- Sample Types: Select a minimum of five different food categories (e.g., heat-processed milk, raw poultry, ready-to-eat foods) out of a defined list of 15 to represent a "broad range of foods" [1].
- Inoculation: Artificially inoculate food samples with target microorganisms at multiple predetermined contamination levels, including low, medium, and high counts for quantitative methods.
Method Comparison Study (Primary Validation):
- Testing: Analyze the inoculated samples in parallel using both the alternative method and the reference method.
- Replication: Perform a sufficient number of replicates (e.g., n=5 per contamination level) to ensure statistical power.
Interlaboratory Study:
- Collaboration: Engage a minimum number of independent laboratories to repeat the method comparison study.
- Purpose: This confirms the method's robustness and transferability across different laboratory environments, operators, and equipment.
Data Analysis and Performance Characterization: Calculate the following key performance indicators from the collected data:
- Accuracy/Relative Accuracy: The closeness of agreement between the results from the alternative method and the reference method.
- Precision: Expressed as repeatability (within-lab) and reproducibility (between-lab) standard deviations.
- Linearity: The ability of the method to obtain results directly proportional to the analyte concentration.
- Limit of Detection (LOD): The lowest quantity of the analyte that can be detected.
- Limit of Quantification (LOQ): The lowest quantity of the analyte that can be quantified with acceptable precision and accuracy.
Stage 2: Demonstrating Laboratory Competence (Verification)
Once a method is validated, the responsibility shifts to the individual laboratory to prove its competence in performing it.
The Verification Mandate
Verification is a critical requirement for laboratories operating under ISO/IEC 17025 accreditation [2]. Even for non-accredited labs, it is considered a fundamental best practice [2]. The international standard ISO 16140-3:2021 provides specific guidance on how to verify microbiological methods, offering a unified protocol that was lacking prior to its publication [2].
The Two-Stage Verification Protocol (ISO 16140-3)
ISO 16140-3 breaks down verification into two distinct stages, each with a specific purpose [1].
Table: The Two Stages of Method Verification per ISO 16140-3
| Verification Stage | Purpose | Key Activity |
|---|---|---|
| Implementation Verification | To demonstrate the user laboratory can perform the method correctly as per the validated protocol. | Testing one of the same food items used in the original validation study and comparing results to show the laboratory can achieve similar performance [1]. |
| Food Item Verification | To demonstrate the method performs satisfactorily for the specific, and potentially challenging, sample types routinely tested by the laboratory. | Testing several food items that are specific to the laboratory's scope and confirming method performance using defined characteristics [1]. |
The following diagram maps the decision-making workflow a laboratory must follow to successfully verify a method.
Laboratory Workflow for Method Verification
Personnel Competency Requirements (ISO/IEC 17025)
Underpinning the entire verification process is the requirement for demonstrably competent personnel, as mandated in section 6.2 of ISO/IEC 17025 [11]. The standard requires laboratories to:
- Document competence requirements for each role influencing laboratory results, including education, training, skills, and experience [11].
- Implement procedures for determining competence, selecting, training, supervising, and authorizing personnel [11].
- Continuously monitor competence through techniques like observation, proficiency testing, and peer review [11].
This aligns with global best practices for laboratory workforce competency, which emphasize the need to assess personnel through direct observation, review of quality control records, and evaluation of problem-solving skills [12].
The Scientist's Toolkit: Key Reagents and Materials
The execution of validated and verified methods relies on a suite of essential materials. The following table details key reagent solutions used in microbiological method validation and verification studies.
Table: Key Research Reagent Solutions for Method Validation & Verification
| Reagent/Material | Function in Experimental Protocol |
|---|---|
| Reference Strains | Well-characterized microbial strains from culture collections (e.g., ATCC) used for inoculating samples to assess method accuracy, specificity, and limit of detection. |
| Selective and Non-Selective Media | Agar and broths used to cultivate, isolate, and differentiate target microorganisms from background flora; critical for comparing growth between reference and alternative methods. |
| Buffered Diluents | Solutions like Buffered Peptone Water used to homogenize samples and maintain osmotic balance and pH, ensuring microbial viability during testing. |
| Inactivation Solutions | Chemicals or reagents used to neutralize disinfectants or antimicrobials in a sample (e.g., in commercial sterility testing) to prevent false-negative results. |
| Quality Control Cultures | Strains used to verify the performance and sterility of media, reagents, and the overall testing process on each day of testing. |
| Proprietary Enrichment Media & Substrates | Specialized broths and chromogenic/fluorogenic compounds specific to alternative rapid methods that facilitate the detection and identification of target microbes. |
| (2E,11Z)-octadecadienoyl-CoA | (2E,11Z)-octadecadienoyl-CoA, MF:C39H66N7O17P3S, MW:1030.0 g/mol |
| 3,6-Dihydroxytetradecanoyl-CoA | 3,6-Dihydroxytetradecanoyl-CoA, MF:C35H62N7O19P3S, MW:1009.9 g/mol |
The two-stage framework of validation and verification is a non-negotiable pillar of quality assurance in scientific research and drug development. This structured approach transforms subjective trust into objective evidence. Method validation, governed by standards like ISO 16140-2 and -4, generates the foundational data proving a method is scientifically sound. Method verification, as detailed in ISO 16140-3 and supported by the personnel competency requirements of ISO/IEC 17025, provides the critical proof that a laboratory has the technical capability to implement the method successfully. By rigorously applying this framework, laboratories and researchers can ensure the generation of reliable, defensible, and high-quality data that drives innovation and ensures safety.
The ISO 16140 series of standards, initially developed for the food and feed sectors, provides a robust framework for the validation and verification of microbiological methods. While these standards are foundational in food safety testing, their principles and structured protocols hold significant, yet often underutilized, potential for pharmaceutical microbiology. This technical guide explores the application of ISO 16140, particularly Part 3 on method verification, within pharmaceutical drug development and quality control. Adherence to such internationally recognized validation protocols enhances the reliability of microbiological test results, which is paramount for ensuring the safety and quality of sterile and non-sterile pharmaceutical products, water systems, and manufacturing environments [13] [14].
The core principle of the ISO 16140 series is a two-stage process before a method is put into routine use: first, proving the method itself is fit-for-purpose (validation), and second, demonstrating that the user laboratory can properly perform the method (verification) [1]. This systematic approach is directly transferable to the highly regulated pharmaceutical industry, where method reliability is non-negotiable.
The ISO 16140 Framework: Core Concepts and Structure
Anatomy of the ISO 16140 Series
The ISO 16140 series is a multi-part standard, with each part addressing a specific aspect of method validation or verification. For a pharmaceutical laboratory seeking to implement a new microbiological method, understanding the role of each part is crucial. The following table summarizes the scope of the key parts within the series.
Table 1: Core Parts of the ISO 16140 Series Relevant to Method Implementation
| Standard Part | Title | Primary Focus | Application Context |
|---|---|---|---|
| ISO 16140-1 | Vocabulary [1] | Defines terminology used across the series [15]. | Foundational for ensuring consistent understanding of terms like validation, verification, inclusivity, and exclusivity. |
| ISO 16140-2 | Protocol for the validation of alternative methods against a reference method [1] | Base standard for validating proprietary (commercial) methods via a method comparison study and an interlaboratory study [1] [15]. | Conducted by test kit manufacturers to generate performance data for end-users. |
| ISO 16140-3 | Protocol for the verification of reference and validated alternative methods in a single laboratory [1] [14] | Provides the protocol for a user laboratory to demonstrate its competence in performing a validated method before routine use [13] [1]. | Critical for pharmaceutical quality control labs implementing a new method. |
| ISO 16140-4 | Protocol for method validation in a single laboratory [1] | Allows for validation within a single lab without an interlaboratory study. Results are only valid for that lab [1]. | Applicable for non-proprietary methods or when a full validation is not feasible. |
| ISO 16140-7 | Protocol for the validation of identification methods of microorganisms [1] | Addresses validation of identification procedures (e.g., PCR, MS) where no reference method exists [1]. | Highly relevant for pharmaceutical labs using modern techniques for microbial identification. |
Validation vs. Verification: A Critical Distinction
A fundamental concept within the ISO 16140 framework is the clear distinction between method validation and method verification. These are sequential but distinct activities:
- Method Validation: This is the primary process of proving that a new or alternative method is fit for its intended purpose. Validation provides objective evidence that a method meets the performance requirements for its application [1]. This is typically the responsibility of the method developer or manufacturer and is performed according to parts like ISO 16140-2 or -4.
- Method Verification: This is the subsequent process where a user laboratory demonstrates that it can satisfactorily perform a method that has already been validated [1]. As defined in ISO 16140-3, a user laboratory is a "laboratory that implements a validated alternative method and/or a validated reference method" [16]. Verification confirms that the laboratory's execution of the method aligns with the performance characteristics established during the initial validation.
For a pharmaceutical quality control laboratory, verification (ISO 16140-3) is the standard most directly applicable to introducing a new commercial test kit or a pharmacopeial method into its quality system.
ISO 16140-3: The Verification Protocol for User Laboratories
The Two-Stage Verification Process
ISO 16140-3 outlines a structured two-stage protocol for verification, which ensures a laboratory is not only technically competent but also that the method is suitable for its specific testing needs [1].
Table 2: The Two Stages of Method Verification per ISO 16140-3
| Verification Stage | Purpose | Key Activities | Acceptance Criteria |
|---|---|---|---|
| Implementation Verification | To demonstrate that the user laboratory can perform the method correctly [1]. | Testing one of the same items (e.g., a specific matrix or sample type) that was used during the method's original validation study [1]. | The laboratory's results must be comparable to those achieved during the method's validation. |
| Item Verification | To demonstrate that the method performs satisfactorily for the specific, and potentially challenging, items within the laboratory's own scope of testing [1]. | Testing several "food items" or, in a pharmaceutical context, specific sample types (e.g., active pharmaceutical ingredients, finished products, water) that the lab routinely tests [1]. | Performance must meet pre-defined characteristics (e.g., sensitivity, specificity) for those specific items. |
This workflow illustrates the logical sequence and decision points in the ISO 16140-3 verification process:
A Practical Case: Verification of aListeriaPCR Method
A 2024 study provides a clear template for applying ISO 16140-3 to a rapid microbiological method, in this case, a qualitative real-time PCR (qPCR) assay for detecting Listeria spp. and Listeria monocytogenes [17]. While the study focused on food and environmental swabs, its methodology is directly adaptable to pharmaceutical processing environments.
Table 3: Key Research Reagent Solutions for Method Verification [17]
| Reagent / Material | Function in the Verification Study | Specific Example / Specification |
|---|---|---|
| Reference Strain | Serves as a known positive control to inoculate samples for accuracy and detection limit studies. | Listeria monocytogenes ATCC 19115 (3-5 CFU per sample) [17]. |
| Culture Media | Used for sample enrichment and growth promotion testing. | Half-Fraser Broth [17]. |
| DNA Extraction Kit | Isolates microbial DNA from the sample matrix for subsequent PCR analysis. | SureFast PREP Bacteria kit (r-biopharm) [17]. |
| qPCR Master Mix & Kit | Provides the enzymes, buffers, and probes necessary for the amplification and detection of target DNA. | SureFast Listeria 3plex ONE kit (r-biopharm) [17]. |
| Sample Matrices | Represents the actual items tested during verification. | Implementation: Commercial milk powder. Item: Environmental swabs in Half-Fraser broth [17]. |
Experimental Protocol for Verification [17]:
Sample Preparation and Inoculation:
- For implementation verification, seven 25 g samples of a representative matrix (e.g., milk powder) were diluted with 225 mL of enrichment broth and inoculated with a low count (3-5 CFU) of L. monocytogenes. One uninoculated sample served as a blank.
- For item verification, seven environmental swabs diluted in 10 mL of enrichment broth were similarly inoculated. This mimics the critical environmental monitoring of a pharmaceutical cleanroom.
Incubation and Plating: All inoculated samples and blanks were incubated for 18-20 hours at 37°C. A plate count on Tryptic Soy Agar (TSA) was performed concurrently to confirm the inoculation level.
DNA Extraction: DNA was extracted from the enriched samples using a commercial kit. The study compared a full extraction protocol with a rapid lysis buffer method, highlighting the importance of verifying the entire analytical process.
Real-Time PCR Amplification:
- The qPCR master mix was prepared according to the kit's instructions.
- All samples were analyzed in triplicate to ensure result consistency.
- The run included essential controls: No-Template Control (NTC), Extraction Control, Positive Control (PC), and a Medium Control.
Analysis and Acceptance: The method was considered verified as it successfully detected the target organism in all inoculated samples and gave negative results for all blanks, meeting the pre-defined performance criteria for qualitative methods.
Translating ISO 16140 to Pharmaceutical Microbiology
Strategic Applications and Adaptation
The principles of ISO 16140-3 are highly adaptable to the unique demands of pharmaceutical quality control and R&D. Key application areas include:
- Rapid Microbial Methods (RMMs): The pharmaceutical industry is increasingly adopting RMMs like PCR, flow cytometry, and ATP bioluminescence. These technologies are ideal candidates for a rigorous verification process following ISO 16140-3, which provides a structured protocol to demonstrate their equivalence or superiority to traditional, compendial methods [17].
- Environmental Monitoring: The case study using environmental swabs [17] is directly applicable to the verification of methods used to monitor pharmaceutical cleanrooms for objectionable microorganisms. Item verification would be crucial for different types of surface materials (stainless steel, epoxy resin) and locations within a facility.
- Utility Testing: Methods for testing Water-for-Injection (WFI) and Purified Water systems for microbial counts and specific pathogens can be verified using this framework, ensuring the method is suitable for this low-bioburden matrix.
- Raw Material and Finished Product Testing: The verification process ensures that methods used to test complex matrices, such as active pharmaceutical ingredients (APIs) or finished drug products (e.g., creams, suspensions), are not adversely affected by the product's formulation.
Navigating the "Scope" in a Pharmaceutical Context
A central concept in ISO 16140-3 is the management of "scope" – the range of samples for which a method is applicable [1]. The standard defines:
- Scope of Validation: The sample types for which the method developer has validated the method.
- Scope of the Laboratory Application: The sample types a user laboratory intends to test.
For a pharmaceutical lab, the "categories" are not food types, but rather product types (e.g., sterile solids, sterile liquids, non-sterile creams, water). The item verification stage is where the laboratory must provide evidence that the method is fit for its specific, often narrow, range of tested materials, even if the method was initially validated for a "broad range" of samples [1].
The ISO 16140 series, and ISO 16140-3 in particular, offers a powerful, systematic, and internationally recognized framework for the verification of microbiological methods in pharmaceutical microbiology. By adopting its structured two-stage protocol of implementation and item verification, pharmaceutical researchers and quality control professionals can generate robust, defensible data to support the introduction of new methods. This not only strengthens the overall quality system but also facilitates the adoption of innovative, rapid technologies, ultimately enhancing product safety and accelerating drug development. As the industry evolves, the principles encapsulated in these standards provide a solid foundation for ensuring the reliability and accuracy of microbiological data upon which patient safety depends.
This technical guide provides researchers, scientists, and drug development professionals with a comprehensive framework for understanding the essential vocabulary established in ISO 16140-1:2016, which serves as the foundational lexicon for all method validation and verification activities within the food chain microbiology sector. As a critical component of a broader research thesis on ISO 16140 method verification standards, this document systematically organizes key terms, defines their technical significance, and illustrates their practical applications within experimental protocols. The structured vocabulary enables professionals to navigate complex validation workflows with precision, ensuring consistent interpretation and implementation of methods across laboratories and research institutions. By establishing a common technical language, ISO 16140-1 facilitates clearer communication between test kit manufacturers, accreditation bodies, and end-users, ultimately contributing to greater food and pharmaceutical safety through more reliable microbiological testing outcomes.
The ISO 16140 series of standards was developed to address the critical need for validated food microbiology methods in response to the proliferation of alternative (often proprietary) testing methods appearing on the market [15]. Before this standardization, laboratories lacked a unified protocol for validating these new methods against traditional reference cultures, creating potential inconsistencies in reliability and interpretation of results. The multipart standard provides specific protocols and guidelines for the validation of methods, both proprietary (commercial) and non-proprietary [18].
Within this framework, ISO 16140-1:2016, "Microbiology of the food chain - Method validation - Part 1: Vocabulary," serves as the terminological foundation upon which all other parts are built [15] [18]. This standard establishes a common technical language that ensures consistent understanding and application across the entire method validation and verification process. Its importance is underscored by its application across diverse stakeholders, including food and feed testing laboratories, test kit manufacturers, competent authorities, and food and feed business operators [18]. The vocabulary defined in Part 1 enables precise communication regarding method performance characteristics, validation requirements, and verification protocols, thereby supporting the overall objective of the ISO 16140 series: to enhance the reliability of microbiological test results and contribute to greater product safety [15].
Table: Structure of the ISO 16140 Series
| Standard Part | Title | Focus Area | Status |
|---|---|---|---|
| ISO 16140-1:2016 | Vocabulary | Terminology used in microbial testing | Published |
| ISO 16140-2:2016 | Protocol for the validation of alternative methods against a reference method | Validation of proprietary methods | Published |
| ISO 16140-3 | Protocol for verification of reference and validated alternative methods in a single laboratory | Single-laboratory verification | Recently amended (2025) |
| ISO 16140-4 | Protocol for single-laboratory (in-house) method validation | In-house validation | Under development |
| ISO 16140-5 | Protocol for factorial interlaboratory validation for non-proprietary methods | Interlaboratory validation | Under development |
| ISO 16140-6:2019 | Protocol for validation of alternative methods for microbiological confirmation and typing | Confirmation and typing procedures | Published |
Core Vocabulary from ISO 16140-1:2016
Fundamental Validation Terminology
Understanding the precise definitions of fundamental validation terms is critical for proper implementation of microbiological methods. These terms establish the performance benchmarks and acceptance criteria that determine whether a method is suitable for its intended purpose.
Validation: The process of demonstrating that an alternative method is at least as effective as the reference method for detecting or enumerating the target microorganism [15]. The process includes two main phases: the method comparison study and the interlaboratory study, with separate protocols for qualitative and quantitative methods [18]. Validation according to ISO 16140-2 leads to higher reliability of alternative method test results [15].
Verification: The process conducted by an end-user to demonstrate their competence in properly implementing a previously validated method within their own laboratory [19]. The ISO 16140-3 standard specifically addresses the verification protocol for reference and validated alternative methods implemented in a single laboratory, filling a previous gap in internationally accepted guidelines for this purpose [19].
Reference Method: A standardized method used as the benchmark against which alternative methods are compared during validation [15]. The technical requirements and guidance for establishing or revising standardized reference methods are provided in ISO 17468:2016 [19].
Alternative Method: A method, often proprietary, that may differ in principle or technique from the reference method but is designed to achieve the same analytical outcome [15] [18]. These methods are generally cheaper to use, produce results faster than traditional culturing methods, and require fewer technical skills to perform [18].
Proprietary Method: A commercially developed and distributed alternative method, typically characterized by standardized reagents, equipment, and protocols supplied by a manufacturer [15] [18]. Over a hundred alternative methods have been validated based on the ISO 16140 standard [15].
Method Performance Characteristics
The following performance characteristics form the basis for evaluating and comparing microbiological methods in validation studies. These parameters provide the quantitative metrics necessary to objectively assess method reliability.
Table: Key Method Performance Characteristics in ISO 16140-1
| Term | Definition | Application Context |
|---|---|---|
| Accuracy | The closeness of agreement between a test result and an accepted reference value | Quantitative enumeration methods |
| Precision | The closeness of agreement between independent test results obtained under stipulated conditions | Both qualitative and quantitative methods |
| Specificity | The ability of a method to detect the target microorganism without interference from related non-target microorganisms | Detection and confirmation methods |
| Limit of Detection (LOD) | The lowest level of microorganisms that can be detected in a specified matrix | Qualitative detection methods |
| Relative Detection Level | The probability of detection of an alternative method relative to the reference method | Comparative method validation studies |
Scope-Related Definitions
The concept of "scope" is critically important in both validation and verification activities, as it defines the boundaries of applicability for any given method. ISO 16140-1 establishes precise definitions for different types of scope that must be distinguished.
Scope of the Method: The full range of matrices (food categories, ingredients, environmental samples) and microorganisms for which the method is designed to be applicable [19]. This represents the manufacturer's intended use claims for the method.
Scope of the Method Validation: The specific matrices and microorganisms for which the applicability of the method has been experimentally demonstrated through a formal validation study according to ISO 16140-2 [19]. This scope is typically narrower than the full scope of the method.
Scope of Laboratory Application: The specific matrices and microorganisms for which an end-user laboratory applies a validated method within their routine testing activities [19]. The laboratory must verify competence for each category included in this scope.
The relationship between these different scopes forms the basis for the verification process outlined in ISO 16140-3, where laboratories must demonstrate their ability to properly perform methods within their specific application scope before introducing them for routine use [19].
Experimental Protocols and Verification Workflows
Method Verification Process in a Single Laboratory
The method verification process according to ISO 16140-3 follows a structured two-step approach based on the scope definitions, designed to ensure laboratory competence and result reliability [19]. This protocol provides the methodological framework that laboratories must implement when introducing previously validated methods.
The first step, implementation verification, aims to demonstrate the fundamental competence of the laboratory personnel to perform the method correctly according to the established protocol [19]. This is achieved by testing a single matrix or food item and obtaining results that meet predefined acceptability criteria, confirming that the laboratory can technically execute the method procedures.
The second step, item verification, addresses the laboratory's ability to apply the method to the specific matrices or food items that fall within their routine testing scope [19]. For this step, laboratories must strategically select challenging items that represent the scope of their application, potentially including multiple categories with different chemical and physical properties that might affect method performance.
Protocol for Verification of Identification Methods
The recently published Amendment 1 (2025) to ISO 16140-3:2021 introduces a specific "Protocol for verification of validated identification methods of microorganisms" [20] [21]. This amendment extends the verification framework to include microbial identification techniques, which are crucial for confirmation and typing procedures in both food and pharmaceutical microbiology.
While the specific experimental details of the new amendment are not fully elaborated in the available search results, the protocol likely follows the same fundamental principles as the broader verification framework while addressing the unique aspects of identification methods. These would include:
- Reference Strain Verification: Using well-characterized microbial strains to confirm the method's identification capabilities.
- Challenge Panels: Testing against closely related non-target organisms to confirm specificity.
- Blinded Samples: Incorporating proficiency testing elements to objectively assess performance.
- Comparison to Reference Methods: Parallel testing with established identification protocols.
This amendment reflects the ongoing evolution of the ISO 16140 series to address emerging methodological needs and technological advancements in microbiological testing [20].
Essential Research Reagents and Materials
Successful implementation of methods following ISO 16140 vocabulary requires specific research reagents and materials that ensure consistency, reliability, and reproducibility across laboratories. The following table details key components of the research reagent solutions essential for method validation and verification studies.
