Culture-Based vs Molecular Diagnostic Methods: A Comprehensive Comparison for Biomedical Research and Clinical Application
This article provides a critical analysis for researchers and drug development professionals comparing traditional culture-based methods with advanced molecular diagnostics.
Culture-Based vs Molecular Diagnostic Methods: A Comprehensive Comparison for Biomedical Research and Clinical Application
Abstract
This article provides a critical analysis for researchers and drug development professionals comparing traditional culture-based methods with advanced molecular diagnostics. It explores the foundational principles, methodological applications, operational challenges, and validation data for both approaches across diverse clinical scenarios including necrotizing soft tissue infections, chronic wounds, antimicrobial resistance surveillance, and urinary tract infections. The content synthesizes current evidence on sensitivity, specificity, turnaround time, and clinical utility, offering practical insights for method selection, troubleshooting, and future directions in diagnostic strategy.
Fundamental Principles: From Traditional Gold Standards to Molecular Revolution
For over a century, culture-based methods have served as the fundamental cornerstone of microbiological diagnosis, providing the definitive standard for detecting and identifying pathogens in clinical and research settings. This preeminence stems from their ability to isolate viable microorganisms, enabling comprehensive phenotypic characterization, antimicrobial susceptibility testing (AST), and detailed strain typing. The historical reliance on culture is deeply embedded in Koch's postulates and traditional microbiological principles, which prioritize the isolation and propagation of pathogens as proof of infectious etiology.
However, the landscape of diagnostic microbiology is undergoing a profound transformation. The inherent limitations of culture methods—particularly their extended time-to-result and variable sensitivity—have become increasingly significant in an era demanding rapid, precise interventions. This has catalyzed the development and adoption of molecular diagnostics that offer revolutionary speed and sensitivity. This article objectively examines the historical context of culture as the gold standard, its documented limitations through comparative experimental data, and the emerging diagnostic paradigms reshaping pathogen detection in modern research and drug development.
The Traditional Gold Standard: Culture-Based Methods
Fundamental Principles and Workflow
Culture-based detection relies on the fundamental principle of propagating microorganisms on or in artificial nutrient media. The standard workflow involves inoculating a clinical specimen onto selective and/or non-selective media, followed by incubation for 24-48 hours or longer to allow for the growth of viable organisms. Subsequently, colony identification is performed using morphological assessment, biochemical tests, or mass spectrometry techniques like MALDI-TOF. For antimicrobial susceptibility testing, isolated colonies are subjected to disk diffusion, gradient diffusion, or automated broth microdilution systems, requiring additional 18-24 hours of incubation [1] [2].
The critical strength of this paradigm lies in its ability to provide a living isolate. This isolate can be used for comprehensive downstream analyses, including full AST profiles, whole-genome sequencing, and studies of pathogenicity. Furthermore, culture methods are widely accessible and do not require the sophisticated instrumentation or specialized technical expertise needed for molecular assays, making them a universal first-line tool across diverse laboratory settings.
Documented Limitations in Modern Context
Despite its historical status, extensive research has quantified significant constraints of culture-based methods:
- Prolonged Time-to-Result (TTR): The multi-step process inherently creates delays. Studies consistently report a TTR of 48 to 72 hours for a complete identification and AST profile [1] [2]. This delay can critically impact patient management in sepsis and other acute infections and slow down research workflows in drug development.
- Limited Sensitivity: Culture sensitivity is dependent on the viability and cultivability of pathogens under artificial laboratory conditions. Fastidious organisms, those inhibited by prior antibiotic exposure, or those present in low microbial bioburden samples may fail to grow, leading to false-negative results. A year-long comparative study on carbapenemase-producing Gram-negative bacilli (CPGNB) reported a sensitivity of just 46.3% for a culture-based strategy when non-fermenting Gram-negative bacilli were disregarded, rising only to 64.8% when they were included [3].
- Labor-Intensive Processes: Culture methods require substantial hands-on technical time for media preparation, specimen plating, subculturing, and manual interpretation, making them less amenable to high-throughput screening in large-scale studies [3].
The Molecular Paradigm: A Comparative Analysis
Molecular diagnostics represent a paradigm shift from cultivating organisms to directly detecting their genetic material. These techniques bypass the need for growth, offering a direct pathway from specimen to result.
- Multiplex PCR (mPCR): Systems like the Allplex Entero-DR assay and the Xpert Carba-R assay can simultaneously identify a panel of resistance genes (e.g., blaKPC, blaNDM, blaVIM, blaIMP, blaOXA-48, blaCTX-M, vanA, vanB) directly from rectal swabs and other specimens within a few hours [2].
- Droplet Digital PCR (ddPCR): This technique offers absolute quantification of nucleic acids, showing high sensitivity for diagnosing bloodstream infections, even with low pathogen loads [4] [5].
- Metagenomic Next-Generation Sequencing (mNGS): mNGS provides a hypothesis-free approach, capable of identifying all nucleic acids in a sample—bacterial, viral, and fungal—without prior knowledge of the pathogen, making it powerful for detecting novel or unexpected organisms [4] [5].
Head-to-Head Performance Data
Recent large-scale studies provide robust quantitative comparisons between culture and molecular methods, particularly for antimicrobial resistance (AMR) surveillance.
Table 1: Comparative Diagnostic Performance for CPGNB/CPE Detection
| Metric | Xpert Carba-R (Molecular) | Culture-Based Method | Study Context |
|---|---|---|---|
| Sensitivity | 90.2% [3] / 97.2% [1] | 46.3% - 64.8% [3] | 29,446 samples; moderate-prevalence setting [3] |
| Specificity | >99% [1] | Not directly comparable (Reference) | 4,120 high-risk patients [1] |
| Avg. Hands-on Time | 1.3 minutes [3] | 89.97 minutes [3] | Hands-on time per sample [3] |
| Total Turnaround Time (TAT) | ~1.26 hours [1] | ~55.35 hours [1] | From sample to final result [1] |
| Key Advantage | Speed, sensitivity, automation | Specificity, provides viable isolate | - |
Table 2: Performance of a Multiplex PCR Assay (Allplex Entero-DR) [2]
| Parameter | Result |
|---|---|
| Samples Analyzed | 300 rectal swabs |
| Positive by Multiplex PCR | 188 (62.6%) |
| Sensitivity | 100% |
| Negative Predictive Value (NPV) | 100% |
| Targets Detected | blaKPC, blaOXA-48, blaVIM, blaNDM, blaIMP, blaCTX-M, vanA, vanB |
The data demonstrates the consistent superiority of molecular methods in speed and sensitivity. The near 100% Negative Predictive Value (NPV) is particularly noteworthy; it means a negative molecular test can reliably exclude colonization or infection with a high degree of confidence, allowing researchers and clinicians to rule out targets efficiently [2].
Experimental Protocols: A Closer Look
Detailed Protocol: Culture-Based CPGNB Detection
The following methodology is representative of the protocols used in the cited comparative studies [3] [1]:
- Specimen Collection & Inoculation: Rectal swabs are collected in transport media (e.g., Copan Faecal Swab with Cary-Blair medium). An aliquot (e.g., 10 μL) of the transport medium is inoculated onto selective chromogenic agar plates, such as ChromID CARBA SMART or similar.
- Incubation: The inoculated agar plates are incubated at 35–37°C under aerobic conditions for 24-48 hours.
- Colony Identification: Colonies with morphology suggestive of target organisms (e.g., metallic blue on ChromID CARBA SMART for E. coli) are selected for further analysis. Identification is confirmed using techniques like MALDI-TOF mass spectrometry.
- Confirmation of Carbapenemase Production:
- Phenotypic Testing: A modified Hodge test or similar phenotypic assay may be performed.
- Molecular Confirmation: Isolated colonies are typically subjected to a confirmatory PCR-based test (e.g., Xpert Carba-R) to identify the specific carbapenemase gene present.
Detailed Protocol: Direct Molecular Detection (Xpert Carba-R Assay)
The protocol for direct-from-specimen testing is significantly streamlined [3] [1]:
- Sample Preparation: The rectal swab is suspended in a specific Sample Reagent (containing sodium citrate and cysteine). The mixture is vortexed for 10 seconds to homogenize the sample and lyse the bacteria.
- Loading & Automation: A precise volume (e.g., 1.7 mL) of the homogenized mixture is transferred into the single-use Xpert Carba-R cartridge using a provided pipette.
- Integrated Analysis: The cartridge is loaded into the GeneXpert platform, which automates all subsequent steps: nucleic acid extraction, purification, amplification via real-time PCR, and target detection.
- Result Reporting: The system software automatically analyzes the fluorescence data and reports the presence or absence of the targeted carbapenemase genes (blaKPC, blaNDM, blaVIM, blaIMP-1, blaOXA-48). The entire process from cartridge loading to result is typically completed in under 90 minutes with minimal hands-on time.
Workflow Visualization
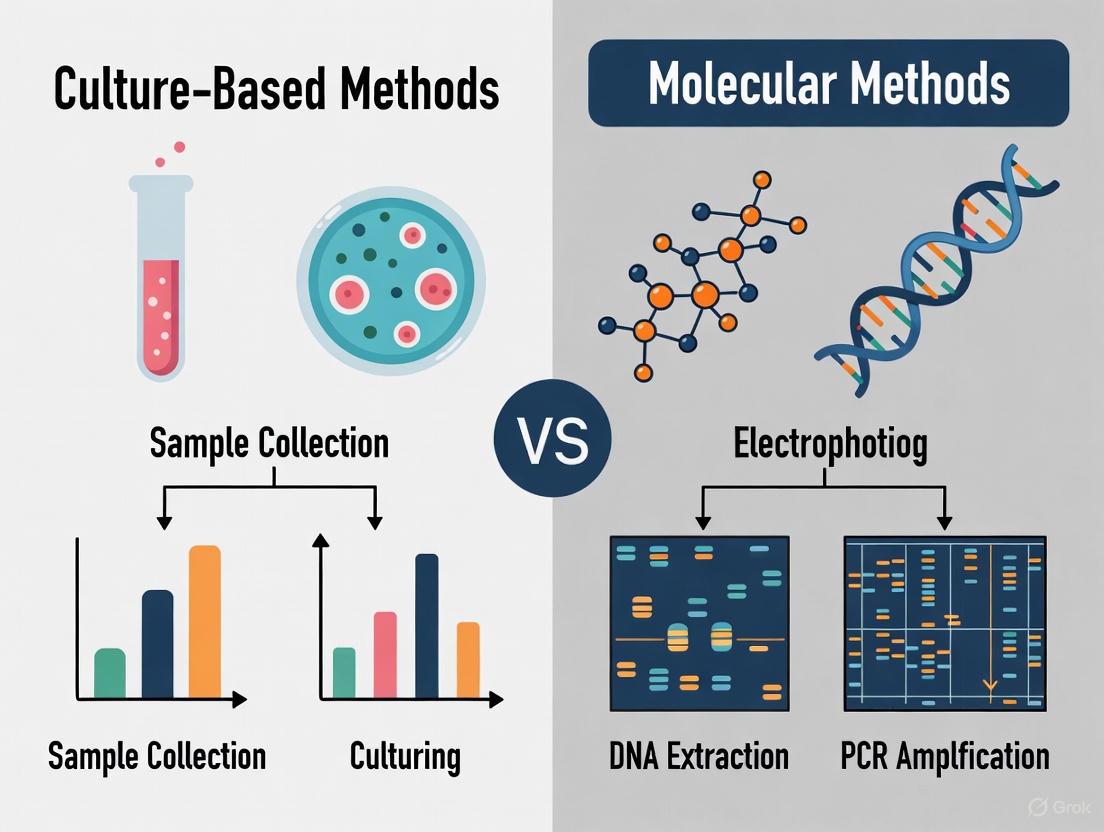
The following diagram illustrates the stark contrast in complexity and time investment between the two methodologies, highlighting the key bottleneck of incubation in the culture-based workflow.
The Scientist's Toolkit: Essential Research Reagents & Materials
The experiments cited rely on specific, commercially available reagents and platforms to ensure reproducibility and accuracy.
Table 3: Key Research Reagents and Platforms for AMR Detection Studies
| Item Name | Function / Target | Application in Research |
|---|---|---|
| ChromID CARBA SMART Agar (bioMérieux) | Selective chromogenic culture medium | Differentiates carbapenemase-producing Enterobacterales based on colony color; used as a culture-based comparator [3]. |
| Xpert Carba-R Assay (Cepheid) | Multiplex real-time PCR | Detects & differentiates five major carbapenemase gene families (blaKPC, blaNDM, blaVIM, blaIMP-1, blaOXA-48) directly from specimens or isolates [3] [1]. |
| GeneXpert Platform (Cepheid) | Automated molecular diagnostic system | Integrates sample preparation, amplification, and detection in a single, self-contained cartridge; enables rapid, hands-off molecular testing [1]. |
| Allplex Entero-DR Assay (Seegene) | Multiplex real-time PCR | Simultaneously detects a broad panel of β-lactamase (blaCTX-M, carbapenemases) and vancomycin resistance (vanA/B) genes from surveillance samples [2]. |
| Copan Faecal Swab (COPAN) | Specimen collection & transport | Contains liquid Cary-Blair medium to preserve the viability of microorganisms during transport for both culture and molecular testing [1] [2]. |
| 1,2-O-Dilinoleoyl-3-O-Beta-D-Galactopyranosylracglycerol | 1,2-O-Dilinoleoyl-3-O-Beta-D-Galactopyranosylracglycerol, MF:C45H78O10, MW:779.1 g/mol | Chemical Reagent |
| (S)-2-(3-Bromophenyl)propanoic acid | (S)-2-(3-Bromophenyl)propanoic acid, MF:C9H9BrO2, MW:229.07 g/mol | Chemical Reagent |
Challenges and Nuances in Molecular Diagnostics
Despite their superior analytical performance, molecular methods are not without limitations, which are crucial for researchers to consider when interpreting data.
- Discordance in Genotype Detection: A significant challenge is the occasional discordance between direct molecular testing and culture-based results. For instance, one study noted that the positive predictive value (PPV) for the blaIMP-1 gene using the Xpert Carba-R assay was 0%, as none of the nine positive detections from stool were confirmed in corresponding cultured isolates [1]. This highlights that molecular tests can detect genes from non-viable organisms or those present below the threshold for culture growth, which may not always represent a active, transmissible colonization.
- The Clinical Accuracy Gap: Perhaps the most critical nuance is that the dramatic improvement in analytical sensitivity and speed has not always translated into unequivocal improvements in patient outcomes in clinical trials. As noted by Li et al., "While molecular diagnostics excel in sensitivity, their real-world impact on specificity and patient prognosis - clinical accuracy - remains limited" [4] [5]. This gap can stem from challenges in interpreting multi-positive results, distinguishing colonization from infection, and the complex interplay of host factors in determining clinical outcomes [5].
- Inability to Provide a Live Isolate: Molecular methods detect genetic targets but do not yield a viable isolate for further study. This is a critical limitation for research requiring downstream phenotypic analyses, such as comprehensive antimicrobial susceptibility testing, whole-genome sequencing, or investigating pathogenicity mechanisms.
The evidence demonstrates that while culture-based methods retain an essential role in microbiology by providing a viable isolate for comprehensive phenotypic characterization, their status as an unassailable "gold standard" is no longer tenable in many diagnostic and research contexts. Their principal limitations—prolonged turnaround times and suboptimal sensitivity—are quantitatively addressed by modern molecular techniques.
Molecular diagnostics have established a new benchmark for speed and analytical sensitivity, as rigorously documented in head-to-head comparisons for AMR surveillance. However, the transition to a molecular-centric paradigm is nuanced. Researchers must critically navigate challenges such as result interpretation, genotype-phenotype correlation, and the current lack of a live isolate for further investigation. The future of microbiological diagnosis lies not in the supremacy of one method over the other, but in their strategic integration. Leveraging the unparalleled speed of molecular tools for initial screening and rapid guidance, followed by the phenotypic precision of culture for confirmation and isolate retrieval, represents the most powerful and rational path forward for both clinical science and drug development.
Clinical microbiology is defined by the ongoing pursuit of a critical balance: the need for rapid, actionable results versus the requirement for accurate, comprehensive pathogen characterization. For decades, this balance has been maintained by culture-based methods that represent the historical cornerstone of pathogen identification. These methods, which include isolation on selective media, phenotypic profiling, and antibiotic susceptibility testing (AST), provide the foundational framework for clinical bacteriology [6] [7]. However, the landscape of infectious disease diagnostics is undergoing a profound transformation. The emergence and global spread of antimicrobial resistance (AMR), now considered a major global health burden, has intensified the need for faster diagnostic solutions [8]. This urgency is compounded by data showing that delayed administration of effective antimicrobials is directly associated with increased mortality in patients with severe sepsis and septic shock [8] [6].
In response to these pressures, molecular diagnostic techniques have rapidly evolved as powerful alternatives or complementary tools. These methods, particularly nucleic acid amplification tests (NAATs), offer the potential to drastically reduce the time to results, in some cases providing actionable data within hours rather than days [9] [10]. This guide provides a systematic, evidence-based comparison of these two diagnostic paradigms—culture-based versus molecular methods—framed within the broader thesis that the future of clinical microbiology lies not in the supremacy of one approach over the other, but in their strategic integration. We will objectively compare their performance using published experimental data, detail key methodologies, and visualize their workflows to provide researchers and drug development professionals with a clear understanding of the current diagnostic landscape.
Core Principles and Methodologies: A Detailed Comparison
Conventional Culture-Based Methods: The Established Gold Standard
Conventional culture methods form the multi-step backbone of traditional clinical microbiology. The process begins with sample inoculation onto solid or liquid culture media. For bloodstream infections, this typically involves incubating blood samples in culture bottles, which can take up to 5 days for bacterial growth detection, though it often occurs within the first 24 hours [6]. Following detection of microbial growth, the next step is bacterial isolation to obtain pure colonies, which typically requires an additional 24 hours [6]. The isolated colonies then undergo phenotypic identification based on morphological characteristics, Gram staining, and biochemical profiling.
The final and often most critical step is phenotypic Antimicrobial Susceptibility Testing (AST), which evaluates bacterial response to antimicrobial agents in vitro to guide therapeutic decisions [8]. The gold standard phenotypic AST methods include:
- Broth and Agar Dilution: A standard bacterial inoculum is added to agar or broth containing two-fold serial dilutions of an antimicrobial agent. After overnight incubation, the Minimum Inhibitory Concentration (MIC) is determined as the lowest concentration that inhibits visible bacterial growth [8] [11].
- Kirby-Bauer Disk Diffusion: A standard inoculum is spread on a Mueller-Hinton Agar plate, and antibiotic-impregnated disks are placed on the surface. After 18-24 hours of incubation, the diameter of the zone of inhibition around each disk is measured and interpreted using established clinical breakpoints [8].
- Gradient Diffusion Methods (E-test): A predefined antibiotic gradient is applied to a strip placed on an inoculated agar plate. After incubation, the MIC is read at the intersection of the elliptical zone of inhibition with the strip [8].
The primary limitation of these conventional methods is their prolonged turnaround time, requiring at least 72 hours from specimen collection to final susceptibility results, which can critically delay targeted antimicrobial therapy [6].
Molecular Methods: The Rise of Rapid Diagnostics
Molecular techniques for pathogen detection have emerged to address the speed limitations of culture-based methods. These approaches primarily rely on detecting pathogen-specific nucleic acids (DNA or RNA) and can be broadly categorized into two types: single-pathogen tests and multiplexed panels.
A pivotal step in any molecular workflow is the efficient extraction of bacterial DNA, which significantly impacts downstream detection sensitivity. Multiple DNA extraction methodologies have been developed and compared in the literature:
- Column-Based Extraction: Kits such as the QIAamp DNA Blood Mini Kit (Qiagen) use silica-based columns to bind and purify DNA after lysis. While widely used, one study found this method had an accuracy of 65.0% for E. coli detection from whole blood, underperforming compared to newer methods [12].
- Magnetic Bead-Based Extraction: Methods like the K-SL DNA Extraction Kit and the automated GraBon system use magnetic beads to isolate bacteria from whole blood before lysis, providing a cleaner sample. These demonstrated superior accuracy rates of 77.5% and 76.5% respectively for E. coli detection [12].
- Enzymatic and Non-Enzymatic Enrichment Methods: The MolYsis system enzymatically removes human DNA to enrich for pathogen DNA but is noted to be labor-intensive [13]. The novel Polaris method provides a non-enzymatic, more rapid pathogen DNA enrichment, enabling reliable detection from 5 ml of blood with a 70-75% detection rate at clinically relevant concentrations of 1 CFU/ml [13].
- In-House Extraction Protocols: Some studies have developed modified in-house methods, such as a chloroform-isoamyl alcohol protocol, which showed statistically similar sensitivity to commercial kits while maintaining high rapidity and much lower cost [9].
Following DNA extraction, the primary molecular detection techniques include:
- Polymerase Chain Reaction (PCR) and Electrophoresis: Conventional and real-time PCR amplify target DNA sequences, with products detected via gel electrophoresis or fluorescent probes in real-time. One study protocol involved initial denaturation at 95°C for 10 min, followed by 40 cycles of denaturation, annealing (at 52-58°C), and elongation, with final analysis by agarose gel electrophoresis [9].
- Loop-Mediated Isothermal Amplification (LAMP): This technique operates at a constant temperature (65°C) for 30-60 minutes, using multiple primers for high specificity and sensitivity. It is considered simpler and more rapid than PCR as it doesn't require thermal cycling equipment [9]. One evaluation found LAMP more promising than PCR-electrophoresis due to its simplicity, high rapidity, and sensitivity [9].
- Microarray-Based Systems: Platforms like the Clart Pneumovir Kit use hybridization patterns on a microarray chip to detect multiple pathogens simultaneously, with analysis performed using optical equipment [10].
- Automated, Integrated Systems: Newer systems combine extraction, amplification, and detection. For instance, the hypothetical MyCrobe system (envisioned for 2025) integrates nucleic acid and antigen detection from clinical specimens to provide results in approximately 15 minutes [7].
Performance Comparison: Experimental Data and Analysis
Speed, Sensitivity, and Accuracy
The following tables synthesize quantitative performance data from published comparative studies to provide an objective assessment of method capabilities.
Table 1: Comparison of DNA Extraction Method Performance from Whole Blood
| Extraction Method | Technology Type | Pathogen Detected | Accuracy/Detection Rate | Sample Volume | Time Requirements |
|---|---|---|---|---|---|
| QIAamp DNA Blood Mini Kit [12] | Column-based | E. coli | 65.0% | 200 µL | Standard |
| S. aureus | 67.5% | 200 µL | Standard | ||
| K-SL DNA Extraction Kit [12] | Magnetic bead-based | E. coli | 77.5% | 200 µL | Standard |
| S. aureus | 67.5% | 200 µL | Standard | ||
| GraBon System [12] | Automated magnetic bead | E. coli | 76.5% | 500 µL | Standard |
| S. aureus | 77.5% | 500 µL | Standard | ||
| Polaris Method [13] | Non-enzymatic enrichment | S. aureus (10 CFU/mL) | 100% | 5 mL | ~45 minutes |
| S. aureus (1 CFU/mL) | 70-75% | 5 mL | ~45 minutes | ||
| MolYsis Method [13] | Enzymatic enrichment | S. aureus (10 CFU/mL) | 50-67% | 5 mL | ~2 hours |
| S. aureus (1 CFU/mL) | 17-50% | 5 mL | ~2 hours | ||
| In-House (Phenol-Chloroform) [9] | Chemical purification | Foodborne Pathogens | Similar to commercial kits | 1 mL | Lower cost, high rapidity |
Table 2: Performance of Rapid Phenotypic AST Platforms for Bloodstream Infections
| Platform (Manufacturer) | Technology Principle | Acceptable Specimens | Time to Result (after positive culture) | Categorical Agreement (CA) | Essential Agreement (EA) |
|---|---|---|---|---|---|
| VITEK REVEAL (bioMérieux) [14] [8] | Colorimetric sensors detecting volatile organic compounds from bacterial metabolism | Positive Blood Cultures | ~5 hours | 98.3% | 97.1% |
| PhenoTest BC (Accelerate Diagnostics) [8] | Morphokinetic cellular analysis, fluorescence in situ hybridization | Positive Blood Cultures | ID: 2 h, AST: 7 h | 92-99% | 82-97% |
| QuickMIC (Gradientech) [8] | Microscopic analysis of microfluidic device | Positive Blood Cultures | 2-4 hours | 78-100% | 45-100% |
| FASTinov [8] | Flow cytometry with fluorescent dyes (growth-independent) | Positive Blood Cultures | ~2 hours | >96% | N/R |
| dRAST (QuantaMatrix) [8] | Time-lapse microscopic imaging | Positive Blood Cultures | 4-7 hours | 91-92% | >95% |
Table 3: Molecular vs. Conventional Method Detection for Respiratory Viruses [10]
| Virus | Immunofluorescence/ Viral Culture (IF/VC) | Seeplex RV12 | Clart Pneumovir |
|---|---|---|---|
| RSV | 11 | 7 | 12 |
| Adenovirus | 13 | 14 | 13 |
| Rhinovirus | 2 | 17 | 27 |
| Human Bocavirus (HBoV) | N/D | N/D | 16 |
| Total Positives (n=80 samples) | 37 | 40 | 62 |
Critical Analysis of Comparative Performance
The data reveal distinct, complementary strengths and limitations for each methodological approach. Culture-based methods maintain their position as the comprehensive gold standard, providing viable isolates for further characterization and full phenotypic AST profiles. However, their most significant drawback remains the extended turnaround time of 48-72 hours or more to final results [6]. Furthermore, conventional methods require specialized infrastructure, are labor-intensive, and have a complex supply chain that can limit implementation in low-resource settings [6].
Molecular methods demonstrate clear advantages in speed, with some rapid AST platforms delivering results in 2-7 hours after a positive blood culture [8] [14]. Sensitivity is also a key strength, with technologies like the Polaris system enabling detection at clinically relevant concentrations as low as 1 CFU/mL blood [13]. However, molecular methods face their own challenges. They generally require expensive equipment and trained personnel [9] [11]. The detection of nucleic acids does not necessarily indicate viable, clinically relevant infection, potentially leading to false positives from non-viable organisms or environmental contamination [10]. Perhaps most critically for AMR management, most genotypic methods detect only a limited number of pre-defined resistance targets and may miss novel or uncommon resistance mechanisms [6]. One review noted that a carbapenemase gene is identifiable in fewer than 50% of bacteria found to be phenotypically carbapenem resistant [6].
Visualizing Diagnostic Workflows
The following diagrams illustrate the procedural flow and time investment for both conventional and modern diagnostic pathways, highlighting critical decision points and opportunities for integration.
Diagram 1: Comparative diagnostic workflows showing the significant time difference between conventional culture-based methods (72+ hours) and molecular methods (3-8 hours).