Table: Essential Research Reagents and Materials for ISO 16140 Compliance
| Reagent/Material | Technical Function | Application Context |
|---|---|---|
| Reference Strains | Well-characterized microorganisms serving as positive controls and for specificity testing | Method validation, implementation verification, ongoing quality control |
| Certified Reference Materials | Matrix materials with certified microbial counts or presence/absence for target organisms | Accuracy studies, method comparison, verification procedures |
| Selective Enrichment Media | Culture media promoting growth of target microorganisms while inhibiting competitors | Reference method procedures, cultural confirmation steps |
| Chromogenic Substrates | Biochemical compounds producing color changes upon enzyme activity of specific microorganisms | Alternative method components, confirmation tests, identification protocols |
| Inactivation Reagents | Chemical solutions that neutralize antimicrobial components in samples | Product validity testing, recovery improvement in challenging matrices |
| Performance Testing Cultures | Standardized microbial suspensions for demonstrating method competence | Implementation verification, laboratory proficiency testing |
These reagents form the foundation of both validation and verification studies, enabling laboratories to generate reliable performance data and make informed decisions about method adoption and implementation [15] [19]. The use of standardized, well-characterized reagents is essential for demonstrating that a laboratory can achieve the required performance standards before implementing methods for routine testing [19].
The specialized vocabulary established in ISO 16140-1:2016 provides an indispensable technical foundation for all stakeholders involved in microbiological method validation and verification within the food chain and related sectors. This standardized terminology creates the essential common language that enables clear communication between method developers, validation bodies, accreditation authorities, and end-user laboratories. As the ISO 16140 series continues to evolve with new parts and amendments—including the recently published Amendment 1 to Part 3 addressing identification methods—the vocabulary in Part 1 will continue to serve as the cornerstone for interpretation and implementation [20] [15].
For researchers, scientists, and drug development professionals, mastery of this terminology is not merely an academic exercise but a practical necessity for designing robust validation studies, properly implementing methods in laboratory settings, and accurately interpreting results against defined performance criteria. The structured approach to verification outlined in ISO 16140-3, built directly upon the vocabulary of Part 1, provides laboratories with a clear framework for demonstrating competence while maintaining flexibility to address their specific testing needs [19]. As microbiological testing technologies continue to advance, this standardized vocabulary will ensure that new methods can be evaluated consistently and implemented reliably, ultimately supporting the shared goal of enhanced product safety and public health protection.
Implementing ISO 16140-3: A Step-by-Step Protocol for Method Verification
Method verification is a critical requirement for laboratories accredited to ISO/IEC 17025, serving as a demonstration that a validated method can be performed competently within the user's laboratory [2]. The ISO 16140 series provides internationally recognized standards for the validation and verification of microbiological methods in the food and feed chain [1]. Within this framework, ISO 16140-3:2021 specifies the protocol for the verification of reference methods and validated alternative methods for implementation in the user laboratory [22]. This standard provides a structured, two-stage process that ensures a laboratory can correctly perform a method that has already been formally validated, confirming the method's performance characteristics within the specific laboratory environment [1] [2].
The verification process is fundamentally distinct from validation. Validation proves that a method is fit-for-purpose through interlaboratory studies, while verification demonstrates that a laboratory can satisfactorily perform a validated method [1]. This distinction is crucial for laboratories implementing methods for routine testing, as it provides objective evidence of competency and reliability [2].
The Two-Stage Verification Framework
ISO 16140-3:2021 outlines two sequential stages of verification that laboratories must complete before implementing a method for routine use [1]. These stages progress from confirming basic competency with the method to establishing performance across the laboratory's intended scope of testing.
Stage 1: Implementation Verification
Implementation verification serves as the initial proof of capability. Its purpose is to demonstrate that the user laboratory can perform the method correctly by obtaining results consistent with those established during the method's validation [1].
- Objective: To confirm technical competency in executing the method procedure
- Requirement: Testing one or more items that were previously characterized and used in the validation study
- Performance Criteria: Results must align with established reference values within defined acceptance criteria
This stage verifies that laboratory personnel, equipment, and environment can collectively reproduce the method's expected outcomes on known samples before proceeding to more challenging matrices.
Stage 2: Item Verification
Item verification expands the assessment to confirm method performance across the specific sample types routinely tested by the laboratory [1]. This stage addresses the reality that validation studies cannot practically test all possible sample matrices.
- Objective: To demonstrate method performance on challenging items within the laboratory's scope
- Requirement: Testing multiple food items representing the categories and types the laboratory typically analyzes
- Performance Characteristics: Evaluation against defined performance metrics relevant to the method type (detection, quantification, confirmation, or typing)
Item verification ensures the method produces reliable results for the specific applications required by the laboratory, even for sample types not explicitly included in the original validation study.
Experimental Protocols and Methodologies
Protocol for Qualitative Methods
For qualitative methods (detection), the verification focuses on accuracy, specificity, and limit of detection:
- Inoculation Studies: Use representative target organisms and related non-target strains
- Matrix Testing: Include a minimum of five food categories relevant to laboratory scope
- Control Requirements: Include positive, negative, and procedural controls in each run
- Data Analysis: Calculate relative accuracy, false positive, and false negative rates against reference method or known spike levels
Protocol for Quantitative Methods
For quantitative methods (enumeration), verification emphasizes accuracy, precision, and quantitation limit:
- Replicate Testing: Analyze multiple replicates at different contamination levels
- Statistical Analysis: Calculate mean, standard deviation, and relative standard deviation
- Comparison to Reference: Establish correlation with reference method results
- Acceptance Criteria: Demonstrate statistical equivalence within predefined limits
Protocol for Confirmation and Typing Methods
For confirmation and typing procedures, specific protocols apply as described in Clause 7 of ISO 16140-3 [1]:
- Strain Panel Testing: Use well-characterized target and non-target strains
- Comparative Analysis: Evaluate results against reference identification methods
- Specificity Assessment: Verify discrimination capability between related strains
Table 1: Key Performance Characteristics for Method Verification
| Method Type | Primary Characteristics | Secondary Characteristics | Acceptance Criteria |
|---|---|---|---|
| Qualitative | Relative Accuracy, Detection Limit | Specificity, False Positive/Negative Rates | ≥95% relative accuracy vs reference method |
| Quantitative | Mean, Standard Deviation, RSDr | Linearity, Quantitation Limit | RSDr ≤ reference method RSDR |
| Confirmation | Correct Identification Rate | Specificity, Discrimination Power | ≥90% correct identification |
Visualization of the Verification Workflow
The following diagram illustrates the logical relationship and sequential flow between the two stages of verification and their key outcomes:
Diagram 1: Two-Stage Verification Workflow
The Researcher's Toolkit: Essential Materials for Verification Studies
Successful execution of method verification requires specific materials and controls. The table below details essential research reagent solutions and their applications in verification studies:
Table 2: Essential Research Reagents for Method Verification
| Reagent/Material | Function in Verification | Application Examples |
|---|---|---|
| Reference Strains | Positive controls for target organisms; establish method accuracy | ATCC/DSMZ strains for qualitative method detection limits |
| Chromogenic Media | Selective isolation and presumptive identification of target microbes | Detection of E. coli, coliforms, Salmonella in food matrices |
| Enrichment Broths | Promote growth of target organisms while inhibiting background flora | Buffered Peptone Water for Salmonella pre-enrichment |
| Molecular Detection Kits | Confirmatory identification through genetic markers | PCR reagents for virulence gene detection in pathogens |
| Inactivation Reagents | Neutralize antimicrobial components in food matrices | Neutralizers for testing sanitizers and disinfectants |
| Quality Control Strains | Verify method specificity and discrimination capability | Non-target strains for exclusivity testing in molecular assays |
| 8-Hydroxydodecanoyl-CoA | 8-Hydroxydodecanoyl-CoA, MF:C33H58N7O18P3S, MW:965.8 g/mol | Chemical Reagent |
| (2E,9Z,12Z)-octadecatrienoyl-CoA | (2E,9Z,12Z)-octadecatrienoyl-CoA, MF:C39H64N7O17P3S, MW:1028.0 g/mol | Chemical Reagent |
Implementation Considerations and Challenges
Laboratories implementing the two-stage verification process must address several practical considerations:
Scope Selection
The selection of appropriate food categories and items for verification requires careful consideration of the method's validated scope and the laboratory's intended applications [1]. Laboratories should:
- Prioritize challenging matrices with inherent antimicrobial properties
- Include representative samples from each major category in testing scope
- Consider sample homogeneity and stability during verification studies
Transition Period Management
For reference methods not yet fully validated, ISO 16140-3 provides transition protocols (Annex F) that recognize standardization organizations need time to complete validation studies [1]. Laboratories should:
- Document all verification activities during transition periods
- Monitor standardization progress for updated validation data
- Plan for full verification once reference method validation is complete
Data Management and Documentation
Comprehensive documentation is essential for demonstrating verification compliance. Laboratories must maintain:
- Raw data from all verification experiments
- Statistical analyses and comparison studies
- Deviation investigations and corrective actions
- Final verification report with conclusion on method suitability
The two-stage verification process established in ISO 16140-3:2021 provides laboratories with a robust framework for demonstrating methodological competence [1] [2]. This structured approach ensures reliable test results while maintaining flexibility for laboratory-specific applications, ultimately supporting food safety and quality across the global supply chain.
In the pharmaceutical industry, the reliability of analytical results is paramount, directly impacting drug safety, efficacy, and regulatory compliance. This reliability is heavily influenced by two fundamental processes: sample preparation and matrix selection. Sample preparation serves as the critical bottleneck in bioanalysis, designed to extract desired analytes and remove redundant components from complex biological matrices [23]. The sample matrix, defined as everything present in a typical sample except the analytes of interest, can profoundly influence analytical results [24]. When developing a method, scientists must carefully consider the influence of the sample matrix, as failure to do so can lead to troubleshooting situations when results prove inexplicable [24].
The context of method verification, particularly within the framework of ISO 16140 standards, provides essential guidance for these processes. The ISO 16140 series is dedicated to the validation and verification of microbiological methods, with Part 3 specifically addressing the protocol for verifying reference methods and validated alternative methods in a single laboratory [1]. These standards establish that before a method can be used routinely, laboratories must demonstrate both that the method is fit for purpose (validation) and that the laboratory can properly perform the method (verification) [1]. This framework ensures that sample preparation and matrix selection strategies yield consistent, accurate, and reproducible results across pharmaceutical applications.
The Critical Role of Sample Matrix in Analytical Methods
Defining Sample Matrix and Its Impact
The sample matrix encompasses all components in a sample except the target analytes. In pharmaceutical applications, this varies significantly based on the sample type. For bioanalytical methods measuring drugs in plasma, the matrix would be untreated plasma; for pharmaceutical formulations, it would be a placebo containing all excipients but no active ingredient [24]. Only when analyzing pure compounds, such as raw material for purity assessment, can the matrix be largely ignored, though even supposedly pure compounds may contain reaction impurities or by-products [24].
Regulatory authorities recognize the substantial influence of matrix effects. The International Conference on Harmonization (ICH) includes specificity as a key validation parameter, defining it as "the ability to assess unequivocally the analyte in the presence of components which may be expected to be present," specifically mentioning matrix as a potential interferent [24]. Similarly, the United States Pharmacopoeia (USP) Chapter 1226 on "Verification of Compendial Procedures" emphasizes that "excipients in a drug product can vary widely among manufacturers and may have the potential to directly interfere with the procedure" [24]. The Food and Drug Administration (FDA) refers to this same concept as selectivity in bioanalytical method validation [24].
Matrix Effects and Specificity Challenges
Matrix components can cause numerous analytical challenges, including ion suppression or enhancement in mass spectrometry, interference with detection, and alterations in analyte recovery. Chromatographic simulations demonstrate how matrix interference peaks can co-elute with or closely approach analyte peaks, reducing resolution and compromising accurate quantification [24]. When interference and analyte peaks completely overlap, it becomes impossible to determine whether the response comes from the analyte, the interference, or both [24].
The FDA recommends testing blank matrices from at least six sources to check for potential interferences in bioanalytical methods [24]. However, even this thorough approach may not be foolproof, as demonstrated by an example where a method developed using commercial plasma sources failed when analyzing samples from subjects with different genetics, diets, and health conditions [24]. This underscores the importance of selecting matrix sources that closely resemble final test samples.
Biological Matrices in Pharmaceutical Bioanalysis
Pharmaceutical research utilizes diverse biological matrices, each presenting unique challenges and considerations for sample preparation. The selection of appropriate matrices is crucial for obtaining meaningful analytical results that accurately reflect the biological system under investigation.
Table 1: Common Biological Matrices in Pharmaceutical Bioanalysis
| Matrix | Composition | Challenges | Pharmaceutical Applications |
|---|---|---|---|
| Blood, Plasma, Serum | Plasma: glucose, proteins, hormones, minerals, blood cells. Serum: plasma without fibrinogens [23]. | High protein content, phospholipids, diverse metabolites [23]. | Pharmacokinetic studies, therapeutic drug monitoring, biomarker quantification. |
| Urine | 95% water, inorganic salts (sodium, phosphate, sulfate, ammonia), urea, creatinine, proteins [23]. | High salt content, variable pH, dilution factors [23]. | Drug metabolism studies, excretion profiling, compliance testing. |
| Hair | Keratin-based structure, incorporates substances during growth [23]. | Low analyte concentrations, requires extensive washing, digestion needed [23]. | Chronic drug exposure assessment, forensic toxicology, historical monitoring. |
| Saliva | 99% water, electrolytes, cytokines, enzymes, hormones, antimicrobial components [23]. | Variable viscosity, food contamination, limited sample volume [23]. | Non-therapeutic drug monitoring, rapid screening, pediatric applications. |
| Tissues | Soft tissues (liver, kidney); Tough tissues (muscle, heart); Hard tissues (bone, nail) [23]. | Homogenization challenges, cellular debris, low drug levels in some tissues [23]. | Drug distribution studies, target site concentrations, toxicology assessments. |
| Feces | Indigestible food matter, inorganic substances, bacteria [23]. | Non-homogeneous, complex matrix, laden with macromolecules [23]. | Gut metabolism studies, herbal medicine analysis, digestive disorders. |
Additional matrices relevant to pharmaceutical applications include human breast milk, which is important for assessing drug excretion in breastfeeding mothers; sweat and skin surface lipids for transdermal drug delivery studies; and cerebrospinal fluid (CSF) for central nervous system drug investigations [23]. Each matrix requires specific sample preparation strategies to address its unique composition and complexity.
Sample Preparation Techniques: From Classical to Modern Approaches
Effective sample preparation is crucial for isolating analytes from complex matrices, reducing interference, and improving analytical sensitivity. Techniques range from simple precipitation to highly selective extraction methods.
Basic Techniques for Matrix Simplification
Dilute-and-Shoot approaches represent the simplest preparation method, involving minimal sample handling and dilution with an appropriate solvent. This low-cost technique is primarily suitable for relatively clean matrices like urine but is generally ineffective for high-protein samples due to potential ion suppression or instrument issues [25].
Protein Precipitation (PPT) is a common, straightforward method for protein-rich samples like plasma, serum, or whole blood. It utilizes organic solvents such as methanol to denature and precipitate proteins. After incubation at low temperatures and centrifugation, the supernatant is collected for analysis. Additives like zinc sulfate can enhance protein precipitation or aid cell lysis. While PPT effectively reduces matrix complexity, it offers limited selectivity and may not remove all interfering components [25].
Selective Extraction Techniques
Solid-Phase Extraction (SPE) selectively retains analytes on sorbent phases based on chemical characteristics such as polarity or charge. Impurities are washed away, and analytes are eluted with strong organic solvents. SPE improves consistency, reduces matrix effects, and is particularly valuable for complex samples or high-throughput environments. Various sorbents, including ion exchange types, can be selected or combined depending on analyte chemistry [25].
Liquid-Liquid Extraction (LLE) separates analytes based on solubility differences between aqueous biological fluids and immiscible organic solvents. This technique effectively removes many matrix interferences but is labor-intensive and challenging to automate [23]. Supported Liquid Extraction (SLE) improves upon LLE by using a porous support to retain the aqueous phase, allowing better partitioning of nonpolar analytes into organic solvents. SLE offers cleaner extracts and better reproducibility than traditional LLE [25].
Modern Microextraction Techniques
Recent developments focus on microextraction techniques that offer advantages in automation, solvent consumption, and efficiency. Solid-Phase Microextraction (SPME), introduced in 1990, represents a non-exhaustive method that integrates sampling, preconcentration, and extraction into a single step [23]. This technique provides simple operation, high accuracy, improved sample clean-up, and minimal solvent consumption [23].
Other emerging techniques include Dispersive Liquid-Liquid Microextraction (DLLME) and Electromembrane Extraction (EME), which have gained acceptance in clinical investigations due to their efficiency and minimal solvent requirements [23]. These techniques continuously evolve to meet the increasing demand for convenient and eco-friendly sample preparation approaches in pharmaceutical laboratories.
ISO 16140 Framework: Method Verification and Matrix Considerations
The ISO 16140 series provides a standardized framework for method validation and verification in microbiological analysis, with important principles applicable to pharmaceutical applications. This framework explicitly addresses matrix considerations through defined verification protocols.
Validation vs. Verification
The ISO standards distinguish between two essential stages before implementing a method: validation establishes that a method is fit for purpose, while verification demonstrates that a laboratory can properly perform the validated method [1]. Validation typically involves a method comparison study followed by an interlaboratory study, whereas verification occurs within a single laboratory [1].
Two-Stage Verification Process
ISO 16140-3 specifies two distinct verification stages:
Implementation Verification: The laboratory demonstrates it can correctly perform the method by testing one of the same items evaluated in the validation study, confirming similar results can be obtained [1].
Item Verification: The laboratory demonstrates capability in testing challenging items within its scope of accreditation by testing several such items and confirming defined performance characteristics [1].
This approach ensures that a laboratory can successfully implement a validated method across relevant matrices. The standard acknowledges that method validation cannot practically test all possible sample types, so the verification process must confirm method performance with specific matrices of interest to the laboratory.
Matrix Categories in Method Validation
ISO 16140-2 defines categories in the food chain as "a group of sample types of the same origin," with an overview provided in Annex A of the standard [1]. Since validation studies cannot test all existing categories, they typically base validation on 5 out of 15 defined food categories. When a minimum of 5 different food categories are validated, the method is considered validated for a "broad range of foods" [1].
This category approach has implications for pharmaceutical applications, suggesting that method validation should encompass representative matrix types, with verification confirming performance for specific matrices of interest.
Experimental Design and Workflow for Sample Preparation
A systematic approach to sample preparation ensures consistent, reliable results. The following workflow outlines key considerations for developing and verifying sample preparation methods.
Diagram 1: Sample preparation method development workflow
Sample Preparation Protocol for Microbiological Detection
Research on Listeria detection demonstrates a verified approach to sample preparation for pathogen detection according to ISO 16140-3:2021 [17]. The protocol includes:
Sample Preparation:
- For implementation verification: 25g milk powder diluted with 225mL of enrichment Half-Fraser broth
- For item verification: ready-to-use environmental swabs diluted in 10mL of Half-Fraser broth
- Inoculation with 3-5 CFU of Listeria monocytogenes reference strain
- Incubation for 18-20 hours at 37°C [17]
DNA Extraction:
- Two extraction methods: SureFast PREP Bacteria kit (full extraction) and lysis buffer only (rapid assay)
- Centrifugation and purification steps for the full extraction protocol [17]
Real-Time PCR Amplification:
- Master mix preparation with 19.3μL reaction mix and 0.7μL Taq per sample
- Thermal protocol: initial denaturation at 95°C for 1 minute, followed by 45 cycles of denaturation at 95°C for 10 seconds and annealing/extension at 60°C for 15 seconds
- Multiple controls included: no-template control, extraction control, positive control, zero control, and medium control [17]
This comprehensive protocol demonstrates the level of detail required for verified sample preparation methods in regulatory-compliant laboratories.
The Scientist's Toolkit: Essential Research Reagent Solutions
Selecting appropriate reagents and materials is crucial for successful sample preparation in pharmaceutical applications. The following table outlines key solutions and their functions.
Table 2: Essential Research Reagent Solutions for Sample Preparation
| Reagent/Material | Function | Application Examples |
|---|---|---|
| Solid-Phase Extraction (SPE) Cartridges | Selective retention of analytes based on chemical characteristics; removal of interfering matrix components [25]. | Drug purification from plasma, urine clean-up, metabolite isolation. |
| Protein Precipitation Reagents | Denaturation and precipitation of proteins through organic solvents or additives; reduction of matrix complexity [25]. | Plasma protein removal, serum sample preparation, whole blood processing. |
| Enrichment Broths | Selective amplification of target microorganisms; suppression of competing flora [17]. | Pathogen detection in food/pharmaceutical products, environmental monitoring. |
| Lysis Buffers | Cellular disruption and nucleic acid release; inactivation of nucleases [17]. | DNA/RNA extraction for PCR-based methods, genetic analysis. |
| Enzymatic Digestion Reagents | Breakdown of specific matrix components; release of bound analytes [23]. | Tissue homogenization, hair digestion, complex matrix analysis. |
| Internal Standards | Correction for variability in extraction efficiency and matrix effects; improvement of quantitative accuracy [24]. | LC-MS/MS quantification, method validation, compensation of recovery losses. |
| trans-2-Enoyl-OPC4-CoA | trans-2-Enoyl-OPC4-CoA, MF:C35H54N7O18P3S, MW:985.8 g/mol | Chemical Reagent |
| N-Hexanoyl-biotin-galactosylceramide | N-Hexanoyl-biotin-galactosylceramide, MF:C40H72N4O10S, MW:801.1 g/mol | Chemical Reagent |
Automation and Emerging Trends in Sample Preparation
The field of sample preparation continues to evolve, with automation and novel techniques addressing challenges of efficiency, reproducibility, and sensitivity.
Automation of Sample Preparation
Automation is becoming essential as laboratories face staffing shortages and increasing sample volumes. Solutions from providers like Hamilton and Tecan streamline sample preparation tasks including pipetting, plate transfers, and offline SPE [25]. One laboratory implementation cut total sample preparation time from six hours to three, and reduced hands-on analyst time from three hours to just 10 minutes by using a Tecan platform with SPE plates [25].
While automation offers significant benefits, it introduces new challenges including programming complexity, accounting for sample variability, managing liquid classes for different matrices, and replicating the precision of skilled manual pipetting [25].
Emerging Techniques
Dried Blood Spots (DBS) and Microsampling offer minimally invasive collection with improved sample logistics. Fixed-volume devices with or without pre-punched filter cards can simplify automation and downstream analysis. Challenges include hematocrit effects, uneven sample spread, storage issues, and potential for contamination or hemolysis [25].
Direct Analysis Techniques such as paper spray ionization mass spectrometry eliminate the need for extensive sample preparation and chromatographic separation. The Thermo Scientific VeriSpray PaperSpray ion source enables direct MS-based ionization for analyzing dried samples, particularly useful for complex matrices like whole blood [25].
Microextraction Techniques continue to advance, with developments in SPME, DLLME, and EME offering improved sensitivity, minimal solvent consumption, and better integration with analytical instrumentation [23]. These techniques align with the growing demand for green analytical chemistry approaches in pharmaceutical laboratories.
Effective sample preparation and appropriate matrix selection form the foundation for reliable analytical results in pharmaceutical applications. The complexity of biological matrices necessitates robust, well-characterized sample preparation techniques that can address matrix effects while maintaining analyte integrity. The framework provided by ISO 16140 standards emphasizes the importance of method verification, ensuring that laboratories can successfully implement validated methods for their specific matrices and applications.
As pharmaceutical research advances toward more complex analyses and lower detection limits, sample preparation strategies continue to evolve. Automation addresses throughput and reproducibility demands, while novel techniques offer improved selectivity and efficiency. By aligning sample preparation strategies with both analytical goals and regulatory frameworks, pharmaceutical laboratories can ensure the generation of high-quality, reliable data to support drug development and manufacturing processes.
Inter-laboratory replicability presents a significant challenge in microbiome research, particularly in studies aimed at understanding the molecular mechanisms that underpin soil health and plant growth [26]. The vision for overcoming this challenge lies in developing and validating standardized 'fabricated ecosystems'—closed laboratory ecological systems where all initial biotic and abiotic factors are specified and controlled [26]. This approach mirrors the adoption of shared model organisms in other biological disciplines. The ISO 16140 series provides a critical framework for method validation and verification in microbiological methods, establishing technical rules that are essential for proving a method is fit for purpose and that a laboratory can properly perform it [1]. This guide details the protocols and quality control measures necessary to achieve reproducible results, framed within the context of ISO 16140 standards that guide research verification and validation.
Quality Control Frameworks: ISO 16140 Validation and Verification
Before a microbiological method can be reliably used in a laboratory, two distinct stages are required according to the ISO 16140 series [1]. The first stage is method validation, which proves the method is fit for its intended purpose. The second stage is method verification, where a laboratory demonstrates its competence in performing a previously validated method.
Stages of Method Validation and Verification
- Method Validation: Conducted through a method comparison study (typically by one laboratory) followed by an interlaboratory study. For methods validated within a single laboratory only, no interlaboratory study is conducted [1].
- Method Verification: Applicable only to methods previously validated through an interlaboratory study. This stage consists of:
- Implementation Verification: Demonstrating the user laboratory can perform the method correctly by testing one of the same items evaluated in the validation study.
- Item Verification: Demonstrating the laboratory can test challenging items within its accreditation scope by testing several such items using defined performance characteristics [1].
Protocol Selection Framework
The ISO 16140 series provides different validation pathways depending on the method type and context, guiding researchers in selecting the appropriate validation protocol for their specific needs, whether for proprietary alternative methods, reference method verification, single-laboratory validation, or factorial interlaboratory validation for non-proprietary methods [1].
Experimental Protocols: Standardized Inoculation and Sterility Testing
A recent multi-laboratory ring trial investigating the reproducibility of plant phenotypes, exometabolite profiles, and microbiome assembly provides a exemplary model for standardized inoculation protocols [26]. The study involved five laboratories following identical protocols to ensure comparability.
Detailed Inoculation Methodology
The general inoculation procedure follows these critical steps, which were standardized across all participating laboratories [26]:
- EcoFAB 2.0 Device Assembly: Using standardized sterile habitats to ensure consistent environmental conditions.
- Brachypodium distachyon Seed Preparation: Involving dehusking, surface sterilization, and stratification at 4°C for 3 days.
- Germination: On standardized agar plates for 3 days under controlled conditions.
- Seedling Transfer: Moving seedlings to the EcoFAB 2.0 device for an additional 4 days of growth.
- Sterility Testing: Verifying the absence of contamination before proceeding with inoculation.
- SynCom Inoculation: Introducing synthetic bacterial communities into the EcoFAB 2.0 device at specified cell densities.
- Maintenance Phase: Regular water refill and root imaging at three standardized timepoints.
- Sampling and Harvest: Collecting samples and harvesting plants at 22 days after inoculation (DAI) for analysis.
Sterility Testing Protocol
All participating laboratories tested the sterility of the EcoFAB 2.0 devices by incubating spent medium on Luria-Bertani (LB) agar plates at two different time points. This rigorous sterility testing resulted in less than 1% (2 out of 210) of all tests showing colony formation, demonstrating the effectiveness of the sterilization protocols [26].
Quantitative Data Presentation: Reproducible Experimental Outcomes
The multi-laboratory study generated consistent quantitative data across different research settings, demonstrating the effectiveness of standardized protocols.
Table 1: Reproducible Plant Biomass Changes Across Laboratories
| Treatment | Shoot Fresh Weight Change | Shoot Dry Weight Change | Root Development Impact |
|---|---|---|---|
| Axenic (Control) | Baseline | Baseline | Baseline |
| SynCom16 | Significant decrease | Significant decrease | Decreased root development after 14 DAI |
| SynCom17 | Significant decrease | Significant decrease (greater than SynCom16) | Consistent decrease after 14 DAI |
Table 2: Reproducible Microbiome Assembly After 22 Days
| Community | Dominant Isolate | Relative Abundance (%) | Variability Across Labs |
|---|---|---|---|
| SynCom17 Inoculum | Mixed Community | Even distribution | Low (standardized inoculum) |
| SynCom17 Final (Root) | Paraburkholderia sp. OAS925 | 98 ± 0.03 | Very low |
| SynCom16 Inoculum | Mixed Community | Even distribution | Low (standardized inoculum) |
| SynCom16 Final (Root) | Rhodococcus sp. OAS809 | 68 ± 33 | High |
| Mycobacterium sp. OAE908 | 14 ± 27 | High | |
| Methylobacterium sp. OAE515 | 15 ± 20 | High |
The data show that SynCom17-inoculated plants consistently resulted in a significant decrease in shoot fresh weight and dry weight relative to axenic treatments across all laboratories [26]. More notably, the root microbiome inoculated with SynCom17 was overwhelmingly dominated by Paraburkholderia sp. OAS925 across all laboratories (98 ± 0.03% average relative abundance), demonstrating remarkable reproducibility [26]. In contrast, SynCom16 communities (lacking Paraburkholderia) showed much higher variability across laboratories, with different bacterial isolates dominating in different laboratory settings [26].
Visualizing Workflows: Standardized Experimental Processes
The following diagrams illustrate the key experimental and quality control workflows necessary for achieving reproducible results in inoculation studies.
Multi-Lab Reproducibility Study Workflow
ISO 16140 Method Validation Framework
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents and Materials for Reproducible Inoculation Studies
| Reagent/Material | Function | Standardization Benefit |
|---|---|---|
| Synthetic Microbial Communities (SynComs) | Defined, reproducible microbial inoculum with known composition | Limits complexity while retaining functional diversity and microbe-microbe interactions [26] |
| EcoFAB 2.0 Devices | Sterile, fabricated ecosystem habitat | Provides consistent, controlled environment for microbiome studies [26] |
| Standardized Growth Media | Consistent nutritional baseline | Eliminates media composition as a source of variation |
| Cryopreserved Bacterial Stocks | Long-term stability of reference strains | Ensures genetic consistency across experiments and laboratories [26] |
| Optical Density to CFU Conversion Standards | Accurate inoculum quantification | Ensures consistent starting cell densities across experiments [26] |
| DNA Extraction Kits | Nucleic acid isolation | Reduces technical variation in downstream sequencing applications |
| 3-oxo-(2S)-Methylisocapryloyl-CoA | 3-oxo-(2S)-Methylisocapryloyl-CoA, MF:C30H50N7O18P3S, MW:921.7 g/mol | Chemical Reagent |
| 3-Oxo-6Z-Dodecenoyl-CoA | 3-Oxo-6Z-Dodecenoyl-CoA, MF:C33H54N7O18P3S, MW:961.8 g/mol | Chemical Reagent |
The integration of standardized inoculation protocols with rigorous quality control frameworks based on ISO 16140 standards provides a pathway to overcoming the reproducibility challenges in microbiome research. The demonstrated success of multi-laboratory studies using standardized fabricated ecosystems, synthetic microbial communities, and detailed protocols shows that reproducible results are achievable when appropriate controls and standardization measures are implemented. As research continues to leverage microbiomes for agricultural, medical, and environmental applications, adherence to these validation frameworks and protocols will be essential for generating reliable, comparable data across the scientific community.
The detection and monitoring of Listeria monocytogenes represent a significant challenge in quality control settings within the food and pharmaceutical industries. This opportunistic pathogen is a major public health concern due to its ability to survive common stress levels such as high salinity, acidity, refrigeration temperatures, and low water activity [27]. Traditional culture-based methods for pathogen detection, while effective, are time-consuming, labor-intensive, and may fail to detect viable but non-cultivable cells [28] [27]. In response to these limitations, molecular technologies like real-time PCR (qPCR) have emerged as powerful alternatives, offering enhanced specificity, sensitivity, and significantly reduced detection times [27].
The verification of analytical methods is a critical requirement for laboratories accredited to ISO 17025 and is considered a best practice even in non-accredited facilities [2]. Until recently, no internationally recognized standard existed for this verification process. The publication of ISO 16140-3:2021 provides specific guidance on how to verify microbiological methods, establishing a standardized framework for laboratories to demonstrate method competence [2]. This case study details the application of ISO 16140-3:2021 for verifying a rapid qPCR method for the qualitative detection of Listeria spp. and L. monocytogenes, providing a model for implementation within a broader thesis on ISO 16140 method verification standards.
Background and Principles
Fundamentals of Real-Time PCR (qPCR)
Real-time PCR (qPCR) has revolutionized molecular biology by enabling accurate quantitative measurement of nucleic acids. This technique combines the amplification capabilities of traditional PCR with real-time detection, allowing researchers to monitor the accumulation of PCR products as they form [29]. Unlike traditional PCR that relies on end-point detection, qPCR focuses on the exponential phase of amplification, which provides the most precise and accurate data for quantification [29]. During this phase, the instrument calculates the threshold (fluorescence intensity above background) and the CT value (the cycle at which the sample reaches the threshold), which is used for absolute or relative quantitation [29].
When applied to RNA targets through reverse transcription quantitative PCR (RT-qPCR), this methodology enables sensitive gene expression analysis and pathogen detection [29]. The two common detection chemistries for qPCR are TaqMan probes (fluorogenic 5' nuclease chemistry) and SYBR Green dye, each with distinct advantages for specific applications [29].
ISO 16140-3:2021 Framework
ISO 16140-3:2021, titled "Microbiology of the food chain - Method verification - Part 3: Protocol for the verification of reference methods and validated alternative methods in a single laboratory," provides a standardized protocol for laboratories to verify their competence in implementing methods for detecting microorganisms in the food chain [27] [2]. The standard offers guidance on verifying both proprietary (commercial) methods and non-proprietary methods, ensuring that laboratories can demonstrate consistent and reliable performance regardless of the method's origin.
Industry perspectives highlight that the publication of ISO 16140-3:2021 filled a critical gap in the international standards landscape. Before its introduction, laboratories lacked unified guidance on method verification procedures, leading to potential inconsistencies in implementation and assessment [2]. The standard now serves as a foundational document for laboratories seeking to verify methods for routine testing, providing a structured framework that encompasses all critical verification parameters.
Experimental Design and Methodology
Verification Strategy
The verification process was designed to evaluate both the implementation of the qPCR method for Listeria detection and its specific application for environmental monitoring. According to ISO 16140-3:2021, verification should confirm that a laboratory can successfully implement a validated method and achieve specified performance criteria [27]. The experimental approach included two distinct components:
Implementation Verification: This initial phase confirmed the laboratory's capability to properly establish the qPCR method using a defined matrix. A commercial milk powder was selected due to its similarity to products typically analyzed in the laboratory and its complex composition, which includes powdered skimmed milk, whey, oils, maltodextrins, probiotics, proteins, salts, minerals, and vitamins [27].
Item Verification: This subsequent phase focused on the specific application of the method for detecting Listeria spp. and L. monocytogenes in environmental swabs, representing a critical monitoring point in industrial settings [27].
Sample Preparation and Inoculation
The sample preparation protocol followed ISO 16140-3:2021 guidelines to ensure consistent and representative contamination levels:
- Reference Strain: Listeria monocytogenes ATCC 19115 (10–100 CFU/100 μL) was used as the reference quantitative strain for both verification tests [27].
- Inoculation Level: Samples were inoculated with 3–5 CFU of L. monocytogenes to challenge the method at low contamination levels relevant to real-world scenarios [27].
- Sample Matrix Preparation:
- Inoculation Confirmation: At the time of inoculation, plate counts on non-selective Tryptic Soy Agar (TSA) were performed according to ISO 7218 to confirm the concentration of the reference strain [27].
- Incubation: After inoculation, milk powder samples and environmental swabs were incubated for 18–20 hours at 37°C (±1°C), while TSA plates were incubated for 4 days at 34°C (±4°C) [27].
DNA Extraction Methods
Two DNA extraction approaches were evaluated to determine their impact on detection performance:
- Solid-Phase Extraction: For milk powder enrichments, DNA was extracted using the SureFast PREP Bacteria kit (r-biopharm), which employs bead-based homogenization and silica-membrane purification [27].
- Rapid Lysis Method: For environmental swabs, DNA extraction was performed both with the SureFast PREP Bacteria kit and with the lysis buffer provided by the SureFast Listeria 3plex ONE kit after 26–28 hours of incubation, following the manufacturer's instructions [27].
The extraction controls included medium control, zero control, and extraction control to monitor potential contamination and extraction efficiency throughout the process.
qPCR Amplification and Analysis
The qPCR amplification protocol was rigorously controlled to ensure reproducible results:
- Master Mix Preparation: The PCR master mix was prepared under a PCR hood using 19.3 μL of reaction mix and 0.7 μL of Taq polymerase for each sample, with an additional 10% volume to account for pipetting variability [27].
- Thermal Cycling Conditions: The following protocol was applied:
- Initial denaturation: 95°C for 1 minute
- Amplification: 45 cycles of:
- Denaturation: 95°C for 10 seconds
- Annealing/Extension: 60°C for 15 seconds (with maximum ramp rate) [27]
- Controls: Each amplification run included five essential controls:
- No-template control (NTC)
- Extraction control
- Positive control (PC)
- Zero control
- Medium control [27]
- Replication: All samples were analyzed in triplicate to assess technical variability [27].
- Instrumentation: Amplification and analysis were performed with the QIAquant 96 5plex real-time PCR instrument [27].
Workflow Visualization
The following diagram illustrates the complete experimental workflow for the verification process:
Key Reagents and Research Solutions
Successful implementation of the qPCR verification protocol requires specific reagents and controls standardized according to ISO requirements. The table below details the essential research reagent solutions and their functions in the verification process:
| Reagent/Kit | Function | Specification |
|---|---|---|
| Half-Fraser Broth | Selective enrichment medium | Promotes growth of Listeria while inhibiting background flora [27] |
| SureFast Listeria 3plex ONE | qPCR detection kit | Contains primers, probes, and master mix for multiplex detection [27] |
| SureFast PREP Bacteria | DNA extraction kit | Solid-phase nucleic acid purification using silica membrane [27] |
| L. monocytogenes ATCC 19115 | Reference strain | Quantitative control (10-100 CFU/100 μL) for verification [27] |
| qPCR Controls | Process monitoring | NTC, extraction, positive, zero, and medium controls [27] |
Verification Results and Performance Data
The verification study generated comprehensive data on the performance characteristics of the qPCR method for Listeria detection. The results demonstrated consistent performance across both implementation and item verification phases:
Implementation Verification Results
The inoculum confirmation according to ISO 7218 validated the low-level contamination model, with plate counts confirming 17 CFU from 10 μL of the reconstituted reference strain, aligning with the manufacturer's declaration of 10-100 CFU per 100 μL [27]. Following the 18-20 hour enrichment period, the qPCR method successfully detected all inoculated samples (7/7 positive), while the blank sample remained negative, demonstrating 100% detection rate at the low inoculum level of 3-5 CFU [27].
Item Verification Results
The environmental swab testing similarly showed complete concordance with expected results. All seven inoculated swabs tested positive for L. monocytogenes, while the blank control remained negative [27]. Notably, the rapid lysis extraction method yielded equivalent results to the solid-phase extraction method, offering a time-saving alternative for routine testing without compromising detection capability [27].
Method Performance Characteristics
The overall performance characteristics of the verified qPCR method are summarized in the table below:
| Performance Characteristic | Result | Assessment |
|---|---|---|
| Specificity | 100% (no false positives) | No cross-reactivity with background flora [27] |
| Sensitivity | 100% (all true positives detected) | All inoculated samples correctly identified [27] |
| Limit of Detection | 3-5 CFU/sample | Reliable detection at low contamination levels [27] |
| Reproducibility | 100% across replicates | Consistent results in triplicate analyses [27] |
| Robustness | Consistent with different extraction methods | Comparable performance with solid-phase and rapid lysis [27] |
Discussion
Technical and Practical Implications
The verification results demonstrate that the qPCR method meets all acceptance criteria specified in ISO 16140-3:2021 for the qualitative detection of Listeria spp. and L. monocytogenes. The 100% detection rate at low inoculum levels (3-5 CFU) confirms the method's superior sensitivity, which is particularly valuable for detecting low-level contamination that poses significant risk in industrial settings [27]. This performance aligns with findings from other studies applying molecular methods for pathogen detection, where rt-PCR consistently demonstrated superior sensitivity and reliability compared to traditional culture methods, especially in complex matrices [28].
The successful application of both solid-phase and rapid lysis DNA extraction methods provides laboratories with flexibility to choose between maximum nucleic acid purity (solid-phase) and rapid processing time (lysis buffer) based on their specific needs. This flexibility is particularly valuable for high-throughput laboratories where processing time significantly impacts operational efficiency.
Compliance with ISO 16140-3:2021 Requirements
The verification study addressed all critical requirements of ISO 16140-3:2021, including method implementation assessment, inclusivity/exclusivity testing, determination of limit of detection, and evaluation of robustness [27] [2]. The use of a standardized reference strain (ATCC 19115) and controlled inoculation levels ensured the reproducibility of results, while the inclusion of multiple controls (NTC, extraction, positive, zero, and medium) demonstrated adequate contamination prevention and process control [27].
Industry experts emphasize that proper implementation of ISO 16140-3:2021 requires careful attention to experimental design, including appropriate sample size (number of replicates), statistical analysis of results, and comprehensive documentation [2]. This case study adhered to these principles by testing seven replicates per matrix, performing technical triplicates in qPCR analysis, and maintaining complete documentation of all procedures and results.
Implementation Challenges and Solutions
During the verification process, several potential challenges emerged that laboratories should anticipate when implementing similar methods:
- Matrix Effects: Complex matrices like milk powder and environmental swabs can contain PCR inhibitors that affect amplification efficiency. The inclusion of an internal amplification control (IAC) in the qPCR reaction is essential to identify inhibition issues [27].
- Low-Level Inoculum Variability: Confirming the exact concentration of low-level inocula (3-5 CFU) presents technical challenges. The use of reference quantitative strains with confirmed concentrations and plate count verification is critical to ensure accurate inoculation levels [27].
- DNA Extraction Efficiency: Inconsistent DNA extraction can significantly impact detection sensitivity. Standardizing extraction protocols and including extraction controls helps monitor and maintain consistent performance [27].
This case study demonstrates the successful verification of a rapid qPCR method for detecting Listeria spp. and L. monocytogenes according to ISO 16140-3:2021 requirements. The verified method demonstrated 100% sensitivity and specificity, with reliable detection at 3-5 CFU/sample in both milk powder and environmental swab matrices. The comprehensive verification protocol provides a model for laboratories implementing molecular methods for pathogen detection, highlighting the importance of standardized procedures, appropriate controls, and rigorous documentation.
The implementation of ISO 16140-3:2021-compliant verification processes represents a significant advancement in quality control for industries requiring rapid and reliable pathogen detection. By providing a standardized framework for method verification, the standard enables laboratories to demonstrate technical competence while ensuring the safety and quality of products through more sensitive and rapid detection of hazardous microorganisms. As molecular methods continue to evolve, the principles established in ISO 16140-3:2021 will serve as a foundation for verifying new technologies that further enhance the speed, accuracy, and efficiency of pathogen detection in industrial settings.
For researchers, scientists, and drug development professionals, the integrity of laboratory data is paramount. The ISO/IEC 17025 standard provides the international benchmark for the competence of testing and calibration laboratories, creating a framework of trust in results that is crucial for regulatory compliance and scientific advancement [30]. This guide examines the core requirements of the standard, with a specific focus on the pivotal roles of documentation and data analysis in achieving and maintaining accreditation. Furthermore, it frames these activities within the specific context of method verification as outlined by the ISO 16140 series, providing a structured pathway for laboratories to demonstrate technical competence and generate reliable, defensible data [1].
For laboratories implementing sophisticated techniques like non-targeted and suspect screening using high-resolution mass spectrometry (HRMS), a robust quality management system based on ISO/IEC 17025 is not just beneficial but essential for ensuring the reproducibility and robustness of results, especially when transitioning from research applications towards regulatory purposes [31].
Core Principles of ISO/IEC 17025:2017
The ISO/IEC 17025:2017 standard is structured around two fundamental sets of requirements: management system requirements and technical requirements. While management system requirements focus on the operational aspects of the laboratory, the technical requirements are directly concerned with the quality and validity of the laboratory's output. The standard's components include Scope, Normative References, Terms and Definitions, General Requirements, Structural Requirements, Resource Requirements, Process Requirements, and Management System Requirements [30].
A critical conceptual foundation for any laboratory is understanding the distinction between accreditation and certification. Accreditation, as defined in ISO/IEC 17025, is the formal recognition by an authoritative body (like A2LA) of a laboratory's competence to carry out specific testing or calibration tasks. In contrast, management system certification (such as ISO 9001) is a third-party attestation that a management system complies with a defined set of requirements. For testing laboratories, it is accreditation that attests to their technical competence [30].
Table: Key Clauses of ISO/IEC 17025:2017 Affecting Documentation and Data Analysis
| Clause Number | Clause Title | Significance for Documentation & Data |
|---|---|---|
| 7.2 | Selection, verification and validation of methods | Mandates rigorous validation data and documented procedures for all methods [31]. |
| 7.5 | Technical records | Requires clear, accurate, and secure record-keeping for all original observations, derived data, and calculations [31]. |
| 7.6 | Evaluation of measurement uncertainty | Demands documented procedures and analyses for estimating uncertainty, a key data analysis task [31]. |
| 7.8 | Reporting of results | Specifies the minimum information that must be included in test reports to ensure completeness and traceability [31]. |
| 7.11 | Control of data and information management | Requires laboratories to have procedures for data transfer, processing, and storage to ensure integrity and confidentiality [31]. |
The Interplay of ISO 17025 and ISO 16140 for Method Verification
The ISO 16140 series of standards is dedicated to the validation and verification of microbiological methods in the food and feed chain, and it serves as an excellent model for understanding the relationship between method validation/verification and laboratory competence [1]. For the purposes of ISO/IEC 17025 accreditation, understanding the distinction and connection between these two processes is critical.
- Method Validation is the process of proving that a method is fit for its intended purpose. This is the first stage before a method can be used and is typically conducted through a method comparison study and an interlaboratory study, as described in ISO 16140-2 [1]. Validation provides performance data for a method, allowing potential users to make an informed choice.
- Method Verification is the subsequent process where a laboratory demonstrates that it can satisfactorily perform a validated method. This is described in ISO 16140-3 and involves two stages: implementation verification (demonstrating the lab can get results comparable to the validation study) and (food) item verification (demonstrating the method works for the specific sample types tested by the lab) [1].
For a laboratory seeking accreditation, the process involves verifying that it has properly implemented a validated method, and this entire process must be thoroughly documented as evidence of competence.
Figure 1: The pathway from method validation to laboratory accreditation, showing the critical verification stage.
A Guide to Essential Documentation
Documentation is the backbone of a laboratory's quality management system. It provides the framework for ensuring processes are performed consistently and correctly, and it supplies the objective evidence required during an accreditation assessment to demonstrate compliance with the standard [30].