Diagram 2: Classification of rapid phenotypic AST platforms by their underlying detection technologies, showcasing the diversity of innovation in this field.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 4: Key Reagents, Kits, and Platforms for Diagnostic Method Comparison
| Product/Platform Name | Type/Category | Primary Function | Key Features / Experimental Role |
|---|---|---|---|
| QIAamp DNA Blood Mini Kit (Qiagen) [12] | DNA Extraction Kit | Column-based nucleic acid purification | Benchmark for comparison studies; processes 200 µL blood samples directly. |
| NucleoSpin Food (Macherey-Nagel) [9] | DNA Extraction Kit | DNA purification from complex food matrices | Used in comparative studies for pathogen detection from food samples. |
| K-SL DNA Extraction Kit (KingoBio) [12] | DNA Extraction Kit | Magnetic bead-based bacterial DNA extraction | Incorporates bacterial isolation from whole blood before lysis; enhances purity. |
| GraBon (KingoBio) [12] | Automated Platform | Automated DNA extraction system | Uses same reagents as K-SL kit with robotic handling; processes 500 µL sample. |
| MolYsis Complete5 Kit (Molzym) [13] | DNA Extraction Kit | Enzymatic pathogen DNA enrichment | Selectively removes human DNA from up to 5 mL blood; improves sensitivity. |
| Polaris System (Biocartis) [13] | Pathogen DNA Enrichment | Non-enzymatic pathogen DNA isolation | Fast (45 min), sensitive detection from 5 mL blood; compared to MolYsis. |
| VITEK REVEAL (bioMérieux) [14] [8] | Rapid AST System | Phenotypic susceptibility testing | Colorimetric sensors detect metabolic VOCs; ~5h TTR from positive blood culture. |
| PhenoTest BC (Accelerate Diagnostics) [8] | Rapid ID & AST System | Combined identification & AST | Uses morphokinetic analysis and FISH; AST in 7h from positive culture. |
| WarmStart Colorimetric LAMP Master Mix [9] | Amplification Reagent | Isothermal nucleic acid amplification | Enables visual detection of amplification; used in rapid, equipment-free protocols. |
| OneTaq Hot Start Master Mix (NEB) [9] | Amplification Reagent | PCR amplification | Standard master mix for conventional PCR-based detection protocols. |
| MyCrobe System (Hypothetical) [7] | Integrated Molecular System | Hand-held molecular diagnostics | Conceptual future device combining nucleic acid and antigen detection in minutes. |
| Pyrocatechol monoglucoside | Pyrocatechol monoglucoside, MF:C12H16O7, MW:272.25 g/mol | Chemical Reagent | Bench Chemicals |
| 2',4'-Dihydroxy-3,7':4,8'-diepoxylign-7-ene | 2',4'-Dihydroxy-3,7':4,8'-diepoxylign-7-ene, MF:C18H18O4, MW:298.3 g/mol | Chemical Reagent | Bench Chemicals |
The diagnostic landscape is rapidly evolving, influenced by several powerful trends. Automation and Artificial Intelligence (AI) are poised to dominate the future of clinical laboratories. AI is expected to reduce time-consuming repetitive tasks, suggest reflex testing based on initial results, and enhance the accuracy and throughput of laboratory operations [15]. Digital pathology and AI-powered algorithms are also being developed to increase efficiencies and help alleviate workforce shortages [15]. Furthermore, automation systems, widely adopted during the COVID-19 pandemic, are now being deployed to handle manual aliquoting and pre-analytical steps, improving quality, reliability, and turnaround time [15].
The paradigm is shifting from a competitive to a complementary diagnostic framework. The future of clinical microbiology lies in the strategic integration of both culture-based and molecular methods, leveraging the strengths of each. Culture methods remain essential for comprehensive phenotypic AST, outbreak investigation, and epidemiological surveillance, as they provide the live isolates necessary for these purposes [6]. Molecular methods, with their unprecedented speed, are critical for early, sensitive pathogen detection, guiding initial empiric therapy, and detecting pathogens that are slow-growing or difficult to culture [9] [10].
In conclusion, while molecular techniques offer revolutionary speed and sensitivity, phenotypic culture-based methods continue to provide the indispensable reference standard for antimicrobial susceptibility testing. The most effective diagnostic pipelines will therefore utilize an integrated approach: employing rapid molecular assays for early detection and initial guidance, while relying on cultured isolates for definitive phenotypic confirmation and further characterization. This synergistic model, enhanced by automation and AI, represents the most promising path forward for improving patient outcomes and combating the global threat of antimicrobial resistance.
The shift from traditional culture-based methods to molecular techniques represents a paradigm shift in microbiological research and clinical diagnostics. Culture-based methods, long considered the gold standard, are often limited by prolonged turnaround times, low sensitivity for fastidious organisms, and the inability to detect non-culturable pathogens. Molecular methods, founded on nucleic acid extraction, amplification, and sequencing, have overcome these limitations, offering unprecedented speed, sensitivity, and specificity. This guide provides a comparative analysis of these foundational technologies, equipping researchers and drug development professionals with the data needed to select optimal methodologies for their specific applications.
Nucleic Acid Extraction Technologies
The efficacy of any molecular assay is fundamentally dependent on the quality and quantity of the extracted nucleic acid. The choice of extraction method significantly influences downstream results, making selection a critical first step.
Comparison of Extraction Method Performance
The following table summarizes the performance of various nucleic acid extraction methods based on recent comparative studies.
Table 1: Quantitative Comparison of Nucleic Acid Extraction Methods
| Extraction Method | Sample Type | Key Performance Findings | Reference |
|---|---|---|---|
| Magnetic Bead-Based | Cervical Swabs (HPV) | Detection rate of 20.66%; superior anti-interference; cost increased by 13.14% but detection rate increased by 106.19%. | [16] |
| Boiling Method | Cervical Swabs (HPV) | Detection rate of 10.02%; failed when hemoglobin > 30 g/L. | [16] |
| Combination Approach | Processed Chestnut Rose Juice | Highest DNA quality and PCR amplification efficiency; more time-consuming and costly. | [17] |
| Modified CTAB-Based | Processed Chestnut Rose Juice | High DNA concentration; poor DNA quality and PCR performance. | [17] |
| Automated Systems (KingFisher, Maxwell, GenePure) | Human Stool Samples | Demonstrated differences in DNA yield, purity, and subsequent 16S rRNA sequencing profiles; bead-beating crucial for microbial lysis. | [18] |
Detailed Experimental Protocols
To ensure reproducibility, below are the detailed protocols for two key compared methods.
Protocol 1: Magnetic Bead-Based DNA Extraction for HPV Detection [16] This protocol uses the qEx-DNA/RNA virus T183 kit (Tianlong Corporation) on a PANA 9600s instrument.
- Lysis: A 300 µL sample is transferred to a plate and mixed with lysis buffer to break open cells and viruses.
- Binding: Magnetic beads are added, which bind the liberated nucleic acids.
- Washing: The bead-nucleic acid complex is subjected to multiple wash steps to remove contaminants like proteins and salts. The process is automated, with magnetic attraction used to separate beads from supernatants.
- Elution: Purified DNA is eluted from the magnetic beads in a low-salt elution buffer. The final 5 µL eluate is used for subsequent PCR reactions.
Protocol 2: DNA Extraction from Processed Food Matrices [17] This "combination approach" for challenging samples like Chestnut rose juice involves:
- Lysis: Cell lysis using a combination of chemical and mechanical methods to break down tough plant and processed food matrices.
- Purification: A multi-step purification process, often involving silica-based columns or specialized solutions, to remove PCR inhibitors common in food (e.g., polyphenols, polysaccharides).
- Assessment: The quantity and quality of the extracted DNA are assessed using a NanoDrop spectrophotometer and gel electrophoresis. The DNA's amplifiability is confirmed with real-time PCR using species-specific primers (e.g., for the Internal Transcribed Spacer 2 (ITS2) region).
Extraction Workflow and Selection
The following diagram illustrates the decision-making workflow for selecting an appropriate nucleic acid extraction method based on sample type and downstream application.
Nucleic Acid Amplification Techniques
Following extraction, nucleic acid amplification is employed to detect and quantify specific genetic targets. While Polymerase Chain Reaction (PCR) is the most ubiquitous, several isothermal techniques offer compelling alternatives.
Comparison of Amplification Techniques
The table below provides a side-by-side comparison of the key characteristics of major amplification technologies.
Table 2: Characteristics of Major Nucleic Acid Amplification Techniques (NAATs) [19]
| Technique | Principle | Template | Temperature | Key Advantages | Primary Limitations |
|---|---|---|---|---|---|
| PCR | Thermal cycling, enzyme: DNA polymerase | DNA | Thermo-cycling | High sensitivity, gold standard, versatile | Requires thermal cycler |
| RT-PCR | Reverse transcription + PCR | RNA | Thermo-cycling | High sensitivity for RNA, quantitative | Requires thermal cycler |
| LAMP | Auto-cycling strand displacement, enzyme: Bst polymerase | DNA | Isothermal (~65°C) | Rapid, simple, visual detection, equipment-free | Complex primer design |
| NASBA | Enzymatic RNA amplification, enzymes: Reverse transcriptase, RNase H, T7 RNA polymerase | RNA | Isothermal (~41°C) | High sensitivity for RNA, rapid | Expensive kits, complex master mix |
| TMA | Similar to NASBA | RNA / DNA | Isothermal | Highly sensitive, rapid (<2 hours) | - |
| SDA | Enzymatic nicking and displacement | DNA | Isothermal | High sensitivity, can amplify ss/dsDNA | Shorter product size (<1kb) |
Key Research Reagent Solutions
A successful molecular amplification assay relies on a suite of specialized reagents.
Table 3: Essential Reagents for Nucleic Acid Amplification and Analysis
| Reagent / Kit | Function | Example Use-Case |
|---|---|---|
| Tellgenplex HPV27 DNA Test | Multiplex PCR and hybridization for 27 HPV genotypes. | Genotyping of human papillomavirus from cervical swabs. [16] |
| ZymoBIOMICS Microbial Community Standard | Defined mock microbial community. | Positive control and standardization for 16S rRNA amplicon sequencing studies. [18] |
| Nextera DNA Library Prep Kit | Preparation of sequencing libraries from fragmented DNA. | Library construction for Illumina NGS platforms. [18] |
| DNA Binding Magnetic Beads | Solid-phase reversible immobilization for nucleic acid purification. | Automated extraction of DNA/RNA from various biological samples. [16] [18] |
| Real-time PCR Master Mix | Optimized buffer, enzymes, dNTPs, and fluorescent dye/probe chemistry. | Quantitative PCR (qPCR) for gene expression or pathogen detection. [17] |
Nucleic Acid Sequencing Technologies
Sequencing technologies have evolved from reading single genes to deciphering entire genomes, enabling comprehensive analysis of genetic information.
Next-Generation Sequencing (NGS) Platforms
Next-Generation Sequencing (NGS), or Massively Parallel Sequencing (MPS), is the cornerstone of modern genomics, allowing for the simultaneous sequencing of millions of DNA fragments [20] [21].
Table 4: Comparison of Key DNA Sequencing Platforms and Technologies [20] [22] [21]
| Sequencing Technology / Platform | Read Length | Key Features | Primary Applications |
|---|---|---|---|
| Illumina (NovaSeq X, MiSeq) | Short-read (200-300 bp) | High accuracy, ultra-high throughput, low cost per genome. | Whole Genome Sequencing (WGS), targeted sequencing, metagenomics, transcriptomics. |
| Ion Torrent (GeneStudio S5) | Short-read (up to 600 bp) | Semiconductor-based detection, rapid run times, scalable chip formats. | Targeted sequencing, cancer research, infectious disease. |
| Oxford Nanopore (MinION, PromethION) | Long-read (ultra-long >100 kb) | Real-time sequencing, portable, direct RNA sequencing, high throughput. | Genome assembly, structural variant detection, real-time surveillance, epigenetics. |
| PacBio (HiFi Reads) | Long-read ( >15 kb) | High accuracy (>99.9%), circular consensus sequencing. | De novo genome assembly, haplotype phasing, variant discovery. |
| Roche SBX (Sequencing by Expansion) | N/A (Novel chemistry) | Novel Xpandomer chemistry, CMOS-based detection, high throughput. (Launch 2026) | High-throughput genome sequencing. [21] |
| Element AVITI | Short-read (300 bp) | Q40-level accuracy, flexible and cost-effective benchtop system. | Broad research applications. [21] |
The Integrated Molecular Diagnostics Workflow
The synergy between extraction, amplification, and sequencing is best demonstrated in advanced diagnostic applications. The following diagram outlines a modern workflow for pathogen detection, such as in culture-negative infective endocarditis, integrating molecular methods with traditional approaches.
The molecular toolkit, comprising nucleic acid extraction, amplification, and sequencing technologies, has fundamentally transformed biological research and clinical diagnostics. As this guide illustrates, the selection of methods is not a one-size-fits-all endeavor. The optimal choice hinges on the sample matrix, the required sensitivity and specificity, the scale of the project, and the available resources. While culture-based methods retain value for antimicrobial susceptibility testing, the future lies in integrated, multimodal approaches. The continued evolution of these technologies—particularly the rise of third-generation sequencing, point-of-care molecular platforms, and the integration of AI for data analysis—promises to further enhance our ability to decipher complex biological systems, accelerate drug discovery, and usher in a new era of precision medicine.
Biofilms are structured communities of microbial cells enclosed in a self-produced matrix of extracellular polymeric substances (EPS) that adhere to biological or inert surfaces [23] [24]. This matrix, composed of polysaccharides, proteins, lipids, and extracellular DNA (eDNA), creates a protective environment that allows microbes to persist in extreme conditions and resist antimicrobial agents and host immune responses [25] [26]. It is estimated that up to 80% of bacterial and archaeal cells exist in biofilm form in nature, representing the predominant mode of microbial life [25] [26].
The diagnostic challenge emerges from this very structure. The EPS matrix acts as a physical and chemical barrier, while the heterogeneous nature of biofilms—containing metabolically dormant cells alongside active ones—creates populations with differential susceptibility to treatments [24] [27]. Traditional culture-based methods, developed for free-floating (planktonic) bacteria, frequently fail to accurately identify the complex microbial consortia within biofilms, leading to inadequate treatments and persistent infections [28] [29]. This review systematically compares traditional culture-based and modern molecular diagnostic methods for biofilm-associated infections, providing researchers with evidence-based guidance for method selection.
How Biofilms Confer Resistance and Evade Detection
The Protective Architecture of Biofilms
The resilience of biofilms stems from their complex structure and composition. The EPS matrix provides mechanical stability and limits the penetration of antimicrobial agents [24] [27]. Beyond this physical barrier, biofilms exhibit heterogeneous metabolic activity, with gradients of nutrients and oxygen creating varied microenvironments from the surface to the core [24] [26]. This spatial organization supports the survival of dormant persister cells that exhibit exceptional tolerance to antibiotics [27].
Table 1: Key Components of the Biofilm Extracellular Matrix and Their Protective Functions
| Matrix Component | Primary Functions | Impact on Resistance & Detection |
|---|---|---|
| Exopolysaccharides | Structural integrity, adhesion, barrier formation | Limits antibiotic penetration; traps antimicrobial agents |
| Extracellular DNA (eDNA) | Structural support, genetic information exchange | Facilitates horizontal gene transfer of resistance genes |
| Proteins & Enzymes | Metabolic cooperation, matrix stabilization | Degrades some antimicrobial compounds; enhances stability |
| Water (up to 97%) | Hydration, nutrient diffusion | Creates dissolution gradients for antimicrobial agents |
Genetic Regulation and Communication
Biofilm development is precisely regulated through quorum sensing (QS), a cell-density dependent communication system that coordinates gene expression across the microbial community [24] [27]. In Gram-negative bacteria, LuxI/LuxR-type systems using acyl-homoserine lactones (AHLs) regulate biofilm maturation and virulence factor production, while Gram-positive bacteria employ oligopeptide-based two-component systems [27]. This coordinated behavior enables biofilms to mount unified defensive responses to environmental threats, including antibiotic challenges.
The following diagram illustrates the structural and genetic factors that contribute to the diagnostic challenges of biofilms:
Comparative Analysis of Diagnostic Approaches
Fundamental Limitations of Culture-Based Methods
Traditional culture methods face insurmountable challenges when confronting biofilm-associated infections. These techniques were designed for planktonic bacteria in their logarithmic growth phase, not for the complex, slow-growing, and heterogeneous communities found in biofilms [28]. The very process of sampling often fails to dislodge deeply embedded microorganisms, and the culture conditions cannot replicate the specific environmental requirements of all biofilm inhabitants [29].
Critical limitations include:
- Inadequate disaggregation: Standard processing may not effectively disperse biofilm clusters, resulting in underestimation of microbial diversity [28] [29].
- Non-cultivable organisms: Many bacteria within biofilms enter a viable but non-culturable (VBNC) state or have specific nutritional requirements not met by standard media [28].
- Selection bias: Routine culture media favor fast-growing species over slow-growing or anaerobic organisms, distorting the representation of the true microbial community [29].
- Polymicrobial oversight: In mixed infections, dominant species may overgrow and mask the presence of clinically significant co-infections [30] [29].
The Molecular Revolution in Biofilm Diagnostics
Molecular techniques bypass the need for cultivation, instead detecting microbial genetic material regardless of the physiological state of the organisms. These methods have revealed a startling disparity between what culture shows and the actual complexity of biofilm infections [28] [29].
Table 2: Methodological Comparison of Culture vs. Molecular Identification for Biofilm Diagnostics
| Parameter | Culture-Based Methods | Molecular Methods (16S rRNA Sequencing) |
|---|---|---|
| Sensitivity | Low (detects ~1% of total microbiota) | High (theoretically a single copy of target DNA) |
| Time to Result | 24-72 hours (plus additional for identification) | 6-8 hours for PCR-DGGE; 24-48 hours for sequencing |
| Polymerobial Detection | Limited, often misses mixed communities | Excellent, specifically designed for complex mixtures |
| Required Bacterial Viability | Essential | Not required (detects viable, dead, and VBNC cells) |
| Quantification Capability | Quantitative (CFU/mL) | Semi-quantitative to quantitative (depending on method) |
| Species Identification Range | Limited to known, cultivable species | Broad, including uncultivated and novel species |
Quantitative Evidence: A Revealing Comparison
A landmark study comparing both methodologies across 168 chronic wounds demonstrated the dramatic superiority of molecular approaches. While culture methods identified only 17 different bacterial taxa, molecular identification using 16S rDNA sequencing revealed 338 different bacterial taxa in the same sample set [28]. This represents a 20-fold increase in microbial diversity detection with molecular methods.
Similarly, in urinary catheter-related samples, molecular techniques detected a significantly broader spectrum of microbes, including the emerging opportunistic pathogen Actinotignum schaalii, which was frequently missed by culture [29]. The same study reported that 86.1% of positive samples were polybacterial, far exceeding what routine culture could detect [29].
Experimental Protocols for Biofilm Analysis
Sample Processing and DNA Extraction Protocol
Effective biofilm analysis requires specialized sample processing to disrupt the EPS matrix and release embedded microorganisms:
Sonication Procedure:
- Place sample in 5 mL of Brain Heart Infusion (BHI) broth
- Perform two 5-minute sonication cycles interspersed with 2 minutes of vortexing [29]
- Centrifuge the sonication fluid and suspend the pellet in lysis buffer
DNA Extraction:
- Add sterile steel and glass beads to the sample
- Process in a TissueLyser at 30 Hz for 5 minutes for complete bacterial lysis
- Use commercial DNA extraction kits (e.g., QIAamp DNA Mini Kit) following manufacturer's protocols
- Elute DNA in 30 μL water and dilute to a final concentration of 20 ng/μL [28]
16S rRNA Amplification and Sequencing
The molecular workflow for biofilm analysis typically follows these steps:
For 16S rRNA amplification:
- Use modified primers 28F (5′-GAGTTTGATCNTGGCTCAG-3′) and 519R (5′-GTTTACNGCGGCKGCTG-3′) to amplify a 500 bp region [28]
- For FLX-Titanium amplicon pyrosequencing, add linkers and barcodes to primers: 28F-A (5′-CCATCTCATCCCTGCGTGTCTCCGACTCAG-barcode-GAGTTTGATCNTGGCTCAG-3′) and biotinylated 519R-B [28]
- Perform PCR under optimized conditions for complex samples
Advanced Transcriptomic Analysis of Biofilms
For comprehensive understanding of biofilm gene expression, RNA-sequencing (RNA-seq) with specialized bioinformatic tools can identify differentially expressed genes under various conditions. The scorecard method, a Python-based software tool, helps manage the heterogeneity of gene expression data across multiple experimental conditions by grouping genes based on relative fold-change and statistical significance [31]. This approach is particularly valuable for identifying:
- Genes consistently up- or down-regulated across experiments
- Antibiotic resistance mechanisms
- Metabolic adaptations in biofilm phenotypes
- Virulence factors specific to biofilm mode of growth [31]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Biofilm Studies
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| DNA Extraction Kits | QIAamp DNA Mini Kit | Efficient DNA extraction from complex biofilm matrices |
| PCR Reagents | Modified 16S primers (28F/519R) | Amplification of bacterial rRNA genes from mixed communities |
| Specialized Media | Wilkins-Chalgren Agar, BHI with supplements | Cultivation of fastidious and anaerobic biofilm organisms |
| Sequencing Platforms | Illumina MiSeq, Pyrosequencing | High-throughput analysis of microbial community composition |
| Bioinformatic Tools | Scorecard Python library, RipSeq Mixed | Analysis of complex transcriptomic and sequencing data |
| Disruption Reagents | Enzymatic matrix disruptors (dispersin B, DNase I) | EPS breakdown for improved microbial recovery |
| 6-Methylthioguanine-d3 | 6-Methylthioguanine-d3, MF:C6H7N5S, MW:184.24 g/mol | Chemical Reagent |
| Hydroxymethyl Clenbuterol-d6 | Hydroxymethyl Clenbuterol-d6, MF:C12H18Cl2N2O2, MW:299.22 g/mol | Chemical Reagent |
The evidence overwhelmingly demonstrates that traditional culture-based methods are inadequate for comprehensive analysis of biofilm-associated infections. The 20-fold higher detection rate of microbial diversity with molecular methods fundamentally changes our understanding of infectious diseases and explains why many chronic infections persist despite apparently negative culture results [28].
For researchers and clinicians, the implications are profound. Molecular techniques—particularly 16S rRNA sequencing and advanced transcriptomic approaches—provide unprecedented insights into the true complexity of biofilm communities [31] [29]. While culture retains value for antibiotic susceptibility testing and certain clinical scenarios, it should no longer be considered the gold standard for biofilm diagnosis.
The future of biofilm management lies in embracing these advanced molecular tools, developing standardized protocols for their implementation, and integrating their findings into therapeutic strategies. Only through this paradigm shift can we hope to effectively address the significant clinical challenges posed by biofilm-associated infections.
The field of clinical microbiology has undergone a profound transformation over the past century, moving from traditional culture-based methods grounded in Koch's postulates to modern genomic approaches that offer unprecedented resolution and speed. This paradigm shift represents not merely a technological upgrade but a fundamental change in how we detect, identify, and understand infectious diseases. The original Koch's postulates, formulated in the late 19th century, established a systematic framework for linking specific microorganisms to diseases through four criteria: consistent presence in disease, isolation in pure culture, disease reproduction in healthy hosts, and re-isolation from experimentally infected hosts [32] [33]. While these principles revolutionized medical microbiology, their limitations in addressing complex modern challenges have driven the development of molecular approaches that now complement and often surpass traditional methods [32].
The emergence of genomic medicine has introduced powerful new tools for pathogen identification, leveraging advances in DNA sequencing, bioinformatics, and computational analysis to transform diagnostic capabilities [34]. This shift has been particularly driven by the recognition that traditional methods struggle with unculturable organisms, polymicrobial infections, and the need for rapid results in clinical settings [35] [36]. The integration of genomic approaches has enabled researchers and clinicians to move beyond the constraints of Koch's original framework while preserving its core emphasis on establishing causal relationships between pathogens and disease [32].
Koch's Postulates: The Classical Framework
Original Principles and Historical Significance
Robert Koch's postulates, formulated in 1884, provided the first systematic methodology for establishing microbial pathogenesis [33]. The four original criteria required that:
- The microorganism must be found in diseased but not healthy individuals
- The microorganism must be cultured from the diseased individual
- Inoculation of a healthy individual with the cultured microorganism must recapitulate the disease
- The microorganism must be re-isolated from the inoculated, diseased individual [37] [33]
These principles created a rigorous experimental framework that allowed Koch and his contemporaries to definitively link specific bacteria to diseases such as anthrax and tuberculosis, marking the birth of modern infectious disease microbiology [32]. The postulates established causation standards that guided pathogen research for decades and remain foundational in medical education for developing scientific reasoning and diagnostic logic [32].
Limitations and Challenges
Despite their historical importance, Koch's postulates revealed significant limitations when applied to various infectious agents:
- Asymptomatic carriers: Koch himself discovered that asymptomatic individuals could carry Vibrio cholerae and Salmonella typhi, contradicting the first postulate's requirement that pathogens be absent in healthy hosts [37] [33]
- Unculturable organisms: Approximately 1% of bacterial species can be cultured using standard laboratory techniques, leaving many potential pathogens undetectable [32]
- Host-specific pathogens: Some microorganisms, such as Mycobacterium leprae and human-specific viruses, cannot infect available animal models, making it impossible to fulfill the third postulate [32] [33]
- Polymicrobial diseases: Many infections involve complex microbial communities where no single organism independently causes disease [32]
- Ethical constraints: Deliberate infection of human subjects to satisfy the third postulate raises significant ethical concerns [38] [33]
These limitations became increasingly apparent with the discovery of viruses, parasitic organisms with complex life cycles, and conditional pathogens whose disease manifestation depends on host factors [38] [32].
The Molecular Revolution: Transition to Genomic Medicine
Revised Postulates for Modern Microbiology
Recognizing the limitations of classical approaches, microbiologists have proposed various modifications to Koch's postulates:
Molecular Koch's postulates, introduced by Stanley Falkow in 1988, shifted focus from whole organisms to specific virulence genes [32] [33]. These criteria require that:
- The phenotype or property under investigation should be associated with pathogenic members of a genus or pathogenic strains of a species
- Specific inactivation of the gene(s) associated with the suspected virulence trait should lead to a measurable loss in pathogenicity or virulence
- Reversion or allelic replacement of the mutated gene should restore the pathogenicity [33]
Nucleic acid-based postulates proposed by Fredricks and Relman in 1996 emphasized sequence-based detection, requiring that a pathogen's nucleic acids be present in diseased tissues, correlate with disease development, and predictively align with known biological characteristics of related organisms [32].
For parasitic diseases, tailored postulates have been developed that account for complex life cycles, asymptomatic carriage, and host susceptibility factors [38]. These include requirements for consistent detection using validated methods, correlation with clinical symptoms, reproduction of disease in suitable animal models, and therapeutic response to anti-parasitic treatment [38].
Technological Drivers of the Paradigm Shift
The transition from traditional to genomic approaches has been fueled by revolutionary technological advances:
Next-generation sequencing (NGS) platforms, particularly Illumina sequencing-by-synthesis, have dramatically reduced the cost of DNA sequencing while generating enormous datasets [39]. This "democratization of technology" has made large-scale genomic studies accessible to most research groups [39].
Third-generation sequencing technologies from Oxford Nanopore and Pacific Biosystems produce much longer reads (several to hundreds of kilobase pairs) and enable single-molecule sequencing without amplification [34].
Functional genomic tools including transposon insertion sequencing (Tn-seq) and CRISPR interference (CRISPRi) methods allow genome-wide fitness profiling and targeted gene inactivation [39]. These approaches identify genes essential for bacterial survival under specific conditions, linking genes to important phenotypes like virulence and antibiotic resistance [39].
Table 1: Key Technological Advances Enabling Genomic Medicine
| Technology | Key Features | Applications in Microbiology |
|---|---|---|
| Next-generation sequencing (NGS) | High-throughput, massively parallel, reduced cost | Bacterial GWAS, strain typing, outbreak investigation |
| Third-generation sequencing | Long reads, single-molecule sequencing | Complete genome assembly, structural variation analysis |
| Tn-seq/TraDIS | Genome-wide fitness profiling | Essential gene identification, virulence factor discovery |
| CRISPRi | Targeted gene knockdown | Functional validation of virulence genes |
| Microarray/Ibis T5000 | Multiplex pathogen detection | Rapid identification of known pathogens |
Comparative Analysis: Traditional vs. Molecular Methods
Methodological Principles and Workflows
Traditional culture-based methods and molecular genomic approaches operate on fundamentally different principles:
Traditional methods rely on phenotypic characteristics of microorganisms, including growth patterns, biochemical reactions, and morphological features [36]. The workflow typically involves specimen collection, culture on selective media, isolation of pure colonies, biochemical identification, and antimicrobial susceptibility testing [36]. This process requires viable organisms and can take 24-72 hours for preliminary results, with complete identification and susceptibility profiles requiring additional time [36].
Molecular methods target specific genomic sequences or molecular markers associated with pathogens [36]. Common workflows include nucleic acid extraction, amplification (e.g., PCR), and detection through various platforms [35] [36]. These approaches can provide results within hours, significantly reducing turnaround time compared to culture methods [36].
The following diagram illustrates the key workflows for both traditional and molecular diagnostic methods:
Figure 1: Comparative workflows of traditional culture-based versus molecular genomic diagnostic methods, highlighting significant differences in processing time and technique.