The Documentation Pyramid
Laboratory documentation should be structured hierarchically:
- Quality Manual: The top-level document that outlines the laboratory's commitment to quality and describes the entire management system as it aligns with ISO/IEC 17025.
- Procedures: Describe how specific activities are performed (e.g., handling of test items, internal audits, management reviews).
- Work Instructions: Provide detailed, step-by-step directions for performing specific tasks or operating equipment.
- Records: Objective evidence that procedures and instructions have been followed (e.g., calibration certificates, raw data, audit reports, training records).
Key Documents for Data Integrity
Specific documents are critical for demonstrating control over data and analysis:
- Standard Operating Procedures (SOPs): For all data-related processes, including data backup, version control, and electronic data validation.
- Technical Records: Must include all original observations, derived data, and sufficient information to facilitate repeatability and traceability. This includes notebooks, printouts, and chromatograms [31].
- Validation and Verification Reports: Comprehensive documentation of all validation and verification studies, including protocols, raw data, results, and conclusions.
- Uncertainty Budgets: Detailed records of the sources of uncertainty and their quantification [31].
Preparing the documentation of your laboratory operations can be the most time-consuming step in the accreditation process and may take several months to complete [30]. Using templates and examples from organizations like the FDA or USDA can provide insight, but ultimately, the documentation must reflect your laboratory's specific processes [30].
Data Analysis and Management for Compliance
Clause 7.11, "Control of data and information management," is a critical addition in the 2017 version of the standard, explicitly addressing the digital nature of modern laboratories. It requires laboratories to have confidence in the integrity of their data throughout its lifecycle, from generation to storage and reporting [31].
Ensuring Data Integrity
For complex data analysis workflows, such as those used in non-targeted HRMS, specific considerations must be addressed:
- Data Transfer and Calculations: Procedures must be implemented to check the integrity of data transferred automatically between systems. The computational steps used in data processing (e.g., in tools like XCMS or Compound Discoverer) must be documented and verified [31].
- Version Control: Any software, including bioinformatics tools and scripts used for data processing, must be under version control to ensure consistency and traceability [31].
- Technical Records for NTA/SS: For non-targeted and suspect screening analyses, technical records must extend beyond final results to include raw HRMS data files, processing parameter settings, and the detailed steps and confidence levels associated with the annotation/identification process [31].
Evaluation of Measurement Uncertainty
Clause 7.6 requires laboratories to evaluate measurement uncertainty for all calibrations and certain types of tests [31]. This is a fundamental data analysis task that must be documented for each validated method. The uncertainty budget should identify all significant sources of uncertainty, such as sampling, sample preparation, instrument precision, and reference material purity, and quantify their contribution to the combined uncertainty.
Experimental Protocols for Method Validation and Verification
The following protocols provide a framework for generating the necessary validation and verification data required for accreditation.
Protocol for Method Verification (Based on ISO 16140-3)
Purpose: To demonstrate that a laboratory can competently perform a previously validated method within its own facility [1].
Materials:
- Reference materials or certified reference materials (CRMs).
- In-house quality control materials.
- The validated method's full protocol and required equipment.
Methodology:
- Implementation Verification: Test the same (food) item that was used in the original validation study. Perform a minimum number of replicates (as defined by the method or ISO 16140-3) to demonstrate that the laboratory can achieve performance characteristics (e.g., accuracy, precision) comparable to those stated in the validation study [1].
- Item Verification: Select several challenging (food) items that are representative of the samples the laboratory will test and fall within the scope of the method's validation. Test these items and use defined performance characteristics (e.g., specificity, accuracy, limit of detection) to confirm the method performs satisfactorily for these items [1].
Data Analysis: Compare the results obtained during implementation and item verification against the method's validation claims. Statistical acceptance criteria must be pre-defined. All data, analysis, and conclusions must be documented in a verification report.
Protocol for Internal Audits
Purpose: To determine the laboratory's compliance with the requirements of ISO/IEC 17025 and its own management system (per clause 8.8) [30].
Materials: Internal audit procedure, audit checklist, non-conformity report form.
Methodology:
- Planning: Develop an internal audit schedule that covers all elements of the management system annually.
- Execution: A qualified internal auditor (who is independent of the activity being audited) reviews procedures, interviews personnel, and examines records and data against the requirements.
- Reporting: Document all findings, including non-conformities and opportunities for improvement.
- Follow-up: Implement corrective actions for any non-conformities and verify their effectiveness.
Data Analysis: The results of the internal audit are a key data set for the management review. They should be analyzed to identify systemic weaknesses or trends that require additional resources or process changes [30].
Table: Essential Research Reagent Solutions for ISO 16140 Method Verification
| Reagent/Material | Function in Verification Process |
|---|---|
| Certified Reference Materials (CRMs) | Provides a traceable and definitive value for accuracy testing and instrument calibration. |
| Reference Strains (Microbiology) | Essential for determining method specificity, accuracy, and limit of detection for microbiological methods. |
| In-House Quality Control Materials | A characterized, stable material used for ongoing precision and performance monitoring. |
| Blind Proficiency Test Samples | Samples provided by an external provider to objectively assess the laboratory's testing performance. |
| Calibration Standards | Used to establish the quantitative relationship between instrument response and analyte concentration. |
The Path to Accreditation: Integrating Documentation and Data
Achieving accreditation is a structured process that integrates all the elements discussed above. The journey from initial decision to accredited status can be broken down into key steps [30]:
Figure 2: The key stages in the ISO/IEC 17025 accreditation journey, highlighting the central role of documentation and review.
Two of the most critical steps for integrating documentation and data are the Internal Audit (Step 6) and the Management Review (Step 7). The internal audit is a self-assessment against the standard and your own documentation, designed to identify gaps [30]. The management review, required by clause 8.9, is a meeting of top management to review the suitability and effectiveness of the management system based on inputs such as audit results, corrective actions, customer feedback, and results from proficiency tests [30]. This review must have the authority to drive improvements and allocate resources, ensuring the system is a living, evolving part of the laboratory's operations [30].
For research and drug development laboratories, ISO/IEC 17025 accreditation is not merely a certificate on the wall; it is a comprehensive system that ensures the generation of reliable and defensible data. As this guide has detailed, rigorous documentation and robust data analysis and management are the twin pillars supporting this system. By framing these activities within the established framework of method validation and verification, such as that provided by the ISO 16140 series, laboratories can create a compelling case for their technical competence. The journey to accreditation demands a significant investment of time and resources, particularly in documenting processes and validating methods. However, this investment pays dividends in the form of increased confidence in results, a structured framework for continuous improvement, and a powerful competitive advantage in the demanding fields of scientific research and regulatory compliance.
Overcoming Implementation Challenges: Transition Periods and Method Optimization
In the rigorously controlled environments of pharmaceutical development and food safety testing, analytical and microbiological methods form the bedrock of product quality and consumer safety. Regulatory frameworks and international standards typically mandate that laboratories use fully validated methods to ensure result reliability. However, a practical challenge emerges: many established reference methods, particularly those published by standardization organizations like ISO and CEN, were developed before modern validation requirements and therefore lack complete validation data [1]. This creates a significant compliance gap for laboratories requiring immediate use of these methods for routine testing or regulatory submissions.
This guide addresses the strategic approach to this challenge, framed within the context of ISO 16140 method verification standards. The ISO 16140 series, particularly Part 3, provides a structured pathway for laboratories to verify non-validated reference methods during a defined transition period [1]. This process ensures data integrity and regulatory compliance even while the standardization bodies work towards full validation of these reference methods. For researchers and drug development professionals, understanding this protocol is essential for maintaining operational continuity without compromising scientific rigor during this interim phase.
Regulatory Background and the Concept of Transition Periods
The Validation-Verification Distinction
A foundational principle in laboratory quality systems is the distinction between method validation and method verification. Method validation is a comprehensive process that proves an analytical method is acceptable for its intended use, establishing its performance characteristics through rigorous testing of parameters such as accuracy, precision, specificity, detection limit, quantitation limit, linearity, and robustness [6] [8]. It is typically required when developing new methods or when a method is significantly modified.
In contrast, method verification is the process whereby a laboratory provides objective evidence that a previously validated method is suited for, and performs as expected within, its specific environment and with its personnel [6] [10]. It confirms that the laboratory can competently implement a method that has already been proven fit-for-purpose elsewhere. Under normal circumstances, verification is only applicable to methods that have undergone a full interlaboratory validation study [1].
The Genesis of the Transition Period
The "transition period" is a pragmatic regulatory solution to a historical problem. Many reference methods from authoritative bodies like ISO were established before the current stringent validation requirements defined in standards like ISO 16140 were enacted. Consequently, these methods are technically "non-validated" by today's standards, creating an implementation dilemma for accredited laboratories that are required to use verified methods [1].
Recognizing that standardization organizations need time to validate these existing reference methods, ISO 16140-3 incorporates a transition period protocol. This allows laboratories to verify and use these not-yet-validated reference methods temporarily, pending full validation by the relevant committees [1]. This approach balances the need for methodological rigor with the practical realities of laboratory operation and regulatory compliance.
ISO 16140-3 Framework for Verifying Non-Validated Reference Methods
The Special Case Protocol (Annex F)
For non-validated reference methods, ISO 16140-3 provides a specific protocol outlined in its Annex F [1]. This annex serves as the primary guide for laboratories navigating the transition period. The core objective of this protocol is to demonstrate that the laboratory can perform the non-validated reference method reliably and that the method itself produces acceptable results for the laboratory's intended sample types.
The verification process under Annex F involves testing the method's performance characteristics, which may include [1] [10]:
- Accuracy/Trueness: Demonstrating closeness of agreement between the test result and an accepted reference value.
- Precision: Evaluating the closeness of agreement among a series of measurements under specified conditions (e.g., repeatability, intermediate precision).
- Specificity/Selectivity: Ability to assess the analyte unequivocally in the presence of other components.
- Limit of Detection (LOD): The lowest amount of analyte that can be detected, but not necessarily quantified.
- Limit of Quantitation (LOQ): The lowest amount of analyte that can be quantitatively determined with suitable precision and accuracy.
- Linearity: The ability of the method to obtain test results directly proportional to the analyte concentration.
- Range: The interval between the upper and lower concentrations of analyte for which the method has suitable precision, accuracy, and linearity.
- Robustness: A measure of the method's capacity to remain unaffected by small, deliberate variations in procedural parameters.
The extent of verification is risk-based and depends on factors such as the method's complexity, the laboratory's prior experience, the type of instrumentation, and the nature of the samples being tested [10].
Experimental Design and Selection of Sample Items
A critical aspect of the verification study is the careful selection of sample items (e.g., food categories, pharmaceutical products) that are representative of the laboratory's future testing scope. ISO 16140-3 provides guidance on selecting categories and items based on the intended scope of laboratory application [1].
The following table outlines the core performance characteristics typically assessed during the verification of a non-validated reference method, along with their experimental considerations.
Table 1: Performance Characteristics for Verification of Non-Validated Reference Methods
| Performance Characteristic | Experimental Protocol & Methodology | Key Considerations |
|---|---|---|
| Accuracy/Trueness | Analysis of certified reference materials (CRMs) or spiked samples at known concentrations; comparison with results from a validated reference method. | Recovery rates should fall within acceptable predefined limits (e.g., 80-120% for certain analytes). |
| Precision | Multiple analyses of homogeneous samples by the same analyst on the same day (repeatability) and by different analysts/different days (intermediate precision). | Expressed as relative standard deviation (RSD%); acceptance criteria depend on the analyte and matrix. |
| Specificity/Selectivity | Analysis of samples containing potentially interfering substances to demonstrate that the method can distinguish and quantify the analyte. | Critical for complex matrices like food, feed, or biological samples. |
| Limit of Detection (LOD) & Quantitation (LOQ) | Analysis of blank and low-concentration samples; LOD/LOQ can be determined via signal-to-noise ratio or based on the standard deviation of the response and the slope. | Must be sufficient for the method's intended purpose, such as detecting contaminants at regulatory limits. |
| Linearity & Range | Analysis of a calibration curve using a series of standard solutions across the claimed range of the method. | The correlation coefficient (r) is typically ≥0.99 for quantitative methods. |
Workflow for Verification During the Transition Period
The process for verifying a non-validated reference method follows a logical sequence from initial assessment to final implementation. The diagram below visualizes this workflow, from identifying the need for verification to the final implementation of the method for routine use.
Practical Implementation and the Scientist's Toolkit
Essential Research Reagent Solutions
Successfully executing a verification protocol requires careful selection and use of key materials. The following table details essential reagents and their critical functions in the verification process.
Table 2: Key Research Reagent Solutions for Method Verification
| Reagent/Material | Function in Verification Protocol |
|---|---|
| Certified Reference Materials (CRMs) | Provides a matrix-matched material with a certified analyte concentration; essential for determining method accuracy/trueness and for calibration. |
| In-House Reference Standards | A well-characterized, stable material used as a secondary standard for daily system suitability tests and quality control during the verification study. |
| Commercial Quality Control Samples | Used to monitor the precision and stability of the method over time during the verification experiments. |
| Selective Agar Media & Enrichment Broths | For microbiological methods, these are used to assess specificity and the ability to recover target microorganisms from a complex background flora. |
| Analytical Grade Solvents & Reagents | Ensure robustness and reproducibility of the method by minimizing variability and contamination introduced by low-purity chemicals. |
Navigating Food Categories and Matrices
A particular complexity in verifying microbiological methods for the food chain is the immense diversity of sample matrices. ISO 16140-2 defines a system of categories (e.g., heat-processed milk and dairy products, raw meat, ready-to-eat foods) to manage this diversity [1]. During the validation of an alternative method, a "broad range of foods" is often claimed after successful testing of a minimum of five out of the fifteen defined food categories.
For verification, a laboratory must strategically select challenging food items from within its own testing scope that may differ from those used in the original validation study. This "food item verification" stage demonstrates that the laboratory is capable of testing the specific, often challenging, items relevant to its operations [1].
The protocol for verifying non-validated reference methods during the transition period is a vital mechanism for ensuring laboratory compliance and data quality while standardization bodies work towards full method validation. For researchers and drug development professionals, the structured approach outlined in ISO 16140-3 Annex F provides a scientifically defensible pathway to implement these necessary methods.
Adhering to this protocol requires meticulous experimental design, careful documentation, and a clear understanding of the method's intended scope. As the deadlines for the transition period approach (e.g., the 2028 deadline for validating larger test portion sizes [1]), laboratories should proactively plan for the eventual full validation of these reference methods. Ultimately, this process underscores a shared commitment to scientific rigor and public health protection, bridging historical practices with contemporary quality standards.
In the pharmaceutical industry, liquid chromatography-mass spectrometry (LC-MS) has become the predominant analytical method for the quantitative determination of analytes in biological matrices due to its high specificity, sensitivity, and throughput [32] [33]. However, the accuracy and reliability of these methods can be significantly compromised by matrix effects (ME), a phenomenon where compounds co-eluting with the analyte interfere with the ionization process in the mass spectrometer, leading to ion suppression or enhancement [32] [33]. These effects introduce substantial challenges during method validation, negatively affecting critical parameters such as reproducibility, linearity, accuracy, and sensitivity [32]. Within the framework of ISO 16140 method verification standards, demonstrating that a method is robust to matrix effects is crucial for establishing its fitness for purpose in regulated laboratories [1]. This technical guide explores the detection and elimination strategies for matrix effects, providing a structured approach for researchers and scientists developing and validating analytical methods for challenging pharmaceutical samples.
Understanding Matrix Effects: Mechanisms and Impact
Matrix effects occur when interfering compounds from the sample matrix co-elute with the target analyte and alter its ionization efficiency in the mass spectrometer interface [32] [33]. The mechanisms behind these effects vary depending on the ionization technique. In electrospray ionization (ESI), ionization occurs in the liquid phase before the charged analyte is transferred to the gas phase. Interfering compounds can compete for charge or disrupt droplet formation and evaporation, leading to signal suppression [32]. In contrast, atmospheric pressure chemical ionization (APCI), where the analyte is transferred to the gas phase as a neutral molecule before ionization, is generally less prone to matrix effects, though they are not eliminated entirely [32]. The interfering species can range from hydrophilic molecules like inorganic salts in urine to hydrophobic compounds such as phospholipids, proteins, and metabolites in plasma and other biological fluids [32]. The extent of matrix effects is often unpredictable and can vary significantly between different sample matrices, different lots of the same matrix, and even between different analytes in the same sample [32]. This variability poses a significant threat to the accuracy of quantitative results, as it can lead to both false positives and false negatives, ultimately compromising drug development and quality control decisions.
Detection and Evaluation of Matrix Effects
Early assessment of matrix effects is critical for developing rugged and precise analytical methods. The evaluation should not be merely a final step in validation but an integral part of method development [32]. The table below summarizes the primary techniques used for evaluating matrix effects.
Table 1: Methods for the Evaluation of Matrix Effects in LC-MS
| Method Name | Description | Output | Key Limitations |
|---|---|---|---|
| Post-Column Infusion [32] [33] | A constant flow of analyte is infused post-column while a blank matrix extract is injected. | Qualitative profile of ion suppression/enhancement across the chromatographic run. | Does not provide quantitative data; laborious and requires specialized setup [32]. |
| Post-Extraction Spike [32] [33] | The response of an analyte spiked into a blank matrix extract is compared to its response in a pure solution. | Quantitative measurement of matrix effect at a specific concentration (e.g., % suppression/enhancement). | Requires a blank matrix, which is not available for endogenous analytes [32]. |
| Slope Ratio Analysis [32] | The slope of a calibration curve in matrix is compared to the slope in a pure solution across a concentration range. | Semi-quantitative assessment of matrix effect over the entire calibration range. | Only provides a semi-quantitative result [32]. |
Detailed Experimental Protocols
Protocol for Post-Column Infusion [32] [33]
- Setup: Connect a T-piece between the HPLC column outlet and the MS ion source. A syringe pump is used to deliver a constant infusion of the analyte standard solution at a defined concentration and flow rate.
- Analysis: Inject a processed blank sample extract (e.g., blank plasma extract) onto the LC column. Use the intended chromatographic method with MS detection.
- Data Interpretation: A stable signal baseline indicates no matrix effects. A depression in the signal (a "dip") indicates ion suppression at that specific retention time, while a signal increase indicates ion enhancement. This helps identify "clean" retention windows for the analyte.
Protocol for Post-Extraction Spike Method [32] [33]
- Sample Preparation: Prepare at least six lots of blank matrix. Process them according to the intended sample preparation procedure.
- Spiking: Spike the analyte of interest into the processed blank matrix extracts at a low, mid, and high concentration (within the calibration range). Also, prepare standard solutions of the analyte in a pure solvent (e.g., mobile phase) at the same concentrations.
- Analysis: Analyze all samples and calculate the peak areas.
- Calculation: Calculate the matrix effect (ME) for each lot and concentration using the formula:
- ME (%) = (Peak Area of analyte in spiked matrix extract / Peak Area of analyte in pure solution) × 100%
- A value of 100% indicates no matrix effect, <100% indicates suppression, and >100% indicates enhancement. The precision (relative standard deviation, RSD) of the ME across different matrix lots should also be calculated.
Strategies for Minimizing Matrix Effects
When method sensitivity is crucial, the primary goal is to minimize matrix effects by preventing interfering compounds from reaching the ion source [32]. The following table outlines key strategies.
Table 2: Strategies for Minimizing Matrix Effects in LC-MS
| Strategy Category | Specific Approach | Mechanism of Action | Considerations |
|---|---|---|---|
| Sample Preparation | Solid-Phase Extraction (SPE) | Selectively retains analyte and/or removes interfering compounds. | Recovery must be optimized; can be expensive [32] [33]. |
| Protein Precipitation (PPT) | Removes proteins by denaturation. | Can be ineffective for phospholipids and may concentrate other interferences [32]. | |
| Liquid-Liquid Extraction (LLE) | Partitions analyte and interferences based on solubility. | Good for non-polar analytes; may not remove all interferences [33]. | |
| Selective Sorbents (e.g., MIP) | Uses tailored materials to bind specific interferences. | Highly effective but not always commercially available [32]. | |
| Chromatography | Improved Separation | Increases resolution to separate analyte from co-eluting interferences. | The most effective approach; may require longer run times [32] [33]. |
| Column Chemistry | Switching to alternative stationary phases (e.g., HILIC). | Can alter retention of interferents. | |
| Mobile Phase Additives | Using volatile additives to modify selectivity. | Some additives can suppress signal [33]. | |
| MS & Instrumentation | Sample Dilution | Reduces absolute amount of matrix entering the system. | Only feasible for very sensitive assays [33]. |
| Source Conditions | Optimizing desolvation temperature and gas flows. | Can help but often insufficient for strong MEs [33]. | |
| Use of APCI/APPI | Switching to less ME-prone ionization techniques. | APCI is often less susceptible than ESI [32]. |
Detailed Protocol: Standard Addition Method
The standard addition method is a powerful technique to compensate for matrix effects, especially for endogenous analytes where a blank matrix is unavailable [33]. It accounts for the specific matrix effect in each individual sample.
Procedure [33]:
- Sample Aliquots: Take at least four aliquots of the identical sample.
- Spiking: Leave one aliquot unspiked (the "sample"). Spike the remaining aliquots with known and increasing amounts of the analyte standard.
- Analysis: Analyze all aliquots using the LC-MS method.
- Calibration and Calculation: Plot the measured instrument response (peak area) against the concentration of the added standard. Extrapolate the line backwards until it intersects the x-axis. The absolute value of the x-intercept represents the original concentration of the analyte in the sample. This method inherently corrects for the matrix effect present in that specific sample.
Strategies for Compensating for Matrix Effects
When minimization strategies are insufficient, compensation techniques are required. The choice of strategy often depends on the availability of a blank matrix [32].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Addressing Matrix Effects
| Item | Function/Description | Application Context |
|---|---|---|
| Stable Isotope-Labeled Internal Standard (SIL-IS) | An isotopically labeled version of the analyte (e.g., with ²H, ¹³C, ¹âµN) that has nearly identical chemical and chromatographic properties but a different mass. It is the gold standard for compensating for matrix effects as it co-elutes with the analyte and experiences the same ionization suppression/enhancement [33]. | Quantification of drugs and metabolites in biological fluids; considered the most effective compensation strategy. |
| Structural Analogue Internal Standard | A compound with a similar chemical structure and chromatographic retention to the analyte. A less expensive alternative to SIL-IS, though its effectiveness can be lower if it does not perfectly mimic the analyte's behavior [33]. | Method development when SIL-IS is prohibitively expensive or unavailable. |
| Blank Matrix | A biological fluid (e.g., plasma, urine) from which the endogenous analyte has been removed or is confirmed to be absent. Used for preparing calibration standards and quality control samples in the matrix-matching technique [32] [33]. | Preparation of calibration curves for exogenous compounds; essential for the post-extraction spike method. |
| Surrogate Matrix | An alternative matrix (e.g., buffer, stripped serum, artificial urine) used to prepare calibration standards when a true blank matrix is unavailable. Its suitability must be demonstrated by showing a similar MS response for the analyte compared to the original matrix [32]. | Quantification of endogenous compounds where a true blank is impossible to obtain. |
| Selective Sorbents (e.g., Phospholipid Removal Plates) | Specialized SPE sorbents designed to remove specific classes of interfering compounds, such as phospholipids, which are a major cause of ion suppression in ESI [32]. | Sample preparation for plasma/serum assays to proactively minimize matrix effects at the source. |
Integration with ISO 16140 Method Verification Framework
The strategies for addressing matrix effects are not standalone exercises; they are integral components of method validation and verification as outlined in the ISO 16140 series [1]. Before a method is used in a laboratory, it must first be validated (proven fit-for-purpose) and then verified (the laboratory must demonstrate it can perform the method correctly) [1]. ISO 16140-3 specifically provides the protocol for the verification of reference methods and validated alternative methods in a single laboratory [20] [1]. The standard outlines a two-stage verification process: implementation verification (demonstrating the lab can perform the method correctly using an item from the validation study) and (food) item verification (demonstrating capability for challenging items within the lab's scope) [1]. While the terminology is derived from food microbiology, the principles are directly transferable to pharmaceutical analysis. A robust study evaluating matrix effects, using the detection and compensation strategies detailed in this guide, provides essential data to support both the validation and verification process, ensuring regulatory compliance and the generation of reliable, high-quality data.