Performance Comparison in Clinical Settings
Multiple studies have directly compared the performance of traditional and molecular methods in clinical diagnostics:
A 2016 study on necrotizing soft tissue infections (NSTIs) demonstrated that molecular methods identified microorganisms in 90% of surgical samples, compared to 70% with culture-based methods [35]. Molecular approaches frequently detected additional microorganisms beyond those identified by culture, revealing greater microbial complexity in these infections [35].
In clinical microbiology laboratories, molecular methods have replaced culture for numerous applications including MRSA surveillance, gastrointestinal pathogen panels, Streptococcus pyogenes detection, Bordetella pertussis identification, and viral pathogen detection [36]. The transition has been driven by molecular methods' superior sensitivity and specificity, combined with significantly reduced turnaround times [36].
Table 2: Performance Comparison of Traditional vs. Molecular Methods
| Parameter | Traditional Methods | Molecular Methods |
|---|---|---|
| Turnaround Time | 24-72 hours for preliminary results, 3-5 days for complete workup | Hours to 1 day |
| Sensitivity | Lower (depends on organism viability) | Higher (amplification enables detection of few copies) |
| Specificity | Lower (based on phenotypic characteristics) | Higher (based on genetic targets) |
| Viability Assessment | Yes (requires live organisms) | No (detects DNA from live and dead organisms) |
| Polymicrobial Detection | Challenging (may miss slow-growing organisms) | Excellent (multiple targets can be detected simultaneously) |
| Quantification | Possible (colony counts) | Limited on most platforms |
| Antimicrobial Susceptibility | Direct testing possible | Usually infers resistance from genetic markers |
| Cost | Lower | Higher |
Applications in Specific Clinical Scenarios
The complementary strengths of traditional and molecular methods make each suitable for different clinical scenarios:
Molecular methods excel in situations requiring rapid results that directly impact patient management. For example, meningitis/encephalitis panels can identify multiple pathogens within hours, enabling appropriate antibiotic selection when time is critical [36]. Similarly, gastrointestinal pathogen panels can simultaneously test for multiple bacterial, viral, and parasitic pathogens that would require separate cultures and staining procedures using traditional methods [36].
Traditional methods remain valuable when antimicrobial susceptibility testing is required, when dealing with organisms not covered by molecular panels, or when specimen quality may impact molecular test performance [36]. Culture also enables quantification of bacterial load, which can be clinically relevant in certain infections [36].
For complex infections like necrotizing soft tissue infections, the combined use of both methods provides the most comprehensive picture. Molecular methods offer rapid identification of likely pathogens, while culture provides isolates for susceptibility testing [35].
Genomic Medicine in Contemporary Research and Diagnostics
Advanced Genomic Applications
Genomic approaches have enabled sophisticated research methodologies that transcend traditional diagnostic capabilities:
Genome-wide association studies (GWAS) in bacteria use comparative genomics to identify genomic elements statistically associated with specific phenotypes or environmental conditions [39]. This approach has successfully identified candidate genes involved in host specificity, virulence, and antibiotic resistance across numerous bacterial species [39].
Whole-genome fitness profiling using transposon insertion sequencing (Tn-seq) identifies genes essential for bacterial survival under specific conditions by monitoring the frequency of transposon insertions across the genome [39]. This method has linked genes to metabolic pathways, stress response, antibiotic resistance, and virulence [39].
Bacterial GWAS approaches now incorporate quantitative trait variation, machine learning, and phylogenetic analyses to account for population structure and identify convergent evolution in divergent strains [39].
Implementation Challenges and Solutions
Despite their advantages, genomic methods face implementation challenges:
Bioinformatic expertise is required for data analysis and interpretation, creating a barrier for some clinical laboratories [39] [34]. Solutions include user-friendly bioinformatics pipelines and increased training for laboratory personnel.
Cost considerations remain significant, particularly for comprehensive genomic analyses [34]. However, decreasing sequencing costs and the development of targeted panels make genomic approaches increasingly accessible.
Regulatory and standardization issues need addressing as molecular methods evolve rapidly compared to traditional approaches [36]. Ongoing efforts by regulatory agencies aim to produce updated guidelines addressing current laboratory practices and technical standards [36].
Data interpretation challenges arise from detecting multiple organisms or genetic markers of uncertain significance [35]. This requires correlation with clinical findings and appropriate stewardship of molecular testing.
Experimental Protocols and Research Applications
Key Methodologies in Genomic Microbiology
Bacterial Genome-Wide Association Studies (GWAS)
- Sample Collection: Hundreds of bacterial isolates from different environments or conditions [39]
- Genome Sequencing: Whole-genome sequencing using NGS platforms [39]
- Variant Identification: Detection of SNPs, k-mers, or accessory genetic elements [39]
- Association Analysis: Statistical testing for genetic elements associated with phenotypes, accounting for population structure [39]
- Validation: Functional validation of candidate genes through mutagenesis or other experimental approaches [39]
Transposon Insertion Sequencing (Tn-seq)
- Library Construction: Generation of comprehensive transposon insertion mutants [39]
- Selection Pressure: Growth under defined in vitro or in vivo conditions [39]
- DNA Preparation: Amplification and sequencing of transposon-genome junctions [39]
- Data Analysis: Mapping insertion sites and calculating fitness coefficients [39]
- Hit Identification: Statistical identification of genomic regions with significantly fewer insertions (essential genes) [39]
Metagenomic Sequencing for Pathogen Detection
- Sample Processing: Direct DNA extraction from clinical samples without culture [35]
- Library Preparation: Fragmentation, adapter ligation, and amplification [34]
- Sequencing: High-throughput sequencing on platforms such as Illumina or Oxford Nanopore [39] [34]
- Bioinformatic Analysis: Taxonomic classification using reference databases [35]
- Pathogen Identification: Correlation of abundance with clinical findings [35]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Genomic Microbiology
| Reagent/Category | Function | Examples/Applications |
|---|---|---|
| NGS Library Prep Kits | Prepare DNA fragments for sequencing | Illumina Nextera, NEBNext Ultra |
| Transposon Mutagenesis Systems | Generate comprehensive mutant libraries | Himar1 mariner transposon, EZ-Tn5 |
| CRISPR Interference Systems | Targeted gene knockdown | dCas9-sgRNA complexes for bacterial gene repression |
| 16S rRNA Sequencing Reagents | Microbial community profiling | Primers targeting hypervariable regions, clone libraries |
| Whole Genome Amplification Kits | Amplify limited DNA samples | MDA (Multiple Displacement Amplification) |
| Bioinformatics Pipelines | Analyze sequencing data | SPAdes (genome assembly), Bowtie2 (read alignment), DESeq2 (differential abundance) |
| DNA Extraction Kits | Isolate DNA from complex samples | Soil, stool, and tissue DNA extraction kits |
| Selective Culture Media | Traditional isolation of pathogens | Chromogenic media for specific pathogen identification |
| 3-epi-Ochratoxin A-d5 | 3-epi-Ochratoxin A-d5|Isotope-Labeled Internal Standard | 3-epi-Ochratoxin A-d5 is a deuterium-labeled internal standard for precise Ochratoxin A quantification in research. For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
| Midazolam 2,5-Dioxide-d6 | Midazolam 2,5-Dioxide-d6, CAS:1215321-98-4, MF:C18H13ClFN3O2, MW:363.8 g/mol | Chemical Reagent |
The integration of genomic approaches into clinical microbiology continues to accelerate, driven by ongoing technological advances and decreasing costs. Third-generation sequencing technologies are producing longer reads that improve genome assembly and enable detection of structural variations [34]. The application of machine learning and artificial intelligence to genomic datasets promises to enhance pattern recognition and predictive modeling for outbreak investigation and transmission tracking [39].
The concept of "reverse microbial etiology" exemplifies the paradigm shift from reactive to proactive approaches [32]. Rather than waiting for disease outbreaks to identify pathogens, this approach establishes pathogen warning systems through ongoing environmental surveillance [32]. This aligns with the transition in healthcare from treatment-centered models to comprehensive frameworks integrating prevention, diagnosis, treatment, and health maintenance [32].
The complementary relationship between traditional and molecular methods will likely continue evolving. While molecular approaches offer unprecedented speed and resolution, traditional culture methods remain essential for antimicrobial susceptibility testing, outbreak investigation, and understanding the biological characteristics of pathogens [36]. The future of clinical microbiology lies not in complete replacement of traditional methods but in their strategic integration with genomic approaches to provide comprehensive diagnostic capabilities.
In conclusion, the shift from Koch's postulates to genomic medicine represents a fundamental transformation in how we detect and understand infectious diseases. While Koch's principles established crucial foundational standards for establishing causation, modern genomic approaches have overcome their limitations through molecular detection, sophisticated analysis, and rapid diagnostics. This paradigm shift has expanded our view of host-pathogen interactions, revealed previously unrecognized microbial complexity, and provided powerful new tools for clinical diagnostics and public health. As genomic technologies continue to evolve, they will undoubtedly uncover new dimensions of microbial pathogenesis while further transforming the diagnosis, treatment, and prevention of infectious diseases.
Methodological Approaches and Real-World Applications in Clinical and Research Settings
For over a century, microbial culture has served as the fundamental cornerstone of microbiological diagnosis, providing the benchmark for detecting and identifying pathogens [40]. However, contemporary diagnostic laboratories are increasingly navigating a paradigm shift, integrating or substituting traditional culture-based methods with advanced molecular techniques [40]. This transition is driven by the recognition of well-documented limitations inherent in culture, including prolonged turnaround times, intensive labor requirements, and the frequent failure to identify difficult-to-culture or fastidious microorganisms [41] [40]. Molecular diagnostics (MDx), particularly nucleic acid amplification tests (NAATs), offer a compelling alternative with superior speed, sensitivity, and specificity [40].
This guide provides an objective, data-driven comparison of these methodologies, framing the discussion within the broader thesis of culture-based versus molecular method research. It is designed to equip researchers, scientists, and drug development professionals with the empirical evidence and procedural knowledge necessary to select the optimal technique for their specific sample type and microbial target.
Performance Comparison: Culture vs. Molecular Diagnostics
Extensive head-to-head studies across various clinical scenarios consistently demonstrate the enhanced sensitivity and efficiency of molecular methods compared to traditional culture. The following table summarizes quantitative performance data from recent comparative studies.
Table 1: Quantitative Performance Comparison of Culture vs. Molecular Diagnostics
| Study & Sample Type | Target Pathogen(s) | Method | Sensitivity | Key Performance Findings | Turnaround Time |
|---|---|---|---|---|---|
| Podiatric Wound Infections [41] | Polymicrobial pathogens (S. aureus, P. aeruginosa, etc.) | Traditional Culture | Reference | Underdetected ~30% of clinically significant pathogens found by PCR. | Several days |
| Real-time PCR Panel | 98.3% (vs. culture) | Detected 110 significant pathogens missed by culture; high sensitivity in polymicrobial wounds. | Significantly faster (specific time not given) | ||
| CPGNB Rectal Swabs [3] | Carbapenemase-producing Gram-negative bacilli | Culture-based (ChromID CARBA SMART) | 64.8% | Required substantial hands-on time (~90 minutes). | Lengthy (includes incubation) |
| Direct Molecular (Xpert Carba-R) | 90.2% | Superior sensitivity; minimal hands-on time (~1.3 minutes). | ~1 hour (hands-on time) | ||
| Campylobacter Enteritis [40] | Campylobacter species | Culture | 51.2% | Difficulties due to fastidious growth requirements. | Up to 10 days |
| PCR | 100% (relative to PCR-positive) | Significantly superior sensitivity, specificity, and positive predictive value. | Within a day | ||
| Urinary Tract Infections [40] | Polymicrobial infections | Urine Culture | 22% | Poorly detects polymicrobial infections. | 24-48 hours |
| Multiplex PCR | 95% | Significantly more sensitive for detecting co-infections. | Within a day |
Detailed Experimental Protocols for Key Studies
This protocol is designed for a year-long, large-scale comparison study in a moderate-prevalence setting.
- Sample Type: Rectal swabs from patients.
- Sample Collection & Processing:
- Collect swabs and process for both culture and molecular methods from the same specimen.
- Culture-Based Method:
- Inoculation: Plate the sample onto chromID CARBA SMART selective agar.
- Incubation: Incubate plates under appropriate conditions to isolate Gram-negative bacilli.
- Confirmation: Perform conventional PCR on isolated colonies to confirm the presence of carbapenemase genes.
- Inclusion of NFGNB: The study emphasized including non-fermenting Gram-negative bacilli (NFGNB) in the analysis, which significantly increased the sensitivity of the culture strategy from 46.3% to 64.8%.
- Direct Molecular Method:
- Testing: Use the Cepheid Xpert Carba-R assay directly from the specimen.
- Procedure: Follow manufacturer's instructions for nucleic acid extraction, amplification, and detection of carbapenemase genes.
- Reference Standard: A composite reference standard was used, where detection by either method was considered a true positive.
- Data Analysis:
- Calculate sensitivity for each method against the reference standard.
- Measure hands-on technologist time for both methods.
- Track potential patient contact precautions averted by faster, more sensitive molecular results.
This protocol uses a dual-swab approach to minimize sampling variability for a direct comparison.
- Sample Type: Dual-swab specimens from clinical wound cases (e.g., diabetic foot ulcers, pressure ulcers).
- Sample Collection:
- Collect two swabs from the same wound site simultaneously.
- Culture-Based Testing:
- Processing: Send one swab to a commercial reference laboratory for standard culture and antimicrobial susceptibility testing (AST).
- Gram Stain: Review Gram stain results for morphological features (e.g., Gram-positive cocci, Gram-negative rods).
- Molecular Testing (Real-time PCR):
- Nucleic Acid Extraction: Extract from the second swab using the MagMAX Microbiome Ultra Nucleic Acid Isolation Kit on a mechanical bead-based lysis system (e.g., Omni Bead Ruptor Elite).
- PCR Amplification & Detection: Perform real-time PCR using a nanoscale SmartChip Real-Time PCR System with TaqMan assays targeting a comprehensive panel of bacterial and fungal pathogens, plus antibiotic resistance genes.
- Statistical Analysis:
- Concordance: Calculate organism-level concordance.
- Diagnostic Metrics: Determine sensitivity, specificity, PPV, NPV, accuracy, and F1 score using culture as the initial reference.
- Advanced Modeling: Use logistic regression models incorporating 16S rRNA Ct values and Gram morphology. Employ Latent Class Analysis (LCA) to estimate accuracy without assuming a perfect gold standard.
This protocol addresses the challenge of quantifying and comparing growth data from liquid cultures, common in research settings.
- Sample Type: Microbial liquid cultures (e.g., Saccharomyces cerevisiae).
- Culture Setup:
- Inoculation: Grow starter cultures and back-dilute into fresh medium in a 96-well plate (e.g., 200 μL culture volume).
- Automated Monitoring: Use a shaking/incubating plate reader to automatically measure optical density (OD660) every 15 minutes for 24-48 hours.
- Data Processing & Quantification:
- Plot Growth Curves: Plot OD660 versus time for each replicate.
- Calculate Mean Growth: For each growth curve, calculate the mean of all OD660 measurements across the entire time course, generating a single value representing overall growth.
- Normalize: Normalize the mean growth values of test conditions to a control condition (e.g., empty vector control or untreated cells).
- Statistical Comparison: Display normalized data as a bar graph and perform statistical comparisons (e.g., t-tests) on the normalized, quantitative values.
The workflow for a standard comparative diagnostic study, from sample collection to data interpretation, can be visualized as follows:
The Scientist's Toolkit: Essential Research Reagents & Solutions
Successful execution of the protocols above requires specific, high-quality reagents and tools. The following table details key solutions for both culture and molecular workflows.
Table 2: Essential Research Reagent Solutions for Culture and Molecular Techniques
| Item | Function/Description | Example Application |
|---|---|---|
| Vitroids & LENTICULE Discs [42] | Ready-to-use, certified microbial reference materials in a solid, water-soluble matrix. Provide a defined CFU count with stability of 16-24 months. | Quality control for media testing; reliable, standardized inoculum for growth promotion tests without maintaining stock cultures. |
| chromID CARBA SMART Agar [3] | A selective chromogenic culture medium. | Selective isolation and presumptive identification of carbapenemase-producing Gram-negative bacilli from surveillance samples. |
| MagMAX Microbiome Ultra Nucleic Acid Isolation Kit [41] | A kit optimized for efficient simultaneous extraction of DNA and RNA from complex samples, including difficult-to-lyse microbes. | Nucleic acid extraction for comprehensive molecular panels targeting diverse pathogens in wound samples. |
| Xpert Carba-R Assay [3] | A fully integrated, automated cartridge-based NAAT for direct detection of carbapenemase resistance genes from specimens. | Rapid screening and detection of carbapenemase producers directly from rectal swabs, bypassing culture. |
| Omni Bead Ruptor Elite [41] | A mechanical bead-beating homogenizer. | Effective disruption of bacterial cell walls (both Gram-positive and Gram-negative) for superior DNA yield in molecular workflows. |
| SmartChip Real-Time PCR System [41] | A nanoscale, high-throughput real-time PCR system. | Simultaneous detection and quantification of a wide array of pathogens and antibiotic resistance genes in a single run. |
| N-(t-butyl ester-PEG3)-N-bis(PEG3-amine) | N-(t-butyl ester-PEG3)-N-bis(PEG3-amine), MF:C29H61N3O11, MW:627.8 g/mol | Chemical Reagent |
| Amino-PEG16-t-butyl ester | Amino-PEG16-t-butyl ester, MF:C39H79NO18, MW:850.0 g/mol | Chemical Reagent |
Discussion & Concluding Analysis
The collective evidence demonstrates that molecular diagnostics offer transformative advantages in speed, sensitivity, and workflow efficiency for pathogen detection. The ability of multiplex PCR panels to identify polymicrobial infections and difficult-to-culture pathogens represents a significant advancement over traditional methods [41] [40]. Furthermore, the quantifiable reduction in hands-on time with automated molecular systems [3] can free up valuable technical resources in the laboratory.
However, the role of culture remains critical. It is indispensable for obtaining isolates for antimicrobial susceptibility testing (AST), which is vital for guiding targeted therapy and managing antibiotic resistance [40]. Culture also provides the live organisms necessary for public health surveillance, outbreak investigation, and molecular subtyping [40]. Consequently, a reflex culture approach—where specimens with positive molecular results are subsequently cultured—is often recommended for public health priorities [40].
In conclusion, the choice between culture and molecular techniques is not a simple substitution but a strategic decision. Molecular methods are superior for rapid, comprehensive detection, while culture remains the foundation for phenotypic characterization. The future of microbiological diagnosis lies in the intelligent integration of both methodologies, leveraging the strengths of each to optimize patient care, antibiotic stewardship, and public health outcomes.
The accurate and timely detection of pathogens is a cornerstone of public health, clinical diagnostics, and drug development. For decades, culture-based methods have served as the gold standard for identifying bacterial and fungal pathogens. However, the emergence of molecular techniques, particularly polymerase chain reaction (PCR) and its quantitative counterpart (qPCR), has revolutionized diagnostic workflows. This guide provides an objective comparison of the performance between traditional culture-based methods and modern molecular techniques, framing this comparison within the broader thesis of evolving microbiological research methodologies. We summarize critical experimental data from recent studies and detail the protocols that yield these insights, offering researchers a clear evidence base for selecting appropriate diagnostic tools.
Performance Comparison: Culture vs. Molecular Methods
Extensive research directly comparing culture-based and molecular methods consistently demonstrates differences in sensitivity, speed, and overall detection capability. The tables below summarize key quantitative findings from multiple clinical studies across various pathogens and sample types.
Table 1: Comparative Detection Rates of Common Respiratory Bacteria in COPD Patients (Culture vs. qPCR)
| Pathogen | Study | Detection by Culture (%) | Detection by qPCR (%) |
|---|---|---|---|
| Haemophilus influenzae | AERIS (n=2,293 samples) | 26.2 | 43.4 |
| NTHI-004 (n=974 samples) | 23.6 | 47.1 | |
| NTHI-MCAT-002 (n=1,736 samples) | 10.4 | 32.7 | |
| Moraxella catarrhalis | AERIS | 6.3 | 12.9 |
| NTHI-004 | 6.0 | 19.0 | |
| NTHI-MCAT-002 | 4.1 | 15.5 | |
| Streptococcus pneumoniae | AERIS | 17.4 | 11.0* |
| NTHI-004 | 6.1 | 15.6 | |
| NTHI-MCAT-002 | 3.8 | 15.5 |
Note: The lower qPCR rate in the AERIS study for S. pneumoniae was attributed to the misidentification of S. pseudopneumoniae/mitis isolates by conventional culture methods [43].
Table 2: Diagnostic Performance Metrics of qPCR for Group B Streptococcus
| Metric | cfb-based qPCR (%) | sip-based qPCR (%) |
|---|---|---|
| Sensitivity | 94.1 | 92.7 |
| Specificity | 99.0 | 99.5 |
| Positive Predictive Value (PPV) | 97.1 | 98.5 |
| Negative Predictive Value (NPV) | 97.8 | 97.3 |
| Accuracy | 97.6 | 97.6 |
Data from a study of 259 pregnant Vietnamese women, where qPCR demonstrated excellent agreement (Kappa >0.93) with chromogenic culture [44].
Table 3: Advantages and Disadvantages of qPCR vs. Culture-Based Methods
| Feature | qPCR | Culture |
|---|---|---|
| Speed | Rapid (2 - 6 hours) [45] | Slow (24 - 96 hours) [45] |
| Sensitivity | High (detects low-density carriage) [46] | Lower (misses low-density colonization) [46] |
| Specificity | High (targets specific genetic sequences) [43] | Moderate (can misidentify species) [43] |
| Quantification | Yes (provides pathogen load data) [47] | Semi-quantitative only |
| Ability to Detect Viability | No (detects genetic material) | Yes (requires live organisms) |
| Antibiotic Susceptibility Testing | Not possible (though can detect some resistance genes) [48] | Yes (the gold standard) [45] |
| Impact of Prior Antibiotics | Low (detects DNA from non-viable organisms) [43] | High (prevents growth of viable organisms) [43] |
| Cost and Complexity | Higher (specialized equipment and expertise) [47] | Lower (widely available and cost-effective) [45] |
Experimental Insights and Data Analysis
Enhanced Sensitivity and Detection of Co-Colonization
The higher detection rates of qPCR are largely attributed to its superior sensitivity. A study on pneumococcal carriage in African children found that qPCR identified pneumococcus in 82% of nasopharyngeal swabs compared to 71% for culture [46]. This enhanced sensitivity is crucial for detecting multiple serotypes. While culture found co-colonization with multiple serotypes in only 4.5% of samples, qPCR revealed it in 28.7% of samples. The majority of serotypes detected only by qPCR were present at lower densities (<10^4 CFU/ml), which are typically missed by culture [46]. This ability to uncover the true complexity of microbial carriage has significant implications for understanding disease transmission and the impact of vaccines.
Impact of Sample Integrity on Culture Results
The integrity of the sample itself is a critical factor favoring molecular methods. An analysis from the NTHI-004 study highlighted a major limitation of culture: its dependence on viable organisms. When fresh sputum samples that were initially culture-positive were re-tested after a freeze-thaw cycle, less than 50% remained culture-positive [43]. This demonstrates that freezing samples, often necessary for transport to central laboratories, drastically reduces the sensitivity of culture. In contrast, qPCR performed on the same frozen samples maintained high detection rates, as it detects stable DNA rather than relying on viable bacteria [43].
Clinical Utility in Complex Cases
Molecular panels are proving their worth in complex clinical scenarios. A study on hospitalized patients with HIV in a low-income setting found that conventional sputum culture identified a possible bacterial cause in less than 25% of community-acquired pneumonia cases. In contrast, a multiplex PCR panel (BioFire FilmArray Pneumonia Panel) detected a potential bacterial etiology in 83.2% of patients and a viral pathogen in 49.5% [48]. This 64.5% improvement in diagnostic yield can critically inform antimicrobial stewardship, allowing for faster de-escalation from broad-spectrum antibiotics.
Detailed Experimental Protocols
To ensure reproducibility and provide a clear understanding of the methodologies behind the data, this section outlines standard protocols for both culture and qPCR as applied in respiratory sample analysis.
Culture-Based Protocol for Sputum Samples
The following workflow was used in large clinical studies to process sputum samples from COPD patients [43].
Key Steps:
- Sample Collection: Sputum is collected via spontaneous expectoration or induction and transported fresh to the laboratory [43].
- Liquefaction: Samples are treated with dithiothreitol (DTT) to break down mucoid matrices [43].
- Culture: Processed sputum is inoculated onto selective and non-selective agar plates (e.g., chocolate agar, blood agar) [43].
- Incubation: Plates are incubated at 35-37°C in appropriate atmospheres for 24-48 hours [45].
- Identification: Bacterial colonies are identified based on morphology, followed by phenotypic characterization (e.g., Gram stain, biochemical tests) or MALDI-TOF mass spectrometry [43].
- Antimicrobial Susceptibility Testing (AST): If required, isolated pathogens are subjected to disk diffusion or MIC testing to determine resistance profiles, a key advantage of culture [45].
qPCR Protocol for Pathogen Detection
The protocol below describes the centralized qPCR testing used on frozen sputum samples in clinical trials [43].
Key Steps:
- Sample Collection and Storage: Sputum is collected and treated with DTT. The sample is then frozen and can be transported to a central laboratory for analysis [43].
- Nucleic Acid Extraction: DNA is purified from the processed sample using commercial extraction kits. This step is critical for removing PCR inhibitors.
- Reaction Setup: The extracted DNA is combined with a qPCR master mix containing primers and probes specific to the target pathogen(s) (e.g., H. influenzae, S. pneumoniae), DNA polymerase, dNTPs, and buffer [43].
- Amplification and Detection: The plate is run on a real-time PCR instrument. The instrument undergoes thermal cycling (denaturation, annealing, extension) while monitoring fluorescence. A positive signal occurs when the fluorescence exceeds a threshold limit, yielding a cycle threshold (Ct) value [47].
- Analysis: The Ct value is inversely proportional to the amount of target DNA in the original sample, providing semi-quantitative data on pathogen load [45].
Essential Research Reagent Solutions
The successful implementation of these diagnostic protocols relies on a suite of specific reagents and materials. The following table details key solutions required for the qPCR workflow.
Table 4: Key Research Reagent Solutions for qPCR-Based Pathogen Detection
| Reagent/Material | Function | Examples & Notes |
|---|---|---|
| Nucleic Acid Extraction Kits | Purifies DNA/RNA from clinical samples, removing inhibitors that can affect PCR. | Kits using silica-membrane technology or magnetic beads are standard. |
| qPCR Master Mix | Provides the core components for the amplification reaction, including buffer, DNA polymerase, dNTPs, and MgClâ‚‚. | Often supplied with a passive reference dye for normalization. |
| Sequence-Specific Primers | Short DNA sequences that define the start and end points of the target DNA segment for amplification. | Must be highly specific to the pathogen of interest to ensure accuracy. |
| Fluorescent Probes (e.g., TaqMan) | oligonucleotides that bind to a specific sequence within the amplicon and emit fluorescence when cleaved, enabling real-time detection. | Provides superior specificity over intercalating dyes [47]. |
| Positive & Negative Controls | Validate the performance of the qPCR assay. Positive controls contain the target sequence, while negative controls (no-template) check for contamination. | Critical for ensuring result reliability and assay quality control. |
| Commercial Multiplex Panels | Integrated kits that allow simultaneous detection of multiple pathogens in a single reaction. | e.g., Biofire FilmArray Pneumonia Panel [48]; Sansure, GeneFinder, TaqPath for SARS-CoV-2 [49]. |
The evidence from recent clinical studies firmly establishes that qPCR offers significant advantages over culture-based methods in speed, sensitivity, and the ability to detect complex colonization patterns, particularly when using frozen samples. However, culture remains an indispensable tool for obtaining live isolates for antimicrobial susceptibility testing and epidemiological typing. The choice between these methods is not a matter of simple replacement but of strategic integration. Researchers and clinicians must align their selection with the specific requirements of the situation—opting for qPCR when speed, sensitivity, and high-throughput are paramount, and relying on culture when viability and phenotypic resistance data are critical. A combined approach often provides the most comprehensive diagnostic insight, driving forward both patient care and public health outcomes.
Next-generation sequencing (NGS) has revolutionized the field of infectious disease diagnostics and outbreak investigation. This guide provides an objective comparison of two primary NGS approaches—Metagenomic Next-Generation Sequencing (mNGS) and Whole-Genome Sequencing (WGS)—contrasting them with traditional culture-based methods. Designed for researchers and drug development professionals, it synthesizes current experimental data and implementation frameworks to inform strategic decisions in clinical and public health microbiology.
For over a century, culture-based techniques have formed the cornerstone of microbiological diagnosis. However, these methods present significant limitations for outbreak investigation, including prolonged turnaround times (often 24-72 hours), inability to detect non-culturable or fastidious organisms, and poor performance in polymicrobial infections [50]. Molecular methods like real-time PCR, while faster, are limited to detecting predefined targets, making them ineffective for discovering novel or unexpected pathogens [51].
The advent of next-generation sequencing has introduced powerful, high-resolution tools for outbreak detection and pathogen characterization. Whole-genome sequencing (WGS) provides complete genomic coverage of cultured isolates, enabling precise taxonomic classification, phylogenetic tracking of outbreaks, and comprehensive detection of antimicrobial resistance (AMR) determinants [50] [52]. In contrast, metagenomic next-generation sequencing (mNGS) enables culture-free, hypothesis-free detection of a broad array of pathogens directly from clinical specimens, making it particularly valuable for cases of unknown etiology or complex polymicrobial infections [50] [53].
Table 1: Core Characteristics of Diagnostic and Surveillance Methods
| Method | Principle | Typical Turnaround Time | Key Advantages | Major Limitations |
|---|---|---|---|---|
| Culture-Based | Growth of microorganisms on selective media | 24-72 hours | Gold standard for viability; enables antimicrobial susceptibility testing | Prolonged TAT; cannot detect non-culturable organisms; subjective interpretation [41] [3] |
| Targeted PCR | Amplification of predefined pathogen sequences | 2-6 hours | Rapid; high sensitivity for targeted pathogens | Limited to known targets; cannot detect novel pathogens [51] |
| Whole-Genome Sequencing (WGS) | Comprehensive sequencing of cultured isolates | 2-5 days (including culture) | High-resolution strain typing; detects AMR genes and virulence factors; excellent for outbreak tracing | Requires pure culture; longer TAT than molecular methods [52] [54] |
| Metagenomic NGS (mNGS) | Sequencing all nucleic acids in a sample | 1-3 days | Culture-independent; detects unexpected, novel, or mixed infections; hypothesis-free | Host DNA interference; complex bioinformatics; higher cost per sample [50] [53] |
Performance Comparison: Quantitative Data from Real-World Studies
Diagnostic Sensitivity and Specificity
Multiple studies have directly compared the performance of molecular methods (including NGS approaches) against traditional culture. In a year-long comparative study of carbapenemase-producing Gram-negative bacilli detection, direct molecular testing (Xpert Carba-R assay) demonstrated 90.2% sensitivity, significantly outperforming the culture-based strategy which showed 46.3% sensitivity when non-fermenting Gram-negative bacilli were disregarded, and 64.8% when they were included [3].
For wound infection diagnostics, a comparative evaluation of real-time PCR and culture found that PCR detected 110 clinically significant pathogens that were missed or ambiguously reported (approximately 30%) by culture. Latent class analysis estimated PCR sensitivity at 95.6% and specificity at 91.0%, underscoring the limitations of culture in resolving polymicrobial infections [41].
Impact on Outbreak Detection and Public Health Response
The implementation of WGS for surveillance of Shiga toxin-producing Escherichia coli (STEC) in France has demonstrated remarkable effectiveness. Over a 5-year period (2018-2022), sequencing of 1,002 isolates enabled high-resolution cluster detection using core-genome multilocus sequence typing (cgMLST) with hierarchical clustering, providing statistically validated thresholds for outbreak determination that varied by serotype (5-16 allelic differences) [54].
A paradigm-shifting study at a University of Pittsburgh Medical Center affiliate hospital implemented prospective real-time WGS surveillance, sequencing isolates weekly to proactively identify outbreaks. Over two years, this system identified 172 outbreaks ranging from 2-16 patients, with 12.1% of 3,921 healthcare-associated isolates linked to outbreaks. Crucially, when infection prevention and control teams intervened based on sequencing alerts, they stopped further transmission in 95.6% of outbreaks, preventing an estimated 62 outbreaks and 5 deaths while saving approximately $700,000—a more than 3-fold return on investment [55].
Table 2: Comparison of NGS Approaches for Outbreak Investigation
| Parameter | Whole-Genome Sequencing (WGS) | Metagenomic NGS (mNGS) |
|---|---|---|
| Primary Application | High-resolution strain typing and outbreak tracing [52] [54] | Comprehensive pathogen detection in complex infections [50] |
| Specimen Requirement | Pure cultured isolates | Direct clinical specimens (CSF, blood, BAL, tissue) [50] |
| Pathogen Detection | Targeted to cultured organism | Unbiased detection of bacteria, viruses, fungi, parasites [53] |
| Turnaround Time | 2-5 days (including culture step) | 1-3 days (culture-independent) [50] |
| Sensitivity Limitations | Dependent on culture growth | Limited by host DNA background; requires depletion methods [50] [56] |
| Strain Resolution | Excellent for tracking transmission routes [54] | Variable; depends on sequencing depth and bioinformatics [50] |
| AMR Detection | Comprehensive resistome analysis [52] | Limited to detected resistance genes [50] |
| Key Advantage | Gold standard for epidemiological investigations [55] | Ideal for diagnostically challenging cases [50] |
Experimental Protocols and Methodologies
Whole-Genome Sequencing for Outbreak Surveillance
The French STEC surveillance program provides a robust protocol for WGS implementation in public health [54]:
Bacterial Isolation and DNA Extraction: Pure isolates are obtained from clinical specimens using standard culture methods. High-quality DNA is extracted using automated systems.
Library Preparation and Sequencing: Libraries are prepared using enzymatic fragmentation (e.g., Nextera transposition) and adapter ligation. Sequencing is performed on Illumina platforms (MiSeq, NextSeq) to achieve minimum 30x coverage.
Bioinformatic Analysis:
- Quality Control: Assessment of raw sequence quality using tools like FastQC
- Genome Assembly: De novo assembly using tools such as SPAdes or Velvet
- cgMLST Analysis: Using EnteroBase hierarchical clustering (HC5 threshold) for initial cluster detection
- SNP Analysis: Confirmatory single-nucleotide polymorphism analysis for outbreak confirmation
- Phylogenetic Analysis: Construction of transmission trees using maximum-likelihood methods
Epidemiologic Correlation: Integration of genomic data with patient metadata to confirm transmission routes.
Metagenomic NGS for Direct Pathogen Detection
The mNGS workflow for direct detection from clinical specimens involves [50] [53]:
Sample Processing and Nucleic Acid Extraction: Clinical specimens (CSF, blood, BAL) undergo mechanical bead-based lysis for comprehensive cell disruption. Total nucleic acid is extracted using commercial kits (e.g., MagMAX Microbiome Ultra).
Host DNA Depletion: Enzymatic or probe-based methods selectively deplete human DNA to enhance microbial signal.
Library Preparation: Fragmentation and adapter ligation with unique molecular barcodes for sample multiplexing.
Sequencing: Typically performed on Illumina platforms (150bp paired-end reads) with appropriate controls.
Bioinformatic Analysis:
- Quality Filtering: Removal of low-quality reads and adapters
- Host Read Subtraction: Alignment to human reference genome (hg38)
- Taxonomic Classification: Comparison to microbial databases using tools like Kraken2 or IDSeq
- Assembly and Binning: For high-complexity samples, contig assembly and metagenomic binning using tools like COMEBin or MetaBAT2 [56]
Benchmarking Metagenomic Binning Tools
Recovering metagenome-assembled genomes (MAGs) from complex samples requires sophisticated binning tools. A comprehensive benchmark of 13 metagenomic binning tools across different data types revealed that:
- Multi-sample binning outperforms single-sample and co-assembly approaches across short-read, long-read, and hybrid data, recovering up to 125% more moderate-quality MAGs in marine samples [56]
- COMEBin and MetaBinner ranked as top performers across multiple data-binning combinations
- MetaWRAP demonstrated the best overall performance for bin refinement, recovering the highest number of high-quality MAGs [56]
Table 3: Performance of Metagenomic Binning Tools Across Data Types
| Binning Tool | Short-Read Data | Long-Read Data | Hybrid Data | Key Algorithm |
|---|---|---|---|---|
| COMEBin | Excellent | Excellent | Excellent | Contrastive learning with data augmentation [56] |
| MetaBinner | Excellent | Good | Good | Ensemble algorithm with multiple features [56] |
| VAMB | Good | Good | Good | Variational autoencoders [56] |
| MetaBAT 2 | Good | Fair | Good | Tetranucleotide frequency + coverage [56] |
| Binny | Good (co-assembly) | Fair | Fair | Multiple k-mer + HDBSCAN clustering [56] |
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 4: Key Research Reagent Solutions for NGS-Based Outbreak Investigation
| Reagent/Category | Function | Example Products | Application Notes |
|---|---|---|---|
| Nucleic Acid Extraction Kits | Isolation of high-quality DNA/RNA from diverse sample types | MagMAX Microbiome Ultra, QIAamp DNA Microbiome | Bead-based mechanical lysis improves recovery from Gram-positive organisms [41] |
| Host Depletion Reagents | Selective removal of human DNA to enhance microbial signal | NEBNext Microbiome DNA Enrichment, QIAseq Hybridase | Critical for low-biomass samples; enzymatic vs. probe-based approaches [50] |
| Library Preparation Kits | Fragmentation, adapter ligation, and amplification for sequencing | Illumina DNA Prep, Nextera XT, Swift Accel | Enzymatic fragmentation reduces hands-on time vs. mechanical shearing [52] |
| Sequencing Platforms | High-throughput DNA sequencing | Illumina NovaSeq, MiSeq; Oxford Nanopore GridION | Short-read for accuracy; long-read for assembly completeness [50] [51] |
| Bioinformatics Tools | Taxonomic classification, assembly, and phylogenetic analysis | IDSeq, PathoScope, One Codex, EnteroBase | Cloud-based platforms improve accessibility for non-bioinformaticians [50] |
| Quality Control Standards | Monitoring extraction efficiency, contamination, and sensitivity | Artificial mock communities, internal control spikes | Essential for validating entire workflow and comparing across laboratories [52] |
| Iodoacetamido-PEG3-NHS ester | Iodoacetamido-PEG3-NHS ester, MF:C15H23IN2O8, MW:486.26 g/mol | Chemical Reagent | Bench Chemicals |
| 6-Azidohexanoic Acid STP Ester | 6-Azidohexanoic Acid STP Ester, MF:C12H10F4N3NaO5S, MW:407.28 g/mol | Chemical Reagent | Bench Chemicals |
The evidence demonstrates that next-generation sequencing technologies, particularly WGS and mNGS, provide transformative capabilities for outbreak investigation that surpass traditional culture-based methods. WGS offers unparalleled resolution for tracking transmission pathways and understanding outbreak dynamics, while mNGS enables comprehensive pathogen detection in diagnostically challenging cases. The integration of these approaches into public health surveillance systems, as demonstrated by programs in France and the United States, represents a paradigm shift toward more precise, proactive outbreak detection and containment.
As sequencing technologies continue to evolve with improvements in cost, portability, and analytical frameworks, their implementation will likely expand beyond reference laboratories to become essential tools for hospital infection prevention and public health response teams worldwide. The future of outbreak investigation lies in the strategic combination of these genomic approaches with traditional methods, creating integrated systems that leverage the unique strengths of each technology to protect public health.
The rapid and accurate identification of pathogens is a cornerstone of effective clinical management of infectious diseases, impacting patient outcomes and antimicrobial stewardship [57] [48]. Traditional, culture-based diagnostic methods, while considered a historical gold standard, are often limited by lengthy turnaround times, typically requiring 48 to 72 hours to yield results [48] [58]. This delay can lead to empirical antibiotic use, which contributes to mortality and the global rise of antimicrobial resistance [48] [58]. The field of microbial diagnostics has therefore been evolving towards novel platforms that offer greater speed, accuracy, and automation.
Among these, Matrix-Assisted Laser Desorption/Ionization Time-of-Flight Mass Spectrometry (MALDI-TOF MS) has revolutionized culture-based identification, allowing for rapid, cost-effective microbial analysis once a colony is isolated [57] [59]. Concurrently, molecular techniques, particularly those leveraging Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR), have emerged as powerful tools for detecting pathogen-specific nucleic acids with high specificity and speed, sometimes bypassing the need for culture altogether [60] [61]. The integration of automation throughout these workflows further enhances reproducibility, throughput, and efficiency [58] [62]. This guide provides a comparative analysis of these novel platforms, framing them within the ongoing research comparing culture-based and molecular methods, and provides supporting experimental data and methodologies for researchers and drug development professionals.
The following table summarizes the core principles, strengths, and limitations of MALDI-TOF MS and CRISPR-based assays.
Table 1: Core Characteristics of Novel Diagnostic Platforms
| Feature | MALDI-TOF MS | CRISPR-Based Assays |
|---|---|---|
| Detection Target | Proteomic profile (primarily ribosomal proteins) [59] | Pathogen-specific nucleic acid sequences (DNA or RNA) [60] [61] |
| Principle | Ionized proteins are separated by mass-to-charge (m/z) ratio to generate a unique fingerprint [59] | Cas enzymes (e.g., Cas12, Cas13) are guided to cleave target sequences, activating collateral cleavage of reporter molecules [60] [61] |
| Typical Turnaround Time | Minutes after colony isolation [59] | ~60 minutes from sample to result [60] |
| Key Strength | Rapid, low-cost, high-throughput identification from culture [57] [59] | Ultra-specific, rapid detection; potential for isothermal amplification and point-of-care use [60] [61] |
| Key Limitation | Generally requires pure culture, limited direct specimen testing [59] | Can require nucleic acid extraction and pre-amplification; risk of amplicon contamination [60] |
The Role of Automated Systems
Automation is a critical enforcer for both MALDI-TOF MS and molecular techniques. In MALDI-TOF MS, automated sample preparation systems, such as the Aurora VERSA workstation, standardize the previously manual and variable processes of matrix application, analyte mixing, and target spotting [62]. This automation significantly improves reproducibility and data quality while enabling high-throughput analysis [62]. Similarly, automated machine learning (AutoML) platforms can rapidly process and identify complex patterns within mass spectra, enhancing diagnostic accuracy without the need for extensive manual data science expertise [63]. For molecular diagnostics and antibiotic susceptibility testing (AST), emerging microtechnologies and automated systems aim to integrate sample processing, fluid handling, and detection into streamlined, lab-on-a-chip devices, potentially accelerating the entire diagnostic pipeline [58].
Performance Comparison: Supporting Data
Recent head-to-head studies provide robust quantitative data on the performance of different platforms.
Comparative Performance of MALDI-TOF MS Systems
A 2023 study directly compared three MALDI-TOF MS systems—Bruker MALDI Biotyper, bioMérieux Vitek MS, and Zybio EXS2600—using a collection of 356 difficult-to-identify bacterial isolates, with 16S rRNA gene sequencing as a reference [57].
Table 2: Head-to-Head Comparison of Three MALDI-TOF MS Systems [57]
| System | Valid Results Achieved | Agreement with Sequencing (All Valid Results) | Misidentification Rate (Single-Species Level) |
|---|---|---|---|
| Bruker MALDI Biotyper | 98.6% | 98.9% | 0% |
| Zybio EXS2600 | 94.4% | 98.5% | 2.6% |
| bioMérieux Vitek MS | 93.3% | 99.7% | 1.1% |
The study concluded that despite minor performance differences, all three systems provided comparable results and were suitable for medical diagnostic laboratories [57].
Expanding Functionality: Resistance Detection by MALDI-TOF MS
MALDI-TOF MS's utility extends beyond identification to functional phenotypic assays, such as detecting carbapenemase activity. A 2024 study compared the Bruker MBT STAR-Carba IVD Kit with Zybio's Carbapenemase Activity Kit using 40 carbapenem-resistant Enterobacterales (CRE) isolates [64].
Table 3: Comparison of MALDI-TOF MS-Based Carbapenemase Detection Assays [64]
| Parameter | Bruker MBT STAR-Carba | Zybio Carbapenemase Activity Kit |
|---|---|---|
| Valid Results Obtained | 93% (37/40) | 85% (34/40) |
| Sensitivity | 92% (24/26) | 96% (25/26) |
| Specificity | 91% (10/11) | 64% (7/11) |
| Positive Predictive Value (PPV) | 96% | 85% |
| Negative Predictive Value (NPV) | 83% | 88% |
The study found that while the Zybio assay demonstrated high sensitivity, the Bruker system provided greater specificity and fewer false-positive results [64].
CRISPR-Based Assays for Targeted Pathogen Detection
CRISPR assays show exceptional specificity for targeted pathogen detection. A 2022 study developed a "CRISPR-top" assay for Klebsiella pneumoniae detection, integrating loop-mediated isothermal amplification (LAMP) with CRISPR/Cas12b detection in a one-pot reaction at 56°C [60]. The key performance metrics were:
- Specificity: 100% - correctly identified all 64 K. pneumoniae clinical isolates and 41 non-K. pneumoniae strains [60].
- Sensitivity: 96% (24/25) in clinical sputum samples, compared to 100% (33/33) specificity [60].
- Limit of Detection (LOD): 1 pg of genomic DNA per reaction, which was 10-fold more sensitive than LAMP alone [60].
Detailed Experimental Protocols
To ensure reproducibility, detailed methodologies from key cited studies are outlined below.
Objective: To evaluate the performance of three MALDI-TOF MS systems for bacterial identification against 16S rRNA gene sequencing.
- Bacterial Strains: 356 pre-characterized isolates from human specimens, stored at -80°C, were subcultured onto fresh agar plates.
- Culture Conditions: Overnight culture on Columbia sheep blood agar or chocolate agar at 5% COâ‚‚ for fastidious organisms, or on Schaedler agar in anaerobic conditions for anaerobes.
- Sample Processing (Parallel): A single trained technician applied each isolate to the three different MALDI targets using corresponding reagents.
- First Attempt: Direct smear application from agar plate.
- Second Attempt: If no green result (species-level ID), repeat direct smear.
- Third Attempt: If the second attempt fails, apply formic acid extraction pretreatment according to manufacturers' protocols.
- Systems and Databases:
- Bruker MALDI Biotyper: MBT IVD Library Revision G (Claim 6) database.
- bioMérieux VITEK MS: Knowledge Base V3.2 database.
- Zybio EXS2600: V.1.0.0.0 database.
- Reference Method: 16S rRNA gene sequencing (NCBI GenBank), with ≥98% sequence identity considered a valid result.
Objective: To establish a one-pot, isothermal assay for rapid and accurate detection of K. pneumoniae.
- Target Gene: The capsular polysaccharide synthesis regulator gene, rcsA.
- Primer and Probe Design: Design LAMP primers (FIP, BIP, LF, F3, B3) and a crRNA guide specific to the rcsA gene.
- Reaction Optimization:
- Optimal Primer Mix: 0.53 µM each FIP/BIP, 0.27 µM LF, 0.13 µM each F3/B3.
- Optimal ssDNA Probe Concentration: 2 µM.
- Optimal Temperature: 56°C.
- One-Pot Assay Workflow:
- Combine extracted genomic DNA (or processed sample) with the LAMP primer mixture, Cas12b enzyme, crRNA, and fluorescent ssDNA reporter in a single tube.
- Incubate at 56°C for 60 minutes.
- Measure fluorescence in real-time or at endpoint.
- Specificity Testing: Test against a panel of 64 K. pneumoniae clinical isolates and 41 non-K. pneumoniae strains.
- Limit of Detection (LOD): Determine by testing 10-fold serial dilutions of K. pneumoniae genomic DNA.
Objective: To compare the performance of Bruker STAR-Carba and Zybio Carbapenemase Activity kits for detecting carbapenemase activity in CRE isolates.
- Bacterial Isolates: 40 consecutive, non-duplicate CRE isolates from clinical specimens.
- Reference Testing: Carbapenemase status confirmed by a combination of methods (e.g., PCR for resistance genes, immunologic assays, phenotypic tests).
- Bruker MBT STAR-Carba Protocol:
- Inoculate a loopful of bacteria into the provided incubation buffer containing meropenem.
- Incubate at 37°C for 30 minutes ± 15 minutes.
- Stop the reaction and centrifuge.
- Spot the supernatant onto a Bruker target plate, overlay with matrix, and analyze with the Microflex LT MALDI-TOF MS.
- Software automatically interprets the spectrum for meropenem degradation.
- Zybio Carbapenemase Activity Kit Protocol:
- Prepare a high-concentration bacterial suspension.
- Mix the suspension with the provided imipenem solution.
- Incubate at 35°C for 1 hour.
- After incubation, acidify the solution, centrifuge, and spot the supernatant onto a Zybio target plate.
- Analyze using the EXS2600 MS and its dedicated software.
- Data Analysis: Results classified as "Carbapenemase Positive," "Carbapenemase Negative," or "No Result." Performance calculated against the reference method.
Workflow Visualization
The diagram below illustrates the general workflows for MALDI-TOF MS and CRISPR-based assays, highlighting key steps and decision points.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Reagents and Materials for Featured Platforms
| Item | Function / Application | Example from Search Results |
|---|---|---|
| MALDI Matrix (e.g., HCCA) | Absorbs laser energy and facilitates soft ionization of analyte proteins [59]. | α-cyano-4-hydroxycinnamic acid (HCCA) [59] |
| Formic Acid / Acetonitrile | Solvent for protein extraction; enhances protein release for robust or encapsulated microbes [57] [59]. | Formic acid extraction protocol [57] |
| Reference Spectral Databases | Library of known microbial protein spectra for comparative identification [57] [59]. | MBT IVD Library (Bruker), Vitek MS Knowledge Base (bioMérieux) [57] |
| Cas Enzymes (Cas12b, Cas13, etc.) | Core effector proteins in CRISPR assays; provide target-specific binding and collateral cleavage activity [60] [61]. | Cas12b used in CRISPR-top assay [60] |
| Guide RNA (crRNA) | Directs the Cas enzyme to the specific target nucleic acid sequence [61]. | crRNA designed for the rcsA gene [60] |
| Fluorescent ssDNA Reporter | Molecule cleaved collateral by activated Cas enzymes; its cleavage generates a detectable fluorescent signal [60]. | ssDNA fluorescence probe used in CRISPR-top [60] |
| LAMP Primer Sets | Enables isothermal amplification of target DNA, increasing sensitivity for CRISPR detection [60]. | Primers for FIP, BIP, LF, F3, B3 targeting rcsA [60] |
| Automated Sample Prep System | Standardizes and accelerates sample preparation for MALDI-TOF MS, improving reproducibility [62]. | Aurora VERSA workstation [62] |
| Fmoc-Lys(Boc)-PAB-PNP | Fmoc-Lys(Boc)-PAB-PNP, MF:C40H42N4O10, MW:738.8 g/mol | Chemical Reagent |
| threo-Guaiacylglycerol-beta-O-4'-dehydrodisinapyl ether | threo-Guaiacylglycerol-beta-O-4'-dehydrodisinapyl ether, MF:C31H36O11, MW:584.6 g/mol | Chemical Reagent |
The diagnostic landscape is being reshaped by platforms like MALDI-TOF MS and CRISPR-based assays, each offering distinct advantages. MALDI-TOF MS provides an unparalleled, cost-effective solution for high-throughput, rapid identification of cultured isolates and is expanding into functional resistance testing [57] [59] [64]. In contrast, CRISPR-based assays offer exceptional specificity and the potential for rapid, direct detection of pathogens from samples, potentially reducing dependency on culture [60] [61]. The integration of automation and machine learning across these platforms further enhances their robustness, reproducibility, and clinical utility [58] [63] [62].
The choice between these technologies—or their complementary use—depends on the clinical or research context, including required turnaround time, the need for phenotypic information versus sheer detection speed, and available resources. As these technologies continue to mature and integrate, they hold the collective promise of a future with faster, more precise infectious disease diagnostics, ultimately leading to improved patient outcomes and strengthened antimicrobial stewardship.
The accurate and timely identification of pathogens is a cornerstone of effective clinical management for infectious diseases. For decades, culture-based methods have served as the gold standard in microbiology laboratories, providing vital information for diagnosis and treatment. However, the emergence of sophisticated molecular diagnostics is fundamentally changing the landscape of microbial identification. This guide provides a comparative analysis of these methodologies across three critical clinical applications, presenting objective performance data to inform researchers, scientists, and drug development professionals.
Comparative Performance Data Across Clinical Applications
The following table summarizes key quantitative findings from studies that directly compared culture-based and molecular methods in different clinical contexts.
Table 1: Comparative Performance of Culture vs. Molecular Methods in Clinical Applications
| Clinical Application | Method Category | Key Performance Findings | Pathogens/Species Identified | Reference |
|---|---|---|---|---|
| Necrotizing Soft Tissue Infections (NSTIs) | Culture | Pathogens identified in 70% of surgical samples. | Standard aerobic and anaerobic bacteria. | [35] |
| Multi-Molecular Panel (16S clone libraries, Ibis T5000, 454 pyrosequencing) | Pathogens identified in 90% of samples; frequently detected additional microorganisms compared to culture. | Streptococcus pyogenes, Acinetobacter baumannii, Streptococcus pneumoniae, fungi, mycoplasma, Fusobacterium necrophorum. | [35] | |
| Chronic Wounds | Aerobic Culture | 17 different bacterial taxa identified. | Common aerobic bacteria. | [65] |
| Molecular (16S rDNA sequencing) | 338 different bacterial taxa identified; the majority of bacteria found molecularly were not identified by culture. | Extensive polymicrobial communities, including fastidious and anaerobic bacteria. | [65] | |
| Urinary Tract Infections (UTIs) | Conventional Urine Culture | Sensitivity of ~60% for detecting acute UTI; selects for fast-growing, mainly aerobic bacteria. | E. coli, Enterococcus, Staphylococcus species. | [66] |
| Next-Generation Sequencing (NGS) | Significantly higher sensitivity in identifying urinary bacteria; greater species diversity per sample. | Diverse range of bacteria, including slow-growing, anaerobic, and fastidious organisms. | [66] |
Detailed Experimental Protocols
To ensure reproducibility and provide insight into experimental design, this section details the methodologies from key cited studies.
Protocol for Molecular Analysis of NSTIs
This protocol is derived from a study analyzing tissue samples from patients with NSTIs [35].
- Sample Collection and Preparation: Tissue samples are obtained during surgical debridement. Each sample is divided into three aliquots for standard culture, molecular analyses, and optional FISH experiments. The aliquot for molecular analysis is transferred to a tube containing glycerol and stored frozen until processing.
- DNA Extraction: Bacterial lysis is achieved using a mechanical tissue homogenizer (e.g., Qiagen TissueLyser) with a mixture of steel and glass beads in RLT buffer. DNA is then purified from the lysate using a commercial kit (e.g., QIAamp DNA Mini Kit) according to the manufacturer's tissue protocol. The extracted DNA is eluted in water and diluted to a standardized concentration (e.g., 20 ng/μL).
- Molecular Identification (Multi-Method Approach):
- Clone Library Construction & Sanger Sequencing: Near full-length 16S rRNA genes are amplified via PCR, cloned into a vector, and transformed into bacteria. Multiple colonies are picked and Sanger sequenced to identify the microbial diversity present.
- Pyrosequencing (e.g., 454-based): A hypervariable region of the 16S rRNA gene (e.g., V1-V3) is amplified with barcoded primers. The amplicons are pooled and sequenced en masse, providing thousands of sequences per sample for a deep diversity profile.
- Quantitative PCR (qPCR): Species-specific primers and probes (e.g., for Streptococcus pyogenes) are used to quantify the bacterial load in the sample using a real-time PCR system.