Matrix effects present a significant challenge in the quantitative LC-MS analysis of pharmaceutical samples, but their impact can be managed through a systematic approach. A combination of effective sample preparation, chromatographic optimization, and the judicious application of compensation techniques like stable isotope-labeled internal standards or the standard addition method forms the cornerstone of a robust strategy. By integrating these practices into the method development and validation workflow, and aligning them with the rigorous principles of standards like the ISO 16140 series, scientists can ensure their analytical methods produce accurate, reliable, and defensible results, thereby supporting the entire drug development and quality control pipeline.
Troubleshooting Common PCR Inhibition Issues in Complex Samples
Polymerase chain reaction (PCR) inhibition is a frequent and significant challenge in molecular diagnostics and environmental testing, particularly when analyzing complex samples. Inhibitors are heterogeneous substances that can originate from the sample itself or be introduced during processing, leading to partial inhibition, underestimation of target nucleic acids, or complete amplification failure [34]. The complex matrix of wastewater, for example, contains various inhibitory substances including complex polysaccharides, lipids, proteins, metal ions, RNases, and other compounds that interfere with molecular-based detection methods [35]. Similarly, clinical samples like blood, stool, and respiratory specimens contain inherent inhibitors such as immunoglobulins, hematin, and complex polysaccharides that can compromise PCR efficiency [36] [34].
In the context of regulatory compliance and method validation, understanding and mitigating PCR inhibition is essential for developing robust detection assays. The ISO 16140 series provides a framework for method validation and verification, emphasizing the need for reliable performance characteristics across different sample matrices [1]. This technical guide examines the mechanisms of PCR inhibition, detection methods, and mitigation strategies within a structured quality assurance framework, providing researchers with practical approaches for overcoming inhibition in complex samples.
Biochemical Mechanisms of Inhibition
PCR inhibitors interfere with the amplification process through multiple biochemical mechanisms. Inhibitors may bind directly to single or double-stranded nucleic acids, preventing primer annealing or template denaturation. For example, humic acids interact with both template DNA and polymerase, preventing the enzymatic reaction even at low concentrations [34]. Other inhibitors, including calcium and complexing agents like tannic acids, deplete magnesium ions that are essential cofactors for DNA polymerase activity [34]. DNA polymerase degradation represents another mechanism, where proteases, detergents, urea, or phenol present in samples can degrade or denature the enzyme [34]. In real-time PCR assays, additional interference can occur with fluorescent probes or through increased background fluorescence, affecting quantification accuracy [34].
Common Inhibitors by Sample Type
The sources of PCR inhibitors vary significantly across different sample matrices, each presenting unique challenges:
- Blood-derived samples: Contain immunoglobulin G (IgG), which has high affinity for single-stranded DNA, hematin, and heparin [34].
- Stool and fecal samples: Feature complex polysaccharides, bilirubin, bile salts, and various metabolic products [36].
- Plant materials: Contain polysaccharides (dextran sulfate, xylan) and phenolic compounds that inhibit PCR, particularly in RT-PCR assays [34].
- Environmental samples (wastewater, soil, sludge): Include humic and fulvic acids, fats, proteins, polyphenols, heavy metals, and detergents [35] [34].
- Food and cosmetic matrices: Comprise fats, proteins, preservatives, and emulsifiers that can interfere with amplification [28].
Table 1: Common PCR Inhibitors and Their Mechanisms of Action
| Sample Type | Common Inhibitors | Primary Inhibition Mechanism |
|---|---|---|
| Blood | IgG, hematin, heparin | Binds to single-stranded DNA, inhibits polymerase |
| Stool | Polysaccharides, bilirubin | Polymerase inhibition, magnesium chelation |
| Wastewater | Humic acids, metals, RNases | Interaction with template and polymerase |
| Plant tissues | Polyphenols, polysaccharides | Polymerase degradation, nucleic acid binding |
| Milk | Calcium, plasmin | Competitive magnesium binding, enzyme degradation |
| Soil | Humic substances, organic matter | Nucleic acid binding, polymerase inhibition |
Detection and Assessment of PCR Inhibition
Internal Amplification Controls
Effective detection of PCR inhibition requires appropriate controls that mimic the behavior of target nucleic acids. Pathogen-specific amplification controls consist of target DNA sequences added to the reaction, with inhibition indicated by a significant change in the quantification cycle (Cq) compared to expected values [36]. Alternatively, heterologous internal controls use synthetic sequences lacking homology to biological sequences, such as the XenoRNA Control, which are added during sample preparation [37]. These controls should be introduced early in the extraction process to monitor both extraction efficiency and amplification inhibition.
Quantitative Assessment Methods
The cycle threshold (Cq) shift approach compares the Cq values of internal controls in unknown samples versus negative controls, with significant delays (typically ≥3 cycles) indicating inhibition [36]. For human-derived samples, amplification of reference genes like albumin or RNase P can be used, though this approach has limitations due to variable human DNA content across samples [36]. Standard curve deviations in quantitative PCR, particularly changes in amplification efficiency, can also signal the presence of inhibitors, while digital PCR platforms may show reductions in positive partitions or changes in cluster patterns in the presence of inhibitors [35].
Strategies for Overcoming PCR Inhibition
Sample Preparation and Purification
Effective sample preparation is the first line of defense against PCR inhibition. Sample dilution represents the simplest approach, with 10-fold dilution being commonly effective for reducing inhibitor concentrations, though this also dilutes the target and may affect sensitivity [35]. Improved nucleic acid extraction methods utilizing silica columns, magnetic beads, or cation exchange resins can more selectively purify nucleic acids while removing contaminants [34]. For wastewater samples, commercial inhibitor removal kits containing column matrices specifically designed for efficient removal of polyphenolic compounds, humic acids, and tannins have proven effective [35].
PCR Enhancers and Additives
Various chemical additives can enhance PCR robustness in the presence of inhibitors by multiple mechanisms:
- Proteins: Bovine Serum Albumin (BSA) and T4 gene 32 protein (gp32) bind inhibitory compounds; gp32 at 0.2 μg/μl has shown particular effectiveness in wastewater samples [35].
- Organic solvents: Dimethyl sulfoxide (DMSO) and formamide lower melting temperatures and destabilize secondary structures [35] [34].
- Non-ionic detergents: Tween-20 and Triton X-100 stimulate Taq DNA polymerase activity and reduce false terminations [34].
- Biologically compatible solutes: Betaine and glycerol enhance hydrophobic interactions and reduce strand separation temperatures [34].
Table 2: Effective PCR Enhancers and Their Applications
| Enhancer | Effective Concentration | Recommended Sample Types | Mechanism of Action |
|---|---|---|---|
| T4 gp32 protein | 0.2 μg/μl | Wastewater, environmental | Binds inhibitory substances, protects polymerase |
| BSA | 0.1-0.5 μg/μl | Blood, stool, plants | Binds inhibitors, acts as protease target |
| DMSO | 1-5% | High GC templates | Lowers Tm, prevents secondary structures |
| Betaine | 0.5-1.5 M | Complex templates | Equalizes base stability, reduces secondary structures |
| Tween-20 | 0.1-1% | Various | Stabilizes polymerase, reduces false terminations |
Enzyme Selection and Reaction Optimization
Choosing appropriate DNA polymerases significantly impacts inhibition tolerance. * inhibitor-resistant polymerase blends* demonstrate superior performance in complex matrices; for instance, DNA polymerases from Thermus thermophilus (rTth) and Thermus flavus (Tfl) exhibit maintained efficiency in the presence of 20% blood, whereas Taq polymerase is completely inhibited by just 0.004% blood [34]. Engineered polymerase variants with increased affinity for primer-template complexes or fused to single-stranded DNA binding domains show enhanced resistance to common inhibitors [34]. Additionally, increasing polymerase concentration (within reasonable limits) can sometimes overcome mild inhibition, though this approach requires careful optimization to maintain specificity [34].
Method Verification and ISO 16140 Framework
Validation Within Quality Management Systems
The ISO 16140 series provides standardized protocols for validating alternative microbiological methods, with specific relevance to molecular detection methods in complex matrices [1]. The validation process involves two critical stages: initial method validation to prove the method is fit for purpose, typically through method comparison studies and interlaboratory testing, followed by method verification where a laboratory demonstrates its competence in performing the validated method [1]. For PCR-based methods, this includes establishing performance characteristics such as sensitivity, specificity, accuracy, and robustness in the presence of potential inhibitors.
Implementation in Routine Testing
Implementation verification according to ISO 16140-3 requires testing the same items evaluated in the validation study to demonstrate comparable results [1]. For PCR inhibition assessment, this includes establishing acceptance criteria for internal controls, such as defined Cq value ranges for amplification controls [36]. Item verification further demonstrates laboratory capability for challenging samples within its scope, using defined performance characteristics to confirm method suitability [1]. Ongoing quality control should incorporate inhibition monitoring, with Levey-Jennings charts tracking the performance of positive controls to detect systematic issues related to inhibition [36].
Diagram 1: PCR Inhibition Troubleshooting Workflow
Research Reagent Solutions
Table 3: Essential Research Reagents for PCR Inhibition Management
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Inhibitor-Resistant Polymerases | rTth, Tfl, engineered Taq variants | Maintain activity in inhibitory matrices |
| PCR Enhancers | BSA, T4 gp32 protein, DMSO, betaine | Bind inhibitors, improve amplification efficiency |
| Internal Controls | XenoRNA, pathogen-specific controls | Monitor inhibition in sample processing |
| Nucleic Acid Purification Kits | Silica columns, magnetic beads, inhibitor removal resins | Remove contaminants while preserving nucleic acids |
| Reference Materials | Characterized inhibitory samples (soil, wastewater) | Method validation and quality control |
PCR inhibition in complex samples presents a multifaceted challenge that requires systematic approaches for detection and mitigation. Effective management combines appropriate sample preparation, strategic use of PCR enhancers, selection of robust enzymatic systems, and comprehensive method validation within established quality frameworks like ISO 16140. The continued development of inhibitor-resistant reagents and standardized controls will further enhance the reliability of molecular detection across diverse applications, from clinical diagnostics to environmental monitoring. By implementing these evidence-based strategies, researchers can overcome the persistent challenge of PCR inhibition, ensuring accurate and reproducible results in complex matrices.
In the highly regulated field of drug development and food safety testing, demonstrating the reliability of analytical methods is paramount. The ISO 16140 series provides the international standard for the validation and verification of microbiological methods, offering a structured framework for laboratories, test kit manufacturers, and regulatory authorities [1]. This guidance is particularly crucial for researchers and scientists in pharmaceutical development who must ensure their testing protocols are both scientifically sound and compliant with evolving regulatory expectations.
A fundamental principle within this framework is the clear distinction between two critical stages: method validation and method verification. Validation is the initial process of proving that a method is fit for its intended purpose, typically involving a method comparison study and often an interlaboratory study [1]. Verification, on the other hand, is the subsequent process where a single laboratory demonstrates that it can competently perform a method that has already been validated [1]. The optimization of test portion sizes is a technical consideration that impacts both of these stages, influencing the accuracy, reproducibility, and regulatory acceptance of test results.
The Regulatory Framework: ISO 16140 and Test Portion Sizes
The ISO 16140 Series Structure
The ISO 16140 standard is organized into multiple parts, each addressing specific aspects of method validation and verification. For professionals navigating these requirements, understanding the scope of each part is essential.
Table: Parts of the ISO 16140 Series Relevant to Validation and Verification
| ISO Part | Title | Primary Focus |
|---|---|---|
| ISO 16140-2 | Protocol for the validation of alternative (proprietary) methods against a reference method | Base standard for alternative methods validation, includes interlaboratory studies [1]. |
| ISO 16140-3 | Protocol for the verification of reference methods and validated alternative methods in a single laboratory | Guides laboratories on demonstrating competence with a pre-validated method [1]. |
| ISO 16140-4 | Protocol for method validation in a single laboratory | For validation studies whose results are confined to the laboratory that conducted them [1]. |
The Critical Role of Test Portion Size
The test portion size is a key method parameter defined as the quantity of the test material taken for testing. Its optimization is critical for several reasons:
- Representativeness: A larger test portion may better represent a heterogeneous sample, improving the detection of low-level or unevenly distributed contaminants.
- Statistical Power: Adequate portion size is necessary to meet the statistical requirements for detection limits and quantification.
- Method Compatibility: The test portion must be compatible with the physicochemical constraints of the method (e.g., enrichment volumes, instrument linear range).
The general regulatory principle is that a method, including its specified test portion size, must be validated. Historically, some reference methods were not validated for larger test portion sizes (e.g., 375 g), creating a compliance gap for laboratories needing to use these sizes [1].
Transition Period for Larger Test Portion Validation
Recognizing this gap, standardization organizations have provided a transition pathway. Amendment 1 of ISO 16140-4, published in 2024, outlines a protocol for the validation of larger test portion sizes within a single laboratory [1].
- Transition Period: Laboratories have a temporary allowance until January 1, 2028, to validate larger test portion sizes using the principles in ISO 16140-4:2020/Amd.1:2024 [1].
- Flexibility for Existing Data: The standard offers flexibility for laboratories that already possess validation data for a larger test portion size, acknowledging this as a temporary solution until standardized reference methods are updated [1].
- End-State Goal: Once a larger test portion size is formally validated for a reference method, the requirement for a user laboratory shifts from full validation to a simpler verification that it can achieve performance criteria with that portion size [1].
Experimental Design for Test Portion Size Validation
Validating a test portion size is not an isolated activity; it is an integral part of demonstrating that a method is fit for purpose. The following workflow and experimental protocols provide a roadmap for conducting these studies.
Defining the Experimental Scope
Before commencing laboratory work, a precise experimental plan must be established.
- Objective Definition: Clearly state the purpose—e.g., "to validate a 375g test portion for the detection of Listeria monocytogenes in ready-to-eat meats using [Method Name]."
- Acceptance Criteria: Define pre-defined performance metrics that will signify success. These should be based on regulatory guidelines, stakeholder requirements, and the performance of existing methods.
- For qualitative methods: Sensitivity (PPA), Specificity (NPA), Relative Limit of Detection (RLOD).
- For quantitative methods: Accuracy (e.g., percent recovery), Precision (repeatability and reproducibility), Linearity, and Measurement Uncertainty.
- Sample Selection: Select a representative range of sample matrices. ISO 16140-2 recommends testing a minimum of 5 out of 15 defined food categories to be considered validated for a "broad range of foods" [1]. Categories should be chosen to challenge the method, including those with high fat, protein, or background microflora.
Detailed Experimental Protocol for a Qualitative Method
This protocol outlines the key steps for validating a larger test portion size for a pathogen detection method.
Materials and Reagents
Table: Essential Research Reagent Solutions for Method Validation
| Reagent/Material | Function in the Experiment |
|---|---|
| Reference Strains | Well-characterized target and non-target strains used for inclusivity and exclusivity testing to confirm method specificity. |
| Selective Enrichment Broths | Media designed to promote the growth of the target microorganism while inhibiting competitors. |
| Chromogenic Agar Plates | Culture media containing substrates that produce color changes upon reaction with enzymes specific to the target microbe, allowing for visual identification. |
| Inactivated Sample Matrix | A control sample matrix (e.g., powdered milk, meat slurry) that has been sterilized to provide a consistent, non-infectious background for spiking studies. |
| Buffered Peptone Water | A general-purpose diluent used for preparing serial dilutions of microorganisms and homogenizing sample portions. |
Inclusivity and Exclusivity Testing
- Inclusivity: Test a panel of at least 50-100 genetically diverse strains of the target microorganism. The alternative method with the new test portion should correctly identify ≥ 99% of these strains [1].
- Exclusivity: Test a panel of 20-30 non-target, but closely related, microorganisms. The method should produce negative results for ≥ 99% of these exclusivity strains, confirming high specificity.
Method Comparison Study against a Reference Method
This study directly compares the performance of the alternative method (with the new test portion) against the reference method.
- Sample Preparation: Artificially contaminate a set of samples across the selected food categories at three key levels: a low inoculum level (near the expected limit of detection), a medium level, and a high level. Include an appropriate number of uninoculated negative controls.
- Testing Protocol: For each sample, test the same base homogenate using both the alternative method and the reference method. The study should be conducted in a blinded fashion.
- Data Analysis: Results are compiled into a 2x2 table comparing positive and negative results between the two methods. From this, Percent Positive Agreement (PPA) and Percent Negative Agreement (NPA) are calculated to demonstrate statistical equivalence.
Protocol for Quantitative Method Validation
For quantitative methods (e.g., enumeration of hygiene indicators), the focus shifts to metrics of numerical accuracy.
- Sample Preparation and Testing: Inoculate samples with known concentrations of the target microbe across the dynamic range of the method. Assay these samples using the alternative method with the new test portion.
- Data Analysis:
- Accuracy/Recovery: Calculate the mean percent recovery of the alternative method versus the expected count.
- Precision: Determine the repeatability (within-lab) standard deviation and coefficient of variation.
- Linearity: Assess the relationship between the results from the alternative method and the reference method across the analytical measurement range. A correlation coefficient (r) is often calculated.
Data Analysis and Compliance Documentation
Statistical Analysis of Validation Data
The data collected from the experiments must be rigorously analyzed against the pre-defined acceptance criteria.
Table: Key Performance Characteristics for Method Validation
| Performance Characteristic | Calculation Formula | Acceptance Criterion (Example) |
|---|---|---|
| Percent Positive Agreement (PPA) | (Number of positives by both methods / Number of positives by reference method) x 100 | ≥ 98% [1] |
| Percent Negative Agreement (NPA) | (Number of negatives by both methods / Number of negatives by reference method) x 100 | ≥ 98% [1] |
| Relative Limit of Detection (RLOD) | Comparison of the detection level of the alternative method versus the reference method | Not statistically different or superior |
| Relative Accuracy/Recovery | (Result from alternative method / Expected value from reference method) x 100 | 80 - 110% |
| Precision (CV%) | (Standard Deviation / Mean) x 100 | < 10-15% (dependent on analyte) |
The Pathway from Validation to Routine Verification
Once a method, including its test portion size, is successfully validated, the pathway for its implementation in a user laboratory is clearly defined by the ISO 16140 series, moving from broad validation to laboratory-specific verification.
As shown in the diagram, after a method is validated, a user laboratory must perform a two-stage verification process per ISO 16140-3 [1]:
- Implementation Verification: The laboratory demonstrates it can perform the validated method correctly by testing one of the same items used in the validation study and obtaining a similar result [1].
- Item Verification: The laboratory then demonstrates its capability by testing several challenging food items specific to its scope of testing, confirming the method performs well for these matrices [1].
The optimization of test portion sizes is a scientifically rigorous process embedded within the comprehensive framework of the ISO 16140 standards. For researchers and drug development professionals, adhering to the structured protocols for validation (proving the method is fit-for-purpose) and subsequent verification (proving laboratory competency) is non-negotiable for regulatory compliance and product safety. The ongoing updates to the ISO 16140 series, including the recent amendments for identification methods and the defined transition period for larger test portion sizes, underscore the dynamic nature of quality standards. By proactively engaging with these protocols and meticulously documenting experimental data, laboratories can not only ensure compliance but also contribute to the advancement of robust, reliable analytical methods that safeguard public health.
The ISO 16140 series on microbiology of the food chain method validation represents a comprehensive framework for ensuring the reliability and accuracy of microbiological testing methods in food and feed safety. This technical guide explores how engagement with ISO committee members and participation in structured expert networks provides invaluable insights for effectively implementing these standards. For researchers, scientists, and drug development professionals, understanding the practical application of these standards through the lens of those who create them offers a significant competitive advantage in method verification and validation processes.
The development and maintenance of the ISO 16140 series is facilitated through ISO Technical Committee (TC) 34/Subcommittee (SC) 9/Working Group (WG) 3, which focuses specifically on method validation. These committees bring together global experts from various sectors including testing laboratories, kit manufacturers, food businesses, and regulatory authorities. The collaborative nature of these groups ensures that the standards address real-world challenges while maintaining scientific rigor, making expert participation an essential component for both standards development and implementation [2].
Understanding the ISO 16140 Framework
The ISO 16140 Series Structure
The ISO 16140 series consists of multiple parts, each addressing specific aspects of method validation and verification. Understanding this structure is fundamental to proper implementation:
- Part 1: Vocabulary - Defines essential terminology
- Part 2: Protocol for the validation of alternative (proprietary) methods against a reference method - Serves as the base standard for alternative methods validation [1]
- Part 3: Protocol for the verification of reference methods and validated alternative methods in a single laboratory - Guides laboratories in demonstrating method proficiency [1]
- Part 4: Protocol for method validation in a single laboratory
- Part 5: Protocol for factorial interlaboratory validation for non-proprietary methods
- Part 6: Protocol for the validation of alternative (proprietary) methods for microbiological confirmation and typing procedures
- Part 7: Protocol for the validation of identification methods of microorganisms [1]
This structured approach ensures comprehensive coverage of validation and verification needs across different laboratory scenarios and method types.
Distinction Between Method Validation and Verification
A critical insight from committee experts emphasizes the fundamental distinction between method validation and verification, which represent two mandatory stages before implementing a method in a laboratory:
- Method Validation: Proof that a method is fit for purpose, conducted through method comparison studies and interlaboratory trials [1]
- Method Verification: Demonstration that a laboratory can properly perform a validated method [1]
This distinction is crucial for laboratories to understand their responsibilities when implementing new methods. As emphasized by ISO committee members, verification is only applicable to methods that have been previously validated through interlaboratory studies [1].
Expert Participation Pathways in ISO Committees
Committee Structure and Engagement Models
Engagement with ISO committees follows structured pathways that facilitate effective contribution from domain experts:
Table: ISO Committee Engagement Pathways
| Participation Level | Access & Responsibilities | Expertise Required |
|---|---|---|
| Technical Committee (TC) Level | Direct access to committee documents and ballots; shares information with TAG membership | Broad technical knowledge across domain areas |
| Working Group (WG) Level | Direct access to WG documents and ballots; contributes to specific technical development | Deep specialized expertise in specific methodology |
| U.S. Technical Advisory Group (TAG) | Develops U.S. consensus positions; provides input to ANSI's ISO Team | Representative stakeholder perspective |
U.S. participation in ISO committees is coordinated through ANSI-accredited Technical Advisory Groups (TAGs) that serve as national mirror committees to ISO Technical Committees. These TAGs comprise relevant experts from diverse stakeholder categories who collaborate to develop U.S. consensus positions on ISO activities and ballots [38].