- Data Analysis: Sequence data from cloning and pyrosequencing are processed to remove low-quality reads, then compared against reference databases (e.g., GenBank) for taxonomic assignment. qPCR data are analyzed based on standard curves to determine absolute quantification.
Protocol for Bacterial Tag-Encoded FLX-Titanium Amplicon Pyrosequencing (bTEFAP) of Chronic Wounds
This protocol details the method used for high-throughput microbial identification in chronic wound specimens [65].
- Sample Collection: Debridement samples are collected from chronic wounds during standard-of-care management and transported to the laboratory.
- DNA Extraction: Samples are centrifuged, and the pellet is suspended in RLT buffer with β-mercaptoethanol. Complete lysis is performed using a TissueLyser with steel and glass beads. DNA is recovered from the supernatant using a spin-column-based kit (e.g., QIAamp DNA Mini Kit) and eluted in nuclease-free water.
- Partial Ribosomal Amplification: A ~500 bp region of the 16S rRNA gene is amplified using modified universal bacterial primers (28F and 519R). The forward primer includes linker A and a unique 8-base barcode for each sample; the reverse primer is biotinylated. PCR is performed with a hot-start Taq master mix under the following conditions: 95°C for 5 min; 35 cycles of 95°C for 30s, 54°C for 40s, and 72°C for 1min; final elongation at 72°C for 10 min.
- Amplicon Pooling and Cleaning: The PCR products are purified using a magnetic bead-based clean-up system (e.g., Agencourt Ampure Beads) to remove short fragments and primers. Barcoded amplicons from multiple samples are then pooled in equimolar ratios.
- Massively Parallel Pyrosequencing: The pooled amplicon library is sequenced on a high-throughput platform (e.g., Roche FLX Titanium) according to the manufacturer's specifications.
- Bioinformatic Analysis: Post-run, sequences are de-multiplexed based on their barcodes. Quality-filtered sequences are clustered into operational taxonomic units (OTUs) and classified taxonomically by alignment with curated databases.
Visualization of Method Workflows
The following diagram illustrates the core workflows for culture-based and molecular methods, highlighting key differences in process and output.
The Scientist's Toolkit: Essential Research Reagents & Materials
Successful execution of the described molecular protocols requires a suite of specialized reagents and instruments.
Table 2: Key Research Reagent Solutions for Molecular Microbial Identification
| Item | Function/Application | Specific Examples/Notes |
|---|---|---|
| Nucleic Acid Extraction Kit | Purification of DNA/RNA from complex clinical samples. | QIAamp DNA Mini Kit; mechanical lysis with beads (e.g., from Qiagen) is often critical for complete cell disruption in tissues. |
| PCR Enzymes & Master Mix | Amplification of target genetic markers (e.g., 16S rRNA gene). | HotStarTaq Plus Master Mix Kit; chosen for high fidelity and performance with complex templates. |
| Primer Sets | Target-specific amplification for sequencing or qPCR. | Universal 16S primers (e.g., 28F/519R); species-specific primers/probes for qPCR (e.g., for S. pyogenes). |
| Sequencing Kit & Platform | Generation of sequence data for identification. | 454 GS FLX Titanium kits & sequencer; Illumina MiSeq kits & sequencer for NGS. |
| Bioinformatics Software | Analysis of raw sequence data: quality control, taxonomic assignment, diversity analysis. | QIIME, MOTHUR; used for processing 16S amplicon data and comparing against databases like Greengenes or SILVA. |
| Gastrin I (1-14), human | Gastrin I (1-14), human, MF:C79H100N16O27, MW:1705.7 g/mol | Chemical Reagent |
| Cytidine-1',2',3',4',5'-13C5 | Cytidine-1',2',3',4',5'-13C5, MF:C9H13N3O5, MW:248.18 g/mol | Chemical Reagent |
Antimicrobial Resistance (AMR) Surveillance
The global challenge of AMR necessitates robust surveillance systems. While traditional surveillance has relied on phenotypic AST of cultured isolates, molecular methods are increasingly critical.
- Phenotypic Surveillance (Culture-Based): This method, used by systems like the WHO GLASS, tests bacterial isolates against a panel of antibiotics to determine minimum inhibitory concentrations (MICs) and categorize them as susceptible, intermediate, or resistant. It provides a direct measure of resistance but is slow and misses underlying genetic mechanisms [67].
- Genotypic Surveillance (Molecular): Techniques like PCR and Whole Genome Sequencing (WGS) directly detect resistance genes (e.g., mecA, bla genes) and mutations. WGS, in particular, offers a comprehensive view of the "resistome" and can predict resistance phenotypes while also providing isolate typing data for outbreak investigation. A key limitation is that not all genotypic resistance is consistently expressed [68] [69].
The integration of both phenotypic and genotypic data provides the most powerful approach for understanding and tracking the spread of AMR on a global scale [67].
Operational Challenges and Strategic Optimization for Diagnostic Laboratories
This guide provides an objective comparison between culture-based and molecular diagnostic methods, focusing on the critical bottlenecks of cost, turnaround time, and technical expertise. Based on current experimental studies, we present performance data and detailed methodologies to inform research and development decisions.
Performance Comparison: Culture-Based vs. Molecular Methods
The following tables summarize key quantitative comparisons between culture-based and molecular methods from recent, direct comparative studies.
Table 1: Overall Performance and Workflow Metrics
| Performance Metric | Culture-Based Method (with NFGNB inclusion) [3] | Direct Molecular Testing (Xpert Carba-R) [3] | Multiplex Real-Time PCR (Allplex Entero-DR) [2] |
|---|---|---|---|
| Sensitivity | 64.8% | 90.2% | 100% (Negative Predictive Value) |
| Average Hands-on Time | 89.97 minutes | 1.3 minutes | Not Specified |
| Total Workflow Time (TAT) | ≥48 hours [2] | ~1.5 hours (90 minutes) [3] | ~4 hours (Extraction: 2h 45min; Amplification: 1h 15min) [2] |
| Detection of Non-fermenting Gram-negative Bacilli (NFGNB) | Requires specific inclusion and separate workflow | Routine, on-panel detection | Capable for Pseudomonas and Acinetobacter spp. |
Table 2: Financial and Operational Considerations
| Consideration | Culture-Based Methods | Molecular Methods |
|---|---|---|
| Equipment & Reagent Costs | Generally lower per test. Costs accumulate from various media, reagents, and identification kits. | Higher initial instrument investment and cost per test for proprietary cartridges/kits [70] [71]. |
| Laboratory Infrastructure | Requires standard microbiology lab equipment (incubators, biosafety cabinets). | Requires dedicated molecular biology infrastructure (PCR workstations, real-time PCR machines) [72] [71]. |
| Technical Expertise Required | Expertise in microbiology (culture interpretation, biochemical testing). | Expertise in molecular biology (nucleic acid extraction, PCR principles, result interpretation) [70]. |
| Throughput & Automation | Low to medium. Many steps are manual, limiting scalability. | Medium to high. Platforms offer high levels of automation, enabling batch processing and walk-away operation [73]. |
Detailed Experimental Protocols from Cited Studies
This protocol outlines the methods for a large-scale, head-to-head comparison of culture-based and molecular testing for carbapenemase-producing Gram-negative bacilli (CPGNB).
1. Sample Collection and Preparation:
- Sample Type: Rectal swab samples were obtained from patients.
- Duration: The study was conducted over a year (April 2019 to March 2020).
- Scale: 29,446 samples from 17,097 unique patients were tested.
2. Culture-Based Method (Comparator):
- Primary Culture: Samples were inoculated onto chromID CARBA SMART chromogenic agar.
- Incubation: Agar plates were incubated aerobically at 35–37°C for 18–24 hours.
- Confirmation: Presumptive positive colonies were subjected to identification and confirmation via conventional polymerase chain reaction (PCR) for carbapenemase genes.
- Expanded Analysis: In a sub-analysis, non-fermenting Gram-negative bacilli (NFGNB) isolated on culture were also identified and underwent whole-genome sequencing to detect carbapenemase genes.
3. Direct Molecular Method (Intervention):
- Technology: The Cepheid Xpert Carba-R assay was used.
- Process: This is a fully integrated, automated platform that performs sample lysis, nucleic acid extraction, amplification, and detection in a single, self-contained cartridge.
- Targets: The assay detects and differentiates between common carbapenemase gene families (e.g., KPC, NDM, VIM, IMP, OXA-48).
4. Data and Analysis Collected:
- Primary Outcome: Sensitivity of each method for detecting CPGNB.
- Secondary Outcomes: Hands-on time for laboratory personnel; number of patient contact precautions averted or generated by each testing strategy.
This protocol describes the methodology for evaluating a multiplex PCR assay against routine culture for detecting multi-drug resistant (MDR) pathogens directly from rectal swabs.
1. Sample Collection:
- Sample Type: Routinary rectal swabs collected in Cary-Blair transport medium.
- Source: Patients from high-risk hospital wards (Haematology, ICU, etc.).
- Study Period: Six-month evaluation (January–June 2024).
2. Culture-Based Method (Gold Standard):
- Inoculation: 10 µL of transport medium was inoculated onto two agar types:
- MacConkey Agar: Supplemented with meropenem (10 µg) and ceftazidime (30 µg) disks for ESBL and carbapenemase producer screening.
- Tryptone Soya Agar with Sheep Blood: Supplemented with a vancomycin (30 µg) disk for vancomycin-resistant enterococci screening.
- Incubation: Agar plates were incubated at 37°C overnight.
- Identification & AST: Grown colonies were identified by MALDI-TOF MS. Antimicrobial Susceptibility Testing (AST) was performed using VITEK AST cards or the Kirby-Bauer method, following EUCAST guidelines.
- Phenotypic Confirmatory Testing: Resistant isolates underwent supplementary testing:
- Gram-negatives: Cepheid Xpert Carba-R cartridges for carbapenemase genes.
- Gram-positives: Immunochromatographic test (RESIST CTX-M) for CTX-M enzyme.
- Inoculation: 10 µL of transport medium was inoculated onto two agar types:
3. Molecular Method (Evaluation):
- Technology: Allplex Entero-DR assay (Seegene) and Entero-DR Plus assay (Arrow Diagnostics) multiplex real-time PCR.
- Targets: The kits detect blaKPC, blaOXA-48, blaVIM, blaNDM, blaIMP, blaCTX-M, vanA, vanB genes, and identify Acinetobacter spp. and Pseudomonas spp.
- Workflow:
- Nucleic Acid Extraction: Automated extraction and PCR setup were performed using the Seegene STARlet system.
- Amplification & Detection: PCR amplification was carried out on a Bio-Rad CFX96 thermal cycler.
Workflow Visualization
The fundamental difference between the two methodologies is starkly evident in their workflows, as depicted below.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Kits for Antimicrobial Resistance Surveillance
| Research Reagent / Kit | Function / Application | Key Characteristics |
|---|---|---|
| chromID CARBA SMART Agar [3] | Selective chromogenic medium for culture-based detection of CPO. | Allows presumptive identification based on colony color. Faster than non-chromogenic media but still requires confirmation. |
| Xpert Carba-R Assay (Cepheid) [3] | Integrated, automated real-time PCR for direct detection of carbapenemase genes from specimens. | Detects KPC, NDM, VIM, IMP, OXA-48. Fully automated, minimal hands-on time. |
| Allplex Entero-DR Assay (Seegene) [2] | Multiplex real-time PCR for detection of ESBL, carbapenemase, and vancomycin resistance genes. | Detects a broad panel of targets (blaKPC, blaOXA-48, blaVIM, blaNDM, blaIMP, blaCTX-M, vanA/B). |
| BD MAX System [73] | Fully automated, walk-away platform for nucleic acid extraction, purification, amplification, and detection. | Can run manufacturer-developed tests and user-defined protocols. Shown to have high extraction efficiency. |
| MacConkey Agar with Antibiotic Disks [2] | Conventional culture medium for screening Gram-negative pathogens and preliminary resistance profiling. | Low-cost, versatile. Requires long incubation and subsequent confirmatory tests. |
The data demonstrates a clear trade-off between molecular and culture-based methods. Molecular methods (Xpert Carba-R, multiplex PCR) offer decisive advantages in turnaround time, sensitivity, and labor efficiency, making them superior for rapid screening and infection control. However, these benefits come at a higher per-test cost and require significant technical infrastructure. Conversely, culture-based methods remain the gold standard for providing live isolates essential for antimicrobial susceptibility testing and epidemiological studies, with lower reagent costs but substantially longer time-to-result and greater hands-on labor. The optimal choice depends on the specific research or clinical question, weighing the need for speed and efficiency against the requirement for isolate availability and overall budget constraints.
In the comparative analysis of culture-based versus molecular diagnostic methods, sample quality and handling constitute foundational pre-analytical variables that directly determine assay performance. While technological advancements continue to enhance detection capabilities, improper sample collection, transport, or processing can irrevocably compromise results regardless of methodological sophistication [74] [5]. For researchers selecting between culture and molecular approaches, understanding how sample-related factors distinctly influence each methodology is essential for experimental design validity. This guide systematically examines how sample characteristics differentially affect culture and molecular techniques, presents experimental data quantifying these impacts, and provides evidence-based protocols for optimizing sample handling to maximize accuracy across both methodologies.
Culture-based and molecular detection methods operate on fundamentally different principles, resulting in distinct sample requirements and vulnerabilities. Culture methods depend on microbial viability and the ability to proliferate under laboratory conditions, making them susceptible to antibiotics in samples, improper transport temperatures, and delays that reduce viability [5] [45]. Conversely, molecular methods like PCR detect genetic material regardless of viability, rendering them insensitive to these factors but vulnerable to PCR inhibitors and DNA degradation [45] [75].
Table 1: Fundamental Methodological Differences Affecting Sample Requirements
| Characteristic | Culture-Based Methods | Molecular Methods (PCR) |
|---|---|---|
| Detection Target | Viable, cultivable organisms | Pathogen-specific genetic material |
| Critical Sample Factors | Microbial viability, absence of antibiotics, appropriate transport conditions | Presence of PCR inhibitors, nucleic acid integrity |
| Speed | Slow (24-96 hours) [45] | Rapid (2-6 hours) [45] |
| Sensitivity to Prior Antibiotics | High (false negatives common) [5] | Low (detects non-viable pathogens) [45] |
| Quantification Capability | Semi-quantitative (CFU counts) | Quantitative (Ct values) [45] |
Key Sample Quality Factors: Experimental Evidence and Impact Assessment
Bacterial Load and Distribution Heterogeneity
The spatial distribution of microorganisms in samples significantly impacts detection probability, particularly for culture methods. Research on orthopaedic infections demonstrates that bacterial aggregation introduces substantial sampling variability, especially with low bacterial loads [74]. Mathematical modeling reveals that when bacteria form aggregates exceeding the detection threshold of individual samples, the probability of false-negative results increases dramatically despite increased sampling [74].
Table 2: Impact of Bacterial Aggregation on Detection Probability
| Aggregation Scenario | Recommended Specimen Number | Detection Probability | Clinical Implication |
|---|---|---|---|
| Low aggregation (single cells/small clusters) | 5 tissue specimens | High (>90%) [74] | Reliable detection with standardized sampling |
| High aggregation (large biofilms) | 5+ tissue specimens | Low (<50%) despite increased sampling [74] | Culture-negative infections likely; supplemental methods needed |
| Critical mitigation strategy | Tissue homogenization to disrupt aggregates | Increased surface area for detection [74] | Enhances both culture and molecular detection |
Sample Type and Collection Method
The inherent characteristics of different sample types present distinct challenges for culture versus molecular methods. Respiratory specimens exemplify these differences: culture requires careful handling to maintain fastidious organism viability, while molecular methods necessitate inhibitor removal for reliable amplification [45]. For Candida auris detection, rectal swabs transported in appropriate medium (eSwab) maintain both viability for culture and nucleic acid integrity for PCR, enabling parallel testing [76].
Time and Transport Conditions
Transport delays and temperature excursions differentially affect culture and molecular methods. Culture viability diminishes rapidly with time, particularly for fastidious organisms like Neisseria meningitidis, requiring rapid processing or specialized transport media [75]. Molecular methods are less affected by time delays for DNA targets but require immediate freezing for RNA detection. Experimental comparisons show that culture sensitivity for Candida auris decreases significantly with refrigeration delays, while PCR results remain stable for extended periods when properly preserved [76].
Experimental Protocols: Establishing Method Comparison
Protocol 1: Controlled Spiking Study for Sensitivity Determination
Objective: Compare limit of detection (LOD) between culture and molecular methods using controlled inocula [76].
Materials:
- Sterile rectal swabs in eSwab medium (Copan Diagnostics)
- Candida auris reference strains (9 strains representing 5 clades)
- CHROMagar Candida and CHROMagar Candida Plus (CHROMagar)
- Dulcitol 10% NaCl enrichment broth [76]
- Nucleic acid extraction system (MagNA Pure 96, Roche)
- qPCR reagents (SensiFast No-ROX, Meridian Bioscience)
- LC480-II qPCR platform (Roche)
Methodology:
- Standardize C. auris concentrations using cell counter (Cellometer)
- Spike swabs at concentrations of 10, 50, 100, and 150 CFU per inoculum
- Add mixtures of other Candida species to simulate co-colonization
- Process samples in parallel:
- Culture: Streak on chromogenic agars, incubate at 37°C/42°C
- Molecular: Extract DNA, run sodC-based and ctrA-based PCR assays
- Confirm identities using MALDI-TOF MS
- Calculate sensitivity and specificity for each method
Experimental Findings: This methodology demonstrated that qPCR on direct samples showed 100% sensitivity and specificity, while culture sensitivity decreased to 44% at lower concentrations (≤50 CFU) and in polymicrobial samples [76].
Protocol 2: Method Comparison for Asymptomatic Carriage Detection
Objective: Evaluate sodC-based PCR versus ctrA-based PCR and culture for Neisseria meningitidis detection in carriers [75].
Materials:
- Pharyngeal swabs in STGG medium (skim milk, tryptone, glucose, glycerol)
- Chocolate and Modified Thayer Martin agars (Oxoid)
- Biochemical test materials (oxidase, carbohydrate utilization)
- PCR reagents for sodC and ctrA targets
- Antimicrobial susceptibility testing materials
Methodology:
- Collect pharyngeal swabs from asymptomatic carriers
- Process for culture: inoculate selective media, identify isolates
- Perform parallel molecular testing:
- Extract DNA from swabs and isolates
- Run sodC-targeted and ctrA-targeted PCR assays
- Compare detection rates between methods
- Perform antimicrobial susceptibility testing on isolates
Experimental Findings: sodC-based PCR detected N. meningitidis in 76.6% of swabs versus 46.7% for ctrA-based PCR and significantly lower rates for culture, demonstrating the impact of genetic target selection and method choice on detection sensitivity [75].
Workflow Visualization: Sample Handling Impact
Sample Handling Workflow and Critical Factors
Mathematical Modeling: Bacterial Distribution Impact
Bacterial Distribution Impact on Detection
Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for Method Comparison Studies
| Reagent/Material | Function | Method Application | Considerations |
|---|---|---|---|
| eSwab medium (Copan) | Maintains viability and nucleic acid integrity | Dual-purpose for culture and molecular methods | Enables parallel testing from single sample [76] |
| CHROMagar Candida/Plus | Differential isolation of Candida species | Culture-based detection | Incubation temperature (37°C vs. 42°C) affects specificity [76] |
| Dulcitol 10% NaCl broth | Selective enrichment for C. auris | Culture enhancement | No significant added value observed in validation [76] |
| STGG medium | Stabilizer for bacterial viability | Longitudinal carriage studies | Maintains N. meningitidis viability [75] |
| sodC PCR assay | Targets Cu-Zn superoxide dismutase gene | Molecular detection | Superior to ctrA for carriage isolates (100% vs 67% detection) [75] |
| MagNA Pure 96 system (Roche) | Automated nucleic acid extraction | Molecular method preparation | Standardizes pre-analytical molecular processing [76] |
Sample quality and handling parameters directly determine the accuracy of both culture and molecular detection methods, though through different mechanisms. Culture methods remain indispensable for antimicrobial susceptibility testing but are vulnerable to pre-analytical factors affecting viability [45]. Molecular methods provide superior sensitivity and speed but require careful attention to inhibitor removal and genetic target selection [75]. The optimal diagnostic approach often involves strategic combination of both methodologies, leveraging their complementary strengths while mitigating their respective vulnerabilities through optimized sample handling protocols. For research applications, explicit reporting of sample quality metrics and handling protocols is essential for valid cross-study comparisons and methodological advancement.
The shift from traditional, culture-based microbiological methods to advanced molecular techniques represents a paradigm shift in diagnostic microbiology and drug development. While culture has been the cornerstone of pathogen identification for over a century, molecular methods now offer unprecedented speed, sensitivity, and comprehensive profiling capabilities. However, this transition introduces significant data management challenges, requiring sophisticated computational infrastructure to interpret complex molecular data and integrate it meaningfully with existing healthcare systems such as Electronic Health Records (EHRs). This guide provides an objective comparison of these methodologies, supported by recent experimental data, to inform researchers, scientists, and drug development professionals navigating this technological evolution.
Performance Comparison: Culture-Based vs. Molecular Methods
Direct comparative studies consistently demonstrate that molecular methods outperform traditional culture in several key metrics, particularly sensitivity and turnaround time, though they present different challenges in data interpretation and clinical integration.
Table 1: Overall Diagnostic Performance Metrics from Recent Comparative Studies
| Study & Method | Sensitivity | Specificity | Turnaround Time | Key Advantage |
|---|---|---|---|---|
| CPGNB Screening [3] | ||||
| ⋯ Xpert Carba-R (Molecular) | 90.2% | - | ~2 hours | Superior sensitivity for CPGNB |
| ⋯ Culture-Based (excluding NFGNB) | 46.3% | - | 24-48 hours | - |
| Podiatric Wound Infections [41] | ||||
| ⋯ Comprehensive PCR Panel | 98.3%* / 95.6% | 73.5%* / 91% | Hours | Comprehensive pathogen profile |
| ⋯ Traditional Culture | Reference | High (exact value NS) | 24-72 hours | Provides live isolates for AST |
| MDR Surveillance (Rectal Swabs) [2] | ||||
| ⋯ Allplex Entero-DR Assay (qPCR) | 100% (for on-panel targets) | - | ~4 hours | High NPV for excluding colonization |
| ⋯ Conventional Culture | Lower (exact value NS) | - | ≥48 hours | Allows antimicrobial susceptibility testing |
Conventional culture-referenced framework; *Latent Class Analysis (LCA) estimate; CPGNB: Carbapenemase-Producing Gram-Negative Bacilli; NFGNB: Non-Fermenting Gram-Negative Bacilli; NS: Not Specified; NPV: Negative Predictive Value.*
Molecular methods demonstrate a marked improvement in sensitivity, detecting a broader range of pathogens, including fastidious, anaerobic, or antibiotic-exposed organisms that often evade culture [35] [41]. The year-long CPGNB screening study of 29,446 samples concluded that direct molecular testing "demonstrated superior sensitivity" compared to the culture-based strategy [3]. Furthermore, molecular techniques drastically reduce the time-to-result (TTR) from days to hours, enabling more timely clinical decisions [3] [2].
A significant challenge for molecular methods, however, is data interpretation. PCR can detect DNA from non-viable organisms or background flora, potentially leading to false positives if not contextualized correctly [41]. Advanced statistical models that incorporate bacterial load (e.g., 16S rRNA Ct values), Gram stain morphology, and resistance gene co-detection are being developed to assign clinical relevance and improve specificity [41].
Detailed Experimental Protocols and Workflows
Protocol 1: Comparative Evaluation of PCR vs. Culture for Wound Infections
A 2025 study by Dehghani et al. provides a robust framework for a head-to-head comparison, using statistical models to address the lack of a perfect gold standard [41].
- Specimen Collection: Dual-swab specimens were collected from 93 clinical wound cases (e.g., diabetic foot ulcers, pressure ulcers, surgical sites). This approach minimized sampling bias for parallel testing.
- Culture-Based Testing: One swab was processed by a commercial reference laboratory using standard culture on MacConkey and blood agar plates. Isolates were identified using MALDI-TOF MS, and antimicrobial susceptibility testing (AST) was performed using VITEK cards or Kirby-Bauer methods.
- Molecular Testing (PCR): The second swab underwent nucleic acid extraction via mechanical bead-based lysis. Real-time PCR was performed using a nanoscale SmartChip system with TaqMan assays targeting a comprehensive panel of bacterial and fungal pathogens, as well as antibiotic resistance genes (ABR).
- Data Analysis and Diagnostic Classification:
- Conventional Framework: Performance was calculated using culture as the reference standard (True Positive: PCR and culture match; False Positive: PCR detects a pathogen missed by culture).
- Latent Class Analysis (LCA): A three-indicator model (PCR, culture, Gram stain) was used to estimate accuracy without assuming a perfect reference standard.
- Predictive Modeling: A logistic regression model used 16S rRNA Ct values and Gram stain morphology to calculate the infection probability for organisms detected only by PCR.
Protocol 2: Multiplex Real-Time PCR for MDR Pathogen Surveillance
A 2025 study evaluating the Allplex Entero-DR assay illustrates the protocol for high-throughput surveillance of multi-drug resistant (MDR) organisms [2].
- Specimen Collection: 300 routine rectal surveillance swabs were collected in Cary-Blair transport medium from high-risk hospital wards.
- Culture-Based Method (Reference): Swabs were inoculated onto selective agar plates (MacConkey agar with meropenem/ceftazidime disks for ESBL/carbapenemase producers; blood agar with vancomycin disks for VRE). After overnight incubation, suspected colonies were identified by MALDI-TOF MS, and AST was performed. The total TTR was at least 48 hours.
- Molecular Testing (qPCR): The study used the Seegene STARlet system for automated nucleic acid extraction and PCR setup. Multiplex qPCR amplification on the Bio-Rad CFX96 thermal cycler targeted genes for ESBL (blaCTX-M), carbapenemases (blaKPC, blaOXA-48, blaVIM, blaNDM, blaIMP), and vancomycin resistance (vanA, vanB). The total hands-on time was approximately 4 hours.
- Data Integration and Reporting: Results were anonymized and contextualized based on the patient's location. For instance, the detection of Acinetobacter spp. or Pseudomonas spp. without resistance markers was only routinely reported for intensive care patients due to the higher risk of subsequent infection.
Figure 1: A simplified workflow comparing the sequential steps of culture-based methods against the faster, parallel nature of molecular diagnostics. TAT: Turnaround Time; LCA: Latent Class Analysis.
The Scientist's Toolkit: Key Research Reagent Solutions
Selecting the appropriate reagents and platforms is critical for generating reliable, interpretable data in molecular diagnostics.
Table 2: Essential Research Reagents and Platforms for Molecular Testing
| Item / Platform | Function / Application | Key Characteristics |
|---|---|---|
| Nucleic Acid Extraction Kits (e.g., MagMAX Microbiome Ultra) | Isolation of DNA/RNA from complex clinical samples. | Effective for Gram-positive and Gram-negative bacteria; includes mechanical bead-beating for robust lysis [41]. |
| Multiplex qPCR Assays (e.g., Allplex Entero-DR, Cepheid Xpert Carba-R) | Simultaneous detection of multiple pathogens and/or resistance genes from a single sample. | Qualitative or semi-quantitative; high-throughput; some offer integrated extraction/amplification [3] [2]. |
| PCR Enzymes & Master Mixes (e.g., TaqMan assays) | Amplification of target DNA sequences during PCR. | High specificity and sensitivity; compatible with multiplexing and real-time detection platforms [41] [77]. |
| Automated Nucleic Acid Extractors (e.g., Seegene STARlet) | Standardizes and automates the nucleic acid extraction process. | Reduces hands-on time and variability, crucial for high-volume testing [2]. |
| Real-Time PCR Thermal Cyclers (e.g., Bio-Rad CFX96, SmartChip System) | Platforms that perform PCR amplification with fluorescent monitoring. | Enable real-time, quantitative analysis; high-throughput capabilities [41] [2]. |
Data Management and Integration Hurdles
The volume and complexity of data generated by molecular methods create significant bottlenecks that extend beyond the wet-lab workflow.
- Interoperability and EHR Integration: A primary challenge is the semantic misalignment between different healthcare data standards (e.g., HL7 FHIR, SNOMED CT), which complicates the exchange and interpretation of molecular results across health systems [78]. Without standardized interfaces, integrating complex pathogen genomic data or resistance gene profiles into structured EHR fields for clinical decision support remains difficult.
- Data Volume and Computational Demands: While techniques like qPCR generate more manageable data streams, next-generation sequencing (NGS) produces vast amounts of data, requiring sophisticated bioinformatics pipelines for analysis, storage, and management [77]. This shift places a burden on institutional computational resources and necessitates specialized expertise.
- Clinical Utility and Actionability: A significant hurdle is transforming raw molecular data into clinically actionable information. Detecting multiple pathogens or resistance genes in a sample does not always distinguish between active infection, colonization, or background noise [41]. Developing intelligent systems that incorporate contextual data (e.g., patient symptoms, immune status) is essential to guide appropriate therapy and avoid diagnostic ambiguity.
- Governance and Security: Molecular data, especially genomic information, is highly sensitive. Ensuring patient privacy, securing data against breaches, and establishing clear data governance and consent protocols are critical challenges that must be addressed within the healthcare data ecosystem [79] [78].
Figure 2: The data lifecycle from generation to clinical application, highlighting major integration hurdles and emerging solution frameworks. APIs: Application Programming Interfaces.
The evidence consistently shows that molecular methods offer significant advantages over culture-based techniques in diagnostic sensitivity, turnaround time, and the ability to comprehensively profile complex microbial communities. However, the adoption of these advanced techniques is not merely a laboratory upgrade; it represents a fundamental shift that demands a parallel evolution in data management capabilities. The true value of molecular data is only realized when it can be seamlessly integrated, accurately interpreted, and contextually presented within clinical workflows to inform patient care. Overcoming the hurdles of interoperability, data volume, clinical interpretation, and governance is therefore not an IT sidebar but a central challenge for researchers, clinicians, and drug developers aiming to leverage the full potential of molecular diagnostics in precision medicine. Future success will depend on collaborative efforts that bridge the gap between laboratory science, data science, and clinical practice.
The global laboratory landscape is undergoing a significant transformation driven by technological advancements and increasing data complexity. Within today's laboratories—whether pharmaceutical R&D centers, hospital clinical labs, or manufacturing quality control facilities—the volume and complexity of data have grown tremendously, creating an imperative for digital solutions [80]. Workflow automation, robotics, and Laboratory Information Management Systems (LIMS) have emerged as critical technologies that streamline operations, reduce errors, and enhance productivity. These solutions act as the digital backbone of the modern lab, handling everything from sample login and barcoding to test scheduling, results entry, quality control validation, and final report generation [80].
This transformation occurs within the broader context of "Industry 4.0" in the life sciences sector, a shift driven by technologies like artificial intelligence (AI), data analytics, and machine learning [81]. By 2025, approximately 80% of organizations are expected to adopt intelligent automation, recognizing its potential to boost productivity, increase performance, and reduce operating costs [82]. This guide provides an objective comparison of leading workflow solutions, framed within a thesis comparing traditional culture-based methods with advanced molecular techniques, to help researchers, scientists, and drug development professionals navigate this evolving landscape.
Comparative Analysis of Culture-Based vs. Molecular Methods
The choice between traditional culture-based methods and modern molecular techniques represents a fundamental decision point in laboratory workflow design. Recent experimental data highlights the distinct advantages and limitations of each approach, particularly in clinical diagnostics and surveillance applications.
Performance Comparison of Diagnostic Methods
A 2024 study comparing these methodologies for detecting multi-drug-resistant (MDR) pathogens directly from rectal swabs revealed significant differences in performance characteristics [2]. The research evaluated 300 rectal swabs from various hospital units, including Haematology, Intensive Care, and Emergency Room patients, using both culture-based methods and multiplex real-time PCR molecular kits (Allplex Entero-DR assay and Entero-DR Plus assay) [2].
Table 1: Performance Comparison of Culture-Based vs. Molecular Methods for MDR Pathogen Detection
| Performance Metric | Culture-Based Method | Molecular Method (Multiplex Real-Time PCR) |
|---|---|---|
| Time to Result (TTR) | ≥48 hours [2] | Approximately 4 hours [2] |
| Sensitivity | Lower; decreases depending on biological sample [2] | 100% for Allplex targets [2] |
| Negative Predictive Value (NPV) | Variable | 100% [2] |
| Ability to Detect Specific Resistance Genes | Limited; requires supplementary testing [2] | Direct detection of blaKPC, blaOXA-48, blaVIM, blaNDM, blaIMP, blaCTX-M, vanA, and vanB [2] |
| Identification of Double-Carbapenemase Genes | Challenging and time-consuming [2] | Effectively demonstrates diffusion [2] |
Experimental Protocol for Method Comparison
The referenced study followed a rigorous experimental protocol to ensure valid comparison [2]:
- Sample Collection: Rectal samples were collected using Copan Faecal Swab with liquid Cary-Blair medium.
- Parallel Processing: Each sample underwent simultaneous conventional culture-based and molecular workflows.
- Culture-Based Method: Inoculation onto MacConkey agar with meropenem/ceftazidime disks and blood agar with vancomycin disk. After overnight incubation, colonies were identified by MALDI-TOF MS and tested for antimicrobial susceptibility using VITEK AST cards or Kirby-Bauer method. Phenotypically resistant isolates required additional molecular or immunochromatographic tests for gene confirmation.
- Molecular Method: Automated nucleic acid extraction and PCR setup using Seegene STARlet, followed by amplification on Bio-Rad CFX96 thermal cycler using Allplex Entero-DR and Entero-DR Plus assay kits.
- Data Analysis: Results from both methods were anonymized and compiled for comparative analysis.
This experimental design underscores a critical trade-off: while culture remains the most reproducible technique that allows for colony identification and antimicrobial susceptibility testing, molecular methods provide dramatically faster results with superior sensitivity for specific genetic markers [2].
Laboratory Information Management Systems (LIMS): Core Platform for Integration
A Laboratory Information Management System (LIMS) serves as the central platform for integrating automation, data management, and compliance within modern laboratories. At its core, a LIMS handles sample management, workflow automation, data collection, and regulatory compliance for labs of all types [80].
Leading LIMS Vendors and Capabilities
The LIMS market includes a mix of established providers and innovative newcomers, each offering distinct strengths suited to different laboratory environments.
Table 2: Comparison of Leading Laboratory Information Management Systems (2025)
| LIMS Vendor | Key Features | Deployment Options | Strengths | Considerations |
|---|---|---|---|---|
| LabWare LIMS [80] | Highly configurable sample lifecycle management, robust instrument integration, built-in ELN/LES modules. | On-premises, Cloud, SaaS | Proven compliance track record (21 CFR Part 11, GLP); High scalability for large enterprises. | Complex implementation often requiring consultants; Higher cost structure. |
| LabVantage LIMS [80] [83] | Fully web-based platform, integrated biobanking module, optional ELN and LES. | On-premises, Cloud | Modern user interface; Strong in pharmaceutical R&D and biobanking. | Can be resource-intensive to update. |
| STARLIMS [83] | Sample lifecycle tracking, quality control, regulatory compliance for FDA/ISO standards. | Information Not Specified | Long-standing reliability in clinical and public-health labs. | Can be rigid and less flexible. |
| Thermo Fisher SampleManager LIMS [83] | Tight integration with Thermo instruments, environmental monitoring, equipment calibration. | Information Not Specified | Robust, enterprise-grade solution for process automation. | Less flexible in multi-vendor environments. |
| Scispot [83] | Unified, API-first platform (LIMS, ELN, SDMS), AI-ready, customizable workflows without coding. | Cloud-native, SaaS | High interoperability and agility; Modern, AI-centric design. | Less established track record for large, regulated enterprises. |
LIMS in the Context of Method Selection
The choice of a LIMS significantly influences how efficiently a lab can leverage both culture-based and molecular methods. Modern LIMS facilitate standardized procedures and enforce Good Laboratory Practices (GLP), which is crucial for maintaining data integrity regardless of the diagnostic method used [80]. Furthermore, they provide the instrument integration capabilities necessary for automatically capturing results from both traditional automated culture systems and modern PCR platforms, thereby reducing manual errors and improving traceability [80]. In regulated sectors, a LIMS plays a critical role in meeting compliance standards such as FDA 21 CFR Part 11 for electronic records and ISO/IEC 17025, which is essential for labs validating new molecular methods alongside traditional techniques [80].
Automation and Robotics: Enhancing Efficiency and Connectivity
Automation in the laboratory extends beyond information management to encompass physical processes through robotics and integrated systems. In 2025, automation is becoming more widely deployed, particularly in processes like manual aliquoting and the pre-analytical steps of assay workflows [81].
Impact on Laboratory Workflows
The implementation of automation and robotics delivers measurable benefits:
- Reduced Error: Automating tasks like barcoding, sorting, and decapping samples reduces the likelihood of human error [81].
- Increased Productivity: Automation increases throughput and allows lab-based staff more time to focus on higher-value activities, such as quality control troubleshooting or managing complex test processes [81].
- Improved Connectivity: The Internet of Medical Things (IoMT) enables instruments, robots, and "smart" consumables to communicate seamlessly, creating highly efficient, connected workflows [81]. A recent survey indicates that 95% of laboratory professionals believe adopting automated technologies improves their ability to deliver patient care [81].
Workflow Automation Logic
The following diagram illustrates the logical relationship and decision points in a modern, automated laboratory workflow that integrates both analytical processes and data management.
The Scientist's Toolkit: Essential Research Reagent Solutions
Implementing the workflows and methods discussed requires specific reagents and materials. The following table details key components used in the comparative study of culture-based and molecular methods for MDR pathogen detection [2].
Table 3: Essential Research Reagents and Materials for MDR Pathogen Detection
| Item Name | Function/Application | Specific Example/Kit |
|---|---|---|
| Copan Faecal Swab | Collection, storage, and transportation of rectal swab specimens in liquid Cary-Blair medium. | Copan Faecal Swab [2] |
| Selective Culture Media | Supports growth of target organisms while inhibiting others; used for primary culture. | MacConkey Agar with antibiotic disks (e.g., meropenem, ceftazidime) [2] |
| Multiplex Real-Time PCR Kit | Simultaneous detection of multiple resistance genes directly from samples. | Allplex Entero-DR Assay (detects blaKPC, OXA-48, VIM, NDM, IMP, CTX-M, vanA, vanB) [2] |
| Supplementary Identification Kit | Identifies specific bacterial species from grown colonies. | MALDI-TOF MS Biotyper Sirius System [2] |
| Automated Antimicrobial Susceptibility Test | Determines Minimum Inhibitory Concentration (MIC) values for phenotypic resistance. | VITEK AST cards [2] |
| Rapid Immunochromatographic Test | Rapid, phenotypic detection of specific enzymes (e.g., CTX-M). | RESIST CTX-M [2] |
The integration of workflow automation, robotics, and Laboratory Information Systems represents the future of efficient, data-driven laboratory operations. The comparative data between culture-based and molecular methods clearly demonstrates that a hybrid, context-dependent approach is often most effective. Molecular techniques offer unparalleled speed and sensitivity for specific genetic markers, making them ideal for rapid screening and precise resistance mechanism identification [2]. Culture-based methods remain indispensable for obtaining isolates for further study and conducting phenotypic antimicrobial susceptibility testing [2].
Successful implementation requires careful strategic planning. Laboratories must prioritize system interoperability to ensure seamless data flow between instruments, robots, and the LIMS [83]. They must also address cybersecurity concerns, especially as workflows become more connected and data-rich [81]. Furthermore, with an increasing emphasis on sustainability, labs are adopting automation and greener processes not only for efficiency but also to align with environmental goals [81]. The selection of a LIMS and automation solutions should ultimately be driven by the lab's specific workflow needs, data volume, compliance requirements, and growth trajectory. By making informed choices, laboratories can transform their operations, enhance productivity, and better serve the needs of research and patient care.
The accurate and timely detection of pathogens is a cornerstone of effective clinical diagnostics and antimicrobial stewardship. For decades, culture-based methods have served as the traditional gold standard. However, these methods face significant challenges when confronting real-world biological complexities, including prior antibiotic exposure, samples with low microbial biomass, and the presence of non-cultivable pathogens [84] [41]. These limitations can lead to false-negative results, delayed targeted therapy, and ultimately, poorer patient outcomes.
Molecular diagnostics, particularly PCR-based methods, have emerged as powerful alternatives that circumvent many of these biological hurdles. This guide provides an objective, data-driven comparison of these two approaches, synthesizing evidence from recent clinical studies to inform researchers, scientists, and drug development professionals. The analysis is framed within the critical thesis that while culture offers the benefit of live isolates for further testing, molecular methods often provide superior diagnostic performance in clinically challenging scenarios.
Performance Data Comparison
The following tables summarize key quantitative findings from recent comparative studies, highlighting the performance disparities between culture-based and molecular methods across different clinical applications.
Table 1: Overall Diagnostic Performance in Challenging Scenarios
| Clinical Application | Metric | Culture-Based Method | Molecular Method (PCR) | Citation |
|---|---|---|---|---|
| CPGNB Screening (Rectal Swabs) | Sensitivity | 64.8% (with NFGNB included) | 90.2% | [3] |
| Hands-on Time (per sample) | 89.97 minutes | 1.3 minutes | [3] | |
| Podiatric Wound Infections | Sensitivity (vs. Culture) | Reference | 98.3% | [41] |
| Specificity (vs. Culture) | Reference | 73.5% | [41] | |
| Specificity (via Latent Class Analysis) | Not Reported | 91.0% | [41] | |
| Emergency Department Pneumonia | Median Turnaround Time | 48-50 hours | 12-14 hours | [85] |
| Diagnostic Yield | 56.8% - 61.6% | 80.0% - 80.6% | [85] |
Table 2: Impact on Clinical Workflow and Stewardship
| Parameter | Impact of Culture-Based Method | Impact of Molecular Method | Citation |
|---|---|---|---|
| Pathogen Detection Scope | Limited to cultivable organisms; often misses anaerobes and fastidious bacteria. | Broad detection of panels of pathogens, including anaerobes, viruses, and fastidious species. | [41] [85] |
| Effect of Prior Antibiotics | Significant reduction in yield due to loss of microbial viability. | Minimal impact; detects pathogen DNA regardless of viability. | [41] |
| Antibiotic Stewardship | Delayed targeted therapy; higher rates of empiric regimen changes. | Faster targeted therapy; increased guideline-concordant empiric therapy; shorter antibiotic courses. | [85] |
| Hands-on Time | High, requiring extensive manual processing. | Low, with high automation potential. | [3] |
Detailed Experimental Protocols
To ensure the reproducibility of these comparative findings, this section outlines the key methodologies employed in the cited studies.
Protocol 1: Comparative Evaluation for Carbapenemase-Producing Gram-Negative Bacilli (CPGNB)
This protocol is derived from a large-scale, year-long comparative study. [3]
- Sample Collection: Rectal swab samples were obtained from patients upon admission.
- Culture-Based Arm:
- Primary Culture: Samples were inoculated onto chromID CARBA SMART chromogenic agar.
- Confirmation: Presumptive positive colonies were confirmed using conventional polymerase chain reaction (PCR) for carbapenemase genes.
- Special Consideration: The study specifically included and performed whole-genome sequencing on non-fermenting Gram-negative bacilli (NFGNB) isolated on culture, which are sometimes disregarded in routine screening.
- Molecular Arm: Direct-from-specimen testing was performed using the Cepheid Xpert Carba-R assay, a real-time PCR test, without a prior culture step.
- Reference Standard: A sample was considered a true positive for CPGNB if it was detected by either testing method.
- Additional Metrics: The study calculated hands-on time for laboratory personnel and modeled the number of patient contacts averted by faster, more sensitive detection.
Protocol 2: Comparative Diagnostic Evaluation in Podiatric Wound Infections
This protocol focuses on a dual-swab approach for wound infection diagnosis. [41]
- Sample Collection: Dual-swab specimens were collected from each clinical wound case, allowing for parallel testing and minimizing sampling bias.
- Culture-Based Arm: Culture and antimicrobial susceptibility testing were performed by a commercial reference laboratory according to their standard protocols. Gram stains were assessed for morphological features.
- Molecular Arm:
- DNA Extraction: Nucleic acid was extracted using the MagMAX Microbiome Ultra Nucleic Acid Isolation Kit, which included a mechanical bead-based lysis step to disrupt tough bacterial cell walls.
- PCR Amplification & Detection: Real-time PCR was performed using a nanoscale SmartChip Real-Time PCR System with TaqMan assays. The panel targeted a comprehensive set of clinically relevant bacterial and fungal pathogens, as well as key antibiotic resistance genes.
- Statistical Analysis: Diagnostic performance was calculated with culture as the reference standard. Additionally, Latent Class Analysis (LCA), a statistical method that does not assume a perfect gold standard, was used to provide unbiased accuracy estimates. Logistic regression models incorporating 16S rRNA cycle threshold (Ct) values and Gram stain morphology were also used to assess the clinical relevance of PCR-only detections.
Signaling Pathways and Workflows
The biological limitations of culture-based methods are often rooted in specific cellular states and pathways. The following diagrams, generated with Graphviz, illustrate these concepts and the contrasting testing workflows.
VBNC State Induction Pathway
Diagram 1: Induction of the Viable But Non-Culturable (VBNC) State. This pathway illustrates how environmental stresses trigger a cascade of cellular events, notably the activation of Toxin-Antitoxin Systems (TAS), leading to a dormant state characterized by metabolic shutdown and high tolerance to antimicrobials. [84] This state renders the bacteria unable to proliferate on standard culture media, leading to false-negative diagnostic results.
Diagnostic Workflow Comparison
Diagram 2: Comparative Diagnostic Workflows. This diagram contrasts the multi-step, time-consuming culture-based pathway, which is vulnerable to multiple biological limitations at the initial growth stage, with the streamlined molecular pathway that bypasses the need for microbial proliferation to generate a faster result.
The Scientist's Toolkit: Research Reagent Solutions
The following table details key reagents and materials essential for implementing the molecular protocols discussed in this guide, particularly for overcoming the specified biological limitations.
Table 3: Essential Research Reagents for Molecular Detection of Challenging Pathogens
| Item | Function/Application | Key Characteristic |
|---|---|---|
| Chromogenic Agar (e.g., chromID CARBA SMART) | Selective isolation and presumptive identification of carbapenemase-producing organisms in culture-based methods. | Contains substrates that cause specific bacteria to produce colored colonies based on enzyme activity. [3] |
| Bead-Based Lysis Kit (e.g., MagMAX Microbiome Ultra) | Mechanical and chemical disruption of a wide range of bacterial cell walls (Gram-positive and Gram-negative) for DNA release. | Essential for efficient DNA extraction from tough-to-lyse organisms and non-viable cells. [41] |
| Multiplex PCR Panels (Seasonally Adapted) | Simultaneous detection of multiple viral and bacterial pathogens in a single reaction. | Can be tailored to local epidemiology (e.g., seasonal respiratory panels) to increase diagnostic relevance and yield. [85] |
| TaqMan Assays | Real-time PCR detection of specific pathogen DNA sequences and antibiotic resistance genes. | Provides high specificity and sensitivity, allowing for quantitative or qualitative detection. [41] |
| Internal Control Templates | Monitors extraction efficiency, amplification performance, and rules out PCR inhibition in each sample. | Critical for validating negative results and ensuring assay reliability, especially in complex samples. [41] |
Performance Validation and Comparative Analysis of Diagnostic Accuracy
The accurate and timely diagnosis of infectious diseases is a cornerstone of effective patient management and antimicrobial stewardship. For decades, culture-based methods have served as the gold standard in clinical microbiology, providing vital information on pathogen identity and antimicrobial susceptibility. However, the landscape of diagnostic microbiology is rapidly evolving with the advent of molecular diagnostic techniques, which offer the promise of unprecedented speed, sensitivity, and specificity. This guide provides a systematic, evidence-based comparison of the analytical sensitivity and specificity of these competing methodologies across various clinical applications, presenting objective data to inform research directions and diagnostic strategies within the scientific community.
Performance Metrics in Clinical Applications
The comparative performance of molecular and culture-based methods varies across different infection types and sample matrices. The following section synthesizes quantitative findings from recent head-to-head studies.
Urinary Tract Infections (UTIs)
Table 1: Performance Comparison for UTI Diagnosis
| Metric | PCR Method | Culture Method | Study Context |
|---|---|---|---|
| Positive Percent Agreement | 95.32% (Baseline), 88.06% (EOS) | Reference Standard | Complicated UTIs in adults [86] |
| Negative Percent Agreement | 38.30% (Baseline), 62.91% (EOS) | Reference Standard | Complicated UTIs in adults [86] |
| Correlation of Cq with ≥10ⵠCFU/mL | 83.3% overall agreement | Reference Standard | Clinical urine samples (n=168) [87] |
| Gram-Negative Correlation | 87.6% agreement (121/138) | Reference Standard | Clinical urine samples [87] |
| Gram-Positive Correlation | 63.3% agreement (19/30) | Reference Standard | Clinical urine samples [87] |
A 2025 comparative study on complicated UTIs (cUTIs) demonstrated that PCR-guided management offers several advantages, enabling the early adoption of narrower antibiotic therapies and improving clinical outcomes. The study reported good agreement between PCR and culture in positive cases, but highlighted challenges in negative case agreement, suggesting PCR may detect pathogens missed by culture [86]. Further investigating quantitative correlation, research has established that qPCR quantification cycle (Cq) values can reliably predict clinically relevant bacterial loads. For Gram-negative bacteria, Cq values of <23, 23-28, and >28 corresponded with ≥10ⵠCFU/mL, <10ⵠCFU/mL, and negative cultures, respectively [87].
Joint Infections
Table 2: Performance Comparison for Joint Infection Diagnosis
| Metric | Biofire FilmArray JA Panel | Culture Method | Study Context |
|---|---|---|---|
| Sensitivity | 96.3% | Reference Standard | Native and prosthetic joint infections (n=165 SF samples) [88] |
| Specificity | 97.8% | Reference Standard | Native and prosthetic joint infections (n=165 SF samples) [88] |
| Pathogen Detection Rate | 24/27 culture-positive cases plus 11 additional culture-negative cases | 27/165 (16.3%) | Prospective cohort [88] |
| Mean Turnaround Time | ~14 hours | ~35 hours | Clinical practice setting [88] |
A 2025 prospective evaluation of the Biofire FilmArray Joint Infection (BJA) panel demonstrated its high real-world performance. The assay identified pathogens in 11 culture-negative cases, uncovering complex polymicrobial infections often missed by culture. The significantly shorter turnaround time (approximately 21 hours faster) facilitated earlier optimization of antibiotic therapy in 11 cases, showcasing its direct clinical impact [88]. The evolving diagnostic landscape for Prosthetic Joint Infection (PJI) increasingly integrates molecular techniques like PCR and next-generation sequencing (NGS) with synovial biomarkers to overcome the limitations of culture, particularly in biofilm-associated and low-virulence infections [89].
Pleural and Other Infections
For pleural infections, molecular methods exhibit a markedly higher detection rate compared to conventional culture. A prospective observational study using shotgun metagenomics and bacterial metataxonomics identified pathogens in 54% (14/26) of cases, compared to only 38% (10/26) with culture [90]. These techniques revealed complex polymicrobial infections not captured by traditional methods, though challenges remain in interpreting results from low-biomass specimens and distinguishing true pathogens from background microbial noise [90].
In the context of Helicobacter pylori eradication, molecular methods for detecting antibiotic resistance have developed rapidly. Multiplexed qPCR assays for clarithromycin and levofloxacin resistance mutations demonstrate sensitivities and specificities approaching 100%, showing high concordance with phenotypic E-test methods [91]. These non-invasive methods can quickly and accurately determine resistance status, guiding personalized eradication therapy.
Detailed Experimental Protocols
To ensure reproducibility and critical appraisal, this section outlines the key methodologies employed in the cited comparative studies.
Protocol 1: qPCR vs. Culture in UTI (Correlative Quantification)
This protocol describes the procedure for establishing a correlation between qPCR Cq values and culture-based CFU counts [87].
- Sample Preparation: Serial dilutions (10⸠to 10ⰠCFU/mL) of common UTI pathogens (e.g., E. coli, K. pneumoniae, E. faecalis) are prepared in sterile urine using a 0.5 McFarland standard as a starting point.
- Culture-Based Quantification:
- For each dilution, 100 µL is plated in triplicate on Tryptic Soy Agar (TSA) or Mueller-Hinton Agar (MHA).
- Plates are incubated overnight at 37°C.
- Colony counts are performed, and CFU/mL is calculated.
- Nucleic Acid Extraction and qPCR:
- 1.0 mL of each dilution is centrifuged, and the cell pellet is resuspended in a molecular transport medium (e.g., PrimeStore).
- Total nucleic acid is extracted using a system like the ThermoFisher KingFisher Flex.
- qPCR is performed in triplicate using a syndromic UTI panel (e.g., HealthTrackRx OpenArray UTI panel) on a platform such as the QuantStudio 12K Flex.
- Data Analysis: Average Cq values for each dilution are plotted against the log10 CFU/mL values to generate standard curves. A correlational algorithm is established to define Cq thresholds corresponding to the clinically relevant cutoff of 10âµ CFU/mL.
Protocol 2: Multiplex PCR vs. Culture in Joint Infection
This protocol describes the evaluation of a syndromic PCR panel for synovial fluid samples [88].
- Sample Collection and Processing: Synovial fluid (SF) is collected aseptically from patients with symptoms consistent with native or prosthetic joint infection.
- Reference Culture Method: SF is inoculated onto standard aerobic and anaerobic culture media according to clinical laboratory protocols. Cultures are monitored for growth for a standard duration (e.g., 5-14 days).
- Molecular Testing with Syndromic Panel:
- A portion of the SF sample is used with the Biofire FilmArray Joint Infection (BJA) panel or similar multiplex PCR system.
- The sample is loaded into the self-contained pouch or cartridge, which integrates nucleic acid extraction, amplification, and detection.
- The panel detects a predefined set of pathogens (e.g., 31 bacteria and yeast) and resistance genes.
- Discrepancy Analysis: Results discordant with culture are re-analyzed using supplementary methods, such as species-specific PCRs or 16S-rDNA sequencing.
- Data Collection: Clinical data, including time to result and antibiotic therapy changes, are collected to assess clinical impact.
Protocol 3: Metagenomics vs. Culture in Pleural Infection
This protocol outlines the use of next-generation sequencing for complex infection diagnosis [90].
- Prospective Cohort Enrollment: Consecutive patients with clinically suspected pleural infection and control patients with non-infective effusions are enrolled.
- Sample Analysis:
- Conventional Culture: Pleural fluid is subjected to standard microbiological culture.
- Shotgun Metagenomics: Total DNA is extracted from pleural fluid. Sequencing libraries are prepared and sequenced on a high-throughput platform (e.g., Illumina). The resulting reads are analyzed against reference databases for taxonomic assignment and functional analysis.
- Bacterial Metataxonomics: 16S rRNA gene amplicon sequencing is performed to profile the bacterial community.
- Quantitative PCR (qPCR): Specific qPCR assays may be used to quantify total bacterial load.
- Bioinformatic Analysis: Sequencing data is processed to identify pathogens, assess microbial diversity, and filter out potential contaminants. The diagnostic performance of molecular methods is compared against culture and a composite clinical standard.
Signaling Pathways, Workflows & Logical Diagrams
The shift from culture-based to molecular diagnostics represents a fundamental change in workflow and logic. The following diagrams illustrate these processes.
Comparative Diagnostic Workflow
Diagram 1: Comparative diagnostic workflow. The culture-based pathway (green) involves sequential, time-consuming steps for isolation, identification, and susceptibility testing. The molecular pathway (red) consolidates extraction and detection, providing simultaneous pathogen and resistance marker identification, drastically reducing turnaround time [88] [89].