Accessing Committee Documents and Ballots
Committee members gain privileged access to developing standards through structured channels:
- At the ISO Committee level: U.S. TAG leaders receive direct access to ISO Committee documents and ballots, which they disseminate to TAG membership with additional context and voting deadlines [38]
- At the Working Group level: Appointed U.S. experts obtain direct access to their WGs' documents and ballots through the ISO Portal [38]
- Document repositories: The ISO Portal provides centralized access to committee documents, ballots, and meeting materials, facilitating informed contributions from experts [38]
This structured access ensures that committee members can thoroughly review and contribute to developing standards throughout the creation process.
Method Verification Protocols: Insider Perspectives
The Two-Stage Verification Process
ISO 16140-3 outlines a structured two-stage verification process for validated methods, a approach refined through committee expertise:
Stage 1: Implementation Verification focuses on demonstrating that the user laboratory can correctly perform the method by testing one of the same food items evaluated in the validation study. This confirms that laboratory personnel can achieve results comparable to those from the validation study [1].
Stage 2: Item Verification addresses the laboratory's capability to test challenging food items within its specific scope of accreditation. This involves testing several such items and using defined performance characteristics to confirm the method performs adequately for these specific matrices [1].
Food Category Considerations in Verification
Committee experts emphasize the importance of understanding food categories in verification studies. The standard defines a "broad range of foods" as validation across five out of fifteen defined food categories. This approach recognizes the practical limitations of validating methods across all possible food matrices while ensuring sufficient diversity to predict method performance across categories [1].
Table: Key Amendments to ISO 16140 Standards (2024-2025)
| Standard | Amendment & Publication Date | Key Focus Area |
|---|---|---|
| ISO 16140-2 | Amendment 1: September 2024 | New calculations for qualitative method evaluation; RLOD of interlaboratory study; special cases for commercial sterility testing |
| ISO 16140-3 | Amendment 1: August 2025 | Protocol for verification of validated identification methods of microorganisms |
| ISO 16140-4 | Amendment 2: August 2025 | Protocol for single-laboratory validation of identification methods of microorganisms |
Essential Research Reagents and Materials
Implementation of ISO 16140 verification protocols requires specific research reagents and materials to ensure accurate and reproducible results:
Table: Essential Research Reagent Solutions for Method Verification
| Reagent/Material | Function in Verification Process | Application Context |
|---|---|---|
| Reference Materials | Provides benchmark for method performance comparison; essential for implementation verification | Qualitative and quantitative method verification |
| Certified Reference Strains | Ensures accurate microbial identification; validates confirmation procedures | Identification method verification per ISO 16140-7 |
| Selective Agar Media | Supports growth of target microorganisms; validated for specific confirmation procedures | Method confirmation steps as specified in ISO 16140-6 |
| Proprietary Test Kit Components | Manufacturer-specific reagents validated for alternative method performance | Implementation of validated alternative methods |
| Quality Control Materials | Monitors ongoing method performance; detects method drift | Routine quality assurance post-verification |
Experimental Protocols for Method Verification
Protocol 1: Implementation Verification for Qualitative Methods
Based on committee insights, implementation verification for qualitative methods follows this detailed protocol:
- Sample Selection: Obtain the same food item used in the original validation study (as specified in the validation certificate or report)
- Inoculation Preparation: Create samples with target microorganisms at appropriate concentration levels, including near-limit of detection levels
- Testing Protocol: Perform the method according to the manufacturer's instructions or standardized protocol
- Comparison Analysis: Compare results with those obtained in the validation study for concordance
- Acceptance Criteria: Demonstrate equivalent performance within predefined acceptance ranges [1]
This protocol ensures the laboratory can replicate the performance characteristics established during the formal validation process.
Protocol 2: Food Item Verification for Challenging Matrices
For verifying performance with challenging food items specific to a laboratory's scope:
- Item Selection: Select a minimum of three challenging food items representative of the laboratory's testing scope
- Inoculation Strategy: Inoculate items with target microorganisms at specified levels, including low levels to assess detection capability
- Testing Replication: Perform testing with sufficient replication to generate statistically meaningful data (typically minimum of five replicates per level)
- Performance Assessment: Evaluate method performance using defined characteristics including sensitivity, specificity, and accuracy
- Data Analysis: Apply statistical methods to demonstrate method performance meets predefined criteria for the specific food items [1]
Best Practices from ISO Committee Members
Strategic Engagement in Standards Development
Seasoned committee members recommend strategic approaches to maximize the benefits of participation in expert networks:
- Early Engagement: Participate during the drafting stage to influence standard development and gain early insight into upcoming requirements
- Working Group Focus: Join specific Working Groups aligned with organizational needs to develop specialized expertise
- Consensus Building: Collaborate with other TAG members to develop national positions that reflect diverse stakeholder perspectives [38]
- Knowledge Transfer: Establish internal processes to disseminate insights from committee participation to relevant organizational stakeholders
As emphasized by DeAnn Benesh, Global Regulatory Affairs Manager at Neogen and co-leader of the ISO 16140-3 drafting group, participation in drafting committees provides invaluable perspective on the intent and application of standard requirements [2].
Implementation Strategies from Industry Experts
Industry experts involved in committee work recommend specific implementation strategies:
- Phased Implementation: Roll out new standards in phases, prioritizing high-impact areas and allowing for organizational learning
- Cross-Functional Teams: Establish cross-functional implementation teams including quality assurance, technical experts, and laboratory personnel
- Gap Analysis: Conduct thorough gap analyses comparing current practices to new standard requirements before implementation
- Training Investment: Develop comprehensive training programs focused on both the technical requirements and intent behind standard provisions
Benjamin Diep, Food Safety Microbiologist at Nestlé Research and co-project leader of ISO 16140-3, emphasizes that "understanding the rationale behind requirements enables more effective implementation and appropriate adaptation to specific laboratory contexts" [2].
Engagement with ISO committee members and participation in structured expert networks provides invaluable insights for effectively implementing ISO 16140 method verification standards. The structured approaches to verification, clear distinction between validation and verification requirements, and practical implementation protocols developed through committee work offer laboratories robust frameworks for ensuring method competency. As standards continue to evolve through amendments and new parts, ongoing engagement with expert networks remains essential for maintaining current knowledge and influencing future directions. For researchers, scientists, and drug development professionals, leveraging these expert networks represents not merely a compliance activity, but a strategic opportunity to enhance methodological rigor and contribute to the advancement of their fields.
Validation Frameworks and Comparative Analysis: Ensuring Method Reliability
Validation of alternative microbiological methods against reference standards is a critical requirement for researchers, scientists, and drug development professionals implementing new detection technologies. The ISO 16140-2 standard provides a structured framework for this validation process, establishing uniform protocols that ensure methodological rigor and data comparability across laboratories and applications. This technical guide examines the core components of ISO 16140-2 validation, with particular emphasis on sensitivity and selectivity testing—parameters fundamental to demonstrating method reliability. Within the broader context of method verification standards, this framework enables scientific and regulatory acceptance of innovative detection technologies that offer improvements in speed, accuracy, and practicality over traditional approaches.
The validation process encompasses both method comparison studies and interlaboratory studies to establish method performance characteristics [39]. For qualitative methods, which detect the presence or absence of target microorganisms, sensitivity and selectivity represent crucial validation parameters that determine a method's fitness for purpose. The protocol mandates specific testing approaches, statistical analyses, and acceptance criteria that alternative methods must meet to achieve validated status, with dossiers remaining valid for six years before requiring renewal [39].
Sensitivity Testing: Concepts and Experimental Protocols
Understanding Detection Probability Metrics
Sensitivity in qualitative microbiological methods refers to the probability of detecting the target microorganism when it is present in a sample. ISO 16140-2 recognizes that this probability is concentration-dependent and utilizes specific metrics to quantify this relationship.
The Level of Detection at 50% probability (LOD₅₀) represents the microbial concentration that yields 50% positive results and serves as the primary sensitivity parameter in standard ISO 16140-2 evaluations [40]. However, for methods requiring higher sensitivity, particularly those needing to detect very low contamination levels (e.g., 1 cfu/test portion), the Level of Detection at 95% probability (LOD₉₅) provides a more relevant and stringent metric [41] [40]. Establishing LOD₉₅ is critical for methods where failure to detect low-level contamination carries significant health risks, as this value represents the contamination level that will be detected with 95% probability [40].
Table 1: Key Sensitivity Metrics in Qualitative Method Validation
| Metric | Definition | Application Context | Interpretation |
|---|---|---|---|
| LODâ‚…â‚€ | Microbial concentration that yields 50% positive detection results | Standard method validation; ISO 16140-2 primary parameter | Lower values indicate higher sensitivity |
| LOD₉₅ | Microbial concentration that yields 95% positive detection results | High-sensitivity methods; low-level contamination detection | More stringent metric; LOD₉₅ < 1.0 cfu/tp indicates excellent sensitivity |
| Relative Detection Level | Comparison of detection capability between alternative and reference methods | Method comparison studies | Demonstrates non-inferiority or superiority to reference method |
Experimental Protocol for Sensitivity Determination
The experimental design for sensitivity testing requires careful preparation of test samples with accurately determined low microbial concentrations. Recent advances have improved the precision of this process through cell sorting technology.
Sample Preparation with Defined Cell Concentrations:
- Strain Selection: Select appropriate target strains representing relevant microorganisms. For example, in Salmonella detection, include both hydrogen sulfide-producing (e.g., Salmonella Typhimurium FSD287) and non-producing (e.g., Salmonella Westhampton FSD347) strains to assess method robustness [40].
- Cell Sorting: Prepare bacterial suspensions and stain with fluorescent markers such as 6-carboxyfluorescein diacetate (CFDA). Use fluorescence-activated cell sorting (FACS) to deposit precise numbers of cells (e.g., 1, 5, and 10 cfu) into test portions [40].
- Viability Verification: Implement a sequential sorting plan to estimate the Colony Forming Probability (CFP) of sorted cells. Sort 10×10 cells onto culture media before and after experimental sorting to confirm viability exceeds 95% [40].
- Food Matrix Integration: Incorporate sorted cells into relevant food matrices (e.g., beef, shrimp) using 25g test portions. Include blank (uninoculated) controls to confirm absence of background interference [40].
Testing and Data Analysis:
- Replicated Testing: Test each concentration level (0, 1, 5, 10 cfu/test portion) with multiple replicates (typically n≥3) across different laboratories [40].
- Statistical Analysis: For methods demonstrating high sensitivity (all test portions at 1 cfu/test portion positive), introduce virtual results of blank conditions approaching zero to enable LOD₉₅ calculation [40].
- LOD₉₅ Determination: Apply statistical models based on Poisson distribution to calculate LOD₉₅ values. The method meets high-sensitivity criteria when LOD₉₅ < 1.0 cfu/test portion [40].
Figure 1: Experimental Workflow for Sensitivity Determination
Selectivity Testing: Inclusivity and Exclusivity
Defining Selectivity Parameters
Selectivity testing verifies a method's ability to accurately detect target microorganisms while appropriately handling non-target organisms. This parameter comprises two complementary components:
Inclusivity measures the method's capability to detect a wide range of target strains, ensuring reliable detection of genetic, phenotypic, and geographical variations within the target microbial species [41]. Comprehensive inclusivity testing requires evaluating method performance with statistically relevant numbers of strains representing the genetic diversity of the target microorganism.
Exclusivity assesses the method's specificity by confirming that non-target microorganisms, particularly closely related species or normal microflora, do not generate false-positive results. Appropriate exclusivity testing requires selection of non-target strains that are phylogenetically or ecologically relevant to the target microorganism.
Experimental Protocol for Selectivity Assessment
Inclusivity Testing Protocol:
- Strain Selection: Select a panel of approximately 50-100 target strains representing genetic and phenotypic diversity, including various serotypes, genotypes, and geographical origins [41].
- Culture Preparation: Prepare standardized inocula of each strain at an appropriate concentration, typically ranging from 1-10 CFU/mL for high-sensitivity methods [41].
- Testing Procedure: Test each strain in replicate (minimum n=3) using the alternative method alongside the reference method.
- Data Analysis: Calculate the percentage of target strains correctly identified as positive. For validated methods, inclusivity rates should exceed 90-95%.
Exclusivity Testing Protocol:
- Strain Selection: Select 20-30 non-target strains, including closely related species, normal microflora from relevant matrices, and microorganisms that may produce similar signals.
- Culture Preparation: Prepare standardized inocula at concentrations that challenge the method's specificity (typically 10³-10ⵠCFU/mL).
- Testing Procedure: Test each non-target strain in replicate using the alternative method.
- Data Analysis: Calculate the percentage of non-target strains correctly identified as negative. For validated methods, exclusivity rates should approach 100%.
Table 2: Research Reagent Solutions for Validation Studies
| Reagent/Equipment | Function in Validation | Application Example |
|---|---|---|
| Fluorescence-Activated Cell Sorter | Precise deposition of single cells for sensitivity studies | Sorting Salmonella at 1, 5, 10 cfu/25g test portion [40] |
| CFDA Stain | Fluorescent labeling for viability assessment and cell sorting | Differentiating viable Salmonella cells during sorting [40] |
| Selective Culture Media | Strain isolation and characterization in selectivity studies | Using CHROMagar Salmonella and DHL agar for Salmonella detection [40] |
| Reference Strains | Method comparability and performance benchmarks | Using FSD287 (Hâ‚‚S+) and FSD347 (Hâ‚‚S-) Salmonella strains [40] |
| Food Matrices | Assessment of matrix effects on method performance | Testing with high-fat, high-pH, or complex food samples [41] |
Advanced Applications and Case Studies
Commercial Sterility Method Validation
The application of ISO 16140-2 principles to commercial sterility testing demonstrates the adaptability of this validation framework to specialized applications. A proposed protocol for commercial sterility methods evaluates alternative technologies against traditional direct streaking methods using inclusivity and LOD₉₅ as performance criteria [41].
In this context, inclusivity testing determines the method's ability to detect all relevant spoilage microorganisms, including both sporeforming and non-sporeforming species. The LOD₉₅ assessment establishes the minimum detectable level of contamination, with studies showing that methods based on cellular metabolism (COâ‚‚ production, Oâ‚‚ consumption) demonstrate superior sensitivity (LOD₉₅ < 1 logâ‚â‚€ CFU/mL) compared to ATP-based methods (LOD₉₅ > 3 logâ‚â‚€ CFU/mL) [41]. This performance data enables informed selection of appropriate sterility testing methods based on specific application requirements.
Single-Cell Detection Capability
Advanced validation approaches now address the critical need for detecting single-cell contamination in food and pharmaceutical products. The SALX System for Salmonella detection exemplifies this high-sensitivity capability, successfully detecting single Salmonella cells (1 cfu/25g test portion) with greater than 95% probability when using the LOD₉₅ metric [40].
This level of sensitivity requires modifications to standard validation approaches, including:
- Precise Inoculation Methods: Using cell sorters to deposit single cells with confirmed viability rather than traditional serial dilution approaches [40].
- Enhanced Statistical Models: Incorporating virtual blank results when all test portions at the lowest concentration test positive, enabling LOD₉₅ calculation even for exceptionally sensitive methods [40].
- Strain Diversity Challenges: Including both typical and atypical strains (e.g., hydrogen sulfide non-producing Salmonella) to thoroughly assess detection capability [40].
Figure 2: ISO 16140-2 Validation Parameter Relationships
The ISO 16140-2 validation framework provides a comprehensive, statistically robust foundation for evaluating alternative microbiological methods, with sensitivity and selectivity testing serving as cornerstone parameters. The progression from traditional LOD₅₀ measurements to more stringent LOD₉₅ assessments reflects the increasing demand for methods capable of detecting minimal contamination levels in complex matrices. Similarly, comprehensive inclusivity and exclusivity testing ensures detection reliability across target strain variations while minimizing false positives from non-target microorganisms.
For researchers and drug development professionals, adherence to these validation protocols generates the compelling data necessary for scientific and regulatory acceptance. The continuing evolution of these standards, particularly regarding single-cell detection and commercial sterility applications, demonstrates the framework's adaptability to emerging technological capabilities and public health requirements. Through rigorous application of these validation principles, the scientific community can confidently implement innovative detection technologies that enhance product safety while maintaining methodological rigor.
Within the rigorous framework of food safety and public health, the verification of microbiological methods is a critical undertaking for any laboratory. This process ensures that the methods used to detect and identify pathogens are reliable, accurate, and fit for their intended purpose. The international standard ISO 16140-3 provides a structured protocol for this verification, specifically for reference methods and validated alternative methods in a single laboratory [20]. A recent amendment, ISO 16140-3:2021/Amd 1:2025, has further expanded this protocol to include validated identification methods of microorganisms, underscoring the dynamic nature of this field and the need for continuous alignment with technological advancements [20]. This guide is framed within the broader context of a thesis on ISO 16140 method verification standards, which serves as the foundational doctrine for ensuring analytical quality and compliance in research and routine testing.
The core objective of a comparative analysis is to generate robust, defensible data that demonstrates an alternative method performs at least as well as the established reference standard. This is not merely an academic exercise but a practical necessity for laboratories seeking to implement faster, more efficient, or more specific methods without compromising the integrity of their results. The process involves a detailed experimental design, meticulous data collection, and a clear presentation of findings to prove the method's validity for its intended scope, including specific food matrices [42].
Core Principles and Regulatory Framework of ISO 16140-3
The ISO 16140 series is designed to harmonize method validation procedures internationally. Part 3 of this standard focuses on the "verification" step, which is the process a user laboratory undertakes to demonstrate its competence in performing a method that has already been formally validated in an interlaboratory study. The verification protocol confirms that the method's performance characteristics, as stated in the validation report, can be achieved in the hands of the user laboratory's personnel, using its equipment, and on its specific sample types [42].
The standard provides detailed criteria on key considerations such as:
- Method and Laboratory Scope: Defining the exact boundaries of the verification, including the microorganisms and food matrices covered.
- Sample Inoculation and Preparation: Standardizing how samples are artificially contaminated or prepared to ensure a fair and reproducible comparison.
- Number of Replicates and Tests: Specifying the minimum data required for a statistically sound analysis.
- Evaluation and Interpretation of Results: Providing the framework and statistical tools for comparing the alternative method's results against the reference method, leading to a conclusive determination of the method's suitability [42].
The 2025 amendment (Amd 1:2025) explicitly incorporates protocols for verification of identification methods, which is crucial for laboratories using phenotypic, genotypic, or proteomic methods to confirm the identity of isolated microorganisms [20] [43]. Adherence to this structured framework is essential for generating data that is accepted by regulatory bodies and the scientific community.
Experimental Design and Verification Protocol
A successful verification study requires a meticulously planned experimental protocol. The following section outlines the core methodology for comparing an alternative method against a reference standard.
Workflow for Method Verification
The diagram below illustrates the logical workflow for conducting a method verification study, from initial planning to final implementation.
Detailed Methodologies for Key Experiments
The verification process hinges on a set of key experiments designed to measure the alternative method's performance against the reference method. The core principle is the parallel testing of a representative set of samples, often including artificially inoculated (sterile and/or contaminated) samples and naturally contaminated samples, using both methods [42].
Selectivity/Specificity Testing:
- Objective: To confirm that the alternative method correctly identifies the target microorganism and does not produce false positives with a panel of non-target, but closely related, microorganisms.
- Protocol: Inoculate a range of pure cultures of the target microorganism and non-target strains into the appropriate food matrices. Process these samples through both the alternative and reference methods. Record the number of true positives, true negatives, false positives, and false negatives.
Inclusivity/Exclusivity Testing:
- Objective (Inclusivity): To demonstrate the method's ability to detect a diverse set of strains within the target microorganism.
- Objective (Exclusivity): To confirm the method does not react with a panel of non-target microorganisms.
- Protocol: Test a wide panel of well-characterized target strains (inclusivity) and non-target strains (exclusivity) from international culture collections. The results are often presented as the percentage of correct reactions.
Detection Limit and Quantification Limit Studies:
- Objective: To determine the lowest number of microorganisms that can be reliably detected (Qualitative methods) or quantified (Quantitative methods) by the alternative method.
- Protocol: Prepare a series of samples inoculated with decreasing concentrations of the target microorganism. For qualitative methods, the detection limit is the lowest level at which all replicates yield a positive result. For quantitative methods, a calibration curve is established, and the limit is calculated based on signal-to-noise ratios or statistical variability.
Precision and Accuracy Studies:
- Objective (Precision): To measure the repeatability (within-lab, same operator, same equipment) of the alternative method.
- Objective (Accuracy): To determine the closeness of agreement between the result from the alternative method and the accepted reference value.
- Protocol: Analyze multiple replicates of a homogeneous sample at different contamination levels on the same day (repeatability) and on different days (intermediate precision). Accuracy can be assessed by comparing the mean result from the alternative method to the reference method's result or a known spiked value.
Data Presentation and Analysis
The heart of any research lies in its data, and the effective communication of comparative results is paramount [44]. Data should be presented in a way that allows readers to quickly grasp the key findings and the relationship between the alternative and reference methods.
The following table summarizes the types of quantitative data and performance criteria typically evaluated in a comparative analysis.
Table 1: Key Performance Indicators for Method Verification Comparative Analysis
| Performance Criterion | Description | Experimental Measure | Target Acceptance Limit (Example) |
|---|---|---|---|
| Relative Accuracy/Sensitivity | Proportion of actual positives correctly identified | (Number of True Positives) / (True Positives + False Negatives) | ≥ Equivalent to reference method |
| Relative Specificity | Proportion of actual negatives correctly identified | (Number of True Negatives) / (True Negatives + False Positives) | ≥ Equivalent to reference method |
| Detection Limit (LOD) | Lowest quantity reliably detected | Lowest inoculation level with 95% positive detection | Within one dilution of reference method |
| Quantification Limit (LOQ) | Lowest quantity reliably measured | Lowest level with defined precision and accuracy | Meets pre-defined statistical criteria |
| Precision (Repeatability) | Closeness of agreement between independent results under identical conditions | Standard Deviation or Relative Standard Deviation (%RSD) | %RSD ≤ pre-defined target (e.g., 10%) |
Visualizing Comparative Data
Choosing the right chart is critical for effective data visualization [45]. For method comparison data, several graph types are particularly effective:
- Bar Charts: Excellent for directly comparing performance metrics like sensitivity, specificity, or percent recovery between the reference and alternative methods [45]. They provide a clear, simple comparison of values between discrete categories.
- Line Plots for Averages: Useful for representing data measured at set intervals, such as the mean counts of microorganisms obtained by both methods over a concentration range or time series. Error bars representing standard deviation must be displayed [44].
- Bland-Altman Plots (Not pictured): A specialized scatter plot used to assess the agreement between two quantitative measurement techniques. It plots the difference between the two methods against the average of the two methods, highlighting any systematic bias.
- 2-D Dot Charts & Boxplots: Ideal for showing the full distribution of raw data or summary statistics (medians, quartiles) for results obtained by two methods on the same set of samples, allowing for a visual assessment of central tendency and dispersion [46].