Diagnostic Decision Pathway for PJI
Diagram 2: PJI diagnostic pathway. This logic flow illustrates the integration of traditional tests (culture), molecular methods (PCR, NGS), and synovial biomarkers in a modern diagnostic algorithm for PJI. Artificial Intelligence (AI) and machine learning (ML) models are increasingly used to synthesize these multi-modal data points to generate a diagnostic probability, guiding definitive treatment, especially in challenging culture-negative cases [89].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Kits for Comparative Studies
| Item Name | Function / Application | Specific Example / Technology |
|---|---|---|
| Nucleic Acid Extraction Kits | Purification of DNA/RNA from clinical samples for molecular assays. | Silica column-based (QIAGEN), magnetic bead-based (ThermoFisher KingFisher Flex) [87] [92] |
| Direct-to-PCR (D2P) Reagents | Extraction-free lysis buffers enabling direct amplification. | Antimicrobial peptide-based lysis buffers for bacterial, fungal, and viral targets [92] |
| Syndromic PCR Panels | Multiplexed detection of pathogens and resistance genes from specific sample types. | Biofire FilmArray Joint Infection (JI) Panel, Gastrointestinal (GI) Panel [88] |
| OpenArray Plates | High-throughput nanofluidic qPCR platform for custom pathogen panels. | HealthTrackRx UTI syndromic panel on QuantStudio 12K Flex platform [87] |
| Metagenomic Sequencing Kits | Library preparation for comprehensive, culture-independent pathogen detection. | Shotgun metagenomics and 16S rRNA sequencing kits for pleural fluid/biopsy samples [90] |
| Peptide Nucleic Acid (PNA) Probes | Enhanced specificity in qPCR assays for detecting single nucleotide polymorphisms (SNPs). | PNA probe-based qPCR for H. pylori clarithromycin resistance mutations [91] |
| Antimicrobial Peptide-based Lysis Buffers | Selective lysis of pathogens in complex samples for Direct-to-PCR workflows. | PCROpsis D2P buffers for UTIs, STIs, and RTIs [92] |
The rapid and accurate identification of pathogens is a cornerstone of effective infectious disease management. For decades, culture-based methods have served as the gold standard in clinical microbiology, relying on the growth and phenotypic characterization of microorganisms. However, the emergence of molecular diagnostic methods has revolutionized pathogen detection through the analysis of microbial genetic material. This shift carries profound implications for both patient outcomes and antimicrobial stewardship programs (ASPs), which coordinate interventions to optimize antimicrobial use. Molecular methods offer significantly reduced turnaround times (TAT), with some platforms providing results within 2.5 hours of a positive Gram stain compared to the 30 or more hours typically required for conventional culture and identification [93]. This assessment comprehensively compares the clinical impact of these diagnostic approaches, evaluating their effects on time to appropriate therapy, mortality, hospital stay, and antimicrobial stewardship efficacy.
Comparative Experimental Methodologies
The evaluation of diagnostic technologies relies on structured clinical studies that compare well-defined laboratory protocols and their subsequent impact on clinical decision-making.
Conventional Culture-Based Protocols
Culture methods begin with inoculating clinical specimens (e.g., blood, urine, tissue) onto selective and non-selective agar plates and into liquid enrichment media. Blood cultures are monitored for up to 5 days for signs of microbial growth. Once growth is detected, subculturing is performed to obtain pure isolates, which are then identified using phenotypic techniques such as biochemical profiling (e.g., VITEK 2, API strips) or matrix-assisted laser desorption/ionization time-of-flight (MALDI-TOF) mass spectrometry. Subsequent antimicrobial susceptibility testing (AST) is performed via disk diffusion, gradient diffusion, or broth microdilution methods, requiring an additional 18-24 hours [35] [94]. The total time from specimen collection to final AST results typically spans 48 to 72 hours or longer for slow-growing or fastidious organisms.
Molecular Diagnostic Protocols
Molecular techniques bypass the need for microbial growth, directly detecting pathogen-specific genetic markers. Common methodologies include:
- Multiplex Nucleic Acid Amplification Tests (NAATs): Platforms like the Verigene BC-GN test utilize a microarray to detect specific pathogens and resistance genes (e.g., CTX-M, KPC, NDM) directly from positive blood cultures in approximately 2.5 hours [93].
- Broad-Range PCR and Sequencing: Amplification of conserved genomic regions (e.g., 16S rRNA gene) followed by Sanger or next-generation sequencing (NGS) allows for identification of a wide spectrum of bacteria, including non-cultivatable species [35] [66].
- Whole Genome Sequencing (WGS): This comprehensive approach sequences the entire genome of a pathogen, enabling high-resolution typing and detailed detection of resistance and virulence markers [95].
These protocols are often integrated with antimicrobial stewardship interventions, where results are rapidly communicated to clinicians with interpretation and tailored therapy recommendations [93] [96].
Quantitative Impact on Patient Outcomes and Antimicrobial Use
Robust clinical data, particularly from bloodstream infections, demonstrate the significant advantage of molecular methods coupled with ASP support over conventional methods.
Table 1: Impact of Molecular vs. Culture-Based Methods on Key Clinical Metrics
| Clinical Metric | Molecular Methods + ASP | Conventional Methods + ASP | P-value |
|---|---|---|---|
| Time to Optimal Therapy (hours) | 20.5 (IQR: 17.0-42.2) | 50.1 (IQR: 27.6-77.9) | < 0.001 [93] |
| Time to Effective Therapy (hours) | 15.9 (IQR: 1.9-25.7) | 28.0 (IQR: 9.5-56.7) | < 0.001 [93] |
| Detection Sensitivity | ~90-97.1% [93] [35] | ~60-70% [35] [66] | Not Applicable |
| Species Diversity Detection | Significantly Higher [35] [66] | Limited to cultivable organisms | Not Applicable |
Analysis of Clinical Outcome Data
The data in Table 1, derived from a multicenter cohort study of Gram-negative bloodstream infections, highlights the dramatic reduction in time to appropriate antimicrobial therapy. This 29.6-hour median improvement in time to optimal therapy is clinically significant, as each hour of delay in effective antimicrobial administration is associated with increased mortality in septic patients [97]. Furthermore, molecular methods demonstrate superior analytical sensitivity and capacity to identify a broader range of pathogens, including polymicrobial infections and slow-growing bacteria that are often missed by culture [35] [95]. This comprehensive detection facilitates more targeted and complete antimicrobial coverage.
Diagnostic and Stewardship Workflows
The integration of rapid molecular diagnostics into clinical practice creates a more efficient pathway for pathogen identification and treatment optimization. The following diagram illustrates the comparative workflows and their impact on clinical decision-making.
Diagnostic Workflow Comparison
The molecular pathway demonstrates a significantly compressed timeline, enabling earlier ASP intervention. When a rapid molecular result is available, stewardship teams can provide specific antibiotic recommendations approximately 30 hours sooner than with conventional culture [93]. This expedited intervention is critical for improving patient outcomes and represents the core value proposition of molecular diagnostics in infectious disease management.
Essential Research Reagent Solutions
The execution of the methodologies described requires specific, high-quality reagents and platforms. The following table details key materials essential for research in this field.
Table 2: Key Research Reagent Solutions for Diagnostic Method Comparison
| Reagent/Material | Function | Example Applications |
|---|---|---|
| Selective & Enrichment Media | Supports growth of specific microorganisms while inhibiting others. | Blood culture bottles, MacConkey agar, Chocolate agar for primary culture [35] [94]. |
| Nucleic Acid Extraction Kits | Isolates and purifies DNA/RNA from clinical samples. | Critical first step for all PCR- and sequencing-based molecular methods [35] [66]. |
| Pathogen-Specific Primer/Probe Panels | Targets unique genetic sequences for amplification and detection. | Multiplex PCR panels (e.g., Verigene, BioFire) for identifying pathogens and resistance genes from positive blood cultures [93] [95]. |
| 16S rRNA Universal Primers | Amplifies conserved bacterial gene regions for identification. | Broad-range bacterial identification and community analysis via Sanger sequencing or NGS [35] [66]. |
| Microarray or Sequencing Kits | Provides reagents for hybridization or library preparation. | Verigene system microarrays; kits for Illumina or Oxford Nanopore sequencing [93] [95]. |
The evidence demonstrates a clear and significant clinical advantage for molecular diagnostic methods over traditional culture-based approaches. The integration of rapid molecular testing with antimicrobial stewardship programs creates a synergistic effect, drastically reducing time to optimal antimicrobial therapy by approximately 30 hours for serious infections like Gram-negative bloodstream infections [93]. This acceleration in appropriate treatment directly addresses a critical factor in sepsis outcomes. While culture remains important for phenotypic antimicrobial susceptibility testing and is more accessible in resource-limited settings, molecular methods provide unparalleled speed, sensitivity, and comprehensive pathogen detection. The future of clinical microbiology lies in hybrid diagnostic models that leverage the strengths of both approaches, further enhanced by emerging technologies like next-generation sequencing and artificial intelligence, to optimize patient outcomes and combat antimicrobial resistance on a global scale [98] [96].
In the challenging landscape of complex infections, accurate identification of polymicrobial pathogens is critical for effective patient management. Traditional culture-based methods have long been the cornerstone of microbiological diagnosis, but emerging molecular technologies now offer compelling alternatives with potentially superior capabilities for detecting mixed infections. The clinical significance of this comparison is substantial, as polymicrobial infections contribute significantly to mortality, prolonged hospital stays, and increased healthcare costs, particularly in cases of necrotizing soft tissue infections, neurosurgical central nervous system infections, and complicated urinary tract infections [99] [35]. This guide provides a comprehensive, evidence-based comparison of these methodological approaches, focusing on their respective performances in detecting complex polymicrobial communities across various clinical scenarios.
Performance Comparison: Quantitative Data Analysis
The diagnostic performance of culture versus molecular methods has been extensively evaluated across multiple infection types. The following tables summarize key comparative metrics from recent clinical studies.
Table 1: Overall Pathogen Detection Performance Across Infection Types
| Infection Type | Method | Detection Rate | Turnaround Time | Polymicrobial Detection Advantage | Study (Year) |
|---|---|---|---|---|---|
| Neurosurgical CNS Infections | Microbial Culture | 59.1% | 22.6 ± 9.4 hours | Reference | [99] (2025) |
| mNGS | 86.6% (p<0.01) | 16.8 ± 2.4 hours | Significantly higher | [99] (2025) | |
| ddPCR | 78.7% (p<0.01) | 12.4 ± 3.8 hours (p<0.01 vs mNGS) | Significantly higher | [99] (2025) | |
| Complicated UTI | Culture & Sensitivity | 78.1% clinical success | 104.4 hours | Reference | [100] (2024) |
| PCR-guided | 88.1% clinical success (p=0.011) | 49.7 hours (p<0.001) | 95% vs 22% for polymicrobial infections | [100] [40] | |
| Necrotizing Soft Tissue Infections | Culture | 70% of samples | Not specified | Reference | [35] (2016) |
| Molecular Methods | 90% of samples | Significantly shorter | Detected additional microorganisms | [35] (2016) | |
| Bloodstream Infections | Molecular tests (from PBCs) | 92-99% sensitivity | Not specified | Broad pathogen panel identification | [101] (2024) |
Table 2: Analytical Performance Characteristics of Molecular Methods
| Method | Principle | Key Advantages | Limitations | Best Applications |
|---|---|---|---|---|
| mNGS (Metagenomic Next-Generation Sequencing) | High-throughput, culture-independent, unbiased pathogen detection | Unbiased detection of novel, rare, and atypical pathogens; not affected by empiric antibiotics | Higher cost; complex bioinformatics; longer turnaround than ddPCR; cannot distinguish viable from non-viable pathogens | Complex CNS infections, unusual presentations, research on novel pathogens [99] |
| ddPCR (Droplet Digital PCR) | Microfluidic partitioning for absolute quantification of target DNA | High sensitivity, reproducibility, simplicity, speed; absolute quantification without standards | Limited to predefined targets; requires prior knowledge of potential pathogens | Rapid diagnosis of known pathogens, quantification of pathogen load [99] |
| Multiplex PCR Panels | Simultaneous amplification of multiple pathogen-specific sequences | Comprehensive pathogen profiling from single specimen; rapid results | Limited to panel targets; may miss uncommon pathogens not included in panel | Gastrointestinal, respiratory, urinary tract infections with broad differential [40] |
| Real-time PCR | Fluorescence-based monitoring of amplification in real-time | High sensitivity and specificity; rapid results; quantitative potential | Limited multiplexing capacity; requires specific equipment | Targeted detection of specific pathogens with known resistance markers [102] |
Experimental Protocols and Methodologies
Sample Processing and Nucleic Acid Extraction
For comprehensive polymicrobial detection, proper sample handling is critical across all methodological approaches:
Sample Collection: Clinical samples (cerebrospinal fluid, pus, tissue debridement, urine) should be collected aseptically and divided into aliquots for culture-based and molecular testing. CSF samples are typically obtained via lumbar puncture or through drainage tubes, while abscess samples are collected during surgical intervention [99].
Transport and Storage: Samples for molecular analysis should be transported in sterile containers with glycerol or ethanol and stored at 4°C if testing occurs within a brief period. For longer storage, preservation at -80°C is recommended to maintain nucleic acid integrity [99] [35].
Nucleic Acid Extraction: For mNGS and ddPCR, total nucleic acid extraction is performed using commercial kits capable of isolating both DNA and RNA. The extraction should include mechanical lysis (bead beating) to ensure disruption of tough microbial cell walls, particularly for Gram-positive bacteria and fungi [99].
Metagenomic Next-Generation Sequencing (mNGS) Protocol
The mNGS methodology provides culture-independent, unbiased pathogen detection:
Library Preparation: Extracted nucleic acids undergo library preparation using tagmentation-based approaches or fragmentation followed by adapter ligation. For comprehensive pathogen detection, both DNA and RNA libraries should be prepared, with RNA undergoing reverse transcription to cDNA [99].
Sequencing: Libraries are sequenced on high-throughput platforms such as Illumina or Oxford Nanopore technologies. For clinical applications, Illumina platforms typically provide sufficient depth (5-10 million reads per sample) for adequate sensitivity while maintaining cost-effectiveness [99].
Bioinformatic Analysis: Sequencing reads are subjected to quality control (adapter trimming, quality filtering), followed by host sequence depletion by alignment to human reference genomes. Microbial identification is performed by alignment to comprehensive microbial databases or through k-mer based classification tools [99].
Droplet Digital PCR (ddPCR) Protocol
ddPCR provides absolute quantification of target pathogens without standard curves:
Droplet Generation: The PCR reaction mixture containing template DNA, primers, probes, and master mix is partitioned into approximately 20,000 nanoliter-sized droplets using a droplet generator [99].
Amplification: Droplets undergo endpoint PCR amplification in a thermal cycler with optimized cycling conditions specific to the target pathogens of interest.
Droplet Reading and Analysis: The amplified droplets are analyzed in a droplet reader that counts fluorescent-positive and negative droplets. Absolute quantification of target DNA is calculated using Poisson statistics based on the fraction of positive droplets [99].
Culture-Based Methods with Reflex Testing
Traditional culture remains essential for certain applications:
Culture Conditions: Samples are inoculated onto enriched and selective media appropriate for the suspected pathogens. Aerobic and anaerobic conditions are maintained using appropriate incubation systems. The time to positive culture (TTPC) typically ranges from 15-28 hours depending on the pathogen [99] [35].
Reflex Culture: The CDC recommends reflex culture - culturing specimens with positive molecular results - for public health surveillance of bacteria including Campylobacter, Salmonella, Shigella, and Shiga toxin-producing Escherichia coli to enable antimicrobial susceptibility testing and molecular subtyping [40].
The following workflow diagram illustrates the parallel processes and decision points in culture-based versus molecular diagnostic approaches:
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagent Solutions for Polymicrobial Detection Studies
| Reagent/Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| Nucleic Acid Extraction Kits | Total nucleic acid extraction kits with mechanical lysis | Simultaneous DNA/RNA isolation; comprehensive pathogen detection | Must include bead-beating for tough microorganisms; should effectively remove PCR inhibitors |
| Library Preparation Kits | Tagmentation-based DNA library prep; RNA-to-cDNA kits | Preparation of sequencing libraries for mNGS | Should maintain fragment diversity; minimize bias; compatible with low-input samples |
| PCR Master Mixes | ddPCR supermixes; multiplex PCR master mixes | Amplification of target sequences in partitioned formats | Must have high efficiency and specificity; optimized for multiplexing |
| Selective Culture Media | Enriched and selective media for fastidious organisms | Cultivation of pathogens with specific growth requirements | Critical for culture comparison studies; should include aerobic and anaerobic conditions |
| Microbial Databases | Curated genomic databases (RefSeq, GenBank) | Reference for sequence alignment and pathogen identification | Regular updates essential; should include antimicrobial resistance markers |
| Bioinformatic Tools | Kraken2, Bracken, Bowtie2, BLAST | Taxonomic classification, host depletion, resistance gene detection | Validation with known controls critical; establish thresholds for clinical significance |
| Quality Control Materials | Known polymicrobial mock communities; extraction controls | Monitoring technical performance across batches | Should include Gram-positive, Gram-negative, and fungal targets |
The comparative analysis of culture-based and molecular methods for polymicrobial detection reveals a complex landscape where each approach offers distinct advantages. Molecular methods, particularly mNGS and ddPCR, demonstrate superior sensitivity and faster turnaround times, enabling more comprehensive detection of mixed infections. Culture remains essential for antimicrobial susceptibility testing and public health surveillance, highlighting the continued value of a complementary diagnostic approach. As molecular technologies evolve and become more integrated into clinical practice, their ability to rapidly identify complex polymicrobial communities will undoubtedly transform patient management and antimicrobial stewardship efforts. Future directions should focus on standardizing methodologies, validating clinical impact, and reducing costs to maximize accessibility across diverse healthcare settings.
The field of clinical microbiology is experiencing a fundamental transformation, moving from traditional culture-based methods toward sophisticated molecular techniques. This evolution is driven by the critical need for rapid, accurate pathogen identification to guide antimicrobial therapy, improve patient outcomes, and manage healthcare costs effectively. Culture-based methods, the long-standing gold standard, involve growing microorganisms on specialized media and identifying them through their biochemical characteristics, a process that can require 48 to 96 hours or more after isolation [103]. In contrast, molecular methods detect pathogen-specific genetic material, slashing turnaround times to a matter of hours. While this speed offers significant clinical advantages, the economic implications—encompassing equipment, reagents, and overall healthcare impact—are complex and multifaceted. This guide provides an objective comparison of these diagnostic approaches, framing the analysis within a broader thesis on their respective roles in modern clinical and research settings.
Economic and Performance Comparison at a Glance
The choice between diagnostic methodologies involves balancing performance, speed, and cost. The following table summarizes the core characteristics of culture-based and molecular methods, providing a foundation for a detailed cost-benefit analysis.
Table 1: Key Characteristics of Culture-Based and Molecular Diagnostic Methods
| Characteristic | Culture-Based Methods | Molecular Methods |
|---|---|---|
| Time to Result | Several days (2-5 days for blood culture) [104] | Same day (several hours) [105] |
| Key Equipment | Automated systems (e.g., API, VITEK), incubators, mass spectrometers (MALDI-TOF) [103] | Automated nucleic acid extraction systems, thermal cyclers, real-time PCR instruments, microarrays [104] [105] |
| Typical Reagents & Consumables | Growth media, substrates, biochemical test kits, identification strips [103] | Nucleic acid extraction kits, amplification reagents, enzymes, probes, calibrators [106] [105] |
| Sensitivity & Specificity | Good, but can be compromised by prior antibiotic therapy [104] | High (e.g., ≥85% sensitivity, >95% specificity for TB NAATs) [107] |
| Ability to Detect Polymicrobial Infections | Limited; inherent microbial fitness can favor some species over others [104] | Excellent; capable of identifying multiple pathogens from a single sample [104] |
| Antimicrobial Susceptibility Testing (AST) | Provides phenotypic AST profile directly | Primarily detects resistance genes (e.g., mecA for methicillin resistance); does not provide phenotypic profile [105] |
| Upfront Instrument Cost | Variable; modern automated systems and MALDI-TOF represent significant investment [103] | High (substantial capital investment) [107] [108] |
| Reagent/Consumable Cost | Generally lower per test | Generally higher per test (e.g., high cartridge costs) [107] |
| Labor Intensity | High for manual methods; reduced with automation | Lower, especially with integrated, automated platforms |
Detailed Methodologies and Experimental Protocols
To ensure reproducibility and provide a clear basis for comparison, this section outlines standard protocols for both diagnostic approaches.
Protocol for Culture-Based Identification and AST
This protocol outlines the standard procedure for processing a blood culture, a common scenario in clinical microbiology.
- Sample Collection and Inoculation: Aseptically collect blood samples and inoculate them into blood culture bottles. This step is critical, as contamination can lead to false positives and significant downstream costs [109].
- Incubation and Monitoring: Place the bottles in an automated, continuous-monitoring blood culture system. The system alerts when microbial growth is detected.
- Subculture and Isolation: Once growth is detected, aliquot the broth onto solid agar plates (e.g., blood agar, chocolate agar) to obtain isolated colonies of the pathogen(s). Incubate plates for 18-24 hours.
- Pure Culture Identification:
- Manual Method: Select isolated colonies for biochemical testing. This could involve traditional tubes (e.g., for indole, oxidase) or miniaturized, multitest kits (e.g., API strips) that test multiple substrates simultaneously [103].
- Automated Method: Use an automated identification system (e.g., VITEK 2) by preparing a standardized suspension of the pure isolate and loading it into a specialized test cartridge.
- Mass Spectrometry (MALDI-TOF): Apply a portion of a bacterial colony directly to a target plate for rapid identification, which can reduce time to identification to hours after isolation [103].
- Antimicrobial Susceptibility Testing (AST): Using a pure culture, perform AST via disk diffusion, gradient diffusion, or, most commonly, automated broth microdilution in systems like VITEK 2. This generates a phenotypic profile of the isolate's susceptibility to various antimicrobials.
Diagram: Culture-Based Diagnostic Workflow
Protocol for Molecular-Based Pathogen Detection and Resistance Gene Identification
This protocol describes a common real-time PCR approach for direct detection from a sample.
- Nucleic Acid Extraction: The first critical step is isolating DNA and/or RNA from the clinical specimen (e.g., blood, sputum). This is typically performed using automated extraction systems and commercial kits that provide high purity and yield [104].
- Target Amplification and Detection (Real-Time PCR):
- Reaction Setup: Combine the extracted nucleic acid with a master mix containing DNA polymerase, dNTPs, primers, and fluorescently labeled sequence-specific probes (e.g., TaqMan probes).
- Amplification: Place the reaction plate in a real-time PCR thermocycler. The instrument runs a programmed series of temperature cycles (denaturation, annealing, extension) to amplify the target genetic sequence.
- Real-Time Monitoring: With each cycle, the probe binds to the amplified target and is cleaved, releasing a fluorescent signal. The instrument monitors this fluorescence, allowing for both detection and quantification of the pathogen.
- Analysis: Software analyzes the amplification curve and determines the presence and, if applicable, the quantity (viral/bacterial load) of the target pathogen. For resistance detection, specific probes for genes like mecA (methicillin resistance) can be included in multiplex assays [105].
Diagram: Molecular Diagnostic Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of either diagnostic approach relies on a suite of key reagents and materials. The following table details these essential components and their functions.
Table 2: Key Reagents and Materials for Diagnostic Methods
| Item | Function | Application Context |
|---|---|---|
| Culture Media (Agar/Broth) | Provides nutrients to support microbial growth and differentiation. | Culture-based isolation and enrichment of pathogens from clinical samples [103]. |
| Biochemical Test Strips/Kits | Miniaturized panels of substrates to create a metabolic profile for identification. | Culture-based identification of bacterial species (e.g., Enterobacteriaceae) after isolation [103]. |
| Nucleic Acid Extraction Kit | Lyses cells and purifies DNA/RNA from clinical samples, removing inhibitors. | Essential first step for all molecular diagnostic assays to ensure amplification efficiency [104] [105]. |
| PCR Master Mix | Contains enzymes, nucleotides, and buffers necessary for nucleic acid amplification. | Core reagent for PCR-based molecular tests, including target amplification and detection [105]. |
| Sequence-Specific Probes & Primers | Short oligonucleotides that bind to unique genetic sequences of the target pathogen. | Enables specific detection and identification of pathogens in molecular assays (e.g., real-time PCR) [104] [105]. |
| Calibrators & Controls | Materials with known values used to standardize assays and monitor performance. | Critical for ensuring the accuracy and reliability of both molecular [106] [110] and automated culture-based systems. |
Comprehensive Cost-Benefit Analysis and Healthcare Economic Impact
A thorough economic evaluation must look beyond the per-test cost to encompass the total impact on the healthcare system. Molecular methods, despite higher upfront costs, can demonstrate significant value by improving patient outcomes and reducing downstream expenses.
Direct and Indirect Cost Considerations
- Molecular Method Costs: The economic burden includes "substantial capital investment, high cartridge costs, and ongoing maintenance requirements" [107]. Furthermore, the cost structure is complex, extending beyond the basic reagent kit to include calibrators, controls, and other consumables, collectively termed the "Cost per Reportable Test" (CPRT) [106]. One study found that inefficient quality control processes could add thousands of dollars in unnecessary monthly costs due to staff time and reagent waste [110].
- Culture-Based Method Costs: While the per-test reagent cost is often lower, the true expense includes longer hospital stays, additional diagnostic tests, and broader empiric antimicrobial therapy driven by slower turnaround times [104]. Contaminated cultures, a common issue, can generate significant downstream costs for unnecessary treatments and extended hospitalization, estimated at thousands of dollars per event [109].
Documented Cost-Effectiveness and Clinical Value
Recent economic syntheses strongly support the cost-effectiveness of molecular tests in high-burden settings. A 2025 systematic review concluded that molecular testing for pulmonary tuberculosis (e.g., Xpert MTB/RIF, TB-LAMP) was either cost-saving or highly cost-effective compared to conventional smear microscopy [107]. Probabilistic models from the review indicated a high (≥90%) probability of these tests being cost-effective.
The value of rapid molecular results is particularly pronounced in severe infections like bacteremia and sepsis. A cost-effectiveness analysis in intensive care units found that adding a molecular method to conventional blood culture for detecting antibiotic-resistant bacteria was "dominant"—meaning it provided better outcomes at a lower total cost—for infections caused by MRSA, carbapenem-resistant Gram-negative bacteria, and VRE [111]. The savings were substantial, equating to millions of Brazilian Reals per death avoided by enabling earlier targeted therapy [111].
Diagram: Diagnostic Result Impact on Patient Care
The choice between culture-based and molecular diagnostic methods is not a simple binary decision but a strategic one that balances diagnostic performance, speed, and total economic impact. Culture-based methods remain indispensable for providing a phenotypic antimicrobial susceptibility profile and for cultivating a wide range of organisms. However, molecular methods offer an undeniable advantage in speed, sensitivity, and the ability to detect difficult-to-culture pathogens and resistance genes directly from samples.
The economic evidence is clear: while the direct laboratory cost of a molecular test is often higher, its ability to guide earlier, appropriate therapy and reduce unnecessary treatment frequently makes it a cost-saving or highly cost-effective intervention from the broader health system perspective. For researchers, scientists, and drug development professionals, this analysis underscores that the optimal diagnostic pathway often involves a complementary use of both technologies, leveraging the speed of molecular methods for initial detection and the phenotypic clarity of culture for confirming susceptibility, thereby maximizing both patient outcomes and economic efficiency.
The rise of antimicrobial resistance (AMR) presents a significant challenge to global public health, complicating the treatment of infectious diseases and contributing to increased morbidity and mortality rates [112] [113]. As bacteria develop mechanisms to evade the effects of antibiotics, selecting the most appropriate antimicrobial therapy becomes increasingly difficult [112]. Within clinical microbiology and antimicrobial research, two fundamental approaches for detecting resistance have emerged: phenotypic susceptibility testing and genotypic resistance gene identification. These approaches are not mutually exclusive but offer complementary insights into bacterial resistance mechanisms [112]. Phenotypic testing describes the observable resistance of a bacterial population to an antibiotic, directly measuring the functional ability of bacteria to survive or continue multiplying despite antimicrobial exposure [112]. In contrast, genotypic resistance refers to the presence of specific genetic determinants within an organism's genome that provide the intrinsic potential for resistance, such as mutations in target genes or acquired genes encoding antibiotic-inactivating enzymes [112]. Understanding the distinctions, applications, strengths, and limitations of these approaches is crucial for researchers, scientists, and drug development professionals working to combat the AMR crisis.