Table 2: Guide to Selecting Comparison Charts for Data Visualization
| Chart Type | Primary Use Case in Method Verification | Advantages | Limitations |
|---|---|---|---|
| Bar Graph [45] | Comparing final performance metrics (e.g., Sensitivity, Specificity) between methods. | Simple, universally understood, clear comparison. | Does not show data distribution or trends over a continuous variable. |
| Line Plot [44] [45] | Depicting trends, such as microbial counts over time or across dilution series for both methods. | Shows trends and relationships between continuous variables. | Can be cluttered with multiple data series; not for categorical data. |
| Boxplot [46] | Visualizing and comparing the distribution (median, IQR, outliers) of quantitative results from two methods. | Summarizes data distribution and identifies outliers; robust for comparing groups. | Hides the exact data points and the shape of the distribution. |
| Scatter Plot [44] | Assessing the correlation and agreement between quantitative results from the reference and alternative method. | Shows the full distribution of raw data and the relationship between two variables. | Can be overplotted with many data points; requires statistical analysis for interpretation. |
The Scientist's Toolkit: Essential Research Reagent Solutions
The execution of a verification study requires a suite of reliable and high-quality materials. The following table details key research reagent solutions and their functions in the context of microbiological method verification.
Table 3: Key Research Reagent Solutions for Microbiological Method Verification
| Reagent / Material | Function in Verification Protocol | Critical Quality Attributes |
|---|---|---|
| Certified Reference Materials (CRMs) | Provides a benchmark with a known, certified concentration of the target microorganism for accuracy and quantification studies. | Certified purity and viability, metrological traceability, stability. |
| Selective & Non-Selective Culture Media | Supports the growth, isolation, and differentiation of target microorganisms as per the reference and alternative methods. | Batch-to-batch consistency, specified selectivity and productivity, shelf-life. |
| Molecular Detection Kits (qPCR) | Used in alternative methods for specific identification and/or quantification of target microbial DNA/RNA. | High specificity and sensitivity, well-characterized limit of detection, minimal inhibition. |
| Immunoassay Reagents (ELISA) | Utilized in alternative methods for detecting microbial antigens or toxins through antibody-antigen reactions. | High affinity and specificity of antibodies, low cross-reactivity, consistent lot performance. |
| Quality Control Strains | Used to confirm the proper functioning of culture media, reagents, and the overall testing process. | Genetically defined, stable phenotypic characteristics. |
| Sample Diluents & Neutralizing Buffers | Used to prepare homogenates, dilute samples, and neutralize residual antimicrobials or disinfectants in the sample. | Effective neutralization, non-toxic to target microbes, preserves microbial viability. |
Visualization and Accessibility in Technical Documentation
Creating clear and accessible visualizations is a fundamental part of modern scientific communication. This is especially important for complex diagrams like workflows and organizational charts.
Accessible Diagram Design
When creating diagrams, it is essential to ensure they are accessible to all users, including those with visual impairments. Key considerations include:
- Color Contrast: The visual presentation of graphical objects must have a contrast ratio of at least 3:1 against adjacent colors [47]. This applies to lines, shapes, and the boundaries of user interface components. Avoid using thin, faint lines that may disappear due to anti-aliasing.
- Text within Graphics: For any node that contains text, the text color (
fontcolor) must be explicitly set to have high contrast against the node's background color (fillcolor). As demonstrated in the workflow diagram above, using dark text on a light background or vice versa ensures legibility. - Text-Based Alternatives: For flowcharts, a powerful accessibility technique is to provide a text-based version. This can be done using ordered lists with "If X, then go to Y" language for branching decisions, or using headings to communicate hierarchical structure [48]. This text version should be published alongside the visual diagram.
Logical Relationship of Data in Verification Studies
The diagram below illustrates the logical relationship between different data types and the resulting statistical measures that form the conclusion of a verification study. Understanding this relationship is key to proper data analysis.
A rigorous comparative analysis, structured according to standards like ISO 16140-3, is indispensable for integrating new methodologies into the analytical laboratory. This process, from careful experimental design and execution to clear data presentation and accessibility-minded visualization, provides the evidence base needed to confidently adopt alternative methods. By following this structured approach, researchers and drug development professionals can ensure their methods are not only scientifically valid but also compliant with international standards, thereby contributing to the overarching goals of product safety, public health, and scientific integrity.
Interlaboratory studies are a cornerstone of method validation, providing the statistical evidence required to demonstrate that an analytical method produces reliable and consistent results when applied across multiple laboratories, instruments, and operators. Within the framework of the ISO 16140 series on method validation for the food chain, these studies are indispensable for establishing method robustness—the capacity of a method to remain unaffected by small, deliberate variations in method parameters—and transferability across different sites [1]. For researchers and drug development professionals, a successfully validated method through an interlaboratory study signifies that the method is fit-for-purpose and that its performance characteristics, such as precision and trueness, are well-understood and documented. This process moves beyond single-laboratory validation, which, while valuable, cannot account for the between-laboratory variability that is a critical component of a method's real-world applicability [1].
The ISO 16140 standard delineates a clear pathway from method development to implementation. The process begins with method validation, which proves the method is fit for its intended purpose, often through an interlaboratory study. This is followed by method verification, where an end-user laboratory demonstrates its competence to perform the previously validated method correctly [1]. Interlaboratory studies are thus the engine for generating the consensus values and precision data (e.g., repeatability and reproducibility standard deviations) that underpin both validated reference methods and the alternative (proprietary) methods that are validated against them. The structured approach outlined in standards like ISO 16140-2 ensures that all parties—test kit manufacturers, testing laboratories, and regulatory authorities—have a common, reliable protocol for assessing method performance, thereby facilitating acceptance of data in regulatory submissions and commercial transactions [1].
Core Principles and Key Terminology
Foundational Concepts
A deep understanding of the core principles and terminology is essential for designing and interpreting interlaboratory studies. The following concepts are central to establishing method robustness:
- Robustness is the measure of a method's capacity to remain unaffected by small but deliberate variations in procedural parameters, such as incubation temperature, pH of a buffer, or reagent concentration. It provides an indication of the method's reliability during normal usage. While often assessed during initial method development within a single laboratory, its confirmation across different sites is inferred through a successful interlaboratory study.
- Ruggedness is a related term, sometimes used interchangeably with robustness, though it often specifically refers to a method's resilience to environmental or operational conditions that might vary between laboratories, such as different analyst techniques, instrument models, or reagent lots.
- Precision quantifies the degree of agreement between independent test results obtained under stipulated conditions. It is typically expressed in terms of standard deviation and is stratified into different levels [1] [49]:
- Repeatability: Precision under conditions where independent test results are obtained with the same method on identical test items in the same laboratory by the same operator using the same equipment within short intervals of time.
- Intermediate Precision: Precision under conditions where test results are obtained with the same method on identical test items in the same laboratory, but with variations such as different days, different operators, or different equipment.
- Reproducibility: Precision under conditions where test results are obtained with the same method on identical test items in different laboratories, using different operators and different equipment. This represents the highest level of variability and is a primary focus of interlaboratory studies.
The ISO 16140 Framework
The ISO 16140 series provides a structured vocabulary and protocol for method validation and verification [1]:
- Validation is the process of proving that a method is fit for its intended purpose. For alternative methods, this typically involves a method comparison study and an interlaboratory study as per ISO 16140-2.
- Verification is the process whereby a laboratory demonstrates that it can satisfactorily perform a validated method. This is described in ISO 16140-3 and involves two stages: implementation verification and (food) item verification.
- Scope of Validation: The range of sample types (e.g., food categories) for which a method has been validated. A method validated for a "broad range of foods" is one tested on a minimum of 5 out of 15 defined food categories but is expected to perform adequately across all categories within that broad range [1].
Experimental Designs for Interlaboratory Studies
Selecting the appropriate experimental design is critical for efficiently extracting accurate and meaningful performance data from an interlaboratory study. The choice depends on the method's characteristics, the performance parameters to be estimated, and practical constraints like the number of available laboratories.
Balanced and Staggered-Nested Designs
The following diagram illustrates the core workflow and design logic for establishing method robustness through interlaboratory studies.
The two most common designs for estimating precision components are the balanced design and the staggered-nested design.
Balanced Design (e.g., as per ISO 5725-2): In this classical approach, each of the
pparticipating laboratories analyzes the same number of replicatesnfor a given test material. This design is straightforward and allows for the direct estimation of repeatability variance (from within-lab replication) and reproducibility variance (from between-lab differences) using classical Analysis of Variance (ANOVA). However, it is less efficient for estimating more than two variance components.Staggered-Nested Design (as per ISO 5725-3): This is a highly efficient design for estimating multiple components of precision, such as repeatability and intermediate precision, simultaneously [49]. In its simplest form for two factors (e.g., laboratory and day), each laboratory
iobtains three test results. Two results (y_i11, y_i12) are obtained under repeatability conditions (e.g., on the same day by the same analyst), and a third result (y_i21) is obtained under intermediate precision conditions (e.g., on a different day). This structure provides data to estimate variance components for repeatability, the intermediate factor (day), and between-laboratory effects without requiring an impractically large number of replicates per lab [49].
Protocols for Qualitative vs. Quantitative Methods
The ISO 16140 series provides distinct protocols tailored to the nature of the method being validated.
- ISO 16140-2: Validation of Alternative (Quantitative and Qualitative) Methods: This is the base standard for validating proprietary methods against a reference method. It involves a two-phase process: a method comparison study followed by an interlaboratory study. Separate protocols are provided for qualitative methods (assessing metrics like relative sensitivity and specificity) and quantitative methods (assessing metrics like relative trueness and precision) [1].
- ISO 16140-4: Single-Laboratory Validation: This protocol is used when a laboratory validates a method for its own use, or as a first step before a full interlaboratory study. The results are only valid for the laboratory that conducted the study, and subsequent verification by other labs is not applicable [1].
- ISO 16140-3: Verification in a User Laboratory: Once a method is validated, this part provides the protocol for a laboratory to demonstrate it can competently perform the method. This involves an "implementation verification" using one of the items from the validation study, followed by an "item verification" on challenging samples specific to the lab's scope of work [1].
Statistical Analysis and Data Interpretation
Robust statistical analysis is paramount for deriving reliable precision estimates from interlaboratory data, especially given the potential for outliers to skew results.
Classical vs. Robust Statistical Methods
The traditional approach to analyzing data from a balanced interlaboratory study is Analysis of Variance (ANOVA), often preceded by statistical outlier tests to identify and eliminate aberrant data points. However, ANOVA is highly sensitive to deviations from the normal distribution and can be unduly influenced by outliers, which can lead to biased estimates of precision [49].
To overcome these limitations, robust statistical methods are recommended. These methods are resistant to the influence of outliers, eliminating the need for arbitrary outlier rejection rules. A leading robust method is the Q/Hampel method, which uses the Qn estimator for scale and the Hampel estimator for location [49]. This method is characterized by a high breakdown point (the proportion of outlying data the estimator can tolerate) and high efficiency (the ratio of its statistical uncertainty to that of the classical estimator under ideal conditions) [49]. Another robust method mentioned in the literature uses the centroid of probability density functions and the Bhattacharyya coefficient to measure similarity between data distributions, which is also consistent and resistant to outliers [50].
Application to Staggered-Nested Design
The application of the Q/Hampel method to a staggered-nested design involves specific algorithms for calculating the robust reproducibility standard deviation (s_R) and the robust intermediate standard deviation (s_I(1)). The calculations are based on the cumulative distribution of all possible pairwise differences between measurement results, making them less dependent on assumptions of normality [49].
The robust reproducibility standard deviation s_R is calculated from all absolute differences between results from different laboratories. The algorithm involves constructing a cumulative distribution function H_1(x) of these differences, followed by a series of steps involving linear interpolation and the application of a correction factor b_p that depends on the number of laboratories p [49]. The formula is:
s_R = [G_1^{-1}(0.25 + 0.75 * H_1(0))] / [√2 * Φ^{-1}(0.625 + 0.375 * H_1(0))] * b_p
Where Φ^{-1}(q) is the q-th quantile of the standard normal distribution [49].
Similarly, the robust intermediate standard deviation s_I(1) is calculated from the within-laboratory differences between results obtained under intermediate conditions (e.g., different days). The calculation uses a different cumulative distribution function H_2,I(1)(x) and a corresponding correction factor c_p [49]:
s_I(1) = [G_2,I(1)^{-1}(0.5 + 0.5 * H_2,I(1)(0))] / [√2 * Φ^{-1}(0.75 + 0.25 * H_2,I(1)(0))] * c_p
The correction factors b_p and c_p are critical for obtaining unbiased estimates and are derived via extensive simulation studies. They are tabulated for different numbers of laboratories p and can also be calculated using provided functional relationships for p > 12 [49].
Quantitative Data Presentation
The following tables summarize key quantitative data and reagent solutions relevant to interlaboratory studies.
Table 1: Key Precision Metrics and Their Definitions
| Metric | Definition | Typical Expression |
|---|---|---|
| Repeatability Standard Deviation (s_r) | Standard deviation of results obtained under repeatability conditions. | Standard Deviation |
| Reproducibility Standard Deviation (s_R) | Standard deviation of results obtained under reproducibility conditions. | Standard Deviation |
| Intermediate Precision Standard Deviation (s_I(1)) | Standard deviation of results obtained under intermediate precision conditions. | Standard Deviation |
| Robust Mean (x*) | A central value for the measured property calculated using a robust estimator (e.g., Hampel). | Concentration / Level |
Table 2: Research Reagent Solutions for Microbiological Method Validation
| Reagent / Material | Function in Experiment |
|---|---|
| Reference Method Media & Reagents | Serves as the benchmark against which the alternative method's performance is compared for trueness and accuracy. |
| Alternative Method Kit Components | Proprietary reagents, media, and disposables specific to the method being validated; performance is characterized. |
| Certified Reference Materials (CRMs) | Provides a material with a known and accepted reference value for assessing the trueness of the method. |
| Inoculated/Contaminated Test Samples | Artificially contaminated samples with specific target microorganisms at defined levels used to assess accuracy and detection limits. |
| Sterile/Non-Target Matrix Samples | Controls used to confirm the method's specificity and the absence of false-positive results. |
Implementation and Best Practices
A Roadmap for Practitioners
Successfully executing an interlaboratory study requires meticulous planning and adherence to a structured protocol. The following workflow outlines the key stages.
Critical Considerations for Robust Studies
- Material Homogeneity and Stability: The test materials distributed to all laboratories must be homogeneous so that any observed variability is attributable to the method and laboratories, not the material itself. Furthermore, the materials must be stable for the duration of the study to ensure results are comparable.
- Clear and Unambiguous Protocol: The study protocol must be detailed, leaving no room for interpretation on critical steps. This includes precise instructions on sample preparation, equipment calibration, and result interpretation to minimize protocol-induced variability.
- Blind Testing: Where possible, encoding samples and randomizing their order of analysis within each laboratory helps prevent bias and ensures that the data reflects the method's routine performance.
- Handling Discrepant Data: The use of robust statistical methods reduces the need for arbitrary exclusion of data. However, all data, including potential outliers, should be documented and reported. Any decision to exclude data must be justified based on pre-defined, objective criteria related to protocol violations or technical failures, not solely on statistical grounds.
- Scope and Applicability: The conclusions of an interlaboratory study are valid for the matrices and concentration levels tested. Extrapolating performance to other sample types should be done with caution and may require additional verification, as outlined in ISO 16140-3 for item verification [1].
Interlaboratory studies, when designed and executed according to established international standards like the ISO 16140 series, provide the most rigorous demonstration of a method's robustness and transferability. The move towards sophisticated experimental designs, such as the staggered-nested design, allows for the efficient estimation of multiple precision components. Furthermore, the adoption of robust statistical methods, like the Q/Hampel estimator, ensures that the resulting precision data is reliable and resistant to the influence of outlying results, thereby providing a truer picture of a method's performance in the hands of multiple users. For the pharmaceutical industry and other regulated sectors, this robust, data-driven foundation is critical for building confidence in analytical methods, ensuring product quality and safety, and meeting regulatory compliance requirements across different sites and geographies.
ISO 16140-6:2019 serves a distinct role within the broader ISO 16140 series on method validation. While other parts address validation of complete detection or quantification methods, ISO 16140-6 specifically validates alternative confirmation and typing procedures for isolated microorganisms in the food chain [51] [1]. This standard provides the technical protocol for comparing alternative confirmation methods against the confirmation procedure of a reference method, which may include molecular techniques like whole genome sequencing [51]. The scope encompasses confirmation methods for bacteria and fungi from products for human and animal consumption, environmental samples, and primary production stages [51].
This standard addresses a critical gap in microbiological method validation by providing a framework for validating the confirmation step that advances a suspected (presumptive) result to a confirmed positive result [52] [53]. Additionally, it covers validation of alternative typing methods where the reference method could be serological (e.g., serotyping of Salmonella) or molecular (e.g., typing of Shiga toxin-producing E. coli) [51]. This specialized focus makes ISO 16140-6 particularly valuable for laboratories seeking to implement efficient, accurate confirmation and typing techniques while maintaining compliance with international standards.
Core Principles and Scope
General Principle and Technical Protocol
The fundamental principle of ISO 16140-6 involves a comparative analysis where the result of an alternative confirmation method is evaluated against the confirmation procedure of a reference method or an established reference confirmation method [51]. This validation approach ensures that alternative methods provide equivalent or superior reliability compared to traditional confirmation techniques. The standard is particularly applicable to bacteria and fungi, with potential case-by-case application to other microorganisms [51].
The technical protocol specified in ISO 16140-6 enables the replacement (partially or completely) of confirmation procedures described in reference methods or alternative methods validated according to ISO 16140-2, but with a critical restriction: the alternative confirmation method can only be used if one of the isolation agars specified in its validation study is employed [51]. This agar-specific validation requirement represents a crucial limitation that laboratories must observe when implementing validated methods.
Scope and Applications
ISO 16140-6 covers two primary applications with distinct technical purposes:
Alternative Confirmation Methods: These methods are designed to advance suspected (presumptive) results to confirmed positive results for isolated microorganisms [52] [53]. Examples include biochemical confirmation of Enterobacteriaceae as specified in ISO 21528-2 [1].
Alternative Typing Techniques: This includes methods for microbial characterization such as serotyping of Salmonella or molecular typing of Shiga toxin-producing E. coli [51]. These techniques generate specific microbial genotypes or "genovars" that can be linked to established serovars through validated databases [54].
The standard is designed for use by organizations or expert laboratories involved in method validation, but can also be applied by single laboratories performing in-house validation under certain conditions as specified in ISO 16140-4 [51].
Validation Methodology and Experimental Design
Method Comparison Study Framework
The validation process according to ISO 16140-6 requires a rigorous experimental design to demonstrate method equivalence. The validation study must clearly define the selective agar(s) from which strains can be confirmed using the alternative method [52] [53]. This specificity is critical, as the validated confirmation method can only be properly applied to strains recovered on agars that were included and shown to be acceptable within the validation study [1].
The experimental protocol involves testing a representative range of microbial strains recovered from specified isolation agars. For example, in the validation of Check&Trace Salmonella 2.0, the method was validated for confirmation of presumptive Salmonella spp. isolated on non-selective NA and selective XLD agars [54]. The study demonstrated equivalence to the reference method (ISO 6579-1 and ISO 6579-3) for confirmation and typing of 59 Salmonella serovars [54].
Interlaboratory Study Requirements
ISO 16140-6 requires interlaboratory validation to establish method robustness across different laboratory environments [1]. This involves multiple laboratories testing identical sample panels using both the alternative confirmation method and the reference confirmation procedure. The resulting data provides statistical evidence of method equivalence and reliability.
The validation of typing methods follows a similar approach. For instance, the Check&Trace Salmonella 2.0 Assay is a qualitative, semi-automated real-time PCR test that detects genetic variation at 21 loci scattered over the entire Salmonella genome, generating specific genotypes (Genovars) that are linked to traditional serovars through an established database [54]. This method validation demonstrated that DNA typing could effectively replace traditional serotyping for the 59 included serovars.
Table 1: Key Performance Characteristics Assessed in ISO 16140-6 Validation Studies
| Performance Characteristic | Assessment Method | Acceptance Criteria |
|---|---|---|
| Relative Accuracy | Comparison of confirmed positive results between alternative and reference method | Statistical equivalence established |
| Specificity | Ability to correctly identify target microorganisms | Minimum 95% for most applications |
| Inclusivity | Detection of target strains from specified serovars or genotypes | Comprehensive for claimed scope |
| Agar Compatibility | Performance across different isolation agars | Defined for each agar type validated |
| Reproducibility | Consistency across different laboratories | Statistical equivalence established |
Workflow Diagram: ISO 16140-6 Validation Process
The following diagram illustrates the key stages in the ISO 16140-6 validation process for alternative confirmation and typing methods:
Implementation in Laboratory Practice
Practical Application and Limitations
Successfully validated alternative confirmation methods can replace confirmation procedures in reference methods, but with strict adherence to validation parameters. A critical implementation requirement is that the validated confirmation method can only be used when strains are recovered on the specific agar media included in the validation study [52] [53]. This restriction ensures that the validation conditions mirror the actual application conditions.
Practical examples illustrate these limitations:
Proper Use: A PCR-based confirmation method for Listeria monocytogenes validated according to ISO 16140-6 using isolates from ALOA agar can properly be used to confirm suspected L. monocytogenes colonies isolated on ALOA agar from dairy products [52].
Improper Use: The same PCR method would be improperly used for: (a) confirming suspected L. monocytogenes colonies isolated on Oxford agar (different selective agar); (b) confirming suspected Listeria species other than L. monocytogenes; or (c) testing isolates from environmental samples if these weren't included in the validation [52].
Certification and Recognition
Validated methods according to ISO 16140-6 can obtain certification through independent organizations such as MicroVal and AFNOR Certification [54] [55]. These certifications provide formal recognition that the method meets international standards and is equivalent to reference methods for specified applications.
In the European Union, the validation and certification requirements for alternative methods are included in Regulation (EC) 2073/2005 [55]. The NF VALIDATION mark issued by AFNOR Certification specifically meets the three fundamental requirements described in Article 5 of this regulation, giving it European recognition [55]. Similarly, MicroVal certificates demonstrate that alternative methods have undergone rigorous validation according to ISO 16140-6 protocols [54].
Table 2: Examples of Commercially Available Methods Validated According to ISO 16140-6
| Method Name | Technology | Application | Validated Against | Certification Body |
|---|---|---|---|---|
| Check&Trace Salmonella 2.0 | Real-time PCR | Confirmation and typing of Salmonella spp. | ISO 6579-1 and ISO 6579-3 | MicroVal [54] |
| Autof ms1000 | MALDI-TOF Mass Spectrometry | Confirmation of isolated colonies | Reference confirmation methods | MicroVal [54] |
| Foodproof Salmonella Detection Kit | PCR-based detection | Confirmation of Salmonella | Reference methods | MicroVal [54] |
Essential Research Reagents and Materials
The implementation of methods validated according to ISO 16140-6 requires specific research reagents and materials that are critical for maintaining validation integrity. The following table details key components and their functions in confirmation and typing workflows:
Table 3: Essential Research Reagent Solutions for ISO 16140-6 Validated Methods
| Reagent/Material | Function | Application Examples |
|---|---|---|
| Selective Isolation Agars | Recovery and preliminary selection of target microorganisms | ALOA for Listeria, XLD for Salmonella [52] [54] |
| DNA Extraction Kits | Nucleic acid purification for molecular confirmation | foodproof StarPrep One Kit, foodproof Magnetic Preparation Kit [54] |
| PCR Master Mixes | Amplification of target sequences in real-time PCR | Check&Trace Salmonella 2.0 assay components [54] |
| Typing Databases | Reference data linking genetic profiles to serovars | Check&Trace database linking Genovars to Salmonella Serovars [54] |
| Mass Spectrometry Matrix | Protein ionization for MALDI-TOF analysis | Reagents for Autof ms1000 confirmation system [54] |
Relationship to Broader ISO 16140 Framework
ISO 16140-6 occupies a specialized position within the comprehensive ISO 16140 series, which includes seven parts addressing different aspects of method validation and verification [1]. The complete framework includes:
- Part 1: Vocabulary - Defines essential terminology
- Part 2: Protocol for validation of alternative methods - Serves as the base standard
- Part 3: Protocol for method verification - Guides laboratory implementation
- Part 4: Protocol for single-laboratory validation
- Part 5: Protocol for factorial interlaboratory validation
- Part 6: Validation of confirmation and typing methods (this standard)
- Part 7: Protocol for validation of identification methods
The relationship between these standards is illustrated in the following diagram, showing how ISO 16140-6 integrates with the broader validation framework:
This integrated framework ensures that confirmation and typing methods validated according to ISO 16140-6 maintain the same rigorous standards as other validated methods in the series, while addressing the specific technical requirements of confirmation and typing procedures.
ISO 16140-6 provides a specialized validation framework for alternative confirmation and typing methods that is essential for laboratories implementing advanced microbiological techniques. The standard's specific requirements for agar compatibility, method comparison, and interlaboratory study ensure that validated methods deliver reliable, equivalent results to reference methods. As molecular technologies continue to evolve, ISO 16140-6 offers a critical pathway for integrating these advances into routine laboratory practice while maintaining compliance with international standards and regulatory requirements.
Sterility testing stands as a critical quality control checkpoint in the pharmaceutical industry, ensuring that parenteral drugs and advanced therapy medicinal products (ATMPs) are free from viable microorganisms before patient administration [56]. For decades, the compendial sterility test, requiring a 14-day incubation period, has been the standard method, often creating a significant bottleneck in product release [57] [58]. The industry has increasingly sought rapid microbiological methods (RMMs) that can reduce this timeline while maintaining or improving analytical accuracy.
This case study examines the validation of an automated sterility testing system for pharmaceutical products, framed within the rigorous context of ISO 16140 method verification standards [1]. The adoption of alternative methods requires a structured approach to demonstrate they are "fit-for-purpose" and provide equivalent or superior results compared to reference methods. The BACTEC automated blood culture system, originally designed for clinical microbiology, has emerged as a validated alternative for sterility testing of complex products like mesenchymal stromal cells (MSCs) and their extracellular vesicles (EVs) [59] [60]. This study details the experimental protocols, performance data, and implementation framework for successfully validating this automated system, offering researchers and drug development professionals a model for integrating rapid sterility testing into their quality control workflows.
Regulatory and Standards Framework
The ISO 16140 Series for Method Validation and Verification
The ISO 16140 series provides a standardized protocol for the validation and verification of microbiological methods, serving as an indispensable guide for laboratories implementing new testing methodologies [1]. This framework is crucial for ensuring that alternative methods meet the stringent requirements of regulatory agencies for pharmaceutical products.
- Method Validation (ISO 16140-2): This stage involves a method comparison study and an interlaboratory study to prove an alternative method is "fit-for-purpose." For sterility testing, this establishes that the automated system performs equivalently to the compendial method [1].
- Method Verification (ISO 16140-3): This subsequent stage requires a laboratory to demonstrate it can satisfactorily perform a validated method. It consists of implementation verification (testing the same items used in the validation study) and item verification (testing challenging items specific to the laboratory's scope) [1] [2].
Pharmacopeial Standards and Regulatory Guidelines
Automated sterility testing systems must comply with pharmacopeial standards, including the United States Pharmacopeia (USP) chapters <71> (Sterility Tests) and <1223> (Validation of Alternative Microbiological Methods), and the European Pharmacopoeia (EP) chapters 2.6.1 (Sterility) and 5.1.6 (Alternative Methods for Control of Microbiological Quality) [59] [61]. Regulatory agencies, including the U.S. Food and Drug Administration (FDA) and European Medicines Agency (EMA), encourage adopting innovative systems that improve testing efficiency, objectivity, and data integrity [57].
Experimental Design and Methodology
The validation study focused on the BD BACTEC automated microbial detection system. This system uses specialized culture vials containing liquid media and a sensor that detects COâ‚‚ produced by microbial metabolism [59]. The system continuously monitors the vials for increases in COâ‚‚ concentration, indicated by a fluorescence signal, and flags them as positive for microbial growth, providing a rapid, automated, and objective alternative to manual visual inspection [59] [60].
Test Microorganisms and Inoculum Preparation
The validation followed pharmacopeial recommendations by selecting a panel of representative microorganisms, including gram-positive bacteria, gram-negative bacteria, yeasts, and molds [59] [60]. These strains are chosen to challenge the system's ability to detect contamination under various conditions.
Inoculum Preparation Protocol:
- Standard Suspension: A 0.5 McFarland standard suspension (approximately 10⸠CFU/mL) was prepared for each test microorganism [59].
- Serial Dilution: A series of sequential dilutions in 0.9% sterile saline solution was prepared to achieve a low microbial concentration [59].
- Target Inoculum: The final inoculum was adjusted to contain 10 to 50 Colony Forming Units (CFU), simulating a low-level contamination event and testing the system's limit of detection [59]. The viability of the inoculum was confirmed using culture on blood agar or Sabouraud media [59].
Test Solutions and Sample Matrix
To validate the method for specific pharmaceutical applications, the test solutions must represent the actual products. In the case of ATMPs, this includes:
- Culture media used in cell expansion [59]
- Antibiotics and supplements [59]
- Excipients in the final product formulation [59]
- Final product suspension matrices, such as Ringer's Lactate for cell-based products [60]
Experimental Protocol and Suitability Testing
The core validation followed a structured, multi-stage protocol to ensure the sample matrix did not interfere with the detection of microorganisms [60].
- Sterility Testing of Uninoculated Media: Confirmed the initial sterility of all reagents and media used in the testing process [60].
- Growth Promotion Test (GPT): Verified that the culture media in the BACTEC vials supported the growth of a low number of viable microorganisms when inoculated directly. This confirms media performance [60].
- Suitability Testing (Bacteriostasis and Fungistasis Test): This critical step demonstrates the compatibility of the test sample with the system. The test product is inoculated with a low number of microorganisms (≤100 CFU), and the system's ability to detect growth is compared to a positive control (saline inoculated with the same organisms). The test is valid only if all positive controls show growth. The method is suitable if the test solutions also show growth for all inoculated organisms within the same timeframe, proving the product does not possess antimicrobial properties that would mask contamination [59] [60].
- Confirmation with Pharmacopeial Method: The results from the automated system are quantitatively compared to the traditional compendial method to demonstrate equivalence [60].
Diagram of the core experimental workflow for validating an automated sterility testing method, from microbial preparation to establishing equivalence with the compendial method.
Results and Performance Data
Quantitative Validation Metrics
The validation of the BACTEC system against pharmacopeial standards demonstrated strong performance across key metrics, confirming its suitability as an alternative sterility testing method [59] [60].
Table 1: Key Performance Metrics for Automated Sterility Testing Validation
| Validation Parameter | Performance Result | Pharmacopeial Requirement / Significance |
|---|---|---|
| Limit of Detection | 5 CFU [60] | Demonstrates system sensitivity for low-level contamination. |
| Accuracy / Repeatability | >95% [60] | Confirms reliability and consistency of results. |
| Detection Time (Bacteria) | 24–72 hours [60] | Significant reduction from 14-day compendial incubation. |
| Detection Time (Fungi) | Within 5 days [59] | Meets acceptance criterion for slower-growing organisms. |
| Quantitative Concordance | Cohen’s κ = 1.0 [60] | Perfect agreement with pharmacopeial method results. |
| Detection Time Correlation | r = 0.92, p < 0.001 [60] | Strong correlation in time-to-positive with reference method. |
Comparison with Other Rapid Sterility Testing Methods
The field of rapid sterility testing includes several technologies, each with validated performance characteristics.
Table 2: Comparison of Rapid Sterility Testing Methods in the Industry
| Technology / System | Principle | Validated Incubation Time | Key Applications |
|---|---|---|---|
| BACTEC System [59] [60] | COâ‚‚ detection via fluorescence in liquid culture | ~3 days (for most bacteria) | ATMPs, cell suspensions in Ringer's Lactate, reagents |
| BACT/ALERT 3D [62] | COâ‚‚ detection colorimetric sensor | ~7 days (50% reduction) | Broad range of pharmaceutical samples |
| Solid-Phase Cytometry (Redberry) [61] | Fluorescent labeling and laser scanning | 4 days | Pharmaceutical products, with extension to ATMPs planned |
| Celsis Advance II (ATP bioluminescence) [58] | Detection of microbial ATP | ~6 days | Medical devices and pharmaceutical products |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of an automated sterility testing method requires specific reagents and materials. The following toolkit is essential for the validation and routine execution of the test.
Table 3: Essential Research Reagent Solutions for Automated Sterility Testing
| Item | Function / Application | Example Specifications / Notes |
|---|---|---|
| BACTEC Culture Vials [59] | Aerobic/F and Anaerobic/F vials provide growth media for different microorganisms. | Contain modified liquid media and a sensor that fluoresces with increasing COâ‚‚. |
| Reference Microorganism Strains [59] [60] | Used for challenge tests to validate method accuracy, precision, and limit of detection. | Panel includes S. aureus, P. aeruginosa, B. subtilis, C. albicans, and A. brasiliensis. |
| Sterile Saline Solution (0.9%) [59] | Diluent for preparing serial dilutions of microorganisms and negative controls. | Must be sterile to avoid introducing external contamination. |
| McFarland Standard [59] | Provides a reference for standardizing the turbidity (microbial density) of inoculum suspensions. | A 0.5 McFarland standard equals approximately 10⸠CFU/mL. |
| RoosterBio / ThermoFisher Reagents [59] | Xeno-free, cGMP-compliant cell culture media and supplements. | Used in the bioprocessing of the ATMPs being tested to ensure test relevance. |
| MALDI-TOF Mass Spectrometry [59] | Confirms the identity of microorganisms used for inoculation and those detected in positive tests. | System such as VITEK MS provides rapid, high-confidence microbial identification. |
Implementation Strategy and Workflow Integration
A Structured Approach to Implementation
The validation and implementation of an alternative sterility test require a systematic, multi-stage process to ensure regulatory compliance and operational efficiency [57]. A proposed 9-step approach includes:
- User Requirement Specification (URS)
- Technology Screening and Selection
- Operational and Functional Qualification (OQ/FQ)
- Method Validation (as detailed in this case study)
- Method Transfer to quality control laboratories
- Regulatory Filing and submission to health authorities
- Training of personnel
- Method Verification in the user laboratory (per ISO 16140-3) [1]
- Routine Use and ongoing performance monitoring [57]
Automation and Future Trends
The integration of robotics with automated sterility testing systems represents the next frontier in enhancing reproducibility, efficiency, and data integrity. Prototypes have been developed where semi-synchronized industrial robots handle sterility tests, including the complex task of manipulating flexible hoses and placing them in peristaltic pumps [63]. This level of automation minimizes human intervention, reduces the risk of cross-contamination, and ensures seamless, error-free documentation in compliance with Good Manufacturing Practice (GMP) [63].
Diagram showing the evolution from manual sterility testing to fully automated workflows incorporating robotics.
This case study demonstrates that the BACTEC automated system can be successfully validated for the sterility testing of pharmaceutical products, including complex ATMPs. The data confirms that the method provides equivalent results to the pharmacopeial test, with the significant advantage of a greatly reduced time-to-result—from 14 days down to 3 days for most bacterial contaminants [59] [60]. The validation framework, aligned with ISO 16140 standards and pharmacopeial guidelines, ensures the method is fit-for-purpose, accurate, and reproducible.
For researchers and drug development professionals, the adoption of validated rapid sterility testing methods like the one described offers a path to accelerate product release timelines without compromising quality or safety. As technology advances, the integration of full automation and even more rapid detection technologies, such as solid-phase cytometry aiming for same-day results [61], will continue to transform the sterility testing landscape, enabling faster delivery of critical therapies to patients.
Conclusion
The ISO 16140 standards provide an essential, structured framework for ensuring the reliability and reproducibility of microbiological methods in pharmaceutical and clinical research. By understanding the distinct roles of validation and verification, implementing the two-stage verification process, and effectively navigating transition periods, research professionals can significantly enhance method reliability and regulatory compliance. As molecular technologies continue to evolve, the ISO 16140 framework adapts through ongoing revisions and amendments, offering robust protocols for emerging methods like identification techniques and commercial sterility testing. The future of pharmaceutical microbiology will increasingly rely on these standardized approaches to validate rapid detection methods, advanced confirmation techniques, and ensure patient safety through rigorous method verification practices that stand up to regulatory scrutiny across global markets.
References
- 1. Method validation and method verification - Introduction - ISO [https://committee.iso.org/sites/tc34sc9/home/essential-information/content-left-area/validation-of-methods/method-validation-and-method-ver.html]
- 2. ISO 16140-3:2021 Method Verification Roundtable [https://www.neogen.com/en/neocenter/resources/iso-16140-32021-method-verification-roundtable-perspectives-from-the-industry/]
- 3. ISO 16140-3:2021/Amd1:2025 - - Amendment 1 [https://webstore.ansi.org/standards/iso/iso161402021amd12025?srsltid=AfmBOorIzdEIzf_9G7D9SASjVI023gixwEKTjGarcNuwzIsYN0MCnV1i]
- 4. ISO 16140-3 AMD 1 - 2025-08 [https://www.dinmedia.de/en/standard/iso-16140-3-amd-1/394927011]
- 5. UNE EN ISO 16140-4:2021/A1:2025 Microbiology of the food ... [https://www.en-standard.eu/une-en-iso-16140-4-2021-a1-2025-microbiology-of-the-food-chain-method-validation-part-4-protocol-for-method-validation-in-a-single-laboratory-amendment-1-validation-of-a-larger-test-portion-size-for-qualitative-methods-iso-16140-4-2020-amd-1-202/?srsltid=AfmBOor0LbNjNOcNkQD96ODBFQsMtlRdCrhCe1eMLcsVaI7B22zHO56q]
- 6. Method Validation vs Method Verification: Which is Better ... [https://www.labmanager.com/method-validation-vs-method-verification-which-is-better-for-use-in-laboratories-33982]
- 7. Method Validation Guidelines [https://www.biopharminternational.com/view/method-validation-guidelines]
- 8. What Is The Difference Between Verification And Validation of ... [https://boracdmo.com/what-is-the-difference-between-verification-and-validation-of-analytical-methods-in-the-pharmaceutical-industry/]
- 9. Method Validation vs. Verification: Breaking Down the ... [https://www.idexxcurrents.com/en/latest/method-validation-vs-verification-breaking-down-the-difference/]
- 10. Method Verification Versus Method Validation [https://www.linkedin.com/pulse/method-verification-versus-validation-pharcell-9xlzf]
- 11. Explaining ISO/IEC 17025 Competency Requirements [https://a2la.org/explaining-iso-iec-17025-competency-requirements/]
- 12. Developing a competency assessment framework for medical ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0294939]
- 13. What You Need to Know About the New ISO 16140-3 ... [https://www.sigmaaldrich.com/US/en/collections/webinars/iso-16140-3-microbiological-method-verification?srsltid=AfmBOopseJPZOvgtEGcP_QisAyRiNLAJGhSDlPlYcO-FQmk-5_ESiLx0]
- 14. New ISO Standard Published [https://www.rapidmicrobiology.com/news/new-iso-standard-for-verifying-validating-food-testing-methods]
- 15. New ISO Standard for Validating Alternative Food ... [https://www.rapidmicrobiology.com/news/new-iso-standard-for-validating-alternative-food-microbiology-methods]
- 16. How to Verify Methods in Your Laboratory with ISO 16140-3 [https://www.linkedin.com/posts/kineanalytix-services-sdn-bhd_laboratoryquality-methodverification-iso17025-activity-7352156003259371520-vOov]
- 17. Verification of a Rapid Analytical Method for the Qualitative ... [https://www.mdpi.com/2076-0817/13/2/141]
- 18. ISO Updates Standard on Validating Microorganism Testing in ... [https://ohsonline.com/articles/2016/06/24/iso-updates-standard-on-validating-microorganism-testing-in-food.aspx?admgarea=ht.RegulationsStandards&m=1]
- 19. Complying with ISO 16140-part 3 [https://www.newfoodmagazine.com/article/114632/complying-with-iso-16140-part-3/]
- 20. ISO 16140-3:2021/Amd 1:2025 - Microbiology of the food ... [https://www.iso.org/standard/88181.html]
- 21. ISO 16140-3:2021/Amd1:2025 - - Amendment 1 [https://webstore.ansi.org/standards/iso/iso161402021amd12025?srsltid=AfmBOoppb_vo5Oko-6ioONABAUkiGHLEqDYb4C0jm4l4CKl9eC6bT4p_]
- 22. ISO 16140-3:2021 - Microbiology of the food chain ... [https://www.iso.org/standard/66324.html]
- 23. Current developments of bioanalytical sample preparation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9463481/]
- 24. The Importance of the Sample Matrix | LCGC International [https://www.chromatographyonline.com/view/importance-sample-matrix-0]
- 25. Sample Preparation Strategies Demystified: Choosing the ... [https://www.thermofisher.com/blog/analyteguru/sample-prep-strategies-demystified-choosing-the-right-fit-for-your-toxicology-workflow/]
- 26. Breaking the reproducibility barrier with standardized ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12416739/]
- 27. Verification of a Rapid Analytical Method for the Qualitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10892580/]
- 28. Development of real-time PCR methods for quality control ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1572201/full]
- 29. Introduction to Quantitative PCR (qPCR) Gene Expression ... [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/gene-expression-analysis-real-time-pcr-information/introduction-gene-expression.html]
- 30. 10 Steps Toward Achieving ISO/IEC 17025 Accreditation [https://a2la.org/10-steps-toward-achieving-iso-iec-17025-accreditation/]
- 31. The ISO/IEC 17025: 2017 Quality Standard as a Guideline [https://pmc.ncbi.nlm.nih.gov/articles/PMC7838891/]
- 32. Compensate for or Minimize Matrix Effects? Strategies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7412464/]
- 33. Strategies for the Detection and Elimination of Matrix ... [https://www.chromatographyonline.com/view/strategies-detection-and-elimination-matrix-effects-quantitative-lc-ms-analysis]
- 34. Inhibit inhibition: PCR inhibition and how to prevent it [https://www.bioecho.com/blog/inhibit-inhibition-pcr-inhibition-and-how-to-prevent-it]
- 35. Evaluation of PCR-enhancing approaches to reduce ... [https://www.sciencedirect.com/science/article/abs/pii/S0048969724069250]
- 36. Inhibition of polymerase chain reaction: Pathogen-specific ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6764677/]
- 37. Ideal Control for PCR Inhibition and Cell Input [https://www.thermofisher.com/us/en/home/references/ambion-tech-support/rna-isolation/tech-notes/ideal-control-for-pcr-inhibition-and-cell-input.html]
- 38. ANSI ISO-related Frequently Asked Questions [https://www.ansi.org/iso/us-representation-in-iso/iso-faqs]
- 39. EN ISO 16140-2 Validation in Food Microbiology | PDF [https://www.scribd.com/document/546209306/NFVALI-2]
- 40. Detection of Single Cell Contamination of Salmonella in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12214205/]
- 41. Validation protocol for commercial sterility testing methods [https://www.sciencedirect.com/science/article/pii/S0956713519301288]
- 42. What You Need to Know About the New ISO 16140-3 ... [https://www.sigmaaldrich.com/BR/en/collections/webinars/iso-16140-3-microbiological-method-verification?srsltid=AfmBOorpOINJMjXKph1CpQ4sxnk8USZGQkrZKMnWcvsmBGOK_9O2J2tn]
- 43. BS EN ISO 16140-3:2021+A1:2025 [https://standardsdevelopment.bsigroup.com/projects/2024-00718]
- 44. Utilizing tables, figures, charts and graphs to enhance the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10394528/]
- 45. 7 Best Comparison Charts for Effective Data Visualization [https://ninjatables.com/types-of-comparison-charts/?srsltid=AfmBOooBltaf97RZsRN2mUQvgqwEY7GVOm-2JyNeupYlOSrAlCs9MnbT]
- 46. 14 Comparing quantitative data between individuals [https://bookdown.org/pkaldunn/SRM-Textbook/BetweenQuantData.html]
- 47. Understanding Success Criterion 1.4.11: Non-text Contrast [https://www.w3.org/WAI/WCAG21/Understanding/non-text-contrast.html]
- 48. Key Considerations for Flowchart Accessibility - MN.gov [https://mn.gov/mnit/about-mnit/accessibility/news/?id=38-436349]
- 49. A Robust Method for Calculating Precision ... [https://www.preprints.org/manuscript/202505.1345]
- 50. Efficient and robust analysis of interlaboratory studies [https://www.sciencedirect.com/science/article/pii/S016974391730268X]
- 51. ISO 16140-6:2019 - Microbiology of the food chain [https://www.iso.org/standard/66327.html]
- 52. The validation study in ISO 16140-6 clearly defines ... [https://www.facebook.com/kas.laboratorytesting/posts/understanding-iso-16140-6-and-alternative-confirmation-methodshello-laboratory-p/1128905455930352/]
- 53. Understanding ISO 16140-6 and Alternative Confirmation Methods [https://www.linkedin.com/posts/kineanalytix-services-sdn-bhd_confirmationmethods-methodvalidation-iso16140-activity-7344545381139009536-A9Q6]
- 54. New ISO 16140-6 validation for Check&Trace Salmonella 2.0 [https://microval.org/2023/01/24/new-iso-16140-6-validation-for-checktrace-salmonella-2-0/]
- 55. Food industry - NF Validation EN - Afnor [https://nf-validation.afnor.org/en/food-industry/]
- 56. How to Validate Sterility Testing Methods for ... [https://cmdclabs.com/how-to-validate-sterility-testing-methods-for-pharmaceuticals-and-medical-implants/]
- 57. Rapid Sterility Test Systems in the Pharmaceutical Industry [https://pubmed.ncbi.nlm.nih.gov/36697213/]
- 58. Nelson Labs Launches Rapid Method for Sterility Testing [https://www.rapidmicrobiology.com/news/nelson-labs-launches-rapid-method-sterility-testing-service-for-medical-devices-and-pharmaceuticals]
- 59. Validation of an automated quality control method to test ... [https://www.htct.com.br/en-validation-an-automated-quality-control-articulo-S2531137924028414]
- 60. Validation of the Bactec system for sterility testing ... [https://www.sciencedirect.com/science/article/pii/S0731708525006247]
- 61. Redberry Successful Validation 4day Sterility Testing Method [https://www.rapidmicrobiology.com/news/redberry-announces-successful-validation-of-a-4-day-sterility-testing-method]
- 62. Rapid Sterility Testing for Bioprocessing - bioMerieux [https://www.biomerieux.com/us/en/our-offer/industry-products/rely-on-a-proven-solution-and-enable-rapid-sterility-testing.html]
- 63. Fraunhofer IPA and SKAN - Research project on robot- ... [https://skan.com/en/research-project-on-robot-assisted-sterility-tests/]