Conceptual Foundations and Key Distinctions
Phenotypic Susceptibility: The Observable Response
Phenotypic resistance detection is grounded in measuring the direct effects of antibiotics on bacterial growth and survival. This approach determines the observable resistance of a bacterial population to an antibiotic through functional assays [112]. The cornerstone of phenotypic testing is the minimum inhibitory concentration (MIC) assay, which measures the lowest concentration of an antibiotic required to inhibit bacterial growth [112] [113]. Phenotypic methods do not require prior knowledge of resistance mechanisms and can detect both known and novel resistance patterns through observable growth endpoints. However, these methods are constrained by their dependence on bacterial growth rates, typically requiring 18-24 hours for results, and may not detect heteroresistance or specific resistance mechanisms without additional confirmatory testing [113] [114].
Genotypic Resistance Gene Identification: The Genetic Blueprint
Genotypic resistance detection focuses on identifying the genetic determinants that confer resistance potential. This approach identifies specific genetic targets within an organism's genome, including mutations in genes encoding essential targets for antibiotics or the acquisition of genes encoding resistance enzymes such as β-lactamases (e.g., CTX-M-15 or ampC) [112] [115]. Genotypic methods provide insights into the molecular mechanisms of resistance and can predict resistance patterns before they manifest phenotypically. The critical distinction lies in what each concept reveals: genotypic testing identifies the genetic potential for resistance, while phenotypic testing directly assesses the functional ability of bacteria to resist antibiotics [112]. This distinction is crucial because not all bacteria with genotypic resistance will necessarily exhibit phenotypic resistance, as factors like gene expression levels, genetic context, and environmental influences affect the translation of genetic potential into observable resistance [112].
Methodological Approaches and Experimental Protocols
Phenotypic Susceptibility Testing Protocols
Disk Diffusion Method
The disk diffusion method (Kirby-Bauer test) represents one of the most widely used phenotypic approaches due to its simplicity and cost-effectiveness [114]. The standardized protocol involves several key steps: First, a bacterial suspension is prepared and adjusted to a standard turbidity (0.5 McFarland standard, approximately 1.5 × 10^8 CFU/mL). This suspension is then uniformly inoculated onto the surface of Mueller-Hinton agar plates. Antibiotic-impregnated disks are subsequently applied to the inoculated agar surface. The plates are incubated at 35±2°C for 16-18 hours, after which the diameters of inhibition zones are measured and interpreted according to Clinical and Laboratory Standards Institute (CLSI) or European Committee on Antimicrobial Susceptibility Testing (EUCAST) guidelines to classify isolates as susceptible, intermediate, or resistant [114]. This method is particularly valuable for resistance surveillance and therapeutic decision-making for routine isolates, though it cannot provide precise MIC values [114].
Broth Microdilution Method
Broth microdilution represents the reference method for determining minimum inhibitory concentrations and is standardized by organizations including CLSI and EUCAST [113] [116]. The experimental workflow begins with preparation of a bacterial inoculum standardized to 0.5 McFarland standard, followed by dilution to achieve a final concentration of approximately 5 × 10^5 CFU/mL in each well of a microtiter plate. The plates contain serial two-fold dilutions of antibiotics in volumes of 50-100 μL per well. Positive control wells contain inoculated media without antibiotics, while negative control wells contain sterile media only. Following incubation at 35±2°C for 16-20 hours, the plates are examined for visible bacterial growth. The MIC is defined as the lowest antibiotic concentration that completely inhibits visible growth [113]. This method provides quantitative data essential for detecting shifts in susceptibility patterns and is particularly valuable for drug development research.
Gradient Diffusion Method
The gradient diffusion method (E-test) combines elements of both diffusion and dilution principles to establish MIC values [114]. This technique utilizes a plastic strip impregnated with a predefined antibiotic concentration gradient. The protocol involves inoculating an agar plate with a standardized bacterial suspension, then applying the E-test strips. During incubation, the antibiotic diffuses into the agar, creating a concentration gradient. The MIC is read at the intersection of the elliptical zone of inhibition with the strip scale. This method is particularly useful for fastidious organisms and when testing a limited number of antibiotics, though it is more expensive than conventional disk diffusion [114].
Genotypic Resistance Detection Protocols
PCR-Based Methods
PCR-based methods represent fundamental approaches for targeted genotypic resistance detection [113]. The standard protocol begins with DNA extraction from bacterial isolates using commercial kits. Specific primer pairs are designed to amplify known resistance genes or mutations. The reaction mixture typically includes template DNA, primers, dNTPs, buffer, and DNA polymerase. Amplification is performed through thermal cycling: initial denaturation at 95°C, followed by 30-40 cycles of denaturation, primer annealing (at temperatures specific to the primer set), and extension at 72°C. Amplification products are then analyzed by gel electrophoresis or real-time detection systems. Multiplex PCR formats enable simultaneous detection of multiple resistance genes in a single reaction [113]. These methods are particularly valuable for rapid screening of specific resistance mechanisms in surveillance programs and outbreak investigations.
Whole-Genome Sequencing (WGS)
Whole-genome sequencing provides a comprehensive analysis of the genetic basis of antimicrobial resistance [117]. The experimental workflow involves several stages: genomic DNA is extracted from bacterial isolates and quantified using fluorometric methods. Sequencing libraries are prepared through fragmentation, end-repair, adapter ligation, and size selection. High-throughput sequencing is performed using platforms such as Illumina, generating short reads (150-300 bp), or Oxford Nanopore, producing long reads (>10 kb). Bioinformatic analysis includes quality control, de novo assembly or reference-based mapping, and annotation using specialized databases (e.g., CARD, ResFinder) to identify resistance genes and mutations [117]. WGS enables the discovery of novel resistance mechanisms and provides insights into the genomic context of resistance genes, including their location on plasmids or chromosomes [118] [117].
Figure 1: Workflow comparison of phenotypic susceptibility testing and genotypic resistance detection methods.
Performance Comparison and Experimental Data
Comparative Analytical Performance
Multiple studies have directly compared the performance of phenotypic and genotypic methods for resistance detection. A 2024 study comparing whole-genome sequencing with phenotypic antimicrobial susceptibility testing in Salmonella isolates demonstrated that WGS achieved an overall sensitivity of 93.4% and specificity of 99.8% in predicting phenotypic resistance [117]. Discrepancies were observed in 16 instances, with 15 being phenotypically resistant but genotypically susceptible, suggesting undefined resistance mechanisms [117]. Another study on Pasteurella multocida isolates found that MIC values from broth microdilution showed a stronger positive correlation with genotypic results compared to disk diffusion, making it a more suitable phenotypic method for determining antibiotic susceptibility [116]. The concordance between genotypic and phenotypic methods varies significantly by antibiotic class, with strong correlations observed for phenicols, tetracyclines, and fluoroquinolones, but poorer correlations for sulfamethoxazole, β-lactams, and macrolides, indicating the presence of unexplained resistance mechanisms [116].
Table 1: Performance Comparison of Phenotypic and Genotypic Detection Methods
| Parameter | Phenotypic Methods | Genotypic Methods |
|---|---|---|
| Time to Result | 16-24 hours (standard methods) [113] | 1-8 hours (PCR); 1-3 days (WGS) [113] [117] |
| Sensitivity | Detects functional resistance regardless of mechanism [112] | 93.4% for predicting phenotypic resistance [117] |
| Specificity | High for detectable growth inhibition [114] | 99.8% for predicting phenotypic resistance [117] |
| Mechanism Detection | Indirect, based on growth response [112] | Direct identification of resistance genes/mutations [112] |
| Novel Mechanism Detection | Possible through abnormal growth patterns [112] | Requires known database matches or advanced analysis [117] |
| Automation Potential | Moderate (automated systems available) [113] | High (high-throughput sequencing platforms) [113] |
Method-Specific Advantages and Limitations
Each resistance detection approach presents distinct advantages and limitations that influence their application in research and clinical settings. Phenotypic methods provide functional assessment of resistance that directly informs therapeutic decisions, detect resistance regardless of genetic mechanism, and represent the current gold standard for AST with established interpretive criteria [112] [114]. However, these methods are limited by prolonged turnaround times (16-24 hours), inability to detect silent resistance genes, dependence on bacterial growth conditions, and limited sensitivity for heteroresistance or slow-growing organisms [113] [114].
Genotypic methods offer rapid detection of resistance mechanisms, capacity to identify resistance before phenotypic expression, comprehensive analysis of all known resistance determinants in a single test (WGS), and ability to track resistance transmission through plasmid and mobile element analysis [117] [115]. The limitations include inability to detect novel resistance mechanisms not present in databases, potential discordance between genotype and phenotype due to regulation or expression, higher equipment and computational requirements, and challenges in interpreting the clinical significance of newly identified genetic determinants [112] [117].
Table 2: Applications and Limitations of Resistance Detection Methods
| Method Category | Specific Applications | Key Limitations |
|---|---|---|
| Disk Diffusion | Routine susceptibility testing, resistance surveillance, epidemiological studies [114] | No MIC value, subjective interpretation, standardized inoculum required [114] |
| Broth Microdilution | Reference AST, MIC determination, drug development studies [113] [116] | Labor-intensive, higher cost, defined antibiotic panels only [113] |
| Gradient Diffusion | Fastidious organisms, individual antibiotic testing, MIC estimation [114] | Higher cost per test, limited antibiotic availability [114] |
| PCR-Based Methods | Rapid screening of specific resistance markers, outbreak investigation, surveillance [113] | Limited to targeted genes, primer specificity issues, false negatives with novel variants [113] |
| Whole-Genome Sequencing | Comprehensive resistance gene identification, novel mechanism discovery, transmission tracking [117] | High cost, bioinformatics expertise required, database-dependent [117] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for Resistance Detection Studies
| Reagent/Material | Application | Function | Examples/Specifications |
|---|---|---|---|
| Mueller-Hinton Agar | Phenotypic testing | Culture medium for disk diffusion and MIC testing | Standardized according to CLSI/EUCAST guidelines [114] |
| Cation-Adjusted Mueller-Hinton Broth | Broth microdilution | Liquid medium for MIC determination | Essential for accurate aminoglycoside and tetracycline testing [113] |
| Antibiotic Disks | Disk diffusion | Source of antibiotic diffusion | Commercially available with standardized antibiotic concentrations [114] |
| Sensititre AVIAN1F Plates | Broth microdilution | Pre-configured antibiotic panels | Contains multiple antibiotics with serial dilutions [117] |
| DNA Extraction Kits | Genotypic methods | Nucleic acid purification | Qiagen DNeasy Blood & Tissue Kit [117] |
| PCR Master Mix | PCR-based detection | Amplification of target genes | Contains DNA polymerase, dNTPs, buffer, MgClâ‚‚ [113] |
| Primer Sets | PCR-based detection | Specific amplification of resistance genes | Targeted to common resistance genes (e.g., blaCTX-M, mecA, vanA) [113] |
| Sequencing Kits | Whole-genome sequencing | Library preparation and sequencing | Illumina DNA Prep kit, MiSeq reagent kits [117] |
| Bioinformatics Tools | WGS data analysis | Resistance gene identification | CARD, ResFinder, GalaxyTrakr [117] |
Integrated Approaches and Future Directions
The integration of phenotypic and genotypic approaches represents the most powerful strategy for comprehensive resistance detection and understanding. Combined methodologies leverage the functional relevance of phenotypic testing with the mechanistic insights of genotypic analysis, providing a complete picture of resistance profiles [112] [117]. This integrated approach is particularly valuable for detecting discordance between genotype and phenotype, which may reveal novel resistance mechanisms or regulatory effects [112]. For instance, a 2024 study on Salmonella isolates identified 15 instances where isolates were phenotypically resistant but genotypically susceptible, prompting investigation into undefined resistance mechanisms [117].
Emerging technologies are bridging the gap between traditional phenotypic and genotypic methods. Machine learning approaches applied to comprehensive surveillance datasets (e.g., Pfizer ATLAS) demonstrate potential for predicting resistance patterns from both phenotypic and genotypic data [115]. Advanced platforms such as MALDI-TOF mass spectrometry, CRISPR-based diagnostics, and microfluidics-enabled AST are reducing turnaround times while providing complementary phenotypic and genotypic information [113] [114]. The ongoing reduction in sequencing costs and development of rapid point-of-care molecular tests will further transform resistance detection paradigms, potentially enabling real-time resistance profiling directly from clinical samples [113] [114].
For researchers and drug development professionals, the selection between phenotypic and genotypic methods should be guided by specific application requirements, available resources, and intended use cases. Phenotypic methods remain indispensable for establishing functional resistance and validating the clinical relevance of genetic determinants, while genotypic approaches provide unprecedented insights into resistance mechanisms and transmission dynamics. As both technologies continue to evolve, their synergistic application will be essential for addressing the ongoing challenge of antimicrobial resistance across clinical, agricultural, and environmental settings.
Conclusion
The comparison between culture-based and molecular methods reveals a complementary rather than replacement relationship in modern diagnostics. While molecular methods offer unprecedented speed, sensitivity, and the ability to detect uncultivable or fastidious pathogens, culture remains indispensable for phenotypic antibiotic susceptibility testing, broader pathogen discovery, and providing viable isolates for further research. The future lies in integrated diagnostic workflows that leverage the strengths of both approaches, supported by AI-driven data analysis, point-of-care molecular platforms, and robust laboratory informatics. For researchers and drug development professionals, this synergy will accelerate pathogen discovery, enhance antimicrobial development, and ultimately advance personalized medicine through more precise infectious disease management.
References
- 1. Diagnostic performance of the direct stool Xpert Carba-R ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12523156/]
- 2. Comparison Between a Multiplex Real-Time PCR Method ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12427671/]
- 3. Head-to-head comparison of culture-based and direct-from ... [https://www.sciencedirect.com/science/article/pii/S295059092500040X]
- 4. Molecular diagnostic technology: beyond analytical accuracy [https://pubmed.ncbi.nlm.nih.gov/40847349/]
- 5. Molecular diagnostic technology: beyond analytical accuracy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12374334/]
- 6. Next-generation rapid phenotypic antimicrobial ... [https://www.nature.com/articles/s41467-024-53930-x]
- 7. Clinical Microbiology in the Year 2025 - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC139721/]
- 8. Rapid Phenotypic and Genotypic Antimicrobial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11351821/]
- 9. A comparison of different DNA extraction methods and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8500797/]
- 10. Benefits and drawbacks of molecular techniques for diagnosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7166422/]
- 11. Comparison and Evaluation of Antimicrobial Susceptibility ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC88426/]
- 12. Comparison evaluation of bacterial DNA extraction ... [https://www.nature.com/articles/s41598-025-87225-y]
- 13. Comparison of Pathogen DNA Isolation Methods from Large ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0072349]
- 14. Comparison of Three Rapid AST System [https://www.rapidmicrobiology.com/journal-club/comparison-of-three-rapid-antimicrobial-susceptibility-testing-systems]
- 15. Experts See 17 Laboratory Trends Dominating 2025 [https://clpmag.com/diagnostic-technologies/experts-see-17-laboratory-trends-dominating-2025/]
- 16. Comparison of boiling versus magnetic bead techniques in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12613369/]
- 17. Comparative evaluation of various DNA extraction methods ... [https://bmcbiotechnol.biomedcentral.com/articles/10.1186/s12896-024-00933-7]
- 18. A Comparison of Three Automated Nucleic Acid Extraction ... [https://www.mdpi.com/2076-2607/12/12/2417]
- 19. Comparison of PCR with Other Nucleic Acid Amplification ... [https://www.mybiosource.com/learn/comparison-of-pcr-with-other-nucleic-acid-amplification-techniques/]
- 20. 2025 and Beyond: The Future of Genomic Data Analysis ... [https://blog.crownbio.com/2025-and-beyond-the-future-of-genomic-data-analysis-and-innovations-in-genomics-services]
- 21. DNA Sequencing: How to Choose the Right Technology [https://frontlinegenomics.com/dna-sequencing-how-to-choose-the-right-technology/]
- 22. Next Generation Sequencers Market Forecast Report 2025 ... [https://finance.yahoo.com/news/next-generation-sequencers-market-forecast-080200693.html]
- 23. A comprehensive review on biofilm-associated infections [https://www.sciencedirect.com/science/article/pii/S2950194625002043]
- 24. Biofilms: structure, resistance mechanism, emerging control ... [https://pubs.rsc.org/en/content/articlehtml/2025/pm/d5pm00094g]
- 25. Bioactivity of microbial biofilms in extreme environments - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12446376/]
- 26. Microbial Biofilms: Where Are We and Where Are We Going? [https://pmc.ncbi.nlm.nih.gov/articles/PMC12351492/]
- 27. Persistent Threats: A Comprehensive Review of Biofilm ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12388178/]
- 28. Comparison of Culture and Molecular Identification ... [https://www.mdpi.com/1422-0067/13/3/2535]
- 29. Molecular Techniques Complement Culture-Based ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2019.00462/full]
- 30. The dual-species biofilm formed by Staphylococcus aureus ... [https://www.nature.com/articles/s41538-025-00581-x]
- 31. Application to Bacterial Biofilm Matrix Transcriptomics [https://link.springer.com/article/10.1007/s00284-025-04435-3]
- 32. Koch's postulates: from classical framework to modern app... [https://www.degruyterbrill.com/document/doi/10.1515/gme-2025-0006/html?srsltid=AfmBOoo2CPCe8LAfRUheXkYdCuWNgGVCuN5oExecX8vk_D1PKke62lGK]
- 33. 16.3: Koch Postulate and Molecular Koch Postulate [https://bio.libretexts.org/Courses/City_College_of_San_Francisco/Introduction_to_Microbiology_(Liu_et_al.)/16%3A_Microbial_Mechanisms_of_Pathogenicity/16.03%3A_Koch_Postulate_and_Molecular_Koch_Postulate]
- 34. Genomic medicine and personalized treatment: a narrative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11981433/]
- 35. Comparing culture and molecular methods for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5100109/]
- 36. Comparing and Contrasting Traditional and Molecular ... [https://blog.microbiologics.com/comparing-and-contrasting-traditional-and-molecular-methods-in-clinical-microbiology/]
- 37. What does it take to satisfy Koch's postulates two centuries ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3775492/]
- 38. Revisiting Koch's postulates: A tailored approach for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12105784/]
- 39. Next-generation microbiology: from comparative genomics to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8082670/]
- 40. Is it time to substitute culture with molecular diagnostics for ... [https://www.thermofisher.com/blog/clinical-conversations/is-it-time-to-substitute-culture-with-molecular-diagnostics-for-infectious-diseases/]
- 41. Comparative Diagnostic Evaluation of Real-Time PCR and ... [https://www.medrxiv.org/content/10.1101/2025.08.26.25334225v1.full-text]
- 42. 微生物å¦æ ‡å‡† [https://www.sigmaaldrich.com/SG/zh/products/analytical-chemistry/reference-materials/microbiology-standards?srsltid=AfmBOoob7Qhfc9FTXfI_lVK4StuVeSRW3G_LVfBvaUc4nkk7MvD4619e]
- 43. Real-time PCR has advantages over culture-based methods ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10000296/]
- 44. Comparison of qPCR and chromogenic culture methods for ... [https://www.sciencedirect.com/science/article/pii/S2352551724000817]
- 45. qPCR vs Culture Testing: Speed, Accuracy & Use-Cases [https://devlabwerks.com/qpcr-vs-culture-which-respiratory-pathogen-test-fits-your-diagnostic-needs/]
- 46. Comparison of traditional culture and molecular qPCR for ... [https://www.nature.com/articles/s41598-017-04915-y]
- 47. Is qPCR More Accurate Than PCR? | PHCbi [https://www.phchd.com/eu/biomedical/knowledge-base/is-qpcr-more-accurate-than-pcr]
- 48. Molecular techniques v. conventional culture: Should there ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12490501/]
- 49. Comparison and Sensitivity Evaluation of Three Different ... [https://pubmed.ncbi.nlm.nih.gov/34372527/]
- 50. Metagenomic Next-Generation Sequencing in Infectious ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384723/]
- 51. Advances in whole genome sequencing for foodborne ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2025.1593219/full]
- 52. Whole-Genome Sequencing in Outbreak Analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4399107/]
- 53. next-generation sequencing for infectious-disease ... [https://www.jci.org/articles/view/178003]
- 54. Lessons from 5 Years of Routine Whole-Genome ... [https://wwwnc.cdc.gov/eid/article/31/13/24-1950_article]
- 55. Real-time sequencing a promising tool for hospital ... [https://www.cidrap.umn.edu/healthcare-associated-infections/real-time-sequencing-promising-tool-hospital-outbreak-detection]
- 56. Benchmarking metagenomic binning tools on real datasets ... [https://www.nature.com/articles/s41467-025-57957-6]
- 57. A head-to-head comparison of three MALDI-TOF mass ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10595064/]
- 58. Emerging Microtechnologies and Automated Systems for ... [https://www.sciencedirect.com/science/article/pii/S2472630322013516]
- 59. The Applications of MALDI-TOF MS in the Diagnosis ... [https://www.mdpi.com/2076-3417/15/14/7863]
- 60. One-Pot Isothermal LAMP-CRISPR-Based Assay for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9430409/]
- 61. Diagnosis of Infectious Diseases by CRISPR/Cas System [https://www.lidsen.com/journals/genetics/genetics-09-02-289]
- 62. The Crucial Role of Automated MALDI-TOF Mass ... [https://www.aurorabiomed.com/streamlining-clinical-diagnosis-the-crucial-role-of-automated-maldi-tof-mass-spectrometry-sample-preparation/?srsltid=AfmBOoqLTLAx9OUU4qslvkuQe3YAm_FW4MrRn0I0iIbKvkpa66GUCjNj]
- 63. Comparative performance of two automated machine learning ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0263954]
- 64. A comparison of two MALDI-TOF MS based assays for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11544138/]
- 65. Comparison of Culture and Molecular Identification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3317672/]
- 66. Molecular Diagnostic Methods Versus Conventional Urine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9459428/]
- 67. Global antibiotic resistance surveillance report 2025 [https://www.who.int/publications/i/item/9789240116337]
- 68. Molecular Methods for Detection of Antimicrobial Resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC11687549/]
- 69. Twenty-first century molecular methods for analyzing ... [https://www.sciencedirect.com/science/article/abs/pii/S0167701221000427]
- 70. Molecular diagnostic technology: beyond analytical accuracy [https://ccforum.biomedcentral.com/articles/10.1186/s13054-025-05620-3]
- 71. Molecular Methods for Identification and Quantification of ... [https://www.mdpi.com/1420-3049/27/23/8262]
- 72. Molecular methods for pathogen and microbial community ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7106020/]
- 73. Performance Comparison of Three Molecular Diagnostic ... [https://www.mddionline.com/ivd/performance-comparison-of-three-molecular-diagnostic-test-systems]
- 74. Detection limitations of bacteria in tissue samples - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12178716/]
- 75. Performance Comparison of Two In-House PCR Methods ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11899361/]
- 76. Keep the Hospital Clean: Diagnostic Performance of Ten ... [https://link.springer.com/article/10.1007/s11046-025-00944-8]
- 77. A Comparison of Molecular Methods for Microbial Testing [https://krakensense.com/blog/a-comparison-of-molecular-methods-for-microbial-testing]
- 78. Challenges and strategies in building a foundational digital ... [https://www.frontiersin.org/journals/health-services/articles/10.3389/frhs.2025.1600689/full]
- 79. The Use of Big Data in Personalized Healthcare to Reduce ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11051308/]
- 80. Guide to LIMS: Core Functions & 2025 System Comparison [https://intuitionlabs.ai/articles/lims-system-guide-2025]
- 81. Top lab trends for 2025 | LabLeaders [https://diagnostics.roche.com/global/en/article-listing/lab-leaders/article/top-lab-trends-2025.html]
- 82. 50+ Workflow Automation Stats & Trends You Can’t Ignore in 2025 - 26 [https://kissflow.com/workflow/workflow-automation-statistics-trends/]
- 83. What are the best software solutions for managing lab ... [https://www.scispot.com/blog/what-are-the-best-software-solutions-for-managing-lab-workflows]
- 84. How to Evaluate Non-Growing Cells—Current Strategies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7912045/]
- 85. Rapid, season-specific PCR testing versus traditional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12318422/]
- 86. Clinical utility of PCR compared to conventional culture ... [https://pubmed.ncbi.nlm.nih.gov/39671979/]
- 87. Clinical Relevance of PCR Versus Culture in Urinary Tract ... [https://www.mdpi.com/2075-4418/15/15/1939]
- 88. Prospective evaluation of real-world performance and ... [https://pubmed.ncbi.nlm.nih.gov/39998242/]
- 89. Beyond Cultures: The Evolving Role of Molecular ... [https://www.mdpi.com/2077-0383/14/19/6886]
- 90. Evaluating the feasibility, sensitivity, and specificity of next- ... [https://pubmed.ncbi.nlm.nih.gov/39812555/]
- 91. Antimicrobial drug susceptibility testing for the ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1626930/full]
- 92. Evaluation of direct-to-PCR (D2P) method for molecular ... [https://www.sciencedirect.com/science/article/pii/S001448002500022X]
- 93. Influence of Antimicrobial Stewardship and Molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8549744/]
- 94. A Comparative Study of Traditional and Molecular Methods ... [https://www.ijfmr.com/research-paper.php?id=54059]
- 95. A 'culture' shift: Application of molecular techniques for ... [https://www.sciencedirect.com/science/article/abs/pii/S0734975019300321]
- 96. State of the Art of Antimicrobial and Diagnostic ... [https://www.mdpi.com/2079-6382/14/2/132]
- 97. The Clinical Impact of Rapid Molecular Microbiological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7528559/]
- 98. World One Health Day: A new review charts a practical ... [https://www.doherty.edu.au/news-events/news/world-one-health-day-review-charts-practical-path-antimicrobial-stewardship]
- 99. Comparison of microbial culture, metagenomic next ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12343261/]
- 100. Clinical utility of PCR compared to conventional culture ... [https://www.sciencedirect.com/science/article/pii/S0732889324004255]
- 101. Systematic review Performance of molecular tests for ... [https://www.sciencedirect.com/science/article/pii/S1198743X24005937]
- 102. Recent Advances in the Use of Molecular Methods for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9229729/]
- 103. Biochemical and Culture-based Approaches to Identification ... [https://clsjournal.ascls.org/content/32/4/166]
- 104. A 'Culture' Shift: Application of Molecular Techniques for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6447436/]
- 105. Molecular Approaches to Diagnosing and Managing ... [https://wwwnc.cdc.gov/eid/article/7/2/70-0312_article]
- 106. An Approach to Include the Cost of Consumables ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11536279/]
- 107. Economic Evaluation of Molecular Testing for Pulmonary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12497363/]
- 108. Laboratory Equipment Market is expected to generate a ... [https://finance.yahoo.com/news/laboratory-equipment-market-expected-generate-144500542.html]
- 109. Cost Analysis of Strategies to Reduce Blood Culture ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4100213/]
- 110. Cost-benefit analysis of two quality control approaches for ... [https://www.sciencedirect.com/science/article/abs/pii/S0031302525001072]
- 111. Cost-Effectiveness of Molecular Method Diagnostic for ... [https://www.sciencedirect.com/science/article/pii/S2212109921001163]
- 112. What Is The Difference Between Phenotypic Versus ... [https://www.idstewardship.com/difference-phenotypic-versus-genotypic-resistance/]
- 113. Detection of antimicrobial resistance via state-of-the-art ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11893576/]
- 114. Detecting antibiotic resistance: classical, molecular ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1673343/full]
- 115. Prediction of antibiotic resistance from ... [https://www.nature.com/articles/s41598-025-14078-w]
- 116. Comparative Analysis of Phenotypic and Genotypic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12466733/]
- 117. Comparison of genotypic and phenotypic antimicrobial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11185115/]
- 118. Phenotypic and genotypic characterization of antibiotic- ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1649307/full]